Abstract
Many cancer patients will develop spinal metastases. Local control is important for preventing neurologic compromise and to relieve pain. Stereotactic body radiotherapy or spinal radiosurgery is a new radiation therapy technique for spinal metastasis that can deliver a high dose of radiation to a tumor while minimizing the radiation delivered to healthy, neighboring tissues. This treatment is based on intensity-modulated radiotherapy, image guidance and rigid immobilization. Spinal radiosurgery is an increasingly utilized treatment method that improves local control and pain relief after delivering ablative doses of radiation. Here, we present a review highlighting the use of spinal radiosurgery for the treatment of metastatic tumors of the spine. The data used in the review were collected from both published studies and ongoing trials. We found that spinal radiosurgery is safe and provides excellent tumor control (up to 94% local control) and pain relief (up to 96%), independent of histology. Extensive data regarding clinical outcomes are available; however, this information has primarily been generated from retrospective and nonrandomized prospective series. Currently, two randomized trials are enrolling patients to study clinical applications of fractionation schedules spinal Radiosurgery. Additionally, a phase I clinical trial is being conducted to assess the safety of concurrent stereotactic body radiotherapy and ipilimumab for spinal metastases. Clinical trials to refine clinical indications and dose fractionation are ongoing. The concomitant use of targeted agents may produce better outcomes in the future.
Keywords: Stereotactic Body Radiotherapy, SBRT, Spine Radiosurgery, Spine Tumors, Spine Metastasis, Image-Guided Radiotherapy, Clinical Trial
INTRODUCTION
The spine is the most common site of bony metastatic disease. At least 40% of patients with advanced cancer will have spinal involvement during the course of their disease and approximately 5-10% of these patients will develop some type of epidural cord compression. More than 90% of metastatic lesions involving the spine are extradural; intradural and intramedullary lesions represent <5% and <1% of lesions, respectively 1,2,3.
Up to 50% of metastatic lesions originate from breast, lung or prostate cancers. With improved systemic treatment and augmented survival times, a greater number of patients with other tumor histologies will develop secondary lesions 1.
Early diagnosis of spinal metastatic disease is critical because functional outcomes depend on neurologic condition at the time of presentation. Tumor-related pain typically appears early in the morning or at night, generally improves with physical activity and frequently precedes the development of other neurological symptoms by weeks or months 4,5.
Uncontrolled spinal tumors typically produce pain and diminish ambulatory ability and performance status. Treatment is primarily palliative and is achieved by gaining local control of the disease. In selected cases, chemotherapy or surgery may pose as alternatives. The proper management of patients with spinal metastasis requires multidisciplinary treatment managed by orthopedic surgeons, neurosurgeons, radiation oncologists, medical oncologists, pain medicine specialists, radiologists and palliative care professionals.
Although palliative radiotherapy plays a prominent role in treating patients with metastatic spine disease, there is increasing literature that supports the use of stereotactic body radiotherapy (SBRT) or spine radiosurgery (SR)-based ablative treatment 6,7,8.
SR is a recently developed radiation therapy technique that delivers high-dose radiation to a tumor while minimizing the radiation delivered to healthy, neighboring tissues. A treatment target is defined by high-resolution imaging, which is also used for treatment planning and dose calculation. Precise delineation of the spinal cord requires registration if computer tomography (CT) images to the T2-weighted magnetic resonance imaging (MRI) series, or a CT myelogram. Treatment is delivered using a combination of externally placed strict immobilization devices and image-guided (IG) intensity-modulated radiation therapy (IMRT) 9,10. The treatment course is reduced to only a few sessions (generally up to 5), with total doses ranging from 12 to 30 Gy delivered in 1 to 5 fractions.
SR aims to improve existing rates of clinical response and tumor control, reduce re-treatment rates for metastatic lesions by increasing the biologic equivalent dose1, minimize radiation doses to healthy organs and allow safer reirradiation in previously treated sites 11. SR spares the spinal cord better than conventional radiotherapy and fractionated IMRT, even when very high doses are prescribed to an area only a few millimeters in size. Immobilization devices and image-guidance (IGRT) tools, such as kilovoltage cone-beam imaging 12, have reduced treatment errors associated with traditional radiotherapy and enabled safe and accurate delivery of the highly conformal dose distributions produced by IMRT techniques 13.
The aim of this article was to review published data on and ongoing trials of SR for metastatic tumors of the spine.
Review Methodology
A literature search was conducted using the MEDLINE database [via PubMed] and the Clinicaltrials.gov database for all article types available through September 2014. No other filter was activated and we assessed all of the published data that were available in English. Controlled vocabulary was leveraged as well as text words to develop the search strategy detailed below.
Our search terms and strategy used the following MEDLINE MeSH terms: ((Spinal Neoplasms [MeSH] OR Neoplasm, Spinal OR Neoplasms, Spinal OR Spinal Neoplasm OR Spine [MeSH] Vertebral Column OR Column, Vertebral OR Columns, Vertebral OR Vertebral Columns OR Spinal Column OR Column, Spinal OR Columns, Spinal OR Spinal Columns OR Vertebra OR Vertebrae) AND (Radiosurgery [MeSH] OR Radiosurgeries OR Radiosurgery, Stereotactic OR Radiosurgeries, Stereotactic OR Stereotactic Radiosurgeries OR Stereotactic Radiosurgery OR Gamma Knife Radiosurgery OR Gamma Knife Radiosurgeries OR Radiosurgeries, Gamma Knife OR Radiosurgery, Gamma Knife OR Stereotactic Body Radiotherapy OR Body Radiotherapies, Stereotactic OR Body Radiotherapy, Stereotactic OR Radiotherapies, Stereotactic Body OR Radiotherapy, Stereotactic Body OR Stereotactic Body Radiotherapies OR CyberKnife Radiosurgery OR CyberKnife Radiosurgeries OR Radiosurgeries, CyberKnife OR Radiosurgery, CyberKnife OR Radiosurgery, Linear Accelerator OR Linear Accelerator Radiosurgeries OR Radiosurgeries, Linear Accelerator OR Linear Accelerator Radiosurgery OR Radiosurgery, Linac OR Radiosurgeries, Linac OR LINAC Radiosurgery OR Radiosurgeries, LINAC)). For the Clinicaltrials.gov database, we used the following search terms: Spinal Neoplasms OR Spine AND Radiosurgery OR Radiation Therapy.
Two authors independently screened all identified studies by title and abstract. Studies with the following inclusion criteria were collected: primary focus on clinical outcome, evaluation of feasibility, assessment of toxicity and presentation of technical aspects. Additional treatment with chemotherapy, targeted therapy, endocrine therapy and surgery were permitted if radiotherapy was the primary intervention under investigation. All references in each included study were manually searched for important missed publications. Re-reporting and clinical trials were manually removed, and only the most recent publications were evaluated 14,15,16.
Studies that did not focus on SR were removed. Articles published in languages other than English were excluded. We also excluded articles with a main focus of epidemiology, research design, diagnosis, basic science or clinical guidelines. Editorial commentaries were removed. Finally, we removed studies with fewer than 20 patients, heterogeneous treatment design (multiple levels of SR dose or SR not the main objective of analysis) and less than 6 months of follow-up. A third evaluator resolved any disagreements.
Review Results
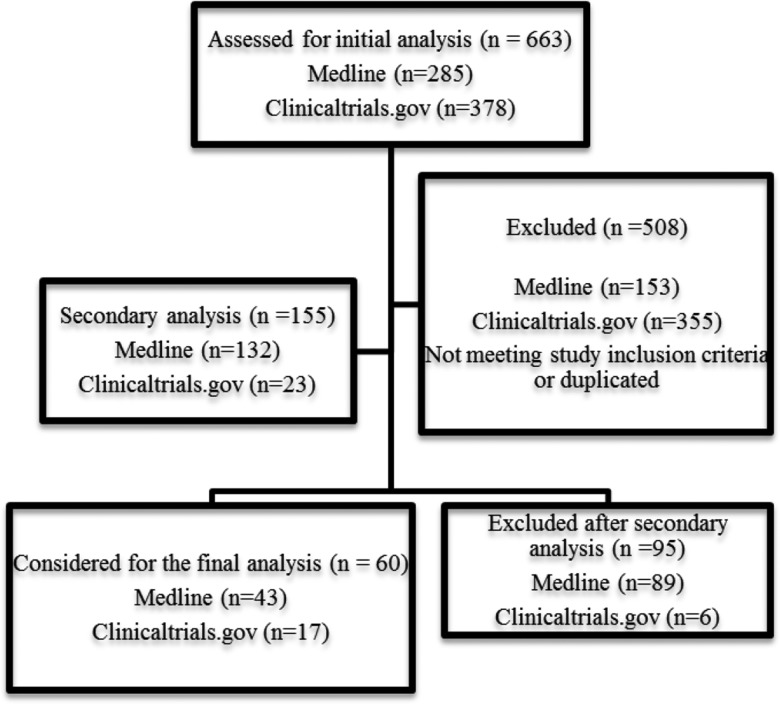
We identified 663 studies [MEDLINE n=285; Clinicaltrials.gov n=378]). After assessing and removing duplicated records (n=10), 653 studies were screened; of these, only 155 met the eligibility criteria for full-text assessment. After manually screening the full-text articles of the remaining studies (n=155 [MEDLINE n=132; Clinicaltrials.gov n=23) for our inclusion criteria, we identified 60 unique articles for qualitative analysis (Figure 1).
Figure 1-.
Flow diagram.
Data Extraction
One investigator (F.Y.M.) independently extracted data from all 60 studies. The following data were collected: study design, year of publication, non-radiotherapy interventions (e.g., hormone therapy, chemotherapy, targeted agents or procedures), type of radiotherapy treatment course (IMRT, IGRT, proton therapy, and brachytherapy), and primary assessed outcome [overall survival (OS), local control, pain control, quality of life measures and toxicity].
Technical Aspects of Spinal Radiosurgery
Dose Delivery Technique: Intensity-Modulated Radiotherapy
The use of IMRT is required to deliver high-dose radiation to vertebra while simultaneously sparing the spinal cord and other adjacent critical organs (e.g., the esophagus or brachial plexus). The development of IMRT was a major improvement over 3D conformal radiotherapy (3DCRT) 17. IMRT is capable of modulating a target-shaped field of uniform radiation intensity into hundreds of pixel-like “beamlets”, each with its own intensity. This advancement allows the delivery of increased radiation intensity to areas within the beam that are contained within the target volume only and reduces the radiation delivered to healthy organs via so-called intensity modulation. As a result, it is possible to create complex dose distributions characterized by steep dose gradients (i.e., significant dose differences over a short distance) to create a target (e.g., vertebra) with a concave shape to avoid hitting organs at risk (e.g., the spinal cord).
IMRT fields are often created through inverse planning optimization algorithms, where doses are prescribed to delineated volumes and potential plan alternatives are generated with guidance from a treatment planner (e.g., a dosimetrist or medical physicist) until a reasonable solution is found. Delivery via these intensity-modulated beams is achieved through the use of physical compensators (which are outdated technology) or, preferably, multi-leaf collimators (MLCs). An MLC serves as an add-on to a conventional rectangular linear accelerator's collimator. MLCs consist of sets of opposed leaf pairs (typically approximately 60 to 80 pairs of tungsten metal bars) that automatically longitudinally displace in and out of a beam's rectangular aperture to produce irregular custom shapes. Via the continuous or stepwise movement of the leaves during radiation emission, it is possible to modulate the intensity across a beam. This modulation of beam intensity improves the therapeutic index by allowing for increased target dose and reducing damage to normal tissues.
With the use of IMRT, a sharp dose gradient of approximately 10% per millimeter can be achieved near the spinal cord 18. For example, in a photon-based IMRT plan, where the spinal cord is 3 mm from the edge of the target volume, 18 Gy can be delivered to more than 90% of the target volume, while the maximum dose to the spinal cord surface would be less than 14 Gy (Figure 2).
Figure 2-.
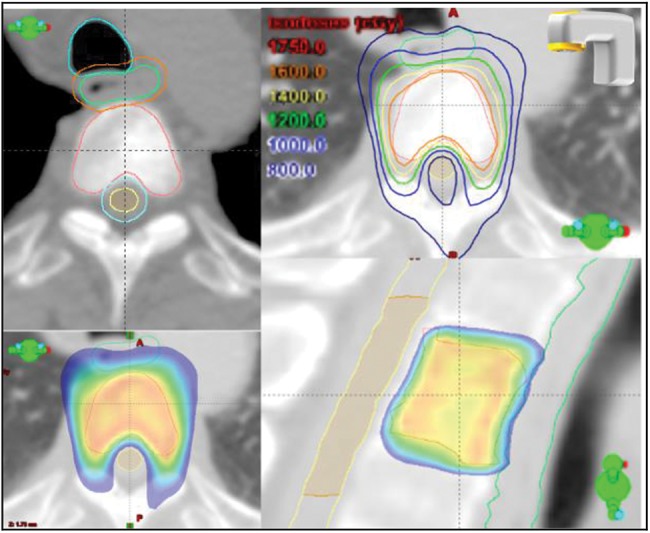
Spine radiosurgery. Target definition (vertebral body), radiotherapy isodose lines (upper right) and dose distribution (below). The axial and sagittal views illustrate “dose-shaping” promoted by IMRT, with sparing of the spinal cord and esophagus. [Male, 62 years old, metastatic melanoma of the spine, stable lesion, ECOG 0, treated with SR via 18 Gy delivered in a single fraction. The distance between the GTV (gross target volume) and the medulla is approximately 2 mm].
The rationale for using proton and other particle beams is the ability to achieve excellent dose distribution at a tumor target with virtually no exit dose delivered beyond the target volume. The Bragg peak phenomenon associated with particle beam radiation results in an extremely steep dose fall-off over a course of a few millimeters (Figure 3). The advantage of this characteristic lies primarily in the lack of exit dose beyond the Bragg peak. However, there is currently no routine indication to use proton radiation for SR.
Figure 3-.
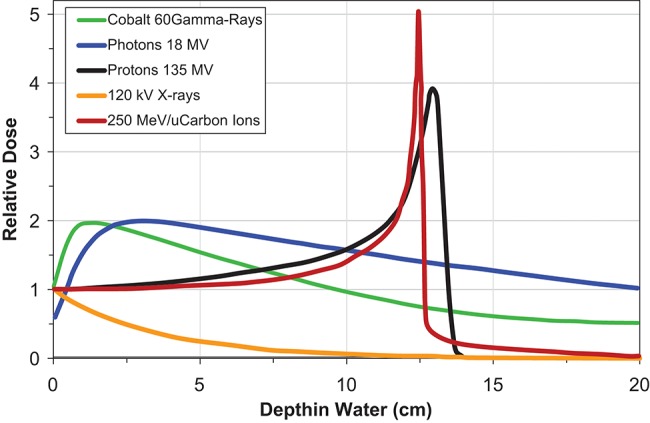
Depth dose curves for photons, cobalt 60, protons and carbon ions.
Patient Setup: Immobilization and Image Guidance
The general treatment parameters for SR are currently based on the use of IMRT and, more recently, volumetric arc therapy (VMAT, which is dosimetrically equivalent but more efficient and faster than IMRT). In addition, SR requires the use of image guidance and setup verification. The overall precision of different components (e.g., mechanical aspects, image guidance and beam targeting) should allow treatment accuracy within 1 mm 19. The primary role of IGRT is to guide patient re-positioning based on a target itself (in this case, the vertebral body being treated). Secondly, depending on the IGRT technique, patient position can be monitored during treatment to assure that the target remains static through frequent intra-fraction imaging. IGRT also requires that a patient remain immobilized in the correct position throughout dose delivery; devices exist specifically for this purpose.
For SR, a patient is immobilized in a stereotactic body frame or immobilization cradle. Such devices are noninvasive and thus do not guarantee that a patient will remain perfectly positioned. Nonetheless, based on pre- and post-treatment imaging findings, an approximate 95% rate of immobilization accuracy has been reported for the noninvasive devices that are currently in use 20. Immobilization has emerged as an issue of great importance because planning technology is ineffective unless a patient is accurately positioned.
Accurate positioning is possible through patient cooperation. After proper positioning is achieved, image acquisition, ideally using onboard cone-beam imaging just before RT treatment, can be initiated. Pretreatment images are registered and compared with target images acquired during simulation to identify and correct setup errors. Typically, these variations are minimal and account for displacements of less than 3 millimeters from the ideal position. These displacements are accounted for by repositioning the patient to match the target before treatment begins. After corrections are made in each direction, spine positioning can be considered truly reliable for a treatment session, with less than 1 mm of error 21.
Clinical Assessment and Patient Selection
Due to the improved OS gained by improving local and systemic therapies and the capacity of SR to improve local tumor control, SR has great potential for increased utilization. Spine metastatic disease is often observed in radiation oncology clinics and studies of SR have indicated that the technique results in excellent local control rates 8,22,23. The indications for SR are still expanding; they currently include pain related to an involved vertebral body, radiographic tumor progression, lesions associated with progressive neurologic deficits, adjuvant therapy after surgical intervention for radioresistant metastasis and the need for reirradiation 8.
Memorial Sloan Kettering Cancer Center (MSKCC) utilizes a multidisciplinary spine team to identify and treat patients who would most benefit from SR. The MSKCC Spine Clinic developed and now implements the algorithm NOMS for metastatic spine disease. This algorithm incorporates assessments of (N)eurologic condition, (O)ncologic status, (M)echanical instability and (S)ystemic disease 24. The goal of this decision framework is to provide a rapid, highly reliable assessment (e.g., low-grade extradural spinal cord compression (ESCC) versus high-grade disease or mechanical versus biologic pain) for the treatment of spinal metastases. Such treatment integrates radiation therapy, interventional neuroradiology and surgical approaches (Table 1) 24,25.
Table 1.
Current NOMS decision framework for high-grade epidural spinal cord compression (ESCC) (Adapted from Laufer et al. 24).
| Neurologic | Oncologic | Mechanical | Systemic | Decision |
|---|---|---|---|---|
| High-grade ESCC ± myelopathy | Radiosensitive | Stable | CRT | |
| Unstable | Stabilization followed by CRT | |||
| Radioresistant | Stable | Able to tolerate surgery | Decompression / stabilization followed by SR | |
| Radioresistant | Stable | Unable to tolerate surgery | CRT | |
| Radioresistant | Unstable | Able to tolerate surgery | Decompression / stabilization followed by SR | |
| Radioresistant | Unstable | Unable to tolerate surgery | Stabilization followed by CRT |
CRT: Conventional radiotherapy; SR: Spine radiosurgery.
Local Disease Control
Local control is defined as the absence of recurrent cord compression within an irradiated field or the absence of progression at a treatment site. The local control achieved with SR has been assessed in many series. Several of these series are highlighted below.
The Radiation Therapy Oncology Group (RTOG) published a phase II study evaluating the use of SR for localized spinal metastases (RTOG 0631). In this multicenter phase II study, patients with 1-3 lesions and a numerical rating pain scale score of ≥5 were treated. A total of 44 patients received 16-18 Gy of single-fraction SR. Grade 1/2 and grade 3 SBRT-related adverse events were observed in seven and zero patients, respectively. The investigators concluded that SR is safe and feasible in the multi-institutional setting 10. Several departments have also published their experiences, which are summarized in Table 2 22,32,45,.
Table 2.
Important clinical results following spine radiosurgery (based on recent prospective and retrospective data).
| Author | Study design | SR indication | N / Dose | IGRT | Reported results |
|---|---|---|---|---|---|
| Ahmed et al. 55 | Prospective case series | SM: primary and reirradiation | 66 patients(85 lesions)24 Gy (SF and HF) | BodyFix or thoracic-T double vacuum system*ExacTrac X-ray system with a 6D robotic couch# | mOS (12 months): 52.2%LC (1 year): 91.2%No grade 4 toxicity |
| Amdur et al. 56 | Prospective case series | SM: primary and reirradiation | 21 patients(12 reirradiation)Dose: 15 Gy | Customizedbody mold / onboard cone-beam CT | OS (12 months): 60%43% pain reliefNo grade 3 or 4 toxicity |
| Garg et al. 57 | Prospective case series | SM: primary SR | 61 patients(63 tumors)16-24Gy (SF) | BodyFix / stereotactic localizer and target frame | LC (18 months): 88%?Supports SR as first-line treatment |
| Klish et al. 58 | Prospective case series | SM: reirradiation | 58 patientsDose: variable | BodyFix / stereotactic localizer and target frame | LC (12 months): 89.3%< 5% of isolated failures of the nonirradiated adjacent vertebral body = focal SR feasible |
| Garg et al. 45 | Prospective case series | SM: reirradiation | 59 patients(63 tumors)30 Gy (5 fractions)27 Gy (3 fractions) | BodyFix stereotactic body frame system / stereotactic localizer and target frame | OS (12 months): 76%LC (12 months): 100%Freedom from neurological injury: 92% |
| Gerszten et al. 22 | Prospective nonrandomized cohort study | SM: primary and reirradiation | 500 patients12.5 - 25 Gy (SF and HF) | CyberKnife: Aquaplast facemask$ | LC: 90% of primary lesions and 88% of lesions treated for radiographic tumor progressionClinical improvement (previous neurologic deficit): 84%Long-term pain improvement: 86% |
| Haley et al. 59 | Prospective case series | Efficacy and cost effectiveness of CRT versus SR | 44 patients(22 CRT and 22 SR)Dose: variable | CyberKnife system | Similar pain reliefNo late complications in either groupCRT: more acute toxicities and was more likely to require additional interventions |
| Folkert et al. 32 | Retrospective case series | SM: primary and reirradiation (sarcoma) | 120 lesions(SF and HF 24 Gy) | Noninvasive customized cradle / onboard imaging (orthogonal KV imaging and cone-beam CT) | OS 60%LC (12 months) 87.9%Low toxicity reported |
| Zelefsky et al. 60 | Retrospective case series | SM: primary and reirradiation (renal cell) | 105 lesions(SF and HF)Dose: 24 Gy | Customized cradle / digitally reconstructed radiographs from the simulation studies for each field's beam's eye view | PFS (36 months - HF): 17%PFS (36 months -SF 24 Gy): 88%SF: improve local control |
Legend: N: number of patients; IGRT: image-guided radiotherapy; SF: single fraction; HF: hypofractionated; SM: spine metastasis; Hypo: hypofractionated; LC: local control; OS: overall survival; PFS: progression-free survival; SR: spine radiosurgery; CRT: conventional radiotherapy; CT: computed tomography.
<?ENTCHAR ast?>: (Medical Intelligence, Schwabmunchen, Germany);
#(Brainlab, Feldkirchen, Germany);
%(Integra- Radionics Burlington, MA);
$(Aquaplast Corp., Wyckoff, NJ).
For metastatic spinal tumors, SR has been postoperatively utilized in several series and in cases of progression following conventional fractionated palliative radiation treatment. Even in these challenging settings, SR achieves local control in approximately 85-94% of cases 22,23,26,18,27. When used as a primary treatment, long-term radiographic tumor control has been demonstrated in 90% of cases 22,.
In an assessment of 103 consecutive spinal metastases in 93 patients without high-grade ESCC who were treated with SBRT (median dose, 24 Gy delivered in a single fraction; range, 18-24 Gy), MSKCC reported an overall local control rate of 90% at a median follow-up of 15 months. There were no deaths attributed to local failure. No patient experienced myelopathy or radiculopathy, even when the maximum spinal dose was raised to 14 Gy from 12 Gy 23.
In another phase I/II trial, 149 patients (166 metastatic spine lesions) were treated with SR. None of the patients showed evidence of mechanical instability or cord compression and 50% of them exhibited radioresistant tumor histology. Each of the patients received a total dose of 27-30 Gy, typically delivered in three fractions. More than half of the patients had been treated with one prior course of conventional radiation therapy (30 Gy delivered in ten fractions). The local tumor progression-free survival reported after SR was 81% at 1 year and 72% at 2 years. Adverse events were minimal and SR was associated with robust pain reduction (26% of the patients were pain-free before SR and 54% were pain-free 6 months after SR). SR also reduced pain medication use and was associated with improved quality of life 31.
In another report, 88 patients with 120 spinal metastases from pathologically proven high-grade sarcoma were treated with hypofractionated [3-6 fractions; median dose, 28.5 Gy; n=52 (43.3%)] or single-fraction SR [median dose, 24 Gy; n=68 (56.7%)]. At a median follow-up of 12.3 months, the 12-month local control rate was 87.9%, and the OS was 60%. Single-fraction SR showed better local control than hypofractionation (p=0.007). The rate of adverse effects was low, and no grade >3 toxicity was reported 32.
Pain Control
Despite the use of heterogeneous methods for pain evaluation (e.g., verbal analysis scale and subjective measurements of pain relief, among others), most series report very high pain control rates (up to 96%) at 12 months 8. Pain control rates were still high even in cases of radioresistant tumors, such as melanoma, sarcoma, renal cell tumors, non-small cell lung cancer, gastrointestinal tumors and others (96% and 85% rates of pain control were achieved for melanoma and renal cell carcinoma, respectively) 8,30,33. SR has also been reported to provide better pain control more rapidly than conventional radiotherapy, with pain relief sometimes observed within 24 hours of treatment 34.
It is thought that conventional radiation doses may be sub-therapeutic for radioresistant tumors. A systematic review of randomized controlled trials (RCTs) reported that conventional radiotherapy can successfully palliate bone pain in 50 to 80% of patients, but complete pain relief is only achieved in up to 30% of patients 35,36. Thus, SR is feasible for the treatment of spinal metastases and promotes high rates of local control and pain relief with low rates of toxicity.
Postoperative Irradiation
It has been suggested that patients with metastatic spinal cord compression (MSCC) will benefit more from high-dose and/or SR radiotherapy than they would from low-dose fractioned radiotherapy. Surgery is fundamental the management of patients with symptomatic MSCC or high-grade spine compression. Patchell et al. reported in a RCT that surgical decompression is significantly beneficial. A larger number of patients who underwent surgery plus postoperative RT regained the ability to walk compared to those who received only RT. Ambulatory status was also maintained for longer in the surgery plus RT arm 37.
However, the exact criteria for surgery in cases of MSCC remain controversial. The following factors are usually necessary for improved outcomes: favorable PS and expected OS, a relatively radioresistant tumor type and MSCC accompanied with mechanical instability 24,25,38,39. Epidural disease is an important limiting factor with respect to SR efficacy. Al-Omair et al. reported that epidural disease progression is the most common cause of treatment failure after SR and a significant predictor of poor local control 40.
To more safely administer an ablative radiation dose, it may be possible to perform separation surgery to create a space of 2–3 mm between a metastatic lesion and the spinal cord. This allows a full dose to be administered to the entire tumor volume while minimizing the radiation dose delivered to the spinal cord. The surgical procedure is performed using epidural decompression and spinal stabilization without gross total or en bloc tumor resection 41,42.
Recently, MSKCC has published their experiences with 186 patients treated from 2002 to 2011 who were managed with separation surgery followed by SR (hypofractionated or single fraction) 43,44. In this cohort, 136 patients exhibited high-grade cord compression or MSCC and the full cohort received spinal decompression surgery followed by SR within a median of 48 days after surgery. Postoperative SR provided durable local control, with a cumulative local progression incidence of 16.4% at 1 year (95% confidence interval: 10.7–22.2).
Thus, for patients presenting with spinal cord compression, separation surgery followed by SR is a safe and effective treatment option. Integrative treatment (i.e., SR and separation surgery) may reduce the extent of surgery and also provide faster and more effective radiotherapy treatment.
Reirradiation of Spinal Metastases
SR is an indicated treatment for cases requiring reirradiation of spinal levels and may be associated with superior tumor control rates and pain relief relative to conventional radiotherapy. However, care must be taken when a reirradiation volume either contains or is very close to the spinal cord, esophagus or other organs at risk. In the reirradiation setting, SR provides a local control rate of 66-93% and a low rate of toxicity when treatment constraints and quality assurances are respected 45,46,47.
Complications
A pain flare or acute worsening of pain has been found to occur in 20% of cases after SR. Such a flare may occur within 24 hours of single-dose radiation or a few days after the use of a hypofractionated scheme 48,49. The pain is usually transient and can be managed with corticosteroids or non-steroidal anti-inflammatory drugs. Radiation-induced spinal cord injury can be a severe event, but it is not often observed. The best method of preventing myelopathy is avoidance of unnecessary radiation to the spinal cord and adherence to planned dose constraints.
Vertebral fracture (VCF) is a common event after SR. VCF has an incidence of approximately 20% and is associated with higher doses per fraction (≥20 Gy) and with 3 of the 6 original Spinal Instability Neoplastic Score (SINS) 50 components, including baseline VCF, a lytic tumor and spinal deformity 51. Attention must be paid to identifying high-risk patients who would benefit from prophylactic kyphoplasty.
Other events, such as risk of mucositis and skin dermatitis, have also been associated with SR. Additionally, there are many factors that may influence SR toxicity. Such factors include tumor proximity to and extension in adjacent normal tissues, concurrent systemic therapy and targeted therapy and comorbidities (e.g., acute infection, prior surgery, diabetes, collagen vascular disease, or any genetic predisposition).
Thus, in SR, end-to-end patient assessment, planning and dosimetry are important for ensuring a safe treatment procedure.
Future Perspectives: Randomized Data and Combination Targeted Therapy
Multiple prospective and retrospective series on SR have been reported. There are increasing expectations for randomized phase III trials, prospective phase II studies and the use of molecularly targeted agents as a new approach to treatment. Data from phase I, II and III trials are summarized in Table 3 9,52,53,.
Table 3.
Spine radiosurgery. Interventions and primary outcome descriptions from clinical trials registered at clinicaltrials.gov.
| Study / Date started | Status | Design | Condition | Intervention | Primary outcomes |
|---|---|---|---|---|---|
| NCT01654068 61 / Jul, 2012 | Recruiting | Phase II | Spinal metastasis | 1) 2-3 SM: 14 Gy SF2) 1 SM: 14 Gy SF | Any skeletal-related event |
| NCT01223248 52 / Oct, 2012 | Recruiting | Phase III | Spinal metastasis | SR 24 Gy SF vs. SR, 27 Gy (HF) | Loco-regional control rates |
| NCT01290562 62 / Jun 2011 | Recruiting | Phase II | Spinal metastasis | 20-24 Gy SF; or 20-24 Gy (HF)No prior RT or prior RT or Post-op | Local control: image / symptoms |
| NCT00573872 63 / Dec 2007 | Not recruiting (active) | Phase I/II | Spinal metastasis | Phase 1: 20-25 Gy (HF) / Phase 2: 9-24 Gy (SF) | TT: Safety |
| NCT01849510 64 / Apr 2013 | Recruiting | Phase II(2 arms) | Spinal metastasis | HF: 12×3 Gy+integrated boost 12×4 Gy / CRT 10×3 Gy | Local control |
| NCT02167633 65 / Jul 2014 | Recruiting | Controlled (2 arms) | MSCC | Decompression surgery plus CRT / SR 16 Gy SF | Ambulatory status |
| NCT00853528 66 / Feb 2009 | Not recruiting (active) | Phase I | Spinal metastasis | Maximum tolerated dose HF SR | Dose escalation |
| NCT00631670 67 / Feb 2008 | Completed | Controlled | Spinal metastasis | 15 Gy SF / 25×2.8 Gy | Safety |
| NCT01525745 68 / Jan 2012 | Completed | Phase II | Spinal metastasis | SR HF / CRT 10 fractions | Pain control: NPRS |
| NCT01826058 69 / Apr 2013 | Recruiting | Phase II | MSCC | 16 -24 Gy SF / 21-36 HF | Neurologic response |
| NCT01254903 70 / Dec 2012 | Recruiting | Phase I | MSCC | 18 Gy SF | Safety |
| NCT00922974 9 / Nov 2009 | Recruiting | Phase II: completedPhase III | Spinal metastasis | SR 16 Gy SF / CRT 1×800 cGy | Pain control |
| NCT01752036 71 / Mar 2013 | Recruiting | Phase II | Spinal metastasis | SR: 30 Gy (HF) | Safety |
| NCT01347307 72 / Sep 2008 | Not recruiting(active) | Phase IV | Spinal metastasis | Benign: 12-16 Gy SF; 21-27 Gy HFMetastases: 14-25 Gy SF; 21-30 Gy HF | Tumor control |
| NCT01231061 73 / Nov 2010 | Completed | Phase II | Spinal metastasis | Arm 1:SR 24 Gy HF / SR 16 Gy SF | Pain control |
| NCT01950195 53 / Jun 2013 | Recruiting | Phase I | Spinal metastasis | SR+ipilimumab | Safety |
| NCT01624220 74 / Jun 2012 | Recruiting | Assignment | Spinal metastasis | SR+4 gold seeds implanted | Safety |
SR: spine radiosurgery; NPRS: numeric pain rating scale; TT: tomotherapy; QA: quality assurance; SF: single fraction; HF: hypofractionated; CRT: conventional radiotherapy; Post Op.: post operative; MSCC: metastatic spinal cord compression.
The RTOG is currently enrolling patients for a phase III trial, which is estimated to include 380 patients. The anticipated completion of primary data collection for this trial is July 2015 9. The trial compares 2 groups of patients: the first arm consists of patients undergoing SR (16 Gy delivered in a single fraction), while the second arm consists of patients undergoing conventional external beam radiotherapy treatment (800 cGy delivered in a single fraction). The patients will be stratified according to number of spine metastases treated (1 vs. 2-3) and radioresistant tumor classification (with radioresistant tumors including soft tissue sarcomas, melanomas, and renal cell carcinomas). The primary outcome is to determine whether SR improves pain control (measured by the 11-point Numerical Rating Pain Scale [NRPS]) compared with conventional external beam radiotherapy. The following secondary outcomes are also included: pain response and pain/lesion control at a treated site(s) compared with conventional external beam radiotherapy, as measured by the NRPS; local control; adverse events measured by NCI CTCAE v3.0 criteria; and long-term side effects (24 months) of SR on vertebral bone (e.g., vertebral compression fractures) and spinal cord, as measured by MRI.
MSKCC and collaborators are conducting a phase II RCT with an estimated enrollment of 200 patients and a primary anticipated completion date of October 2015. This trial includes patients over 18 years in age with metastatic lesions in the bone, spine, soft tissue and lymph nodes that have not been previously irradiated. The patients will be randomized into 2 groups: the first arm will receive SR using a single dose of 24 Gy and the second arm will be treated with fractioned SR using 27 Gy delivered in 3 fractions 30. The primary outcome is a comparison of loco-regional control rates at 24 months. The secondary outcomes are a toxicity comparison at 24 months, determination of failure patterns between the two cohorts at 24 months, and SUV uptake as a measure of tumor response and changes in tumor perfusion evaluated by dynamic contrast-enhanced (DCE)-MRI.
The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University is currently conducting a phase I study that aims to assess the safety of prescribing either SR or stereotactic brain radiosurgery (SRS) in combination with ipilimumab (Bristol-Myers Squibb, New York, NY) to treat patients with newly diagnosed brain or spinal metastases from melanoma. The estimated enrollment is 30 patients, with a primary completion date of December 2016. The primary outcomes are a description of the number and severity of adverse events at 24 months and an assessment of the safety profile of SBRT with concurrent ipilimumab. The secondary outcomes include estimates of local control rates in the brain and spine at 24 months, determination of the systemic control rate and evaluation of progression-free survival 59. Recently published data have reported that using a combination of ipilimumab plus SRS for melanoma brain metastasis is well tolerated and associated with better loco-regional control and possibly better survival rates. However, there was a 20% rate of grade 3 or 4 toxicity using this treatment modality 53.
A retrospective series evaluated 106 metastatic renal cell carcinoma patients (55 spine and 51 brain metastases) who were treated with simultaneous standard sorafenib or sunitinib (anti-angiogenic therapy) and stereotactic radiosurgery (SRS) or SR. The patients received an average dose of 20 Gy per lesion (range, 19–20 Gy) 54. The study showed no skin toxicity, neurotoxicity or myelopathy augment the adverse effects of anti-angiogenic therapy. Additionally, no treatment-related deaths or late complications were reported at 15 months. The local control rates for cerebral lesions at 12 and 24 months were 100% and 96.6%, respectively; for spinal lesions, the local control rates at 12 and 24 months were 94.1% and 90.4%, respectively. This series demonstrated that the use of SR / SRS plus anti-angiogenic therapy in this setting is safe and provides excellent local control.
The use of SR for metastatic tumors of the spine is safe and offers high local control rates. There are extensive data regarding pain control and local control; however, these data are mostly derived from retrospective and nonrandomized prospective series. Further studies are needed to determine appropriate SR fractionation schedules and clinical indications. Two RCTs (clinicaltrials.gov numbers NCT00922974 and NCT01223248) are ongoing and may provide the data needed to gain better insight into the factors that constitute optimal therapy. There is increasing interest in and a subsequent need to characterize combination drug therapy with SR to enhance local control and even improve survival in select groups of patients.
AUTHOR CONTRIBUTIONS
All authors were involved in the conception, methodology design, data collection and interpretation, writing, revision and final analysis of this manuscript.
Footnotes
The biological equivalent dose is a correlation of different radiotherapy dose schedules (total dose and fractionation) that produce similar biological effects.
No potential conflict of interest was reported.
REFERENCES
- 1.Böhm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br. 2002;84((4)):521–9. doi: 10.1302/0301-620x.84b4.12495. 10.1302/0301-620X.84B4.12495 [DOI] [PubMed] [Google Scholar]
- 2.Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine. 1990;15((1)):1–4. [PubMed] [Google Scholar]
- 3.Perrin RG, Livingston KE, Aarabi B. Intradural extramedullary spinal metastasis. A report of 10 cases. J Neurosurg. 1982;56((6)):835–7. doi: 10.3171/jns.1982.56.6.0835. [DOI] [PubMed] [Google Scholar]
- 4.Bilsky MH, Lis E, Raizer J, Lee H, Boland P. The Diagnosis and Treatment of Metastatic Spinal Tumor. The Oncologist. 1999;4((6)):459–69. [PubMed] [Google Scholar]
- 5.Gokaslan ZL, York JE, Walsh GL, McCutcheon IE, Lang FF, Putnam JB, et al. Transthoracic vertebrectomy for metastatic spinal tumors. J Neurosurg. 1998;89((4)):599–609. doi: 10.3171/jns.1998.89.4.0599. [DOI] [PubMed] [Google Scholar]
- 6.Eastley N, Newey M, Ashford RU. Skeletal metastases - the role of the orthopaedic and spinal surgeon. Surg Oncol. 2012;21((3)):216–22. doi: 10.1016/j.suronc.2012.04.001. 10.1016/j.suronc.2012.04.001 [DOI] [PubMed] [Google Scholar]
- 7.Finn MA, Vrionis FD, Schmidt MH. Spinal radiosurgery for metastatic disease of the spine. Cancer Control J Moffitt Cancer Cent. 2007;14((4)):405–11. doi: 10.1177/107327480701400411. [DOI] [PubMed] [Google Scholar]
- 8.Gerszten PC, Mendel E, Yamada Y. Radiotherapy and radiosurgery for metastatic spine disease: what are the options, indications, and outcomes. Spine. 2009;34(22 Suppl):S78–92. doi: 10.1097/BRS.0b013e3181b8b6f5. 10.1097/BRS.0b013e3181b8b6f5 [DOI] [PubMed] [Google Scholar]
- 9.ClinicalTrials.gov [Internet] 2009 Jun 17. Bethesda (MD): National Library of Medicine (US) Identifier NCT00922974; Phase II/III Study of Image-Guided Radiosurgery/SBRT for Localized Spine Metastasis. [cited 2015 June 06] Available from: http://clinicaltrials.gov/show/NCT00922974. [Google Scholar]
- 10.Ryu S, Pugh SL, Gerszten PC, Yin F-F, Timmerman RD, Hitchcock YJ, et al. RTOG 0631 Phase II/III Study of Image-Guided Stereotactic Radiosurgery for Localized (1-3) Spine Metastases: Phase II Results. Int J Radiat Oncol Biol Phys. 2011;81((2)):S131–2. doi: 10.1016/j.prro.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Sahgal A, Ames C, Chou D, Ma L, Huang K, Xu W, et al. Stereotactic body radiotherapy is effective salvage therapy for patients with prior radiation of spinal metastases. Int J Radiat Oncol Biol Phys. 2009;74((3)):723–31. doi: 10.1016/j.ijrobp.2008.09.020. 10.1016/j.ijrobp.2008.09.020 [DOI] [PubMed] [Google Scholar]
- 12.Jaffray DA, Siewerdsen JH, Wong JW, Martinez AA. Flat-panel cone-beam computed tomography for image-guided radiation therapy. Int J Radiat Oncol Biol Phys. 2002;53((5)):1337–49. doi: 10.1016/s0360-3016(02)02884-5. 10.1016/S0360-3016(02)02884-5 [DOI] [PubMed] [Google Scholar]
- 13.Yamada Y, Lovelock DM, Bilsky MH. A review of image-guided intensity-modulated radiotherapy for spinal tumors. Neurosurgery. 2007;61(2):226–35. doi: 10.1227/01.NEU.0000279970.10309.B5. 10.1227/01.NEU.0000279970.10309.B5 discussion 235. [DOI] [PubMed] [Google Scholar]
- 14.Reames BN, Krell RW, Ponto SN, Wong SL. Critical evaluation of oncology clinical practice guidelines. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31((20)):2563–8. doi: 10.1200/JCO.2012.46.8371. 10.1200/JCO.2012.46.8371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grilli R, Magrini N, Penna A, Mura G, Liberati A. Practice guidelines developed by specialty societies: the need for a critical appraisal. Lancet Lond Engl. 2000;355((9198)):103–6. doi: 10.1016/S0140-6736(99)02171-6. 10.1016/S0140-6736(99)02171-6 [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151((4)):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. W64. [DOI] [PubMed] [Google Scholar]
- 17.Webb S. The physical basis of IMRT and inverse planning. Br J Radiol. 2003;76((910)):678–89. doi: 10.1259/bjr/65676879. 10.4103/0971-6203.111309 [DOI] [PubMed] [Google Scholar]
- 18.Yamada Y, Lovelock DM, Yenice KM, Bilsky MH, Hunt MA, Zatcky J, et al. Multifractionated image-guided and stereotactic intensity-modulated radiotherapy of paraspinal tumors: a preliminary report. Int J Radiat Oncol Biol Phys. 2005;62((1)):53–61. doi: 10.1016/j.ijrobp.2004.09.006. 10.1016/j.ijrobp.2004.09.006 [DOI] [PubMed] [Google Scholar]
- 19.Klein EE, Hanley J, Bayouth J, Yin F-F, Simon W, Dresser S, et al. Task Group 142 report: Quality assurance of medical accelerators. Med Phys. 2009;36((9)):4197. doi: 10.1118/1.3190392. 10.1118/1.3190392 [DOI] [PubMed] [Google Scholar]
- 20.Benedict SH, Yenice KM, Followill D, Galvin JM, Hinson W, Kavanagh B, et al. Stereotactic body radiation therapy: The report of AAPM Task Group 101. Med Phys. 2010;37((8)):4078–101. doi: 10.1118/1.3438081. 10.1118/1.3438081 [DOI] [PubMed] [Google Scholar]
- 21.Lovelock DM, Hua C, Wang P, Hunt M, Fournier-Bidoz N, Yenice K, et al. Accurate setup of paraspinal patients using a noninvasive patient immobilization cradle and portal imaging. Med Phys. 2005;32((8)):2606–14. doi: 10.1118/1.1951042. 10.1118/1.1951042 [DOI] [PubMed] [Google Scholar]
- 22.Gerszten PC, Burton SA, Ozhasoglu C, Welch WC. Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine. 2007;32((2)):193–9. doi: 10.1097/01.brs.0000251863.76595.a2. 10.1097/01.brs.0000251863.76595.a2 [DOI] [PubMed] [Google Scholar]
- 23.Yamada Y, Bilsky MH, Lovelock DM, Venkatraman ES, Toner S, Johnson J, et al. High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys. 2008;71((2)):484–90. doi: 10.1016/j.ijrobp.2007.11.046. 10.1016/j.ijrobp.2007.11.046 [DOI] [PubMed] [Google Scholar]
- 24.Laufer I, Rubin DG, Lis E, Cox BW, Stubblefield MD, Yamada Y, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. The Oncologist. 2013;18((6)):744–51. doi: 10.1634/theoncologist.2012-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010;13((3)):324–8. doi: 10.3171/2010.3.SPINE09459. [DOI] [PubMed] [Google Scholar]
- 26.Degen JW, Gagnon GJ, Voyadzis J-M, McRae DA, Lunsden M, Dieterich S, et al. CyberKnife stereotactic radiosurgical treatment of spinal tumors for pain control and quality of life. J Neurosurg Spine. 2005;2((5)):540–9. doi: 10.3171/spi.2005.2.5.0540. [DOI] [PubMed] [Google Scholar]
- 27.Chang EL, Shiu AS, Mendel E, Mathews LA, Mahajan A, Allen PK, et al. Phase I/II study of stereotactic body radiotherapy for spinal metastasis and its pattern of failure. J Neurosurg Spine. 2007;7((2)):151–60. doi: 10.3171/SPI-07/08/151. [DOI] [PubMed] [Google Scholar]
- 28.Gerszten PC, Burton SA, Welch WC, Brufsky AM, Lembersky BC, Ozhasoglu C, et al. Single-fraction radiosurgery for the treatment of spinal breast metastases. Cancer. 2005 Nov 15. 104((10)):2244–54. doi: 10.1002/cncr.21467. 10.1002/cncr.21467 [DOI] [PubMed] [Google Scholar]
- 29.Gerszten PC, Burton SA, Belani CP, Ramalingam S, Friedland DM, Ozhasoglu C, et al. Radiosurgery for the treatment of spinal lung metastases. Cancer. 2006 Dec 1. 107((11)):2653–61. doi: 10.1002/cncr.22299. 10.1002/cncr.22299 [DOI] [PubMed] [Google Scholar]
- 30.Gerszten PC, Burton SA, Quinn AE, Agarwala SS, Kirkwood JM. Radiosurgery for the treatment of spinal melanoma metastases. Stereotact Funct Neurosurg. 2005;83((5-6)):213–21. doi: 10.1159/000091952. 10.1159/000091952 [DOI] [PubMed] [Google Scholar]
- 31.Wang XS, Rhines LD, Shiu AS, Yang JN, Selek U, Gning I, et al. Stereotactic body radiation therapy for management of spinal metastases in patients without spinal cord compression: a phase 1-2 trial. Lancet Oncol. 2012 Apr. 13((4)):395–402. doi: 10.1016/S1470-2045(11)70384-9. 10.1016/S1470-2045(11)70384-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Folkert MR, Bilsky MH, Tom AK, Oh JH, Alektiar KM, Laufer I, et al. Outcomes and toxicity for hypofractionated and single-fraction image-guided stereotactic radiosurgery for sarcomas metastasizing to the spine. Int J Radiat Oncol Biol Phys. 2014 Apr 1;88((5)):1085–91. doi: 10.1016/j.ijrobp.2013.12.042. 10.1016/j.ijrobp.2013.12.042 [DOI] [PubMed] [Google Scholar]
- 33.Gerszten PC, Burton SA, Ozhasoglu C, Vogel WJ, Welch WC, Baar J, et al. Stereotactic radiosurgery for spinal metastases from renal cell carcinoma. J Neurosurg Spine. 2005 Oct;3((4)):288–95. doi: 10.3171/spi.2005.3.4.0288. [DOI] [PubMed] [Google Scholar]
- 34.Ryu S, Rock J, Rosenblum M, Kim JH. Patterns of failure after single-dose radiosurgery for spinal metastasis. J Neurosurg. 2004 Nov;101(Suppl 3):402–5. [PubMed] [Google Scholar]
- 35.Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol Off J Am Soc Clin Oncol. 2007 Apr 10;25((11)):1423–36. doi: 10.1200/JCO.2006.09.5281. 10.1200/JCO.2006.09.5281 [DOI] [PubMed] [Google Scholar]
- 36.Chow E, Zeng L, Salvo N, Dennis K, Tsao M, Lutz S. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol R Coll Radiol G B. 2012;24((2)):112–24. doi: 10.1016/j.clon.2011.11.004. 10.1016/j.clon.2011.11.004 [DOI] [PubMed] [Google Scholar]
- 37.Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet Lond Engl. 2005 20;366((9486)):643–8. doi: 10.1016/S0140-6736(05)66954-1. 10.1016/S0140-6736(05)66954-1 [DOI] [PubMed] [Google Scholar]
- 38.Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative's Neuro-Oncology Disease Site Group. J Clin Oncol Off J Am Soc Clin Oncol. 2005 20;23((9)):2028–37. doi: 10.1200/JCO.2005.00.067. 10.1200/JCO.2005.00.067 [DOI] [PubMed] [Google Scholar]
- 39.Lee C-H, Kwon J-W, Lee J, Hyun S-J, Kim K-J, Jahng T-A, et al. Direct decompressive surgery followed by radiotherapy versus radiotherapy alone for metastatic epidural spinal cord compression: a meta-analysis. Spine. 2014 Apr 20;39((9)):E587–92. doi: 10.1097/BRS.0000000000000258. 10.1097/BRS.0000000000000258 [DOI] [PubMed] [Google Scholar]
- 40.Al-Omair A, Masucci L, Masson-Cote L, Campbell M, Atenafu EG, Parent A, et al. Surgical resection of epidural disease improves local control following postoperative spine stereotactic body radiotherapy. Neuro-Oncol. 2013 Oct;15((10)):1413–9. doi: 10.1093/neuonc/not101. 10.1093/neuonc/not101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moussazadeh N, Laufer I, Yamada Y, Bilsky MH. Separation surgery for spinal metastases: effect of spinal radiosurgery on surgical treatment goals. Cancer Control J Moffitt Cancer Cent. 2014 Apr;21((2)):168–74. doi: 10.1177/107327481402100210. [DOI] [PubMed] [Google Scholar]
- 42.Wang JC, Boland P, Mitra N, Yamada Y, Lis E, Stubblefield M, et al. Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004 Oct;1((3)):287–98. doi: 10.3171/spi.2004.1.3.0287. [DOI] [PubMed] [Google Scholar]
- 43.Moulding HD, Elder JB, Lis E, Lovelock DM, Zhang Z, Yamada Y, et al. Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. J Neurosurg Spine. 2010 Jul;13((1)):87–93. doi: 10.3171/2010.3.SPINE09639. [DOI] [PubMed] [Google Scholar]
- 44.Laufer I, Iorgulescu JB, Chapman T, Lis E, Shi W, Zhang Z, et al. Local disease control for spinal metastases following “separation surgery” and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: outcome analysis in 186 patients. J Neurosurg Spine. 2013;18((3)):207–14. doi: 10.3171/2012.11.SPINE12111. 10.3171/2012.11.SPINE12111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garg AK, Wang X-S, Shiu AS, Allen P, Yang J, McAleer MF, et al. Prospective evaluation of spinal reirradiation by using stereotactic body radiation therapy: The University of Texas MD Anderson Cancer Center experience. Cancer. 2011;117((15)):3509–16. doi: 10.1002/cncr.25918. 10.1002/cncr.25918 [DOI] [PubMed] [Google Scholar]
- 46.Damast S, Wright J, Bilsky M, Hsu M, Zhang Z, Lovelock M, et al. Impact of dose on local failure rates after image-guided reirradiation of recurrent paraspinal metastases. Int J Radiat Oncol Biol Phys. 2011;81((3)):819–26. doi: 10.1016/j.ijrobp.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 47.Mahadevan A, Floyd S, Wong E, Jeyapalan S, Groff M, Kasper E. Stereotactic body radiotherapy reirradiation for recurrent epidural spinal metastases. Int J Radiat Oncol Biol Phys. 2011;81((5)):1500–5. doi: 10.1016/j.ijrobp.2010.08.012. 10.1016/j.ijrobp.2010.08.012 [DOI] [PubMed] [Google Scholar]
- 48.Pan HY, Allen PK, Wang XS, Chang EL, Rhines LD, Tatsui CE, et al. Incidence and predictive factors of pain flare after spine stereotactic body radiation therapy: secondary analysis of phase 1/2 trials. Int J Radiat Oncol Biol Phys. 2014;90((4)):870–6. doi: 10.1016/j.ijrobp.2014.07.037. 10.1016/j.ijrobp.2014.07.037 [DOI] [PubMed] [Google Scholar]
- 49.Chiang A, Zeng L, Zhang L, Lochray F, Korol R, Loblaw A, et al. Pain flare is a common adverse event in steroid-naïve patients after spine stereotactic body radiation therapy: a prospective clinical trial. Int J Radiat Oncol Biol Phys. 2013;86((4)):638–42. doi: 10.1016/j.ijrobp.2013.03.022. 10.1016/j.ijrobp.2013.03.022 [DOI] [PubMed] [Google Scholar]
- 50.Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine. 2010;35((22)):E1221–9. doi: 10.1097/BRS.0b013e3181e16ae2. 10.1097/BRS.0b013e3181e16ae2 [DOI] [PubMed] [Google Scholar]
- 51.Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, et al. Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31((27)):3426–31. doi: 10.1200/JCO.2013.50.1411. 10.1200/JCO.2013.50.1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.ClinicalTrials.gov [Internet] 2010 Oct 14. Bethesda (MD): National Library of Medicine (US) Identifier NCT01223248, A Phase III Randomized Study Comparing Two Dosing Schedules for Hypofractionated Image-Guided Radiation Therapy in Patients With Metastatic Cancer; [cited 2015 June 10] Available from: http://clinicaltrials.gov/show/NCT01223248. [Google Scholar]
- 53.ClinicalTrials.gov [Internet] 2013 Jun 21. Bethesda (MD): National Library of Medicine (US) Identifier NCT01950195; A Pilot Study of Stereotactic Radiosurgery Combined With Ipilimumab in Patients With Newly Diagnosed Melanoma Metastases in the Brain and Spine. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01950195. [Google Scholar]
- 54.Staehler M, Haseke N, Nuhn P, Tüllmann C, Karl A, Siebels M, et al. Simultaneous anti-angiogenic therapy and single-fraction radiosurgery in clinically relevant metastases from renal cell carcinoma. BJU Int. 2011;108((5)):673–8. doi: 10.1111/j.1464-410X.2010.09895.x. 10.1111/j.1464-410X.2010.09895.x [DOI] [PubMed] [Google Scholar]
- 55.Ahmed KA, Stauder MC, Miller RC, Bauer HJ, Rose PS, Olivier KR, et al. Stereotactic body radiation therapy in spinal metastases. Int J Radiat Oncol Biol Phys. 2012;82((5)):e803–9. doi: 10.1016/j.ijrobp.2011.11.036. 10.1016/j.ijrobp.2011.11.036 [DOI] [PubMed] [Google Scholar]
- 56.Amdur RJ, Bennett J, Olivier K, Wallace A, Morris CG, Liu C, et al. A prospective, phase II study demonstrating the potential value and limitation of radiosurgery for spine metastases. Am J Clin Oncol. 2009;32((5)):515–20. doi: 10.1097/COC.0b013e318194f70f. 10.1097/COC.0b013e318194f70f [DOI] [PubMed] [Google Scholar]
- 57.Garg AK, Shiu AS, Yang J, Wang X-S, Allen P, Brown BW, et al. Phase 1/2 trial of single-session stereotactic body radiotherapy for previously unirradiated spinal metastases. Cancer. 2012;118((20)):5069–77. doi: 10.1002/cncr.27530. 10.1002/cncr.27530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klish DS, Grossman P, Allen PK, Rhines LD, Chang EL. Irradiation of spinal metastases: should we continue to include one uninvolved vertebral body above and below in the radiation field. Int J Radiat Oncol Biol Phys. 2011;81((5)):1495–9. doi: 10.1016/j.ijrobp.2010.07.2007. 10.1016/j.ijrobp.2010.07.2007 [DOI] [PubMed] [Google Scholar]
- 59.Haley ML, Gerszten PC, Heron DE, Chang Y-F, Atteberry DS, Burton SA. Efficacy and cost-effectiveness analysis of external beam and stereotactic body radiation therapy in the treatment of spine metastases: a matched-pair analysis. J Neurosurg Spine. 2011;14((4)):537–42. doi: 10.3171/2010.12.SPINE10233. 10.3171/2010.12.SPINE10233. [DOI] [PubMed] [Google Scholar]
- 60.Zelefsky MJ, Greco C, Motzer R, Magsanoc JM, Pei X, Lovelock M, et al. Tumor control outcomes after hypofractionated and single-dose stereotactic image-guided intensity-modulated radiotherapy for extracranial metastases from renal cell carcinoma. Int J Radiat Oncol Biol Phys. 2012;82((5)):1744–8. doi: 10.1016/j.ijrobp.2011.02.040. 10.1016/j.ijrobp.2011.02.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.ClinicalTrials.gov [Internet] 2012 Jul 17. Bethesda (MD): National Library of Medicine (US) Identifier NCT01654068, Conformal High Dose Intensity Modulated Radiation Therapy for Disease to Thoracic and Lumbar Spine; [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01654068. [Google Scholar]
- 62.ClinicalTrials.gov [Internet] 2007 Dez 17. Bethesda (MD): National Library of Medicine (US) Identifier NCT01290562, A Phase II Study of Spinal Radiosurgery; [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01290562. [Google Scholar]
- 63.ClinicalTrials.gov [Internet] 2007 Dec 12. Bethesda (MD): National Library of Medicine (US) Identifier NCT00573872; A Phase II Study of Spinal Radiosurgery. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT00573872. [Google Scholar]
- 64.ClinicalTrials.gov [Internet] 2013 Apr 03. Bethesda (MD): National Library of Medicine (US) Identifier NCT01849510; Efficacy of Dose Intensified Radiotherapy of Spinal Metastases of Solid Tumors by Dose Increased, Homogeneous Radiation of Vertebral Body and Simultaneous Application of Stereotactic Boost. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01849510. [Google Scholar]
- 65.ClinicalTrials.gov [Internet] 2014 Jun 17. Bethesda (MD): National Library of Medicine (US) Identifier NCT02167633; A Randomized Trial of Stereotactic Radiosurgery Versus Decompressive Surgery Followed by Postoperative Radiotherapy in Metastatic Spinal Cord Compression. [cited 2014 September 05] Available from: http://clinicaltrials.gov/ct2/show/NCT02167633. [Google Scholar]
- 66.ClinicalTrials.gov [Internet] 2009 Fev 27. Bethesda (MD): National Library of Medicine (US) Identifier NCT00853528; Cyberknife Radiosurgery for Improving Palliation of Metastatic Tumors of the Spine. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT00853528. [Google Scholar]
- 67.ClinicalTrials.gov [Internet] 2009 Fev 2008. Bethesda (MD): National Library of Medicine (US) Identifier NCT00631670; Stereotactic Body Radiation Therapy for Tumors Near the Spinal Cord. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT00631670. [Google Scholar]
- 68.ClinicalTrials.gov [Internet] 2011 Dec 13. Bethesda (MD): National Library of Medicine (US) Identifier NCT01525745; Randomized Ph II Study of Stereotactic Body Radiotherapy (SBRT) Versus Conventional Radiation for Spine Metastasis. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01525745. [Google Scholar]
- 69.ClinicalTrials.gov [Internet] 2013 April 03. Bethesda (MD): National Library of Medicine (US) Identifier NCT01826058; Spine Stereotactic Body Radiation Therapy for Metastatic Epidural Spinal Cord: Prospective Phase II Study. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01826058. [Google Scholar]
- 70.ClinicalTrials.gov [Internet] 2010 Dec 03. Bethesda (MD): National Library of Medicine (US) Identifier NCT01254903; Phase I Study of Feasibility of Single Session Spine Stereotactic Radiosurgery (SSRS) in the Primary Management in Patients With Inoperable, Previously Unirradiated Metastatic Epidural Spinal Cord Compression (MESCC) [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01254903. [Google Scholar]
- 71.ClinicalTrials.gov [Internet] 2012 Dec 14. Bethesda (MD): National Library of Medicine (US) Identifier NCT01752036; Phase II Study of Post-Operative Stereotactic Radiosurgery for Solid Tumor Spine Metastases. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01752036. [Google Scholar]
- 72.ClinicalTrials.gov [Internet] 2011 May 02. Bethesda (MD): National Library of Medicine (US) Identifier NCT01347307; Phase IV Trial Evaluating the Use of Stereotactic Body Radiotherapy for the Treatment of Spine Metastases and Primary Spine Tumors. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01347307. [Google Scholar]
- 73.ClinicalTrials.gov [Internet] 2010 Oct 29. Bethesda (MD): National Library of Medicine (US) Identifier NCT01231061; Randomized Phase II Study of Image-Guided Radiosurgery / SBRT for Localized Spine Metastasis. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01231061. [Google Scholar]
- 74.ClinicalTrials.gov [Internet] 2012 Jun 18. Bethesda (MD): National Library of Medicine (US) Identifier NCT01624220; A Prospective Study Using Implanted Fiducial Markers to Assess Treatment Accuracy and Esophageal Toxicity in Spinal Stereotactic Body Radiation Therapy. [cited 2014 September 05] Available from: http://clinicaltrials.gov/show/NCT01624220. [Google Scholar]