Abstract
Ventilator associated pneumonia (VAP) is the most common nosocomial infection in Intensive Care Unit. One major factor causing VAP is the aspiration of oral colonization because of poor oral care practices. We feel the role of simple measure like oral care is neglected, despite the ample evidence of it being instrumental in preventing VAP.
Keywords: Nursing practice, oral care, oral hygiene, ventilator-associated pneumonia
Introduction
Ventilation associated pneumonia (VAP) is the most common nosocomial infection in Intensive Care Units (ICUs), with its risk increasing at a rate of 1-3% per day of intubation, signifying 6-20 fold higher risk of developing pneumonia compared to nonventilated ICU patients.[1,2]
Patients with VAP have a longer stay in ICU, and there is an increase in total hospital length of stay averaging an additional 7-9 days.[3,4] VAP also increase health costs and mortality. It is recognized that 36-60%[4] of all health associated infection-related deaths are attributable to VAP. Many techniques are employed to achieve better outcome like the head of bed elevation, daily interruption of sedation to decrease time on mechanical ventilation, prevention of deep vein thrombosis.[5]
Aspiration of oral colonization has been identified as one of the common causes of VAP in ICU,[6] as a result of poor oral care. Whenever endotracheal (ET) tube is in place, most defenses against pneumonia are impaired. The ET tube bypasses the normal filtration and physical capture functions as there is no nasal warming and humidification. The mucociliary defense mechanism is also compromised by ET tube. ET tube disrupts normal mucus clearance, and there is a collection of secretions above the cuff, which contaminates subglottic pool. Contaminated secretions can drain into the trachea and can be aspirated into lungs. ET tube further inhibits cough mechanisms. The oral flora of critically ill adult patients differs from that of a normal healthy adult. Within 48 h of intubation, there is a depletion of fibronectin which is responsible for the predominance of Gram-negative organisms, replacing normally found Gram-positive organisms.[2] Lack of effective oral hygiene, dental plaque deposits develop on the teeth within 72 h which could be reservoirs for potential respiratory pathogens.
Saliva plays an important role in oral clearance with mastication and swallowing. It has an important enzyme, lysozyme that inhibits bacterial growth. In ICU, external stresses result in increased drying of mucosa thereby increasing the risk of caries, periodontal disease, etc. Greater the level of oral bacteria the greater is the amount of biofilm attached to the patient's teeth.
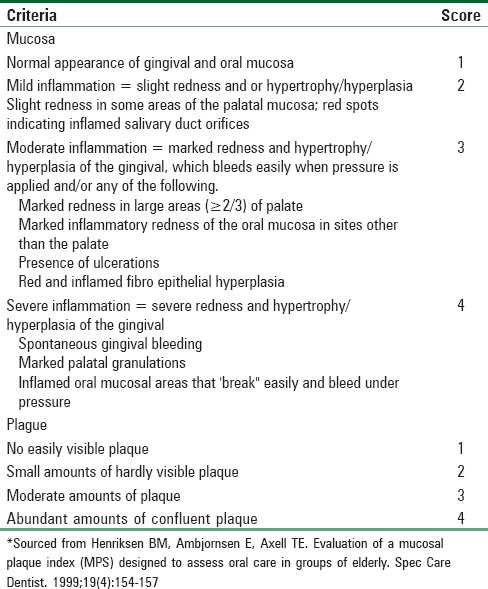
Oral assessment can be done casing Modified Beck Oral Assessment Scale[7] [Table 1] and Mucosal Plaque Score[8] [Table 2]. During a general oral examination, dentist assesses the condition of lips and intraoral soft tissues and look for any hard or soft tissue pathology. Nurses are best to carry out the general assessment.
Table 1.
Beck oral assessment scale (BOAS), modifieda
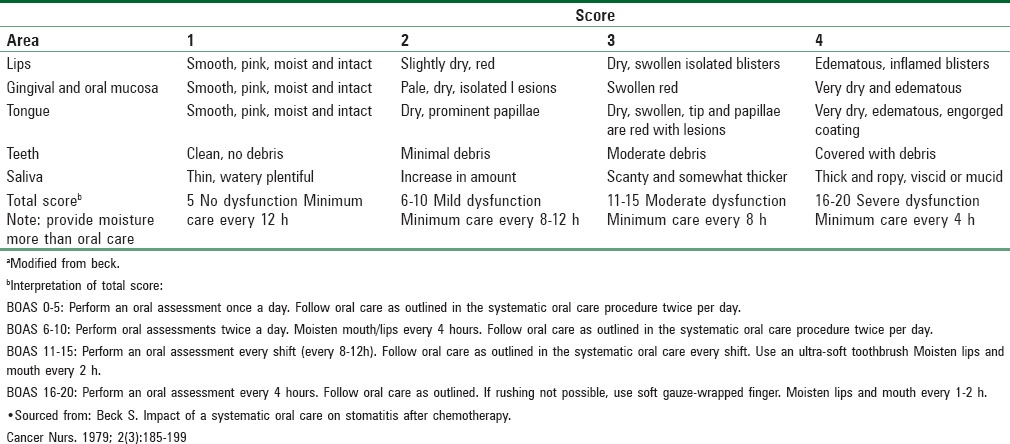
Table 2.
Mucosal plaque score
Centre for disease control and prevention[9] has developed evidence-based patient care treatment practices for reducing VAP. It has been found that incorporation of routine oral hygiene may reduce VAP by as much as 60%.[4] Such practices should include brushing teeth, gums, and tongue at least twice a day with a soft pediatric toothbrush and moistening oral mucosa and lips every 2-4 h. They also recommend the use of 0.12% oral chlorhexidine to rinse the oral cavity twice daily and to suction oral cavity/pharynx in addition to brushing use oral swabs with 1.5% hydrogen peroxide to clean plaque from mouth.
It is necessary that every heath care institution must have written an oral care protocol and training plan so that the patient receives comprehensive oral care in a consistent manner.
The aim of oral hygiene is the regular removal of plaque from the teeth twice daily especially along the gingival margin and proximal tooth surface to prevent periodontal disease. Appropriate treatment of xerostomia, aphthous ulcers, and candidiasis should be done. Teeth should be regularly cleaned with a toothbrush. Soft bristled pediatric toothbrush is recommended for brushing, flossing is also recommended but there is a risk of gingival trauma. Mechanical plaque removal is shown to be very effective in ICU.
The preferred treatment for dry mouth is regular moistening of oral mucosa with water or normal saline, the use of saliva substitute or application of moistening gel. Toothpaste is not essential for efficient plague removal, but its use has the advantage of increased mechanical cleaning application of topical fluoride and refreshing taste.
Recommended Oral Care Interventions for Ventilated Patients[10]
Assessment of oral cavity
Intervention
Conduct an initial admission as well as daily assessment of the lips, oral tissue, tongue teeth, and saliva of each patient on a mechanical ventilator.
Rationale
Assessment allows for initial and early identification of oral hygiene problems and for continued observation of oral health.
Maintain saliva
Intervention
Unit specific protocols should be implemented that assist patients at risk of VAP in maintaining saliva production, oral tissue health, and minimizing the development of mucositis.
Rationale
Saliva provides both mechanical and immunological effects which act to remove pathogens colonizing the oropharynx.
Elevate head
Intervention
Keep the head of the bed elevated at at least 30° (unless medically contraindicated) and position patient so that oral secretion pool into buccal pocket; especially important during such activities as feeding and brushing teeth.
Rationale
Elevation aids in preventing reflux and aspiration of gastric contents; oral secretions may drain into a subglottic area where they become rapidly colonized with pathogenic bacteria.
Subglottic suctioning
Intervention
Patients oral and subglottic secretions should be suctioned continuously or intermittently/routinely with the frequency dependent upon secretion production.
Rationale
Minimize aspiration of contaminated secretion into lung.
Conclusion
Pneumonia is a prevalent disease that is responsible for approximately 75% of all hospital acquired infections. Because of the severity of this disease, it is necessary that medical personnel to have knowledge about risk factors for the development of hospital-acquired Pneumonia and the prevention strategies. Ventilated patients are more at risk as their normal host defense mechanism are impaired. One basic prevention strategy is comprehensive oral care protocol. The rapid potentially pathologic charges that occur in the ventilated patients’ oral environment make oral care a critical component of Hospital Acquired Pneumonia.
Nurses should be properly trained, in general, oral care. Comprehensive oral care should include plaque removal and stimulation of salivary flow. When nurses (and the hospital administration) fully understand the importance of providing oral care, patients’ lives can be spared, and financial recourses can be saved.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Safdar N, Crnich CJ, Maki DG. The pathogenesis of ventilator-associated pneumonia: Its relevance to developing effective strategies for prevention. Respir Care. 2005;50:725–39. [PubMed] [Google Scholar]
- 2.Munro CL, Grap MJ. Oral health and care in the intensive care unit: State of the science. Am J Crit Care. 2004;13:25–33. [PubMed] [Google Scholar]
- 3.Scannapieco FA, Wang B, Shiau HJ. Oral bacteria and respiratory infection: Effects on respiratory pathogen adhesion and epithelial cell proinflammatory cytokine production. Ann Periodontol. 2001;6:78–86. doi: 10.1902/annals.2001.6.1.78. [DOI] [PubMed] [Google Scholar]
- 4.Dennesen P, van der Ven A, Vlasveld M, Lokker L, Ramsay G, Kessels A, et al. Inadequate salivary flow and poor oral mucosal status in intubated intensive care unit patients. Crit Care Med. 2003;31:781–6. doi: 10.1097/01.CCM.0000053646.04085.29. [DOI] [PubMed] [Google Scholar]
- 5.Soh KL, Shariff Ghazali S, Soh KG, Abdul Raman R, Sharif Abdullah SS, Ong SL. Oral care practice for the ventilated patients in intensive care units: A pilot survey. J Infect Dev Ctries. 2012;6:333–9. doi: 10.3855/jidc.1634. [DOI] [PubMed] [Google Scholar]
- 6.Paju S, Scannapieco FA. Oral biofilms, periodontitis, and pulmonary infections. Oral Dis. 2007;13:508–12. doi: 10.1111/j.1601-0825.2007.1410a.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck S. Impact of a systematic oral care protocol on stomatitis after chemotherapy. Cancer Nurs. 1979;2:185–99. [PubMed] [Google Scholar]
- 8.Henriksen BM, Ambjørnsen E, Axéll TE. Evaluation of a mucosal-plaque index (MPS) designed to assess oral care in groups of elderly. Spec Care Dentist. 1999;19:154–7. doi: 10.1111/j.1754-4505.1999.tb01378.x. [DOI] [PubMed] [Google Scholar]
- 9.Hixson S, Sole ML, King T. Nursing strategies to prevent ventilator-associated pneumonia. AACN Clin Issues. 1998;9:76–90. doi: 10.1097/00044067-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Garcia R. A review of the possible role of oral and dental colonization on the occurrence of health care-associated pneumonia: Underappreciated risk and a call for interventions. Am J Infect Control. 2005;33:527–41. doi: 10.1016/j.ajic.2005.02.005. [DOI] [PubMed] [Google Scholar]


