Abstract
Purpose
Homeless individuals face unique challenges in health care. Several US initiatives seeking to advance patient-centered primary care for homeless persons are more likely to succeed if they incorporate the priorities of the patients they are to serve. However, there has been no prior research to elicit their priorities in primary care. This study sought to identify aspects of primary care important to persons familiar with homelessness based on personal experience or professional commitment, and to highlight where the priorities of patients and professionals dedicated to their care converge or diverge.
Methods
This qualitative exercise asked 26 homeless patients and ten provider/experts to rank 16 aspects of primary care using a card sort. Patient-level respondents (n=26) were recruited from homeless service organizations across all regions of the USA and from an established board of homeless service users. Provider/expert-level respondents (n=10) were recruited from veteran and non-veteran-focused homeless health care programs with similar geographic diversity.
Results
Both groups gave high priority to accessibility, evidence-based care, coordination, and cooperation. Provider/experts endorsed patient control more strongly than patients. Patients ranked information about their care more highly than provider/experts.
Conclusion
Accessibility and the perception of care based on medical evidence represent priority concerns for homeless patients and provider/experts. Patient control, a concept endorsed by experts, is not strongly endorsed by homeless patients. Understanding how to assure fluid communication, coordination, and team member cooperation could represent more worthy targets for research and quality improvement in this domain.
Keywords: homeless persons, patient-centered care, primary care, provider perspectives
Video abstract
Introduction
A national effort to prioritize patient-centered care has emerged from 2 decades of scholarship1–4 and is exemplified by the establishment of a Patient-Centered Outcomes Research Institute (PCORI).5,6 Until recently, the potentially unique concerns of homeless patients, a population estimated to number 633,782 nightly,7 have been underrepresented in deliberations on primary care quality. For example, homeless persons are not specified by Congress as a “priority population” for the Agency for Healthcare Research and Quality.5
Persons experiencing homelessness may obtain primary care through federally sponsored and private agencies, including Health Care for the Homeless programs,8 the Department of Veterans Affairs, and charity clinics.9 Several factors lend new impetus to the question of how to assure that their care is patient-centered. First, under new legislation, many homeless persons will acquire Medicaid.10 Additionally, in 2012, the Veterans Health Administration sponsored 37 homeless-tailored primary care clinics, a program whose continuing expansion in 2013 reflects institutional embrace of “homeless-tailored” primary care.11
A premise guiding this study is that any effort to define “patient-centered” primary care for homeless individuals should begin with the declared priorities of homeless patients and those professionals who have focused their careers on advancing their care. Available instruments to assess perceptions of primary care in the general population12,13 may not reflect those priorities, however.
Accordingly, at the outset of an ongoing effort to develop a new instrument to assess homeless patient experiences, this study sought to identify aspects of primary care important to persons familiar with homelessness based on personal experience or professional commitment. Additionally, we wished to highlight where the priorities of homeless patients and professionals dedicated to their care might converge or diverge.
Methods
This study used a card sort exercise to prioritize constructs related to primary care. Card sorts are formal exercises that attempt to elicit subjective perceptions in a structured manner, and such exercises may seek to identify subjective categories, or priority rankings, the latter being the present goal.14
The development of a list of potentially important quality-related constructs drew on work by expert committees of the Institute of Medicine (IoM), including the “10 Rules for Quality” published in its Crossing the Quality Chasm report15 and elements of the definition of primary care crafted by the IoM’s Committee on the Future of Primary Care.16 The IoM primary care definition previously guided Safran’s development of a primary care experience survey.17
To produce a sortable list of constructs, a multidisciplinary research team (including experts in psychology, social work, and primary care) reviewed concepts from the IoM reports, winnowed them down to avoid redundancy, and crafted language to express each of 16 constructs in short sentences in order to facilitate self-administration by providers and patients, some with low literacy.
Each resulting statement included the stem “Primary care should …” followed by language encompassing the construct of interest (Table 1). Each was printed on a separate card and placed into a packet with a return envelope. We instructed participants to bind the cards in order of priority, and return them.
Table 1.
Primary care quality constructs derived from two IoM reports and their ordinal ranking among patients and provider/experts in homeless health carea
| IoM construct | Statements ranked in card sort exercise: “Primary care should …” | Homeless patients | Provider/experts in homeless care |
|---|---|---|---|
| Accessibility | Be easy to get | 1 | 1 |
| Evidence-based decision making | Be based on the best medical knowledge | 2 | 2 |
| Cooperation | Mean all of those who take care of a patient to work as a team and talk to each other | 3 | 4 (tied with source of control) |
| Coordination | Make sure a patient can get all the services they need even if it is from more than one person | 4 (tied with shared knowledge) | 6 |
| Shared knowledge and the free flow of information | Make it easy for patients to get information about their care | 4 (tied with coordination) | 14 |
| Accountability for addressing majority of health needs | Meet most of a patient’s health needs, most of the time | 6 | 3 |
| Sustained partnership | Mean the provider and the patient work together over a long period of time | 7 | 12 |
| Continuous (not just visit-based) healing relationships | Be available any time or any place patients need it | 8 | 10 |
| Anticipation of needs | Plan for a patient’s future needs, instead of waiting for persons to say they have a need | 9 | 7 |
| Patient as a source of control | Give patients control in their health care | 10 | 4 (tied with cooperation) |
| Safety as a system priority | Keep in mind safety | 11 | 11 |
| Transparency | Allow patients to know how well their primary care providers do their jobs | 12 | 15 |
| Choices in primary care should be based on a patient’s values | Be based on your values | 13 | 8 |
| Decrease in waste, optimize value | Not waste money or time | 14 | 16 |
| Context of community and family | Keep in mind the people who are in a patient’s life or not in a patient’s life | 15 | 13 |
| Context of community and family | Keep in mind where a person lives | 16 | 9 |
Notes:
The ordinal ranking shown in this table (from 1 to 16) was obtained as follows. We computed the mean value (ie, its position within the deck of 16 cards provided) for each construct, separately for patients and providers. These mean values were then ordered from lowest (most important) to highest (least important) to illustrate their relative importance to patients and to providers.
Abbreviation: IoM, Institute of Medicine.
Patients who had experienced homelessness were recruited a) from the Consumer Advisory Board of the National Health Care for the Homeless Council (n=5) and b) through veteran-focused homeless service programs in nine US states encompassing all geographic regions of the country, identified primarily from the website of the National Coalition for Homeless Veterans (n=21). For this exercise, homeless-focused provider/experts were persons with significant professional commitment (typically >10 years) to homeless services, or to research and policy in the care of homeless individuals. They were solicited from 17 organizations across 14 states and the District of Columbia with the goal of maximizing participation from all geographic regions of the USA, and assuring a mix of direct service providers and experts (ie, program leaders or homeless health care research experts) in homeless health care from veteran- and non-veteran-focused agencies.
Card response packets were anonymous, reflecting Institutional Review Board rules typically applicable to VA-sponsored research. Given the anonymous and nonsensitive nature of the packets sent, informed consent was implied by return of the packet to the research team. Response rates were comparable; 65% of patients (26 out of 40) and 53% of provider/experts (ten out of 19). Returned cards were numbered 1–16 with response sequences entered in a spread-sheet. We computed the mean value for each construct (ie, its position within the deck of 16 cards), separately for patients and provider/experts. These means ordered from lowest (1= most important) to highest (16= least important) to illustrate their relative importance to patients and to provider/experts. Because the computation of mean values does not illustrate the range of rankings among patients and provider/experts, we also produced vertical scatterplots to allow visual consideration of response “spread” and overlap between patients and provider/experts, using Tableau software (Tableau, Seattle, WA, USA). This activity had the approval of the Institutional Review Board of the Birmingham VA Medical Center.
Results
With respect to average rankings of constructs, patients and provider/experts agreed on the two most important characteristics of homeless patient care: accessibility and evidence-based decision making (Table 1). Cooperation, coordination, and accountability were also ranked in the top six by both groups. Transparency, concerns about minimizing waste of time or money, and matching care to the context of a patient’s community and family were ranked less favorably by both groups.
There were notable divergences in rankings between patients and provider/experts. Patients considered “shared knowledge and the free flow of information” about care to be important (ranked 4th of 16), while provider/experts gave this low priority (14th). Provider/experts assigned high priority to patient control of health care (4th), while patients gave this a far lower priority (10th).
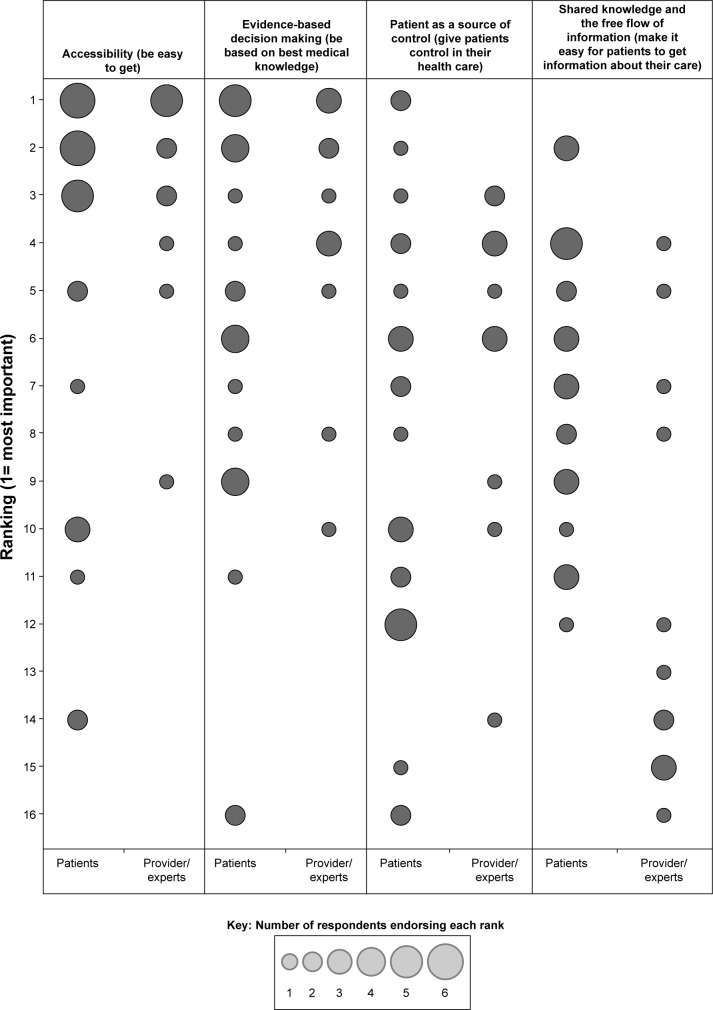
Study of the actual distribution of ranks identified significant spread among patients and among provider/experts. For four constructs where there was notable convergence or divergence, Figure 1 depicts the frequency of rankings from most prioritized (1) to least prioritized (16), with the size of the circle reflecting the number of respondents assigning that ranking. For accessibility and evidence-based decision making, the tendency for both patients and provider/experts to assign high priority is evident. For patient control in their care, lower priority was given by patients, but visual examination shows variation among patients (with predominance toward the less-prioritized end of the scale). For the priority of shared knowledge and free flow of information, despite considerable overlap, patients gave a substantively more favorable ranking than providers.
Figure 1.
Frequency of rankings among patients and provider/experts for selected primary care quality constructs.
Notes: Frequency of rankings (range 1= most important; 16= least important) assigned to four selected primary-care-related constructs in a card sort exercise undertaken by 26 homeless patients and ten provider/experts with professional focus on homeless health care. Two constructs at left (accessibility and evidence-based decision making) obtained high prioritization from both providers and patients. Two shown at right (patient as source of control; shared knowledge and the free flow of information) diverged, although overlap was seen. The circle size reflects the number of persons who endorsed the construct for the rank shown.
Discussion
This exercise highlights areas of convergence and divergence in the priorities for primary care embraced by homeless patients and professionals committed to their care. Homeless patients and provider/experts both prioritize easy access to primary care and the concern that such care be based on the best medical knowledge. Shared prioritization of accessibility is unsurprising.18,19 Conversely, there have been fewer efforts to assess whether homeless persons believe their care is evidence-based, and what effect such perceptions may have on adherence, engagement, or other outcomes.
These results notably highlight a divergence between the perceived value of “control” in care (ranked low by patients but high by provider/experts) versus information about care (prioritized by patients but less so by provider/experts). Devaluation of control relative to information has been seen in other populations,20,21 but this is the first study to suggest that a similar divergence applies between homeless patients and provider/experts. We speculate that issues of control may be particularly sensitive for populations where mental illness and addiction issues are common. The relatively low priority assigned to control suggests that the IoM’s explicit embrace of patient control15 per se may be less resonant for this population.
By contrast, the free flow of information was highly valued by patients. Information and understanding may play roles in alleviating distress, separate from the quality of the treatment administered. Additionally, patient-centered communications may convey respect and inform choices.22
Limitations apply to this study. By their nature, qualitative data do not reflect systematic and representative samples of a population. However, no survey of homeless patients has ever sought to assess their primary care preferences. Moreover, the geographic diversity of participants assigns a degree of credibility to these results in guiding future efforts on this topic.
Separately, it should be acknowledged that revelation of priorities through a sorting exercise necessarily cannot render a rich portrait of personalized meanings respondents might assign to each concept. Detailed interview work would be an appropriate next step. Nonetheless, the brief declarative format used for the cards (eg, “Primary care should be easy to get”) limits the potential for unexpected interpretations.
Despite these limitations, the present findings identify several concepts of importance to the primary care of homeless individuals, if that care is to embody the ideal of patient-centeredness. They suggest that measures of care from the patient’s perspective must seek to operationalize several priority concerns, including perceptions of whether care is accessible, evidence-based care, and characterized by the free flow of information. The findings also invite further research concerning how providers and patients might assign different meanings and interpretations to concepts such as control, information, and cooperation.
Acknowledgments
This study is sponsored by the Department of Veterans Affairs, Health Services Research and Development Branch, Merit Award 07-969. Opinions expressed within this manuscript are those of the authors alone and do not represent positions of the Veterans Health Administration or any entity within the US federal government.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gerteis M, Edgman-Levitan S, Daley J, Delbanco TL. Through the Patient’s Eyes: Understanding and Promoting Patient-Centered Care. San Francisco, CA: Jossey-Bass; 1993. [Google Scholar]
- 2.Bechel DL, Myers WA, Smith DG. Does patient-centered care pay off? Jt Comm J Qual Improv. 2000;26:400–409. doi: 10.1016/s1070-3241(00)26033-1. [DOI] [PubMed] [Google Scholar]
- 3.Weiner SJ, Schwartz A, Weaver F, et al. Contextual errors and failures in individualizing patient care: a multicenter study. Ann Intern Med. 2010;153:69–75. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]
- 4.Sofaer S, Firminger K. Patient perceptions of the quality of health services. Annu Rev Public Health. 2005;26:513–559. doi: 10.1146/annurev.publhealth.25.050503.153958. [DOI] [PubMed] [Google Scholar]
- 5.Patient Protection and Affordable Care Act (Public Law 111–148) Washington, DC: The U.S. Government Publishing Office; 2010. [Google Scholar]
- 6.Washington AE, Lipstein SH. The Patient-Centered Outcomes Research Institute – promoting better information, decisions, and health. N Engl J Med. 2011;365:e31. doi: 10.1056/NEJMp1109407. [DOI] [PubMed] [Google Scholar]
- 7.Office of Planning and Community Development . 2012 Point-in-Time Estimates of Homelessness: Volume 1 of the 2012 Annual Homeless Assessment Report. Washington, DC: United States Department of Housing and Urban Development; 2012. [Google Scholar]
- 8.National Health Care for the Homeless Council . Frequently Asked Questions About Health Care for the Homeless. Nashville, TN: NHCHC; 2011. [Google Scholar]
- 9.Kertesz SG, McNeil W, Cash JJ, et al. Unmet need for medical care and safety net accessibility among Birmingham’s homeless. J Urban Health. 2014;91:33–45. doi: 10.1007/s11524-013-9801-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaiser Commission on Medicaid and the Uninsured . Medicaid Coverage and Care for the Homeless Population: Key Lessons to Consider for the 2014 Medicaid Expansion. Washington, DC: The Henry J. Kaiser Family Foundation; 2012. [Google Scholar]
- 11.O’Toole TP, Buckel L, Bourgault C, et al. Applying the chronic care model to homeless veterans: can a population approach to primary care impact utilization and clinical outcomes? Am J Public Health. 2010;100:2493–2499. doi: 10.2105/AJPH.2009.179416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hays RD, Shaul JA, Williams VS, et al. Psychometric properties of the CAHPS 1.0 survey measures. Consumer Assessment of Health Plans Study. Med Care. 1999;37:MS22–MS31. doi: 10.1097/00005650-199903001-00003. [DOI] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality . CAHPS Clinician & Group Surveys: 12-Month Survey with Patient Centered Medical Home (PCMH) Items. Washington, DC: United States Department of Health and Human Services; 2012. [Google Scholar]
- 14.McKeown B, Thomas D. Q Methodology. Newbury Park, CA: Sage Publications; 1988. [Google Scholar]
- 15.IoM Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 16.Committee on the Future of Primary Care for the Institute of Medicine . Primary Care: America’s Health in a New Era. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 17.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–739. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010;100:1326–1333. doi: 10.2105/AJPH.2009.180109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kushel MB, Vittingoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 20.Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients’ desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med. 1989;4:23–30. doi: 10.1007/BF02596485. [DOI] [PubMed] [Google Scholar]
- 21.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manson NC. Why do patients want information if not to take part in decision making? J Med Ethics. 2010;36:834–837. doi: 10.1136/jme.2010.036491. [DOI] [PubMed] [Google Scholar]