Abstract
Acute flank and abdominal pain are common presenting complaints in the emergency department. With increasing access to point-of-care ultrasound (PoCUS), emergency physicians have an added tool to help identify renal problems as a cause of a patient’s pain. PoCUS for hydronephrosis has a sensitivity of 72–83.3% and a varying specificity, similar to radiology-performed ultrasonography. In addition to assessment for hydronephrosis, PoCUS can help emergency physicians to exclude other serious causes of flank and abdominal pain such as the presence of an abdominal aortic aneurysm, or free fluid in the intraperitoneal space, which could represent hemorrhage. Use of PoCUS for the assessment of flank pain has resulted in more rapid diagnosis, decreased use of computed tomography, and shorter emergency department length of stay.
Keywords: Point of care ultrasound, renal, ureteric, abdominal pain
Introduction
The utility of point of care ultrasound (PoCUS) for risk stratification and for streamlining the evaluation of abdominal trauma, suspected aortic aneurysm and first trimester pregnancy complications, among other abdominal–pelvic problems, has been well established.1–3 In this paper, we discuss another easily acquired PoCUS skill: the evaluation of the renal system in patients with flank and abdominal pain.
Emergency physicians frequently encounter the chief complaint of abdominal and flank pain. In these cases, a renal source of the pain is part of the differential diagnosis and, in patients with nontraumatic flank pain and hematuria, the provisional diagnosis is often renal (ureteric) colic.
Rosen et al. first described the use of emergency department PoCUS for flank pain in 1997.4 Hydronephrosis as a surrogate finding for obstructive urolithiasis was one of the earliest “Core Applications” of emergency PoCUS.5 Despite the technological limitations of the portable ultrasound (US) machine at that time, Rosen’s group was able to reliably detect hydronephrosis at the bedside. PoCUS was shown to have a positive predictive value (PPV) of 85% and this made a case for its routine use in renal colic imaging protocols. The advantages of PoCUS noted in this work included shortening the time to imaging, more rapid patient disposition, and limiting patient exposure to dangerous radiation. More recently, physicians have recognized the potential increased risk of malignancy with multiple computed tomography (CT) scans and practice has returned to a more selective use of CT.6 Renewed interest in US as an alternative diagnostic pathway for renal colic has followed this trend.
The sensitivity of emergency department PoCUS for hydronephrosis has been found to be 72–89%, with a varying specificity from 73% in Rosen’s early study to as high as 98%.4,5,7 These results vary based on patient habitus and operator experience.4,5,7,8 False positives for ureterolithiasis include other causes of hydronephrosis such as pregnancy, ureteral strictures, reflux from a full bladder, peritoneal masses, and obstructive clot. Nonhydronephrosis false positives include: the presence of an extra renal pelvis, peri-pelvic cysts, renal cortex cysts, and other masses. Emergency Medicine (EM) PoCUS false negatives are regularly seen with smaller caliber stones and dehydration.9–11
Other limitations of renal PoCUS include a poor negative predictive value (NPV) for urolithiasis without hydronephrosis.4 As a diagnostic test, PoCUS is limited when compared with CT, as it is less able to detect alternative disease processes.4,7 Despite these problems, renal PoCUS is beneficial to the emergency physician, facilitating risk stratification of patients with renal colic.
Bedside imaging
Renal PoCUS is best performed with a 3–5 MHz curvilinear or “abdominal” probe. Like the focused assessment sonography in trauma examination, which is routine for most clinicians, the hepatic and splenic acoustic windows are utilized to visualize the kidney and proximal ureter. Traditional renal US includes longitudinal and transverse images (Figures 1 and 2).
Figure 1.
Longitudinal view of the kidney
Figure 2.
Transverse view of the kidney
We suggest that the unaffected kidney should be scanned first. The kidney lengths should be measured, with the normal range being from 7 to 14 cm in adults and 4–10 cm in pediatrics.12–14 Image generation will often be optimized by posterior placement of the probe, as well as using an oblique turn to the probe, to bring the kidney into the monitor’s footprint and to avoid rib artifact. Patients with challenging anatomy can be scanned in the lateral decubitus or prone position.
Hydration is necessary to successfully complete this study. Many authors suggest a 500–1000 ml fluid bolus to increase the detection of hydronephrosis in the adult renal colic patient.4,7,12,15 To avoid overhydration of the elderly, congestive heart failure and renal insufficiency patients, it may be prudent to image the inferior vena cava (IVC) to first assess their fluid status. If the IVC demonstrates less than 50% collapse with inspiration (sniff) or an absolute diameter of 2.5 cm, then there is sufficient intravascular volume.16 The IVC can be conveniently assessed in conjunction with the abdominal aorta, a necessary part of initial emergency department PoCUS assessment in the patient with flank pain. Patients older than 50, and with known risks or history of vasculopathy, should have their abdominal aorta imaged for aneurysm (>3 cm) and those at risk of rupture (>5 cm).
In renal PoCUS, the goal is to detect hydronephrosis, which is a dilation of the area from the renal calices/pyramids to the renal pelvis and ureter. This will be seen as a hypoechoic (black) area inside the renal cortex.11,17 If hydronephrosis is present, and especially if it is bilateral, the bladder should be visualized for distension. Concurrent with this examination, a brief scan using color flow Doppler to document bilateral ureteral jets can be performed. Absent or decreased periodicity of ureteral jets, usually unilateral, can suggest ureteric obstruction.15 Standard radiology protocol requires a prolonged >5 min study facilitated by color Doppler settings.15,17,18 Although not technically challenging, this time commitment may make it less attractive to most emergency physicians (Figure 3). Furthermore, ureteral jet parameters have not been demonstrated to be helpful in staging the size of renal stone or need for surgical intervention.15 After bladder scanning, a postvoid renal PoCUS study should then be repeated to see if the previously documented hydronephrosis persists.
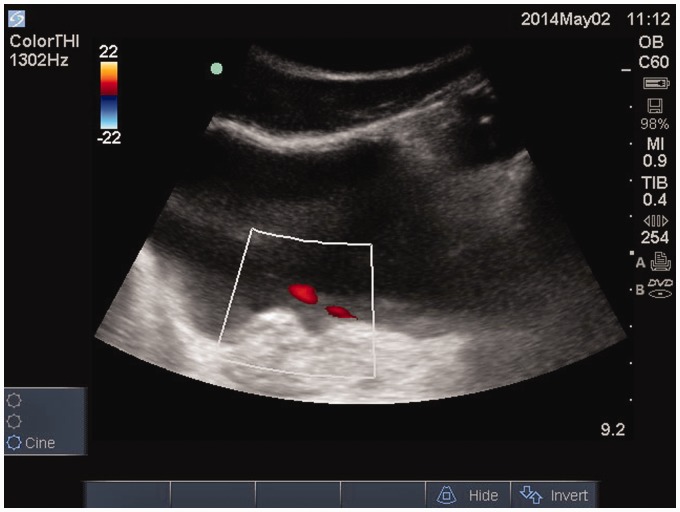
Figure 3.
Transverse bladder with color Doppler showing the left ureteral jet
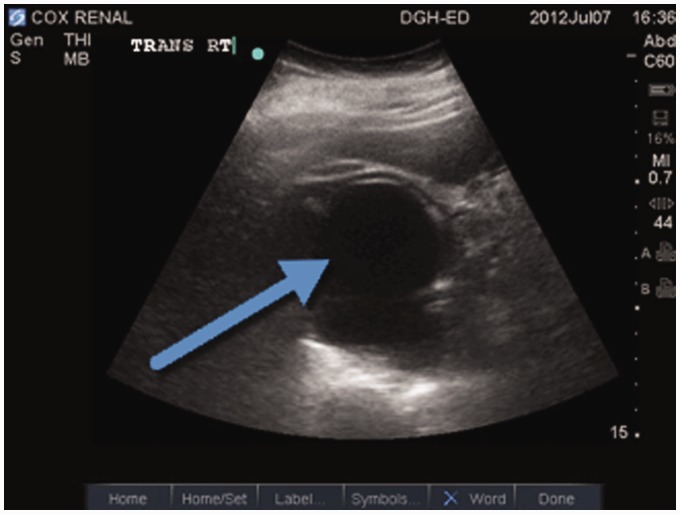
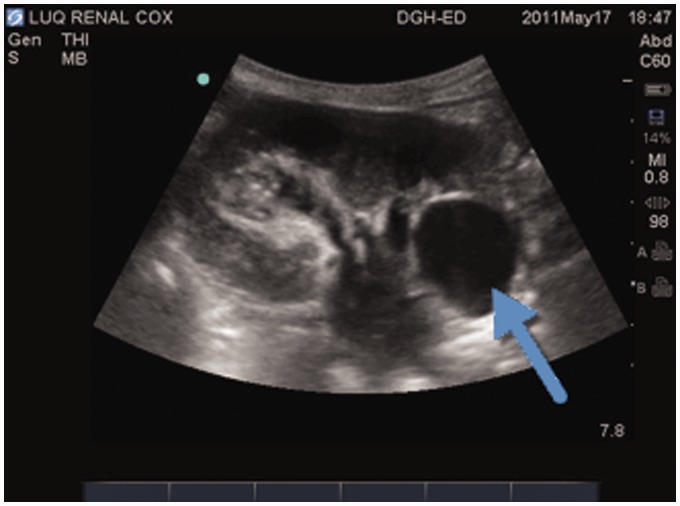
Hydronephrosis is graded as mild, moderate, or severe based on the extent of fluid creating echo free dilation of the collecting system (Figures 4 to 7).11,17 Although these categories are standardly described, the degree of hydronephrosis does not reliably predict the need for urologic intervention.9,10,12 In a retrospective chart review of PoCUS in patients with renal colic, Goertz et al., questioned if the degree of hydronephrosis could predict ureteric stone size. They found that hydronephrosis was not directly proportional to the size of the obstructing stone. However, they concluded that patients with no or mild hydronephrosis were less likely (73%) to have a stone >5 mm.9 Moak et al. in a convenience sample of emergency department (ED) patients noted that any degree of hydronephrosis had 90% sensitivity in detecting ureteral stones >5 mm. Smaller stones create less hydronephrosis and result in a lower sensitivity.10 In a retrospective study of CT confirmed ureteric colic patients, the presence of unilateral renal obstruction did not predict the failure of medical management or the need for operative intervention (Atkinson, unpublished data). As renal PoCUS cannot reliably predict the size of a stone, its value is in confirming clinical suspicion of renal colic as the etiology of the pain syndrome, rather than predicting the need for urological intervention. The clinician can then choose a protocol for risk stratification and possible outpatient management.
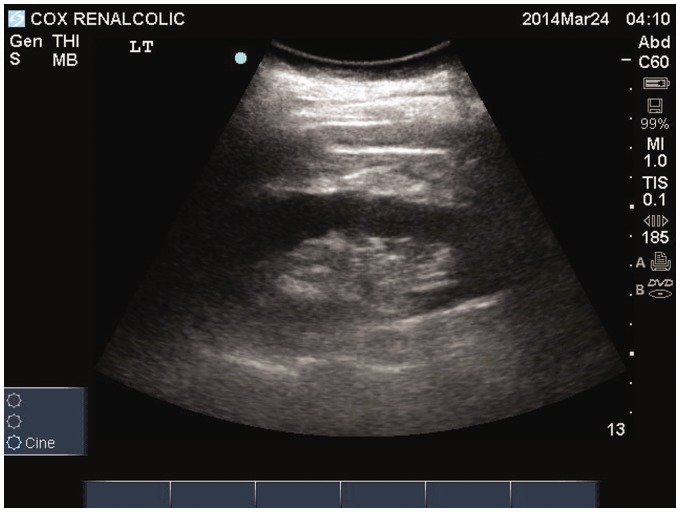
Figure 4.
Normal kidney
Figure 5.
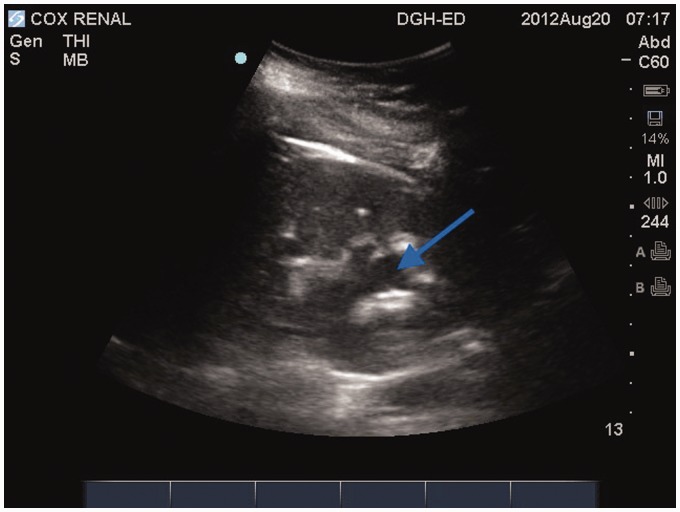
Mild hydronephrosis
Figure 6.
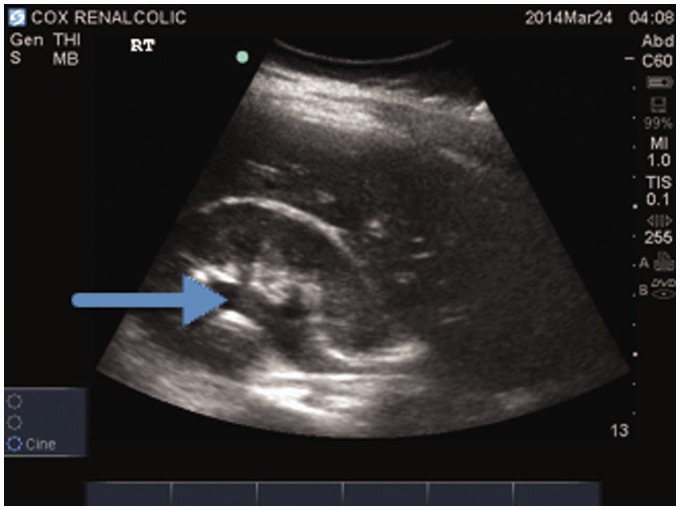
Moderate hydronephrosis
Figure 7.
Severe hydronephrosis
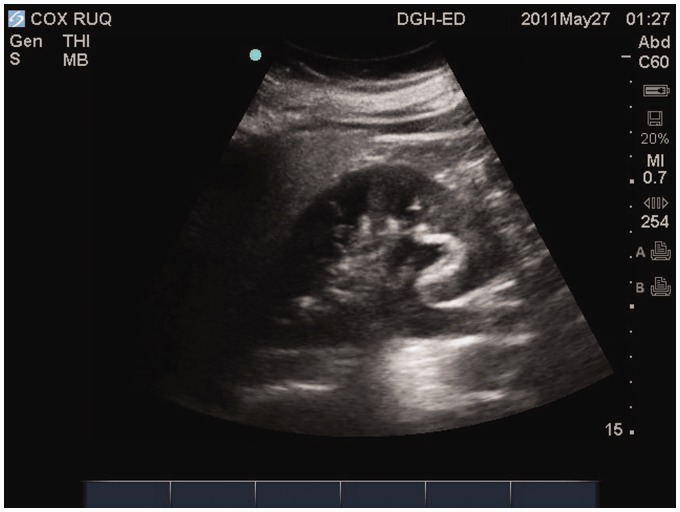
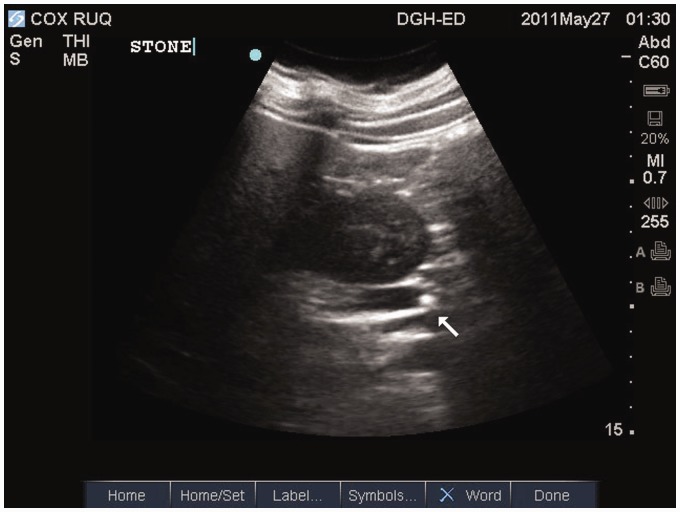
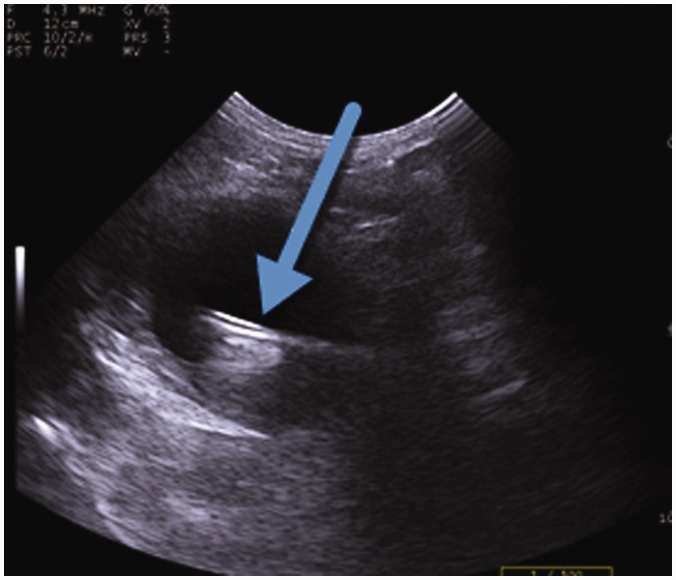
Often, calculi can be visualized within the renal collecting system with PoCUS. They will be recognized by their hyper-echoic (white) appearance, with an associated acoustic shadow artifact. Advanced techniques use color Doppler to find posterior comet tails in the area of the shadow of smaller stones. This “twinkle” artifact can differentiate intrarenal stones that are smaller in caliber from the surrounding renal or ureter tissue.19,20
The PoCUS practitioner should learn to recognize structures that are actually false positives: peri-pelvic cysts, cortical cysts, and the extrarenal pelvis. Peri-pelvic (Figure 8) and cortical cysts may be misinterpreted as hydronephrosis. Hydronephrosis is differentiated by visualization of the communication of the hypoechoic area in the renal pyramids into the utereropelvic junction (UPJ) (Figures 5 and 6).11,21 If there is a dilated UPJ but no dilation of the renal pyramids, an extrarenal pelvis may be present. This anatomical normal variant is another false positive and a recognized pitfall with renal US assessment. In hydronephrosis, the pelvis is often significantly dilated, facilitating visualization of the proximal ureter (Figures 9 and 10). The ureter can be differentiated from the renal vein and artery by using color Doppler.
Figure 8.
Simple cyst in the peri-pelvic location does not communicate with renal pelvis
Figure 9.
Mild hydronephrosis with hydroureter
Figure 10.
Same ureter with retained proximal stone
Other PoCUS findings in renal colic can include fluid in Gerota’s fascia, which correlates with perinephric stranding on noncontrast CT and may indicate extravasation of urine from a ruptured fornix.22
Bladder imaging
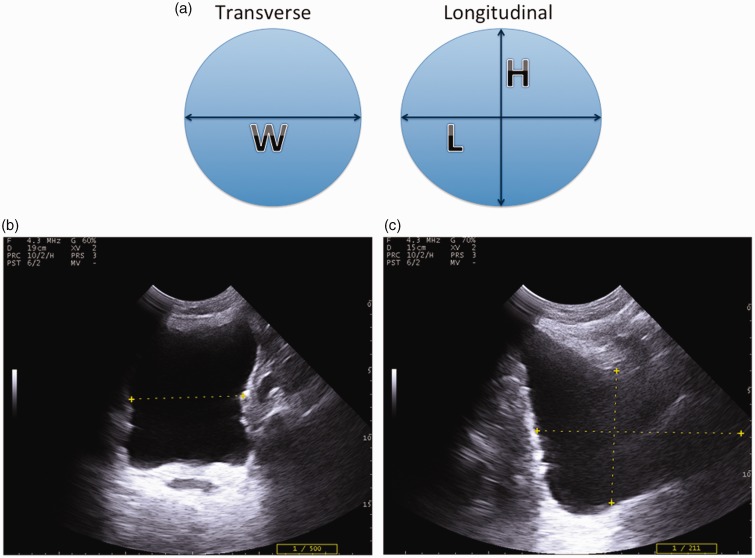
Urinary retention is in the differential diagnosis for patients with abdominal pain at or below the umbilicus. The bladder is easily imaged and measured in the transverse plane (right–left), and sagittal long axis in both directions. Dicuio et al. have published the formula: , to more accurately determine bladder volume using US measurements (Figure 11).18,23–25 Urinary retention is present if postvoid bladder volume is greater than 150 ml.23,24 Alternatives to bladder PoCUS are commercial bladder scanners. However, these machines may not be readily available and more concerning, without direct bladder visualization, may leave operators wondering if they are measuring the correct structure in the pelvis. PoCUS allows direct visualization of the bladder confirming that the proper target is being assessed.
Figure 11.
Bladder dimensions for volume calculation (a. Schematic; b. Transverse; c. Sagittal; W: width; L: length; H: height).
Another useful application of PoCUS is in confirming urinary catheter placement and assessment for migration of the retention balloon into the prostatic urethra. The symmetric, saline-infused balloon makes it easy to visualize on PoCUS images, even in the nondistended bladder. When emergency suprapubic bladder catheter placement is required, PoCUS facilitates needle placement for the introduction of a Seldinger wire. Direct visualization of the needle path assists the physician in avoiding surface vessels (e.g., the superficial epigastric arteries), bowel adhesions, and hernias at the abdominal wall. Thus, PoCUS guidance limits iatrogenic morbidities such as bleeding and intestinal perforation.26
Imaging iatrogenic variants
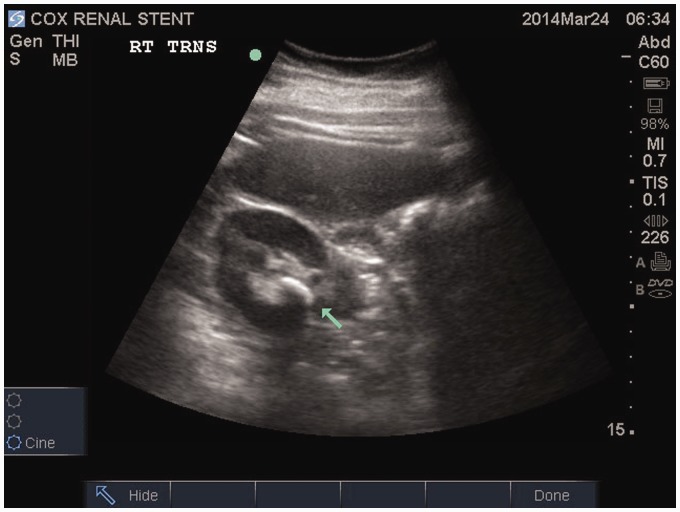
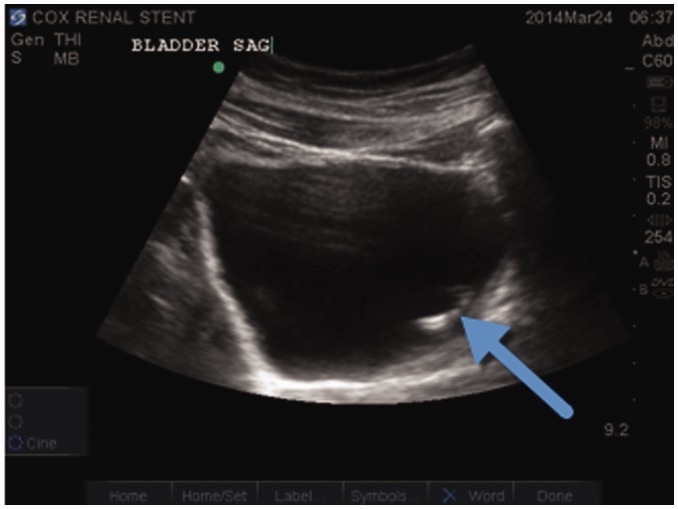
Patients with renal colic undergoing urologic intervention occasionally present to the ED with pain syndromes. In these cases, it is important to assess for migration or obstruction of a previously deployed ureteral stent. Kidney, ureter, bladder (KUB) X-ray can be used to locate the stent. However, renal PoCUS offers an advantage: assessment for hydronephrosis suggestive of stent obstruction. The hyper-echoic pigtail ends of the stent within the kidney and bladder can be imaged confirming proper location (Figures 12 and 13). Similarly, on the rare occasion of a broken indwelling catheter or of patient self-instrumentation with a foreign body, PoCUS can assist in determining its location (Figures 14 and 15).
Figure 12.
Stent in renal collecting system with no hydronephrosis
Figure 13.
Stent visualized in left side of bladder
Figure 14.
KUB with a radio-opaque foreign body in the pelvis of a male patient who believed a foreign body was inserted into his rectum during a period of inebriation
Figure 15.
Bladder EM PoCUS of the patient from Figure 14 showing a hyperechoic structure on the right side of the hypoechoic bladder with ring down artifact. This image provided clinical information contradicting the patient’s history resulting in the timely consultation of the urologic service
Imaging renal variants
Another challenge to the emergency physician is recognizing and categorizing renal variants. Characterization of benign vs. malignant cysts and masses is beyond the scope of most clinicians using renal PoCUS. However, one study utilized a urology resident with basic US training to evaluate emergency patients with flank pain.27 PoCUS was able to detect clinically relevant problems such as abdominal aortic aneurysm, kidney masses, and ureteral obstruction in patients with infection. The study cited a PPV of 85.1% and NPV 89.7% as compared to specialist performed imaging. The early clinical information from PoCUS positively influenced management, shortening the time to intervention by avoiding the usual imaging delay.27
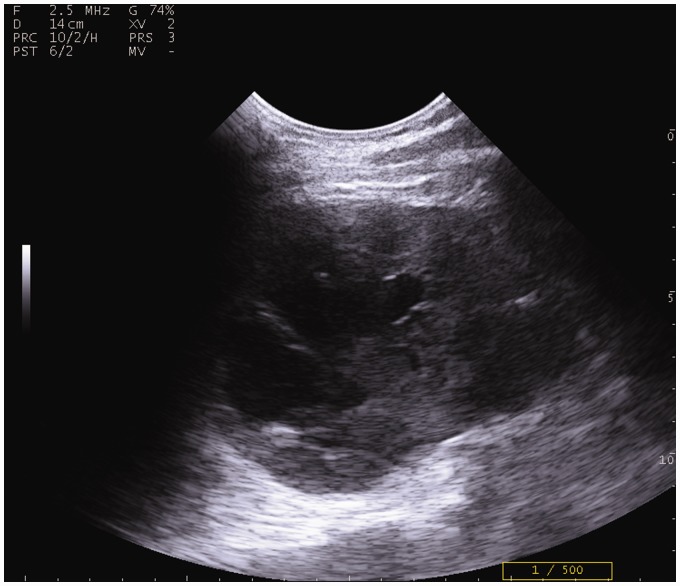
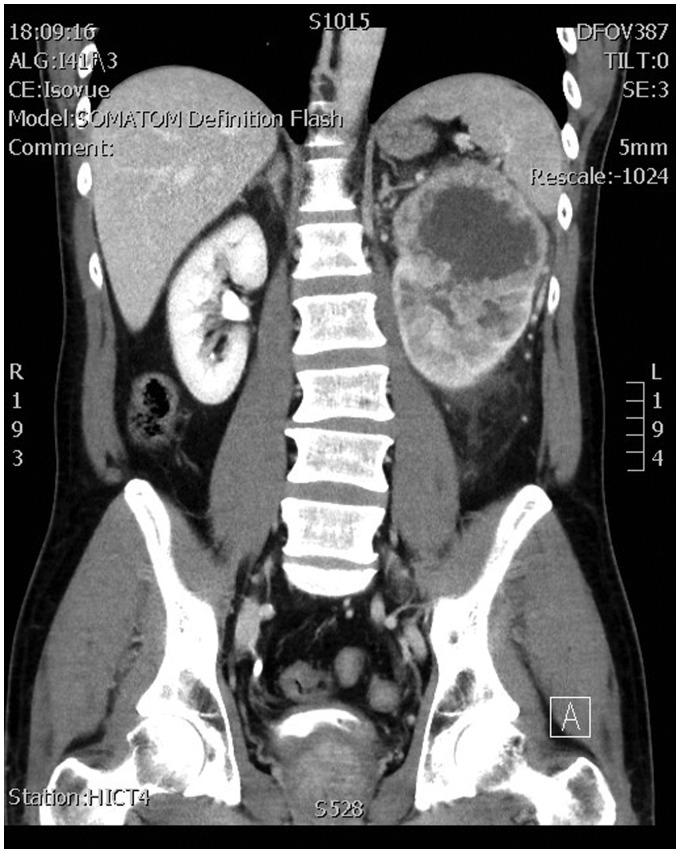
Occasionally, malignancies will be encountered during a routine PoCUS examination. Early recognition of abnormal features can increase survivability of renal cancers.28 Figure 16 shows a patient’s renal lesion that was easily visualized by PoCUS. Note that it is very similar in appearance to the corresponding coronal CT image (Figure 17). The hypoechoic features at the superior pole do not communicate with the pelvis and were correctly identified as cystic and not representative of hydronephrosis.
Figure 16.
Cystic features with septation in the superior pole
Figure 17.
CT coronal cut from same patient with hematuria and left flank pain
Basic guidelines are suggested by the Bosniak staging system for cystic abnormalities. Lesions are considered high risk for malignancy if more than three septations are present or the septations have a thickness greater than 1 mm.21,29,30 The prudent physician, encountering renal variants, should document the PoCUS findings and obtain a diagnostic imaging study in a clinically appropriate time frame.
Coding and billing
The American College of Emergency Physicians (ACEP) has recognized PoCUS and validated its worth to the medical system by issuing coding guidelines and a billing template online.31 Urinary tract EM PoCUS is considered a “Core Application” and has been assigned Current Procedural Code (CPT) 76775-26 for “limited retroperitoneal US” and can include the concurrently performed abdominal aorta exam. A separate CPT 51798-26 has also been assigned for a limited bladder study for urinary retention. As familiarity with emergency department renal PoCUS grows, these CPT codes and ACEP advocacy will improve recognition of this skillset, culminating in reimbursement for PoCUS clinical time and expertise.
Renal colic PoCUS algorithm
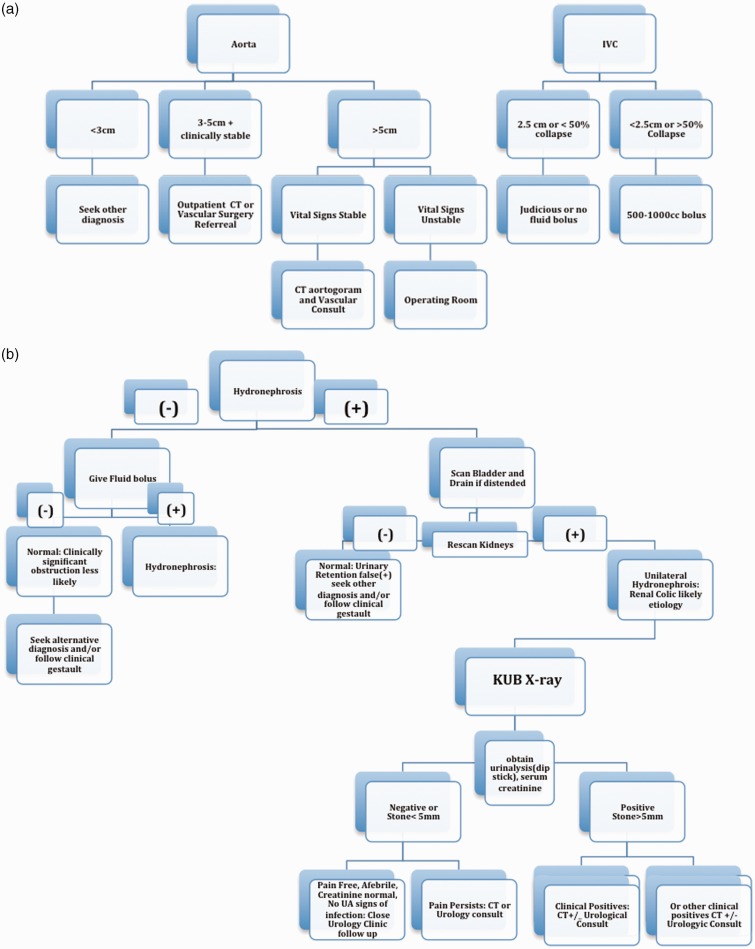
The following protocols for EM assessment of renal colic have been proposed for risk stratification and outpatient management.
Henderson et al. in 1998, using a protocol similar to Dalla Palma et al., found that PoCUS in combination with KUB X-ray had a sensitivity of 97.1%, PPV 80.7%, and NPV 92%.12,32 US was compared to intravenous pyelography, which was the preferred imaging modality at that time.12 The accuracy of the PoCUS images and readings were verified by the Diagnostic Imaging Department. In the initial 20% of the studies selected for qualitative review, 100% concordance between the two interpretations was reported.12
Catalano compared helical CT vs. plain radiography and US in sequential renal colic patients.33 Although CT was more sensitive, they found that all patients requiring interventions were detected with the KUB X-ray and US protocol. Gaspari (2005) noted that haem-positive urinalysis, along with concurrent hydronephrosis on PoCUS was 88% sensitive and 85% specific for a ureteral stone seen on a sequential CT scan.7 Kartal et al. in 2006 prospectively validated a renal colic workup including PoCUS and urinalysis.8 They used the Swadron and Mandavia protocol as adapted in the Noble renal US review.19 Kartal et al. was able to risk stratify emergency patients with unilateral flank pain and safely discharge greater than 50% to outpatient urology follow-up.8 In 2010, Edmonds et al. performed a retrospective review of their emergency department’s Renal Colic protocol. This clinical pathway included diagnostic imaging department US to risk stratify flank pain patients. In their study, when US “missed” ureterolithiasis, only 0.6% (2/352) of patients, required a urologic procedure.34
In centers supported by outpatient urology clinics working collaboratively with the emergency department, the use of one of these renal PoCUS protocols can provide more expedient care safely, while limiting the cost and radiation exposure of CT.
The clinical utility of emergency department renal PoCUS for the risk stratification of patients with renal colic has been recently supported in a large multicenter study published in the New England Journal of Medicine.35 The authors compared clinical management using renal protocol CT, radiology department US, and emergency medicine PoCUS. They found that patients receiving only US benefited from lower radiation exposure. It was further demonstated that there were no significant differences in adverse events between the three groups studied. They noted no difference in patient pain scores, complications, return visits to the emergency department, or diagnostic accuracy. However, secondary imaging with CT was more likely with PoCUS 40%, and radiology department US 27% resulting in only a marginal difference in medical costs across groups. This study further validates renal PoCUS as a reasonable approach to the risk stratification of renal colic patients, and supports its use in patients with recurrent renal colic to avoid repeat CT scanning.
Our emergency department PoCUS Flank Pain Clinical Pathway (Figure 18) summarizes the ideas represented by the previous authors.4,7,8,10,12,19,32–34
Figure 18.
Emergency Department Point of Care Algorithm for suspected renal colic. (a) Step 1; (b) Step 2.
Conclusion
Emergency department PoCUS for the assessment of patients with abdominal and flank pain is a skill easily acquired by clinicians with basic US competency. The literature suggests that using PoCUS as part of a protocol for risk stratification of renal colic patients is safe and expedient. Other causes of flank and abdominal pain such as abdominal aortic aneurysm, urinary retention, bladder foreign bodies, and renal lesions can be diagnosed with bedside US. As PoCUS applications for flank and abdominal pain become more common in emergency medicine protocols, PoCUS assessment of the renal tract may become the new standard of care.
DECLARATIONS
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Not applicable
Guarantor: CC
Contributorship: CC researched the literature, wrote the first draft, created and edited the images and figures. PA, RH, and SM reviewed and edited all versions of the manuscript.
References
- 1.Rubano E, Mehta N, Caputo W, et al. Systemic review: emergency department bedside ultrasonography for diagnosing suspected abdominal aortic aneurysm. Acad Emerg Med 2013; 20: 128–38. [DOI] [PubMed] [Google Scholar]
- 2.Meiniker L, Leibner E, McKenney MG, et al. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med 2006; 48: 227–35. [DOI] [PubMed] [Google Scholar]
- 3.McRae A, Murray H, Edmonds M. Diagnostic accuracy and clinical utility of emergency department targeted ultrasonography in the evaluation of first-trimester pelvic pain and bleeding: a systematic review. Canad J Emerg Med 2009; 11: 355–64. [DOI] [PubMed] [Google Scholar]
- 4.Rosen CL, Brown DF, Sagarin MJ, et al. Ultrasonography by emergency physicians in patients with suspected ureteral colic. J Emerg Med 1998; 16: 865–70. [DOI] [PubMed] [Google Scholar]
- 5.Mandavia D, Aragona J, Chan L, et al. Ultrasound training for emergency physicians—a prospective study. Acad Emerg Med 2000; 7: 1008–14. [DOI] [PubMed] [Google Scholar]
- 6.Brenner D, Hall EJ. Computed tomograpy—an increasing source of radiation exposure. N Engl J Med 2007; 357: 2277–84. [DOI] [PubMed] [Google Scholar]
- 7.Gaspari R, Horst K. Emergency ultrasound and urinalysis in the evaluation of patients with flank pain. Acad Emerg Med 2005; 12: 1180–84. [DOI] [PubMed] [Google Scholar]
- 8.Kartal M, Eray O, Erdogru T, et al. Prospective validation of a current algorithm including bedside US performed by emergency physicians for patients with acute flank pain suspected for renal colic. Emerg Med J 2006; 23: 341–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goertz J, Lotterman S. Can the degree of hydronephrosis predict kidney stone size? Am J Emerg Med 2010; 28: 813–16. [DOI] [PubMed] [Google Scholar]
- 10.Moak J, Lyons MS, Lindsell CJ. Bedside renal ultrasound in the evaluation of suspected ureterolithiasis. Am J Emerg Med 2012; 30: 218–21. [DOI] [PubMed] [Google Scholar]
- 11.Wah TM. Pelvi-ureteric dilatation. In: Allan PL, Baxter GM, Weston MJ. (eds). Clinical Ultrasound, 3rd ed Edinburgh: Churchill Livingstone Elsevier, 2011, pp. 428–44. [Google Scholar]
- 12.Henderson SO, Hoffner RJ, Aragona JL, et al. Bedside emergency department ultrasonography plus radiography of the kidneys, ureters and bladder vs intravenous pyelography in the evaluation of suspected ureteral colic. Acad Emerg Med 1998; 5: 666–71. [DOI] [PubMed] [Google Scholar]
- 13.Allan PL. Kidneys: anatomy and technique. In: Allan PL, Baxter GM, Weston MJ. (eds). Clinical Ultrasound, 3rd ed Edinburgh: Churchill Livingstone Elsevier, 2011, pp. 413–27. [Google Scholar]
- 14.Rosenbaum DM, Korngold E, Teele RL. Sonographic assessment of renal length in normal children. Am J Roentgenol 1984; 142: 467–69. [DOI] [PubMed] [Google Scholar]
- 15.Jandaghi A, Falahatkar S, Alizadeh A, et al. Assessment of ureterovesical jet dynamics in obstructed ureter by urinary stone with color Doppler and duplex Doppler examinations. Urolithiasis 2013; 41: 159–63. [DOI] [PubMed] [Google Scholar]
- 16.Haydar S, Moore ET, Higgins GL, et al. Effect of bedside ultrasonography on the certainty of physician clinical decision making for septic patients in the emergency department. Ann Emerg Med 2012; 60: 346–58. [DOI] [PubMed] [Google Scholar]
- 17.Ellenbogen PH, Scheible FW, Talner LB, et al. Sensitivity of gray scale ultrasound in detection of urinary tract obstruction. Am J Roentgenol 1978; 130: 731–33. [DOI] [PubMed] [Google Scholar]
- 18.Richenberg JL. Ultrasound of the bladder. In: Allan PL, Baxter GM, Weston MJ. (eds). Clinical Ultrasound, 3rd ed Edinburgh: Churchill Livingstone Elsevier, 2011, pp. 550–71. [Google Scholar]
- 19.Noble VE, Brown DF. Renal ultrasound. Emerg Med Clin North Am 2004; 22: 641–59. [DOI] [PubMed] [Google Scholar]
- 20.Tchelepi H. Color comet-tail artifact: clinical applications. Am J Roentgenol 2009; 192: 11–18. [DOI] [PubMed] [Google Scholar]
- 21.Weston MJ. Renal cystic disorders. In: Allan PL, Baxter GM, Weston MJ. (eds). Clinical Ultrasound, 3rd ed Edinburgh: Churchill Livingstone Elsevier, 2011, pp. 486–504. [Google Scholar]
- 22.Daignault M, Turandot S, Lewiss RE. Right flank pain: a case report of an interesting sonographic finding. J Emerg Med 2012; 43: 1059–62. [DOI] [PubMed] [Google Scholar]
- 23.Dicuio M, Creti S, Di Campoli A, et al. Usefulness of a prevoiding transabdominal sonographic bladder scan for uroflowmetry in patients involved in clinical studies of benign prostatic hyperplasia. J Ultrasound Med 2003; 22: 773–76. [DOI] [PubMed] [Google Scholar]
- 24.Dicuio M, Pomara G, Menchini-Fabris F, et al. Measurements of urinary bladder volume: comparison of five ultrasound calculation methods in volunteers. Arch Ital Urol Androl 2005; 77: 60–62. [PubMed] [Google Scholar]
- 25.Kahn S. Bladder Volume. 2013. See http://www.em.emory.edu/ultrasound/ImageWeek/Abdominal/bladder_volume.html (last checked 5 May 2014).
- 26.Jacob P, Prasad-Rai B, Todd AW. Suprapubic catheter insertion using an ultrasound-guided technique and literature review. Brit J Urol Int 2012; 110: 779–84. [DOI] [PubMed] [Google Scholar]
- 27.Surange R, Jeygopal NS, Chowdhury SD, et al. Bedside ultrasound: a useful tool for the on call urologist? Int Urol Nephrol 2001; 32: 591–96. [DOI] [PubMed] [Google Scholar]
- 28.Mandavia D, Pregerson B, Henderson SO. Ultrasonography of flank pain in the emergency department: renal cell carcinoma as a diagnostic concern. J Emerg Med 2000; 18: 83–86. [DOI] [PubMed] [Google Scholar]
- 29.Bosniak MA. The Bosniak renal cyst classification: 25 years later. Radiology 2012; 262: 781–85. [DOI] [PubMed] [Google Scholar]
- 30.Bosniak MA. The use of the Bosniak classification system for renal cysts and cystic tumors. J Urol 1997; 157: 1852–53. [PubMed] [Google Scholar]
- 31.Resnick J, Hoffenberg S, Tayal V, et al. Ultrasound Coding and Reimbursement Document. 2009. Emergency Ultrasound Section. American College of Emergency Physicians. See http://emergencyultrasoundteaching.com/assets/2009_coding_update.pdf (last checked 14 June 2015).
- 32.Dalla Palma L, Stacul F, Bazzocchi M, et al. Ultrasonography and plain film versus intravenous urography in ureteric colic. Clin Radiol 1993; 47: 333–333. [DOI] [PubMed] [Google Scholar]
- 33.Catalano O, Nunziata A, Altei F, et al. Suspected ureteral colic: primary helical CT versus selective helical CT after unenhanced radiography and sonography. Am J Radiol 2002; 178: 379–87. [DOI] [PubMed] [Google Scholar]
- 34.Edmonds ML, Yan JW, Sedran RJ, et al. The utility of renal ultrasonography in the diagnosis of renal colic in emergency department patients. Can J Emerg Med 2010; 12: 201–206. [DOI] [PubMed] [Google Scholar]
- 35.Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasound versus CT for suspected nephrolithiasis. New Eng J Med 2014; 371: 1100–10. [DOI] [PubMed] [Google Scholar]