Abstract
Aim:
To assess the changes in corneal hysteresis (CH) and corneal resistance factor (CRF) 1-year following transepithelial corneal collagen cross-linking (CXL) treatment in eyes of children with keratoconus.
Methods:
This case series was conducted in 22 eyes of 22 children. Children aged < 18 years with progressive keratoconus were included. They were treated with transepithelial CXL. Corneal biomechanical and anterior chamber parameters such as CH, CRF, and peak 1 were noted using ocular response analyzer, Pentacam, intraocular lens master, and anterior segment optical coherence tomography before and 1, 3, 6, and 12 months after treatment.
Results:
Our series had 22 eyes of 22 children with a mean age 15.7 ± 2.1 years. The CH and CRF 1-year after treatment declined (difference of mean 0.1 mmHg (95% confidence interval [CI] 0.04–0.24), P = 0.2] and (difference of mean 0.1 mmHg [95% CI 0.04–0.30], P = 0.3), respectively. Peak 1 and peak 2 increased (difference of mean 0.1 mmHg [95% CI 0.006–0.008], P = 0.2) and (difference of mean 0.1 mmHg [95% CI 0.007–0.006], P = 0.3), respectively. The uncorrected distance visual acuity improved from 0.95 ± 0.34 logMAR to 0.68 ± 0.45 logMAR (P < 0.05). No statistically significant changes during 12 months follow-up were observed in axial length, corneal volume, anterior chamber volume, and anterior chamber depth (P > 0.05).
Conclusion:
Transepithelial CXL in keratoconus in pediatric age group seems to have good stability in corneal biomechanical parameters after 1-year. Further studies with a larger sample and better study design are recommended to confirm our findings.
Keywords: Corneal Hysteresis, Corneal Resistance Factor, Pediatric Keratoconus, Transepithelial Corneal Cross Linking
INTRODUCTION
Corneal biomechanical properties are usually evaluated for research purpose. Introduction of ocular response analyzer (ORA) provided a simple but reliable method to assess the cornea in clinical settings as well.1
Keratoconus is a noninflammatory disease, which affects mainly the central cornea and leads both anatomical and biomechanical changes in corneal tissue.2 Corneal hysteresis (CH) and corneal resistance factor (CRF) are biomechanical markers that are measured using ORA and decline in cornea with keratoconus compared to the healthy corneas.3,4 The eye with keratoconus, as a result, become more elastic and less rigid than normal eyes.5 The biomechanical properties of the cornea are primarily determined by the collagen fibers within the stroma and degree of interfibrillar linkage.6 The visual acuity (VA) due to irregular astigmatism and corneal scarring, the VA declines.
Transepithelial collagen cross-linkage (CXL) is a widely used method to increase the mechanical stiffness of the cornea. The stability of CH in adult eyes with keratoconus was demonstrated by using biomechanical strain measurements.7,8 This treatment modality is also introduced for children with keratoconus.9,10 However, to the best of our knowledge, corneal biomechanical changes and anterior segment changes in eyes of children with keratoconus.
To treat children with keratoconus, transepithelial CXL is preferred as it is technically simpler and less invasive than epithelial off CXL and has less postoperative pain and corneal haze.7,8
We studied the stability of transepithelial CXL treatment over time using changes in CH and CRF as indicators for biomechanical changes in the corneal tissue of children with keratoconus. We also assessed changes in VA and different corneal and anterior chamber parameters.
METHODS
This case series was conducted between May 2012 and October 2013 focusing on children aged <18 years and with progressive keratoconus. The study was approved by the hospital medical and ethical committees. After receiving a detailed description of the nature of the treatment, all patients’ legal guardians provided written informed consent.
Children with a corneal thickness of at least 400 μm at the thinnest point of keratoconus were included. Progressive keratoconus was defined as one or more of the following changes over a period of 24 months: If in 24 months, there was increase of >1 diopter (D) in the steepest keratometry, an increase in >1 D in manifest cylinder or an increase >0.5 D in manifest refractive spherical equivalent, we considered keratoconus to be of progressive nature.
Eye with corneal thickness of <400 um at the thinnest point, history of viral keratitis, severe dry eye, concurrent corneal infection, central or paracentral corneal opacities, previous ocular surgery, and contact lens wear for fewer than 4 weeks before baseline examination were excluded from the study.
Patients were evaluated before and 1, 3, 6, and 12 months after transepithelial CXL.
A complete ophthalmologic evaluation included Slit lamp biomicroscopic (name of slit lamp and country) and fundus examination (name of the instrument, company, and country). The corneal and anterior chamber evaluation was also conducted using Scheimpflug imaging device (Oculus Pentacam, Optikgerate GmbH, Wetzlar, Germany). The axial length (AL) was measured with an intraocular lens Master (Carl Zeiss Meditec, Jena, Germany) and corneal optical coherence tomography (OCT), (Visante OCT, Carl Zeiss Meditec, Jena, Germany) and evaluation of the biomechanical properties of the cornea with ORA (ORA; Reichert Ophthalmic Instruments, Buffalo, NY, USA). Pain assessment was done postoperatively with visual analogue scale.
As specified by Touboul et al.11 using a bidirectional applanation measurement, the ORA was able to present four different parameters:
CH which is the difference between inward applanation amplitude peak 1 and outward applanation amplitude peak 2 (P1–P2), which is related to the viscous dampening property of the corneal tissue which is likely linked to the stromal collagen nature and state of hydration12
CRF which is indicative of the overall resistance of the cornea and is calculated using a linear combination of peak 1 and peak 2 (P1–kP2), and more heavily weighted by the underlying corneal elastic properties13
Corneal compensated intraocular pressure (IOPcc) and Goldmann correlated intraocular pressure (IOPg) measurement is strongly correlated with Goldmann tonometry and is also calculated using a specific linear combination of peak 1 and peak 213
Amplitude of the peaks (peak 1 and peak 2) is a function of how much light hits the infrared detector during each applanation event and it is corresponding to the first inward applanation event, and the second inward applanation event, respectively.14
In order to ensure accurate results, ORA was done 4 times for each eye, by the same operator. Signals that differ significantly in appearance from the other signals from the same eye were deleted.
Transepithelial CXL is similar to Dresden protocol (epithelium – off) in conventional CXL but we used epithelium – on technique without removal of the epithelium and with the use of transepithelial riboflavin (Ricrolin TE, riboflavin 0.1 %, SOOFT, oofta, Italia) which is currently available as a formula containing riboflavin 0.1% and enhancers. The presence of the amino alcohol improves bioavailability and, in combination with enhancers such as ethylenediaminetetraacetic acid disodium salt, enables transepithelial penetration through the intact corneal epithelium. Postoperative treatment comprised moxifloxacin 0.5% eye drops, diclofenac 0.1% eyedrops (Voltaren), and lubricant eye drops (Tears Naturale, Alcon Laboratories, Inc., UK) for 1-month. The recommended dose for all drops was 4 times daily.
Primary outcome measures: Changes from baseline in CH, CRF, and peak 1.
Failure of treatment was considered if there was loss of one or more line of VA, progression of K reading >1 D in the steepest keratometry, an increase in >1 D in manifest cylinder or an increase >0.5 D in manifest refractive spherical equivalent after 12 months of follow-up.
All data were recorded in preformatted data collection forms and analyzed. Statistical calculations were performed using SPSS software (version 21.0, SPSS Inc., NY, USA). The Student's t-test for paired data was used to compare preoperative data and postoperative data. The results were considered statistically significant at P < 0.05 and highly significant at P < 0.001. Biomechanical, pachymetric, VA, and refractive values were compared between baseline and postoperative examination and analyzed. To analyze the possible correlation of central corneal thickness (CCT), CXL outcomes, OCT, and ORA measurements, Pearson correlation coefficients were used.
RESULTS
We had 22 eyes of 22 patients in our series. The mean age of the 18 boys and 4 girls was 15.7 ± 2.1 years (range: 13–18 years). The mean follow-up was 15.0 ± 3.4 months (range: 12–16 months).
IOPcc, IOPg, CH, and CRF are shown in Table 1. The differences between baseline and 12 months postoperatively were not statistically significant for all parameters (P > 0.05). They had all significantly increased at 1-month follow-up (P < 0.05). Peak 1 and peak 2 were statistically significant changed from 1-month to 12 months of follow-up (P < 0.05).
Table 1.
Preoperative and postoperative ORA and refractive data after transepithelial CXL
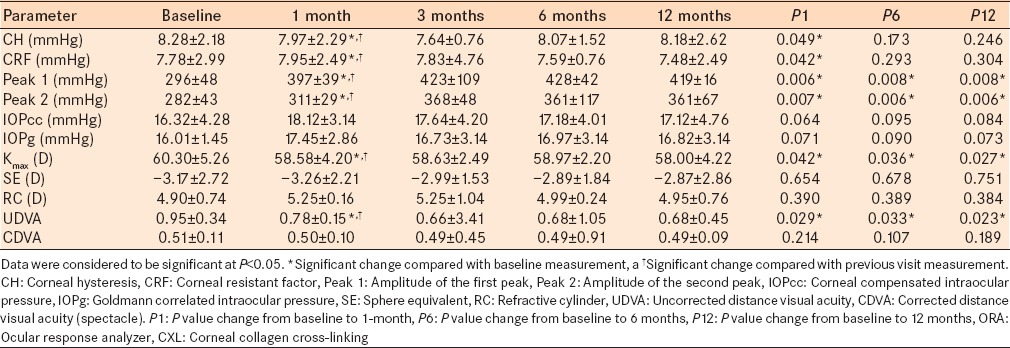
12 months after transepithelial CXL, the mean improvement in the uncorrected distance visual acuity (UDVA) was 0.27 logMAR (P < 0.05). All eyes achieved a UDVA of 20/200 or better. There was a one-line improvement in UDVA of 13 eyes (59.1%). No eye lost lines of preoperative UDVA. There was no statistically significant change from the preoperative CDVA (P > 0.05). All eyes achieved a CDVA of 20/50 or better. In 4 eyes (18.18%), there was a 1-line improvement in CDVA. Figure 1 showed the changes in CH and CRF versus time in cross-linked keratoconic patients and Figure 2 showed the changes in VA versus time in cross-linked keratoconic patients.
Figure 1.
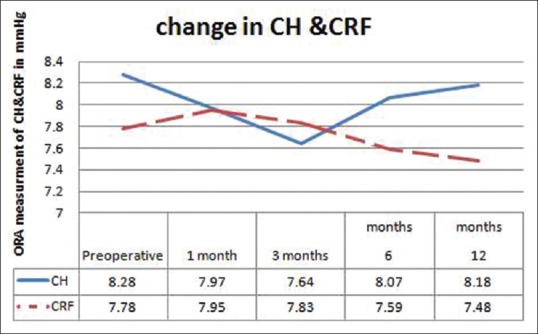
Change in corneal hysteresis and corneal resistant factor versus time in cross-linked keratoconic patients
Figure 2.
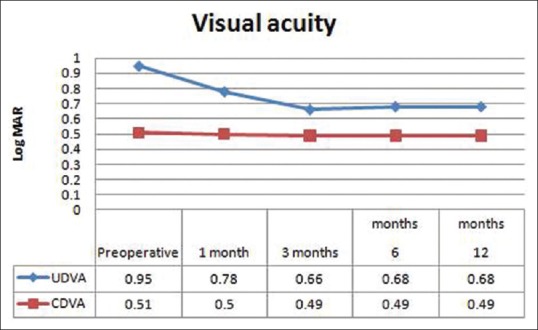
Change in visual acuity versus time in cross-linked keratoconic patients
The pachymetry map showed statistically significant change in CCT after 1-month (P = 0.04), but not after 12 months (P = 0.7) [Table 2]. The mean changes in the absolute curvature in maximum K values after 12 months was −2.3 ± 1.4 D (P < 0.05 give exact value). The thinnest location in the anterior elevation decreased 12 months after treatment (P < 0.05 give exact value). There was no significant change in the posterior elevation at the thinnest location (P > 0.05 give exact value).
Table 2.
Preoperative and postoperative anatomical data after transepithelial CXL
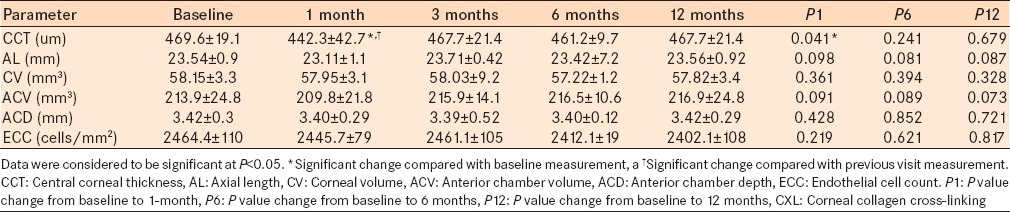
No statistically significant changes during 12 months follow-up were observed in AL, corneal volume (CV), anterior chamber volume (ACV), anterior chamber depth (ACD), and endothelial cell count (ECC) (P > 0.05) as shown in Table 2.
CH and CRF at baseline and 12 months were significantly correlated with CCT at baseline and 12 months, respectively (CHbaseline with CCTbaseline = 0.72, P < 0.001; CH12 with CCT12 = 0.53, P < 0.001; CRFbaseline with CCTbaseline = 0.63, P < 0.001; and CRF12 with CCT12 = 0.51, P < 0.001) [Table 2].
The changes in CH and CRF between baseline and 12 months were not correlated with the changes in UCVA (rCH= −0.06, P = 0.6; rCRF= −0.10, P = 0.4), CDVA (rCH = 0.03, P = 0.8; rCRF = 0.01, P = 0.9), or Kmax (rCH= −0.02, P = 0.8; rCRF = 0.02, P = 0.9).
There was no statistically significant difference in CCT in comparison with Pentacam measures in all the follow-up (P > 0.05). The mean depth of the corneal stromal demarcation line measured by the first observer was 202.61 ± 21.07 μm (range, 186–307 μm) centrally. Figure 3 showed the demarcation line in one cross-linked patients. The CXL demarcation line depth and change in CDVA (r = −0.16, P = 0.325) and change of the steepest keratometry at 6 months (r = 0.084, P = 0.637) were not correlated.
Figure 3.
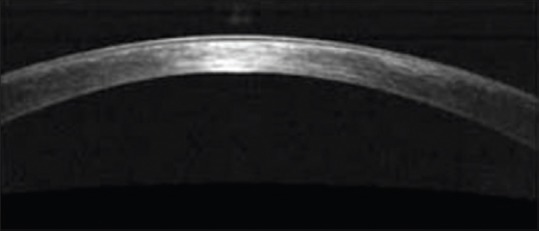
Corneal optical coherence tomography of one patient 6 months post transepithelial corneal collagen cross-linking with demarcation line at a depth of about 300 um
Postoperative pain was mild ranging from 0 to 2 which disappeared with a simple analgesic in the first 48 h.
DISCUSSION
Transepithelial CXL is a promising new treatment for stabilization and strengthening of the cornea in keratoconus in pediatric age group.9,10 No previous study evaluated the corneal biomechanical changes and anterior segment changes in keratoconus in pediatric age group.
In this study, the in vivo biomechanical measurements, CH and CRF remained unchanged 12 months after transepithelial CXL (P > 0.05) although they were both significantly increased at 1-month follow-up (P < 0.05). The lack of significant changes in CH and CRF after 12 months in our study with epithelium – on CXL on keratoconus on pediatric age group was consistent with previously reported ORA results in CXL in keratoconus which showed an increase in corneal biomechanical strength that occurred 1-month after epithelium-off CXL in adult.15,16 Of note, this was concomitant with the statistically significant correlation with corneal thinning that is seen 1-month post cross-linking. Thinner corneas seem to be correlated with lower CH and CRF values.
Absence of significant changes in CH and CRF after 12 months also might be explained by the change in stiffness which might be less than that which can be measured by the sensitivity of the ORA, or it might indicate that transepithelial CXL changed both elasticity and viscosity in a manner that was not detected by the viscoelastic parameters, CH, and CRF or due to change in collagen fiber orientation which becoming more regular as they are cross-linked.17 It is also possible that the biomechanical changes after transepithelial CXL are inherently different than those measured by CH and CRF, and therefore, these metrics may not capture the true biomechanical effect of transepithelial CXL over time. Penetration of the cross-linking is detected by demarcation line in anterior segment OCT. Stojanovic et al. found that the mean demarcation line with epithelium – on CXL was located at a depth of 317 um from the surface which is similar to that seen in epithelium – off CXL.18 This was comparable with the mean demarcation line depth in our study.
The pachymetry map showed a statistically significant reduction in CCT at 1-month followed by nonstatistically significant change in the CCT after 12 months (P > 0.05). This could correspond to the apoptosis that occurred after the treatment (1–3 months) followed by repopulation that occurred thereafter (6–12 months). Wollensak et al.19 found that this apoptotic cell death occurs after exposure to UVA light.
Peak 1 and peak 2 were statistically significant changed from 1-month to 12 months of follow-up (P < 0.05). The peak 1 and peak 2, have been shown to correspond to corneal stiffness which was known to increase significantly after transepithelial CXL.9,10 This was in agreement with other studies in transepithelial CXL in keratoconus in adult20 and conventional CXL.16,21,22
In our study, we found no correlation between ORA, VA, and topographic measurements. This might be related to two factors, the first may be a change in collagen fiber orientation with the collagen fibers becoming more regular as they are cross-linked which made stiffness of the superficial corneal layers that could halt the keratoconus progression and improve the regularity of the corneal surface. The second may be the correction of irregular astigmatism in the central area and equal reduction of the flat corneal meridian and steep corneal meridian, which resulted in a significant reduction in the spherical error without a significant change in the cylindrical error. This was in agreement with Caporossi et al.23
The mean change in the absolute curvature in maximum K value was − 2.3 ± 1.4 D which was statistically significant (P < 0.05). This finding was also addressed by Caporossi et al.23 who recorded a topographic mean reduction in dioptric power of 2.1 ± 0.13 D in the central 3.0 mm and Greenstein et al.24 The observed reduction in K value was probably the result of the increased biomechanical stability of the cornea after CXL.25
No statistically significant changes during 12 months follow-up were observed in AL, CV, ACV, ACD, and ECC (P > 0.05). This was in agreement with other studies of transepithelial CXL in the adult.20,21 This stability of AL and biomechanical corneal properties confirmed the effectiveness of transepithelial CXL treatment without affecting in a negative way the corneal elasticity.
IOPcc and IOPg did not change significantly over the 1st postoperative year (P > 0.05), except during the 1st postoperative month which was in agreement with other studies in adult.11,12,13,26 This may be due to measurement artifact resulting from corneal changes or true elevation of IOP, which return to normal range after 1-month with topical timolol 0.25 mg once daily eye drops.
In our study, no case recorded failure according to visual and topographic measures in the 1st year of follow-up.
CONCLUSION
Transepithelial CXL in keratoconus in pediatric age group has a good stability in corneal biomechanical parameters. A multicentre clinical trial with longer follow-up needed to study the persistent of this effect for a longer duration.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31:156–62. doi: 10.1016/j.jcrs.2004.10.044. [DOI] [PubMed] [Google Scholar]
- 2.Jafri B, Lichter H, Stulting RD. Asymmetric keratoconus attributed to eye rubbing. Cornea. 2004;23:560–4. doi: 10.1097/01.ico.0000121711.58571.8d. [DOI] [PubMed] [Google Scholar]
- 3.Shah S, Laiquzzaman M, Bhojwani R, Mantry S, Cunliffe I. Assessment of the biomechanical properties of the cornea with the ocular response analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci. 2007;48:3026–31. doi: 10.1167/iovs.04-0694. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz D, Piñero D, Shabayek MH, Arnalich-Montiel F, Alió JL. Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J Cataract Refract Surg. 2007;33:1371–5. doi: 10.1016/j.jcrs.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 5.Grewal DS, Brar GS, Jain R, Sood V, Singla M, Grewal SP. Corneal collagen crosslinking using riboflavin and ultraviolet - A light for keratoconus: One-year analysis using Scheimpflug imaging. J Cataract Refract Surg. 2009;35:425–32. doi: 10.1016/j.jcrs.2008.11.046. [DOI] [PubMed] [Google Scholar]
- 6.Boxer Wachler BS, Pinelli R, Ertan A, Chan CC. Safety and efficacy of transepithelial crosslinking (C3-R/CXL) J Cataract Refract Surg. 2010;36:186–8. doi: 10.1016/j.jcrs.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 7.Spadea L, Mencucci R. Transepithelial corneal collagen cross-linking in ultrathin keratoconic corneas. Clin Ophthalmol. 2012;6:1785–92. doi: 10.2147/OPTH.S37335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Filippello M, Stagni E, O’Brart D. Transepithelial corneal collagen crosslinking: Bilateral study. J Cataract Refract Surg. 2012;38:283–91. doi: 10.1016/j.jcrs.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 9.Saman AG. Transepithelial corneal collagen crosslinking for progressive keratoconus in a pediatric age group. J Cataract Refract Surg. 2013;39:1164–70. doi: 10.1016/j.jcrs.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 10.Magli A, Forte R, Tortori A, Capasso L, Marsico G, Piozzi E. Epithelium-off corneal collagen cross-linking versus transepithelial cross-linking for pediatric keratoconus. Cornea. 2013;32:597–601. doi: 10.1097/ICO.0b013e31826cf32d. [DOI] [PubMed] [Google Scholar]
- 11.Touboul D, Roberts C, Kérautret J, Garra C, Maurice-Tison S, Saubusse E, et al. Correlations between corneal hysteresis, intraocular pressure, and corneal central pachymetry. J Cataract Refract Surg. 2008;34:616–22. doi: 10.1016/j.jcrs.2007.11.051. [DOI] [PubMed] [Google Scholar]
- 12.Rouse EJ, Roberts CJ, Mahmoud AM. The measurement of biomechanical parameters as a function of peak applied pressure in the Reichert ocular response analyzer. Invest Ophthalmol Vis Sci. 2007;48:1247. [Google Scholar]
- 13.Luce DA. Methodology for cornea compensated IOP and corneal resistance factor for the Reichert ocular response analyzer. Invest Ophthalmol Vis Sci. 2006;47:2266. [Google Scholar]
- 14.Kerautret J, Colin J, Touboul D, Roberts C. Biomechanical characteristics of the ectatic cornea. J Cataract Refract Surg. 2008;34:510–3. doi: 10.1016/j.jcrs.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Goldich Y, Barkana Y, Morad Y, Hartstein M, Avni I, Zadok D. Can we measure corneal biomechanical changes after collagen cross-linking in eyes with keratoconus? – A pilot study. Cornea. 2009;28:498–502. doi: 10.1097/ICO.0b013e318190734d. [DOI] [PubMed] [Google Scholar]
- 16.Vinciguerra P, Albè E, Mahmoud AM, Trazza S, Hafezi F, Roberts CJ. Intra- and postoperative variation in ocular response analyzer parameters in keratoconic eyes after corneal cross-linking. J Refract Surg. 2010;26:669–76. doi: 10.3928/1081597X-20100331-01. [DOI] [PubMed] [Google Scholar]
- 17.Glass DH, Roberts CJ, Litsky AS, Weber PA. A viscoelastic biomechanical model of the cornea describing the effect of viscosity and elasticity on hysteresis. Invest Ophthalmol Vis Sci. 2008;49:3919–26. doi: 10.1167/iovs.07-1321. [DOI] [PubMed] [Google Scholar]
- 18.Stojanovic A, Chen X, Jin N, Zhang T, Stojanovic F, Raeder S, et al. Safety and efficacy of epithelium-on corneal collagen cross-linking using a multifactorial approach to achieve proper stromal riboflavin saturation. J Ophthalmol 2012. 2012 doi: 10.1155/2012/498435. 498435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wollensak G, Iomdina E, Dittert DD, Herbst H. Wound healing in the rabbit cornea after corneal collagen cross-linking with riboflavin and UVA. Cornea. 2007;26:600–5. doi: 10.1097/ICO.0b013e318041f073. [DOI] [PubMed] [Google Scholar]
- 20.Kilic A, Roberts CJ. Biomechanical and refractive results of transepithelial cross-linking treatment in keratoconic eyes. Int J Keratoconus Ectatic Corneal Dis. 2012;55:75–8. [Google Scholar]
- 21.Sedaghat M, Naderi M, Zarei-Ghanavati M. Biomechanical parameters of the cornea after collagen crosslinking measured by waveform analysis. J Cataract Refract Surg. 2010;36:1728–31. doi: 10.1016/j.jcrs.2010.06.056. [DOI] [PubMed] [Google Scholar]
- 22.Müller LJ, Pels E, Vrensen GF. The specific architecture of the anterior stroma accounts for maintenance of corneal curvature. Br J Ophthalmol. 2001;85:437–43. doi: 10.1136/bjo.85.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: The Siena eye cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 24.Greenstein SA, Fry KL, Hersh PS. Corneal topography indices after corneal collagen crosslinking for keratoconus and corneal ectasia: One-year results. J Cataract Refract Surg. 2011;37:1282–90. doi: 10.1016/j.jcrs.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 25.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 26.Piñero DP, Alio JL, Barraquer RI, Michael R, Jiménez R. Corneal biomechanics, refraction, and corneal aberrometry in keratoconus: An integrated study. Invest Ophthalmol Vis Sci. 2010;51:1948–55. doi: 10.1167/iovs.09-4177. [DOI] [PubMed] [Google Scholar]


