Abstract
Background:
Various anatomical measurements and noninvasive clinical tests, singly or in various combinations can be performed to predict difficult intubation. Upper lip bite test (ULBT) and ratio of height to thyromental distance (RHTMD) are claimed to have high predictability. Hence, we have conducted this study to compare the predictive value of ULBT and RHTMD with the following parameters: Mallampati grading, inter-incisor gap, thyromental distance, sternomental distance, head and neck movements, and horizontal length of mandible for predicting difficult intubation.
Materials and Methods:
In this single blinded, prospective, observational study involving 170 adult patients of either sex belonging to American Society of Anesthesiologists physical Status I–III scheduled to undergo general anesthesia were recruited. All patients were subjected to the preoperative airway assessment and, the above parameters were recorded correlated with Cormack and Lehane grade and analyzed. The number of intubation attempts and use of intubation aids were also noted.
Results:
ULBT and RHTMD had highest sensitivity (96.64%, 90.72%), specificity (82.35%, 80.39%), positive predictive value (92.74%, 91.53%), and negative predictive value (91.3%, 78.8%), respectively, compared to other parameters. While odds ratio and likelihood ratio >1 for all the tests.
Conclusion:
ULBT can be used as a simple bedside screening test for prediction of difficult intubation, but it should be combined with other airway assessment tests for better airway predictability. RHTMD can also be used as an acceptable alternative.
Keywords: Airway assessment tests, difficult laryngoscopy, ratio of height to thyromental distance, upper lip bite tests
Introduction
Endotracheal intubation remains the gold standard for emergency airway management. Airway management is a core skill in emergency medicine, anesthesiology, and critical care. Ensuring an unobstructed airway and adequate oxygenation are first priorities in the resuscitation of the patient. Unlike the elective surgical patient, the trauma and critically ill patients present with many challenges. According to the American Society of Anesthesiologists (ASA), the incidence of difficult and failed intubation in the operating room is 1.2-3.8% and 0.13-0.30%, respectively, while the incidence of difficult direct intubation in the Intensive Care Unit (ICU) or Emergency Medicine Department setting is estimated to be as high as 20%.[1]
Failure in managing the airway is the most important cause of death in patients undergoing general anesthesia. About 50-75% of cardiac arrests during general anesthesia are because of difficult intubation that causes inadequate oxygenation and/or ventilation, which about 55-93% of them cause death or brain death.[2,3,4]
When there is difficult laryngoscopy (characterized by poor glottic visualization) there are chances of difficult intubation in most of the patients. In the patients undergoing surgery difficult intubation varies from 1.5% to 13% according to data reported.[5]
Many preoperative airway assessment tests such as inter-incisor gap (IIG)/mouth opening, mallampati grading (MPG), head and neck movement (HNM), horizontal length of mandible (HLM), sternomental distance (SMD), and thyromental distance (TMD) may be used to predict difficult intubations, but sensitivity and positive predictive value (PPV) of these individual tests are low while false positive (FP) results are high. Different studies are going on to find out simple bedside tests singly or in various combinations for predicting difficult tracheal intubation, which have high sensitivity, specificity, PPV, negative predictive value (NPV), likelihood ratio (LR) with minimal FP, and false negative values.[6,7] However, there are very few studies comparing upper lip bite test (ULBT) and ratio of height to TMD (RHTMD) with other screening tests.[8,9]
Hence, we decided to conduct this study with the primary aim to evaluate sensitivity, specificity, PPV, NPV, relative risk (RR), odds ratio (OR), and LR for various screening tests such as ULBT, RHTMD, IIG, modified mallampati test, TMD, SMD, and HNM in isolation and also compared ULBT and RHTMD with other tests to determine a more comprehensive and accurate as well as simple and clinically applicable parameter for predicting difficult intubation for routine practice in anesthesia as well as for ICU and Emergency medicine setup.
Materials and Methods
After the Institutional Ethical Committee approval and written informed consent, 170 patients of both gender between 20 and 70 years of age belonging to ASA physical Status I-III scheduled to undergo elective surgery under general anesthesia with endotracheal intubation were recruited for this single blinded, prospective, observational study. In our study, patients with airway malformation, oral surgery, neck burns contracture, midline neck swelling, emergency surgery, caesarean section, edentulous patients, limitation of temporomandibular/atlantoaxial joint mobility, and history of neck surgery were excluded from the study.
All patients were subjected to the preoperative airway assessment by the same anesthesiologist to avoid interobserver variability. We recorded the data as per the format suggested by All India Difficult Airway Association. We also assessed height, weight, and body mass index. Height of the patient was measured in centimeter (cm) from vertex to heel with the patient standing.
The oropharyngeal view was assessed using a MPG[10] by asking the patient to sit and open his or her mouth maximally and to protrude the tongue without phonation and classified as below [Figure 1a].
Figure 1.

(a) Mallampati grading, and (b) Cormack and Lehane laryngoscopy grading. Rapid airway access Sérgio L. Amantéa I; Jefferson P. Piva II; Malba Inajá Rodrigues III; Francisco Bruno IV; Pedro Celiny R. GarciaV Print version ISSN 0021-7557 J. Pediatr. (Rio J.) vol. 79 suppl.2 Porto Alegre Nov. 2003
Class I: Soft palate, fauces, uvula, anterior and posterior tonsil pillars visible
Class II: Uvula is obscured by base of tongue
Class III: Soft palate and base of uvula are visible
Class IV: Only hard palate is visible.
ULBT was done to assess the range of freedom of the mandibular movement and the architecture of the teeth concurrently.[11] Each patient was asked to bite their upper lip with lower incisor and categorized as shown in Figure 2a.
Figure 2.
(a) Upper lip bite test, and (b) thyromental distance. Image courtesy: Comparative evaluation of airway assessment tests and their correlation with laryngoscopy. Sharma et al.: Indian Journal of Clinical Anesthesia, January–March 2015;2(1):19–26)
Class I: Lower incisor can hide mucosa of the upper lip
Class II: Lower incisor can partially hide mucosa of the upper lip
Class III: Lower incisor unable to touch mucosa of the upper lip.
IIG was assessed by asking each patient to open the mouth to maximum extent. The distance between upper and lower incisor at the midline was measured, which is usually >3.5 cm.[11]
TMD was measured from the bony point of the mentum while the head was fully extended and mouth closed, using a rigid ruler, shown in Figure 2b. The distance was rounded to nearest 0.5 cm and graded as:
Class I: >6.5 cm
Class II: 6–6.5 cm
Class III: <6 cm.
SMD was measured in cm from sternal notch to the mentum with the head fully extended on the neck with the mouth closed. Normally, it is >12.5 cm.
Horizontal length of the mandible (HLM): It is measured from angle of the mandible to the mentum. Normally, it is ≥9 cm.
Maximum range of HNM was noted as Grade I ≤80° or Grade II ≥80°. The patient was first asked to extend the head and neck fully.[12]
RHTMD[13] was calculated as follows:
RHTMD = Height (in cm)/TMD (in cm) and graded as Grade I <23.5, Grade II ≥23.5.
To predict difficult laryngoscopy cutoff value for various parameters is as shown in Table 1.
Table 1.
Cutoff value for various parameters to predict difficult laryngoscopy

We kept all patients nil by mouth for 8–10 h. After taking written informed consent and patient preoperative vitals were recorded. In the operating room, 20G intravenous (i.v.) cannula was inserted and ringer lactate infusion was started. Standard monitors such as ECG, NIBP, and SPO2 were attached and continuous intraoperative monitoring done. Patients premedicated with injection glycopyrrolate 4 μg/kg i.v., injection ranitidine 1 mg/kg i.v., injection ondansetron 0.08 mg/kg i.v., and injection fentanyl 1 μg/kg i.v. given. After preoxygenation with 100% O2 for 3 min, injection thiopentone 5–6 mg/kg i.v. given and after confirming mask ventilation was possible injection succinylcholine 1.5 mg/kg i.v. was given. After cessation of fasciculations, patients head was put in sniffing position and laryngoscopy was performed with a Macintosh blade No. 3 or 4 blade. Cormack and Lehane (CL) view was assessed after evaluation, if needed external laryngeal pressure was permitted for tracheal intubation.
Laryngoscopy was done by a qualified and experienced anesthesiologist, who was blinded to the results of preoperative airway assessment and Glottic visualization were assessed and noted according to modified CL grade [Figure 1].
Grade I: Full glottic exposure
Grade II: Only posterior commissure of glottis seen
Grade III: Only epiglottis visible
Grade IV: Epiglottis not visible.
During direct laryngoscopy, if CL Grade III or Grade IV view was present, patient kept in difficult laryngoscopy group, and if CL Grade I or Grade II was present, patient kept in easy laryngoscopy group and considered as easy visualization of the larynx.
Endotracheal intubation surgery was performed under standard anesthesia. Patient's vitals were monitored intraoperatively and postoperatively. We observed 170 patients. Standard formula was used for data analysis as shown in Table 2. We used standard t-test for statistical analysis and P ≤ 0.05 was considered statistically significant.
Table 2.
Standard formula for different test for data analysis

Results
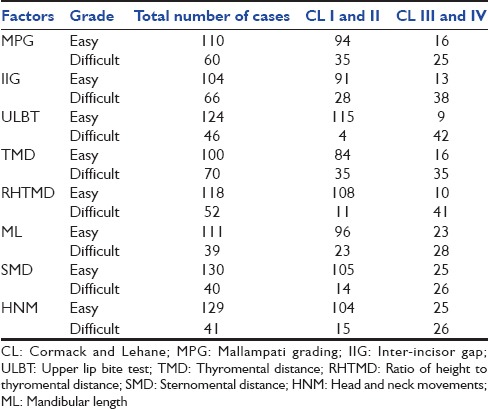
In this study, all the patients were comparable demographically in easy and difficult laryngoscopy groups as shown in Table 3. Distribution of various predictive tests based on CLs laryngoscopy grading as shown in Table 4. The incidence of difficult laryngoscopy was 30% on first laryngoscopic view, but we applied external laryngeal pressure for ease of intubation and hence it was reduced to 20% with no failed intubation. Of the 51 different laryngoscopies, 48 had CL Grade III and 3 had CL Grade IV. All the patients were intubated successfully either with the 2nd attempt or with the change of laryngoscope blade, without any failed intubation.
Table 3.
Demographic data based on Cormack and Lehane's laryngoscopy grading

Table 4.
Distribution of various predictive tests based on Cormack and Lehane laryngoscopy grading
Highest sensitivity, PPV, and NPV were observed with ULBT and RHTMD as compared to other predictive tests. RR and LR were highest for ULBT, while OR were highest for RHTMD. HNM had lowest PPV, NPV, RR, OR, and LR as shown in Figure 3.
Figure 3.

Comparison of various predictive tests
Discussion
It is very crucial for anesthesiologist and intensivist to identify the probable difficulty for intubation to prevent morbidity and mortality due to unexpected difficult intubation. There are many studies and meta-analysis attempting to determine the best single method or combination of methods for predicting difficult intubation.[14,15,16] It is necessary to investigate for a simple and accurate predictive test. Many anatomical landmarks detect potentially difficult laryngoscopies preoperatively. Closed claim analysis found that under the vast majority of the airway-related events, inability to maintain patent airway involve brain damage or death. Preoperative evaluation is very important, but the fact that which of these anatomical landmarks and clinical factors are the best is unknown yet.
We included 170 patients in our study, and the incidence of difficult intubation was 30% with no failed intubation. The other study reported that the incidence of difficult intubation was 1–18%, which was depending to the criteria employed for cutoff limit for difficult intubation, and might be due to wide racial variation, age of patient, and male preponderance.[17] In this study, among the difficult intubation group, the majority were male (61.85%) similar to other study.[18] This male preponderance of difficult intubation may be due to increased muscle mass and neck rigidity present in male.
For the prediction of difficult airway ideal test would have perfect sensitivity and specificity. However, as sensitivity and specificity are interdependent and if one increases other decreases. We considered sensitivity the most important parameter as our target was to identify more number of difficult intubation cases to avoid the potentially serious outcome of unanticipated difficult tracheal intubation.
Our study revealed ULBT as the best predicting test with highest sensitivity and specificity (96.64% and 82.35%, respectively). ULBT has also higher PPV, NPV, RR, and LR compared to other predictive tests [Figure 3]. The results were comparable to the other studies[16,19] Khan et al.[16] who introduced ULBT as a simple and effective method for predicting difficult intubations. The variations in statistical data could be due to population differences.
This study results also shown that RHTMD was second best test, with higher sensitivity, specificity, PPV, NPV, LR, OR, and RR. Schmitt et al.[13] introduced RHTMD, reported that RHTMD has better predictive value for predicting difficult laryngoscopy than TMD. As TMD does not allows for individual's body proportions which are allowed in RHTMD. Krobbuaban et al.[20] and Krishna et al.[21] taken cutoff limit of RHTMD ≥23.5 cm as risk factor for predicting difficult laryngoscopy and observed variable results. Although the different statistical values in our study varied from other studies, but the last conclusion was comparable.
Prediction of difficult intubation of individual and combination of tests was assessed by different statistical methods such as OR, LR, and RR. We found OR > 1 in all of the tests which denoted good association between test and intubation grading. LR was more than 1 in all the tests which signified that the probability of test positively coincided with the intubation grading.
Conclusion
Our study results demonstrates that the ULBT can be used as a simple bedside screening test for prediction of difficult intubation, but it should be combined with other airway assessment tests for better airway predictability and RHTMD can also be used as an acceptable alternative.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Karalapillai D, Darvall J, Mandeville J, Ellard L, Graham J, Weinberg L. A review of video laryngoscopes relevant to the intensive care unit. Indian J Crit Care Med. 2014;18:442–52. doi: 10.4103/0972-5229.136073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zuercher M, Ummenhofer W. Cardiac arrest during anesthesia. Curr Opin Crit Care. 2008;14:269–74. doi: 10.1097/MCC.0b013e3282f948cd. [DOI] [PubMed] [Google Scholar]
- 3.Braz LG, Módolo NS, do Nascimento P, Jr, Bruschi BA, Castiglia YM, Ganem EM, et al. Perioperative cardiac arrest: A study of 53,718 anaesthetics over 9 yr from a Brazilian teaching hospital. Br J Anaesth. 2006;96:569–75. doi: 10.1093/bja/ael065. [DOI] [PubMed] [Google Scholar]
- 4.Safavi M, Honarmand A, Amoushahi M. Prediction of difficult laryngoscopy: Extended Mallampati score versus the MMT, ULBT and RHTMD. Adv Biomed Res. 2014;3:133. doi: 10.4103/2277-9175.133270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iohom G, Ronayne M, Cunningham AJ. Prediction of difficult tracheal intubation. Eur J Anaesthesiol. 2003;20:31–6. doi: 10.1017/s0265021503000061. [DOI] [PubMed] [Google Scholar]
- 6.Domi R. The best prediction test of difficult intubation. J Anaesthesiol Clin Pharmacol. 2010;26:193–6. [Google Scholar]
- 7.Khan ZH, Maleki A, Makarem J, Mohammadi M, Khan RH, Zandieh A. A comparison of the upper lip bite test with hyomental/thyrosternal distances and mandible length in predicting difficulty in intubation: A prospective study. Indian J Anaesth. 2011;55:43–6. doi: 10.4103/0019-5049.76603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah PJ, Dubey KP, Yadav JP. Predictive value of upper lip bite test and ratio of height to thyromental distance compared to other multivariate airway assessment tests for difficult laryngoscopy in apparently normal patients. J Anaesthesiol Clin Pharmacol. 2013;29:191–5. doi: 10.4103/0970-9185.111700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan ZH, Arbabi S. Diagnostic value of the upper lip bite test in predicting difficulty in intubation with head and neck landmarks obtained from lateral neck X-ray. Indian J Anaesth. 2013;57:381–6. doi: 10.4103/0019-5049.118567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211–6. doi: 10.1093/bja/61.2.211. [DOI] [PubMed] [Google Scholar]
- 12.Merah NA, Wong DT, Ffoulkes-Crabbe DJ, Kushimo OT, Bode CO. Modified Mallampati test, thyromental distance and inter-incisor gap are the best predictors of difficult laryngoscopy in West Africans. Can J Anaesth. 2005;52:291–6. doi: 10.1007/BF03016066. [DOI] [PubMed] [Google Scholar]
- 13.Schmitt HJ, Kirmse M, Radespiel-Troger M. Ratio of patient's height to thyromental distance improves prediction of difficult laryngoscopy. Anaesth Intensive Care. 2002;30:763–5. doi: 10.1177/0310057X0203000607. [DOI] [PubMed] [Google Scholar]
- 14.Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, et al. A clinical sign to predict difficult tracheal intubation: A prospective study. Can Anaesth Soc J. 1985;32:429–34. doi: 10.1007/BF03011357. [DOI] [PubMed] [Google Scholar]
- 15.Mallampati SR. Clinical sign to predict difficult tracheal intubation (hypothesis) Can Anaesth Soc J. 1983;30(3 Pt 1):316–7. doi: 10.1007/BF03013818. [DOI] [PubMed] [Google Scholar]
- 16.Khan ZH, Kashfi A, Ebrahimkhani E. A comparison of the upper lip bite test (a simple new technique) with modified Mallampati classification in predicting difficulty in endotracheal intubation: A prospective blinded study. Anesth Analg. 2003;96:595–9. doi: 10.1097/00000539-200302000-00053. [DOI] [PubMed] [Google Scholar]
- 17.Honarmand A, Safavi M, Ansari N. A comparison of between hyomental distance ratios, ratio of height to thyromental, modified Mallamapati classification test and upper lip bite test in predicting difficult laryngoscopy of patients undergoing general anesthesia. Adv Biomed Res. 2014;3:166. doi: 10.4103/2277-9175.139130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basunia SR, Ghosh S, Bhattacharya S, Saha I, Biswas A, Prasad A. Comparison between different tests and their combination for prediction of difficult intubation: An analytical study. Anesth Essays Res. 2013;7:105–9. doi: 10.4103/0259-1162.114014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: An external prospective evaluation. Anesth Analg. 2005;101:284–9. doi: 10.1213/01.ANE.0000154535.33429.36. [DOI] [PubMed] [Google Scholar]
- 20.Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M. The predictive value of the height ratio and thyromental distance: Four predictive tests for difficult laryngoscopy. Anesth Analg. 2005;101:1542–5. doi: 10.1213/01.ANE.0000181000.43971.1E. [DOI] [PubMed] [Google Scholar]
- 21.Krishna HM, Agarwal M, Dali JS, Rampal P, Dua CK. Prediction of difficult laryngoscopy in Indian population: Role of ratio of patient's height to thyromental distance. J Anaesthesiol Clin Pharmacol. 2005;21:257–60. [Google Scholar]



