Abstract
OBJECTIVES:
Vaginal atrophy and breast cancer are common conditions in postmenopausal women and tamoxifen is the standard endocrine treatment for hormone-sensitive tumors. The present study aimed to assess the effect of tamoxifen on Ki-67 protein expression in the vaginal epithelium of castrated rats.
MATERIAL AND METHODS:
Forty Wistar-Hannover adult, virgin, castrated rats were randomly divided into two groups, group I (control, n=20) and group II (tamoxifen, n=20), receiving 0.5 ml of propylene glycol and 250 µg of tamoxifen diluted in 0.5 ml of propylene glycol, respectively, daily by gavage for 30 days. On the 31st day, the rats were euthanized and their vaginas were removed and fixed in 10% buffered formalin for the immunohistochemical study of Ki-67 protein expression. Data were analyzed by the Levene and Student's t tests (p<0.05).
RESULTS:
The mean index of Ki-67 expression in the rat vagina of groups I and II was 4.04±0.96 and 26.86±2.19, respectively (p<0.001).
CONCLUSIONS:
According to the results of the present study, tamoxifen, at the dose and treatment length used, induced a significant increase in the cell proliferation of the vaginal mucosa in castrated rats, as evaluated by Ki-67 protein expression.
Keywords: Tamoxifen, Rat, Vagina, Proliferation, Ki-67
INTRODUCTION
The number of postmenopausal women worldwide has increased due to improved access to healthcare services, better living conditions and increased life expectancy. Women spend approximately one-third of their lifetime in the postmenopausal period and may become vulnerable to chronic degenerative diseases such as breast cancer 1. Breast cancer is the most common malignancy among women, particularly in the postmenopausal period. In Brazil, breast cancer is an important cause of cancer-related death, with approximately 57,120 new cases of breast cancer and 13,345 deaths from this disease estimated for the year 2014 2,3,4. However, the survival of women with breast cancer has increased in the last few years, especially due to early diagnosis and to modes of systemic treatment. Endocrine treatment is the main treatment for women with estrogen receptor-positive breast cancer 5. Tamoxifen is a first-generation selective estrogen receptor modulator (SERM) approved by the US Food and Drug Administration (FDA) for primary chemotherapy and adjuvant treatment of women with breast cancer 6.
The mechanism of action of tamoxifen has not been fully elucidated. However, because it interacts particularly with estrogen receptors, tamoxifen may have an effect on symptoms due to hypoestrogenism, such as vaginal atrophy and dyspareunia, which are common in postmenopausal women with breast cancer 7,8,9,10,11. The vaginal mucosal epithelium has both alpha and beta estrogen receptors, with decreasing beta receptor levels after menopause 10. As shown by some authors, tamoxifen exerts both estrogenic and antiestrogenic effects in the vaginal epithelium of castrated rats 12. Nevertheless, other authors, by using indirect methods such as vaginal cytology, have shown that the drug exerts an estrogenic action on the vaginal mucosa of postmenopausal women 13,14,15. The study of drug effects on the vaginal tissue of postmenopausal women is not possible due to ethical reasons. As few studies have investigated the direct effect of tamoxifen on the vaginal epithelium of castrated rats, the present study was conducted.
MATERIAL AND METHODS
Animals
This study was approved by the Animal Experimentation Ethics Committee (AEEC) of the Universidade Federal do Piauí (UFPI), complying with the guidelines of the Brazilian College of Animal Experimentation (COBEA). Forty Wistar-Hannover virgin female rats obtained from the animal laboratory of the School of Veterinary Science at UFPI were used. The animals were housed inside a plastic cage with a metallic lid. Five animals per cage were kept since birth with free access to filtered water and rodent chow (SUPPRALAB®, São Paulo, Brazil). Ambient conditions were controlled by a 12-hour light/dark cycle, with the lights switched on from 7 a.m. to 7 p.m. Air conditioning maintained the temperature between 20 and 25°C. The animals were randomly divided into two groups: group I (control, n=20) and group II (tamoxifen, n=20). At 90 days of age, the rats in groups I and II weighing an average of 231.5±20.85 g and 231.2±21.74 g (p=0.9647), respectively, were castrated to eliminate gonadal sex steroid production through a dorsal paravertebral incision under anesthesia with 60 mg/kg ketamine and 4 mg/kg midazolam. Twenty-one days later, cytologic examination of Papanicolaou-stained vaginal smears was performed to characterize a decreased estrogen status, which was confirmed by the absence of cell maturation and a predominance of basal cells in all the animals. Group I rats (control) began to receive 0.5 ml/animal/day of propylene glycol (placebo) and Group II rats (experimental) received 250 μg/animal/day of tamoxifen citrate diluted in 0.5 ml of propylene glycol. The placebo and tamoxifen were continuously administered for 30 days, both at the same hour of the day, using a metal tube appropriate for gavage. On the 31st day, the rats from both groups were sacrificed and their vaginas were removed through a longitudinal abdominal incision for histologic and immunohistochemical studies.
Ethics Approval
This study was approved by the Animal Experimentation Ethics Committee (AEEC) of the Universidade Federal do Piauí (UFPI).
Ki-67 Immunohistochemistry
For the immunohistochemical study of Ki-67 expression, tissue specimens were fixed in 10% buffered formalin for a 12-24-hour period and then cut into 5-µm-thick sections. The sections were processed and stained with hematoxylin-eosin, deparaffinized in xylene for 5 minutes, dehydrated in absolute ethanol and washed in buffered saline solution at pH 7.4 for 5 minutes 16. Endogenous peroxidase activity was blocked with 3% hydrogen peroxide (H202) diluted in a buffered solution for 5 minutes. After epitope retrieval, the tissue samples were incubated with primary mouse anti-Ki-67 monoclonal antibody (clone MIB-5/Dako/1:100) in a refrigerator at approximately 4°C overnight. Subsequently, the samples were washed with buffered saline solution and incubated for 45 minutes in the NovoLink Polymer detection system. Color development was accomplished by incubating all the tissue samples in 3-3-diaminobenzidine tetrahydrochloride solution at a concentration of 1 mg/ml in a Tris-buffered solution, with a hydrogen peroxide solution used as a substrate, for 5 minutes. Subsequently, the tissues were counterstained with Harris' hematoxylin or methyl green for 5 minutes, followed by dehydration in ethanol and xylene baths. After the procedure, the slides were examined to quantify the results. Cells expressing Ki-67 protein were identified by the dark brown color of their nuclei.
Quantitative method
Ki-67 expression was quantified by two observers who were blinded to the group identification. Stained images were assessed by using a Nikon E400 light microscope connected to a Samsung color digital video camera, model SCC-131. The video camera captured and transmitted the image to a computer equipped with ImageLab® software, version 2.3, which was developed by Softium Informática Ltda (São Paulo, Brazil) for image analysis. To evaluate Ki-67 expression, 500 vaginal epithelial cells were counted on each slide whether or not the cells were stained with anti-Ki-67 MIB-5 antibody. A total magnification of ×400 was used to examine the slides. Cell counting was initiated at the site of greatest Ki-67 antigen expression. In each case, the percentage of stained cells was obtained by the ratio between the number of cells with stained nuclei and the total number of cells multiplied by 100.
Statistical Analysis
To evaluate group homogeneity relative to weight, Student's t test was used for independent samples. Variance analysis of the percentages of nuclei stained with anti-Ki-67 was conducted using the Levene and Student's tests 17. The significance level was set at p<0.05.
RESULTS
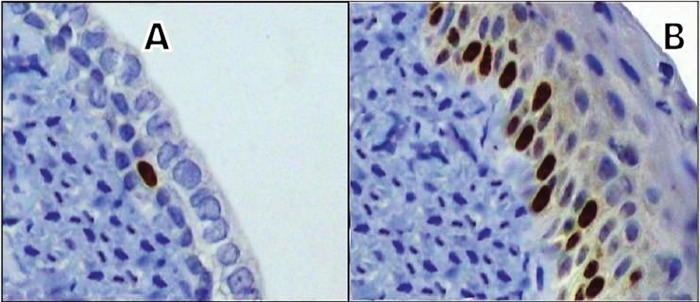
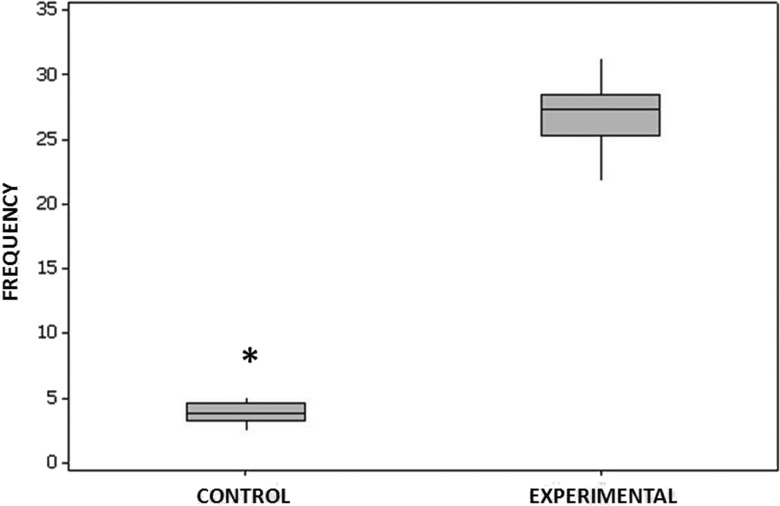
By light microscopy, cytologic examination of the vaginal epithelial cells of control group animals showed the absence of cell maturation and a predominance of basal cells, while tamoxifen-treated animals showed predominant cell maturation. Compared with control group animals, castrated female rats treated with tamoxifen showed a higher concentration of nuclei stained with anti-Ki-67 (Figure 1). The mean percentage of MIB-5-stained nuclei in the vaginal mucosa of group I (control) and group II (tamoxifen) rats was 4.04±0.96 and 26.86±2.19, respectively (p<0.001) (Table 1). The boxplot illustrates the median Ki-67 expression in the vaginal mucosal cells of animals from the control and tamoxifen groups (Figure 2).
Figure 1-.
Photomicrograph of a histological section of the vaginal epithelium of castrated rats showing a greater concentration of Ki-67-stained nuclei in the experimental group (tamoxifen) (B) compared with the control group (A) (original magnification x400).
Table 1.
Mean percentage of Ki-67-stanined nuclei in the vaginal mucosa of groups I (control) and II (tamoxifen).
| GROUP | N | AVERAGE | SE | SD | MINIMUM | MEDIAN | MAXIMUM |
|---|---|---|---|---|---|---|---|
| I | 20 | 4.04 | 0.21 | 0.96 | 2.51 | 3.86 | 6.69 |
| II | 20 | 26.86* | 0.49 | 2.19 | 21.77 | 27.38 | 31.23 |
<?ENTCHAR ast?>: p<0.001
Figure 2.
The median of Ki-67-stained nuclei in the vaginal mucosa of animals in the control and tamoxifen groups, as illustrated by the line in boldface.
DISCUSSION
In the present study, tamoxifen at a dose of 250 μg/animal/day administered for 30 days significantly increased proliferation of the vaginal mucosa in castrated rats, as evaluated by Ki-67 protein expression. The animals received tamoxifen orally (gavage) to mimic the administration route used in women. Furthermore, according to several authors that have studied different routes of administration, the oral route led to higher serum and tissue levels of tamoxifen, thereby increasing the bioavailability of tamoxifen 18,19. Tamoxifen was diluted in propylene glycol, a neutral, colorless and odorless vehicle, allowing for the dilution and administration of predefined doses 20,21.
However, the tamoxifen dose in animal experimental studies is not easy to standardize because rats have a faster metabolism than humans. Equal-weight doses may not reproduce the serum levels and effects of tamoxifen in women 22. Dos Santos et al. 21, who studied the morphometry of the urethra in castrated rats given a 250 µg/day tamoxifen dose for 30 days, observed that tamoxifen was capable of increasing the uterine weight and the thickness of the distal urethral epithelium. Thus, we used a dose of 250 µg/animal/day in this study because it could mimic the effects of tamoxifen on women undergoing breast cancer treatment 22.
Friedrich et al. 13 studied the influence of tamoxifen on vaginal epithelial maturation in postmenopausal women and demonstrated an apparent increase in vaginal epithelial maturation. In another study, Friedrich et al. 14 investigated the effects of tamoxifen on vaginal and cervical epithelial proliferation in postmenopausal women with breast cancer and found an apparent increase not only in the incidence of metaplasia and hyperplasia of endocervical cells but also in vaginal epithelial maturation. According to Bertolissi et al. 15, tamoxifen exerts an early and persistent estrogenic effect on the vaginal epithelium during the first year of therapy in postmenopausal women with breast cancer.
Nevertheless, Berg and Dunfee 23 showed that postmenopausal women with high levels of squamous epithelial cell maturation were 15 times more likely than women in the same age group exhibiting an atrophic pattern to have coexistent endometrial adenocarcinoma because tamoxifen acts in accordance with circulating estrogen levels. Therefore, when estrogen levels are low, tamoxifen behaves as an agonist and may cause endometrial cancer. In contrast, during the premenopausal period, when estrogen levels are higher, tamoxifen appears to have an antiestrogenic action in this tissue 24. Thus, the agonist or antagonist action of SERMs in the endometrium may depend on circulating estrogen levels 25,26.
The results of the present study indicate that tamoxifen, at the dose and length of treatment used in this study, induced a significant increase in cell proliferation of the vaginal mucosa in castrated rats, as evaluated by Ki-67 protein expression. Thus, the assessment of cell proliferation in the vagina of castrated rats, used to as a mimic of postmenopausal women, revealed that tamoxifen displayed partially estrogenic action on the vaginal mucosa of these animals.
AUTHORS CONTRIBUTION
Nery Aguiar AR and Aguiar YQ contributed to the data collection and to the manuscript writing. Alencar AP contributed to the statistical analysis. Conde Jr AM, Lopes-Costa PV and Tavares CB contributed to the data collection. da Silva BB conceived and planned the study and contributed to the data collection, to the manuscript writing and to conducting this study.
ACKNOWLEDGMENTS
We thank all the members of our research team.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Fernandes CE, Morita MH, Ferreira JA, da Silva EP, Wehba AS. Approach to urinary tract disorders in postmenopausal women. Rev Paul Med. 1990;108((5)):230–5. [PubMed] [Google Scholar]
- 2.de Sousa JA, Facina G, da Silva BB, Gebrim LH. Effects of low-dose tamoxifen on breast biomarkers Ki-67, estrogen and progesterone receptors. Int Semin Surg Oncol. 2006;3:29. doi: 10.1186/1477-7800-3-29. 10.1186/1477-7800-3-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch BM, Neilson HK, Friedenreich CM. Physical activity and breast cancer prevention. Recent Results Cancer Res. 2011;186:13–42. doi: 10.1007/978-3-642-04231-7_2. 10.1007/978-3-642-04231-7_1 [DOI] [PubMed] [Google Scholar]
- 4.Estimates of new cases and deaths from breast cancer (INCA, 2014): http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/mama [Google Scholar]
- 5.Singh MS, Francis PA, Michael M. Tamoxifen, cytochrome P450 genes and breast cancer clinical outcomes. Breast. 2011;20((2)):111–8. doi: 10.1016/j.breast.2010.11.003. 10.1016/j.breast.2010.11.003 [DOI] [PubMed] [Google Scholar]
- 6.Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90((18)):1371–88. doi: 10.1093/jnci/90.18.1371. 10.1093/jnci/90.18.1371 [DOI] [PubMed] [Google Scholar]
- 7.Jordan VC. An overview of considerations for testing of tamoxifen as a preventive breast cancer. Ann N Y Acad Sci. 1995;768:141–7. doi: 10.1111/j.1749-6632.1995.tb12117.x. 10.1111/j.1749-6632.1995.tb12117.x [DOI] [PubMed] [Google Scholar]
- 8.Vardy MD, Lindsay R, Scotti RJ, Mikhail M, Richart R, Nieves J, et al. Short-term urogenital effects of raloxifene, tamoxifen, and estrogen. Am J Obstet Gynecol. 2003;189((1)):81–8. doi: 10.1067/mob.2003.374. 10.1067/mob.2003.374 [DOI] [PubMed] [Google Scholar]
- 9.da SILVA BB, Lopes IM, Gebrim LH. Effects of raloxifene on normal breast tissue from premenopausal women. Breast Cancer Res Treat. 2006;95((2)):99–103. doi: 10.1007/s10549-005-9001-2. 10.1007/s10549-005-9001-2 [DOI] [PubMed] [Google Scholar]
- 10.Lara LA, Useche B, Ferriani RA, Reis RM, de Sá MF, de Freitas MM, et al. <italic>The</italic> effects of hypoestrogenism on the vaginal wall<italic>:</italic> interference with the normal sexual response. J Sex Med. 2009;6((1)):30–9. doi: 10.1111/j.1743-6109.2008.01052.x. 10.1111/j.1743-6109.2008.01052.x [DOI] [PubMed] [Google Scholar]
- 11.Kellogg-Spadt S. Vulvovaginal atrophy. Adv Nurse Pract. 2010;18((4)):31–2. [PubMed] [Google Scholar]
- 12.Kim NN, Stankovic M, Armagan A, Cushman TT, Goldstein I, Traish AM. Effects of tamoxifen on vaginal blood flow and epithelial morphology in the rat. BMC Womens Health. 2006;6:14–24. doi: 10.1186/1472-6874-6-14. 10.1186/1472-6874-6-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedrich M, Mink D, Villena-Heinsen C, Woll-Hermann A, Wagner S, Schmidt W. The influence of tamoxifen on the maturation index of vaginal epithelium. Clin Exp Obstet Gynecol. 1998;25((4)):121–4. [PubMed] [Google Scholar]
- 14.Friedrich M, Mink D, Villena-Heinsen C, Woll-Hermann A, Schmidt W. Tamoxifen and proliferation of vaginal and cervical epithelium in postmenopausal women with breast cancer. Eur J Obstet Gynecol Reprod Biol. 1998;80((2)):221–5. doi: 10.1016/s0301-2115(98)00117-1. 10.1016/S0301-2115(98)00117-1 [DOI] [PubMed] [Google Scholar]
- 15.Bertolissi A, Cartei G, Turrin D, Cioschi B, Rizzi V. Behaviour of vaginal epithelial maturation and sex hormone binding globulin in postmenopausal breast cancer patients during the first year of tamoxifen therapy. Cytopathology. 1998;9((4)):263–70. doi: 10.1046/j.1365-2303.1998.00077.x. 10.1046/j.1365-2303.1998.00077.x [DOI] [PubMed] [Google Scholar]
- 16.Masson P. Tumours humaines. Histologie diasgnostic et techniques. 2nded. Paris: Libraire Maloine; 1956. pp. 1061–148. [Google Scholar]
- 17.Kutner MH, Nachtshein CJ, Neter J, Li W. Applied linear statistical models. 5thed. Boston: McGraw-Hill Irwin; 2005. [Google Scholar]
- 18.Degregorio MW, Wilbur BJ, Coronado E, Osborne CK. Serum tamoxifen concentrations in the athymic nude mouse after three methods of administration. Cancer Chemother Pharmacol. 1987;20((4)):316–8. doi: 10.1007/BF00262583. 10.1007/BF00262583 [DOI] [PubMed] [Google Scholar]
- 19.Kisanga ER, Gjerde J, Schjott J, Mellgren G, Lien EA. Tamoxifen administration and metabolism in nude mice and nude rats. J Steroid Biochem Mol Biol. 2003;84((2-3)):361–7. doi: 10.1016/s0960-0760(03)00051-7. 10.1016/S0960-0760(03)00051-7 [DOI] [PubMed] [Google Scholar]
- 20.dos Santos AR, Lopes-Costa PV, da Silva BB. Vascular endothelial growth factor expression in the urethral epithelium of castrated adult female rats treated with tamoxifen. Gynecol Endocrinol. 2009;25((2)):282–6. doi: 10.1080/09513590802488420. 10.1080/09513590802488420 [DOI] [PubMed] [Google Scholar]
- 21.dos Santos AR, Lopes-Costa PV, de Castro JCD, Campos IC, Borges RS, Pires CG, et al. Morphometric analysis of the urethra of castrated female rats treated with tamoxifen. Maturitas. 2008;59((3)):275–80. doi: 10.1016/j.maturitas.2008.02.010. 10.1016/j.maturitas.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 22.Lien EA, Solheim E, Ueland PM. Distribution of tamoxifen and its metabolites in rat and human tissues during steady-state treatment. Cancer Res. 1991;51((18)):4837–44. [PubMed] [Google Scholar]
- 23.Berg JW, Dunfee GR. Cytological presentation of endometrial carcinoma. Cancer. 1958;11((1)):158–72. doi: 10.1002/1097-0142(195801/02)11:1<158::aid-cncr2820110128>3.0.co;2-e. 10.1002/1097-0142(195801/02)11:1<158::AID-CNCR2820110128>3.0.CO;2-E [DOI] [PubMed] [Google Scholar]
- 24.Mourits MJ, De Vries EG, Willemse PH, Ten Hoor KA, Hollema H, Van der Zee AG. Tamoxifen treatment and gynecologic side effects: a review. Obstet Gynecol. 2001;97((5 Pt 2)):855–66. doi: 10.1016/s0029-7844(00)01196-0. 10.1016/S0029-7844(00)01196-0 [DOI] [PubMed] [Google Scholar]
- 25.Patriarca MT, Simöes RD, Smaniotto S, De Teves DC, Simöes Mde D, Evêncio-Neto et al. Morphological action of tamoxifen in the endometrium of persistent estrous rats. Acta Obstet Gynecol Scand. 1996;75((8)):707–10. doi: 10.3109/00016349609065731. 10.3109/00016349609065731 [DOI] [PubMed] [Google Scholar]
- 26.Gielen SC, Kühne LC, Ewing PC, Blok LJ, Burger CW. Tamoxifen treatment for breast cancer enforces a distinct gene-expression profile on the human endometrium: an exploratory study. Endocr Relat Cancer. 2005;12((4)):1037–49. doi: 10.1677/erc.1.01046. 10.1677/erc.1.01046 [DOI] [PubMed] [Google Scholar]