INTRODUCTION AND SCOPE
Carpal tunnel syndrome (CTS) is the most common peripheral nerve entrapment syndrome and frequently presents in working-aged adults. Its mild form causes ‘nuisance’ symptoms including dysaesthesia and nocturnal waking. At its most severe however it can significantly impair motor function and weaken pinch grip. This review will discuss the anatomy of the carpal tunnel and the clinical presentation of the syndrome as well as the classification and diagnosis of the condition. Carpal tunnel syndrome has a profile of well-established risk factors including individual factors and predisposing co-morbidities, which will be briefly discussed. However, there is a growing body of evidence for an association between carpal tunnel syndrome and various occupational factors, which will also be discussed. Management of carpal tunnel syndrome, conservative and surgical will be described. Finally, we will discuss the issue of safe return to work post carpal tunnel release surgery and the lack of evidence-based guidelines.
Keywords: Carpal tunnel syndrome, vibration, repetition, occupation, return to work
Anatomy of the carpal tunnel
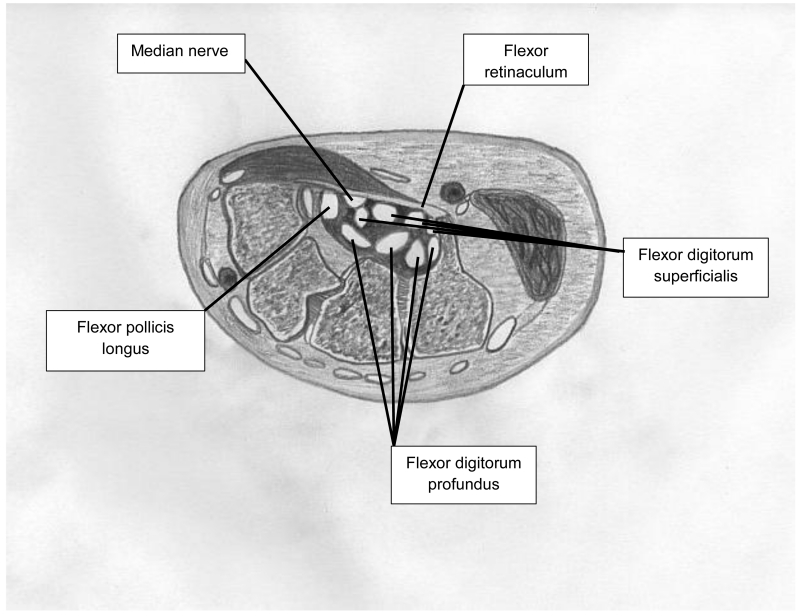
Found at the proximal palmar wrist, the carpal tunnel is defined by the pisiform and hook of the hamate medially and the tuberosities of the scaphoid and trapezium radially. Covering these four boney prominences is thick connective tissue (the flexor retinaculum) which creates a tunnel through which run the long flexor tendons (flexor digitorum profundus, flexor digitorum superficialis and flexor pollicis longus), maintaining them in place during wrist flexion (Figure 1). The median nerve is a major peripheral nerve of the upper limb. Its course takes it from the anterior compartment of the forearm through the carpal tunnel into the wrist, where it branches to provide motor supply to the thenar muscle group and sensory innervation to the palmar surface of the thumb, index, middle and radial half of ring finger. Carpal tunnel syndrome is caused when the canal is narrowed or the palmar tendons or tendon sheaths swell. Constriction in the canal impinges on the median nerve producing symptoms of disturbed sensation, typically in the radial 3½ digits but the symptoms may progress to cause wasting and weakness of the thenar muscles, resulting in weakened pinch grip.
Figure 1. Anatomical diagram of the carpal tunnel in transverse section.
Classification and diagnostic criteria
The typical presentation of carpal tunnel syndrome involves pain and/or dysaesthesia of the fingers (typically the radial 3½ digits but can be diffuse throughout the hand and can radiate proximal to the wrist). Symptoms are often worse at night or in the early morning. Examination in advanced cases may reveal wasting of the thenar eminence and/or weakness of thumb abduction. Provocation tests such as those of Tinel (tapping the flexor retinaculum) and Phalen (full passive flexion of the wrist for 1 minute) are widely used as confirmatory tests in clinical practice. However, the sensitivity and specificity of these tests seem to be much greater in patients with more advanced disease. Therefore, among people about to undergo carpal tunnel decompression, sensitivity and specificity have been shown to be excellent (88-100%) [1] but when the same tests are performed among patients with dysaesthesia in the general population [2-4], considerably poorer performance is found, at least when the ‘gold standard’ is nerve conduction studies. Similarly, electrophysiological nerve conduction tests have shown good diagnostic sensitivity (60-84%) and specificity of >95% among patients awaiting decompression where the ‘gold standard’ was operative relief of symptoms [5]. However, nerve conduction testing is not a perfect gold standard and false positives and negatives are well documented [6] and there is currently no consensus as to optimal technique, standardisation or normalisation for factors such as age, sex, height or skin temperature [7,8].
In clinical practice, the ‘classical’ case of carpal tunnel syndrome can be defined by a combination of symptoms, signs and nerve conduction testing. However, most studies of risk factors for carpal tunnel syndrome have taken place in workplace or population settings where cases are likely to be milder and neither the clinical provocation tests nor the nerve conduction tests (if available at all) have the same level of performance in regards to sensitivity/specificity. Therefore, the lack of a single valid and reliable diagnostic test has led to considerable heterogeneity in the case definitions used in epidemiological studies and it is more difficult to pool results or pool data and produce confident estimates of risk based upon systematic review or meta-analysis.
Differential Diagnosis
The main differential diagnoses of CTS are neuropathies. Cervical radiculopathies at C6-C7 may mimic the sensory symptoms, although in such cases motor involvement will be in the distribution of the radial nerve, affecting wrist flexion and triceps. Pain itself may be difficult to localise and the possibility of an ulnar or small fibre neuropathy should be considered for patients with neuropathic palmar digit pain, along with other causes of medial neuropathy. Wasting of the thenar muscles may also be caused by a T1 radiculopathy.
Rates of occurrence of carpal tunnel syndrome
Widely described as the most common mono-neuropathy, carpal tunnel syndrome has an estimated incidence of 99/100,000/year [9]. Dependent upon the case definition, prevalence rates in the general population have been estimated between 7-19% [4].
Individual risk factors for carpal tunnel syndrome
The results of almost all studies suggest that carpal tunnel syndrome occurs more commonly in women, with an annual incidence of 1.5 per 1000 compared to 0.5 per 1000 for men [10]. Gender also seems to exert an effect on incidence such that the incidence among women peaks aged 45-54 years (so that if a woman has not experienced symptoms by the time of her middle years, she seems to be less likely to experience them for the first time at an older age. In contrast, the incidence in men appears to continue to increase with age. The gender differences may be explained at least partly by hormonal factors as pregnant and breast feeding women have increased risk of carpal tunnel syndrome [11], as well as those in their first menopausal year, taking the oral contraceptive pill or taking hormone replacement therapy [12] and oophorectomy appears to reduce the incidence.
Body mass index and obesity are strongly associated with carpal tunnel syndrome, with every 1 unit increase in body mass increasing risk of the condition by 8% [11]. Some, but only a very small proportion, of excess cases are associated with endocrine conditions such as hypothyroidism, acromegaly and diabetes mellitus. Narrowing of the carpal tunnel canal e.g. through trauma or inflammation due to wrist fractures and inflammatory rheumatic disorders are also risk factors [12].
Carpal tunnel syndrome and its association with occupation
Over the past 20 years there have been a vast number of studies investigating the relationship between carpal tunnel syndrome and occupational activities. The number of studies is now so extensive that there have been a number of published systematic reviews of this literature [13-21]. In addition to the issues described above with classification criteria for CTS, another difficulty in interpreting the reviews has been the lack of standardisation of exposure classification in the individual studies. Very few studies have made in-depth analyses of movements involved in work activities as this is necessarily time-consuming and expensive and thus would need to be limited to few individuals. Exposure classification has therefore generally ranged from simple job titles through to self-reported workplace activities (e.g. repetitive bending/straightening the wrist ≥ 1 hour/day).
In 1992, Hagberg et al published a review of 21 studies including high quality information on occupational associations, and reported an increased risk of CTS in a number of jobs believed to involve repetitive and forceful gripping [13]. Later in the 1990s the US National Institute of Occupational Safety and Health (NIOSH) carried out a large systematic review of musculoskeletal disorders and workplace factors and included carpal tunnel syndrome as an outcome [14]. This too concluded that there was evidence of a positive association with work that involved highly repetitive movements of the hands, and a similar association with work involving forceful movements of the hands. The evidence was stronger if these exposures were combined. However, the reviewers found insufficient evidence that CTS was associated with extreme wrist postures. A third review from the same period (1998) by Abbas et al [15] also concluded that force and repetition were significant risk factors for CTS.
An updated review by Palmer et al in 2007 [16] partially addressed the difficulties with exposure classification, by analysing the 38 individual study reports either on a comparison of job titles, or the physical activities within the job. There were a wide range of occupational titles, including such diverse jobs as forestry workers, stone carvers, slaughterhouse workers, textile workers, dental hygienists and supermarket workers. These could however be divided into three broad classes; jobs entailing the use of vibratory tools, assembly work, and food processing and packing. Many of these occupations involve prolonged or repeated flexion and extension of the wrist. From this review, it was concluded that “there is a substantial body of evidence that prolonged and highly repetitious flexion or extension of the wrist materially increases the risk of carpal tunnel syndrome, especially when allied with a forceful grip.” It found reasonable evidence that regular prolonged use of hand-held vibratory tools was associated with more than double the risk of CTS. On the balance of evidence, it was concluded that the evidence did not demonstrate an important association with use of a computer keyboard and mouse. This association between computer work and CTS was further examined in reviews from 2008 by Thomsen et al [17] and from 2014 by Mediouni et al [18]. Both reviews concluded that there was insufficient epidemiological evidence that computer work causes CTS, although some particular work circumstances involving computer mouse use may be associated with CTS.
The systematic review published by van Rijn et al in 2009 [19] was conducted with the aim of providing a quantitative assessment of the exposure-response relationships between work-related physical and psychosocial factors and the occurrence of CTS. This examined a) associations of CTS with type of work, based on job descriptions, b) associations of CTS with five types of exposure - force, repetitiveness, hand-arm vibration, combined exposure measure and awkward postures, and c) associations of CTS with psychosocial risk factors. The authors found that jobs with the highest risk of CTS included work in the meat- and fish-processing industry, forestry work with chain saws and electronic assembly work. Exposure to high levels of hand-arm vibration, prolonged work with flexed or extended wrist, and high levels of hand force and repetitiveness were also associated with CTS. They concluded that CTS is associated with an average hand force of >4kg, repetitiveness at work with a cycle time <10 seconds, or >50% of cycle time performing the same movements, and a daily 8-hour energy-equivalent frequency-weighted acceleration of 3.9m/s2. No association was found between any psychosocial risk factor and CTS. Again, no clear association was found between computer work and CTS.
In a subsequent meta-analysis, based upon studies carried out between 1980 and 2009, Barcenilla et al [20], reviewed many of the studies included in the reviews above and an additional 14 more recent studies. Using a conservative definition of CTS that included nerve conduction abnormality with symptoms and/or signs, this study found risk factors significantly associated with an increased risk of CTS among workers to be:
vibration (3 studies, odds ratio (OR) 5.40, 95% confidence intervals (95%CI) 3.14-9.31)
hand force (5 studies, OR 4.23, 95%CI 1.53-11.68)
-
repetition (11 studies, OR 2.26, 95%CI 1.73-2.94)
and close to significance for:
combined exposure to both force and repetition (5 studies, OR 1.85, 95%CI 0.99-3.45).
The results of this review also suggested a non-significant association between CTS and wrist posture, based on three studies (OR 4.73, 95%CI 0.42-53.32), an association which has been investigated further in a meta-analysis published by You et al in 2014 [21]. This pooled analysis from nine studies demonstrated a doubling of risk of CTS with increased exposure to wrist extension/flexion (relative risk (RR) 2.01, 95%CI 1.66-2.43).
Compensation for carpal tunnel syndrome among workers in the UK
In the UK, the Industrial Injuries Disablement Benefit is a no-fault compensation scheme payable to employed earners in relation to disablement from occupational accidents or prescribed diseases. Carpal tunnel syndrome is a ‘prescribed’ disease under this scheme for people exposed to occupations which involve the use of hand-held powered vibratory tools (and whose symptoms started whilst working in this occupation) and/or perform repeated palmar flexion and dorsiflexion for at least 20 hours /week over at least 12 months in the 24 months prior to the onset of symptoms [22]. A range of different compensation schemes and arrangements apply across Europe and the reader is encouraged to familiarise themselves with the schemes applicable to their practice.
Management of carpal tunnel syndrome
The initial management of CTS is conservative. A number of conservative options have been tried, including wrist splinting, local and systemic corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), diuretics, ultrasound,
Wrist splinting
Nocturnal splinting to hold the wrist in a neutral position is widely advocated. Interestingly however, this strategy is relatively poorly evidence-based, at least as reported in a 2012 review by the Cochrane collaboration who found that despite 19 studies including almost 1200 participants overall, there was limited evidence that a nocturnal splint was more effective than no treatment in the short term [23]. They also reported that there was insufficient evidence regarding the effectiveness and safety of one splint design or wearing regimen over others and of splinting over the use of other non-surgical interventions for CTS. However, in their systematic review published in 2007, Piazzini and colleagues concluded that there was ‘moderate’ evidence for splinting, particularly if used full-time [24]. It should however be borne in mind that it is very difficult to design a trial to rigorously test the effectiveness of splints when traditional ‘blinding’ of participants is so obviously challenging.
Diuretics and NSAIDs
The evidence does not support specific use of non-steroidal anti-inflammatory drugs [25] or diuretics [24].
Oral corticosteroids
Short-term oral corticosteroids have been shown to be effective for the symptomatic treatment of CTS over two weeks and four weeks of follow-up [26]. However, the side effects of oral corticosteroids and their toxicity profile are such that this is not a recommended therapeutic option in all but the rarest clinical circumstances.
Local corticosteroid injection
According to a review by the Cochrane collaboration including 12 trials involving 651 participants, local corticosteroid injection produced greater clinical improvement in symptoms than placebo after one month [27]. However, they found insufficient evidence of symptom relief beyond one month. Local corticosteroid injection provided significantly greater clinical improvement than oral corticosteroid for up to three months. When compared with anti-inflammatories over 8 weeks of follow-up, there was no evidence that local corticosteroid injection improved clinical outcome. Two local corticosteroid injections did not provide significant added clinical benefit when compared to one injection.
Ultrasound
Pooled data from two trials involving 63 participants failed to show any significant benefit of ultrasound treatment over two weeks of follow-up [26]. However, in another trial, significant symptom improvement was demonstrated after seven weeks of ultrasound (which was maintained at six months) [28].
Carpal tunnel release surgery
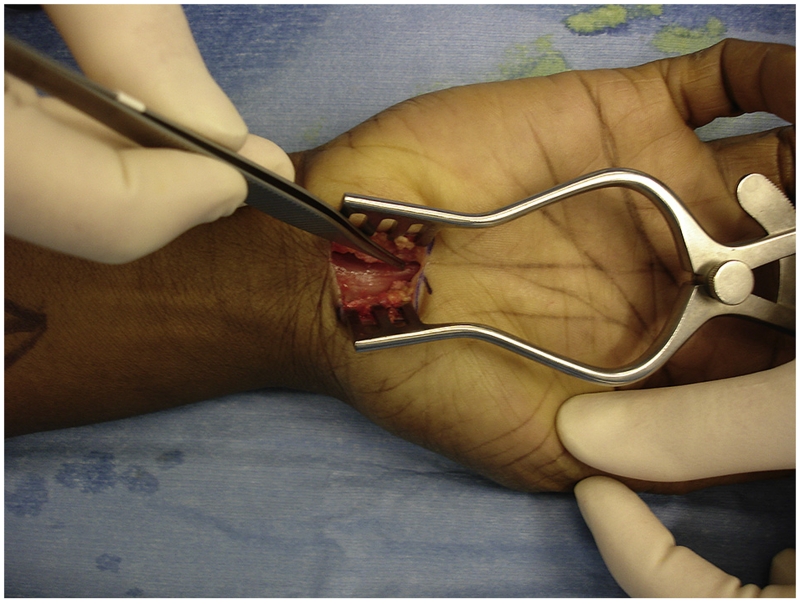
Surgical release of the carpal tunnel is recommended for severe cases of CTS, such as when there is thenar muscle wasting or weakness of thumb opposition, or when conservative management has failed [29]. The first open surgical release of the transverse carpal ligament was performed in Canada in 1924 [30] and carpal tunnel release (CTR) surgery became widely adopted from the 1950s [31] (Figure 2). CTR is the most commonly performed hand operation in the UK, with more than 51,000 performed in England in 2012 [32-33]. Surgical success rates of 54-75% are frequently reported [34,35], although there is some disagreement in how ‘success’ should be best defined [36].
Figure 2.
In their review of the evidence comparing surgical versus non-surgical management, Verdugo and colleagues found four randomised controlled trials involving 317 participants which measured improvement after 3-months of follow-up as a primary outcome) [37]. They concluded that surgery is more effective than non-surgical treatment at follow-up after 3 and 6 months of treatment [37]. Two trials including 245 participants also showed benefit of surgery versus non-surgery at 6 months follow-up [38,39].
More recently, endoscopic CTR has also gained popularity. A recent Cochrane review found no evidence that endoscopic CTR provides superior long- or short-term symptom relief compared to the standard open procedure, but concluded that there was some evidence to suggest that the endoscopic procedure may enable patients to return to work sooner (-6 days, 95% CI -9 to -3 days) [40].
Return to work after carpal tunnel release surgery
Despite the frequency of CTR, there is currently no consensus on the optimal time course and method of returning to work post-operatively. Duration of post-operative sickness absence is reported in some studies but is reported inconsistently and often excludes reference to an individual’s usual working hours or working pattern [36,41]. Aspects such as the need for graded return to work (amended duties or reduced hours), employee and employer satisfaction with occupational performance, and work related pain or discomfort need to be considered.
Even when methodological differences are accounted for, there is wide variability in the reported duration of sickness absence from work after CTR (Table 1). Mean work absence was as low as 4.3 days among self-employed workers in one study [42], while work absences of several months have been reported elsewhere [43,44-47]. Some studies have explored factors which are correlated with delayed return to work post-CTR. Individual characteristics including older age, female gender, obesity, co-existing musculo-skeletal disorders [47] and lower educational attainment [45,48] have all been shown to be independently associated with delayed return to work. Unsurprisingly, work factors are also important, including the type of occupation to which the patient needs to return [45,47,49]. People who need to resume manual work [44,50,], repetitive movements [48,50] and ergonomic stresses [48,50-51] all have delayed return to work as compared with those not exposed to these factors in the workplace. Pre- and post-operative clinical factors have also been found to play a role such that those with highest reported levels of pre-operative symptom severity [52]; those needing pre-operative sickness absence [44-45,52]; those requiring bilateral surgery [47-48]; those done by open rather than endoscopic techniques [40-41,53], and people reporting post-operative pain and scar tenderness [54] all have slower return to work. Poorer mental health status [44,55], lower self-efficacy [45,55], dissatisfaction with surgery [47], poorer job security, poorer support from co-workers [45], higher job demands and lower job control [45,51] are all psychological /psychoscial factors that can impact on return to work. Moreover, people on a lower income [45]; in receipt of worker’s compensation [44,55-56] and who have involved a lawyer [45,48] are all more likely to have slower return to work.
Table. SUMMARY OF THE FINDINGS FROM STUDIES THAT MEASURED WORK OUTCOMES AFTER CARPAL TUNNEL RELEASE SURGERY.
| Study | Numbers of subjects |
Numbers of hands |
Diagnosis | Surgical procedure |
Days absence reported |
Type of employment |
|---|---|---|---|---|---|---|
| Vogt, 2002 | 43 | 50 | Clinical and EMGs | Endoscopic | Self-employed: 4.3 days Employed: 19 days |
|
| Natahn, 1993 | Short incision vs. standard incision, open CTS release | Compensation: 21 days Non-compensations; 10 days |
||||
| Bitar, 2002 | 123 | Open CTS release | USA Workers’ compensation: 72 days USA Workers’ non-compensated: 56 days National Insurance Swedish Group: 36 days |
University employees USA and Sweden | ||
| Wang, 2003 | 20 | 40 | Bilateral open CTS release | Mean 2.6 weeks | ||
| Chaise, 2004 | 233 | Independent workers: 17 days Private sector workers: 35 days Civil servants: 56 days Workers compensation: 49 days |
||||
| Acharya, 2005 | 75 | 112 | Open CTS release | 17 days | ||
| Gimeno, 2005 | 122 | Clinical CTS and EMGs | CTS release | High job strain (high demands & poor control) delayed successful RTW | ||
| Schmelzer, 2005 | 486 | 753 | Clinical CTS 472/486 had EMGs | Uniportal endoscopic | Light duty: 21 days (compensation and non-compensation) Full duty: 43 days (compensation and non-compensation) |
122 Labourer 364 Non Labourer 61 unemployed 48 retired |
| Kahraman, 2006 | 27 | 30 | Biportal endoscopic | 12 days | Military workers | |
| Nesbitt, 2006 | 71 | BILATERAL 142 hands | Clinical bilateral CTS | Endoscopic simultaneously, phased 1-3 weeks or phased > 3 weeks (patient choice) | 2.6 weeks 8.5 weeks 6 weeks |
|
| Pomerance, 2007 | 150 | Open decompression | Insured workers delayed vs. non-insured. No benefit of 2 weeks intensive rehabilitation | |||
| Tian, 2007 | 62 | 70 | Open vs endoscopic (RCT) | Endoscopic group returned to work more quickly | ||
| De Kesel, 2008 | 88 | 107 | Clinical and EMGs when required | Open decompression or one-incision endoscopic | Self-employed: 23 days Employee: 36 days Heavy manual handling: 42 days vs. light manual 36 vs. non-manual 27 |
|
| Wyatt, 2008* | 187 | 281 | Clinical and EMGs | Open decompression (intensive early rehabilitation) | Light duties 11 days Full duties 28 days |
Lamb freezing workers (NZ) |
| Hansen, 2009 | 75 | 75 | Abnormal EMGs | Endoscopic | Mean 19.8 days | |
| Mallick, 2009 | 494 | Clinical CTS with EMGs as required | Open Decompression (intensive Nurse F/Up) | 93% within 2 weeks 99% within 4 weeks |
191 Manual 81 Non-manual 46 Secretarial |
|
| Parot-Schinkel, 2011 | 851 | Received CTS surgery | Mini-open surgery | Median 60 days | ||
| Cowan, 2012 | 65 | Limited incision open release | Modified duty: 11.8 days Full duties: 18.9 days |
|||
| Kohanzadeh, 2012 | Meta-analysis | Endoscopic (2382) vs. open (110) | Endoscopic: 15.3 days Open: 21.8 days |
Current return to work recommendations in UK
Patient information and return to work advice is available from the UK Royal College of Surgeons [57]. Based upon expert opinion, the recommendations indicate timescales for returning to different occupations after CTR as follows:
Supervisory/managerial: 1-2 weeks
Light manual (clerical/secretarial): 2-4 weeks
Medium manual (cleaner/carer/nurse/check-out operative): 4-6 weeks
Heavy manual: 6-10 weeks
Custodial/rescue services: 6-10 weeks
It is not known if this advice is consistently given to patients in practice, or if surgeons routinely provide alternative information. The role of surgeons’ advice on duration of work absence after CTR has only been explored in one small Israeli study including 50 patients [58]. Wide variation was found in the advice given, with recommended sick-leave duration ranging from 1-36 days (median 21 days). Patients did not always follow the advice received (6% returned one week earlier and 28% more than week later); however the surgeons’ recommendations were the strongest predictor of delayed return to work (OR 27.7, 95% CI 1.5-507). Little correlation was found between surgeons’ recommendations and the patient’s type of work, suggesting that patients could, and would, return to work sooner if recommended to do so by their surgeon.
The information provided by other healthcare professionals after CTR should also be considered. Three hundred and eighteen patients attending a nurse-led post-operative clinic were advised to start using their hand immediately and to return to work as soon as they felt able [59]. Ninety-three percent returned to work within two weeks and 99% within one month. Only three workers (all employed in manual occupations) returned to work after this time.
These studies indicate the importance of return to work advice following CTR, but further research is required to identify whether early return to work is realistic or safe for most people and whether employees are able to achieve early return to work in practice.
Conclusion
Carpal tunnel syndrome is a common clinical problem which frequently presents among patients of working age. There is evidence to suggest that occupational factors play a role in carpal tunnel syndrome, particularly work which involves exposure to repetitive movements and/or hand-held vibratory tools. Employed earners who develop the syndrome whilst in an occupation involving these exposures may be eligible for compensation. Conservative management can be helpful for mild symptoms but many people will ultimately undergo carpal tunnel release surgery. Given its frequency, there is surprisingly little guidance about the timing of safe return to work after surgery and an evidence-base is lacking.
Pointers for practice.
Reasonable evidence exists that regular, prolonged use of hand-held powered vibratory tools as well as prolonged and highly repetitious flexion and extension of the wrist (especially with a forceful grip) increase the risk of carpal tunnel syndrome.
On the balance of evidence keyboard and computer use do not cause CTS.
Conservative therapies are helpful for mild, uncomplicated CTS but a significant proportion of people affected will need carpal tunnel release surgery.
Research agenda.
Whilst clinical diagnosis of the individual case is reasonably straightforward given the constellation of signs and symptoms, as well as confirmatory tests, research has been hampered by lack of consensus over a surveillance case definition.
There is clear need for research to understand when it is safe to return to different types of work after CTR surgery.
Footnotes
Conflict of Interest statement- the authors declare there is no conflict of interest
References
- 1.Franzblau A, Werner RA. What is carpal tunnel syndrome? JAMA. 1999;282:186–187. doi: 10.1001/jama.282.2.186. [DOI] [PubMed] [Google Scholar]
- 2.Gerr F, Letz R. The sensitivity and specificity of tests for carpal tunnel syndrome vary with the comparison groups. J Hand Surg. 1998;23-B:151–155. doi: 10.1016/s0266-7681(98)80163-0. [DOI] [PubMed] [Google Scholar]
- 3.Szabo RM, Slater RR, Farver TB, Stanton DB, Sharman WK. The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg. 1999;24-A:704–714. doi: 10.1053/jhsu.1999.0704. [DOI] [PubMed] [Google Scholar]
- 4.Ferry S, Pritchard T, Keenan J, et al. Estimating the prevalence of delayed median nerve conduction in the general population. Br J Rheumatol. 1998;37:630–635. doi: 10.1093/rheumatology/37.6.630. [DOI] [PubMed] [Google Scholar]
- 5.The American Academy of Electrodiagnostic Medicine. The American Academy of Neurology. The American Academy of Physical Medicine and Rehabilitation Practice parameters for electrodiagnosis in carpal tunnel syndrome: summary statement. Muscle Nerve. 1993;16:1390–1391. doi: 10.1002/mus.880161219. [DOI] [PubMed] [Google Scholar]
- 6.Grundberg AB. Carpal tunnel decompression in spite of normal electromyography. J Hand Surg. 1983;8:348–349. doi: 10.1016/s0363-5023(83)80179-8. [DOI] [PubMed] [Google Scholar]
- 7.Nathan PA, Keniston RC, Myers LD, et al. Natural history of median nerve sensory conduction in industry: relationship to symptoms and carpal tunnel syndrome. Muscle Nerve. 1998;21:711–721. doi: 10.1002/(sici)1097-4598(199806)21:6<711::aid-mus2>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 8.Massy-Westropp N, Grimmer K, Bain G. A systematic review of the clinical diagnostic tests for carpal tunnel syndrome. J Hand Surg. 2000;25-A:120–127. doi: 10.1053/jhsu.2000.jhsu025a0120. [DOI] [PubMed] [Google Scholar]
- 9.Von Shroeder HP, Botte MJ. Carpal tunnel syndrome. Hand Clinics. 1996;12:643–55. [PubMed] [Google Scholar]
- 10.Stevens JC, Sun S, Beard CM, et al. Carpal tunnel syndrome in Rochester, Minnesota, 1961 to 1980. Neurology. 1988;38:134–138. doi: 10.1212/wnl.38.1.134. [DOI] [PubMed] [Google Scholar]
- 11.Nordstrom DL, Vierkant RA, DeStefano F, Layde PM. Risk factors for carpal tunnel syndrome in a general population. Occup Environ Med. 1997;54:734–740. doi: 10.1136/oem.54.10.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solomon DH, Katz JN, Bohn R, et al. Non-occupational risk factors for carpal tunnel syndrome. J Gen Intern Med. 1999;14:310–314. doi: 10.1046/j.1525-1497.1999.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hagberg M, Morgenstern H, Kelsh M. Impact of occupations and job tasks on the prevalence of carpal tunnel syndrome. Scand J Work Environ Health. 1992;18:337–345. doi: 10.5271/sjweh.1564. [DOI] [PubMed] [Google Scholar]
- 14.National Institute for Occupational Health and Safety . A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. US Department of Health and Human Sciences/NIOSH; Cincinnati, OH: 1997. Musculoskeletal Disorders and Workplace Factors. Publication no. 97-141. [Google Scholar]
- 15.Abbas MAF, Afifi AA, Zhang ZW, Kraus JF. Meta-analysis of published studies of work-related carpal tunnel syndrome. Int J Occup Environ Health. 1998;4:160–167. doi: 10.1179/oeh.1998.4.3.160. [DOI] [PubMed] [Google Scholar]
- 16.Palmer KT, Harris EC, Coggon D. Carpal tunnel syndrome and its relation to occupation: a systematic literature review. Occup Med. 2007;57:57–66. doi: 10.1093/occmed/kql125. [DOI] [PubMed] [Google Scholar]
- 17.Thomsen JF, Gerr F, Atroshi I. Carpal tunnel syndrome and the use of computer mouse and keyboard: a systematic review. BMC Musculoskeletal Disorders. 2008;9:134. doi: 10.1186/1471-2474-9-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mediouni Z, de Roquemaurel A, Dumontier C, et al. Is carpal tunnel syndrome related to computer exposure at work? A review and meta-analysis. J Occup Environ Med. 2014;56:204–208. doi: 10.1097/JOM.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 19.Van Rijn RM, Huisstede BMA, Koes BW, Burdorf A. Associations between work-related factors and the carpal tunnel syndrome - a systematic review. Scand J Work Environ Health. 2009;35:19–36. doi: 10.5271/sjweh.1306. [DOI] [PubMed] [Google Scholar]
- 20.Barcenilla A, March LM, Chen JS, Sambrook PN. Carpal tunnel syndrome and its relationship to occupation: a meta-analysis. Rheumatology. 2012;51:250–261. doi: 10.1093/rheumatology/ker108. [DOI] [PubMed] [Google Scholar]
- 21.You D, Smith AH, Rempel D. Meta-analysis: association between wrist posture and carpal tunnel syndrome among workers. Safe Health Work. 2014;5:27–31. doi: 10.1016/j.shaw.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Industrial Injuries Advisory IIAC . Work-related upper Limb Disorders. Corporate Document Services; London: 2006. Command paper 6868. Command paper 6868. [Google Scholar]
- 23.Page MJ, Massy-Westropp N, O’Connor D, Pitt V. Splinting for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012 Jul 11;7:CD010003. doi: 10.1002/14651858.CD010003. doi: 10.1002/14651858.CD010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piazzini DB, Aprile I, Ferrara PE, et al. A systematic review of conservative treatment of carpal tunnel syndrome. Clin Rehabil. 2007;21(4):299–314. doi: 10.1177/0269215507077294. [DOI] [PubMed] [Google Scholar]
- 25.Graham B. Nonsurgical treatment of carpal tunnel syndrome. J Hand Surg Am. 2009;34(3):531–4. doi: 10.1016/j.jhsa.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 26.O’Connor D, Marshall SC, Massy-Westropp N, Pitt V. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003 Jan 20;:CD003219. doi: 10.1002/14651858.CD003219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007 Apr 18;:CD001554. doi: 10.1002/14651858.CD001554.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Ebenbichler GR, Resch KL, Nicolakis P, et al. Ultrasound treatment for treating the carpal tunnel syndrome: randomised ’sham’ controlled trial. BMJ. 1998;316:731–5. doi: 10.1136/bmj.316.7133.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker NA, Livengood HM. Symptom severity and conservative treatment for carpal tunnel syndrome in association with eventual carpal tunnel release. J Hand Surg [Am] 2014;39:1792–98. doi: 10.1016/j.jhsa.2014.04.034. [DOI] [PubMed] [Google Scholar]
- 30.Amadio P. The Mayo Clinic and carpal tunnel syndrome. Mayo Clin Proc. 1992;67:42–8. doi: 10.1016/s0025-6196(12)60278-x. [DOI] [PubMed] [Google Scholar]
- 31.Boskovski MT, Thomson JG. Acroparesthesia and carpal tunnel syndrome: A historical perspective. J Hand Surg [Am] 2014;39:1813–21. doi: 10.1016/j.jhsa.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 32.Health and Social Care Information Centre www.hscic.gov.uk.
- 33.Dillon JP, Laing A, Hussain M, Macey A. Improved tolerability of open carpal tunnel release under local anaesthetic: a patient satisfaction survey. Arch Orthop Trauma Surg. 2008;128:125–27. doi: 10.1007/s00402-007-0460-2. [DOI] [PubMed] [Google Scholar]
- 34.Bland JDP. Treatment of carpal tunnel syndrome. Muscle & Nerve. 2007;36:167–71. doi: 10.1002/mus.20802. [DOI] [PubMed] [Google Scholar]
- 35.Coggon D, Ntani G, Harris EC, et al. Impact of carpal tunnel surgery according to pre-operative abnormality of sensory conduction in median nerve: a longitudinal study. BMC Musculoskel Dis. 2013;14:241. doi: 10.1186/1471-2474-14-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jerosch-Herold C, de Carvalho Leite JC, Song F. A systematic review of outcomes assessed in randomized controlled trials of surgical interventions for carpal tunnel syndrome using the International Classification of Functioning, Disability and Health (ICF) as a reference tool. BMC Musculoskel Dis. 2006;7:96. doi: 10.1186/1471-2474-7-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Verdugo RJ, Salinas RA, Castillo JL, Cea JG. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev. 2008 Oct 8;:CD001552. doi: 10.1002/14651858.CD001552.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerritsen AAM, de Vet HCW, Scholten RJPM, Bertelsmann FW, de Krom MCTFM, Bouter LM. Splinting versus surgery in the treatment of carpal tunnel syndrome. A randomized controlled trial. JAMA. 2002;288(10):1245–51. doi: 10.1001/jama.288.10.1245. [DOI] [PubMed] [Google Scholar]
- 39.Ly-Pen D, Andréu JL, de Blas G, Sánchez-Olaso A, Millán I. Surgical decompression versus local steroid injection in carpal tunnel syndrome. A one-year, prospective, randomized, open, controlled clinical trial. Arth Rheum. 2005;52(2):612–9. doi: 10.1002/art.20767. [DOI] [PubMed] [Google Scholar]
- 40.Scholten RJPM, Mink van der Molen A, Uitdehaag BMJ, et al. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;4:CD003905. doi: 10.1002/14651858.CD003905.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanati KA, Mansouri M, Macdonald D, et al. Surgical techniques and return to work following carpal tunnel release: a systematic review and meta-analysis. J Occup Rehabil. 2011;21:474–81. doi: 10.1007/s10926-011-9310-8. [DOI] [PubMed] [Google Scholar]
- 42.Vogt T, Scholz J. Clinical outcome and predictive value of electrodiagnostics in endoscopic carpal tunnel surgery. Neurosurg Rev. 2002;25:218–21. doi: 10.1007/s10143-002-0213-1. [DOI] [PubMed] [Google Scholar]
- 43.Adams ML, Franklin GM, Barnhart S. Outcome of carpal tunnel surgery in Washington state workers’ compensation. Am J Ind Med. 1994;25:527–36. doi: 10.1002/ajim.4700250407. [DOI] [PubMed] [Google Scholar]
- 44.Katz JN, Keller RB, Fossel AH, et al. Predictors of return to work following carpal tunnel release. Am J Ind Med. 1997;31:85–91. doi: 10.1002/(sici)1097-0274(199701)31:1<85::aid-ajim13>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 45.Katz JN, Amick BC, Keller R, et al. Determinants of work absence following surgery for carpal tunnel syndrome. Am J Ind Med. 2005;47:120–30. doi: 10.1002/ajim.20127. [DOI] [PubMed] [Google Scholar]
- 46.Nancollas MP, Peimer CA, Wheeler DR, Sherwin FS. Long-term results of carpal tunnel release. J Hand Surg. 1995;20:470–74. doi: 10.1016/s0266-7681(05)80155-x. [DOI] [PubMed] [Google Scholar]
- 47.Parot-Schinkel E, Roquelaure Y, Ha C, et al. Factors Affecting Return to Work After Carpal Tunnel Syndrome Surgery in a Large French Cohort. Arch Phys Med Rehabil. 2011;92:1863–69. doi: 10.1016/j.apmr.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 48.Butterfield P, Spencer P, Redmond N, et al. Clinical and employment outcomes of carpal tunnel syndrome in oregon workers’ compensation recipients. J Occ Rehabil. 1997;7:61–73. [Google Scholar]
- 49.Cowan J, Makanji H, Mudgal C, et al. Determinants of return to work after carpal tunnel release. J Hand Surg. 2012;37:18–27. doi: 10.1016/j.jhsa.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 50.De Kesel R, Donceel P, De Smet L. Factors influencing return to work after surgical treatment for carpal tunnel syndrome. Occup Med. 2008;58:187–90. doi: 10.1093/occmed/kqn034. [DOI] [PubMed] [Google Scholar]
- 51.Gimeno D, Amick BC, Habeck RV, et al. The role of job strain on return to work after carpal tunnel surgery. Occup Environ Med. 2005;62:778–85. doi: 10.1136/oem.2004.016931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hansen TB, Dalsgaard J, Meldgaard A, Larsen K. A prospective study of prognostic factors for duration of sick leave after endoscopic carpal tunnel release. BMC Musculoskel Dis. 2009;10:144. doi: 10.1186/1471-2474-10-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thoma A, Veltri K, Haines T, Duku E. A systematic review of reviews comparing the effectiveness of endoscopic and open carpal tunnel decompression. Plastic and Reconstructive Surgery. 2004;113:1184–91. doi: 10.1097/01.prs.0000110202.08818.c1. [DOI] [PubMed] [Google Scholar]
- 54.Atroshi I, Larson G, Ornstein E, et al. Outcomes of endoscopic surgery compared with open surgery for carpal tunnel syndrome among employed patients: randomised controlled trial. BMJ. 2006;332:1473. doi: 10.1136/bmj.38863.632789.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Amick BC, Habeck RV, Ossmann J, et al. Predictors of successful work role functioning after carpal tunnel release surgery. JOEM. 2004;46:490–500. doi: 10.1097/01.jom.0000126029.07223.a0. [DOI] [PubMed] [Google Scholar]
- 56.Ynoe de Moraes V, Godin K, Baptista Gomes dos Santos J, Faloppa F. Influence of compensation status on time off work after carpal tunnel release and rotator cuff surgery: a meta analysis. Patient Safety in Surgery. 2013;7:1. doi: 10.1186/1754-9493-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Royal College of Surgeons Get well soon: Helping you make a speedy recovery after carpal tunnel release. 2014 www.rcseng.ac.uk/patients/recovering-from-surgery/carpal-tunnel-release/returning-to-work.
- 58.Ratzon N, Schejter-Margalit T, Froom P. Time to return to work and surgeons’ recommendations after carpal tunnel release. Occup Med. 2006;56:46–50. doi: 10.1093/occmed/kqi194. [DOI] [PubMed] [Google Scholar]
- 59.Mallick A, Clarke M, Wilson S, Newey ML. Reducing the economic impact of carpal tunnel surgery. J Hand Surg [Eur] 2009;34:679–81. doi: 10.1177/1753193409105578. [DOI] [PubMed] [Google Scholar]