Abstract
This study examined the quality of family relationships and its associations with the severity of unmet needs of individuals admitted to a tertiary psychiatric hospital in South Africa. The quality of family relations and perceived unmet needs were assessed using the Lehman Quality of Life Interview and Camberwell Assessment of Needs, respectively. The results show that higher total unmet needs were associated with lower quality of family relations. The main areas of serious unmet needs included accessing government benefits and information, and establishing social relations. The results have implications for hospital-based social workers beyond managing psychiatric symptoms in South Africa.
Keywords: Family relation, need assessment, severe mental illness, social work, South Africa
Introduction
Managing severe mental illness (SMI) is a daunting lifelong responsibility that affects not only those living with SMI, but also their families. A review of the literature indicates that caregiver burden and stress can be very serious problems, and that families are often confronted with inadequate support from mental health professionals (Saunders, 2003). Support for individuals with SMI is particularly challenging in resource-poor sub-Saharan African nations, including in South Africa, due to a lack of availability and/or access to community-based mental health services (Burns, 2011). This is exacerbated in South Africa by a legacy of apartheid policies (1948—1994), which negatively impacted on family cohesion and structure in the country. Within that context, the viability of mining and farming industries in South Africa was dependent on a single-person wage migrant labor system; and the intent behind the enforcing of certain policies (including the Group Areas Act, Native Labour Regulation Act and Native Urban Areas Act) was to promote separation of Black family members (Abdullah, 2013; Sachs, 1990). Despite decades of research from high-income countries investigating relationships between family members and individuals living with SMI, there are few studies that are generalizable to, and take into account, the unique historical and social circumstances of South Africa.
This study examined the quality of relationships between individuals living with SMI and their relatives, specifically with respect to the severity of unmet needs for those affected by SMI in South Africa. Individuals living with SMI with greater unmet needs would appear to require greater/longer family involvement; however, a lack of sufficient family support could also contribute to greater unmet needs. Based on a family caregiver stress perspective (Sales, 2003), diminished family capacity to provide support for the unmet needs of people with SMI can be attributed to various burdens, including physical, emotional/psychological, financial, and social demands (Awad & Voruganti, 2008); and, despite a desire to assist, to a deterioration in the quality of relationships. Likewise, weakened family relations can reduce sources of support which may in turn result in higher unmet needs, reflecting possible negative co-occurring relationship between increased severity of unmet needs and lower quality of family relations.
Methods
Study design and participants
The study, based on a cross-sectional design, was carried out at a referral-based tertiary psychiatric government hospital in KwaZulu-Natal Province between July 2012 and October 2013. Hospital clinicians, who are not part of the research team, referred potential participants to our research personnel to be screened for study eligibility. All consecutive inpatients meeting the following inclusion criteria were approached to enter the study: age 21 years and older; speaking isiZulu or English; and diagnosed with SMI (schizophrenia, schizoaffective disorder, bipolar disorder, and psychosis not otherwise specified). Individuals unable to provide informed consent or with a developmental disability were excluded from the study. A trained research assistant fluent in isiZulu (and English) provided individuals meeting these criteria with a description of the study and written informed consent was obtained. The response rate for the needs assessment study from the total eligible sample was 92.0%. The University of KwaZulu-Natal Biomedical Research Ethics Committee and Columbia University Institutional Review Board approved the study.
Measures
The Camberwell Assessment of Needs (CAN) was administered to identify perceived unmet needs (Phelan et al., 1995) and assist in the design for community-based services. Originally designed to assess the perceived needs of patients with SMI, the CAN has been used in a number of African settings, including South Africa (Flisher, Sorsdahl, & Joska, 2012; Joska & Flisher, 2007), Ethiopia (Fekadu et al., 2014) and Somalia (McCrone et al., 2005). The trained interviewer asked study participants if needs existed in each of 22 domains: (1) accommodation; (2) food; (3) looking after the home; (4) self-care; (5) daytime activities; (6) physical health; (7) psychotic symptoms; (8) information on condition and treatment; (9) psychological distress; (10) safety to self; (11) safety to others; (12) alcohol; (13) drugs; (14) company; (15) intimate relationships; (16) sexual expression; (17) childcare; (18) basic education; (19) telephone; (20) transport; (21) money; and (22) benefits. As the CAN is also designed to elicit views on unmet patient needs from different perspectives, we interviewed attending hospital clinical staff (doctors and nurses) to obtain their views on the needs of their patients in each of the 22 domains. In the event of clinical staff reporting unmet needs in particular domain/s, we then obtained their perspectives on (1) the severity of these needs, (2) the extent of support received and needed from “informal” and “formal” sources, and (3) the adequacy of and satisfaction with support received to address these needs.
In our study, “informal” sources consisted of family, relatives, and friends. “Formal” sources included local community services, which generally comprised local health and social services and faith-based organizations. Responses relating to the severity of perceived needs were based on a 3-point Likert scale (0 = no serious need, 1 = met or partially met, and 2 = serious unmet needs). The extent of perceived support received from “informal” and “formal” sources and the perceived need for support from “formal” services were also each rated on a 3-point Likert scale (0 = no support, 1 = moderate support, and 2 = high support). Lastly, the perceived adequacy of support (right type of help), as well as overall satisfaction with support received, was rated in dichotomized format (0 = no and 1 = yes).
Two subscales from the Lehman Quality of Life Interview (LQoLI) were used to assess the quality of family relations. LQoLI is an instrument frequently used to assess quality of life in individuals with SMI (Cramer et al., 2000; Lehman, 1988; Lehman, Possidente, & Hawker, 1986; Lehman, Postrado, & Rachuba, 1993). The two subscales were for objective and subjective quality of family relations. The objective subscale measure (two items) quantified family communication by frequency of telephone contact and meeting in person. Objective subscale responses are based on a 5-point Likert scale (1 = not at all, 2 = less than once a month, 3 = at least once a month, 4 = at least once a week, and 5 = at least once a day). The subjective subscale measure (four items) assessed the respondent’s feeling about (a) family in general, (b) frequency of family contact, (c) the way the study participant and family act towards each other, and (d) the general quality of family relations. Subjective subscale responses are based on a 7-point Likert scale (1 = terrible, 4 = equally satisfied/dissatisfied, and 7 = delighted). Ratings of objective and subjective quality of family relations were based on the average of the two and four items respectively. The 4-item subjective quality of family relations scale had acceptable internal reliability (Cronbach α = .87). The 2-item objective quality of family relations scale had low internal reliability (Cronbach α = .39). Given the limitations of measuring reliability for a 2-item scale, this Cronbach α coefficient may be an underestimate of reliability (Eisinga, Grotenhuis, & Pelzer, 2013). At interview, information was also collected on sociodemographics (gender, age, race/ethnicity, marital status, residence type), psychiatric diagnosis, and past psychiatric hospital admissions.
Data analysis
Following an examination of the demographic/clinical characteristics of the study participants, the analysis consisted of three components. The first component focused on needs and support. The frequency of perceived unmet needs (no serious needs, met or partially met with no or moderate problems due to help received, and serious unmet needs) reported by patients and hospital clinical staff was tabulated to identify the highest rated domains across the 22 domains of life. Cohen’s Kappa coefficient was computed to assess the extent of inter-rater agreement between patients and clinical staff regarding severity of perceived unmet needs (rated as either no serious needs, met or partially met, or serious unmet needs). A Kappa coefficient of “less than 0” indicates “poor agreement,” “0–0.20” indicates “slight agreement,” “0.21–0.40” indicates “fair agreement,” “0.41–0.60” indicates “moderate agreement,”, “0.61–0.80” indicates “substantial agreement,” and “0.81–1” indicates “almost perfect [excellent] agreement” (Landis & Koch, 1977).
Thereafter, the data on support was analyzed. Both the mean number of domains in which support to study participants from “informal” and “formal” sources was received, and that in which support was needed by “formal” sources, was calculated. The Student t-test was used to detect significant mean differences for all analyses. The proportion of study participants who reported receiving both adequate and satisfactory support, given the severity of their unmet needs, was calculated. The second component of the analysis focused on the quality of family relations. The frequency of response from all six LQoLI family relations items were tabulated; and objective (mean of two items) and subjective (mean of four items) ratings were computed.
Finally we examined the association between total unmet needs and quality of family relations. Total unmet needs were represented by the number of domains (with possible range: 0–22) that were identified by clients as being of moderate or severe severity. Unadjusted and adjusted regression models were utilized to determine the association between both objective and subjective quality of family relations and total unmet needs. Poisson models were used owing to positive skewedness of the dependent variables in the models. The adjusted models controlled for gender, age, psychiatric disorder diagnosis, educational attainment, race/ethnicity, marital status, urban/rural residency, and past history of psychiatric hospital admission within the last 12 months.
Results
Demographic and clinical characteristics
Fifty-seven clients participated in the needs assessment interview (Table 1), the majority of whom were black South Africans (n = 47; 82.5%), and aged 21–29 (n = 24; 42.1%). Approximately half were diagnosed with schizophrenia (n = 26; 45.6%), had hospitalization related to mental health within the past year (n = 29; 50.9%), had attained grade 12 equivalent or higher level of education (n = 31; 54.4%), and resided in rural areas (n = 29; 50.9%).
Table 1.
Demographic and clinical characteristics of needs assessment study respondents (n = 57).
| n | % | |
|---|---|---|
| Gender | ||
| Male | 38 | 66.7 |
| Female | 19 | 33.3 |
| Age category | ||
| 21–29 | 24 | 42.1 |
| 30–39 | 19 | 33.3 |
| 40+ | 14 | 24.6 |
| Education | ||
| <Grade 12 equivalent | 31 | 54.4 |
| ≥ Grade 12 equivalent | 26 | 45.6 |
| Race/ethnicity | ||
| Black | 47 | 82.5 |
| Non-Black | 10 | 17.5 |
| Marital status‡ | ||
| Married/stable partner | 19 | 33.9 |
| Casual partner | 17 | 30.4 |
| No relationship/partner | 20 | 35.7 |
| Residence | ||
| Urban | 28 | 49.1 |
| Rural | 29 | 50.9 |
| Hospitalization related to mental health ≤ 1 year [any hospital] | ||
| Yes | 29 | 50.9 |
| Psychiatric diagnosis | ||
| Schizophrenia | 26 | 45.6 |
| Schizoaffective | 11 | 19.3 |
| Bipolar | 12 | 21.1 |
| Psychosis NOS and other | 8 | 14.0 |
One missing response
Unmet needs across 22 domains of life
The magnitude of unmet needs across the 22 domains of life rated by clients and psychiatric hospital staff are described in Table 2. The average number of unmet needs was two, while clients rated most frequently the following domains as “serious unmet needs”: benefits (15.4%), company/social relations (14.3%), and information (9.3%). They rated most frequently as “partially unmet needs” the following domains: psychotic symptoms (19.6%), psychological distress (16.1%), and intimate relationship (8.9%). The analysis of staff rating indicated that they rated most frequently the following domains as “serious unmet needs”: daily activities, psychotic symptoms and harm to others (10.0% for each). They rated most frequently as “partially unmet needs” the following domains: psychotic symptoms (45.0%), psychological distress (25.0%), and drugs/alcohol (20.0%). Excluding needs associated with drug misuse (κ = 0.35), the inter-rater analysis indicated that Cohen’s kappa coefficients were less than 0.2 in all domains, reflecting no or only slight agreement between clients and staff regarding the unmet needs of individuals with SMI.
Table 2.
Assessment of level of need for 22 items in CAN.
| Client rating
|
Staff rating
|
Client rating
|
Staff rating
|
Client rating
|
Staff rating
|
Client rating
|
Staff rating
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Domain
|
No serious need
|
No serious need
|
Met or partially met need
|
Met or partially met need
|
Serious unmet needs
|
Serious unmet needs
|
Not known
|
Not known
|
||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Accommodation | 54 | 94.7 | 18 | 94.7 | 2 | 3.5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.8 | 1 | 5.3 |
| Food | 54 | 94.7 | 18 | 90.0 | 1 | 5.3 | 1 | 5.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 5.0 |
| Looking after the home | 54 | 94.7 | 15 | 75.0 | 2 | 3.5 | 4 | 20.0 | 1 | 1.8 | 0 | 0.0 | 0 | 0.0 | 1 | 5.0 |
| Self-care | 51 | 96.2 | 17 | 85.0 | 1 | 1.9 | 1 | 5.0 | 0 | 0.0 | 1 | 5.0 | 1 | 1.9 | 1 | 5.0 |
| Daily activities | 51 | 91.1 | 15 | 75.0 | 0 | 0.0 | 2 | 10.0 | 4 | 7.1 | 2 | 10.0 | 1 | 1.8 | 1 | 5.0 |
| Physical health | 49 | 87.5 | 17 | 85.0 | 4 | 7.1 | 3 | 15.0 | 2 | 3.6 | 0 | 0.0 | 1 | 1.8 | 0 | 0.0 |
| Psychotic symptoms | 42 | 75.0 | 9 | 45.0 | 11 | 19.6 | 9 | 45.0 | 2 | 3.6 | 2 | 10.0 | 1 | 1.8 | 0 | 0.0 |
| Information | 45 | 83.3 | 17 | 85.0 | 3 | 5.6 | 1 | 5.0 | 5 | 9.3 | 0 | 0.0 | 1 | 1.9 | 2 | 10.0 |
| Psychological distress | 44 | 78.6 | 14 | 70.0 | 9 | 16.1 | 5 | 25.0 | 2 | 3.6 | 0 | 0.0 | 1 | 1.8 | 1 | 5.0 |
| Self-harm | 50 | 89.3 | 17 | 85.0 | 2 | 3.6 | 0 | 0.0 | 3 | 5.4 | 1 | 5.0 | 1 | 1.8 | 2 | 10.0 |
| Safety to others | 48 | 85.7 | 16 | 80.0 | 4 | 7.1 | 2 | 10.0 | 2 | 3.6 | 2 | 10.0 | 2 | 3.6 | 0 | 0.0 |
| Alcohol | 48 | 85.7 | 10 | 50.0 | 0 | 0.0 | 4 | 20.0 | 4 | 7.1 | 1 | 5.0 | 4 | 7.1 | 5 | 25.0 |
| Drugs | 50 | 90.1 | 13 | 65.0 | 2 | 3.6 | 4 | 20.0 | 3 | 5.5 | 1 | 5.0 | 0 | 0.0 | 2 | 10.0 |
| Company | 47 | 83.9 | 17 | 85.0 | 0 | 0.0 | 0 | 0.0 | 8 | 14.3 | 1 | 5.0 | 1 | 1.8 | 2 | 10.0 |
| Intimate relationships | 46 | 82.1 | 14 | 70.0 | 5 | 8.9 | 0 | 0.0 | 2 | 3.6 | 0 | 0.0 | 3 | 5.4 | 6 | 30.0 |
| Sexual expression | 39 | 70.9 | 10 | 50.0 | 1 | 1.8 | 0 | 0.0 | 4 | 7.3 | 1 | 5.0 | 11 | 20.0 | 9 | 45.0 |
| Child care | 47 | 87.0 | 16 | 80.0 | 0 | 0.0 | 0 | 0.0 | 2 | 3.7 | 0 | 0.0 | 5 | 9.3 | 4 | 20.0 |
| Basic education | 53 | 93.4 | 15 | 75.0 | 2 | 3.6 | 1 | 5.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 4 | 20.0 |
| Telephone | 51 | 94.4 | 17 | 85.0 | 0 | 0.0 | 0 | 0.0 | 2 | 3.7 | 0 | 0.0 | 1 | 1.9 | 3 | 15.0 |
| Transport | 55 | 100.0 | 12 | 63.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 7 | 36.8 |
| Money | 47 | 83.9 | 10 | 55.6 | 2 | 3.6 | 1 | 5.6 | 3 | 5.4 | 1 | 5.6 | 4 | 7.1 | 6 | 33.3 |
| Benefits | 27 | 51.9 | 8 | 57.1 | 0 | 0.0 | 0 | 0.0 | 8 | 15.4 | 0 | 0.0 | 17 | 32.7 | 6 | 42.9 |
The total sample size is based on 57 study participants. Staff assessment about the needs of 20 study participants were obtained. There are missing values in certain domains.
Support provided
The mean number of domains for which support (help) was provided from “formal” and “informal” sources was 1.69 (SE = 0.30) and 2.52 (SE = 0.46), respectively, the latter being significantly higher than the former (Mdiff = 0.83, t = 2.35, p = .02). The mean number of domains requiring support from “formal” sources (M = 5.61, SE = 0.91) exceeded that for which support was provided from the same sources (Mdiff = −3.92, t = −4.50, p < .01). Among study participants with unmet needs in any of the 22 domains of life, approximately half (54.1%) reported receiving adequate (the right type of) support, and were satisfied with the amount of support provided. Among those with serious unmet needs in any of the 22 domains of life, over a third (38.1%) reported receiving adequate support, with approximately half (45.4%) being satisfied with the amount of support provided.
Family relations
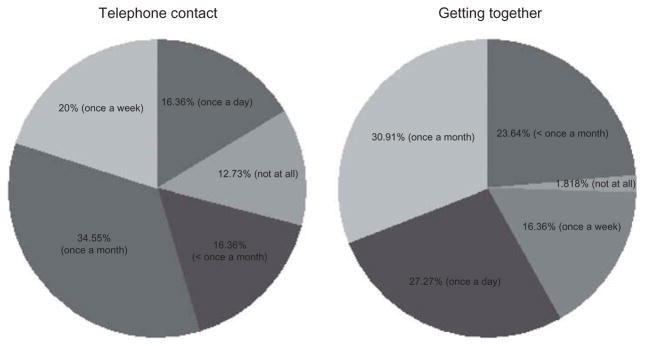
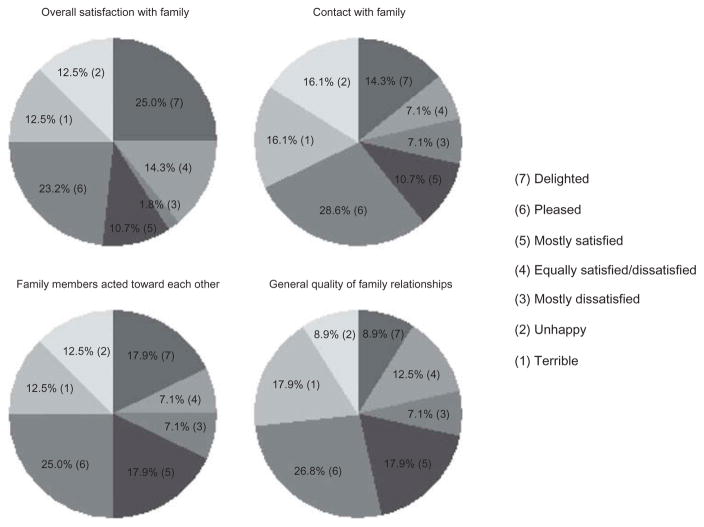
The responses of the two-item objective (frequency of contact) and the four-item subjective (perceived quality of) family relations ratings are presented in Figures 1 and 2, respectively. In terms of the frequency rating, the significant minority of study participants reported little or no contact with family members, while approximately a quarter of participants reported being ‘pleased’ with the quality of family relations. The mean rating for objective and subjective family relations subscales was 3.3 (SE = 0.96) and 4.4 (SE = 1.78) respectively, both of which lie above the middle response values of 3 “once a month” and 4 “Equally satisfied/dissatisfied” on each Likert scale.
Figure 1.
Objective quality of life—family contact.
Figure 2.
Subjective quality of life—satisfaction.
Association between family relations and unmet needs
The results of the bivariate unadjusted Poisson regression models indicated that higher frequency (β= −0.24, z = −2.34, p = 0.02) and perceived quality of family relations (β= −0.15, z = −2.81, p < 0.01) were associated with fewer total unmet needs. The results of the fully adjusted Poisson regression models appear in Table 3. Model 1 indicated that higher frequency (β= −0.32, z = −2.46, p = 0.01) was associated with fewer total unmet needs. It also indicated that higher educational attainment, non-Black ethnicity and residence in a rural area were associated with fewer total unmet needs. Model 2 indicated that a higher perceived quality of family relations (β= −0.15, z = −2.44, p = .02) was associated with fewer total unmet needs. It also indicated that younger age, lower educational attainment, diagnosis (schizophrenia and bipolar disorder), Black ethnicity, and history of psychiatric re-hospitalization (within the last 12 months) were associated with more total unmet needs.
Table 3.
Regression on total unmet needs outcome.
| Model 1
|
Model 2
|
|||||||
|---|---|---|---|---|---|---|---|---|
| b | SE | z | p | b | SE | z | p | |
| Quality of family relation ratings | ||||||||
| Frequency of contact (objective) | −0.32 | 0.13 | −2.46 | 0.01 | ||||
| Perceived interaction (subjective) | −0.15 | 0.06 | −2.44 | 0.02 | ||||
| Gender [Male] | 0.25 | 0.26 | 0.94 | 0.35 | 0.29 | 0.26 | 1.12 | 0.26 |
| Age [30–39] | ||||||||
| 21–29 | 0.62 | 0.33 | 1.90 | 0.06 | 0.57 | 0.29 | 1.99 | <0.05 |
| 40+ | 0.17 | 0.35 | 0.48 | 0.63 | 0.36 | 0.35 | 1.03 | 0.30 |
| Psychiatric disorder [Other] | ||||||||
| Schizophrenia | 1.26 | 0.44 | 2.90 | <0.01 | 1.18 | 0.43 | 2.76 | 0.01 |
| Schizoaffective | 0.52 | 0.48 | 1.07 | 0.28 | 0.54 | 0.48 | 1.14 | 0.25 |
| Bipolar | 1.50 | 0.54 | 2.80 | 0.01 | 1.43 | 0.50 | 2.88 | <0.01 |
| Education [Lower than grade 12] | −0.72 | 0.24 | −3.03 | <0.01 | −0.71 | 0.23 | −3.11 | <0.01 |
| Race/Ethnicity [Non-Black] | 0.98 | 0.37 | 2.68 | 0.01 | 1.12 | 0.38 | 2.95 | <0.01 |
| Marital status [Single] | ||||||||
| Married | 0.30 | 0.35 | 0.87 | 0.38 | 0.11 | 0.34 | 0.33 | 0.74 |
| Stable partner | −0.18 | 0.33 | −0.54 | 0.59 | −0.23 | 0.32 | −0.72 | 0.47 |
| Casual partner | −0.36 | 0.30 | −1.20 | 0.23 | −0.33 | 0.28 | −1.16 | 0.24 |
| Residence [Urban] | −0.84 | 0.27 | −3.12 | <0.01 | −0.49 | 0.26 | −1.92 | 0.06 |
| Past psychiatric hospital admission†[No] | 0.27 | 0.21 | 1.29 | 0.20 | 0.42 | 0.21 | 1.98 | <0.05 |
Coefficients of unadjusted models (for objective and subjective rating above) were (β= −0.24, z = −2.34, p = 0.02) and (β= −0.15, z = −2.81, p < 0.01). Reference category in bracket.
Within the last 12 months.
Discussion
First, our research suggests that poorer quality of family relations (both objective and subjective) was associated with higher total unmet needs. Second, approximately a third of the study participants with serious unmet needs reported receiving appropriate (the right type of) support. Third, the three areas endorsed most frequently by study participants as “serious unmet needs” were: challenges associated with obtaining government benefits; inadequate information about care; and company/social relations. Fourth, the perception of unmet needs differed significantly in almost all domains between study participant and hospital clinical providers. Such finding speaks to the importance of developing collaborative client-centered treatment plans. Lastly, we also learnt that study participants draw more support from “informal” sources (family, relatives, and friends) than from “formal” sources. More than half the participants were at least satisfied with the quality of family relations, with a minority citing inadequate contact with members of their family.
Preventing psychiatric re-hospitalization requires an approach to addressing unmet needs that goes beyond temporary management of psychotic symptoms at tertiary metal health institutions. In addressing unmet needs of individuals with SMI, our results suggest that strategies to improve the provision of support will require close attention to especially vulnerable groups. These include those of Black ethnicity, adolescents, and those with low educational attainment.
Our finding (Mtotal number of needs = 2) [based on an analysis not described in the Methods section] closely resembles that of the most recent South African study (Flisher et al., 2012), which administered the CAN instrument to individuals with SMI (Mtotal number of needs ≈ 3), and reached a similar conclusion that emphasized the importance of addressing psycho-social needs (Joska & Flisher, 2007). More importantly, our study contributes to the limited body of literature on the potential causes and consequences of serious unmet needs, indicating an association with poor quality of family relations in sub-Saharan African. We believe one plausible explanation is that greater unmet needs may necessitate considerable family involvement, leading to cumulative caregiver exhaustion and stress, and straining relations with family members.
In scarce-resource settings, family are likely to be the only source of support in the community for many individuals with SMI following hospital discharge. This highlights the need for family-based services (Dixon et al., 2010; Kreyenbuhl, Buchanan, Dickerson, & Dixon, 2010), which can benefit both patients and family members/caregivers in such settings. With only 0.28 psychiatrists per 100,000 people, according to the World Health Organization-AIMS Report on Mental Health System in South Africa (2007), scarcity of human resources is a major challenge (Note that in comparison there are 11.4 psychiatrists per 100,000 in the United States according to the Dartmouth Atlas of Health Care (2006).) The inadequacy of human resources for mental health services is well-established in South Africa (Burns, 2011) and this places greater responsibility and burden on community-based support systems and families in particular. Importantly, this is not an endorsement that treatment of individuals with SMI be left to family members alone (for many reasons including sustainability, as mentioned in the previous paragraph). On the contrary, culturally competent community-based mental health promotion in South Africa, based on ubuntu (Edwards, Makunga, Ngcobo, & Dhlomo, 2004), requires the provision of meaningful support to families within the community who often lack resources, but who nonetheless shoulder the care of those with mental illness post-institutionalization (Engelbrecht & Kasiram, 2012). Although the definition, interpretation and evolution of the Nguni term ubuntu varies, it is acknowledged as coming from the proverb “Umuntu ngumuntu ngabantu,” roughly translating as “a person is a person through their relationship to others” (Gade, 2011). Reflecting the moral quality of a person or phenomenon (African humanism, a philosophy/ethics, and worldview) of interconnectedness among people (Gade, 2012), ubuntu embraces communalism, solidarity, and human interdependence in small-scale communities (Pieterse, 2004). In this sense, ubuntu provides a strong basis for family-based care that is supported appropriately by public services.
It is important to acknowledge the persistence in South Africa of some cultural (e.g., stigma by family members) and implementation (e.g., lack of trained human resources) barriers that remain significant concerns for the effective implementation of family-based interventions, such as therapy (Asmal et al., 2011) and psychoeducation (Kritzinger, Swartz, Mall, & Asmal, 2011). In collaboration with other sources of “formal” and “informal” support, social work in South Africa is in an important position to help address the unmet needs of psychiatric patients in a way that goes beyond temporary management of psychotic symptoms. Hospital social workers in particular are well placed to be sensitive to the impact of living and family environments, educate patients and families about the importance of adherence to treatment recommendations, and provide linkages to community resources post-psychiatric hospitalization (Beder, 2006). As indicated in our result and consistent with another study (Lasalvia, Ruggeri, Mazzi, & Dall’Agnola, 2000), the perception of unmet needs differed between our study participants and hospital clinical providers. With cultural competency and sensitivity being core ethical principles of their profession (Reamer, 2013), social workers potentially bring unique skills to advocate on behalf of individuals whose critical voice have been silenced (Morley, Ablett, & Macfarlane, 2014). In addition, social workers may enhance and support family strengths, and preserve effective family functioning (Collins, Jordan, & Coleman, 2010). Social work has been a leading social service profession since the 1920s in South Africa (Nicholas, Rautenbach, & Maistry, 2010); and strengthening hospital-based social work capacity is a key strategy to building trust and relationships with patients and their families during the time of hospitalization that can endure well beyond hospital discharge.
A major limitation of our study was the small sample size. In addition, our study was based on a cross-sectional design, and thus a temporal relationship between unmet needs and quality of family relationship could not be established. Consequently we must consider an alternative plausible explanation, namely that poor family relations (possibly in part due to the stress of the illness) lead to weakened family support, which in turn results in unmet needs. In reality it is likely that both mechanisms occur, with a reciprocal relationship between unmet needs and poor family relations. It is not unreasonable to imagine the development of a destructive spiral of ever-worsening family relations and ever-increasing unmet needs.
The existence of such a cycle or model of interdependence between unmet needs and deteriorating family relations should guide a research agenda aimed at developing, testing and implementing interventions aimed at breaking this negative cycle. Such interventions would seek to turn the cycle around, leading to a positive cycle characterised by ever-improving family relations and ever-diminishing unmet needs of patients with SMI. The challenge in low and middle-income countries (LMICs), especially in sub-Saharan Africa, is that there is little evidence currently, and no randomized evidence to our knowledge, supporting sustainable community-based interventions that could directly address the needs of patients with SMI in these contexts.
One strategy is to draw on interventions that have an evidence-base in high-income contexts, such as Assertive Community Treatment (ACT) (Stein & Santos, 1998; Stein & Test, 1980; Test & Stein, 1980), and adapt these in terms of both language and sociocultural context. There are however limitations to adapting interventions such as ACT within LMIC settings. For example, ACT requires a substantial investment of resources and cannot be implemented unless highly trained personnel, including psychiatrists, are readily available. Furthermore, this model does not include systematic links to primary health care, other elements of the broader health and social system, or to families and community stakeholders. While the ACT model is still evolving in the United States (Donahue et al., 2012), it is also now starting to be adapted and tested in South Africa (Botha, Koen, Galal, Jordaan, & Niehaus, 2014). There are several studies outside South Africa currently underway [at the time of this report], evaluating potentially sustainable treatment models for supporting individuals with severe mental illness within the LMIC context. Trials include time-limited Critical Time Intervention-Task Shifting (CTI-TS) in Latin America (da Silva et al., 2013) and Task Sharing for the Care of Severe Mental Disorders in a Low-income Country (TaSCS) in Ethiopia (University of Cape Town, 2015). The previous Critical Time Intervention trials in the United States (Herman et al., 2011; Susser et al., 1997) were delivered by trained social service staff, and therefore social workers will potentially continue to play an important role in the implementation of any evidence-based mental health services within the LMIC context.
While much work remains to be done in this field within under-resourced contexts, we hope that our findings on the complex relationship between patient needs and family relations will inform the development of appropriate and sustainable community-based interventions in South Africa, addressing the unmet needs of individuals with severe mental illness.
Acknowledgments
Funding
Data collection of the study was supported by the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental & Craniofacial Research, National Institute On Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases Health, and NIH Office of Women’s Health and Research through the International Clinical Research Fellows Program at Vanderbilt University (R24 TW007988) and the American Recovery and Reinvestment Act. Andrew Tomita was supported by SA MRC Flagship grant (MRC-RFA-UFSP-01-2013/UKZN HIVEPI) and NIH Research Training Grant (R25TW009337), funded by the Fogarty International Center and the National Institute of Mental Health. Jonathan K Burns and Ezra Susser were supported by a grant from NIMH (R21MH093296). Joy Noel Baumgartner was supported by the NIMH Training Grant (T32MH013043). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH and the South African Medical Research Council.
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/WSHC.
References
- Abdullah S. Multicultural social work and national trauma: Lessons from South Africa. International Social Work. 2013 doi: 10.1177/0020872812461019. [DOI] [Google Scholar]
- Asmal L, Mall S, Kritzinger J, Chiliza B, Emsley R, Swartz L. Family therapy for schizophrenia: Cultural challenges and implementation barriers in the South African context. African Journal of Psychiatry. 2011;14(5):367–371. doi: 10.4314/ajpsy.v14i5.3. [DOI] [PubMed] [Google Scholar]
- Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: A review. Pharmacoeconomics. 2008;26(2):149–162. doi: 10.2165/00019053-200826020-00005. [DOI] [PubMed] [Google Scholar]
- Beder J. Hospital social work: The interface of medicine and caring. New York, NY: Routledge; 2006. [Google Scholar]
- Botha UA, Koen L, Galal U, Jordaan E, Niehaus DJ. The rise of assertive community interventions in South Africa: A randomized control trial assessing the impact of a modified assertive intervention on readmission rates; a three year follow-up. BMC Psychiatry. 2014;14:56. doi: 10.1186/1471-244X-14-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns JK. The mental health gap in South Africa—A human rights issue. Equal Rights Review. 2011;6(99):113. [Google Scholar]
- Collins D, Jordan C, Coleman H. An introduction to family social work. Belmont, CA: Brooks/Cole; 2010. [Google Scholar]
- Cramer JA, Rosenheck R, Xu W, Thomas J, Henderson W, Charney DS. Quality of life in schizophrenia: A comparison of instruments. Schizophrenia Bulletin. 2000;26(3):659–666. doi: 10.1093/oxfordjournals.schbul.a033484. [DOI] [PubMed] [Google Scholar]
- da Silva TFC, Lovisi G, Tavares Cavalcanti M, Dahl C, Conover S, Valencia E, Susser E. Critical time intervention—Task shifting: A new psychosocial intervention for people with severe mental illness in Latin America. Revista Psiquiatria Clínica. 2013;40(6):243. [Google Scholar]
- Dartmouth Atlas for Health Care. Psychiatrists per 100000 residents. Lebanon, NH: Dartmouth Institute for Health Policy and Clinical Practice, Trustees of Dartmouth College; 2006. Retrieved from http://www.dartmouthatlas.org/data/table.aspx?ind=144. [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, … Kreyenbuhl J. The 2009 Schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin. 2010;36(1):48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donahue SA, Manuel JI, Herman DB, Fraser LH, Chen H, Essock SM. Development and use of a transition readiness scale to help manage ACT team capacity. Psychiatric Services. 2012;63(3):223–229. doi: 10.1176/appi.ps.201100041. [DOI] [PubMed] [Google Scholar]
- Edwards S, Makunga N, Ngcobo S, Dhlomo M. Ubuntu: A cultural method of mental health promotion. International Journal of Mental Health Promotion. 2004;6(4):17–22. doi: 10.1080/14623730.2004.9721940. [DOI] [Google Scholar]
- Eisinga R, Grotenhuis M, Pelzer B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health. 2013;58(4):637–642. doi: 10.1007/s00038-012-0416-3. [DOI] [PubMed] [Google Scholar]
- Engelbrecht C, Kasiram MI. The role of Ubuntu in families living with mental illness in the community. South African Family Practice. 2012;54(5):441–446. doi: 10.1080/20786204.2012.10874268. [DOI] [Google Scholar]
- Fekadu A, Hanlon C, Gebre-Eyesus E, Agedew M, Solomon H, Teferra S, Prince M. Burden of mental disorders and unmet needs among street homeless people in Addis Ababa, Ethiopia. BMC Medicine. 2014;12(1):138. doi: 10.1186/s12916-014-0138-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flisher A, Sorsdahl KR, Joska J. Reliability of the Camberwell Assessment of Need for South African mental health service users. International Journal of Social Psychiatry. 2012;58(1):47–54. doi: 10.1177/0020764010382700. [DOI] [PubMed] [Google Scholar]
- Gade CB. The historical development of the written discourses on Ubuntu. South African Journal of Philosophy. 2011;30(3):303–329. doi: 10.4314/sajpem.v30i3.69578. [DOI] [Google Scholar]
- Gade CB. What is Ubuntu? Different interpretations among South Africans of African descent. South African Journal of Philosophy. 2012;31(3):484–503. doi: 10.1080/02580136.2012.10751789. [DOI] [Google Scholar]
- Herman D, Conover S, Gorroochurn P, Hinterland K, Hoepner L, Susser ES. Randomized trial of critical time intervention to prevent homelessness after hospital discharge. Psychiatric Services. 2011;62(7):713–719. doi: 10.1176/appi.ps.62.7.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joska JA, Flisher AJ. Needs and services at an in-patient psychotherapy unit. African Journal of Psychiatry. 2007;10(3):149–156. doi: 10.4314/ajpsy.v10i3.30247. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. The Schizophrenia Patient Outcomes Research Team (PORT): Updated treatment recommendations 2009. Schizophrenia Bulletin. 2010;36(1):94–103. doi: 10.1093/schbul/sbp130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kritzinger J, Swartz L, Mall S, Asmal L. Family therapy for schizophrenia in the South African context: Challenges and pathways to implementation. South African Journal of Psychology. 2011;41(2):140–146. doi: 10.1177/008124631104100203. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- Lasalvia A, Ruggeri M, Mazzi MA, Dall’Agnola RB. The perception of needs for care in staff and patients in community-based mental health services. The South-Verona outcome project 3. Acta Psychiatrica Scandinavica. 2000;102(5):366–375. doi: 10.1034/j.1600-0447.2000.102005366.x. [DOI] [PubMed] [Google Scholar]
- Lehman AF. A quality of life interview for the chronically mentally ill. Evaluation and Program Planning. 1988;11(1):51–62. doi: 10.1016/0149-7189(88)90033-X. [DOI] [Google Scholar]
- Lehman AF, Possidente S, Hawker F. The quality of life of chronic patients in a state hospital and in community residences. Hospital and Community Psychiatry. 1986;37(9):901–907. doi: 10.1176/ps.37.9.901. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Postrado LT, Rachuba LT. Convergent validation of quality of life assessments for persons with severe mental illnesses. Quality of Life Research. 1993;2(5):327–333. doi: 10.1007/BF00449427. [DOI] [PubMed] [Google Scholar]
- McCrone P, Bhui K, Craig T, Mohamud S, Warfa N, Stansfeld SA, … Curtis S. Mental health needs, service use and costs among Somali refugees in the UK. Acta Psychiatrica Scandinavica. 2005;111(5):351–357. doi: 10.1111/acp.2005.111.issue-5. [DOI] [PubMed] [Google Scholar]
- Morley C, Ablett P, Macfarlane S. Engaging with social work: A critical introduction. Port Melbourne, Australia: Cambridge University Press; 2014. [Google Scholar]
- Nicholas L, Rautenbach J, Maistry M. Introduction to social work. Cape Town, South Africa: Juta . . . Company; 2010. [Google Scholar]
- Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T, … Hayward P. The Camberwell assessment of need: The validity and reliability of an instrument to assess the needs of people with severe mental illness. The British Journal of Psychiatry. 1995;167(5):589–595. doi: 10.1192/bjp.167.5.589. [DOI] [PubMed] [Google Scholar]
- Pieterse M. Traditional African Jurisprudence. In: Roederer C, Moellendorf D, editors. Jurisprudence. Cape Town, South Africa: Juta . . . Company; 2004. pp. 438–462. [Google Scholar]
- Reamer FG. Social work values and ethics. New York, NY: Columbia University Press; 2013. [Google Scholar]
- Sachs A. The family in a democratic South Africa: Its constitutional position. Agenda: Empowering Women for Gender Equity. 1990;(8):40–54. doi: 10.2307/4065633. [DOI] [Google Scholar]
- Sales E. Family burden and quality of life. Quality of Life Research. 2003;12(Suppl 1):33–41. doi: 10.1023/A:1023513218433. [DOI] [PubMed] [Google Scholar]
- Saunders JC. Families living with severe mental illness: A literature review. Issues in Mental Health Nursing. 2003;24(2):175–198. doi: 10.1080/01612840305301. [DOI] [PubMed] [Google Scholar]
- Stein LI, Santos AB. Assertive community treatment of persons with severe mental illness. New York, NY: W.W. Norton . . . Company; 1998. [Google Scholar]
- Stein LI, Test MA. Alternative to mental hospital treatment: I. Conceptual model, treatment program, and clinical evaluation. Archives of General Psychiatry. 1980;37(4):392–397. doi: 10.1001/archpsyc.1980.01780170034003. [DOI] [PubMed] [Google Scholar]
- Susser E, Valencia E, Conover S, Felix A, Tsai W, Wyatt RJ. Preventing recurrent homelessness among mentally ill men: A “critical time” intervention after discharge from a shelter. American Journal of Public Health. 1997;87(2):256–262. doi: 10.2105/AJPH.87.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Test MA, Stein LI. Alternative to mental hospital treatment. III. Social cost. Archives of General Psychiatry. 1980;37(4):409–412. doi: 10.1001/archpsyc.1980.01780170051005. [DOI] [PubMed] [Google Scholar]
- University of Cape Town. ClinicalTrials.gov [Internet] Bethesda, MD: National Library of Medicine (US); 2015. Task sharing for the care of severe mental disorders in a low-income Country (TaSCS) Retrieved from http://clinicaltrials.gov/show/NCT02308956 NLM Identifier: NCT02308956. [Google Scholar]
- World Health Organization. WHO-AIMS report on mental health system in South Africa. Cape Town, South Africa: University of Cape Town; 2007. Retrieved from http://www.who.int/entity/mental_health/evidence/south_africa_who_aims_report. [Google Scholar]