Abstract
Multi-azole resistance acquisition by Candida tropicalis after prolonged antifungal therapy in a dog with urinary candidiasis is reported. Pre- and post-azole treatment isolates were clonally related and had identical silent mutations in the ERG11 gene, but the latter displayed increased azole minimum inhibitory concentrations. A novel frameshift mutation in ERG3 was found in some isolates recovered after resistance development, so it appears unlikely that this mutation is responsible for multi-azole resistance.
Keywords: Azole resistance, Candida tropicalis, Dogs, Multilocus sequence typing, Urinary tract infections
Highlights
-
•
Azole resistance acquisition by Candida tropicalis is reported.
-
•
Studied isolates came from a dog with persistent urinary candidiasis.
-
•
Pre- and post-antifungal treatment isolates were clonally related.
-
•
A novel frameshift mutation in the ERG3 gene was found in post-treatment isolates.
1. Introduction
Mounting evidence suggests that acquired resistance to azoles in Candida species may be an emerging and underdiagnosed threat [1]. The extensive use of antifungals in medical institutions could be a major driver of this changing epidemiology, but infection by resistant isolates in azole-naïve patients has also been reported [1], [2].
Candida tropicalis is a leading agent of nosocomial yeast infection in humans, although its relative importance with respect to other Candida species varies widely among geographical areas and patient groups [3], [4]. An extensive array of virulence factors contribute to the high mortality rate attributed to this yeast [3], [4]. The pathogenicity of C. tropicalis in diverse animal species is also well documented, and even healthy individuals can serve as a reservoir of virulent and antifungal-resistant strains [5].
In this article we report the acquisition of multi-azole resistance by C. tropicalis during the course of a chronic infection in a dog with persistent urinary tract infection (UTI) which underwent prolonged antifungal therapy. A previously unknown frameshift mutation in the ERG3 gene, which encode for sterol Δ5,6-desaturase (essential for ergosterol biosynthesis), was found in some post-treatment isolates.
2. Case
In April 2011, 3-year-old male Yorkshire terrier dog was referred to the Clinical Veterinary Hospital of our institution (Universidad Complutense de Madrid, Spain) with a diagnosis of relapsing UTI. The dog had a history of congenital portosystemic shunt and ammonium urate bladder stones, and had been treated with marbofloxacin for a previous episode of bacterial UTI caused by Serratia marcescens. Microscopic examination and culturing of urine specimens obtained by cystocentesis during a first consultation revealed the presence of yeasts, so antifungal treatment with fluconazole (5 mg/kg/12 h PO) and periodic mycological surveillance was prescribed. Prolonged fluconazole therapy (three courses in 2011: from April 12 to May 5, from May 10 to June 20, and from June 30 to October 5) did not result in clinical improvement, so a five-day course of bladder irrigation with amphotericin B (1 h/day with 20 mL of a 200 mg/L solution) was administered in April 2012. Amphotericin B treatment was also unsuccessful and subsequent urine cultures remained positive for yeasts. In June 2012 the animal developed a urethral stone obstruction that was surgically removed, but soon after the procedure it entered into severe hepatic encephalopathy. Due to the guarded prognosis and clinical worsening of the dog's condition the owners elected euthanasia and refused necropsy.
Yeast isolates recovered from clinical specimens (Table 1) were identified as Candida tropicalis on the basis of the morphology and pigmentation of their colonies on ChromAgar medium (TecLaim, Madrid, Spain), and also by sequencing the D1/D2 domains of the large subunit (LSU) rRNA gene [6].
Table 1.
In vitro antifungal susceptibility of the Candida tropicalis isolates characterized in this study.
| Isolate no. | Origin | Date of recovery | CLSI MICs (μg/mL)a |
Sensititre YeastOne MICs (μg/mL)a |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AMB | FLC | ITC | KTC | PSC | VRC | CAS | AMB | 5FC | FLC | ITC | PSC | VRC | ANF | CAS | MCF | |||
| 1 | Urine | Nov. 12, 2010 | 0.5 | 0.125 | 0.031 | 0.004 | 0.063 | 0.016 | 0.125 | 1 | <0.06 | 4 | 0.5 | 0.25 | 0.25 | <0.015 | 0.015 | 0.015 |
| 2 | Urine | May 5, 2011 | 0.5 | 0.125 | 0.016 | 0.004 | 0.031 | 0.016 | 0.063 | 1 | <0.06 | 1 | 0.125 | 0.125 | 0.06 | 0.03 | 0.03 | 0.015 |
| 3 | Urine | Jun. 30, 2011 | 0.5 | 0.125 | 0.016 | 0.004 | 0.063 | 0.016 | 0.125 | 1 | <0.06 | 1 | 0.125 | 0.06 | 0.06 | <0.015 | 0.03 | 0.015 |
| 4 | Urine | Oct. 20, 2011 | 0.5 | 0.125 | 0.031 | 0.004 | 0.031 | 0.016 | 0.125 | 0.5 | <0.06 | 0.5 | 0.06 | 0.03 | 0.03 | 0.06 | 0.03 | 0.015 |
| 5 | Urine | Apr. 12, 2012 | 0.5 | >64 | >16 | 8 | >16 | >16 | 0.063 | 0.5 | <0.06 | >256 | >16 | >8 | >8 | 0.03 | 0.06 | 0.015 |
| 6 | Urine | May 23, 2012 | 0.5 | >64 | >16 | 16 | >16 | >16 | 0.25 | 1 | <0.06 | >256 | >16 | >8 | >8 | 0.06 | 0.06 | 0.03 |
| 7 | Urine | Jun. 7, 2012 | 0.5 | >64 | >16 | >16 | >16 | >16 | 0.125 | 1 | <0.06 | >256 | >16 | >8 | >8 | 0.125 | 0.06 | 0.03 |
| 8 | Bladder calculus | Jun. 11, 2012 | 0.5 | >64 | >16 | >16 | >16 | >16 | 0.25 | 1 | <0.06 | >256 | >16 | >8 | >8 | 0.06 | 0.06 | 0.03 |
Minimum inhibitory concentrations (MICs) were determined after 24 h of incubation at 35 °C. Antifungals tested: 5FC, flucytosine; AMB, amphotericin B; ANF, anidulafungin; CAS, caspofungin; FLC, fluconazole; ITC, itraconazole,; KTC, ketoconazole; MCF, micafungin; PSC, posaconazole; VRC, voriconazole.
Genotyping of isolates was performed by the MLST scheme developed by Tavanti et al. [7], which comprises the following six housekeeping genes: ICL1, encoding for an isocitrate lyase; MDR1, multidrug resistance protein; SAPT2, secreted aspartic protease 2; SAPT4, secreted aspartic protease 4; XYR1, d-xylose reductase I or II; and ZWF1a, putative glucose-6-phosphate dehydrogenase. In all cases, PCR amplification was performed in reaction volumes of 50 µL, consisting of 5 μL of buffer II (10× Applied Biosystems, Austin, TX, USA), 1.5 mM MgCl2 (Applied Biosystems), 200 μM each dNTP (Roche Diagnostics GmbH, Mannheim, Germany), 2 U AmpliTaq Gold DNA polymerase LD (Applied Biosystems), 20 pmol of each forward and reverse primer (Integrated DNA Technologies, Leuven, Belgium; see sequences in Tavanti et al. [7]) and 20 ng of genomic DNA (obtained following the procedure described in Álvarez-Pérez et al. [8]). Amplifications were carried out in a GeneAmp PCR System 9700 thermocycler (Applied Biosystems, Foster City, CA, USA) and consisted of a denaturation step of 7 min at 94 °C, followed by 30 cycles of 60 s at 94 °C for, 60 s at 52 °C, and 65 s at 74 °C, and a final extension step at 74 °C for 10 min. PCR products were purified using the High pure PCR product purification kit (Roche Diagnostics), sequenced in the forward and reverse directions using the ABI Prism Big Dye Terminator v3.0 Ready Reaction Cycle Sequencing Kit (Applied Biosystems) and analyzed on an ABI Prism 3730 sequencer (Applied Biosystems). DNA sequences were assembled and edited with Sequencher v.4.1.4 software (Gene Codes Inc., Ann Arbor, MI, USA). Raw DNA chromatograms were visually checked and scrutinized for heterozygosity, which was defined as the presence of overlapping peaks in the forward and reverse chromatograms. The final sequences were compared with others from the C. tropicalis MLST database (http://pubmlst.org/ctropicalis/). The results of these analyses revealed that all studied isolates belonged to a same diploid sequence type (DST) which was not found in the C. tropicalis MLST database. Therefore, the new allelic profile was submitted to the curator of the MLST database to be assigned a new accession number (DST no. 408; allelic profile: ICL1, 1; MDR1, 103 [new allele]; SAPT2, 4; SAPT4, 3; XYR1, 107 [new allele]; ZWF1a, 4).
In vitro antifungal susceptibility of isolates was determined by the reference Clinical and Laboratory Standards Institute (CLSI) broth microdilution procedure [9]. The antifungal agents (all purchased from Sigma-Aldrich, Madrid, Spain) and concentrations tested were: amphotericin B and caspofungin (0.031 to 16 mg/L), fluconazole (0.031–64 mg/L), and itraconazole, ketoconazole, posaconazole and voriconazole (0.002–16 mg/L). Assay plates were incubated at 35 °C in a humid atmosphere and read macroscopically at 24 and 48 h. The endpoint for minimum inhibitory concentration (MIC) was the antifungal concentration that produced a complete (100%) inhibition of visual growth (for amphotericin B) or prominent inhibition of growth (≤50% inhibition, for the remaining antifungal agents). Candida krusei ATCC 6258 and Candida parapsilosis ATCC 22019 were used as quality control strains and all isolates were tested at least twice on different days. In addition, antifungal susceptibility of isolates was also determined by the commercially prepared Sensititre YeastOne colorimetric antifungal panel (TREK Diagnostics Systems, East Grinstead, UK). On the day of the assay, suspensions of 1.5–8×103 cells/mL were prepared in YeastOne inoculum broth, and the dried panels were rehydrated by dispensing 100 μL of yeast suspension into each well. The panels were covered with adhesive seals and incubated at 35 °C for 24 h. The MIC endpoints were defined as the lowest concentration of antifungal drug preventing the development of a red color (i.e. first blue or purple well).
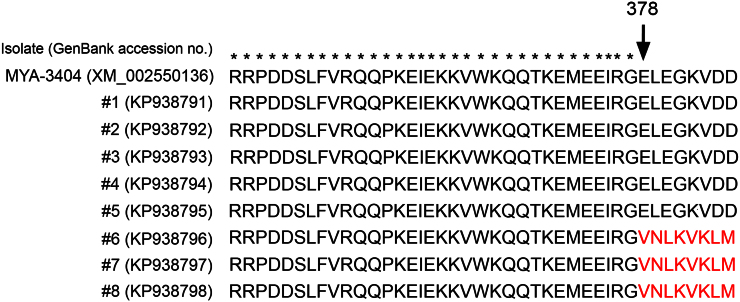
The ERG3 and ERG11 genes, which encode for sterol Δ5,6-desaturase and the azole target 14α-sterol demethylase, respectively, were PCR amplified and sequenced using the panels of oligonucleotide primers described by Forastiero et al. [10] and Vandeputte et al. [11]. PCR reactions consisted of 5 μL of buffer II (10×), 1.5–3 mM MgCl2, 200 μM each dNTP, 2 U AmpliTaq Gold DNA polymerase LD, 20 pmol of the corresponding forward and reverse primers and 50 ng of genomic DNA in a final volume of 50 µL. Amplification consisted of a denaturation step of 5 min at 94 °C, 35 cycles of 60 s at 94 °C, 60 s at 50 °C and 60 s at 72 °C, and a final extension at 72 °C for 10 min. Purification and sequencing of PCR products was performed as described above. ERG3 and ERG11 sequences obtained for the isolates characterized in this study (and also the amino acid sequences deduced from them) were compared using MEGA v.6 software [12] with those of Candida tropicalis MYA-3404 (GenBank accession no. XM_002550136) and C. tropicalis ATCC 750 (accession no. M23673), respectively. All studied isolates had identical nucleotide sequence for the ERG11 gene, and comparison with reference sequences retrieved from the GeneBank revealed the presence of four silent point mutations which were scattered throughout the coding region (Table 2). In addition, isolates recovered after bladder irrigation with amphotericin B had a mutation in the ERG3 gene consisting in the insertion of two consecutive guanine nucleotides near the end of the coding region, which resulted in a change in the reading frame (Table 2, Fig. 1). Notably, the multi-azole resistant isolate recovered six months after the last course of fluconazole therapy but two weeks before amphotericin treatment (isolate #5) did not have any mutation in ERG3.
Table 2.
Mutations observed in the ERG3 and ERG11 sequences of the isolates characterized in this study.a
| Gene | Nucleotide change | Amino acid change | Isolates with the mutation |
|---|---|---|---|
| ERG3 | 2-bp insertion in positions 1130 and 1131 | Frame shift from position 378 onwardsb | #6, 7 and 8 |
| ERG11 | T225C | None | All |
| G264A | None | All | |
| G1362A | None | All | |
| T1554C | None | All |
As determined by comparison with reference wild-type sequences retrieved from the GenBank.
See Fig. 1.
Fig. 1.
Alignment of the amino acid residues of the Erg3p sequences obtained for the isolates characterized in this study (#1–8) with a reference sequence retrieved from the GenBank (Candida tropicalis MYA-3404). Asterisks indicate conserved amino acids. Note the frameshift mutation from position 378 onwards in the sequences of isolates #6, 7 and 8.
All nucleotide sequences determined in this study were deposited in the GenBank database under the accession numbers KP938775–KP938782 (LSU rRNA), KP938799–KP938846 (MLST scheme), KP938791–KP938798 (ERG3) and KP938783–KP938790 (ERG11).
3. Discussion
Reports of clinical isolates of C. tropicalis showing reduced susceptibility to azoles have multiplied in recent years but, however, there is still little information concerning the molecular mechanisms leading to antifungal resistance in this species [10], [11], [13], [14], [15]. This lack of information is particularly evident in the veterinary setting, where detailed molecular characterization of fungal isolates is still uncommon.
Candida strains harboring mutations in the ERG3 gene may be more prevalent than currently supposed, but the viability and clinical relevance of such mutants remains controversial [16], [17]. Isolates obtained in this study after prolonged fluconazole therapy and a course of bladder irrigation with amphotericin B had a 2-bp insertion leading to a previously unknown change in the reading frame. Nevertheless, the first azole-resistant isolate detected had a wild-type ERG3 sequence. In addition, different mutations in the ERG11 gene have been described, but only a few of them have been clearly associated with in vitro and in vivo resistance to azoles [10], [13], [14], [15]. Notably, all pre- and post-azole treatment isolates from this case report had the same silent point mutations in the coding region of ERG11 and, therefore, a role of these mutations in multi-azole resistance seems unlikely. Other factors such as the over-expression of drug targets, up-regulation of transporters, biofilm formation or mitochondrial defects [10], [14] might have contributed to the acquisition of azole resistance observed in this case, and should thus be addressed in future.
Finally, although the results of MLST typing suggest that the strain involved in this case acquired multi-azole resistance during the course of prolonged antifungal therapy, the possibility of re-infection by a clonally-related resistant strain or even mixed infection by azole-resistant and susceptible strains of the same DST cannot be discounted. In any case, the presence of multiple identical mutations in the ERG11 sequences is highly suggestive of a common origin for all studied isolates.
In summary, we report here what seems to be the first case of multi-azole resistance acquisition by Candida tropicalis during the course of a chronic infection unresponsive to prolonged antifungal treatment in a non-human host. Due to the potential role of animals as reservoirs for human Candida infection [18], the risk imposed by the zoonotic spread of azole-resistant strains should be carefully assessed.
Conflict of interest
None of the authors of this paper has a financial or personal relationship with other people or organizations that could inappropriately influence or bias the content of the paper.
Acknowledgments
This work was supported by Universidad Complutense de Madrid-Banco Santander (Grant number: 920630) through the Research Groups Funding Program. Sergio Álvarez-Pérez acknowledges a ‘Juan de la Cierva’ postdoctoral contract funded by the Spanish Ministry of Economy and Competitiveness (JCI-2012-12396).
References
- 1.Arendrup M.C. Update on antifungal resistance in Aspergillus and Candida. Clin. Microbiol. Infect. 2014;20(6):S42–S48. doi: 10.1111/1469-0691.12513. [DOI] [PubMed] [Google Scholar]
- 2.Chong Y., Shimoda S., Yakushiji H., Ito Y., Miyamoto T., Shimono N. Fatal candidemia caused by azole-resistant Candida tropicalis in patients with hematological malignancies. J. Infect. Chemother. 2012;18:741–746. doi: 10.1007/s10156-012-0412-9. [DOI] [PubMed] [Google Scholar]
- 3.Chai L.Y.A., Denning D.W., Warn P. Candida tropicalis in human disease. Crit. Rev. Microbiol. 2010;36:282–298. doi: 10.3109/1040841X.2010.489506. [DOI] [PubMed] [Google Scholar]
- 4.Negri M., Silva S., Henriques M., Oliveira R. Insights into Candida tropicalis nosocomial infections and virulence factors. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31:1399–1412. doi: 10.1007/s10096-011-1455-z. [DOI] [PubMed] [Google Scholar]
- 5.Cordeiro R., de A., Oliveira J.S., Castelo-Branco D., de S., Teixeira C.E., Marques F.J., Bittencourt P.V. Candida tropicalis isolates obtained from veterinary sources show resistance to azoles and produce virulence factors. Med. Mycol. 2015;53:145–152. doi: 10.1093/mmy/myu081. [DOI] [PubMed] [Google Scholar]
- 6.Kurtzman C.P., Robnett C.J. Identification of clinically important ascomycetous yeasts based on nucleotide divergence in the 5’ end of the large-subunit (26S) ribosomal DNA gene. J. Clin. Microbiol. 1997;35:1216–1223. doi: 10.1128/jcm.35.5.1216-1223.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tavanti A., Davidson A.D., Johnson E.M., Maiden M.C., Shaw D.J., Gow N.A. Multilocus sequence typing for differentiation of strains of Candida tropicalis. J. Clin. Microbiol. 2005;43:5593–5600. doi: 10.1128/JCM.43.11.5593-5600.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Álvarez-Pérez S., Mateos A., Domínguez L., Martínez-Nevado E., Blanco J.L., García M.E. Polyclonal Aspergillus fumigatus infection in captive penguins. Vet. Microbiol. 2010;144:444–449. doi: 10.1016/j.vetmic.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Clinical and Laboratory Standards Institute, Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, 3rd ed. Wayne, PA, The Institute, 2008, M27–A3
- 10.Forastiero A., Mesa-Arango A.C., Alastruey-Izquierdo A., Alcazar-Fuoli L., Bernal-Martinez L., Pelaez T. Candida tropicalis antifungal cross-resistance is related to different azole target (Erg11p) modifications. Antimicrob. Agents Chemother. 2013;57:4769–4781. doi: 10.1128/AAC.00477-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vandeputte P., Larcher G., Bergès T., Renier G., Chabasse D., Bouchara J.P. Mechanisms of azole resistance in a clinical isolate of Candida tropicalis. Antimicrob. Agents Chemother. 2005;49:4608–4615. doi: 10.1128/AAC.49.11.4608-4615.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamura K., Stecher G., Peterson D., Filipski A., Kumar S. MEGA6: molecular evolutionary genetics analysis version 6.0. Mol. Biol. Evol. 2013;30:2725–2729. doi: 10.1093/molbev/mst197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eddouzi J., Parker J.E., Vale-Silva L.A., Coste A., Ischer F., Kelly S. Molecular mechanisms of drug resistance in clinical Candida species isolated from Tunisian hospitals. Antimicrob. Agents Chemother. 2013;57:3182–3193. doi: 10.1128/AAC.00555-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang C., Dong D., Yu B., Cai G., Wang X., Ji Y. Mechanisms of azole resistance in 52 clinical isolates of Candida tropicalis in China. J. Antimicrob. Chemother. 2013;68:778–785. doi: 10.1093/jac/dks481. [DOI] [PubMed] [Google Scholar]
- 15.Tan J., Zhang J., Chen W., Sun Y., Wan Z., Li R. The A395T mutation in ERG11 gene confers fluconazole resistance in Candida tropicalis causing candidemia. Mycopathologia. 2015;179:213–218. doi: 10.1007/s11046-014-9831-8. [DOI] [PubMed] [Google Scholar]
- 16.Martel C.M., Parker J.E., Bader O., Weig M., Gross U., Warrilow A.G. Identification and characterization of four azole-resistant erg3 mutants of Candida albicans. Antimicrob. Agents Chemother. 2010;54:4527–4533. doi: 10.1128/AAC.00348-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vale-Silva L.A., Coste A.T., Ischer F., Parker J.E., Kelly S.L., Pinto E. Azole resistance by loss of function of the sterol Δ5,6-desaturase gene (ERG3) Antimicrob. Agents Chemother. 2012;56:1960–1968. doi: 10.1128/AAC.05720-11. Candida albicans does not necessarily decrease virulence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edelmann A., Krüger M., Schmid J. Genetic relationship between human and animal isolates of Candida albicans. J. Clin. Microbiol. 2005;43:6164–6166. doi: 10.1128/JCM.43.12.6164-6166.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]