Abstract
Musculoskeletal ultrasound utilises high-frequency linear transducers to produce high-resolution images of soft tissue structures. It is an increasingly useful tool in the assessment of both acute and chronic musculoskeletal injuries; it is relatively cheap, portable and can be used to facilitate targeted injections. In this review paper, we aim to provide a summary on the normal and abnormal appearances of skeletal tissue in the setting of acute and chronic lower limb sporting injuries.
Keywords: Ultrasound, lower limb, sports, injuries
Introduction
Acute and chronic lower limb injuries frequently occur as a result of sport or exercise. Acute injuries often have a defined onset and mechanism. They commonly occur in team sports such as football or rugby where there is contact between players, sports associated with high speeds such as cycling or skiing, or where there is a risk of falling such as horse riding.1 These injuries are often related to either direct impact or twisting injuries, where the forces imparted exceed maximum physiological thresholds, resulting in combinations of acute bony or soft tissue damage. Acute injuries are also frequently encountered in “explosive” events involving sprinting, jumping or weight lifting.2
Chronic overuse injuries, by comparison, may have a gradual, insidious onset commonly occurring in aerobic endurance sports, such as long-distance running or in technical events where there is a frequently repeated action, such as throwing, hitting a ball or jumping. Repetitive microtrauma, below the threshold for symptoms, exceeds the ability of tissue to repair. Symptoms eventually develop when there is sufficient accumulative damage and may be precipitated by a relatively minor acute event.3
Ultrasound is frequently utilised in the evaluation of lower limb injuries and is particularly useful in the assessment of acute and chronic tendon conditions such as tenosynovitis, tendinopathy and tears.4 Large superficial tendons such as the Achilles and patellar tendon are most suitable for ultrasound assessment providing high-resolution anatomical images with a degree of physiological assessment such as the presence of neovascularisation and response to loading. Smaller superficial tendons, such as tibialis posterior or the peroneal tendons, are more technically challenging but can also be assessed with a high degree of accuracy.5
The severity of acute muscle injuries due to direct or indirect trauma may also be graded with ultrasound and healing monitored, which can assist in predicting return to sport.4,6
Sonographic equipment and technique
High-frequency (10–17 MHz) linear array transducers, with a small footprint provide excellent detail and spatial resolution and are used in musculoskeletal (MSK) ultrasound to assess superficial structures, such as tendons, small joints and muscles.7 Lower frequency transducers may be required to assess deeper structures, such as the hip joint.7
Good ultrasound technique requires a detailed knowledge of MSK anatomy and a careful methodical assessment using the ultrasound probe in both the transverse and longitudinal planes in order to identify pathology. Optimal imaging of a tendon requires the transducer to be perpendicular to the tendon in order to visualise the detailed fibrillar architecture and avoid spurious hypoechoic change due to anisotropy.8
Sonographic palpation is used to identify the site of maximum clinical tenderness, which can be correlated to the underlying structures visible on the scan image, which further increases the sensitivity of ultrasound.6 Colour and power Doppler are also helpful to assess tissue vascularity in the setting of acute inflammation or chronic neovascularistion.
Normal sonographic appearances
Skeletal muscle is composed of multiple individual muscle fibres called myofibrils, which are encased in a thin connective tissue layer, which is referred to as the endomysium. The myofibrils are grouped together into fascicles and surrounded by loose septa called perimysium. Groups of fascicles are bundled together and summate to form the muscle belly, which is encased in a further hyperechoic fascial sheath referred to as the epimysium, which is continuous with the perimysium. These connective tissue septa coalesce to form tendons at each end of the muscle. On ultrasound, the muscle fibres are seen as relatively hypoechoic structures with interposed hyperechoic lines of perimysium separating the fibres and a thin layer of echogenic epimysium surrounding the whole muscle (Figure 1(a)). On transverse scanning, the alternating hyperechoic perimysium and hypoechoic muscle fibres give the so-called “starry night” appearance.9 Each muscle is arranged in a definable pattern in order to perform its specific function. Muscles may be unipennate (a single muscle belly serving a tendon), bipennate or multipennate. Muscles can attach to the bone via a tendon, or insert directly onto the periosteum.
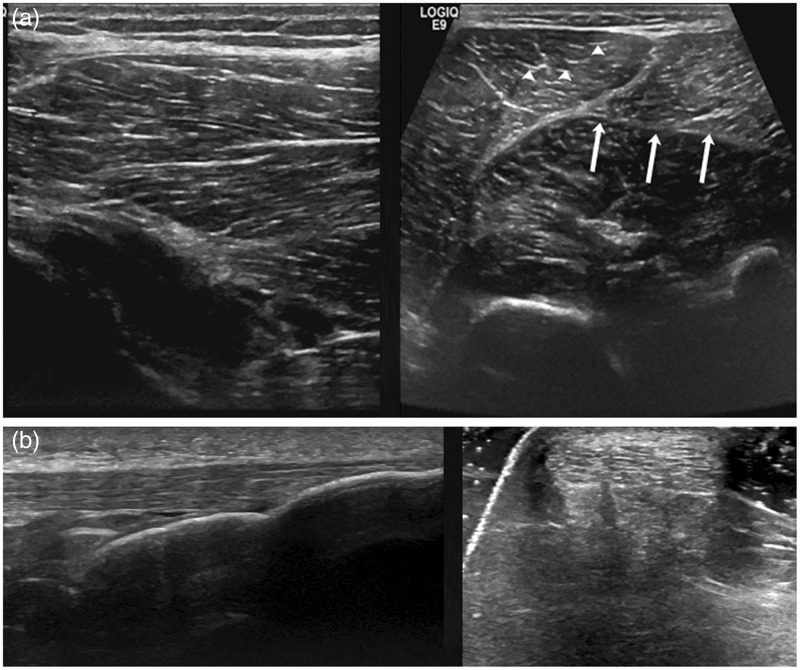
Figure 1.
(a) Longitudinal and transverse views of normal skeletal muscle. The arrow heads show innumerable hyperechoic dots/dashes, which represent the perimysium. The epimysium (arrows) demarcates the hyperechoic fascial boundary surrounding the muscle. (b) Longitudinal and transverse views of a normal Achilles tendon. Normal tendon appears as an array of echogenic parallel lines (bundles of collagen fibres) or as multiple echogenic dots on short axis
Tendons transmit forces from the muscle to the skeleton and consist of an organised array of collagen fibres tightly packed together with supporting connective tissue. They differ from ligaments in their composition, having a greater percentage of collagen fibres and a smaller proteoglycan and elastin component. The collagen fibres are arranged in a parallel fashion, which form bundles of fibres, and in a hierarchical system produce an actual tendon.10 On ultrasound, the normal tendon architecture appears as echogenic parallel lines in longitudinal section or as echogenic dots when imaged in a transverse plane (Figure 1(b)).
Tendon sheaths are typically seen surrounding those tendons coursing around bony structures or passing through fibro-osseous tunnels such as tendons around the ankle and wrist. The tendon sheath comprises two synovial layers, which may contain an abnormal excess amount of fluid in cases of tenosynovitis or tendon degeneration. Some tendons, such as the Achilles tendon, are surrounded by a loose fatty connective tissue called the paratenon, which contributes to the blood supply of the tendon.11 Both ligaments and tendons exhibit anisotropy, therefore, orientation of the ultrasound beam perpendicular to the fascicle is important in order to optimally visualise the echogenic collagen fibres.11
Ligaments consist primarily of type 1 collagen with glyoproteins and elastin representing a smaller percentage of their dry weight. Their primary function is in joint stabilisation as well as providing proprioceptive feedback.12 They can be intra-articular (cruciate ligaments of the knee), extra-articular (calcaneofibular ligament) or capsular (anterior talofibular ligament). The orientation of the collagen fibres is variable and relates to each ligament’s specific function. Ligaments appear as echogenic fibrillar structures and probe orientation is more important when imaging ligaments due to the less organised arrangement of their fibres.8
Principles of injury
Lower limb sports injuries can be attributed to the mechanism and types of forces imparted into the tissues involved. Forces transmitted to muscle, tendon or ligament can be direct or indirect leading to either an acute or chronic type of injury. Basic knowledge of the biomechanical properties of these specialised tissues enables better understanding of the aetiology and types of injuries encountered by athletes.
Direct injuries are due to forces transmitted via an external blow, often in contact sports. The presentation is acute with a clear mechanism of injury often leading to superficial abrasions, ecchymosis and muscle contusion or laceration. Tendons and ligaments are not as commonly injured via this mechanism.13
Indirect injuries can affect muscles, tendons and ligaments, all of which are viscoelastic structures. When a constant load is applied, there is typically a linear relationship between deformation and load throughout an elastic region. With increasing load, the structure enters a yield point, followed by plastic deformation before ultimate failure or rupture.14,15 When the force is great enough to cause injury, damage is dependent on the rate and amount of loading. An acute injury or tear occurs when the tissue is rapidly loaded beyond its ultimate failure point.16 This would be the case for an Achilles tendon rupture when an athlete may describe a sudden feeling of being kicked in the back of the calf and hearing an audible “pop”.17
With repeated cyclical loading that nears the yield point, microfailure and tears may develop. This represents an overuse type injury, which tends to occur more commonly in tendons than in ligaments and may initially be asymptomatic. In this setting, a chronic over use injury may present acutely following an apparently minor incident.
Muscle injuries
Muscle injuries are very common in sport and can occur in a wide range of different muscle groups. A top level football team with 25 squad members can expect around 15 clinically significant muscle injuries each season equating to 148 missed training sessions and 37 missed matches.18 Acute muscle injuries can be classified as direct or indirect depending on the mechanism of injury. Direct injuries result in contusions and lacerations, whereas indirect injuries are muscle tears caused by internal forces with tensile overload, and account for the vast majority of significant muscle injuries seen in high-level athletes.18 Muscle tears frequently result from eccentric contraction where the muscle is developing tension whilst lengthening. This often affects the myotendinous junction of superficial muscles in which there is a predominance of fast twitch type 2 fibres.19 Injuries tend to occur in those muscles which span two joints, such as the rectus femoris and medial head of gastrocnemius.20 Tears can be intramuscular or occur at the myofascial junction and in some cases avulse directly from bone. In elite footballers, tears are seen most commonly within four major muscle groups of the lower limb (hamstrings 37%, adductors 23%, quadriceps 19% and calf muscle 13%).18
There have been several proposed classification systems for the grading of muscle injuries with the latest consensus suggesting that the term tear be used instead of strain in describing muscle injuries. These grading systems group muscle injuries into partial or (sub)total tears.21 The Peetrons classification is a commonly used system, which separates muscle tears into three grades.6
Grade I injuries involve less than 5% of a muscle and may show focal or general areas of increased reflectivity signifying muscle oedema without focal haematoma or muscle fibre retraction, although a small amount of perifascial fluid may be seen.6 Ultrasound may appear normal. Subtle injuries however, particularly in deep muscles, can be easier to detect with MRI.22 Grade II injuries are partial ruptures involving 5–50% of the cross sectional diameter of a muscle with associated bleeding and muscle fibre retraction. Ultrasound will reveal a hypoechoic or anechoic gap within the muscle fibres, where there is discontinuity of fibres and haematoma formation (Figure 2(a) and (b)).23 Hypervascularity at the ruptured muscle ends may be present on power Doppler. Grade III tears involve complete rupture, which is usually associated with retraction (Figure 2(c)). These lesions are often clinically evident with a palpable gap between the retracted muscle ends and on ultrasound there is complete muscle discontinuity with extensive haematoma. The “bell-clapper” sign may be seen, which refers to the rounded margin of the balled-up, retracted muscle, surrounded by haematoma.24 Grade III rupture is much less common than partial tears.23
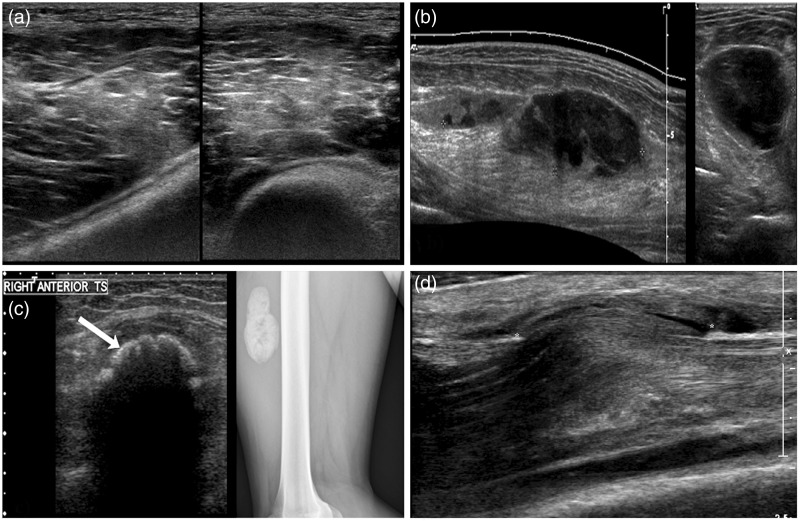
Figure 2.
(a) Longitudinal and transverse views of the left gastrocnemius muscle in a female runner showing a 5.5 cm myofascial separation tear consistent with a grade II injury. Complexity and stranding within the hypoechoic area represents blood clot. Intact muscle fibres are seen on the transverse view. (b) Longitudinal and transverse views of the hamstring muscle in a footballer demonstrating moderately extensive hyperechoic change representing haemorrhage and oedema (white arrow) suggestive of a grade II injury. Contemporaneous MRI images of the same injury show a small discrete haematoma and muscle fibre retraction. (c) A longitudinal view of the hamstrings in a water skier with a corresponding MRI image. The white arrow demonstrates the proximal end of the retracted muscle stump consistent with a grade III injury
Grading of muscle injuries, especially in elite athletes, is important in determining treatment, planning rehabilitation and predicting the lay-off time from full training or competition. Grade I injuries have an average lay-off time of approximately two weeks and grade II approximately four weeks.25 Grade III injuries can have a lay-off time in excess of three months with the biceps femoris muscle being most commonly injured in elite footballers for all grades.18 There may be an additional benefit in further subclassifying grade II injuries into smaller and larger tears. Tears affecting the myofascial junction are often managed differently by physiotherapists.26 Tears close to the tendon insertion or at the myotendinous junction will often take longer to recover.26
Following an acute muscle injury, return to full sporting activity is not usually advocated until healing is complete, although athletes will often continue to train and compete with minor grade I injuries.27 Premature return to sporting activity following a muscle injury can lead to extension of the tear or recurrent injury, which may predispose to excess scar tissue formation. In a study involving professional footballers, 16% of muscle tears were reported to be re-injuries, which take on average 30% longer to heal than the initial injury.25 Scarring appears as a hyperechoic focus with associated architectural distortion and may have a surrounding hypoechoic zone.28 The site of scar formation matches that of the muscle injury and often occurs at a musculotendinous or myofascial junction.
Other sequelae of injury include muscle atrophy and fatty change. This can occur following a large grade II/III injury with localised atrophy, from a neural injury causing muscle denervation or from disuse with diffuse loss of muscle bulk.29 Fatty atrophy classically begins around the central tendon and myotendinous junction resulting in increased reflectivity on ultrasound when compared with normal muscle.6 Comparison with the normal contralateral side can be useful to confirm the abnormal echogenicity and to assess the degree of atrophy.
High-grade muscle injuries may present late as a “pseudomass” representing a condensed mass of disorganised muscle fibres with or without scar tissue. There is often associated retraction, and dynamic sonography during muscle contraction can accentuate the lesion.30
Muscle contusions
Blunt direct trauma produces compression and sheering injury of muscle and can cause an acute intramuscular contusion with haemorrhage. Damage is often most severe in those muscles directly contacting bone where compression forces may be greatest, e.g. vastus intermedius lying adjacent to the femur. Patients will present with immediate and often prolonged pain and a significant deficit in contractility in the affected muscle.31 Joint stiffness and weakness may be long-term sequelae. On ultrasound, a contusion is seen as a focal loss of the normal muscle fibrillar architecture with a heterogeneous region of increased echogenecity, which may cross the fascial boundaries (Figure 3(a)).32 Over several hours, an intramuscular or fascial haematoma may form resulting in a discrete poorly compressible hypoechoic collection of partially clotted blood (Figure 3(b)). After approximately 7–10 days, ultrasound may demonstrate fluctuant echo poor locules signifying clot liquefaction.33 At this stage, the serous component may be amenable to ultrasound-guided aspiration unlike an acute haematoma, which would be thick, gelatinous and difficult to drain. In some cases, haematoma aspiration can reduce symptoms and improve range of motion, allowing progression of the patient’s rehabilitation and potentially expediting recovery and return to sport. Rarely, these injuries can be associated with an acute compartment syndrome requiring measurement of intracompartmental pressures.34
Figure 3.
(a) Longitudinal and transverse views of the vastus medialis obliquus muscle following blunt direct trauma. Diffuse hyperechoic change and loss of fibrillar architecture represents acute bleeding and oedema within the muscle with no loss of continuity. (b) Longitudinal and transverse views of a 9 cm calf haematoma following direct trauma. This may evolve into a more hypoechoic looking seroma which may be amenable to aspiration to expedite recovery. (c) Transverse view of the anterior thigh in a footballer 3 months post blunt trauma. A highly reflective curvilinear opacity within the muscle substance (white arrow) casting dense posterior acoustic shadowing. The corresponding lateral radiograph shows a smooth lobular calcified mass lying anterior to the femoral cortex, consistent with myositis ossificans. (d) An acute muscle hernia in a professional footballer following blunt trauma. Bulging of the tibialis anterior muscle through a defect in the overlying fascia (*) is shown with adjacent haemorrhage
Myositis ossificans
Myositis ossificans is a benign condition characterised by intramuscular ossification that can occur following direct muscle injury and contusion.35 The pathophysiology of myositis ossificans is not fully understood and because it can present with a painful mass, differentiation from a soft-tissue tumour is required. Coarse calcification is a late sign and is evident on plain radiographs. In the early phase, a hypoechoic mass with peripheral echogenic foci is seen.36 Later on, a more focal calcific deposit is demonstrated with associated posterior acoustic shadowing, which is aligned with the long axis of the muscle (Figure 3(c)). Unlike sarcoma, an important differential, the ossification in myositis ossificans begins at the periphery and quite often, further cross-sectional imaging is required in establishing a diagnosis.28
Muscle herniation
This is a relatively uncommon injury, usually due to blunt direct trauma causing fascial disruption and herniation of the underlying muscle through the defect. It is most commonly encountered in the anterior tibial compartment.37 In the acute setting, the fascial tear may be seen as a discrete discontinuation of the fascia with adjacent haemorrhage and localised bulging of the underlying muscle as it herniates through the defect (Figure 3(d)). In the more chronic setting, diagnosis may require dynamic scanning during muscle contraction to demonstrate herniation.
Morel-Lavallée lesion
The Morel-Lavallée lesion is a chronic superficial seroma, which forms between subcutaneous fat and the underlying fascia. It follows a closed degloving injury with sheering forces causing separation of the subcutaneous fat from the underlying fascia, creating a space which fills with lymph, blood and fat.38 Sonographically, this lesion is seen as a well defined, often oval, hypoechoic collection which may have internal echoes, septations and fat globules but no vascularity. It is superficial to the underlying fascia and may demonstrate a capsule of variable thickness (Figure 4). They are most commonly encountered over the lateral aspect of the hip but can occur elsewhere, particularly around the knee.39 Ultrasound can be utilised to guide percutaneous drainage, although collections frequently recur and repeated aspiration, sclerosant injection or surgery may be required.
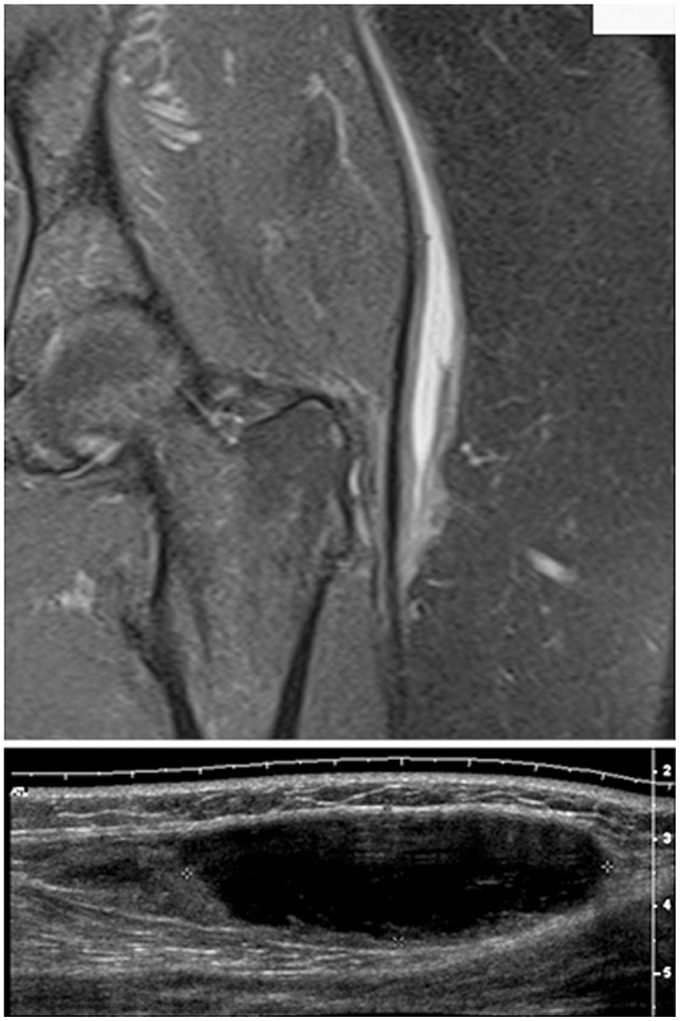
Figure 4.
A coronal fluid sensitive MRI image and a longitudinal ultrasound view, in different patients, showing a pocket of serous fluid lying at the junction of the subcutaneous fat and underlying fascia lata. Often from blunt trauma, the subcutaneous fat sheers off from the underling fascia creating a potential space
Tendon injuries
Tendon injuries can be divided up into acute and overuse injuries. Acute injuries occur suddenly from a specific force, and are often encountered in sports where there is high speed, explosive forces and contact (skiing, football). Tendon injuries can occur at the musculotendinous junction, within the tendon substance, at the bone–tendon junction or, in the case of adolescent athletes, as a bony avulsion of an unfused apophysis.40,41 Acute tendon tears may be partial or complete. In complete tears, the tendon ends can be separated by fluid, blood or herniated adjacent soft-tissue structures (Figure 5(a) and (b)). Dynamic assessment of the tendon with ultrasound during passive stretching can be useful in establishing the diagnosis. Acute injuries are not as common as overuse injuries which often occur in the setting of tendinopathy.42
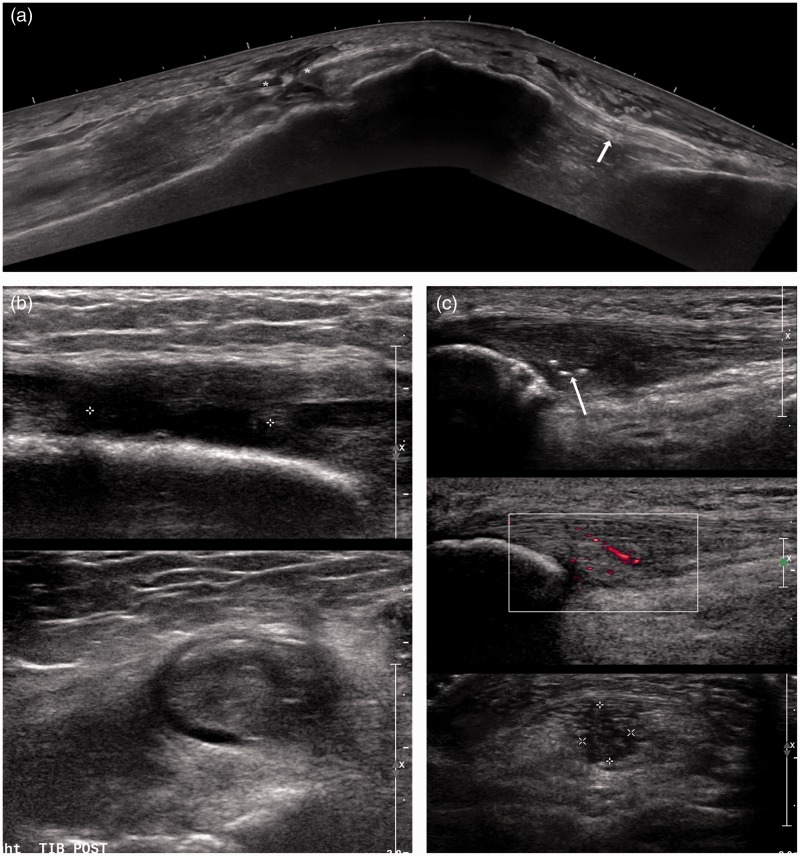
Figure 5.
(a) A panoramic longitudinal view of the extensor mechanism in a middle aged man showing a complete full thickness rupture of the central fibres of the quadriceps tendon. Intact tendon fibres of vastus lateralis were seen. The partially retracted tendon ends are shown (*). Normal fibrillar structure of the patellar tendon is demonstrated (white arrow). (b) Longitudinal and transverse views of the right tibialis posterior tendon. There is complete loss of continuity (grade III) of the tendon with hypoechoic fluid seen within the tendon sheath. (c) Longitudinal and transverse views of the proximal patellar tendon showing thickening, hypoechoic change, and loss of fibrillar architecture. Focal areas of dystrophic calcification represented by three echogenic foci are also present (white arrow). Appearances are consistent with chronic patellar tendinosis with neovascularity within the proximal patellar tendon
Repeated movements impart low-magnitude tissue forces over a period of time. This can lead to repetitive microtrauma, and if not allowed sufficient time to repair, may result in an overuse injury.15 With overuse injuries, there is often a painful, inflammatory phase of tendonitis characterised sonographically by increased vascularity, hypoechoic oedematous tissue, synovitis and possible small tears.40 This may be followed by a degenerative, or tendinopathic period where there is tendon thickening, loss of fibrillar architecture and microcalcification, all of which may be seen on ultrasound (Figure 5(c)).11 Overuse tendon injuries are encountered in a wide variety of sports including distance runners, racquet sports and kicking athletes.
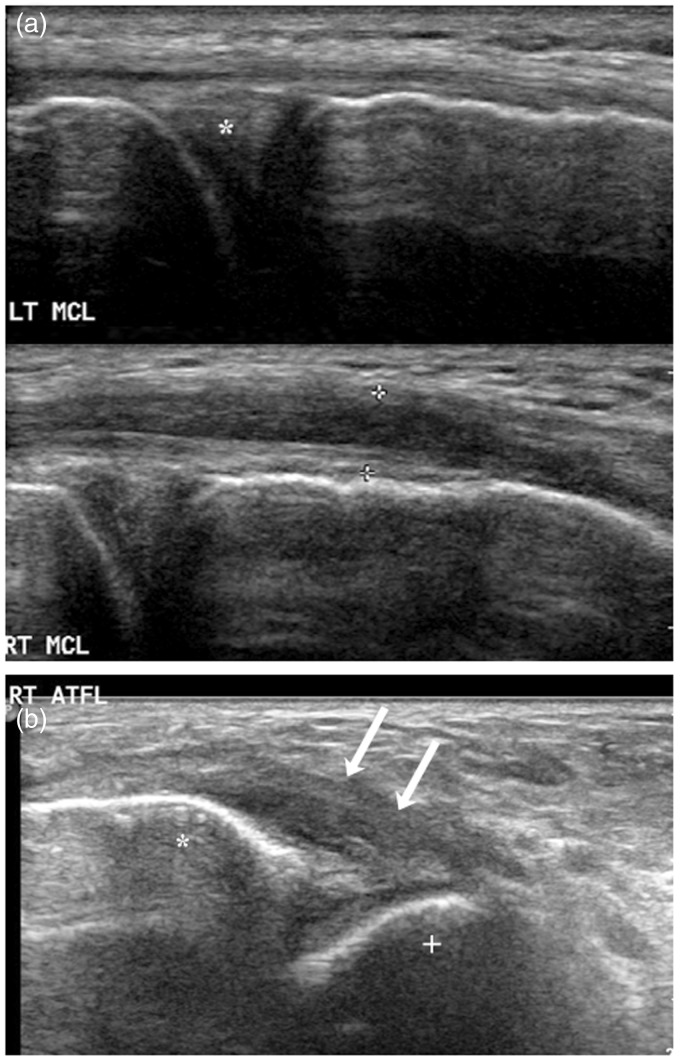
Figure 6.
(a) A longitudinal view of a normal left MCL which appears thin with preserved fibrillar architecture. In comparison, a longitudinal view of an injured right MCL which is thickened and hypoechoic but remains intact (grade II injury). The medial joint space and medial meniscus (*) are seen deep to the MCL. (b) The white arrows demonstrate grossly thickening hypoechoic change to the right anterior talofibular ligament following an inversion injury consistent with an acute grade II injury (* = fibular; + = talus)
Tenosynovitis is an inflammatory condition of the sheath covering the tendon. Thickening and increased vascularity may be demonstrated on ultrasound as well as fluid within the tendon sheath.43 This condition is often encountered within the tendons around the ankle in long-distance runners where the cause is often repetitive microtrauma. Ill-fitting shoes may also be a contributing factor leading to impingement. If conservative methods fail, ultrasound-guided steroid injection into the tendon sheath and not the actual tendon may be beneficial.44
Ligament injuries
Unlike tendons, where overuse injuries predominate, ligaments are classically injured following an acute trauma with the ankle being the most common site. Ligament injuries can occur midsubstance, at the ligament–bone interface or as a bony avulsion injury. Ligament injuries are classified as grade I, II and III.45 Grade I injuries are interstitial tears, often from acute trauma, without macroscopic disruption. The ligament may appear normal sonographically, although there is likely to be adjacent fluid and inflammatory change. Grade II injuries are partial tears and ultrasound demonstrates thickening and partial disruption of the fibres (Figure 6(a) and (b)). In grade III injuries, there is discontinuity of the ligament with retraction of the torn ends and associated oedema/haemorrhage. As with muscle injuries, the higher the grade of ligament injury, the longer the lay-off time for that individual.2,11
Capsular ligaments such as the medial collateral ligament (MCL) of the knee have a good healing potential following a grade III injury, whereas intra-articular ligaments such as the ACL generally do not heal after a complete rupture.16
Ligaments can be evaluated with ultrasound in the acute setting; however, high-grade ligament tears are frequently associated with other intra-articular injuries and assessment with MRI is often preferred. In the chronic setting, ultrasound can be used to demonstrate ongoing thickening, inflammation, impingement or laxity in relation to accessible ligaments such as the MCL and ATFL. From this, it is possible to guide a variety of percutaneous injection techniques.46
Bursitis
Bursitis is inflammation of one of the many bursae found in the lower limb, which are small synovial lined sacs located between tissues, such as bone, tendon, muscle and skin. They serve to reduce friction and rubbing and can become inflamed with repetitive over use injury, such as in long distance runners. Patients usually present with pain at that site and on ultrasound, the bursa may appear thickened and inflamed with anechoic synovial fluid.47 Around the hip, trochanteric and Iliopsoas bursitis can be managed with conservative measures such as physiotherapy, but if that fails, ultrasound-guided steroid injections can be beneficial.48
Conclusion
Ultrasonography is an effective imaging modality in both diagnosing and monitoring lower limb sporting injuries. With a superior spatial resolution to MRI, ultrasound is able to resolve individual muscle fibres and therefore detect injuries to these structures. In allowing the operator real-time contact with the patient, clinical and functional assessment may be carried out in an effort to aid diagnosis. Ultrasound is useful in targeted injections and being portable, sonography may be performed readily at sporting venues thus allowing for a speedy diagnosis and subsequent treatment.
DECLARATIONS
Competing interests: The authors have no conflicts of interest to declare.
Funding: This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical approval: Not applicable.
Guarantor: LK
Contributorship: NP and LK researched literature and conceived the review article. NP wrote the first draft of the manuscript. LK revised the manuscript and provided the clinical cases. All authors reviewed and approved the final version of the manuscript.
References
- 1.De Freitas Guina Fachina RJ, Andrade MDS, Silva FR, et al. Descriptive epidemiology of injuries in a Brazilian premier league soccer team. Open access J Sport Med 2013; 4: 171–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fong DT, Chan Y-Y, Mok K-M, et al. Understanding acute ankle ligamentous sprain injury in sports. Sports Med Arthrosc Rehabil Ther Technol 2009; 1: 14–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weatherall PT, Crues JV. Musculotendinous injury. Magn Reson Imaging Clin N Am 1995; 3: 753–72. [PubMed] [Google Scholar]
- 4.Torriani M, Kattapuram SV. Musculoskeletal ultrasound: an alternative imaging modality for sports-related injuries. Top Magn Reson Imaging 2003; 14: 103–111. [DOI] [PubMed] [Google Scholar]
- 5.Erickson SJ. Sonography of the foot and ankle. Foot Ankle Clin 2000; 5: 29–48 (v). [PubMed] [Google Scholar]
- 6.Peetrons P. Ultrasound of muscles. Eur Radiol 2002; 12: 35–43. [DOI] [PubMed] [Google Scholar]
- 7.Jacobson JA, van Holsbeeck MT. Musculoskeletal ultrasonography. Orthop Clin North Am 1998; 29: 135–67. [DOI] [PubMed] [Google Scholar]
- 8.Jamadar DA, Robertson BL, Jacobson JA, et al. Musculoskeletal sonography: important imaging pitfalls. Am J Roentgenol 2010; 194: 216–25. [DOI] [PubMed] [Google Scholar]
- 9.Grimm A, Prell T, Décard BF, et al. Muscle ultrasonography as an additional diagnostic tool for the diagnosis of amyotrophic lateral sclerosis. Clin Neurophysiol 2015; 126: 820–7. [DOI] [PubMed] [Google Scholar]
- 10.Kannus P. Structure of the tendon connective tissue. Scand J Med Sci Sports 2000; 10: 312–20. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor PJ, Hodgson RJ, Grainger AJ. Tendon and ligament imaging. Br J Radiol 2012; 85: 1157–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frank CB. Ligament structure, physiology and function. J Musculoskelet Neuronal Interact 2004; 4: 199–201. [PubMed] [Google Scholar]
- 13.Bastos FN, Vanderlei FM, Vanderlei LCM, et al. Investigation of characteristics and risk factors of sports injuries in young soccer players: a retrospective study. Int Arch Med 2013; 6: 14–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin TWTW, Cardenas L, Soslowsky LJLJ. Biomechanics of tendon injury and repair. J Biomech 2004; 37: 865–77. [DOI] [PubMed] [Google Scholar]
- 15.Maganaris CN, Narici MV, Almekinders LC, et al. Biomechanics and pathophysiology of overuse tendon injuries: ideas on insertional tendinopathy. Sports Med 2004; 34: 1005–17. [DOI] [PubMed] [Google Scholar]
- 16.Woo SL-Y, Abramowitch SD, Kilger R, et al. Biomechanics of knee ligaments: injury, healing, and repair. J Biomech 2006; 39: 1–20. [DOI] [PubMed] [Google Scholar]
- 17.Saltzman CL, Tearse DS. Achilles tendon injuries. J Am Acad Orthop Surg 1998; 63: 16–25. [DOI] [PubMed] [Google Scholar]
- 18.Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 2011; 39: 1226–32. [DOI] [PubMed] [Google Scholar]
- 19.Kary JM. Diagnosis and management of quadriceps strains and contusions. Curr Rev Musculoskelet Med 2010; 3: 26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garrett WE. Muscle strain injuries. Am J Sports Med 1996; 24(6 Suppl): S2–8. [PubMed] [Google Scholar]
- 21.Mueller-Wohlfahrt H-W, Haensel L, Mithoefer K, et al. Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br J Sports Med 2013; 47: 342–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Megliola A, Eutropi F, Scorzelli A, et al. Ultrasound and magnetic resonance imaging in sports-related muscle injuries. Radiol Med 2006; 111: 836–45. [DOI] [PubMed] [Google Scholar]
- 23.Koh ESC, McNally EG. Ultrasound of skeletal muscle injury. Semin Musculoskelet Radiol 2007; 11: 162–73. [DOI] [PubMed] [Google Scholar]
- 24.Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol 2004; 183: 975–84. [DOI] [PubMed] [Google Scholar]
- 25.Walden M, Ekstrand J, English B, et al. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med 2012; 46: 112–7. [DOI] [PubMed] [Google Scholar]
- 26.Best TM. Soft-tissue injuries and muscle tears. Clin Sports Med 1997; 16: 419–34. [DOI] [PubMed] [Google Scholar]
- 27.Kilcoyne KG, Dickens JF, Keblish D, et al. Outcome of grade I and II hamstring injuries in intercollegiate athletes: a novel rehabilitation protocol. Sports Health 2011; 3: 528–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Woodhouse JB, McNally EG. Ultrasound of skeletal muscle injury: an update. Semin Ultrasound CT MR 2011; 32: 91–100. [DOI] [PubMed] [Google Scholar]
- 29.Girolami M, Galletti S, Montanari G, et al. Common peroneal nerve palsy due to hematoma at the fibular neck. J Knee Surg 2013; 26(Suppl 1): S132–5. [DOI] [PubMed] [Google Scholar]
- 30.Pomeranz SJ, Heidt RS. MR imaging in the prognostication of hamstring injury. Work in progress. Radiology 1993; 189: 897–900. [DOI] [PubMed] [Google Scholar]
- 31.Crisco JJ, Hentel KD, Jackson WO, et al. Maximal contraction lessens impact response in a muscle contusion model. J Biomech 1996; 29: 1291–6. [DOI] [PubMed] [Google Scholar]
- 32.Lee JC, Healy J. Sonography of lower limb muscle injury. Am J Roentgenol 2004; 182: 341–51. [DOI] [PubMed] [Google Scholar]
- 33.Alessandrino F, Balconi G. Complications of muscle injuries. J Ultrasound 2013; 16: 215–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trojian TH. Muscle contusion (thigh). Clin Sports Med 2013; 32: 317–24. [DOI] [PubMed] [Google Scholar]
- 35.Miller AE, Davis BA, Beckley OA. Bilateral and recurrent myositis ossificans in an athlete: a case report and review of treatment options. Arch Phys Med Rehabil 2006; 87: 286–90. [DOI] [PubMed] [Google Scholar]
- 36.Lacout A, Marcy P-Y, Carlier R, et al. Myositis ossificans imaging: keys to successful diagnosis. Indian J Radiol Imaging 2012; 22: 35–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beggs I. Sonography of muscle hernias. Am J Roentgenol 2003; 180: 395–9. [DOI] [PubMed] [Google Scholar]
- 38.Parra JA, Fernandez MA, Encinas B, et al. Morel-Lavallée effusions in the thigh. Skeletal Radiol 1997; 26: 239–41. [DOI] [PubMed] [Google Scholar]
- 39.Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: twenty-seven cases in the national football league. Am J Sports Med 2007; 35: 1162–7. [DOI] [PubMed] [Google Scholar]
- 40.Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. J Musculoskelet Neuronal Interact 2006; 6: 181–90. [PubMed] [Google Scholar]
- 41.Micheli LJ, Fehlandt AF. Overuse injuries to tendons and apophyses in children and adolescents. Clin Sports Med 1992; 11: 713–26. [PubMed] [Google Scholar]
- 42.Robinson P. Sonography of common tendon injuries. Am J Roentgenol 2009; 193: 607–18. [DOI] [PubMed] [Google Scholar]
- 43.Khoury V, Guillin R, Dhanju J, et al. Ultrasound of ankle and foot: overuse and sports injuries. Semin Musculoskelet Radiol 2007; 11: 149–61. [DOI] [PubMed] [Google Scholar]
- 44.Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med 2009; 19: 54–64. [DOI] [PubMed] [Google Scholar]
- 45.Fessell DP, Vanderschueren GM, Jacobson JA, et al. US of the ankle: technique, anatomy, and diagnosis of pathologic conditions. RadioGraphics 1998; 18: 325–40. [DOI] [PubMed] [Google Scholar]
- 46.Allen GM, Wilson DJ. Ultrasound in sports medicine – a critical evaluation. Eur J Radiol 2007; 62: 79–85. [DOI] [PubMed] [Google Scholar]
- 47.Hirji Z, Hunjun JS, Choudur HN. Imaging of the bursae. J Clin Imaging Sci 2011; 1: 22–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Toohey AK, LaSalle TL, Martinez S, et al. Iliopsoas bursitis: Clinical features, radiographic findings, and disease associations. Semin Arthritis Rheum 1990; 20: 41–7. [DOI] [PubMed] [Google Scholar]