Abstract
Background:
No studies compared parenteral dexmedetomidine with its use as an adjuvant to ophthalmic block. We compared between adding dexmedetomidine to bupivacaine in peribulbar block and intravenous (IV) dexmedetomidine during peribulbar block for cataract surgery.
Materials and Methods:
A prospective, randomized, double-blind study on 90 patients for cataract surgery under peribulbar anesthesia. Study included three groups; all patients received 10 ml of peribulbar anesthesia and IV infusion of drugs as follows: Group I: Received a mixture of bupivacaine 0.5% (4.5 ml) + lidocaine 2% (4.5 ml) + normal saline (1 ml) + 150 IU hyaluronidase + IV infusion of normal saline, Group II: Received mixture of bupivacaine 0.5% (4.5 ml) + lidocaine 2% (4.5 ml) + dexmedetomidine 50 μg (1 ml) +150 IU hyaluronidase + IV infusion of normal saline and Group III: Received mixture of bupivacaine 0.5% (4.5 ml) + lidocaine 2% (4.5 ml) + normal saline (1 ml) +150 IU hyaluronidase + IV dexmedetomidine 1 μg/kg over 10 min; followed by 0.4 μg/kg/h IV infusion. We recorded onset, duration of block, Ramsay Sedation Score, intra-ocular pressure (IOP), hemodynamics, and adverse effects.
Results:
There was a significant decrease in the onset of action and increase in the duration of block in Group II as compared with the Group I and Group III. Mean Ramsay Sedation Score was higher in Group III. The IOP showed a significant decrease in Group II and Group III 10 min after injection (P < 0.01). Heart rate showed a significant decrease in Group III in comparison with the two other groups (P < 0.05). Only two patients in Group III developed bradycardia.
Conclusion:
Dexmedetomidine as an additive shortens onset time, prolong block durations and significantly decreases the IOP with minimal side effects. IV dexmedetomidine, in addition, produces intra-operative sedation with hemodynamic stability.
Keywords: Cataract surgery, dexmedetomidine, peribulbar block
Introduction
Ocular surgery may be performed under topical, regional or general anesthesia. The first recorded use of regional anesthesia for surgery was the instillation of cocaine into the conjunctival sac in 1884 by an Austrian ophthalmologist.[1] Recently, a major change in anesthetic practice has taken place, and the majority of ophthalmic surgical patients now undergo regional rather than general anesthesia. This change has been driven in part by the pressure to undertake surgical procedures as day cases, regional anesthesia is more economic, easy to perform, and the risk involved is less. Orbital regional anesthesia can be done using a retrobulbar (intra-conal) block peribulbar (extra-conal) block or sub-Tenon's block.
Davis and Mandel[2] in 1986 described the peribulbar block, peribulbar block has delayed onset and need a higher volume of local anesthetic (LA) than a retrobulbar block. But peribulbar block is away from intra-conal space and so produce fewer complication.[3,4]
Many additives such as clonidine, hyaluronidase, sodium bicarbonate, muscle relaxants, and opioids were added to LAs drugs in the ocular block for rapid the onset and long the duration of analgesic effect of LA.[5,6,7,8]
Dexmedetomidine is a selective alpha two adrenoreceptor agonist. It provides dose-dependent sedation, analgesia, sympatholysis, and anxiolysis without relevant respiratory depression.[9] Now, dexmedetomidine is used as adjuvant to LA drugs in peripheral nerve block, brachial plexus block and intrathecal anesthesia with satisfactory results.[10] Our study aimed to compare between intravenously (IV) administered dexmedetomidine and its use as an additive to LA for peribulbar block. The comparison focused on the efficacy and safety of dexmedetomidine in either situation.
Materials and Methods
This prospective randomized, double-blind, and controlled study was conducted on 90 patients American Society of Anesthesiologists I and II, age ranged between 28 and 65 years and scheduled for eye surgery under local peribulbar anesthesia.
Patient informed written consent and Local Ethical Committee approval have been obtained before patient's allocation.
Exclusion criteria included age younger than 18 years, the usual contraindications for regional anesthesia such as patients refusing LA, clotting abnormalities, impaired mental status, or allergy to any of the study medications. Furthermore, patients were excluded if they had the severe cardiac disease, chronic obstructive lung disease, and a history of sleep apnea.
These patients were randomly allocated using a computer-generated list into three equal groups all received 10 ml of local peribulbar anesthesia and IV infusion of drugs as follows:
Group I (control group): Received mixture of bupivacaine 0.5% (4.5 ml) + lidocaine 2% (4.5 ml) + normal saline (1 ml) +150 IU hyaluronidase + IV infusion of normal saline.
Group II: Received mixture of bupivacaine 0.5% (4.5 ml) + lidocaine 2% (4.5 ml) + dexmedetomidine 50 μg (1 ml) + 150 IU hyaluronidase + IV infusion of normal saline.
Group III: Received mixture of bupivacaine 0.5% (4.5 ml) + lidocaine 2% (4.5 ml) + normal saline (1 ml) + 150 IU hyaluronidase + IV dexmedetomidine 1 μg/kg over 10 min; followed by 0.4 μg/kg/h IV infusion.
All infusions were started just before peribulbar injection and stopped at the end of surgery.
At the preoperative visit, the anesthetic technique and study protocol were explained to the patients in details. The patients fasted for 8 h and were un-premedicated to the operating room. A peripheral IV line inserted and standard monitoring including noninvasive blood pressure (BP), five leads electrocardiography, heart rate (HR), and oxygen saturation applied. Supplemental O2 at 2 L/min via nasal cannula was used throughout the procedure.
26-G, 13 mm a short beveled needle 26-G, 13-mm inserted through the conjunctiva in the inferotemporal quadrant as far laterally as possible. The needle directed perpendicularly parallel to the orbital floor for the whole length of the needle then 5 ml of study drug mixture injected slowly after negative aspiration to avoid intravascular injection. The remaining 5 ml of the drug injected at 2 mm medial and inferior to the supraorbital notch. Then ocular massage applied gently to the eyeball.
The following measures were assessed:
Onset of block: Time started from injection of LAs till complete paralysis of lids and globe.
Duration of block which was the time started from complete block till eyes move freely.
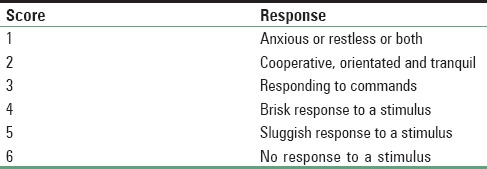
Sedation level: By Ramsay Sedation Scale at every 10 min during surgery and every 30 min during first 2 h [Table 1][11]
Intra-ocular pressure (IOP): Before injection of LA (baseline) and after a complete akinesia of the globe before surgical incision.
Patients’ hemodynamics: HR and mean arterial blood pressure (MAP) recorded every 5 min. During the surgery and in the immediate postoperative period (at 15 and 30 min).
- Adverse effects including all of the following:
- Bradycardia (HR <50 beats/min).
- Hypotension (MAP <50 mmHg sustained for more than 10 min).
- Respiratory rate (RR) depression (RR <10/min).
- Oxygen desaturation (SpaO2 <92%) recorded.
Table 1.
Ramsay Sedation Scale
Statistical analysis
Data analysis was done using SPSS version 21(Armonk, NY: IBM Corp). Quantitative data presented as mean and standard deviation and were analyzed by one-way ANOVA test. MAP and HR data were analyzed by repeated measure ANOVA test. Qualitative data presented as numbers and percentage and were analyzed using Chi-square test.
Results
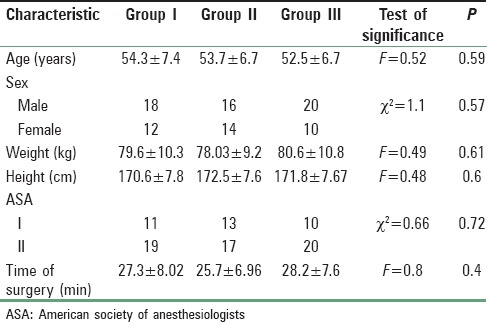
Demographic characteristics and time of the procedure showed the nonsignificant difference among groups [Table 2].
Table 2.
Demographic characteristics
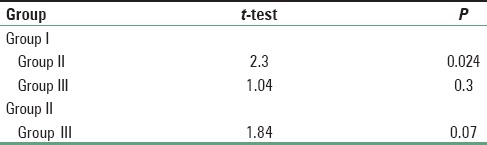
There was a significant decrease in the onset of the block in Group II in comparison with both other groups. Post-hoc analysis revealed no difference between Groups I and III [Table 3a and b].
Table 3a.
Onset of block
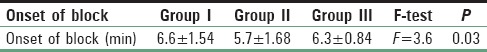
Table 3b.
Onset of block
Duration of the block in Group II patients showed a significant increase in the length of the block followed by Group III in comparison with Group I [Table 4a and b].
Table 4a.
Duration of block
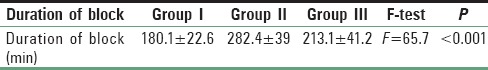
Table 4b.
Duration of block
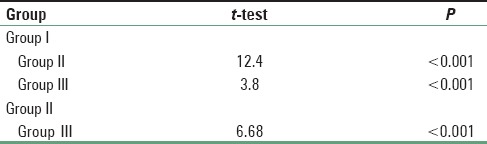
Mean Ramsay Sedation Score in Group III showed a significant increase in comparison with the two other groups while there was no significant difference between Group I and Group II [Figure 1].
Figure 1.
Ramsay sedation score
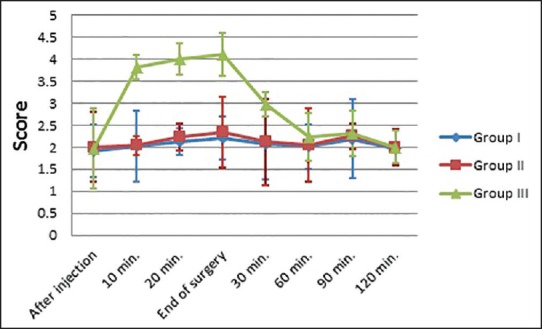
There was a significant decrease in IOP in Group II and Group III 10 min after injection. Post-hoc analysis revealed that Group III showed a significant decrease in comparison with Groups I and II. It also revealed that Group II showed a highly significant decrease in comparison with Group I (P < 0.005) [Table 5a and b].
Table 5a.
Comparison among groups regarding intra-ocular pressure (mmHg)
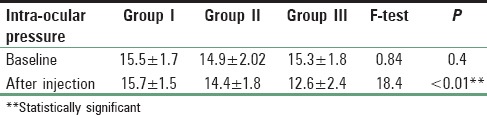
Table 5b.
Comparison among groups regarding intra-ocular pressure (mmHg)
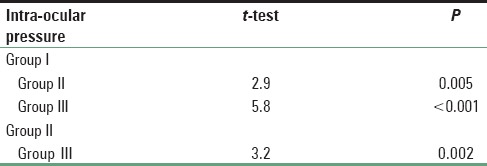
Heart rate showed a significant decrease in Group III as compared to the other two groups (P < 0.05) during the time of dexmedetomidine infusion. MAP showed a nonsignificant difference among groups [Figures 2 and 3].
Figure 2.
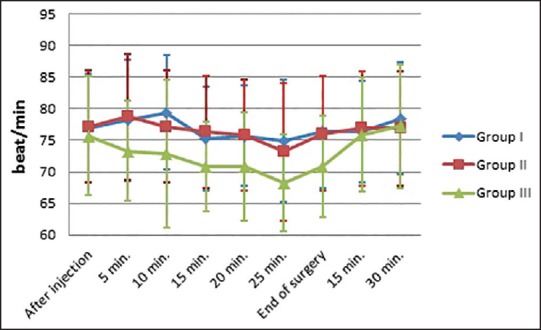
Comparison among groups regarding heart rate
Figure 3.
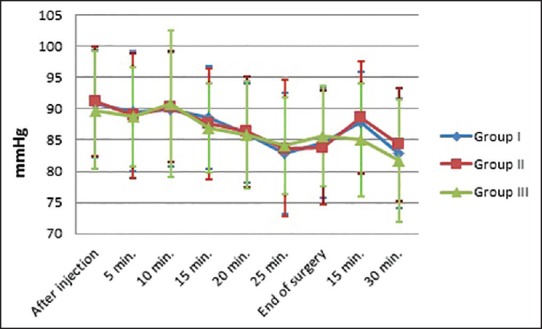
Comparison among groups regarding mean arterial blood pressure
Regarding complications, only two patients in Group III developed bradycardia treated by atropine 0.01 mg/kg.
Discussion
Dexmedetomidine is a selective alpha two adrenoreceptor agonist. It provides dose-dependent sedation and analgesia without relevant respiratory depression, now dexmedetomidine is used as adjuvant to LA drugs in peripheral nerve block and eye block.
In this study, we noticed that there was a significant decrease in the onset of block when use dexmedetomidine as adjuvant to LA in patients undergoing cataract surgery with peribulbar block (Group II) 5.7 ± 1.68 min in comparison to when use LA alone (Group I) 6.6 ± 1.54 min or when use dexmedetomidine as IV sedation with peribulbar block (Group III) 6.3 ± 0.84 min P = 0.03. On the other hand, duration of the block showed a significant increase in the length of the block in Group II 282.4 ± 39 min followed by Group III 213.1 ± 41.2 min in comparison with Group I 180.1 ± 22.6 min P < 0.001. About adequate level of sedation, mean Ramsay sedation score in Group III showed a significant increase in comparison with the two other groups while there was no significant difference between Group I and Group II. Furthermore, there was a significant decrease in IOP in Group II 14.4 ± 1.8 mmHg and Group III 12.6 ± 2.4 mmHg 10 min after injection in comparison to group I 15.7 ± 1.5 mmHg, post-hoc analysis revealed that Group III showed a significant decrease in comparison with Groups I and II. It also revealed that Group II showed a highly significant decrease in comparison with Group I (P < 0.005). Finally, HR showed a significant decrease in Group III as compared to the other two groups (P < 0.05). But MAP showed a nonsignificant difference among groups.
The effect of dexmedetomidine as an adjuvant to LA in patients undergoing cataract surgery with peribulbar block in the present study accepted by Channabasappa et al.[12] reported that a combination of bupivacaine and lidocaine with dexmedetomidine in peribulbar anesthesia provides the sedation that enables full cooperation. This mixture also helps to decrease the IOP significantly, shorten sensory and motor block onset time and extend motor and sensory block durations.
And this goes in line with the current study carried out by Memis et al.[13] who concluded that the addition of 0.5 μg/kg dexmedetomidine to lidocaine 1% for IV regional anesthesia (IVRA) improves quality of anesthesia and perioperative analgesia without causing side effects. Furthermore, Kol et al.,[14] found that the addition of dexmedetomidine to prilocaine in IVRA led to shortened sensory block onset time and prolonged sensory block recovery time without causing adverse effects. Esmaoglu et al.[15] reported that dexmedetomidine as an adjuvant to levo-bupivacaine for axillary brachial plexus block markedly prolongs the duration of the block and shortens the onset time in addition to prolongation of postoperative analgesia.
In the present study, IV administration of dexmedetomidine during peribulbar block, prolongs the duration of block, decreases the IOP and provides a satisfactory level of intra-operative sedation with hemodynamic stability. Although akinesia and analgesia can be achieved with a regional block, appropriate sedation may lower the IOP and pain on injection, prevent the hypertensive response to anxiety and LA injection, and provide patient comfort. The mechanism of action of dexmedetomidine is activation of the receptors in the brain, and spinal cord inhibits neuronal firing by presynaptic activation of the α2 adrenoceptor inhibits the release of norepinephrine, terminating the propagation of pain signals. Postsynaptic activation of α2 adrenoceptors in the central nervous system inhibits the sympathetic activity and thus can decrease BP and HR. Combined, these effects can produce analgesia, sedation; also the responses to activation of the receptors include contraction of vascular and other smooth muscle and decreased IOP.
Abdalla et al.[16] who studied the effects of IV infusions of a small dose of dexmedetomidine during ophthalmic surgery under LA (0.5 μg/kg.) for 10 min followed by (0.2 μg/kg/h) for 50 min. They noticed that the dexmedetomidine in that dose has an adequate control of HR, BP and decreases IOP in addition to a sedative effect.
Rutkowska et al.[17] examined the effect of parenteral dexmedetomidine on patients with the end-stage renal disease during brachial plexus block and concluded that it can prolong the duration of brachial plexus block.
The previous studies[12,13,14,15,16,17] provide an evidence that dexmedetomidine through either parenteral or systemic route can augment the regional blocks. Our study represents another aspect for the augmentation of the regional blocks but this time in the ophthalmic regional block.
Conclusion
Dexmedetomidine is a useful drug as an additive to bupivacaine in peribulbar anesthesia, as it shortens onset time, prolong block durations, significantly decreases the IOP with minimal side effects. On the other hand, IV administration of dexmedetomidine during peribulbar block, extending the time of block, reduces the IOP and provides a satisfactory level of intra-operative sedation with hemodynamic stability.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Goerig M, Bacon D, van Zundert A. Carl Koller, cocaine, and local anesthesia: Some less known and forgotten facts. Reg Anesth Pain Med. 2012;37:318–24. doi: 10.1097/AAP.0b013e31825051f3. [DOI] [PubMed] [Google Scholar]
- 2.Davis DB, 2nd, Mandel MR. Posterior peribulbar anesthesia: An alternative to retrobulbar anesthesia. J Cataract Refract Surg. 1986;12:182–4. doi: 10.1016/s0886-3350(86)80040-2. [DOI] [PubMed] [Google Scholar]
- 3.Davis DB, 2nd, Mandel MR. Efficacy and complication rate of 16,224 consecutive peribulbar blocks. A prospective multicenter study. J Cataract Refract Surg. 1994;20:327–37. doi: 10.1016/s0886-3350(13)80586-x. [DOI] [PubMed] [Google Scholar]
- 4.Riad W, Akbar F. Ophthalmic regional blockade complication rate: A single center audit of 33,363 ophthalmic operations. J Clin Anesth. 2012;24:193–5. doi: 10.1016/j.jclinane.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Eldeen HM, Faheem MR, Sameer D, Shouman A. Use of clonidine in peribulbar block in patients undergoing cataract surgery. Aust J Basic Appl Sci. 2011;5:247–50. [Google Scholar]
- 6.Sarvela PJ. Comparison of regional ophthalmic anesthesia produced by pH-adjusted 0.75% and 0.5% bupivacaine and 1% and 1.5% etidocaine, all with hyaluronidase. Anesth Analg. 1993;77:131–4. doi: 10.1213/00000539-199307000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Zahl K, Jordan A, McGroarty J, Sorensen B, Gotta AW. pH-adjusted bupivacaine and hyaluronidase for peribulbar block. Anesthesiology. 1990;72:230–2. doi: 10.1097/00000542-199002000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Abdellatif AA, El Shahawy MA, Ahmed AI, Almarakbi WA, Alhashemi JA. Effects of local low-dose rocuronium on the quality of peribulbar anesthesia for cataract surgery. Saudi J Anaesth. 2011;5:360–4. doi: 10.4103/1658-354X.87263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paris A, Tonner PH. Dexmedetomidine in anesthesia. Curr Opin Anaesthesiol. 2005;18:412–8. doi: 10.1097/01.aco.0000174958.05383.d5. [DOI] [PubMed] [Google Scholar]
- 10.Gandhi RR, Shah AA, Patel I. Use of dexmedetomidine along with bupivacaine for brachial plexus block. Natl J Med Res. 2012;2:67–9. [Google Scholar]
- 11.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Channabasappa SM, Shetty VR, Dharmappa SK, Sarma J. Efficacy and safety of dexmedetomidine as an additive to local anesthetics in peribulbar block for cataract surgery. Anesth Essays Res. 2013;7:39–43. doi: 10.4103/0259-1162.113987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Memis D, Turan A, Karamanlioglu B, Pamukçu Z, Kurt I. Adding dexmedetomidine to lidocaine for intravenous regional anesthesia. Anesth Analg. 2004;98:835–40. doi: 10.1213/01.ane.0000100680.77978.66. [DOI] [PubMed] [Google Scholar]
- 14.Kol IO, Ozturk H, Kaygusuz K, Gursoy S, Comert B, Mimaroglu C. Addition of dexmedetomidine or lornoxicam to prilocaine in intravenous regional anesthesia for hand or forearm surgery: A randomized controlled study. Clin Drug Investig. 2009;29:121–9. doi: 10.2165/0044011-200929020-00006. [DOI] [PubMed] [Google Scholar]
- 15.Esmaoglu A, Yegenoglu F, Akin A, Turk CY. Dexmedetomidine added to levobupivacaine prolongs axillary brachial plexus block. Anesth Analg. 2010;111:1548–51. doi: 10.1213/ANE.0b013e3181fa3095. [DOI] [PubMed] [Google Scholar]
- 16.Abdalla MI, Al Mansouri F, Bener A. Dexmedetomidine during local anesthesia. J Anesth. 2006;20:54–6. doi: 10.1007/s00540-005-0351-z. [DOI] [PubMed] [Google Scholar]
- 17.Rutkowska K, Knapik P, Misiolek H. The effect of dexmedetomidine sedation on brachial plexus block in patients with end-stage renal disease. Eur J Anaesthesiol. 2009;26:851–5. doi: 10.1097/EJA.0b013e32832a2244. [DOI] [PubMed] [Google Scholar]


