Abstract
Introduction:
Effective management of endodontic pain represents a continuing challenge. Many of the dental professionals are facing significant problems associated with postendodontic pain. Hence, the postendodontic pain has to be prevented at its primary stage without waiting for its occurrence. This trial was carried out to evaluate the use of a preoperative, single oral dose of diclofenac sodium for the prevention and control of postendodontic pain.
Materials and Methods:
Fifty patients were randomly assigned to two groups, placebo and diclofenac sodium (100 mg). The medications were administered 30 min before the start of standard endodontic treatment. Postoperative pain was assessed after 6, 12, and 24 h by using a visual analog scale.
Results:
Postendodontic pain showed a statistically significant difference between both groups at 6 and 12 h (P < 0.05) and there was no significant difference at 24 h.
Conclusion:
Postendodontic pain was substantially reduced by preoperative administration of single oral dose of diclofenac sodium. It is thus possible to conclude that these favorable results might help to prevent postendodontic pain, especially in patients with a low pain threshold.
Keywords: Diclofenac sodium, postendodontic pain, pretreatment analgesic, visual analog scale
INTRODUCTION
Endodontic posttreatment pain continues to be a significant problem facing the dental profession.[1] Among patients presenting with preoperative pain, it has been reported that up to 80% of this population continue to report pain after endodontic treatment, with pain levels ranging from mild to severe.[2,3] The possible causes for endodontic inter-appointment pain are related to endodontic instrumentation, irritating irrigants, intracanal medications, periapical contamination, and temporary restorations in hyperocclusion. Irritation of periradicular tissues during root canal therapy causes an acute inflammatory reaction, potentially leading to pain and/or swelling.[3]
Certain factors may influence the progression of postoperative pain, such as a history of preoperative pain and the need for re-treatment.[4] Many chemical mediators have been associated with this inflammatory process. Prostaglandins increase vascular permeability, elevate chemotactic activity, induce fever, and increase sensitivity of pain receptors to other active inflammatory mediators.[2,3]
A variety of approaches have been recommended for the management of interappointment pain. These include occlusal reduction, intracanal medication, prescription of analgesics, and the use of steroidal and nonsteroidal anti-inflammatory agents.[2,3,4] The potential for these anti-inflammatory drugs to directly or indirectly prevent pain at the site of tissue injury is evidenced by the suppression of the release of inflammatory mediators.[4]
A preoperative single oral dose of anti-inflammatory drugs can modulate release of inflammatory mediators and reduce the occurrence of side effects compared with repeated doses during the postoperative period.[3] Few studies have evaluated the effect of nonsteroidal anti-inflammatory drugs (NSAIDs) with regard to prevention and control of postendodontic pain after root canal instrumentation. Thus, the purpose of the present trial was to evaluate the effect of diclofenac sodium (100 mg) administered as a single, preoperative oral dose for the prevention and control of postendodontic pain.
MATERIALS AND METHODS
Fifty patients, statistically selected between the ages of 20 and 60 years, were selected at the Department of Conservative Dentistry and Endodontics. Ethical clearance and informed consent was obtained to conduct the trial. Clinical examinations were conducted by three operators. The examination included a thermal (cold) test, percussion and palpation evaluation, periodontal probing, mobility assessment, and a periapical radiograph. All past and present symptoms were noted. A diagnosis was determined on the basis of the history as well as clinical and radiographic features.
The inclusion criteria for the study were requirement for nonsurgical endodontic therapy in single or multirooted teeth; vital and irreversible pulpitis without periapical abscess; and patients having moderate-severe pain. Exclusion criteria were the patients who had taken analgesic and anti-inflammatory drugs, periodontal diseases, requirement for prophylactic antibiotics, pregnancy or lactation, mental disabilities, systemic diseases that contraindicated endodontic therapy, and any known sensitivity or other adverse reactions to NSAIDs.
The patients were randomly allocated using simple randomization technique into 2 experimental groups: Group 1, diclofenac sodium (Diclomol, Win Medicare, 100 mg-oral) and Group 2, placebo (sucrose and lactose tablets). Both medications were administered 30 min before conventional root canal therapy. To maintain the double-blind design, a second investigator provided the two agents, and each tablet was disguised so that the patient as well as the operator was not aware of the medication. Treatment in all cases whether it was vital or nonvital teeth were completed in a single visit or at least till chemo-mechanical preparation was done.
Each patient was anesthetized with a solution of 2% lidocaine HCl with 1:100,000 epinephrine, followed by tooth isolation with rubber dam, and access opening was done. Working length was determined by both radiograph and apex locator methods using number 15 size K-file, and subsequently the canals were cleaned and shaped using a crown-down technique. The canals were enlarged to a 4% (number 25) and 6% (number 25) K3-rotary system depending on the size of the canal, which were 0.5-1.0 mm short of the radiographic apex. Copious irrigation with a normal saline solution (0.9% of NaCl) and 2.5% sodium hypochlorite was used between each file throughout the entire procedure.
When instrumentation was completed, the canals were dried using paper points. The canals were filled with Gutta-percha and AH-Plus sealer in case of single visit root canal treatment (RCT). In case of teeth with multiple visits, RCT till cleaning and shaping was completed. The access cavity was closed with zinc oxide eugenol cement. The occlusion was evaluated and reduced, if necessary.
Patients were instructed to complete a pain diary 6, 12, and 24 h after root canal instrumentation. The method used to measure clinical pain intensity was the visual analog scale (VAS), which consisted of a 10 cm line anchored by two extremes, “no pain” and “pain as bad as it could be.” Patients were asked to make a mark on the line that represented their level of perceived pain. Aceclofenac was prescribed to the patients as rescue medicine, if needed. Thus, pain intensity was assigned into four categorical scores:
None (0);
Mild (1-3);
Moderate (4-6); and
Severe (7-10).
Baseline comparisons of the study were performed by using Fisher's exact test. The status of pain at each level between groups was analyzed using a Chi-square test. All calculations were made through the program SPSS Version 19.0 (SPSS Inc, Armonk, NY, USA). The significance levels were set at 5% (P < 0.05).
RESULTS
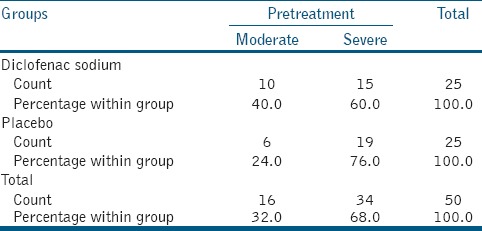
A total of 50 volunteers completed the study having moderate pain (58%) and severe pain (42%). Subjects with preoperative pain between diclofenac sodium (60%) and placebo (76%) had no significant difference [Table 1].
Table 1.
Preoperative pain between diclofenac sodium and placebo
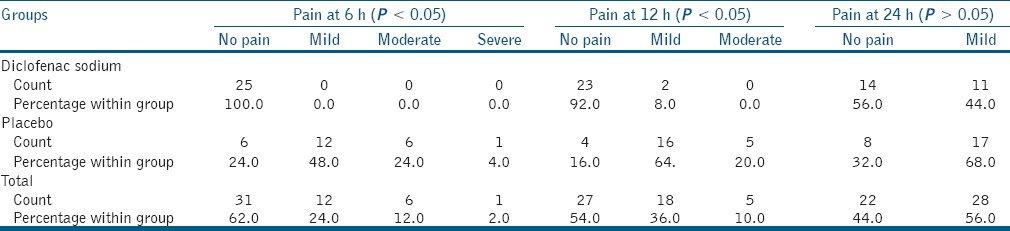
Postendodontic pain showed a statistically significant difference between groups at 6 and 12 h (P < 0.05) and there was no significant difference at 24 h. Diclofenac sodium treatment was associated with the lowest levels of endodontic pain [Table 2]. Few patients had reported with a pain at 24 h of endodontic therapy in both the groups. No side effects were reported for any of the medications used.
Table 2.
Postendodontic pain showed a statistically significant difference between groups at 6, 12 h, and no significant difference at 24 h
DISCUSSION
Traditionally, impacted third molar extractions and periodontal surgery have served as excellent models for testing analgesic and anti-inflammatory drugs.[5,6,7] The dental literature presents few studies evaluating oral administration of dexamethasone for the prevention and control of postendodontic pain.[8,9,10]
Protocols for assessing endodontic pain differ from oral surgery models in several respects. Patients in need of endodontic treatment might have different systemic conditions and might vary in age or the degree of pulpal pathology; these factors could introduce bias into a study.[8,9,10,11] Periapical anatomy is another important factor that can lead to different inflammatory responses after root canal therapy.[10,12] Thus, the evaluation of analgesic and anti-inflammatory drugs in oral surgical procedures cannot be directly extrapolated for determining the appropriate approach to treat endodontic pain.
Placebo groups are commonly used in drug efficacy studies. For ethical reasons, all patients were informed about the possibility of receiving a placebo. Both groups received rescue medication to be used if they experienced pain, and these patients were excluded from the study, but no patient reportedly took rescue medication. A combination of placebo and biopulpectomy has been shown to relieve pain in 71% of individuals.[13] Studies in patients with preexisting pain have shown a significant reduction in pain in patients by using placebo after biopulpectomy.[11,14] In the present study, placebo did not result in significant pain reduction at the 12-h time point. In comparison with placebo at the 6- and 12-h time points (P < 0.05), diclofenac sodium was able to significantly reduce pain intensity.
VAS was used to evaluate pain intensity; this scale has been used in most of the previous studies that analyzed pain after endodontic treatment.[12,13,14,15] The VAS is more sensitive to small changes than simple descriptive ordinal scales. One of the limitations of the VAS is that it must be administered on paper or electronically. Caution is required when photocopying the scale because this can lead to significant changes in its length. The failure of VAS is between 4% and 11%, but this can be reduced if the tool is carefully explained to the patient.[16] In the present study, the VAS scale was explained in detail to the volunteers, and changes of photocopies were avoided.
In comparison with placebo at the 12-h time point, diclofenac sodium was able to significantly reduce pain intensity. However, these results were not observed at 24 h. The percentage of patients who experienced no pain with the use of diclofenac sodium was 100% and 92.0% at 6 and 12 h, respectively; for placebo, the respective values were 24.0% and 16.0%.
This was one of the pioneer studies to use a preoperative single oral dose of diclofenac sodium for control and prevention of postendodontic pain. Oral administration was preferred because the technique is clinically effective and convenient; the use of intramuscular or intravenous injection may lead to discomfort and fear and is not well accepted by some patients.[1,5,8] Most patients and dentists would prefer to provide an anti-inflammatory agent to be taken immediately before or self-administered as needed by the patient after anesthesia has worn off. However, in the present research, diclofenac sodium was administered 30 min before the conventional root canal therapy. Primary mechanism responsible for its anti-inflammatory, antipyretic, and analgesic actions is inhibition of prostaglandin synthesis by the inhibition of cyclooxygenase. Diclofenac may also be a unique member of the NSAIDs. There is some evidence that diclofenac inhibits the lipoxygenase pathways, thus reducing formation of the leukotrienes (also pro-inflammatory autacoids). There is also speculation that diclofenac may inhibit phospholipase A2 as part of its mechanism of action. These additional actions may explain the high potency of diclofenac — it is the most potent NSAID on a broad basis.[12]
However, there are few clinical trials (involving endodontic and oral surgery procedures) that evaluate the optimal moment for oral analgesic/anti-inflammatory agent administration. Certain studies report preoperative prescriptions ranging in duration from 1 to 12 h.[5,17,18] This double-blind randomized trial allowed sufficient comparison between both groups. The sample was distributed similarly regarding age, gender, and teeth to avoid bias. Although certain studies have shown a relationship between preoperative and postoperative pain,[11,19] single or multiple visit, vital/nonvital teeth, single/multi rooted teeth, abscess, varied anatomy, asymptomatic teeth, etc., can also present postendodontic pain.[1,8] Further, future clinical trials are required to show an efficacy of pretreatment analgesics to prevent postendodontic pain.[13,14,15,19]
CONCLUSION
Despite the limitations of the present study, postendodontic pain was substantially reduced by preoperative administration of a single oral dose of diclofenac sodium as compared to the placebo group. It is possible that these favorable results might help to prevent postendodontic pain, especially in patients with a low pain threshold.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marshall JG. Consideration of steroids for endodontic pain. Endod Topics. 2002;3:41–51. [Google Scholar]
- 2.Jalalzadeh SM, Mamavi A, Shahriari S, Santos FA, Pochapski MT. Effect of pretreatment prednisolone on postendodontic pain: A double-blind parallel-randomized clinical trial. J Endod. 2010;36:978–81. doi: 10.1016/j.joen.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 3.Pochapski MT, Santos FA, de Andrade ED, Sydney GB. Effect of pretreatment dexamethasone on postendodontic pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:790–5. doi: 10.1016/j.tripleo.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Ince B, Ercan E, Dalli M, Dulgergil CT, Zorba YO, Colak H. Incidence of postoperative pain after single- and multi-visit endodontic treatment in teeth with vital and non-vital pulp. Eur J Dent. 2009;3:273–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Pilatti GL, André dos Santos F, Bianchi A, Cavassim R, Tozetto CW. The use of celecoxib and dexamethasone for the prevention and control of postoperative pain after periodontal surgery. J Periodontol. 2006;77:1809–14. doi: 10.1902/jop.2006.060128. [DOI] [PubMed] [Google Scholar]
- 6.Leone M, Richard O, Antonini F, Rousseau S, Chabaane W, Guyot L, et al. Comparison of methylprednisolone and ketoprofen after multiple third molar extraction: A randomized controlled study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e7–9. doi: 10.1016/j.tripleo.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Alexander RE, Throndson RR. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:406–15. doi: 10.1067/moe.2000.109778. [DOI] [PubMed] [Google Scholar]
- 8.Glassman G, Krasner P, Morse DR, Rankow H, Lang J, Furst ML. A prospective randomized double-blind trial on efficacy of dexamethasone for endodontic interappointment pain in teeth with asymptomatic inflamed pulps. Oral Surg Oral Med Oral Pathol. 1989;67:96–100. doi: 10.1016/0030-4220(89)90310-1. [DOI] [PubMed] [Google Scholar]
- 9.Liesinger A, Marshall FJ, Marshall JG. Effect of variable doses of dexamethasone on posttreatment endodontic pain. J Endod. 1993;19:35–9. doi: 10.1016/S0099-2399(06)81039-3. [DOI] [PubMed] [Google Scholar]
- 10.Krasner P, Jackson E. Management of post treatment endodontic pain with oral dexamethasone: A double-blind study. Oral Surg Oral Med Oral Pathol. 1986;62:187–90. doi: 10.1016/0030-4220(86)90044-7. [DOI] [PubMed] [Google Scholar]
- 11.Gopikrishna V, Parameswaran A. Effectiveness of prophylactic use of rofecoxib in comparison with ibuprofen on postendodontic pain. J Endod. 2003;29:62–4. doi: 10.1097/00004770-200301000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Torabinejad M, Cymerman JJ, Frankson M, Lemon RR, Maggio JD, Schilder H. Effectiveness of various medications on postoperative pain following complete instrumentation. J Endod. 1994;20:345–54. doi: 10.1016/S0099-2399(06)80098-1. [DOI] [PubMed] [Google Scholar]
- 13.Menhinick KA, Gutmann JL, Regan JD, Taylor SE, Buschang PH. The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int Endod J. 2004;37:531–41. doi: 10.1111/j.1365-2591.2004.00836.x. [DOI] [PubMed] [Google Scholar]
- 14.Attar S, Bowles WR, Baisden MK, Hodges JS, McClanahan SB. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J Endod. 2008;34:652–5. doi: 10.1016/j.joen.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Ryan JL, Jureidini B, Hodges JS, Baisden M, Swift JQ, Bowles WR. Gender differences in analgesia for endodontic pain. J Endod. 2008;34:552–6. doi: 10.1016/j.joen.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 16.Williamson A, Hoggart B. Pain: A review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 17.Schmelzeisen R, Frölich JC. Prevention of postoperative swelling and pain by dexamethasone after operative removal of impacted third molar teeth. Eur J Clin Pharmacol. 1993;44:275–7. doi: 10.1007/BF00271371. [DOI] [PubMed] [Google Scholar]
- 18.Schultze-Mosgau S, Schmelzeisen R, Frölich JC, Schmele H. Use of ibuprofen and methylprednisolone for the prevention of pain and swelling after removal of impacted third molars. J Oral Maxillofac Surg. 1995;53:2–7. doi: 10.1016/0278-2391(95)90486-7. [DOI] [PubMed] [Google Scholar]
- 19.Menke ER, Jackson CR, Bagby MD, Tracy TS. The effectiveness of prophylactic etodolac on postendodontic pain. J Endod. 2000;26:712–5. doi: 10.1097/00004770-200012000-00010. [DOI] [PubMed] [Google Scholar]


