Brief Summary
We assessed the impact of quality improvement projects, including a patient motivational program, implemented over a 2 year period. Median patient attendance and completion rates increased significantly. Motivational programs appear helpful in increasing participation in early outpatient cardiac rehabilitation
Keywords: Cardiac Rehabilitation, Participation, Completion, Adherence, Quality Improvement
Introduction
Recent studies have demonstrated a dose-response benefit in cardiac rehabilitation (CR), in that patients who attend more CR sessions have lower subsequent mortality rates than those who attend fewer sessions.1-3 This effect size is substantial suggesting a 1% mortality reduction for each session of CR attended.2, 3
These findings created a new imperative to increase the number of CR sessions per patient. A number of psychosocial interventions have previously been tested, but results have been mixed and study quality is markedly heterogeneous.4 Furthermore, many of these interventions were time and labor intensive (such as counseling and home visits) and were probably costly. Consequently, there remains a significant lack of effective strategies which significantly increase the average number of sessions per patient during CR without significantly adding to cost or program burden.
In addition, incentive (or motivational) programs have recently been shown to improve outcomes in other behavioral domains such as smoking cessation,5 weight loss,6 and workplace physical activity.7 If used appropriately, incentives are generally considered acceptable for motivating healthy behavior change.8
To our knowledge, no published studies have tested the impact of quality improvement and motivational interventions on CR attendance, although this idea has been recently proposed.9 To this end, we carried out an analysis of our recent experience with quality improvement and motivational interventions. We hypothesized that our quality improvement projects would effectively improve CR attendance and completion.
Patients and Methods
We retrospectively analyzed all participants who enrolled in CR at Mayo Clinic, MN by attending ≥1 session of CR during the study period of May 2009 to January 2012. Data were collected in mid May 2012 which allowed nearly 5 months for CR completion. We excluded patients who lacked a valid research consent, a full intake assessment, or who utilized our program for activities other than phase II outpatient CR. We obtained patient billing records and tabulated the total number of sessions for each episode of CR per patient. We grouped patients by start month, calculated the average number of sessions per patient group per month, and then linked these averages to the timing of our quality improvement interventions. We excluded patients who enrolled after January 2012 due to insufficient follow-up time (<5 months) for completion of CR. This study was reviewed and approved by [our] Institutional Review Board.
Policy and Program Interventions
Prior to 2010, our CR program customized the recommended number of cardiac rehabilitation sessions based on individual patient characteristics and progress toward goals. Patients who progressed quickly graduated from CR after relatively few sessions, but those with greater baseline disability or slower progress were held for the maximal number of sessions. However, in approximately March 2010, shortly after the publication by Hammill et al.2, this policy was changed to recommend a “full dose” of CR to all patients, in order to provide maximal benefits to all patients.
To further improve patient participation in CR, in November 2010 we implemented a 7 minute video, “Cardiac Rehabilitation: A Home for your Heart.” This video described the CR program and outlined the benefits of CR on mortality, morbidity, and quality of life. This video was shown to all CR-eligible inpatients prior to hospital discharge and on the first day of early outpatient CR. This video recently won a Silver Reel award for excellence in patient communication.10
Motivational Program Intervention
In July 2011, we introduced a motivational program in the Phase II program which was based upon a business-model performance management action plan. We monitored patient attendance and gave monthly feedback and reinforcement to all CR staff members.
Patients tracked their own attendance with a small punch card. As a reward, after every 6th session, (from session 6 to 36) patients were given, in order, a parking pass, a T-shirt, a water bottle, a second parking pass, a tote bag, and finally a long-sleeve sweatshirt. In general, the items were intended as token rewards. Their main purpose was to create regular reinforcement and encouragement from program staff.
A second major component of the motivational program plan was a parallel staff motivational program designed to help the patient program succeed. Similarly, staff members were given a punch card. This card was marked when staff members showed the video to a patient, gave a patient their first punch card, or when a patient obtained a reward. Similarly, the punch card was marked when patients who failed to keep appointments were rescheduled and attended a future CR exercise session. In these efforts, team work was encouraged and rewarded. The first reward for staff members was a choice of T-shirt, tote bag or water bottle. The second reward was a sweatshirt. The third reward was a choice of the remaining items. On average, it took staff members between 2-3 months of effort to obtain a reward.
Lastly, when a patient completed their 22nd session, their first name was written on a dry-erase white board labeled, “Cardiac Rehab All-Stars” which was displayed prominently near the entrance to CR. From that point on, each subsequent session from session 22 to session 36 was tracked for all patients attending CR to observe and to generate further encouragement and reinforcement.
Billing Codes
We utilized current procedural terminology (CPT) codes of 93798 and 93797 to determine the total number of CR sessions attended during the study period. CPT 93798 was the code for telemetry-monitored exercise sessions. CPT 93797 was the code used for non-monitored CR sessions, which included billing for dietitian visits, comprehensive nurse intakes, and physician-lead orientation sessions during CR. The maximal number of sessions included in this analysis was limited to 36 per patient per Medicare guidelines.
Completion
We defined completion of CR as attendance at ≥ 30 sessions but also utilized an additional definition of attendance at all 36 sessions. Although Hammill et al.2 used the 36 session cut off, we utilized a 30 session definition to more broadly capture a “full dose” of CR and allow for some slight disagreement between clinical and billing records among individual patients.
Financial Analysis
For cost analysis, we assumed that all patients reaching a session milestone were given the indicated reward. We assumed a full set of rewards for each staff member (15 total staff members.) We further estimated that daily program administration time accumulated to 30 minutes and multiplied this by the average hourly rate paid to bachelor’s level exercise-physiologist staff members. We obtained video production and reward costs. We calculated the number of sessions added per $100 spent on the given intervention. We did not include any indirect costs such as overhead, infrastructure, maintenance, or the increased use of existing program resources.
Statistical Analysis
Descriptive statistics were calculated for age, gender, race, body-mass index, and primary indication for CR. Because of skewness in the data, non-parametric tests were applied. We used Spearman’s correlation coefficient for average number of sessions by enrollment month and also report the number of sessions as median and interquartile ranges. We divided the cohort into 4 groups, one for each period that separated the various initiatives. By time period, group 1 (baseline) was from May 2009 to February 2010, group 2 (policy change) from March 2010 to October 2010, group 3 (video) from November 2010 to June 2011, and group 4 (motivational program) from July 2011 to January 2012. Wilcoxon ranked sum test was utilized to perform successive pair-wise comparisons between periods and between Olmsted county and non-Olmsted county patients within time periods. Chi-square testing was utilized to compare completion rates across the time periods. The differences in mean values between periods were utilized in the financial analysis.
Because this was a quality improvement project with improvement as the only expected outcome, we considered a one-sided p value of <0.05 as significant. All statistical testing was performed using JMP vs. 9.0.1 (SAS institute, Cary, NC.)
Results
We identified 1,151 patients eligible for analysis during the study period. We excluded 48 patients due to lack of valid research consent. Patient characteristics are found in Table 1. Our population was, on average, middle aged, mostly male, non-Hispanic white, and residents of Olmsted County. An average of 33 ± 7 patients enrolled per month with no change over the study period (p = 0.30.) There were 35 patients who enrolled in CR >1 time due to recurrent events, but these repeat enrollments were evenly distributed across study periods (Chi2 = 2.1, p = 0.33.)
Table 1.
Patient Demographic and Clinical Characteristics
| Baseline Characteristic (N=1103) | n |
|---|---|
| Demographics | |
| • Age, y (M±SD) | 64 ±13 |
| • Gender, male | 776 (70%) |
| • Non-Hispanic White (Caucasian) | 1010 (92%) |
| • Olmsted County | 670 (61%) |
| Cardiovascular risk factors | |
| • Hypertension | 803 (73%) |
| • Diabetes | 334 (30%) |
| • Former cigarette use | 183 (17%) |
| • Current cigarette use | 42 (4%) |
| • Body mass index, (kg/m2±SD) | 30±6 |
| Primary indication for cardiac rehabilitation | |
| • Angina | 172 (16%) |
| • Coronary artery bypass surgery | 186 (17%) |
| • Heart transplant | 63 (6%) |
| • Myocardial infarction | 269 (24%) |
| • Percutaneous coronary intervention | 226 (21%) |
| • Valve repair or replacement | 118 (11%) |
| • Other | 69 (6%) |
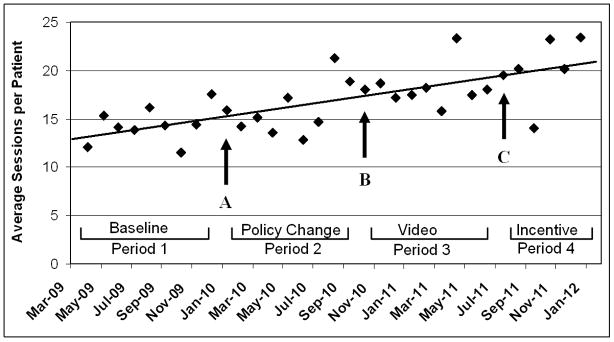
We found consistent and gradual improvement in average patient attendance at CR, r = 0.18, p <0.001 (Figure 1.) By period, average attendance (± SD) was 15 ± 11, 16 ± 12, 18 ± 12 and 20 ± 13 sessions per patient per period respectively. There was noticeable month-to-month variation but without clear seasonal or monthly trends.
Figure 1.
Quality Improvement Activities and Their Effects on Patient Attendance at Cardiac Rehabilitation
Each point represents the average number of sessions per patients enrolling in cardiac rehabilitation for the given month. Point A represents a policy change towards maximizing total number of sessions. Point B represents institution of the patient orientation video. Point C represents the institution of the motivational/incentive program. The comparative periods are shown visually. As seen, there is a significant positive trend in the average sessions per patient over time (r = 0.18, p < 0.001.)
We found significant improvements in the median attendance from period 1 to period 4 for all patients as well as for Olmsted Count and non-Olmsted County residents (Table 2.) Median attendance improved by 40% from 12 to 20 sessions/patient. The implementation of the video significantly improved median attendance (period 2 vs. 3) for all groups, but the reward program (period 3 vs. 4) demonstrated only significant improvements in Olmsted residents. For all time periods, Olmsted residents attended significantly more sessions than non-local residents (p < 0.001 for all comparisons).
Table 2.
Total Number of Cardiac Rehabilitation Sessions per Patient Group per Time Period
| Group | Time Perioda | P-value | ||||||
|---|---|---|---|---|---|---|---|---|
| 1b | 2 | 3 | 4 | 1 vs. 2 | 2 vs. 3 | 3 vs. 4 | 1 vs. 4 | |
| Total | 12 [5, 23] (314) | 12.5 [5, 26] (280) | 17 [7, 33] (266) | 20 [7, 35] (243) | .15 | .01 | .07 | <.001 |
| Olmsted County | 15 [6, 27] (176) | 16.5 [6, 29] (172) | 19 [8, 35] (164) | 27.5 [9, 35] (158) | .33 | .05 | .04 | <.001 |
| Non-Olmsted County | 9 [4, 17] (138) | 10 [5, 19] (108) | 13 [6, 23] (102) | 15 [5, 25] (85) | .22 | .02 | .47 | .004 |
| P-valuec | <.001 | <.001 | .001 | <.001 | ||||
Reported as median number of sessions per patient, [Interquartile range], (total number of patients)
Time period 1 was the baseline, period 2 followed the policy change, period 3 followed the introduction of the welcoming video, and period 4 followed the introduction of the motivational program.
P-value for Olmsted county vs. Non-Olmsted county patients
Table 3 shows the average attendance by indication for CR as well as the overall responsiveness to program changes. Among all subgroups, older patients (age ≥ 65 years) were the most responsive group to program interventions and demonstrated a median increase of 16.5 sessions per patient improving from 13.5 [6 to 26] to 30 [10 to 35] for period 1 to 4 respectively, (p < 0.001).
Table 3.
Median Attendance and Responsiveness to Interventions by Subgroup.
| Subgroup | Median Attendance | Responsiveness to Program Changes | |
|---|---|---|---|
| Sessions [IQ Range] | Chi2* | p-value | |
| Age | |||
| • ≥ 65 years | 18 [6 to 34] | 29.3 | < 0.001 |
| • < 65 years | 13 [5 to 23] | 8.9 | 0.03 |
| Gender | |||
| • Male | 15 [6 to 29] | 16.3 | 0.001 |
| • Female | 14 [6 to 28] | 15.8 | 0.001 |
| Indication for Cardiac Rehabilitation | |||
| • Coronary Artery Bypass Surgery | 20 [9 to 35] | 7.9 | 0.04 |
| • Myocardial Infarction | 18 [7 to 32] | 18.9 | 0.001 |
| • Heart Transplant | 15 [9 to 23] | 7.3 | 0.06 |
| • Percutaneous Coronary Intervention | 13 [5 to 29] | 1.6 | 0.65 |
| • Valve Surgery | 12 [5 to 12] | 7.1 | 0.07 |
| • Angina | 11 [5 to 20] | 5.2 | 0.15 |
| • Other | 10 [5 to 24] | 2.5 | 0.48 |
Chi2 reported across all four study time periods.
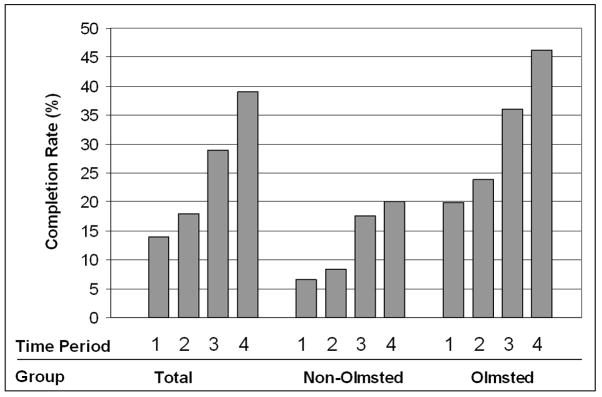
Completion of CR significantly improved over the study period as shown in Figure 2. Total completion rates increased from 14% to 39% (Chi2 = 49, p < 0.001), with 46% of local patients completing CR program by study end. When using the 36 session definition of completion, we found similar significant improvements in completion rates rising from 4% to 16%, (Chi2 = 32, p < 0.001.)
Figure 2.
Percentage of Patients Completing Cardiac Rehabilitation by Attending ≥30 Sessions
As shown, completion rate improved over time (X2 = 49, p < 0.001, X2 = 13, p = 0.004, and X2 = 33, p < 0.001 for Total, non-local, and local respectively), with [local] County patients more likely to complete the program. Time period 1 was the baseline, period 2 followed the policy change, period 3 followed the introduction of the welcoming video, and period 4 followed the introduction of the motivational program.
Recurring financial costs demonstrated a maximal cost of $54 for patients who completed the full motivational program, but an actual cost of just $19 per patient. One-time costs included the staff rewards of $810, and video production of $21,000. We attributed an average increase per patient of 2 sessions (95% CI, -0.3 to 4.1) to the motivational program and 2.5 sessions (95% CI, 0.5 to 4.5) for the video. Thus, for every $100 spent, attendance increased by an average of 6.6 (95% CI, -1 to 14) and 3 (95% CI, 1 to 6) CR sessions for the motivational program and video, respectively.
Discussion
The primary finding of this study was that continual, purposeful, and planned quality improvement efforts significantly increased patient participation in CR. We demonstrated an increase in the median number of CR sessions attended per patient from 12 to 20 in just 2 years with data from more than 1,000 patients. In addition, such activities favorably affected CR program completion rates such that almost 40% of patients receive the “full dose” and maximal benefits of early outpatient CR. It is difficult to say which of the three interventions (policy change, video, or motivational program) most effectively increased patient attendance. While the overall effect was clearly positive, statistical significance was not met for every comparison or intervention, and there appeared to be a greater impact in local and elderly patients. However, taken together the message is clear: the cumulative effect of these quality improvement projects was a large increase in patient participation in CR.
To our knowledge, this is the first study to explore the impact of quality improvement efforts on CR attendance or “dose”. Successfully increasing patient participation is an important goal for CR programs because such changes are expected to decrease subsequent morbidity and mortality. Using retrospective Medicare data from Hammill et al,2 and prospective Canadian data from Martin et al,3 there appears to be an 1% decreased risk of death or myocardial infarction for each CR session attended, suggesting that the cumulative interventions described in this paper could produce an approximate 5-8% decrease in risk of death or myocardial infarction over 4 years.
The policy change appeared to make little difference, suggesting that words alone are unlikely to substantially change patient and staff behavior. However, it is difficult to rule out a significant impact of the policy because it was the driving force behind the subsequent process changes that occurred.
The motivational program was successful in several ways. First, it improved the total sessions among Olmsted County patients. Second, there was an overall trend towards increased participation for all patients, both local and non-local. Third, the parallel staff motivational program helped keep CR staff members engaged in the program. Fourth, the program succeeded in emphasizing the importance of attendance at CR and used the token rewards as a method to reinforce positive patient behavior, rather than as the main focus. These key features appear to have contributed to the program’s impact. However, the motivational program was unsuccessful in improving attendance for patients living outside of Olmsted County. This is not surprising given that these patients must travel substantially greater distances and time to attend a 1 hour CR session.
For the past decade, our CR program operated in a background of high referral (>90%) and enrollment rates (>60%) but lower participation rates, with an average dose of 13-14 sessions per patient for [local] residents.11-14 This project now brings our institutional dose for patients age ≥ 65 years above the national median of 25 sessions per patient for Medicare recipients.2 It is unclear if higher doses are obtainable with additional quality improvement projects in our center.
Regarding the cost-analysis of these programs, we note that CR has consistently been found to be cost-effective.15-18 In addition, CR increases quality of life and decreases mortality.19 Furthermore, incentives are generally considered ethical in promoting specific health related behaviors.8 Consequently, the costs described in this analysis are likely a small price to pay for the benefit they are expected to produce. If health care in the United States moves towards a more capitated environment, as appears to be the trend, the use of motivational programs in CR would appear to be an appealing and cost-efficient option to improve the delivery of CR and secondary prevention services.
Our motivational program was developed under close legal supervision and counsel, taking careful steps to make sure we adhered to anti-kick back and anti-competition regulations. In our case, the motivational program was considered permissible for the following reasons: 1) CR is an important and strongly recommended therapy with proven mortality reductions, 2) the Centers for Medicare and Medicaid Services (CMS) and other medical organizations have been implementing strategies that encourage greater use of CR services in order to reduce the treatment gap that currently exists in delivery of CR to eligible patients,20 3) reimbursement by CMS for CR services is generally below the cost for delivering such services (i.e., increasing CR participation by Medicare patients may actually lead to no better than a break-even financial impact on a medical center or practice), 4) the cumulative value of the rewards was generally less that $50 on an annual basis, 5) the rewards were given only after commencement of the program and were not used to entice patients to enroll, 6) patients were already established as patients within our health care system, (7) there were no other competing CR programs in our [local] County during the time period under study, and 8) the Office of the Inspector General has previously issued a favorable advisory pertaining to rewards/incentives in a reasonably similar situation.21
Limitations and Strengths
The primary limitation of our study was the inability to draw strong conclusions about the impact of any single intervention (policy change, video, and motivational program.) This was because each intervention was part of a continued effort, and added sequentially to previous efforts. The overall trend was favorable without distinct plateaus, and significant monthly scatter in the average number of sessions per patient weakened the overall comparisons among time periods. Second, the interventions were not randomized and are inherently subject to confounding effects. Third, this was a single center study performed in a relatively uniform population composed mostly (92%) of non-Hispanic white men. Consequently, generalization to other centers, particularly diverse urban locations with greater proportions of women and minorities, might be inappropriate. Fourth, this analysis included only the first few months after implementation of the motivational program. As a result, patient numbers were smallest for this period and may not accurately reflect the true impact of the program (i.e., there is a possibility of type II or beta error). On the other hand, motivational programs tend to be maximally effective in the first few months after implementation with a subsequent decline in effectiveness.23 As our follow-up period was only 6 months, we may find with longer follow-up that the impact of the motivational program declines over time. Fifth, we were unable to evaluate the long-term economic and health outcomes of these interventions. Sixth, we did not evaluate the effect of insurance co-pays as a modifying factor in patient attendance at CR. This factor was unavailable in our database but may have played an important modifying role in the decision for patients to attend and complete CR.
Strengths of this study include the large number of subjects, a clear historical baseline, distinct interventional dates, and the use of billing data rather than program records for the determination of average number of sessions and their financial effects. Further, no additional staff members were hired during the study period, costs were modest, and the motivational program was easily incorporated into the daily routine.
Conclusions
We demonstrated a significant increase in patient attendance in CR with a series of quality improvement projects over the course of 2 years. The average number of sessions increased substantially as did the number of patients completing CR. Such efforts, if applied to CR programs across the nation may potentially help improve delivery of CR to eligible patients and may potentially help improve patient morbidity and mortality.
Acknowledgments
We would like thank [name removed for peer review] for assistance with the financial analysis as well as all CR staff for their continued dedication to excellence and quality improvement.
Funding: Statistical consultation was supported by CTSA Grant Number TL1 TR000137 from the National Center for Advancing Translational Science (NCATS).
Footnotes
Disclosures: None for all authors.
References
- 1.Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 2.Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly medicare beneficiaries. Circulation. 2010;121:63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin BJ, Hauer T, Arena R, Austford LD, Galbraith PD, Lewin AM, Knudtson M, Ghali WA, Stone JA, Aggarwal S. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012 Jul 9; doi: 10.1161/CIRCULATIONAHA.111.066738. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Davies P, Taylor F, Beswick A, Wise F, Moxham T, Rees K, Ebrahim S. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD007131.pub2. CD007131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volpp KG, Troxel AB, Pauly MV, Glick HA, Puig A, Asch DA, Galvin R, Zhu J, Wan F, DeGuzman J, Corbett E, Weiner J, Audrain-McGovern J. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360:699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 6.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: A randomized trial. JAMA. 2008;300:2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robison JI, Rogers MA, Carlson JJ, Mavis BE, Stachnik T, Stoffelmayr B, Sprague HA, McGrew CR, Van Huss WD. Effects of a 6-month incentive-based exercise program on adherence and work capacity. Med Sci Sports Exerc. 1992;24:85–93. [PubMed] [Google Scholar]
- 8.Madison KM, Volpp KG, Halpern SD. The law, policy, and ethics of employers’ use of financial incentives to improve health. J Law Med Ethics. 2011;39:450–468. doi: 10.1111/j.1748-720X.2011.00614.x. [DOI] [PubMed] [Google Scholar]
- 9.Ades PA, Gaalema DE. Coronary heart disease as a case study in prevention: Potential role of incentives. Prev Med. 2012 Jan 27; doi: 10.1016/j.ypmed.2011.12.025. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 10.International; MCA. 43rd annual MCA-I media festival winners. Media Communications Association International; [May 25th, 2012]. at http://www.mca-i.org/en/rel/1736/ [Google Scholar]
- 11.Goel K, Lennon RJ, Tilbury RT, Squires RW, Thomas RJ. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 2011;123:2344–2352. doi: 10.1161/CIRCULATIONAHA.110.983536. [DOI] [PubMed] [Google Scholar]
- 12.Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, Koepsell E, Roger VL. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–859. doi: 10.1016/j.ahj.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pack Q, G K, Lahr B, Greason K, Squires R, Thomas RJ. Cardiac rehabilitation reduces mortality following coronary artery bypass: A 10-year community study. J Am Coll Cardiol. 2012;59:E 1713 A. [Google Scholar]
- 14.Witt BJ, Jacobsen SJ, Weston SA, Killian JM, Meverden RA, Allison TG, Reeder GS, Roger VL. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004;44:988–996. doi: 10.1016/j.jacc.2004.05.062. [DOI] [PubMed] [Google Scholar]
- 15.Ades PA, Pashkow FJ, Nestor JR. Cost-effectiveness of cardiac rehabilitation after myocardial infarction. J Cardiopulm Rehabil. 1997;17:222–231. doi: 10.1097/00008483-199707000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Huang Y, Zhang R, Culler SD, Kutner NG. Costs and effectiveness of cardiac rehabilitation for dialysis patients following coronary bypass. Kidney Int. 2008;74:1079–1084. doi: 10.1038/ki.2008.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu CM, Lau CP, Chau J, McGhee S, Kong SL, Cheung BM, Li LS. A short course of cardiac rehabilitation program is highly cost effective in improving long-term quality of life in patients with recent myocardial infarction or percutaneous coronary intervention. Arch Phys Med Rehabil. 2004;85:1915–1922. doi: 10.1016/j.apmr.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Briffa TG, Eckermann SD, Griffiths AD, Harris PJ, Heath MR, Freedman SB, Donaldson LT, Briffa NK, Keech AC. Cost-effectiveness of rehabilitation after an acute coronary event: A randomised controlled trial. Med J Aust. 2005;183:450–455. doi: 10.5694/j.1326-5377.2005.tb07121.x. [DOI] [PubMed] [Google Scholar]
- 19.Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, Rees K, Thompson DR, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD001800.pub2. CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas RJ, King M, Lui K, Oldridge N, Pina IL, Spertus J. AACVPR/ACCF/AHA 2010 update: Performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: A report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association task force on performance measures (writing committee to develop clinical performance measures for cardiac rehabilitation) Circulation. 2010;122:1342–1350. doi: 10.1161/CIR.0b013e3181f5185b. [DOI] [PubMed] [Google Scholar]
- 21.Office of Inpsector General. OIG Advisory Opinion No.08-14. 2008 Sep 24; [Google Scholar]
- 22.John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG. Financial incentives for extended weight loss: A randomized, controlled trial. J Gen Intern Med. 2011;26:621–626. doi: 10.1007/s11606-010-1628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]