Abstract
The British Medical Ultrasound Society (BMUS), the Consortium for the Accreditation of Sonographic Education (CASE), education providers and the NHS are working together to review how best to develop education for the future sonographic workforce. There is currently a national vacancy rate of approximately 12% across NHS Trusts. Education course placements are often limited to the number of clinical training places available within departments, resulting in a disparity between vacancies and the numbers of qualified sonographers graduating. Clearly there is a need for education to match the service demand. A term often used as a solution to the workforce problem is ‘direct entry’ ultrasound education. Anecdotally this term has caused confusion amongst health care professionals and as such the aim of this work was to gain an understanding of the views and opinions of BMUS members and interested professionals about direct entry training and subsequent development of any future training programmes. BMUS undertook an online survey with 286 responses. The survey provided insight into the opinions of ultrasound practitioners and the complexities of developing a relevant educational programme for the future sonographer workforce. The results suggested a number of concerns with direct entry ultrasound programmes, including insufficient training places, lack of health care background knowledge, lack of imaging knowledge and no state registration specific to sonographers. Benefits of direct entry to ultrasound training were perceived to be increasing the number of sonographers trained each year, whilst training people in their first choice profession with skills developed specific to the sonographer role. Support for direct entry ultrasound training was limited to 51% of respondents who would advocate this form of ultrasound training if it led to qualified sonographers with the same skills as sonographers exiting from current CASE accredited programmes.
Keywords: Direct entry, undergraduate ultrasound, postgraduate ultrasound, sonographer education, training
Introduction
There is a shortage of qualified sonographers in the United Kingdom.1,2 This is a statement heard repeatedly at regional and national meetings and events such as the annual scientific meetings hosted by The British Medical Ultrasound Society (BMUS).3 It is estimated by the Society and College of Radiographers (SCoR)4 that there is at least a 12% vacancy rate across the United Kingdom, which cannot be filled with qualified sonographers. This is clearly impacting on service delivery and sonography is now listed as a shortage specialty by the UK Government Migration Advisory Committee (MAC).1 This situation is not new; in 2003, BMUS published a policy statement regarding the provision of ultrasound services in the United Kingdom.5 The statement highlighted the dangers of inadequate service provision, in particular that examinations performed by staff not specifically nor adequately trained in ultrasound scanning and interpretation may be misleading and dangerous to patients. These sonographer shortages are likely to continue as workloads increase, changes to working practices, such as 7-day working,2 are implemented and imminent retirement of experienced sonographers.2
Appropriate training in ultrasound is clearly the key to providing a safe diagnostic and interventional ultrasound service in any setting.5,6 Understanding what is appropriate training is less well defined. Providing appropriate training in a clinical setting is becoming increasingly difficult7 given the pressures mounting on diagnostic services in terms of increased demand and complexity of examinations, coupled with a shortage of qualified staff and an ageing population.8,9
In 2013, the SCoR published two separate documents exploring the issues of Ultrasound Training, Employment and Registration6 and Direct Entry Undergraduate Ultrasound Programmes.10 Both documents address relevant important issues, such as recommendations for training and registration, but provide no solutions as to how the profession is to increase numbers of qualified sonographers. At the time of writing this paper, work is being undertaken by NHS England, who have established a sonographer workforce working party, to review the current and future state of sonographer recruitment, retention and training needs. BMUS wanted to understand members’ opinions, to ensure it could make an informed contribution to the working party, supporting members’ views. The aim of this study was to determine members’ understanding of direct entry and their opinions on some of the issues relating to the topic.
Sonographer education pathways
Until the early 1990s, ultrasound education and qualificatory awards were provided for radiographers by the College of Radiographers (CoR). Qualified radiographers traditionally were offered clinical training places within their local departments with regional theoretical education being provided using the CoR syllabus. The Diploma of Medical Ultrasound (DMU) was awarded to radiographers following completion of the log book and examinations set by the CoR.11 Whilst radiographers were developing their ultrasound skills and services, ultrasound examinations were also undertaken by non-radiographers, with many medical physics departments providing services within the hospital setting. However, the majority of ultrasound examinations were performed by radiographers12 and from personal experience it was uncommon to find other non-radiographers such as midwives and physiotherapists undertaking diagnostic ultrasound examinations.
Following the move of radiography education from the CoR to higher education institutes (HEIs) in the 1990s, ultrasound education began to diversify with more non-radiographer practitioners entering the profession. Currently in the United Kingdom, medical ultrasound is taught at postgraduate level with the majority of sonographers entering from a healthcare background such as radiography or midwifery.4 The most common pathway for sonographers is an undergraduate degree in radiography, midwifery or nursing followed by a period of practical experience as a qualified member of staff before the individual joins a post graduate programme to undertake their ultrasound training.2 There are exceptions, with some individuals opting to progress directly to the ultrasound programme,13 but the norm has been established for many years. It is understood that there are increasing pressures on these primary professions themselves, leading to a reduction of suitable trainees entering ultrasound training programmes. The demand for ultrasound services has since risen exponentially,14 with NHS examinations rising from approximately 4 million in 1995–1996 to over 9 million in 2012–2013,14 leading to a subsequent demand for more ultrasound practitioners. Additionally, there is increasing pressure on radiographers with changes being made to workforce numbers in response to the ‘A&E 4 Hour Target’ implemented in 20041,5 and 7 day working.2 A shortage of sonographers entering from the traditional radiography route began to be appreciated with alternative recruitment pathways being explored.
Over time, HEI course developments have occurred in response to local needs for more sonographers, such as modular pathways for nurses or midwives, to complete a postgraduate certificate in a specialist area, e.g. obstetrics, negotiated specialist modules and short focussed courses16 but there is no national universally accepted programme being developed. Some HEIs are now looking at recruiting any graduates onto a medical ultrasound post-graduate (Pg) course, providing they have reached a specific academic level, and using the term of post-graduate direct entry.17 Direct entry education pathways were first muted by the SCoR in 2009,4 as a possible solution to increasing the number of graduates entering the ultrasound profession.
As an alternative to direct entry, one HEI has developed a ‘3 + 1’ programme; the 3 years being a BSc radiography programme with an additional post-graduate year.13 This is the full time post-graduate diploma (PgDip) medical ultrasound course offered to existing radiography students with a first class or 2:1 BSc (hons) degree in radiography. The successful students continue to be registered at the university to complete the PgDip in their ‘+1 year,’ with local departments providing clinical placements. This ‘3 + 1’ model effectively bypasses the need for an individual to undertake an education break and gain employment prior to continuing their ultrasound education. This model was developed in a Local Education and Training Board (LETB) region which already provides funding to Trusts to employ trainee sonographers, although this funding is under threat of cuts.13 Therefore, this graduate education programme (3 + 1) gives a great financial advantage to the local education budget, as funding is provided for university fees and a small student bursary as opposed to the training salary, backfill costs for an existing member of the radiography workforce and fees of the traditional training route.
Many postgraduate ultrasound courses in the United Kingdom are accredited by the Consortium for the Accreditation of Sonographic Education (CASE)16 and have a minimum exit qualification of post graduate certificate (PgCert). CASE also accredits shorter, focused courses that allow, for example, a physiotherapist to train in a specific area of musculoskeletal practice. The question facing CASE is whether it is now appropriate to accredit undergraduate ultrasound education6 and whether its member organisations, including BMUS, support this.
In the United Kingdom at present, no primary degree in medical ultrasound is available,6 although it is understood that such courses are being considered by HEIs for future development. BMUS and the SCoR recognise that there are major issues which need to be considered and understood prior to the development of undergraduate education, not least the acceptance that statutory registration for sonographers is not attainable currently.4,10 Both organisations recognise that the key stakeholders of the employers, HEIs, LETBs and, not least, ultrasound practitioners need to engage with discussions about how best to educate the future workforce to ensure appropriate training and an increased number of suitably qualified sonographers. It is with these issues in mind that the professional issues education stream at the 2014 BMUS Annual Scientific Meeting (ASM) was organised and delivered by a range of experienced experts in this field.3
Terminology relating to direct entry has caused confusion in personal discussions with health care professionals. There are two forms of direct entry that have been discussed in meetings. These are direct entry undergraduate (Ug) programmes, which take students without a degree and train them to BSc (hons) level in the same way that radiography students and other health care professionals are trained. The other is postgraduate (Pg) direct entry in which someone with a BSc (hons) degree in a non-health related subject (or health related if they selected that route) can train to become a sonographer and exit with an MSc.4
Registration
Without doubt, statutory registration of sonographers is a contentious issue. The United Kingdom Association of Sonographers, along with BMUS, SCoR and other professional bodies, campaigned for the terms sonographer/ultrasonographer to become protected titles and therefore a registered profession.18 There is a debate to be had within the profession as to the value of registration and whether there are alternative options that can be used to equally safeguard patients,10 but no clear directive is apparent. As previously suggested, direct entry courses are being developed.17 However, employment opportunities may be limited if the graduates are unable to gain statutory registration and this is deemed essential by an employer for someone to practice ultrasound. The matter demands discussion with employers and educationalists prior to any course development that provides training but limited employment opportunities in the United Kingdom.
It is acknowledged that there are already sonographers practicing who do not have statutory registration. Indeed there is anecdotal evidence that vascular scientists are being trained to complete the PgDip in obstetrics and gynaecology and general medicine and subsequently undertaking examinations without registration. The SCoR established the public voluntary register to enable ultrasound practitioners to register themselves and evidence their practice.19 However, acceptance on to the voluntary register does not in itself authenticate competence or fitness to practice and debate is required as to whether education alone is sufficient to validate practice of individuals in the long term.
Members’ views of direct entry courses
With all of these issues in mind it became apparent that the views of ultrasound practitioners and educationalists regarding ultrasound education for future sonographers had to be collected. BMUS holds a large ultrasound annual scientific meeting (ASM) in the United Kingdom with over 450 delegates attending the meeting in 2014. BMUS membership is made up from a range of ultrasound professionals including radiologists, physicists, scientists, midwives, vets and, largely, sonographers who constitute approximately half of the total members.20 During discussion sessions at the 2014 ASM there appeared to be a lack of clarity about the options for future service delivery and in particular what various professional bodies, HEIs and sonographers meant by the term ‘direct entry.’ It was suggested that a survey of member’s opinions would provide more detailed information about the views of interested parties. With approval from BMUS Council, and with input from CASE, a short survey was produced. The survey was designed to gain insight into the ultrasound professionals’ understanding and opinions regarding direct entry ultrasound training and potential subsequent development of training courses. The survey was not designed to gain an opinion of whether members agreed with undergraduate education. There are many factors to be taken into account prior to such a decision being made and the survey was designed to explore such issues. This article aims to highlight some of the survey findings.
Method
An online survey (available with the online version of this article at http://ult.sagepub.com) was written and designed by the chair of the 2014 ASM and BMUS representatives on CASE Council. The questions were devised to explore the most pertinent and recurring issues that arose during discussions by the authors with their peers. Subsequent discussions at the BMUS Council meeting in November 2014 highlighted further information that would be valuable in formulating a policy and stance on future education programme development. The survey was approved by the BMUS Council at the November 2014 meeting and the current CASE chair. The survey consisted of 8 closed questions with some free text facilities for respondents to provide additional information. Due to time constraints to ensure the survey was available for the December 2014 ASM, a pilot study was not carried out. The finalised survey was sent electronically using SurveyMonkey® to all members of the British Medical Ultrasound Society and all registrants of the 2014 BMUS ASM with known email addresses. Members were excluded if no contact email address was available. The survey was sent in January 2015, with a response deadline of 28 February 2015, to 1450 participants.
Respondents were asked to choose either single or multiple responses, dependent upon the question asked. The results were collated via SurveyMonkey® in tables ranked in preference with free text comments being given separately.
Results
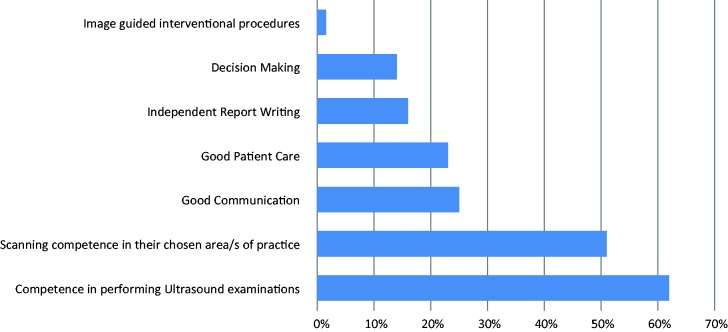
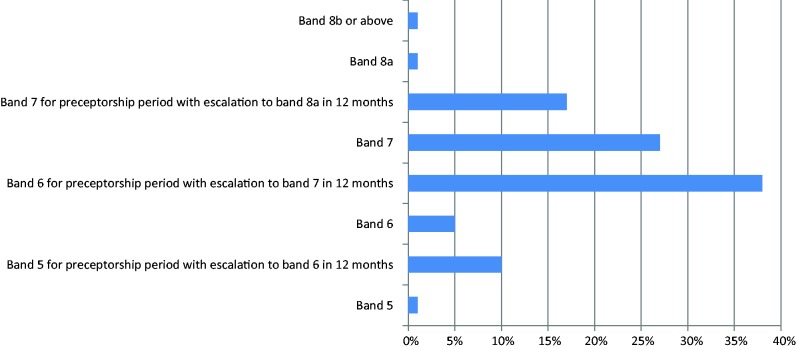
Of 1450 questionnaires sent, 286 responses were received (19.7% response rate). Respondents suggested that the main key skill required of a newly qualified sonographer was competency in scanning (Figure 1). Initial pay banding between Band 6, with a preceptorship period before progressing to Band 7 (38%) or Band 7 (27%) were the most commonly suggested pay scales for newly qualified sonographers (Figure 2).
Figure 1.
Key skills required of a newly qualified sonographer? (multiple responses)
Figure 2.
Appropriate pay band for a newly qualified sonographer (single response)
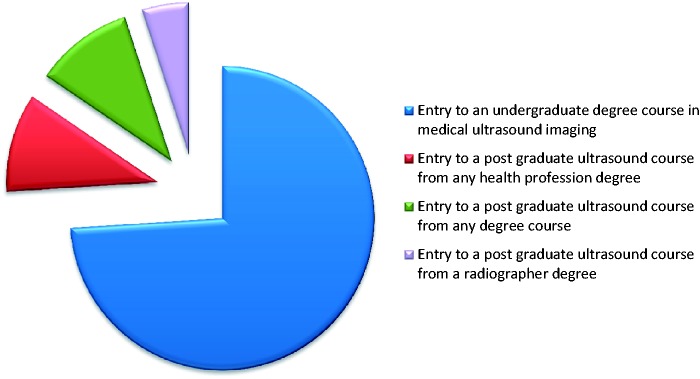
When asked what the term ‘direct entry’ meant to respondents, 74% suggested entry to an undergraduate degree course in medical ultrasound imaging, 10.5% of respondents suggested a postgraduate ultrasound course from any health care profession degree and 10.5% responded that is was a postgraduate ultrasound course from any degree course (Figure 3). Only 5% of respondents suggested entry to a postgraduate ultrasound course from a radiography degree, which is the current method of training many sonographers.
Figure 3.
What does the term ‘direct entry’ mean?
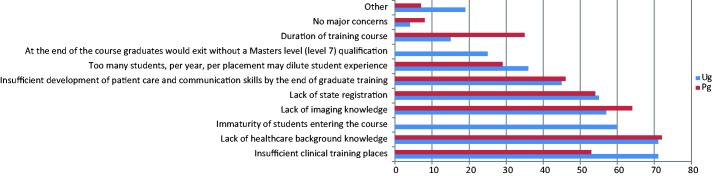
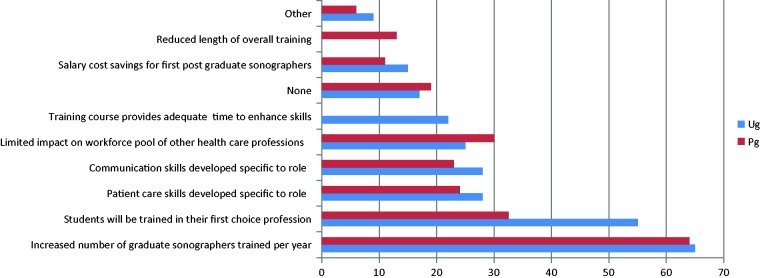
When ranking the responses to major concerns about the two different direct entry routes proposed, insufficient clinical training places and lack of health care background knowledge ranked highest for undergraduate entry (71% each), followed by immaturity of students entering the course (60%), lack of imaging knowledge (57%) and lack of state registration (55%) (Figure 4). The ‘other’ category was selected by 19% of respondents and included comments about a range of issues including limited anatomy, pathophysiology and healthcare knowledge and/or life skills (n = 17), including one statement: Healthcare background knowledge is of immense importance in medical ultrasound. There is no substitute for this prerequisite. All areas of ultrasound are at specialist level. You can’t just learn how to scan without prior knowledge of the specialist area. Placement concerns were commented on by 7 respondents and issues relating to the level and role of the direct entry qualified sonographer were raised in 11 survey results. For postgraduate entry, the highest ranking concerns were lack of health care background knowledge (72%), lack of underpinning imaging knowledge (64%) and lack of state registration (54%) (Figure 4). In relation to major benefits of the two options, the highest ranking for Ug were increased number of sonographers trained each year (65%), students will be trained in their first choice profession (55%) and patient care skills and communication skills will be developed specific to the role (28% each) (Figure 5). For Pg, results were similar for the highest ranked response with increased numbers trained each year (65%), then trained in their first choice career (32%) and limited impact on workforce pool of other health care professionals (30%) (Figure 5).
Figure 4.
Major concerns relating to the types of direct entry programme
Figure 5.
Major benefits relating to the types of direct entry programme
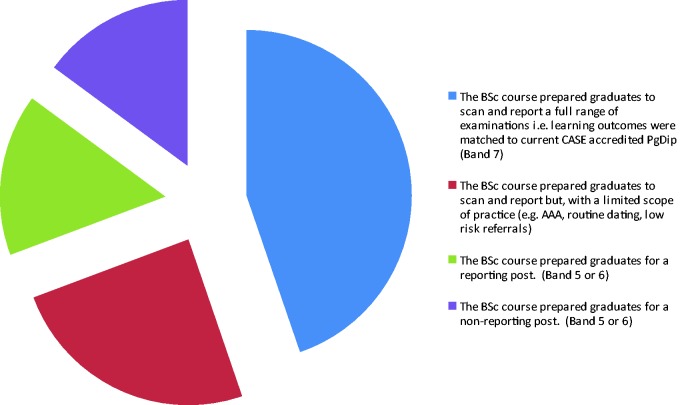
Respondents were also asked whether they would support direct entry undergraduate training in different circumstances, with a yes / no response. The highest positive response (51%) was for graduates to be trained to scan and report a full range of examinations in the same way that current CASE accredited programmes train students. This suggests that 49% of respondents provided a negative response to this question. For other options, the positive (yes) response rates were much lower, with 28% for a BSc course that prepared graduates to scan and report a limited scope of practice, 18% for a course that prepared graduates for a reporting post at Band 5 or 6 and 17% for a BSc course that prepared graduates for a non-reporting post (Figure 6).
Figure 6.
Would you support direct entry undergraduate training if: (multiple responses)
The final question asked respondents for further comments and views on the different models of ultrasound education. There were 146 respondents who made some comment within this section. A few main themes emerged from this qualitative data in addition to data from responses to the open text parts of the previous questions. The main themes were:
Lack of health care background knowledge and/or communication skills (n = 24).
No state registration and regulation (n = 22).
Level and pay banding (n = 19).
Pay and banding issues or suggestions (n = 19).
Quality issues, including the need for safe, competent qualified sonographers, capable of independent report writing and decision making (n = 18) and ensuring quality over cost (n = 10).
Role related issues, including the technically complex nature of the sonographer’s role (n = 8), the possibility of direct entry devaluing or ‘watering down’ the qualification (n = 14) and the potential for a two tier system emerging. Concerns about training for current health care professionals and/or limited CPD opportunities for the current workforce to develop their career (n = 10).
Suggestions for types of direct entry programmes that might meet the education needs of direct entry sonographers (n = 17).
Current issues with capacity (n = 13).
Support for direct entry (n = 15), of which 7 were related to undergraduate direct entry and 6 postgraduate direct entry.
Specific negative comments about direct entry education included 7 for Ug and 3 for Pg. There were also 11 respondents who commented on the bias in question 6, which forced a response to select a form of direct entry. Most of these respondents said that they did not support any of the direct entry options.
Rigorous admissions process required (n = 9).
Resources needed to train direct entry students and the potential burden this might create for departments. Comments included financial resources, staff and available rooms. Suggestions for using simulation prior to placement were also included.
Discussion
Despite the low response rate of 19.7% a wide range of opinions were collated and it is clear that there is little consensus about how future ultrasound education should be delivered. The survey did not aim to specifically determine whether respondents agreed or disagreed with direct entry education, which is a limitation of the study. The results should be interpreted with caution, but do provide an insight into the views of interested professionals. The information gained by this survey is of value to BMUS for informing discussion with stakeholders about direct entry ultrasound education.
The aim of the survey was to gain insight into BMUS members’ understanding of direct entry ultrasound. Whilst 74% of members understood this to be undergraduate education, there are members and HEIs who understand this term to be something different. The term ‘direct entry’ can relate to both Ug and Pg entry to an ultrasound programme from anyone with an unrelated qualification, which might be a college leaver with A-levels for the Ug pathway or someone with a BSc (hons) in an unrelated subject for the Pg pathway. This survey has demonstrated that the term is confusing, as suggested by the SCoR10 and is assumed to mean undergraduate education by many respondents. The SCoR document refers to Ug education when using the term ‘direct entry’ within the document, although Pg direct entry is acknowledged, as this is already an option within the United Kingdom. The terminology used is an issue which professional bodies and HEIs need to be mindful of and clarity of terminology is required in future publications and discussions.
It is evident from the qualitative feedback from the survey that an increase in the capacity of the ultrasound workforce is needed, as suggested by respondents in comments such as ‘we will be at crisis point in the next few years…the demand on services is ever increasing.’ The survey ascertained that there are core skills a newly qualified sonographer should have, regardless of the entry route taken; these included clinical competency, good patient care and communication, decision making and report writing skills. The question relating to core skills asked respondents to rank skills in order or importance, which could have been challenging, as many of the core skills given as possible responses are basic skills required of any health care professional, as shown in the NHS 6Cs.21 This is an NHS England initiative in response to NHS failings and subsequent reports to ensure that care, compassion, competence, communication, courage and commitment underpin all health care professionals’ work.21 These core skills need to be considered and incorporated when developing future education programmes.
Determining the level of pay for newly qualified sonographers needs careful consideration if direct entry programmes are introduced at different levels (Ug and Pg). The questionnaire simply asked about the appropriate pay band for a newly qualified sonographer, without clarification as to whether this relates to the current system or one of the direct entry options. Entry level pay at Band 6 with preceptorship to achieve Band 7 has much support from respondents. The notion of a preceptorship period, following initial qualification would meet current best practice guidelines.22,23 This would also link to the survey of ultrasound professionals’ opinions, in which 92% agreed that a preceptorship period should be available for new ultrasound practitioners.24 Pay banding could be a challenge for employers and managers if a range of entry routes are developed, requiring much discussion to ensure sonographers are fairly rewarded for their skills and not undervalued with limited or no career progression. Interestingly, one respondent’s views were different from the majority that recommended Band 7 or 8a being the preferred final banding after preceptorship (83%) and suggested that paying all sonographers at Band 7 ‘stifles professional progression’ as few Band 7 sonographers have an MSc or the ‘drive to future proof the profession.’ Within the literature there is also evidence to suggest a disparity for some midwife sonographers, who were paid less than radiographer sonographers, which can lead to dissatisfaction and resentment amongst ultrasound practitioners,25 highlighting another important issue to be aware of during future training and employment discussions.
There are significant concerns about the number of training places available for direct entry programmes, with one respondent reporting that ‘most DGHs are not large enough to accommodate multiple students’ and another asked ‘how will students get adequate hands-on time?’ Four respondents suggested simulators could be used to help students develop basic competency prior to starting in the clinical departments. One recommended that ‘we should also be looking at training in the virtual environment to limit the impact on clinical services in the early year(s),’ whilst other comments included forging links with medical education or radiology academies to develop simulation and interprofessional learning. Various methods of simulated learning have been used in health care education26–29 and the use of simulator training within ultrasound education, prior to students entering clinical placements, has been evaluated in different settings.7,30 Simulation has also been suggested as a potential method of ensuring standardised clinical competency assessment, along with other methods of assessing competency.31 The use of simulation may go some way to reducing placement pressure and is a valid consideration when planning any new educational courses.
Concerns about maturity of students for Ug direct entry and lack of background healthcare knowledge for any direct entry programme were also raised within the survey, with comments including ‘I believe the autonomous practice of a sonographer demands a prior knowledge / experience of working in the healthcare environment’ and ‘my opinion is that direct entry sonographers do not have enough background experience to enable them to become confident sonographers.’ However, evidence from the ‘3 + 1’ ultrasound course13,32 would suggest that this concern is perception rather than reality. There is no published data to underpin this at present but local experience suggests that these students have comparable competence and maturity to the more experienced but equally newly qualified sonographers exiting from the traditional routes. The questionnaire did not elicit information about maturity for the Pg direct entry option, as current entry to ultrasound programmes is at Pg level, suggesting a presumption that maturity comes with age, which might be open to further debate outside the scope of this article. Another option suggested by a small number of respondents was a 4-year direct entry programme either with a shortened radiography pathway, with ultrasound added to it or as a 4-year ultrasound direct entry programme, the initial 3 years leading to a BSc (hons) qualification and the final year leading to an MSc qualification. One respondent suggested that the whole imaging education should be reviewed, highlighting that a number of applicants want to specialise in other areas of imaging such as MRI, mammography or nuclear medicine. The respondent recommended a ‘generic imaging BSc’ with core skills taught initially before the second part of the course, providing options for specialising in one imaging field e.g. ultrasound or MRI. Two respondents raised concerns about attrition rates, which may be higher than current ultrasound programmes, as students are less likely to have had experience in the NHS and ‘without experience in imaging, how do you know ultrasound is the modality you would choose?’ A few comments related to the need for rigorous admissions processes, to ensure that students have the required skills and understanding of the role, in addition to the core attributes needed to work in health care.21
The possibility of direct entry programmes, particularly at Ug level devaluing sonographers or ‘watering down’ the qualification or potentially leading to a two tier system were highlighted as concerns by a number of respondents, for example ‘I am strongly opposed to BSc direct entry. I feel it will undermine years of hard work to improve our professional standing.’ A number of comments related to the scope of practice and how this would differ for the types of direct entry programme. One response suggested ‘I would only support this if there was a clear consensus on what the scope of practice of a graduate sonographer would be. At present we are nowhere near defining this.’ Respondents suggested that any training programme needs to ensure safe, competent and qualified sonographers and there is a need for appropriate communication skills, decision making and report writing to be an essential part of the role of anyone undertaking ultrasound examinations. A respondent summed this up by stating: ‘I have concerns that we will have a two tier, poorly regulated profession. Introducing non-reporting sonographers is a backward step. However, if properly regulated and the standards in the profession are maintained it will alleviate the recruitment problem we have in ultrasound.’ Other comments relating to the scope of practice and competency of direct entry sonographers include:
One of my main concerns is the potential for the work already being done by qualified sonographers to become devalued. To expand, if it is deemed acceptable for a graduate from an ultrasound degree to qualify for a Band 5 or 6 role without a route for progression to Band 7 to work covering the level of work and scope that qualified sonographers already practice, this may open the flood gates to re-band sonography at a lower level.
I don't see what the role of a Band 5/6 would be, unless it is in a limited scope of practice. If that was the case, would that leave the Band 7 having to undertake advanced communication and be supervising a number of Band 5/6 practitioners?
Ultrasound is a highly technical and specialised imaging modality with highly qualified and experienced staff. The qualifications should not be watered down to suit demands and produce less capable sonographers.
Having direct entry ‘sonographers’ limited to a non- or limited reporting role would not solve the present staffing problems. These people would be cheap but essentially useless, and employment of this sub-grade of sonographers would increase the burden on fully qualified sonographers.
My concern with an undergraduate course would be the current lack of a clear role and career structure for the graduates. This needs to be clarified by the SCoR and BMUS.
Whilst there is concern about the introduction of direct entry ultrasound programmes, several benefits where identified by respondents. There is an expectation that there may be an increased number of sonographers trained per year, which could help meet the current staffing demands, although clinical placements, as previously discussed, could be a limiting factor on the number of graduates that can be supported annually. Another major benefit of direct entry at Ug or Pg level is that students will be trained in their first choice profession rather than entering via an alternative route, thus reducing the pressures on other healthcare professions such as radiography or midwifery. This has to be balanced by the concerns of respondents about on-going training availability for the current workforce such as radiographers, nurses and midwives wanting to train as sonographers. For the Pg option, the duration of training would be reduced significantly, as demonstrated in the case of the currently proposed programme,17 which would be 2 years full time, rather than the current 3 years full time BSc followed by 1 to 2 years MSc ultrasound training. This could lead to a cost saving for the NHS in training health care professionals to undertake a primary career for which they have no real interest. Other advantages of direct entry are that students would be studying for a longer period of time with both Ug and Pg options, with training specifically focussed to ultrasound, providing tailored patient care and communication skills relevant to their role as a sonographer. One respondent suggested: ‘The shortage of sonographer numbers shows the current system is not working. Training from undergraduate level will address this and allow for full time dedicated education.’ The ultrasound community has to develop and evolve to ensure a workforce that can meet service needs and provide safe, effective patient care. It is clear that staffing levels are suboptimal, with the SCoR survey in 2009 suggesting that a third of qualified sonographers were due for retirement within the next 10 years.4 As one respondent recollected: ‘an undergraduate course is controversial but so was non - radiologists doing ultrasound in the past and look where we are now.’
Interestingly, lack of state registration ranked 5th for Ug and 3rd for Pg direct entry programmes when respondents were asked about major concerns with direct entry ultrasound education, although many comments were included within the free text sections of the questionnaire such as ‘the title sonographer should have the same protection as radiographer which would prevent problems… people practicing as a substandard sonographer.’ Without a change of policy from the current government the issue of registration remains as is; it will not be possible for ‘sonographer’ to be a protected title and as such statutory registration of sonographers will not occur.6 This issue has to be considered primarily by employers. The risk of employing a non-state registered professional will lay with the employing institution. Currently there is variation in practice in the United Kingdom with some employers accepting non-registered sonographers.10 This matter requires discussion between ultrasound managers, sonographers and employers. There is little to be gained in developing direct entry programmes if, after qualification, these sonographers are unable to find employment within their chosen field of practice, although as highlighted by one respondent: ‘there are already a significant number of excellent non HCPC registered sonographers.’
Current discussions about direct entry ultrasound education are similar to those of other professional groups in previous years. There was much debate when midwifery direct entry was first considered.33 However, evidence suggests that midwives stay in the profession longer than their nurse midwife colleagues.33 Stevens33 did, however, suggest that career progression and options to move into alternative areas of practice are limited for midwives, which would apply to direct entry sonographers. In the current survey, some respondents have suggested that musculoskeletal (MSK) injuries should be considered when evaluating direct entry programmes. One respondent suggested that improving workload management by increasing appointment times and reducing pressure on existing staff would reduce the ‘exit of existing staff’ and reduce the chance of musculoskeletal injuries. Another respondent suggested that a direct entry Ug programme could increase the risk of ‘MSK injury due to the length of time in the profession if training is undertaken after leaving school.’ Risk of MSK injuries can be reduced by appropriate working practices, good training and on-going high-quality risk management strategies.34 However, anecdotally, some sonographers have been known to continue to practice radiography to reduce their risk of injury or returned to radiography following a work related musculoskeletal disorder linked to ultrasound practice. This option would not be available to a direct entry qualified sonographer.
Overall, this survey has been a useful exercise for BMUS and the ultrasound community. It has obtained opinions from members that will assist in ensuring informed decisions and choices are made in the future of ultrasound education.
Limitations
The respondents were self-selecting, which can lead to those with strong positive or negative opinions responding. In relation to the number of questionnaires sent, the response rate was low; however, useful data was collected from the 286 respondents. The time constraints meant that a pilot study was not undertaken. Had a pilot study been carried out, some questions could have been amended to provide additional options, such as question 6, which forced respondents into accepting one option before they could complete the survey, leading to bias in the responses. Some participants commented that they did not support any of the four options available. It is recognised that the survey questions and terminology lacked clarity at times, in particular using the term AHP, which is an allied health professional, when in fact a health care provider would have been a more relevant term. However, this has not detracted from the value of this piece of work in continuing the debate about the important issues of education, registration and career progression. Further work could include focus group discussions to explore some of the issues raised within this survey further.
Question 7, reviewing concerns relating to Pg direct entry training, had slightly different wording compared with the same question for Ug direct entry programmes. Immaturity of students entering the course was not listed for postgraduate direct entry students, which may lead to some inconsistency and bias in responses. In a similar way, questions 5 and 8 refer to training time in different and potentially leading ways. Asking about undergraduate training, question 5 lists: ‘training course provides adequate time to enhance skills,’ while for postgraduate training, question 8 lists ‘possible reduced length of overall training period for each sonographer.’ The post graduate question is unclear as to whether the reduced overall training period relates to the current post graduate training of health care professionals such as radiographers, nurses, midwives, the training of health care professionals, which includes their original professional training, or in relation to undergraduate direct entry programmes.
Conclusion
The survey, we understand, is the first to elicit the opinions of the ultrasound community about developments in ultrasound education, particularly relating to direct entry ultrasound programmes. It is clear that many respondents think of ‘direct entry’ as an undergraduate BSc (hons) programme, whereas direct entry can also be at postgraduate level for those with an unrelated first degree. The main concerns of respondents to direct entry ultrasound training are insufficient training places, lack of health care background and knowledge, immaturity (Ug), lack of Master’s level qualification (Ug), short duration of training (Pg), insufficient patient care and communication skills and too many students per year for each placement, diluting the student experience. The possibility of direct entry programmes devaluing sonographers or leading to a two tier system were raised as concerns and the potential risk to the reputation of sonographers if direct entry qualified sonographers do not have the full range of competencies, decision making and report writing skills. Benefits of direct entry education include increasing the workforce of sonographers, students training in their first choice career, reducing the impact on other health care professions, and developing patient care and communication skills specific to the role.
In addition to the concerns and benefits already discussed, other issues raised within the questionnaire need consideration by stakeholders involved in discussions about the development of ultrasound education and workforce planning. These include salary scales, state registration and protection of the public, as ultrasound is not a state registered profession, and on-going training and development options for current ultrasound practitioners and other health care professionals who want to become sonographers. There is a need for further debate within the ultrasound profession as to whether there is a role for a Band 5 or 6 practitioner sonographer and if so, what that role would be and how career development can be planned.
It is clear that much negotiation and discussion is required by all key stakeholders involved with providing both ultrasound services and training. BMUS is working with other professional bodies, the LETBs and the Health Education England Executive to develop a standard and qualifications framework for recruitment of sonographers. This working party is to undertake an option appraisal for establishing a formal entry training programme and for supporting a career framework. The ultrasound profession needs to engage with this matter and open dialogue with local education providers and employers if any progress is to be made. The issue of sonographer shortage is not diminishing and is likely to worsen in the immediate future. However, with support and engagement from all involved with delivering ultrasound services and education, as well as with those who fund training, a viable solution to increasing the workforce will be found. What is apparent is that there is no ‘quick fix.’ Models of education and training need to be found that meet the needs of the local health economy whilst at the same time not jeopardising employment potential of the future sonographic workforce.
declarations
Competing interests: PCP is the BMUS Professional Development Officer.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: BMUS Council and the Chair of CASE approved the questionnaire and study design.
Guarantor: PCP
Contributorship: PCP conceived the study and did the data analysis as part of a membership survey for BMUS. PCP drafted the survey questions, researched the literature, wrote the first and second draft of the manuscript and approved the final version of the manuscript. GH revised the second draft, analysed the results and approved the final draft of the manuscript.
acknowledgements
The authors would like to extend their sincere thanks to all respondents who took part in this survey. The authors would like to thank BMUS Council members and H Venables (Derby University) and S Richards (Teeside University), who are BMUS representatives on CASE committee, for their input into the survey design. The BMUS office distributed the questionnaire and collated the results.
References
- 1.Migration Advisory Committee. Skilled Shortage Sensible: Full Review of the Recommended Shortage Occupation Lists for the UK and Scotland, a Sunset Clause and the Creative Occupations. 2013. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/257241/mac-report.pdf. (last checked 14 April 2015).
- 2.Stewart L, Tidmarsh J, Bagdadi N. West Midlands Ultrasound Workforce Summary Report 2013–2018. Health Education West Midlands, 2014. See http://wm.hee.nhs.uk/files/2014/01/Enc.-9-Sonography-Workforce-Shortages.pdf (last checked 29 July 2015).
- 3.Allen A. Securing the future of the sonography workforce in the East Midlands 2013/14. In: Proceedings of the British Medical Ultrasound Society 46th Annual Scientific Meeting, 9–11 December 2014, The Point, Emirates Old Trafford, Manchester, UK. Ultrasound 2015;23:NP5.
- 4.Society of Radiographers. Developing and Growing the Sonographer Workforce: Education and Training Needs. SCoR, 2009. See http://www.sor.org/learning/document-library/developing-and-growing-sonographer-workforce-education-and-training-needs (last checked 28 November 2014).
- 5.British Medical Ultrasound Society. Extending the Provision of Ultrasound Services in the UK. BMUS, 2003. See http://www.bmus.org/policies-guides/pg-protocol01.asp (last checked 28 November 2014).
- 6.Society and College of Radiographers. Ultrasound Training, Employment and Registration. SCoR, 2014. See https://www.sor.org/learning/document-library/ultrasound-training-employment-registration-and-professional-indemnity-insurance-0 (last checked 9 August 2015).
- 7.Williams C, Edie J, Mulloy B, et al. Transvaginal ultrasound simulation and its effect on trainee confidence levels: a replacement for initial clinical training? Ultrasound 2013; 21: 50–6. [Google Scholar]
- 8.Beardmore C. Team Working in Clinical Imaging. Society and College of Radiographers, 2012. See http://www.sor.org/learning/document-library/team-working-clinical-imaging (last checked 29 July 2015).
- 9.Centre for Workforce Intelligence. Workforce Risks and Opportunities. Diagnostic Radiographers. Education Commissioning Risks Summary from 2012. 2012. See www.cfwi.org.uk/publications/diagnostic…risks…/attachment.pdf (last checked 29 July 2015).
- 10.Society of Radiographers. Direct Entry Undergraduate Ultrasound Programmes (with Competency to Practise): A Briefing from the Society and College of Radiographers. 2013. See https://www.sor.org/learning/document-library/direct-entry-undergraduate-ultrasound-programmes-competency-practise-briefing-society-and-college (last checked 28 November 2014.
- 11.Aitken V, Kilborn J. 1989 guidelines for completion of the college of radiographers' D.M.U. logbook. Radiogr Today 1989; 55: 17–20. [PubMed] [Google Scholar]
- 12.Thompson N. The scope of practice in medical ultrasound. Society of Radiographers, 2009. See www.sor.org/printpdf/book/export/html/6034 (last checked 29 July 2015).
- 13.Wilson R, Parker P. Radiography specialities ultrasound training pilot scheme – the clinical training department experience. In: Abstract from The British Medical Ultrasound Society 45th Annual Scientific Meeting, 9–11 December 2013, The Sage, Gateshead, UK.
- 14.NHS England. NHS Imaging and Radiodiagnostic Activity in England 2012/13. 2013. See http://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2013/04/KH12-release-2012-13.pdf (last checked 30 July 2015).
- 15.Department of Health: Improving Emergency Care in England. London, TSO, 2005. See http://www.publications.parliament.uk/pa/cm200405/cmselect/cmpubacc/445/445.pdf (last checked 24 May 2015).
- 16.The Consortium for the Accreditation of Sonographic Education. So Which Courses are Accredited? CASE, 2015. See http://www.case-uk.org/ (last checked 30 July 2015).
- 17.University of Cumbria. Direct Entry Accelerated Route: Medical Ultrasound, 2015. See http://www.cumbria.ac.uk/Courses/Subjects/HealthAndSocialCare/Postgraduate/MedicalUltrasoundMScDirectEntry.aspx (last checked 30 July 2015).
- 18.Lee R, Paterson A. Sonographers and registration to practice. Ultrasound 2004; 12: 64–7. [Google Scholar]
- 19.Society and College of Radiographers. Register of Sonographers. SCoR, 2015. See www.sor.org/practice/ultrasound/register-sonographers (last checked 4 August 2015).
- 20.British Medical Ultrasound Society. Membership of BMUS. 2008. See http://www.bmus.org/about-bmus/join.asp (last checked 4 August 2015).
- 21.NHS England. Compassion in Practice: One Year On. 2013. See http://www.england.nhs.uk/wp-content/uploads/2013/11/comp-pract-1yr-on.pdf (last checked 8 August 2015).
- 22.Department of Health. Preceptorship Framework. DoH, 2010. See https://www.rcn.org.uk/__data/assets/pdf_file/0010/307756/Preceptorship_framework.pdf (last checked 8 May 2015).
- 23.The Royal College of Radiologists, The Society and College of Radiographers. Standards for the Provision of an Ultrasound Service. London: RCR, 2014.
- 24.Harrison G. Ultrasound clinical progress monitoring: who, where and how? Ultrasound 2015. Published online before print 17 August 2015. DOI: 10.1177/1742271X15600006. [DOI] [PMC free article] [PubMed]
- 25.Edwards H. Midwife Sonographer Activity in the UK. London: The Royal College of Midwives, 2009. See https://www.rcm.org.uk/learning-and-career/learning-and-research/ebm-articles/midwife-sonographer-activity-in-the-uk (last checked 8 August 2015).
- 26.Berg K, Mealey K, Weber D, et al. Are medical students being taught invasive skills using simulation? Simul Healthc 2013; 8: 72–7. [DOI] [PubMed] [Google Scholar]
- 27.Roberts F, Addison B, Goodhand K, et al. The experience, perceptions and attitudes of healthcare students undertaking an inter-professional ward simulation. A pilot study. In: QAA 10th International Enhancement Themes Conference, June 2013, Glasgow, UK. See http://www.enhancementthemes.ac.uk/docs/paper/the-experience-perceptions-and-attitudes-of-healthcare-students-underaking-ward-simulation.pdf?sfvrsn=6 (last checked 8 August 2015).
- 28.Borneuf AM, Haigh C. The who and where of clinical skills teaching: a review from the UK perspective. Nurse Educ Today 2010; 30: 197–201. [DOI] [PubMed] [Google Scholar]
- 29.Persoon M, Schout B, Martens E, et al. A simulator for teaching transrectal ultrasound procedures: How useful and realistic is it? Simul Healthc 2010; 5: 311–4. [DOI] [PubMed] [Google Scholar]
- 30.Gibbs V. An investigation into sonography student experiences of simulation teaching and learning in the acquisition of clinical skills. Ultrasound 2014; 22: 173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harrison G. Summative clinical competency assessment: a survey of ultrasound practitioners' views. Ultrasound 2015; 23: 11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilson J. Workforce planning. Training: solutions to a sustainable workforce. In: Abstract from The British Medical Ultrasound Society 45th Annual Scientific Meeting, 9–11 December 2013, The Sage, Gateshead, UK.
- 33.Stevens S. Direct Entry Now Means No Exit from the Midwifery Profession. 2010. See http://www.nursingtimes.net/home/specialisms/continence/direct-entry-now-means-no-exit-from-the-midwifery-profession/5015601.article (last checked 8 August 2015). [PubMed]
- 34.Harrison G, Harris A. Work related musculoskeletal disorders in ultrasound: can you reduce your risk? Ultrasound 2015. Published online before print 30 June 2015. DOI: 10.1177/1742271X15593575. [DOI] [PMC free article] [PubMed]