Abstract
Vaccine development has had a huge impact on human health. However, there is a significant need to develop efficacious vaccines for several existing as well as emerging respiratory infectious diseases. Several challenges need to be overcome to develop efficacious vaccines with translational potential. This review focuses on two aspects to overcome some barriers — 1) the development of nanoparticle-based vaccines, and 2) the choice of suitable animal models for respiratory infectious diseases that will allow for translation. Nanoparticle-based vaccines, including subunit vaccines involving synthetic and/or natural polymeric adjuvants and carriers, as well as those based on virus-like particles offer several key advantages to help overcome the barriers to effective vaccine development. These include the ability to deliver combinations of antigens, target the vaccine formulation to specific immune cells, enable cross-protection against divergent strains, act as adjuvants or immunomodulators, allow for sustained release of antigen, enable single dose delivery, and potentially obviate the cold chain. While mouse models have provided several important insights into the mechanisms of infectious diseases, they are often a limiting step in translation of new vaccines to the clinic. An overview of different animal models involved in vaccine research for respiratory infections, with advantages and disadvantages of each model, is discussed. Taken together, advances in nanotechnology, combined with the right animal models for evaluating vaccine efficacy, has the potential to revolutionize vaccine development for respiratory infections.
Keywords: Nanovaccines, Animal models, Translation, Vaccine efficacy
Graphical abstract
1. Introduction
Respiratory infectious diseases remain a significant global threat to human health [1] and impose a heavy burden on our healthcare system [2]. These include diseases caused by well-known pathogens such as Bacillus anthracis, Streptococcus pneumonia, Mycobacterium tuberculosis, Yersinia pestis, influenza virus, and respiratory syncytial virus (RSV); as well as emerging zoonotic ones including severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), new strains of influenza, and Henipavirus. The influenza virus alone has caused more deaths in the 20th century than any other virus [3]. While vaccines have been enormously successful in combating infectious diseases [4] and are estimated to prevent over 3 million deaths worldwide annually [5], significant challenges remain on many fronts [6] as a result of which there are no effective vaccines currently available for several of the diseases [7], [8] listed above.
The current challenges facing vaccine development and translational research include identification of suitable antigen candidates, eliciting appropriate immune responses for protection, providing cross-protection against different strains of the pathogens, maintenance of the cold chain, repeated administration, route of administration and the need to identify appropriate animal models that will lead to similar responses in humans. To address potential solutions being pursued to address all these varied challenges would be outside the scope of any review, and several other review articles have focused on approaches to overcome many of these challenges [9], [10]. This review specifically focuses on two aspects: recent developments in nanoparticle-based delivery of respiratory vaccines; and choice of suitable animal models for respiratory infections to address the challenges associated with effective vaccine development.
Historically, vaccine development for influenza and many other viral infections has focused on the use of live or attenuated viruses [4], which require egg-based manufacturing systems that suffer from drawbacks of limited capacity and flexibility [3]. However, with recent developments in nanotechnology, material science and advances in immunology, subunit vaccines have gained prominence [9]. Nanoparticles (NPs) based on synthetic polymers as well as virus-like particles (VLP) offer several advantages and ways to address many of the challenges listed above. NPs provide the ability to deliver combinations of antigens in a single dose, target the vaccine formulation to specific cell types such as antigen presenting cells (APCs), allow encapsulation of either protein or DNA antigens or whole viruses, encapsulate domains that can elicit strong cross-neutralizing antibodies to protect against different strains [11], act as adjuvants or immunomodulators, allow for sustained antigen release, enable single dose delivery to enhance patient compliance, and potentially obviate the cold chain [12]. There are several lead nanoparticle vaccine candidates that have shown great promise in mouse and other pre-clinical models, but have failed in clinical trials [13]. Therefore the selection of appropriate animal models for vaccine development is a key requirement that can aid in the translation of promising vaccine technologies to the clinic for many of these diseases [14]. Both of these pathways for the development of more effective vaccines — nanoparticle-based vaccines and use of appropriate animal models for vaccine evaluation, are described in greater detail below. Taken together, advances in nanotechnology, combined with the right animal models for evaluating vaccine efficacy, has the potential to revolutionize vaccine development and translation for respiratory infections.
2. Nanoparticle-based vaccine delivery systems
Nanoscale materials have unique physicochemical properties in terms of their size, surface area, chemical composition and structure [15]. Unique properties of nano or microparticles (100–1000 nm size) have been widely utilized in drug and vaccine delivery [16], [17], [18]. Encapsulation of vaccine antigens (Ags) in biodegradable polymer-based NPs, or VLP-based strategies have proved to be powerful vaccine delivery systems [19], [20], especially to mucosal sites. In addition, targeting particulate vaccines to mucosal M cells helps in rapid internalization, processing and presentation of Ags by APCs to naïve T cells [21], [22]. Soluble Ags might be poorly immunogenic, but when entrapped in NPs, elicit strong immune responses as the NPs can act as adjuvants [23], [24]. NP size and surface characteristics can control their opsonization and clearance kinetics [25]. For optimal uptake of particulate Ags by APCs, the preferred size of NPs should be around 500 nm [26]. NP-based vaccines of approximately 500 nm size co-administered with toll-like receptor (TLR) ligands have been shown to induce long-lasting antigen-specific T cell response and production of high-affinity neutralizing antibodies [27]. Particles of up to 5 μm in size have been shown to protect encapsulated antigens and drugs from enzymatic or ionic degradation in vivo [17], [28]. Immunization using NP (200–600 nm)-based vaccines was found to enhance IFN-γ production and provided long-lasting antigen-specific humoral and cell-mediated immune responses [27], [29], [30], [31].
On the basis of physiological parameters such as hepatic filtration, tissue extravasation, tissue diffusion, and kidney excretion, the optimal size of NPs used in vivo varies. In addition to surface characteristics, the size of NPs plays a critical role in the bio-distribution of NPs [32]. NPs of 5–250 nm size range are found to be beneficial for drug delivery systems because of their ability to overcome multiple biological barriers and releasing a therapeutic load in the optimal dosage range [32]. However, when NPs of 50–500 nm size were delivered in vivo, high levels of agglomeration of the larger sized NPs was found in the liver [33]. Blood clearance of the smaller sized NPs is twice faster than larger formulations [32]. Orally delivered NPs of 20–40 nm are taken up readily by intestinal epithelial cells, while NPs larger than 100 nm are taken up mainly by specialized follicular epithelial cells called M cells [34], which in turn deliver them to underlying APCs to initiate immune response [35]. Studies in rats using larger size polystyrene and poly(lactic acid) NPs of 100–500 nm size showed uptake of particles exclusively by M cells [36], [37], [38].
2.1. Nanoparticle-based vaccine delivery to mucosal sites
Delivery of the vaccines to mucosal sites is ideal for eliciting appropriate immune responses to combat respiratory infections [39] because it mimics the entrance pathway of many of the pathogens [40]. Approximately 80% of the body's total immune cells are present at mucosal surfaces and mucosa-associated lymphoid tissues (MALT) [41]. The MALT is strategically located to orchestrate local immune functions against infections. Key immune cells in MALT involved in initiation of mucosal immunity are epithelial ‘M’ (Microfold, Membranous or Microvilli) cells and ‘professional’ APCs such as dendritic cells (DCs) and macrophages (Mϕs) [42]. M cells are dedicated to sampling, capture and transcytosis of microorganisms and particulate Ags to underlying APCs in the MALT, and are thus considered as the principal targets of the mucosal vaccine delivery system [21].
However, a variety of factors limit the mucosal delivery of vaccines, and these include mucociliary clearance, presence of deteriorating enzymes, pH extremes, low permeation, and metabolic degradation. To overcome these limitations, mucoadhesive polymeric NPs can be designed to pass through the mucus barrier and thus are promising mucosal delivery vehicles for vaccines [21]. Particulate Ags administered directly to mucosal sites have an inherent affinity for mucosal M cells and APCs, and are phagocytosed passively by APCs [43]. Particulate Ags delivered through an intranasal route have been found to be sampled readily by M cells of the nasal associated lymphoid tissues (NALT) and are delivered to underlying APCs in the respiratory tract [44]. M cells are strategically located in the epithelium of the small and large intestines, tonsils and adenoids, and airways, involved in sampling of particulate antigens [45]. But presence of M cells is still not clear in the mucosal sites of the reproductive tract and the deep airways. However, cells with typical features of M cells have been reported in the nasal passage epithelium of mice, suggesting the NALT-independent mode of antigen sampling in the respiratory tract is also possible [46]. NPs protect entrapped protein Ags from protease-mediated degradation at mucosal surfaces, thus aiding in preserving intact Ags for long periods of time at mucosal surfaces, and facilitating extended availability for sampling by M cells and APCs [47].
Mucus membrane is a single layer of epithelial cells in the mucosa protecting the body from entry of extraneous substances. Mucus is a viscoelastic gel layer that protects the mucosa, and it is composed of crosslinked and entangled mucin fibers secreted by goblet cells and submucosal glands [48] . The bulk viscosity of healthy human mucus is typically 1000–10,000 times higher than the viscosity of water. Mucosal delivery of vaccines is a challenge due to adverse physiological conditions at the mucosa such as mucociliary clearance, pH extremes, deteriorating enzymes, low permeation, and metabolic enzymatic degradation [49] . Therefore, mucoadhesive biodegradable polymer based NPs provide numerous advantages in delivery of vaccines and drugs [50]. They have desired chemistry to attach to mucus, inhibit the action of proteolytic enzymes, and modulate epithelial permeability once they reach the mucosa [51]. Thus, such polymer derived NPs are highly useful in mucosal delivery of vaccines, especially in the respiratory tract [52] .
NPs of 40–120 nm size engineered to display strong adhesive interactions with mucus and cell membranes are taken up by intestinal epithelial cells and facilitate the transport of conjugated substances into the lamina propria [53]. Similarly, mucus-penetrating NPs are also used in drug and gene delivery, as they avoid rapid mucus clearance mechanisms and provide targeted or sustained drug delivery for localized therapies in mucosal tissues. Neutrally charged, hydrophobic NPs rapidly aggregate in physiological conditions and are trapped in mucus via multivalent adhesive interactions with hydrophobic domains of mucin fibers [48] . Diffusion of PLGA NPs coated with anionic DNA via the cationic surfactant dimethyl dioctadecyl ammonium bromide was found to imporve NPs transport rate by 10-fold in pig gastric mucus compared to slightly smaller, hydrophobic polystyrene particles [48], [54]. All these data suggest that charge, size, and chemistry of the particles play a critical role in mucosal delivery systems, and both mucoadhesive and mucus-penetrating NPs facilitate the delivery of cargo to mucosal tissues. Thus, appropriate selection of the polymer to synthesize nanoparticle delivery systems is critical to deliver drug or vaccine to mucosal tissues.
2.2. Synthetic and natural polymers for NP-based vaccine delivery
The use of next generation biomaterials to develop polymeric nanovaccine delivery vehicles offers several advantages over more conventional vaccine adjuvants (Alum, MPLA, MF59) including thermal stability, reduced reactogenicity, shelf-life stability of the payload, and ability to induce mucosal immunity with both antibody- and cell-mediated responses [55], [56], [57], [58], [59], [60], [61]. By tailoring polymer chemistry and degradation kinetics, antigen release kinetics can be controlled and it is anticipated that the optimal nanovaccine will more closely mimic the immune response induced by the natural infection [12]. In this context, rapidly degrading (i.e., hydrophilic) nanoparticles may release antigen quickly and reduce antigen availability, impacting the ability of such nanovaccine formulations to induce sustained antibody responses [57]. In addition, the danger signals presented to the immune system by such formulations are weak as evidenced by waning profiles of pro-inflammatory cytokines [62]. Thus, hydrophobic and pathogen-mimicking nanovaccine formulations that enhance antigen availability and lead to the production of long-lived plasma cells more effectively prime the immune response and lead to long-lived protection [57]. Polymeric adjuvants can be further tailored to incorporate immunomodulatory properties [12]. A wide variety of biodegradable and biocompatible natural and synthetic polymers have proven to be useful for vaccine delivery and are approved by the US Food and Drug Administration (FDA) and European Medicines Agency [18], [28]. They include natural polymers like albumin, alginate, chitosan, collagen, cyclodextrin and gelatin; and synthetic polymers like polyesters, polylactides, polyacrylates, polylactones, polysulfones, polyanhydrides and poly(lactic-co-glycolic acid) (PLGA) [17], [63]. These polymers also act as adjuvants, but additional potent adjuvants in the vaccine formulations are usually necessary to boost the vaccine efficacy [64], [65]. Biodegradable NPs made of chitosan, PLGA, polyanhydrides, and liposomes have been in use to deliver candidate vaccines to mucosal sites [66].
PLGA is a widely used polymer in drug and vaccine delivery [49], [50], [67], [68], and it is non-toxic even at very high doses [67]. Until now, greater than 60% of patents filed on the development of PLGA NP vaccines involve delivery through the intranasal route [48]. NPs entrapping a killed influenza virus vaccine along with an adjuvant was administered intranasally to mice, rabbits, and pigs and found to elicit a protective immune response. In pigs, the intranasal route conferred better immunity compared to the intramuscular route of vaccination [69]. A single dose of intranasally delivered PLGA NP-entrapped Schistosoma mansoni Ags in mice elicited protective neutralizing antibody response detected in both the lungs and blood [70]. PLGA NP-entrapped bovine parainfluenza type 3 virus inoculated intranasally once elicited enhanced antibody response in mice [71]. A hallmark of PLGA NP-mediated vaccine delivery is its ability to induce enhanced and balanced Th1 and Th2 immune responses, essential for complete clearance of intracellular pathogens [72], [73], [74]. Therefore, to reinforce the efficiency of PLGA NPs mucosal vaccines, it is required to target the vaccine to mucosal M cells and DCs with the help of M cell targeting molecules, such as Ulex europaeus Agglutinin-I (UEA), specific immunoglobulins, and TLR ligands [44], [75], [76]. Intranasal vaccination of mice with PLGA NPs entrapping HIV peptides and UEA elicited enhanced and prolonged antibody and T cell response at both mucosal and systemic sites compared to vaccination by other routes [77]. UEA entrapped in PLGA NPs targets particles to M cells resulting in a 2–4 fold increase in specific antibody titers [77]. Surface anchored UEA on PLGA NPs entrapped with hepatitis B virus enhanced the vaccine targeting to M cells in vitro. And in orally vaccinated mice, significantly augmented SIgA and Th1 cytokines production was observed compared to NPs without M cell targeting agents [78]. In mice, PLGA NPs entrapped with hepatitis B, rotavirus, influenza, or parainfluenza viruses generated protective immune response when delivered to mucosal sites [69], [71], [79], [80].
PLGA NPs also mediate activation, maturation, and antigen presentation by APCs [81]. Since NPs facilitate sustained release of vaccine Ags, they mediate induction of robust B and T cell responses [82]. NP-based vaccines are capable of eliciting cell-mediated and humoral response in the lungs of mice [56], [57], [58], [59], [60], [61]. PLGA NPs can provide slow release of antigens and can elicit robust effector and memory immune responses [83]. A recent study has shown that the duration of available vaccine Ags to effector T-cells (also to a lesser extent memory T cells) can control the magnitude of CD4 and CD8 T-cell responses, which require sustained antigenic stimulation for their maximal expansion [84]. PLGA NPs have been shown to promote cross-presentation of vaccine Ags, as the phagosome-disruptive properties of PLGA NPs facilitate delivery of Ags to the cytosol for MHC class I loading and CD8+ T cell activation [85], [86], [87], [88], [89], [90]; which in turn helps in the generation of memory T cell response and efficient clearance of invading pathogens [83]. The interaction of NPs with pathogen recognition receptors on APCs (especially B cells) can lead to affinity maturation and production of highly avid antibodies [91].
Polyanhydride-based nanoparticle vaccine delivery systems have been designed against several respiratory diseases, including influenza, pneumonia, anthrax, and pneumonic plague [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105]. Polyanhydrides are biodegradable materials suitable for intranasal delivery in the form of micro or nanoparticles [106], and can enable sustained release kinetics of encapsulated antigen, resulting in long-lived, high avidity antibody titers induced with otherwise suboptimal doses of antigen [97], [103], [107]. Polyanhydride nanoparticles have been shown to be a versatile vaccine adjuvant/delivery platform that can enhance the immune response to recombinant proteins [97], [103], [107]. Amphiphilic polyanhydride nanoparticles have been demonstrated to preserve the structure and antigenicity of recombinant proteins upon release [98], [108], [109], [110], [111], [112]. In addition to amplifying humoral immunity, polyanhydride nanoparticle-based vaccines (i.e., nanovaccines) activate APCs [105], [113], [114], have been shown to be immunomodulatory [97], and are capable of promoting cell-mediated immunity by expansion of antigen-specific memory CD8+ T cells [115].
In addition to PLGA, and polyanhydrides, other polymeric systems, liposomes, nano-emulsions [8] and micellar delivery systems [116], [117], [118] have shown promise as NP-based vaccine delivery systems. Chitosan, a cationic mucoadhesive polymer, has shown efficacy in NP-vaccines for diphtheria and other infections [119], [120]. Chitosan NPs have shown an immune potentiating ability that is mediated by innate immune cells, in addition to enhanced production of IL-6 and IFN-γ [121]. Phagocytosed NPs induce activation and maturation of mouse APCs due to their inherent adjuvant properties [88]. In an earlier study, rapid uptake of chitosan NPs by APCs derived from mice followed by gradual release of Ags, and increased expression of co-stimulatory molecules and activation of DCs and antigen presentation by MHC class I and II molecules was observed [122], [123]. Phagocytosis of polystyrene latex microspheres by Mϕs activate the signal transduction events in innate immune cells [124]. Other polysaccharides such as dextran derivatives [125], alginate [126] and starch [127] micro and nanoparticles have shown good macrophage uptake, high antibody titers, mucosal and systemic immune responses, and protection against challenge.
2.3. Virus-like particles for vaccine delivery
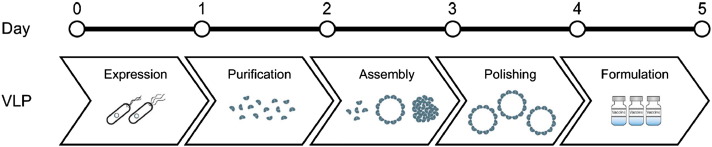
VLP are formed from assemblies of viral proteins that can effectively crosslink B cell receptors, exhibiting immunostimulatory properties of viruses, without the potential for infection [128]. VLPs are structurally diverse and functionally versatile and can trigger both arms of the immune response and are taken up by APCs. The licensed human papilloma virus vaccine is based on VLP technology [129]. Different antigens can be displayed on the surface of VLPs. VLPs can be commercially produced in various host systems such as Escherichia coli, yeast, insect cell cultures and CHO cells, enabling facile production of efficient vaccines for diseases such as influenza in several expression systems [3]. Several VLP-based vaccine candidates are currently in clinical trials (Fig. 1 ) [129]. VLPs delivered intranasally have been shown to produce high lung mucosal antibody titers without additional adjuvants [130]. However, prediction of functional epitopes and the ability to present native 3D structures of the epitopes on the carriers are challenges that need to be overcome. Enhanced molecular modeling and computational design efforts to help overcome these challenges, and biomolecular engineering advances to present large antigens on VLPs are urgently needed to reduce vaccine development time and high vaccine costs associated with VLP vaccine production [129].
Fig. 1.
Microbial platform for VLP-based vaccines.
Adapted from [129] with permission from John Wiley and Sons.
3. Animal models for human respiratory disease studies and vaccine development
Identifying suitable large animal surrogates for understanding the efficacy of novel candidate vaccines as well as insights on human disease pathogenesis, is likely to have high impact for translational research to improve human health, as the predictive validity of preclinical animal models has been disappointing [13]. In some disease areas, greater than 90% of promising new treatments failed in clinical trials [131] because the targeted pathogenic process can be expressed differently in the animal model as opposed to humans. In general, there are fundamental immunobiological differences between young inbred mice and human patients [132]. Inbred mice also lack genetic diversity and the exposure to environmental pathogens. Large animal models, such as non-human primates (NHPs) and large farm animals can potentially provide better predictive validity [13]. Basic biological research using murine models has brought enormous knowledge following the development of technologies for production of monoclonal antibodies, and transgenic and gene knockouts. However, many recent studies have questioned the utility of mouse models for understanding certain diseases, vaccines, and drug screening efforts [133], [134], [135], [136]. For example, mice are resistant to the development of classic TB disease, minimizing their utility for evaluation of TB vaccines [137]. There are substantial differences in pathogenesis in RSV mouse models versus in human patients [138].
The route of administration (intranasal, subcutaneous, etc.) has an impact on the choice of the animal model and the efficacy of the vaccine. The mucosal immune inductive sites in the respiratory tract are concentrated in aggregates of MALT adjacent to mucosal surfaces of the nasal cavity, nasopharynx, larynx, trachea and bronchus; these are called NALT, lymphoid tissues of the Waldeyer's ring in the nasopharynx (tonsils), larynx and trachea associated lymphoid tissues (LALT and TALT), and bronchus-associated lymphoid tissues (BALT) [41], [139]. Unlike in rodents, in farm animals (such as pigs, cattle, sheep, and horses), tonsils and LALT are well developed, and LALT is on the epiglottis in the vestibulum laryngis and the plica aryepiglottica [140] present in the form of lymphatic nodules [139].
3.1. Non-human primate models
NHPs are excellent preclinical models for vaccine development and translation because of their evolutionary proximity to humans, similarities in host defense components as well as in clinical and pathological presentation of disease, and their large size allow for frequent blood sampling [141]. There is an expanding genome sequence data for various NHPs, leading to the greater use of omics- approaches to profile NHP responses to viral infections and vaccinations [142].
Asian macaques are one of the most frequently used NHPs in infectious disease research. NHPs and the macaques species in particular, are naturally susceptible to TB infection and display all the typical features of human TB, including identical histological structure of TB granulomas [143]. NHPs such as chimpanzees have also been used, but suffer from ethical constraints [144]. Unfortunately, all of the existing animal models for TB other than NHPs suffer from specific drawbacks and fail to mimic the human disease perfectly [137]. Macaque models have also aided research related to H5N1 and H1N1 pandemic influenza disease models [142] and are emerging as viable animal models for MERS–CoV [145].
African green monkeys (AGM) also provide a good model for influenza studies [146], [147] as the distribution of sialic acid receptors is similar to that in humans, and live attenuated pandemic influenza virus vaccines were found to replicate similarly in these monkeys as in humans [147]. AGMs also provide a more uniformly lethal model of henipavirus infections compared to the more variable response seen in squirrel monkeys [148] and are considered the gold standard for testing the efficacy of vaccines against henipaviruses. They have also shown utility as models for evaluating countermeasures against RSV infections [149].
RSV has been found to cause severe respiratory failure, especially in infants. There is no vaccine available for RSV, partly because of the difficulties associated with the lack of a suitable animal model to study the pathophysiology of the disease and evaluate vaccines [150]. Infant baboon models of RSV have shown clinical and pathological changes similar to those observed in human infant patients and offer a promising model for the disease [138]. In contrast, chimpanzee (and other monkey models) experience only mild infections and do not experience the lower respiratory tract infections seen in human infant RSV [138]. Since RSV vaccines need to elicit mucosal immunity at both upper and lower respiratory tracts to effectively prevent RSV infection, the baboon model provides advantages over the chimpanzee model for RSV [151]. Baboons have also been shown to be excellent animal models for pertussis, with 100% inoculated baboons developing clinical pertussis, compared to only 25% of rhesus macaques [152].
SARS–CoV studies have been limited in NHP models, with a few studies involving African green monkeys, marmosets, cynomolgus and rhesus macaques. Variability in the results points to a need for more studies with large sample sizes to draw meaningful conclusions [153]. Cynomolgus macaques are however preferred for Ebola studies since the immunologic and physiologic responses are thought to be similar to those in humans [154], and they are also good models for anthrax infections [155]. Conflicting results have been reported with respect to the efficacy of pneumonic plague vaccines based on the F1-V fusion protein when evaluated in cynomolgus macaques and African green monkeys [156], [157]. While protection was demonstrated in the macaques, there was considerably less success in the African green monkey, once again underlining some of the complexities associated with using NHPs as preclinical animal models for vaccine efficacy against respiratory infections.
However, the cost, availability, need for specialized personnel and facilities, and ethical concerns prevent large-scale use of NHP models for vaccine development studies [13] and limit their use. The U.S. federal government recently announced that captive chimpanzees will also be protected under the Endangered Species Act. Moreover, because species such as the rhesus macaques are genetically diverse and outbred, sufficient statistical power requires the use of larger animals and greater numbers of replicates [142].
3.2. Small animal models
Due to commonalities in the course of clinical infection with TB in guinea pigs and humans, they are commonly used for vaccine evaluation. However, there is a limited resource of immunological reagents for quantitative evaluation of the immune responses in this model [137] compared to mice. Guinea pigs were also one of the earliest models to be used for henipavirus infections, but variability in results led to reduced interest in this model [158]. Cotton rats are commonly used models for RSV and other respiratory infections [159] such as metapneumovirus infections [160]. RSV replication occurs in lower airways and the virus is present in both the upper and lower respiratory tracts, leading to pneumonia [161]. Golden Syrian hamsters are good animal models for SARS–CoV because their respiratory tracts enable virus replication and can elicit good neutralizing antibody response [153]. These hamsters have also been used for henipaviruses to study transmission and pathogenesis [162]. Rabbits are relatively resistant to M. tuberculosis, but are susceptible to Mycobacterium bovis, producing pulmonary cavities like humans [137]. They are also a potential model for MERS–CoV infections [163] and for anthrax [164], [165]. In many of these cases, however, limited immunological reagents and techniques are available compared to mouse models, which limit studies of immunological pathways.
Ferrets are one of the earliest and the most widely used model for influenza [166] because they are susceptible to a wide range of human isolates without prior adaptation [167]. They have similar influenza receptor distributions to that of humans in the respiratory system and exhibit upper respiratory infection patterns and clinical symptoms similar to that in humans [168]. Moreover, ferrets are the only mammalian model suitable for studies of both pathogenesis and transmission [169] of influenza viruses [167], as they can transmit human viruses to naïve animals by direct contact or respiratory droplets [170], [171]. In addition, histochemical studies in ferrets correlate well with differences in pathology between seasonal [172] and pandemic viruses [173] seen in humans leading to similarities in the different disease outcomes seen in both species [174]. An aged ferret model has also been developed to investigate influenza morbidity in the elderly population [175]. Ferrets have also been shown to be good models for pathogenesis of other respiratory viruses such as paramyxoviruses such as henipaviruses [166] as they develop the full spectrum of diseases seen in humans. However, unlike in hamsters, no correlation between challenge dose and clinical outcome was seen in ferrets with henipavirus infections [176]. In the case of coronaviruses, there was variability in the infection and presentation of disease symptoms for SARS–CoV in a ferret model [177], [178]. Ferrets and other small animal models were found not to be susceptible to MERS–CoV and do not enable replication of the virus, restricting the efficacy evaluation of MERS vaccines in small animal models [153], [179]. The sequencing of the ferret genome opens new avenues, but the greatest disadvantage of ferret models remains the limitation of species-specific reagents.
Fruit bats are natural reservoirs for several viruses such as henipaviruses and Ebola, and the viruses usually cause asymptomatic infections in the hosts. However, viruses, after crossing the species barrier turn virulent. They have been used in the generation of neutralizing antibodies and the mechanisms by which viral replication in bats is controlled are being investigated [158]. Cats are also susceptible to henipavirus infections and become clinically ill, and can be used to assess the potential of vaccines [158].
3.3. Large farm animal models
Although rodents and primates are taxonomically closer than pigs, the divergence of all three occurred over only half a million years ago, such that taxonomic relationships are largely irrelevant [180]. Calibrated comparisons show that the rodent genome has changed faster since that divergence, resulting in greater identity between pig and human than human and mouse [181], [182]. The availability of the swine genome sequence (assembly 10.2) [183] and new transgenic and gene knockout capabilities [184], [185], [186], [187], [188] have together increased the use of pigs in biomedical research. The pig is a better suited biomedical model than rodents in many respects, due not only to its size but also to its anatomic, physiologic, and genomic similarities to humans [189], [190]. In addition, like humans, the pig is monogastric, omnivorous, and an outbred species, and it shares a comparable immune system. For all these reasons, the pig is considered as an important large animal model species for human health research including obesity, reproductive, cardiovascular and nutritional disorders, infectious diseases, and vaccine research [191], [192], [193], [194].
In particular, the pig is considered as an ideal animal model for studies related to respiratory infections because, its lung has marked similarities to that of humans in terms of the tracheobronchial-tree structure, airway morphology, abundance of airway submucosal glands, and in production of cytokines and chemokines [195], [196], [197]. The electrophysiological properties of the airway epithelium and submucosal glands of the pig resembles that of humans [198], [199], [200]. Therefore, the pig has been used for studies on chronic bronchitis and cystic fibrosis [201], [202]. Unlike rodents, the pig is a natural host for wide range of influenza viruses, because its airway epithelial cells contain receptors preferred by both avian and mammalian influenza viruses [203], [204], [205]. In addition, cytokine profiles in influenza infected pigs and humans are highly comparable [206], [207]. Pigs also offer advantages for cutaneous delivery of vaccines compared to mice because of larger surface areas, possibility of repeated sampling and similarities between human and pig skins, compared to those of mice [208]. Therefore, pigs represent an excellent, but underutilized animal models for respiratory infections such as influenza [209].
The pig is an ideal model for NP-based vaccine studies. NP-based delivery vehicles for vaccines (i.e., nanovaccines) and drugs have been extensively evaluated in mouse models. However, there are several limitations in translating novel rodent findings to improve human health [210]. Therefore, the pig may serve as a useful large animal model for nanovaccine research. Rapid uptake of PLGA NPs entrapped UV-killed porcine reproductive respiratory syndrome virus (PRRSV) (NanoPRRS) by porcine Mϕs and DCs, translocation of viral Ags into their endosomal compartment, and increased expression of the activation marker CD80/86 was observed [211]. Studies have demonstrated immune potentiating activity of NPs in mice, pigs, and macaques; but immune correlates were not evaluated in detail in vaccinated and virus challenged animals [212]. In a pre-challenge study, NanoPRRS vaccine was administered intranasally to pigs and observed significantly increased frequency of CD8+ T cells, Th/memory cells, with increase in the secretion of innate (IFN-α), proinflammatory (IL-6), and Th1 (IFN-γ) cytokines [211].
In pigs, a single dose of NanoPRRS vaccine administered intranasally and challenged with a virulent heterologous virus, showed reduced clinical PRRS symptoms with decreased gross and microscopic lung lesions and reduction in viremia (but not viral load in the lungs). Immunologically, enhanced virus-specific IgA in the lungs, increased virus neutralization (VN) titers (3 log2) and high levels of IFN-γ production were detected [211], [213]. In a similarly vaccinated and homologous virus challenged pigs, viremia was cleared early with augmented antibody and cytokine responses [214]. To further improve the efficacy of NanoPRRS, the vaccine was co-administered with a potent adjuvant (M. tuberculosis whole cell lysate, M. tb WCL) that we identified earlier [205], [215], and observed complete clearance of detectable infectious challenged heterologous PRRSV (genetically 15% different) from the lungs [73], [74]. Immunologically, increased VN titers (4 log2) and IFN-γ+ lymphocytes were observed [74], [213]. In yet another study, coexpressed GP3 and GP5 of type 1 PRRSV coated on chitosan NPs was administered twice intramuscularly with Quil A adjuvant and challenged with a homologous virus, results suggested one log reduction in the viral RNA load in the blood and lungs. Immunologically, increased IFN-γ production was associated with amplified CD4+ and CD8+ T cell frequencies and lymphocyte proliferation with VN titers of 4 log2 [216]. This study confirmed the advantages of NP-mediated delivery of viral vaccine to pigs.
Intranasal delivery of biodegradable polymeric NPs encapsulating viral vaccines has shown huge promise in eliciting enhanced breadth of cross-protective immunity in rodent models and in pigs [73], [74], [211]. PRRSV induced VN activity is weak and delayed [217], [218], but in NanoPRRS vaccinated pigs VN titers were detectably quite early and steadily increased [83]. Inactivated vaccines generally induce Th2 responses [219], but NP-based vaccines drive either balanced Th1–Th2 or Th1-biased responses [77]. In NanoPRRS administered pigs vaccinated intranasally, balanced Th1–Th2 responses were observed, indicated by increased IgG1 and IgG2 production and enhanced IFN-γ and IL-4 production [73], [74]. Recently, PLGA NPs entrapping five conserved IAV peptides delivered intranasally as a mist to pigs enhanced the breadth of the T cell response, with reduction in detectable challegned infective lung virus load, but it did not boost the VN titers (Hiremat and Renukaradhya 2015, manuscript submitted). To improve the efficacy of inactivated swine influenza virus vaccine, in an ongoing study PLGA NPs were entrapped with an inactivated H1N2 (δ1-lineage) virus and delivered as a mist intranasally to pigs, and our results indicated the complete clearance of challenged infective heterologous zoonotic H1N1 (γ-lineage) virus from the lungs of 80% of vaccinated animals (Dhakal and Renukaradhya 2015, unpublished data). All these studies have suggested the induction of enhanced cross-reactive immune responses by the NP delivery system in pigs.
While pigs can be effective animal models for respiratory vaccines, other large farm animals such as cattle and lambs have also been explored for specific infectious diseases such as RSV. Cattle are natural hosts for bovine RSV [220], which does not infect humans, but F glycoproteins in bovine RSV and human RSV have 80% amino acid sequence identity along with some cross-reactive neutralizing epitopes [14]. The spectrum of diseases caused in calves overlaps with human RSV disease, making it a viable model [161]. Since RSV mainly affects infants and young children worldwide, similarities in developmental, structural, physiological and immunological features between newborn lamb lungs and human infants make it a good model for assessment of potential RSV vaccines [221]. In rodents, the alveolar development occurs postnatally, while in lambs and humans, it occurs prenatally, allowing for a better model for preterm human infants. In addition, the ovine lung is susceptible to secondary bacterial infections that commonly occur with RSV infections. The ethical issues associated with use of NHPs can also be circumvented with the use of lamb models for RSV.
A summary of various animal models that have been used for different respiratory infections is provided in Table 1 .
Table 1.
Various animal models used in different respiratory infectious disease research to evaluate countermeasures.
| Animal model | Respiratory infectious disease |
|---|---|
| Macaques | Influenza [142], TB [143], MERS–CoV [145], SARS–CoV [153], Ebola [154], Anthrax [155], pneumonic plague [156] |
| African green monkeys | Influenza [146], [147], henipavirus [148], RSV [149], SARS–CoV [153], pneumonic plague [157] |
| Baboons | RSV [138], [151], pertussis [152] |
| Guinea pigs | TB [137], henipavirus [158] |
| Cotton rats | RSV [159], [161], metapneumovirus [160] |
| Golden Syrian hamsters | SARS–CoV [153], henipaviruses [162] |
| Rabbits | MERS–CoV [163], anthrax [164], [165] |
| Cats | Henipaviruses [158] |
| Ferrets | Influenza pathogenesis and transmission [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], henipaviruses [166] |
| Pigs | Influenza [203], [204], [205], [206], [207], [208], [209] |
| Cattle | RSV [220], [161] |
| Lambs | RSV [221] |
4. Conclusions and future prospects
There is an urgent need to develop alternative strategies to use of viral vaccines. Nanoparticle-based subunit vaccines and VLPs provide promising alternative approaches that are gaining significant momentum. The move away from viral vectors can potentially accelerate the production of vaccines, enable single dose delivery, immunomodulation, cross-protection against various strains of the pathogen and enable targeting to specific cell types. Various biodegradable polymers, both natural and synthetic, are being explored for encapsulation of the antigens for vaccine development. VLPs can provide the advantages of viruses without many of the associated challenges such as infections. However, the choice of suitable animal models for testing the efficacy of these new vaccines is very important aspect to enable successful translation of these experimental vaccines to the clinic. While mice models are easier to implement, and relatively inexpensive, they might not provide clinically relevant answers in many cases. The discussion presented herein reveals that there is no universal animal model for respiratory infections. Depending on the questions to be answered, the route of administration of the vaccine and the scale of the study, animal models should be carefully chosen to provide reliable testing of vaccine countermeasures, which can then enable successful translation to the clinic [222].
Acknowledgments
We gratefully acknowledge funding from the U.S. Army (Grant #W81XWH-10-1-0806) to S.K.M. and B.N., National Pork Board (NPB# 09-213), USDA-AFRI PRRSCAP2 (2008-55620-19132) and the OARDC, The Ohio State University to G.J.R. S.K.M. acknowledges support from the Stanley Chair in Interdisciplinary Engineering. B.N. gratefully acknowledges support from the National Institutes of Health (R01 AI111466-01) and the Vlasta Klima Balloun Professorship. All the authors acknowledge support from the Iowa State Nanovaccine Initiative.
References
- 1.Lipscomb M.F., Hutt J., Lovchik J., Wu T., Lyons C.R. The pathogenesis of acute pulmonary viral and bacterial infections: investigations in animal models. Annu. Rev. Pathol. 2010;5:223–252. doi: 10.1146/annurev-pathol-121808-102153. [DOI] [PubMed] [Google Scholar]
- 2.Ferkol T., Schraufnagel D. The global burden of respiratory disease. Ann Am. Thorac. Soc. 2014;11:404–406. doi: 10.1513/AnnalsATS.201311-405PS. [DOI] [PubMed] [Google Scholar]
- 3.Jegerlehner A., Zabel F., Langer A., Dietmeier K., Jennings G.T., Saudan P., Bachmann M.F. Bacterially produced recombinant influenza vaccines based on virus-like particles. PLoS One. 2013;8:e78947. doi: 10.1371/journal.pone.0078947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arvin A.M., Greenberg H.B. New viral vaccines. Virology. 2006;344:240–249. doi: 10.1016/j.virol.2005.09.057. [DOI] [PubMed] [Google Scholar]
- 5.Ehreth J. The global value of vaccination. Vaccine. 2003;21:596–600. doi: 10.1016/s0264-410x(02)00623-0. [DOI] [PubMed] [Google Scholar]
- 6.Fontana J.M., Alexander E., Salvatore M. Translational research in infectious disease: current paradigms and challenges ahead. Transl. Res. 2012;159:430–453. doi: 10.1016/j.trsl.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin Montañés C., Gicquel B. New tuberculosis vaccines. Enferm. Infecc. Microbiol. Clin. 2011;29(Suppl. 1):57–62. doi: 10.1016/S0213-005X(11)70019-2. [DOI] [PubMed] [Google Scholar]
- 8.Lindell D.M., Morris S.B., White M.P., Kallal L.E., Lundy P.K., Hamouda T., Baker J.R., Jr., Lukacs N.W. A novel inactivated intranasal respiratory syncytial virus vaccine promotes viral clearance without th2 associated vaccine-enhanced disease. PLoS One. 2011;6:e21823. doi: 10.1371/journal.pone.0021823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson-Welder J.H., Torres M.P., Kipper M.J., Mallapragada S.K., Wannemuehler M.J., Narasimhan B. Vaccine adjuvants: current challenges and future approaches. J. Pharm. Sci. 2009;98(4):1278–1316. doi: 10.1002/jps.21523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ross K.A., Huntimer L.M., Vela Ramirez J.E., Adams J.R., Carpenter S.L., Kohut M.L., Bronich T., Webby R., Legge K.L., Mallapragadal S.K., Wannemuehler M.J., Narasimhan B. Vaccine technologies against avian influenza: current approaches and new directions. J. Biomed. Nanotechnol. 2014;10:2261–2294. doi: 10.1166/jbn.2014.1983. [DOI] [PubMed] [Google Scholar]
- 11.Du L., Zhao G., Sun S., Zhang X., Zhou X., Guo Y., Li Y., Zhou Y., Jiang S. A critical ha1 neutralizing domain of h5n1 influenza in an optimal conformation induces strong cross-protection. PLoS One. 2013;8:e53568. doi: 10.1371/journal.pone.0053568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallapragada S.K., Narasimhan B. Immunomodulatory biomaterials. Int. J. Pharm. 2008;364:265–271. doi: 10.1016/j.ijpharm.2008.06.030. [DOI] [PubMed] [Google Scholar]
- 13.t Hart B.A., Bogers W.M., Haanstra K.G., Verreck F.A., Kocken C.H. The translational value of non-human primates in preclinical research on infection and immunopathology. Eur. J. Pharmacol. 2015;759:69–83. doi: 10.1016/j.ejphar.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Shaw C.A., Ciarlet M., Cooper B.W., Dionigi L., Keith P., O'Brien K.B., Rafie-Kolpin M., Dormitzer P.R. The path to an rsv vaccine. Curr. Opin. Virol. 2013;3:332–342. doi: 10.1016/j.coviro.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Magenheim B., Benita S. Nanoparticle charecterization: a comprehensive physicochemical approach. STP Pharma. Sci. 1991;1:221–241. [Google Scholar]
- 16.Nel A., Xia T., Madler L., Li N. Toxic potential of materials at the nanolevel. Science. 2006;311:622–627. doi: 10.1126/science.1114397. [DOI] [PubMed] [Google Scholar]
- 17.Panyam J., Labhasetwar V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv. Drug Deliv. Rev. 2003;55:329–347. doi: 10.1016/s0169-409x(02)00228-4. [DOI] [PubMed] [Google Scholar]
- 18.Duncan R. Nanomedicine gets clinical. Mater. Today. 2005;8:16–17. [Google Scholar]
- 19.Langer R., Cleland J.L., Hanes J. New advances in microsphere-based single-dose vaccines. Adv. Drug Deliv. Rev. 1997;28:97–119. doi: 10.1016/s0169-409x(97)00053-7. [DOI] [PubMed] [Google Scholar]
- 20.Hanes J., Chiba M., Langer R. Polymer microspheres for vaccine delivery. Pharm. Biotechnol. 1995;6:389–412. doi: 10.1007/978-1-4615-1823-5_16. [DOI] [PubMed] [Google Scholar]
- 21.Woodrow K.A., Bennett K.M., Lo D.D. Mucosal vaccine design and delivery. Annu. Rev. Biomed. Eng. 2012;14:17–46. doi: 10.1146/annurev-bioeng-071811-150054. [DOI] [PubMed] [Google Scholar]
- 22.des Rieux A., Fievez V., Garinot M., Schneider Y.J., Preat V. Nanoparticles as potential oral delivery systems of proteins and vaccines: a mechanistic approach. J. Control. Release. 2006;116:1–27. doi: 10.1016/j.jconrel.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 23.Bacon A., Makin J., Sizer P.J., Jabbal-Gill I., Hinchcliffe M., Illum L., Chatfield S., Roberts M. Carbohydrate biopolymers enhance antibody responses to mucosally delivered vaccine antigens. Infect. Immun. 2000;68:5764–5770. doi: 10.1128/iai.68.10.5764-5770.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertram U., Bernard M.C., Haensler J., Maincent P., Bodmeier R. In situ gelling nasal inserts for influenza vaccine delivery. Drug Dev. Ind. Pharm. 2010;36:581–593. doi: 10.3109/03639040903382673. [DOI] [PubMed] [Google Scholar]
- 25.Moghimi S.M., Szebeni J. Stealth liposomes and long circulating nanoparticles: critical issues in pharmacokinetics, opsonization and protein-binding properties. Prog. Lipid Res. 2003;42:463–478. doi: 10.1016/s0163-7827(03)00033-x. [DOI] [PubMed] [Google Scholar]
- 26.Foged C., Brodin B., Frokjaer S., Sundblad A. Particle size and surface charge affect particle uptake by human dendritic cells in an in vitro model. Int. J. Pharm. 2005;298:315–322. doi: 10.1016/j.ijpharm.2005.03.035. [DOI] [PubMed] [Google Scholar]
- 27.Kasturi S.P., Skountzou I., Albrecht R.A., Koutsonanos D., Hua T., Nakaya H.I., Ravindran R., Stewart S., Alam M., Kwissa M., Villinger F., Murthy N., Steel J., Jacob J., Hogan R.J., Garcia-Sastre A., Compans R., Pulendran B. Programming the magnitude and persistence of antibody responses with innate immunity. Nature. 2011;470:543–547. doi: 10.1038/nature09737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McNeil S.E. Nanotechnology for the biologist. J. Leukoc. Biol. 2005;78:585–594. doi: 10.1189/jlb.0205074. [DOI] [PubMed] [Google Scholar]
- 29.Gregory A.E., Titball R., Williamson D. Vaccine delivery using nanoparticles. Front. Cell. Infect. Microbiol. 2013;3:13. doi: 10.3389/fcimb.2013.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diwan M., Elamanchili P., Cao M., Samuel J. Dose sparing of cpg oligodeoxynucleotide vaccine adjuvants by nanoparticle delivery. Curr. Drug Deliv. 2004;1:405–412. doi: 10.2174/1567201043334597. [DOI] [PubMed] [Google Scholar]
- 31.Lutsiak M.E., Kwon G.S., Samuel J. Biodegradable nanoparticle delivery of a th2-biased peptide for induction of th1 immune responses. J. Pharm. Pharmacol. 2006;58:739–747. doi: 10.1211/jpp.58.6.0004. [DOI] [PubMed] [Google Scholar]
- 32.Alexis F., Pridgen E., Molnar L.K., Farokhzad O.C. Factors affecting the clearance and biodistribution of polymeric nanoparticles. Mol. Pharm. 2008;5:505–515. doi: 10.1021/mp800051m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nagayama S., Ogawara K., Fukuoka Y., Higaki K., Kimura T. Time-dependent changes in opsonin amount associated on nanoparticles alter their hepatic uptake characteristics. Int. J. Pharm. 2007;342:215–221. doi: 10.1016/j.ijpharm.2007.04.036. [DOI] [PubMed] [Google Scholar]
- 34.Howe S.E., Lickteig D.J., Plunkett K.N., Ryerse J.S., Konjufca V. The uptake of soluble and particulate antigens by epithelial cells in the mouse small intestine. PLoS One. 2014;9:e86656. doi: 10.1371/journal.pone.0086656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Corr S.C., Gahan C.C., Hill C. M-cells: origin, morphology and role in mucosal immunity and microbial pathogenesis. FEMS Immunol. Med. Microbiol. 2008;52:2–12. doi: 10.1111/j.1574-695X.2007.00359.x. [DOI] [PubMed] [Google Scholar]
- 36.Jani P., Halbert G.W., Langridge J., Florence A.T. The uptake and translocation of latex nanospheres and microspheres after oral administration to rats. J. Pharm. Pharmacol. 1989;41:809–812. doi: 10.1111/j.2042-7158.1989.tb06377.x. [DOI] [PubMed] [Google Scholar]
- 37.Jani P., Halbert G.W., Langridge J., Florence A.T. Nanoparticle uptake by the rat gastrointestinal mucosa: quantitation and particle size dependency. J. Pharm. Pharmacol. 1990;42:821–826. doi: 10.1111/j.2042-7158.1990.tb07033.x. [DOI] [PubMed] [Google Scholar]
- 38.Primard C., Rochereau N., Luciani E., Genin C., Delair T., Paul S., Verrier B. Traffic of poly(lactic acid) nanoparticulate vaccine vehicle from intestinal mucus to sub-epithelial immune competent cells. Biomaterials. 2010;31:6060–6068. doi: 10.1016/j.biomaterials.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 39.Bolton D.L., Song K., Wilson R.L., Kozlowski P.A., Tomaras G.D., Keele B.F., Lovingood R.V., Rao S., Roederer M. Comparison of systemic and mucosal vaccination: impact on intravenous and rectal siv challenge. Mucosal Immunol. 2012;5:41–52. doi: 10.1038/mi.2011.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hasegawa H., van Reit E., Kida H. Mucosal immunization and adjuvants. Curr. Top. Microbiol. Immunol. 2015;386:371–380. doi: 10.1007/82_2014_402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holmgren J., Czerkinsky C., Lycke N., Svennerholm A.M. Mucosal immunity: implications for vaccine development. Immunobiology. 1992;184:157–179. doi: 10.1016/S0171-2985(11)80473-0. [DOI] [PubMed] [Google Scholar]
- 42.Dlugonska H., Grzybowski M. Mucosal vaccination–an old but still vital strategy. Ann. Parasitol. 2012;58:1–8. [PubMed] [Google Scholar]
- 43.Inaba K., Inaba M., Naito M., Steinman R.M. Dendritic cell progenitors phagocytose particulates, including Bacillus Calmette–Guerin organisms, and sensitize mice to mycobacterial antigens in vivo. J. Exp. Med. 1993;178:479–488. doi: 10.1084/jem.178.2.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chadwick S., Kriegel C., Amiji M. Nanotechnology solutions for mucosal immunization. Adv. Drug Deliv. Rev. 2010;62:394–407. doi: 10.1016/j.addr.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 45.Kraehenbuhl J.P., Neutra M.R. Epithelial m cells: differentiation and function. Annu. Rev. Cell Dev. Biol. 2000;16:301–332. doi: 10.1146/annurev.cellbio.16.1.301. [DOI] [PubMed] [Google Scholar]
- 46.Kim D.Y., Sato A., Fukuyama S., Sagara H., Nagatake T., Kong I.G., Goda K., Nochi T., Kunisawa J., Sato S., Yokota Y., Lee C.H., Kiyono H. The airway antigen sampling system: respiratory m cells as an alternative gateway for inhaled antigens. J. Immunol. 2011;186:4253–4262. doi: 10.4049/jimmunol.0903794. [DOI] [PubMed] [Google Scholar]
- 47.Gupta R.K., Chang A.C., Siber G.R. Biodegradable polymer microspheres as vaccine adjuvants and delivery systems. Dev. Biol. Stand. 1998;92:63–78. [PubMed] [Google Scholar]
- 48.Lai S.K., Wang Y.Y., Hanes J. Mucus-penetrating nanoparticles for drug and gene delivery to mucosal tissues. Adv. Drug Deliv. Rev. 2009;61:158–171. doi: 10.1016/j.addr.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garg N.K., Mangal S., Khambete H., Tyagi R.K. Mucosal delivery of vaccines: role of mucoadhesive/biodegradable polymers. Recent Pat. Drug Deliv. Formul. 2010;4:114–128. doi: 10.2174/187221110791185015. [DOI] [PubMed] [Google Scholar]
- 50.Mishra N., Goyal A.K., Tiwari S., Paliwal R., Paliwal S.R., Vaidya B., Mangal S., Gupta M., Dube D., Mehta A., Vyas S.P. Recent advances in mucosal delivery of vaccines: role of mucoadhesive/biodegradable polymeric carriers. Expert Opin. Ther. Pat. 2010;20:661–679. doi: 10.1517/13543771003730425. [DOI] [PubMed] [Google Scholar]
- 51.Lehr C.M. Lectin-mediated drug delivery: the second generation of bioadhesives. J. Control. Release. 2000;65:19–29. doi: 10.1016/s0168-3659(99)00228-x. [DOI] [PubMed] [Google Scholar]
- 52.Alpar H.O., Somavarapu S., Atuah K.N., Bramwell V.W. Biodegradable mucoadhesive particulates for nasal and pulmonary antigen and DNA delivery. Adv. Drug Deliv. Rev. 2005;57:411–430. doi: 10.1016/j.addr.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 53.Mathiowitz E., Jacob J.S., Jong Y.S., Carino G.P., Chickering D.E., Chaturvedi P., Santos C.A., Vijayaraghavan K., Montgomery S., Bassett M., Morrell C. Biologically erodable microspheres as potential oral drug delivery systems. Nature. 1997;386:410–414. doi: 10.1038/386410a0. [DOI] [PubMed] [Google Scholar]
- 54.Dawson M., Krauland E., Wirtz D., Hanes J. Transport of polymeric nanoparticle gene carriers in gastric mucus. Biotechnol. Prog. 2004;20:851–857. doi: 10.1021/bp0342553. [DOI] [PubMed] [Google Scholar]
- 55.Shakya A.K., Nandakumar K.S. Applications of polymeric adjuvants in studying autoimmune responses and vaccination against infectious diseases. J. R. Soc. Interface. 2013;10:15. doi: 10.1098/rsif.2012.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brenza T., Petersen L., Zhang Y., Huntimer L., Ramer-Tait A., Hostetter J., Wannemuehler M., Narasimhan B. Pulmonary biodistribution and cellular uptake of intranasally administered monodisperse particles. Pharm. Res. 2015;32:1368–1382. doi: 10.1007/s11095-014-1540-y. [DOI] [PubMed] [Google Scholar]
- 57.Haughney S.L., Ross K., Boggiatto P., Wannemuehler M.J., Narasimhan B. Effect of nanovaccine chemistry on humoral immune response kinetics and maturation. Nanoscale. 2014;6:13770–13778. doi: 10.1039/c4nr03724c. [DOI] [PubMed] [Google Scholar]
- 58.Li A., Moon J., Abraham W., Suh H., Elkhader J., Seidman M., Yen M., Im E.-J., Foley M., Barouch D., Irvine D. Generation of effector memory t cell–based mucosal and systemic immunity with pulmonary nanoparticle vaccination. Sci. Transl. Med. 2013;5:204ra30. doi: 10.1126/scitranslmed.3006516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nembrini C., Stano A., Dane K., Ballester M., ven der Vlies A.J., Marsland B., Swartz M., Hubbell J. Nanoparticle conjugation of antigen enhances cytotoxic t-cell responses in pulmonary vaccination. Proc. Natl. Acad. Sci. U. S. A. 2011;108:E989–E997. doi: 10.1073/pnas.1104264108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nochi T., Yuki Y., Takahashi H., Sawada S.-I., Mejima M., Kohda T., Harada N., Kong I., Sato A., Kataoka N., Tokuhara D., Kurokawa S., Takahashi Y., Tsukada H., Kozaki S., Akiyoshi K., Kiyono H. Nanogel antigenic protein-delivery system for adjuvant-free intranasal vaccines. Nat. Mater. 2010;9:572–578. doi: 10.1038/nmat2784. [DOI] [PubMed] [Google Scholar]
- 61.Ross K., Haughney S., Petersen L., Boggiatto P., Wannemuehler M., Narasimhan B. Deposition and uptake behavior of pathogen-mimicking nanovaccines in the first 48 hours. Adv. Healthcare Mater. 2014;3:1071–1077. doi: 10.1002/adhm.201300525. [DOI] [PubMed] [Google Scholar]
- 62.Seong S., Matzinger P. Hydrophobicity: an ancient damage-associated molecular pattern that initiates innate immune responses. Nat. Rev. Immunol. 2004;4:469–478. doi: 10.1038/nri1372. [DOI] [PubMed] [Google Scholar]
- 63.Rytting E., Nguyen J., Wang X., Kissel T. Biodegradable polymeric nanocarriers for pulmonary drug delivery. Expert Opin. Drug Deliv. 2008;5:629–639. doi: 10.1517/17425247.5.6.629. [DOI] [PubMed] [Google Scholar]
- 64.Malyala P., Chesko J., Ugozzoli M., Goodsell A., Zhou F., Vajdy M., O'Hagan D.T., Singh M. The potency of the adjuvant, cpg oligos, is enhanced by encapsulation in plg microparticles. J. Pharm. Sci. 2008;97:1155–1164. doi: 10.1002/jps.21065. [DOI] [PubMed] [Google Scholar]
- 65.Bolhassani A., Safaiyan S., Rafati S. Improvement of different vaccine delivery systems for cancer therapy. Mol. Cancer. 2011;10:3. doi: 10.1186/1476-4598-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thomas C., Rawat A., Hope-Weeks L., Ahsan F. Aerosolized pla and plga nanoparticles enhance humoral, mucosal and cytokine responses to hepatitis b vaccine. Mol. Pharm. 2011;8:405–415. doi: 10.1021/mp100255c. [DOI] [PubMed] [Google Scholar]
- 67.Semete B., Booysen L., Lemmer Y., Kalombo L., Katata L., Verschoor J., Swai H.S. In vivo evaluation of the biodistribution and safety of plga nanoparticles as drug delivery systems. Nanomedicine. 2010;6:662–671. doi: 10.1016/j.nano.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 68.Armstead A.L., Li B. Nanomedicine as an emerging approach against intracellular pathogens. Int. J. Nanomedicine. 2011;6:3281–3293. doi: 10.2147/IJN.S27285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Singh M., Briones M., O'Hagan D.T. A novel bioadhesive intranasal delivery system for inactivated influenza vaccines. J. Control. Release. 2001;70:267–276. doi: 10.1016/s0168-3659(00)00330-8. [DOI] [PubMed] [Google Scholar]
- 70.Baras B., Benoit M.A., Dupre L., Poulain-Godefroy O., Schacht A.M., Capron A., Gillard J., Riveau G. Single-dose mucosal immunization with biodegradable microparticles containing a Schistosoma mansoni antigen. Infect. Immun. 1999;67:2643–2648. doi: 10.1128/iai.67.5.2643-2648.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shephard M.J., Todd D., Adair B.M., Po A.L., Mackie D.P., Scott E.M. Immunogenicity of bovine parainfluenza type 3 virus proteins encapsulated in nanoparticle vaccines, following intranasal administration to mice. Res. Vet. Sci. 2003;74:187–190. doi: 10.1016/s0034-5288(02)00180-7. [DOI] [PubMed] [Google Scholar]
- 72.Gajewski T.F., Pinnas M., Wong T., Fitch F.W. Murine th1 and th2 clones proliferate optimally in response to distinct antigen-presenting cell populations. J. Immunol. 1991;146:1750–1758. [PubMed] [Google Scholar]
- 73.Binjawadagi B., Dwivedi V., Manickam C., Ouyang K., Torrelles J.B., Renukaradhya G.J. An innovative approach to induce cross-protective immunity against porcine reproductive and respiratory syndrome virus in the lungs of pigs through adjuvanted nanotechnology-based vaccination. Int. J. Nanomedicine. 2014;9:1519–1535. doi: 10.2147/IJN.S59924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Binjawadagi B., Dwivedi V., Manickam C., Ouyang K., Wu Y., Lee L.J., Torrelles J.B., Renukaradhya G.J. Adjuvanted poly(lactic-co-glycolic) acid nanoparticle-entrapped inactivated porcine reproductive and respiratory syndrome virus vaccine elicits cross-protective immune response in pigs. Int. J. Nanomedicine. 2014;9:679–694. doi: 10.2147/IJN.S56127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peek L.J., Middaugh C.R., Berkland C. Nanotechnology in vaccine delivery. Adv. Drug Deliv. Rev. 2008;60:915–928. doi: 10.1016/j.addr.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Azizi A., Kumar A., Diaz-Mitoma F., Mestecky J. Enhancing oral vaccine potency by targeting intestinal m cells. PLoS Pathog. 2010;6:e1001147. doi: 10.1371/journal.ppat.1001147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Manocha M., Pal P.C., Chitralekha K.T., Thomas B.E., Tripathi V., Gupta S.D., Paranjape R., Kulkarni S., Rao D.N. Enhanced mucosal and systemic immune response with intranasal immunization of mice with hiv peptides entrapped in plg microparticles in combination with Ulex europaeus-i lectin as m cell target. Vaccine. 2005;23:5599–5617. doi: 10.1016/j.vaccine.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 78.Gupta P.N., Khatri K., Goyal A.K., Mishra N., Vyas S.P. M-cell targeted biodegradable plga nanoparticles for oral immunization against hepatitis b. J. Drug Target. 2007;15:701–713. doi: 10.1080/10611860701637982. [DOI] [PubMed] [Google Scholar]
- 79.Nayak B., Panda A.K., Ray P., Ray A.R. Formulation, characterization and evaluation of rotavirus encapsulated pla and plga particles for oral vaccination. J. Microencapsul. 2009;26:154–165. doi: 10.1080/02652040802211709. [DOI] [PubMed] [Google Scholar]
- 80.Thomas C., Gupta V., Ahsan F. Influence of surface charge of plga particles of recombinant hepatitis b surface antigen in enhancing systemic and mucosal immune responses. Int. J. Pharm. 2009;379:41–50. doi: 10.1016/j.ijpharm.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 81.Yoshida M., Babensee J.E. Differential effects of agarose and poly(lactic-co-glycolic acid) on dendritic cell maturation. J. Biomed. Mater. Res. A. 2006;79:393–408. doi: 10.1002/jbm.a.30798. [DOI] [PubMed] [Google Scholar]
- 82.Nixon D.F., Hioe C., Chen P.D., Bian Z., Kuebler P., Li M.L., Qiu H., Li X.M., Singh M., Richardson J., McGee P., Zamb T., Koff W., Wang C.Y., O'Hagan D. Synthetic peptides entrapped in microparticles can elicit cytotoxic t cell activity. Vaccine. 1996;14:1523–1530. doi: 10.1016/s0264-410x(96)00099-0. [DOI] [PubMed] [Google Scholar]
- 83.Demento S.L., Cui W., Criscione J.M., Stern E., Tulipan J., Kaech S.M., Fahmy T.M. Role of sustained antigen release from nanoparticle vaccines in shaping the t cell memory phenotype. Biomaterials. 2012;33:4957–4964. doi: 10.1016/j.biomaterials.2012.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Blair D.A., Turner D.L., Bose T.O., Pham Q.M., Bouchard K.R., Williams K.J., McAleer J.P., Cauley L.S., Vella A.T., Lefrancois L. Duration of antigen availability influences the expansion and memory differentiation of t cells. J. Immunol. 2011;187:2310–2321. doi: 10.4049/jimmunol.1100363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kovacsovics-Bankowski M., Rock K.L. A phagosome-to-cytosol pathway for exogenous antigens presented on mhc class i molecules. Science. 1995;267:243–246. doi: 10.1126/science.7809629. [DOI] [PubMed] [Google Scholar]
- 86.Moon J.J., Suh H., Bershteyn A., Stephan M.T., Liu H., Huang B., Sohail M., Luo S., Um S.H., Khant H., Goodwin J.T., Ramos J., Chiu W., Irvine D.J. Interbilayer-crosslinked multilamellar vesicles as synthetic vaccines for potent humoral and cellular immune responses. Nat. Mater. 2011;10:243–251. doi: 10.1038/nmat2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Reddy S.T., van der Vlies A.J., Simeoni E., Angeli V., Randolph G.J., O'Neil C.P., Lee L.K., Swartz M.A., Hubbell J.A. Exploiting lymphatic transport and complement activation in nanoparticle vaccines. Nat. Biotechnol. 2007;25:1159–1164. doi: 10.1038/nbt1332. [DOI] [PubMed] [Google Scholar]
- 88.Heit A., Schmitz F., Haas T., Busch D.H., Wagner H. Antigen co-encapsulated with adjuvants efficiently drive protective t cell immunity. Eur. J. Immunol. 2007;37:2063–2074. doi: 10.1002/eji.200737169. [DOI] [PubMed] [Google Scholar]
- 89.Smith D.M., Simon J.K., Baker J.R., Jr. Applications of nanotechnology for immunology. Nat. Rev. Immunol. 2013;13:592–605. doi: 10.1038/nri3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schliehe C., Redaelli C., Engelhardt S., Fehlings M., Mueller M., van Rooijen N., Thiry M., Hildner K., Weller H., Groettrup M. Cd8-dendritic cells and macrophages cross-present poly(d,l-lactate-co-glycolate) acid microsphere-encapsulated antigen in vivo. J. Immunol. 2011;187:2112–2121. doi: 10.4049/jimmunol.1002084. [DOI] [PubMed] [Google Scholar]
- 91.Amorij J.P., Kersten G.F., Saluja V., Tonnis W.F., Hinrichs W.L., Slutter B., Bal S.M., Bouwstra J.A., Huckriede A., Jiskoot W. Towards tailored vaccine delivery: needs, challenges and perspectives. J. Control. Release. 2012;161:363–376. doi: 10.1016/j.jconrel.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 92.Carrillo-Conde B., Garza A., Anderegg J., Narasimhan B. Protein adsorption on biodegradable polyanhydride microparticles. J. Biomed. Mater. Res. A. 2010;95:40–48. doi: 10.1002/jbm.a.32815. [DOI] [PubMed] [Google Scholar]
- 93.Carrillo-Conde B., Schiltz E., Yu J., Minion F., Phillips G., Wannemuehler M.J., Narasimhan B. Encapsulation into amphiphilic polyanhydride microparticles stabilizes Yersinia pestis protein antigens. Acta Biomater. 2010;6:3110–3119. doi: 10.1016/j.actbio.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 94.Determan A.S., Graham J.R., Pfeiffer K.A., Narasimhan B. The role of microsphere fabrication methods on the stability and release kinetics of ovalbumin encapsulated in polyanhydride microspheres. J. Microencapsul. 2006;23:832–843. doi: 10.1080/02652040601033841. [DOI] [PubMed] [Google Scholar]
- 95.Determan A.S., Trewyn B.G., Lin V.S., Nilsen-Hamilton M., Narasimhan B. Encapsulation, stabilization, and release of bsa-fitc from polyanhydride microspheres. J. Control. Release. 2004;100:97–109. doi: 10.1016/j.jconrel.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 96.Kipper M.J., Shen E., Determan A., Narasimhan B. Design of an injectable system based on bioerodible polyanhydride microspheres for sustained drug delivery. Biomaterials. 2002;23:4405–4412. doi: 10.1016/s0142-9612(02)00181-3. [DOI] [PubMed] [Google Scholar]
- 97.Kipper M.J., Wilson J.H., Wannemuehler M.J., Narasimhan B. Single dose vaccine based on biodegradable polyanhydride microspheres can modulate immune response mechanism. J. Biomed. Med. Res. 2006;76:798–810. doi: 10.1002/jbm.a.30545. [DOI] [PubMed] [Google Scholar]
- 98.Lopac S.K., Torres M.P., Wilson-Welder J.H., Wannemuehler M.J., Narasimhan B. Effect of polymer chemistry and fabrication method on protein release and stability from polyanhydride microspheres. J. Biomed. Mater. Res. B. 2009;91:938–947. doi: 10.1002/jbm.b.31478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Petersen L., Ramer-Tait A., Broderick S., Kong C., Ulery B., Rajan K., Wannemuehler M.J., Narasimhan B. Activation of innate immune responses in a pathogen-mimicking manner by amphiphilic polyanhydride nanoparticle adjuvants. Biomaterials. 2011;32:6815–6822. doi: 10.1016/j.biomaterials.2011.05.063. [DOI] [PubMed] [Google Scholar]
- 100.Petersen L., Sackett C., Narasimhan B. A novel, high throughput method to study in vitro protein release from polymer nanospheres. J. Comb. Chem. 2010;12:51–56. doi: 10.1021/cc900116c. [DOI] [PubMed] [Google Scholar]
- 101.Petersen L., Sackett C., Narasimhan B. High throughput analysis of protein stability in polyanhydride nanoparticles. Acta Biomater. 2010;6:3873–3881. doi: 10.1016/j.actbio.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 102.Torres M.P., Determan A.S., Anderson G.L., Mallapragada S.K., Narasimhan B. Amphiphilic polyanhydrides for protein stabilization and release. Biomaterials. 2007;28:108–116. doi: 10.1016/j.biomaterials.2006.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ulery B., Kumar D., Ramer-Tait A., Wannemuehler M.J., Metzger D., Narasimhan B. Design of a protective single-dose intranasal nanoparticle-based vaccine platform for respiratory infectious diseases. PLoS One. 2011;6:e17642. doi: 10.1371/journal.pone.0017642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ulery B., Petersen L., Phanse Y., Kong C., Broderick S., Kumar D., Ramer-Tait A., Carrillo-Conde B., Bellaire B., Rajan K., Wannemuehler M.J., Narasimhan B. Rational design of “pathogen-mimicking” amphiphilic materials as nanoadjuvants. Sci. Rep. 2011;1:198. doi: 10.1038/srep00198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ulery B., Phanse Y., Sinha A., Wannemuehler M.J., Narasimhan B., Bellaire B. Polymer chemistry influences uptake of nanospheres by immune cells. Pharm. Res. 2009;26:683–690. doi: 10.1007/s11095-008-9760-7. [DOI] [PubMed] [Google Scholar]
- 106.Fu J., Fiegel J., Krauland E., Hanes J. New polymeric carriers for controlled drug delivery following inhalation or injection. Biomaterials. 2002;23:4425–4433. doi: 10.1016/s0142-9612(02)00182-5. [DOI] [PubMed] [Google Scholar]
- 107.Huntimer L., Wilson-Welder J.H., Ross K., Carrillo-Conde B., Pruisner L., Wang C., Narasimhan B., Wannemuehler M.J., Ramer-Tait A. Single immunization of a suboptimal dose of antigen encapsulated into polyanhydride microparticles promotes high titer and avid antibody responses. J. Biomed. Mater. Res. 2013;101B:91–98. doi: 10.1002/jbm.b.32820. [DOI] [PubMed] [Google Scholar]
- 108.Carrillo-Conde B., Schiltz E., Yu J., Minion F.C., Phillips G.J., Wannemuehler M.J., Narasimhan B. Encapsulation into amphiphilic polyanhydride microparticles stabilizes Yersinia pestis antigens. Acta Biomater. 2010;6:3110–3119. doi: 10.1016/j.actbio.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 109.Determan A.S., Wilson J.H., Kipper M.J., Wannemuehler M.J., Narasimhan B. Protein stability in the presence of polymer degradation products: consequences for controlled release formulations. Biomaterials. 2006;27:3312–3320. doi: 10.1016/j.biomaterials.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 110.Haughney S.L., Petersen L.K., Schoofs A.D., Ramer-Tait A.E., King J.D., Briles D.E., Wannemuehler M.J., Narasimhan B. Retention of structure, antigenicity, and biological function of pneumococcal surface protein a (pspa) released from polyanhydride nanoparticles. Acta Biomater. 2013;9:8262–8271. doi: 10.1016/j.actbio.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Petersen L., Phanse Y., Ramer-Tait A.E., Wannemuehler M.J., Narasimhan B. Amphiphilic polyanhydride nanoparticles stabilize Bacillus anthracis protective antigen. Mol. Pharm. 2012;9:874–882. doi: 10.1021/mp2004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ross K.A., Loyd H., Wu W., Huntimer L., Wannemuehler M.J., Carpenter S., Narasimhan B. Structural and antigenic stability of h5n1 hemagglutinin trimer upon release from polyanhydride nanoparticles. J. Biomed. Mater. Res. A. 2014;102:4161–4168. doi: 10.1002/jbm.a.35086. [DOI] [PubMed] [Google Scholar]
- 113.Petersen L., Xue L., Rajan K., Wannemuehler M., Narasimhan B. The simultaneous effect of polymer chemistry and device geometry on the in vitro activation of murine dendritic cells. Biomaterials. 2009;30:5131–5142. doi: 10.1016/j.biomaterials.2009.05.069. [DOI] [PubMed] [Google Scholar]
- 114.Torres M.P., Wilson-Welder J.H., Lopac S.K., Phanse Y., Carrillo-Conde B., Ramer-Tait A., Bellaire B., Wannemuehler M.J., Narasimhan B. Polyanhydride microparticles enhance dendritic cell antigen presentation and activation. Acta Biomater. 2011;7:2857–2864. doi: 10.1016/j.actbio.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Huntimer L.M., Ross K.A., Darling R.J., Winterwood N.E., Boggiatto P., Narasimhan B., Ramer-Tait A.E., Wannemuehler M. Polyanhydride nanovaccine platform enhances antigen-specific cytotoxic t cell responses. Technology. 2014;2:171–175. [Google Scholar]
- 116.Adams J.R., Goswami M., Pohl N.L.B., Mallapragada S.K. Synthesis and functionalization of virus-mimicking cationic block copolymers with pathogen-associated carbohydrates as potential vaccine adjuvants. RSC Adv. 2014;4:15655–15663. [Google Scholar]
- 117.Adams J.R., Haughney S.L., Mallapragada S.K. Effective polymer adjuvants for sustained delivery of protein subunit vaccines. Acta Biomater. 2015;14:104–114. doi: 10.1016/j.actbio.2014.11.050. [DOI] [PubMed] [Google Scholar]
- 118.Newman M.J., Todd C.W., Balasubramanian M. Design and development of adjuvant-active non-ionic block copolymers. J. Pharm. Sci. 1998;87:1357–1362. doi: 10.1021/js980072c. [DOI] [PubMed] [Google Scholar]
- 119.Arca H.C., Gunbeyaz M., Senel S. Chiosan-based systems for the delivery of vaccine antigens. Expert Rev. Vaccines. 2009;8:937–953. doi: 10.1586/erv.09.47. [DOI] [PubMed] [Google Scholar]
- 120.McNeela E.A., O'Connor D., Jabbal-Gill I., Davis S.S., Pizza M., Peppoloni S., Rappuoli R., Mills K.H. A mucosal vaccine against diphtheria: formulation of cross reacting material (crm(197)) of diphtheria toxin with chitosan enhances local and systemic antibody and th2 responses following nasal delivery. Vaccine. 2000;19:1188–1198. doi: 10.1016/s0264-410x(00)00309-1. [DOI] [PubMed] [Google Scholar]
- 121.Shibata Y., Foster L.A., Metzger W.J., Myrvik Q.N. Alveolar macrophage priming by intravenous administration of chitin particles, polymers of n-acetyl-d-glucosamine, in mice. Infect. Immun. 1997;65:1734–1741. doi: 10.1128/iai.65.5.1734-1741.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Aiba S. Studies on chitosan: 4. Lysozymic hydrolysis of partially n-acetylated chitosans. Int. J. Biol. Macromol. 1992;14:225–228. doi: 10.1016/s0141-8130(05)80032-7. [DOI] [PubMed] [Google Scholar]
- 123.Guermonprez P., Valladeau J., Zitvogel L., Thery C., Amigorena S. Antigen presentation and t cell stimulation by dendritic cells. Annu. Rev. Immunol. 2002;20:621–667. doi: 10.1146/annurev.immunol.20.100301.064828. [DOI] [PubMed] [Google Scholar]
- 124.Nagao G., Ishii K., Hirota K., Makino K., Terada H. Role of lipid rafts in innate immunity and phagocytosis of polystyrene latex microspheres. Colloids Surf. B: Biointerfaces. 2011;84:317–324. doi: 10.1016/j.colsurfb.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 125.Schully K.L., Sharma S., Peine K.J., Pesce J., Elberson M.A., Fonseca M.E., Prouty A.M., Bell M.G., Borteh H., Gallovic M., Bachelder E.M., Keane-Myers A., Ainslie K.M. Rapid vaccination using an acetalated dextran microparticulate subunit vaccine confers protection against triplicate challenge by Bacillus anthracis. Pharm. Res. 2013;30:1349–1361. doi: 10.1007/s11095-013-0975-x. [DOI] [PubMed] [Google Scholar]
- 126.Bowersock T.L., Hogesesh H., Suckow M., Guimond P., Martin S., Borie D., Torregrosa S., Park H., Park K. Oral vaccination of animals with antigens encapsulated in alginate microspheres. Vaccine. 1999;17:1804–1811. doi: 10.1016/s0264-410x(98)00437-x. [DOI] [PubMed] [Google Scholar]
- 127.Rydell N., Stertman L., Sjoholm I. Starch microparticles as vaccine adjuvants. Expert Opin. Drug Deliv. 2005;2:807–828. doi: 10.1517/17425247.2.5.807. [DOI] [PubMed] [Google Scholar]
- 128.Walpita P., Barr J., Sherman M., Basler C.F., Wang L. Vaccine potential of nipah virus-like particles. PLoS One. 2011;6:e18437. doi: 10.1371/journal.pone.0018437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lua L.H., Connors N.K., Sainsbury F., Chuan Y.P., Wibowo N., Middelberg A.P. Bioengineering virus-like particles as vaccines. Biotechnol. Bioeng. 2014;111:425–440. doi: 10.1002/bit.25159. [DOI] [PubMed] [Google Scholar]
- 130.Richert L.E., Servid A.E., Harmsen A.L., Rynda-Apple A., Han S., Wiley J.A., Douglas T., Harmsen A.G. A virus-like particle vaccine platform elicits heightened and hastened local lung mucosal antibody production after a single dose. Vaccine. 2012;30:3653–3665. doi: 10.1016/j.vaccine.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kola I., Landis J. Can the pharmaceutical industry reduce attrition rates? Nat. Rev. Drug Discov. 2004;3:711–715. doi: 10.1038/nrd1470. [DOI] [PubMed] [Google Scholar]
- 132.Mestas J., Hughes C.C. Of mice and not men: differences between mouse and human immunology. J. Immunol. 2004;172:2731–2738. doi: 10.4049/jimmunol.172.5.2731. [DOI] [PubMed] [Google Scholar]
- 133.Seok J., Warren H.S., Cuenca A.G., Mindrinos M.N., Baker H.V., Xu W., Richards D.R., McDonald-Smith G.P., Gao H., Hennessy L., Finnerty C.C., Lopez C.M., Honari S., Moore E.E., Minei J.P., Cuschieri J., Bankey P.E., Johnson J.L., Sperry J., Nathens A.B., Billiar T.R., West M.A., Jeschke M.G., Klein M.B., Gamelli R.L., Gibran N.S., Brownstein B.H., Miller-Graziano C., Calvano S.E., Mason P.H., Cobb J.P., Rahme L.G., Lowry S.F., Maier R.V., Moldawer L.L., Herndon D.N., Davis R.W., Xiao W., Tompkins R.G. Inflammation and L.S.C.R.P. host response to injury, genomic responses in mouse models poorly mimic human inflammatory diseases. Proc. Natl. Acad. Sci. U. S. A. 2013;110:3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Perrin S. Preclinical research: make mouse studies work. Nature. 2014;507:423–425. doi: 10.1038/507423a. [DOI] [PubMed] [Google Scholar]
- 135.Groneberg D.A., Witt C., Wagner U., Chung K.F., Fischer A. Fundamentals of pulmonary drug delivery. Respir. Med. 2003;97:382–387. doi: 10.1053/rmed.2002.1457. [DOI] [PubMed] [Google Scholar]
- 136.Chung H., Pamp S.J., Hill J.A., Surana N.K., Edelman S.M., Troy E.B., Reading N.C., Villablanca E.J., Wang S., Mora J.R., Umesaki Y., Mathis D., Benoist C., Relman D.A., Kasper D.L. Gut immune maturation depends on colonization with a host-specific microbiota. Cell. 2012;149:1578–1593. doi: 10.1016/j.cell.2012.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gupta U.D., Katoch V.M. Animal models of tuberculosis. Tuberculosis (Edinb.) 2005;85:277–293. doi: 10.1016/j.tube.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 138.Papin J.F., Wolf R.F., Kosanke S.D., Jenkins J.D., Moore S.N., Anderson M.P., Welliver R.C., Sr. Infant baboons infected with respiratory syncytial virus develop clinical and pathological changes that parallel those of human infants. Am. J. Physiol. Lung Cell. Mol. Physiol. 2013;304:L530–L539. doi: 10.1152/ajplung.00173.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Krejci J., Nechvatalova K., Blahutkova M., Faldyna M. The respiratory tract in pigs and its immune system: a review. Vet. Med. 2013;58:206–220. [Google Scholar]
- 140.Liebler-Tenorio E.M., Pabst R. Malt structure and function in farm animals. Vet. Res. 2006;37:257–280. doi: 10.1051/vetres:2006001. [DOI] [PubMed] [Google Scholar]
- 141.Sasseville V.G., Mankowski J.L., Baldessari A., Harbison C., Laing S., Kaliyaperumal S., Matz-Rensing K., Miller A.D., Schmidt L.D., Kaplan-Kees J., Dick E.J., Jr., Reader J.R., Liu D., Crawford L.K., Lane J.H., Corner S.M., Pardo I.D., Evans M.G., Murnane R., Terio K.A. Meeting report: emerging respiratory viral infections and nonhuman primate case reports. Vet. Pathol. 2013;50:1145–1153. doi: 10.1177/0300985813495898. [DOI] [PubMed] [Google Scholar]
- 142.Palermo R.E., Tisoncik-Go J., Korth M.J., Katze M.G. Old world monkeys and new age science: the evolution of nonhuman primate systems virology. ILAR J. 2013;54:166–180. doi: 10.1093/ilar/ilt039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kaushal D., Mehra S., Dideir P.J., Lackner A.A. The non-human primate model of tuberculosis. J. Med. Primatol. 2012;41:191–201. doi: 10.1111/j.1600-0684.2012.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jeyanathan M., Thanthrige-Don N., Afkhami S., Lai R., Damjanovic D., Zganiacz A., Feng X., Yao X.D., Rosenthal K.L., Fe Medina M., Gauldie J., Ertl H.C., Xing Z. Novel chimpanzee adenovirus-vectored respiratory mucosal tuberculosis vaccine: overcoming local anti-human adenovirus immunity for potent tb protection. Mucosal Immunol. 2015 doi: 10.1038/mi.2015.29. [DOI] [PubMed] [Google Scholar]
- 145.Yao Y., Bao L., Deng W., Xu L., Li F., Lv Q., Yu P., Chen T., Xu Y., Zhu H., Yuan J., Gu S., Wei Q., Chen H., Yuen K.Y., Qin C. An animal model of mers produced by infection of rhesus macaques with MERS coronavirus. J. Infect. Dis. 2014;209:236–242. doi: 10.1093/infdis/jit590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mayer A.E., Johnson J.B., Parks G.D. The neutralizing capacity of antibodies elicited by parainfluenza virus infection of African green monkeys is dependent on complement. Virology. 2014;460–461:23–33. doi: 10.1016/j.virol.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Matsuoka Y., Suguitan A., Jr., Orandle M., Paskel M., Boonnak K., Gardner D.J., Feldmann F., Feldmann H., Marino M., Jin H., Kemble G., Subbarao K. African green monkeys recapitulate the clinical experience with replication of live attenuated pandemic influenza virus vaccine candidates. J. Virol. 2014;88:8139–8152. doi: 10.1128/JVI.00425-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rockx B., Bossart K.N., Feldmann F., Geisbert J.B., Hickey A.C., Brining D., Callison J., Safronetz D., Marzi A., Kercher L., Long D., Broder C.C., Feldmann H., Geisbert T.W. A novel model of lethal Hendra virus infection in African green monkeys and the effectiveness of ribavirin treatment. J. Virol. 2010;84:9831–9839. doi: 10.1128/JVI.01163-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Jones B.G., Sealy R.E., Rudraraju R., Traina-Dorge V.L., Finneyfrock B., Cook A., Takimoto T., Portner A., Hurwitz J.L. Sendai virus-based rsv vaccine protects African green monkeys from rsv infection. Vaccine. 2012;30:959–968. doi: 10.1016/j.vaccine.2011.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Simoes E.A., DeVincenzo J.P., Boeckh M., Bont L., Crowe J.E., Jr., Griffiths P., Hayden F.G., Hodinka R.L., Smyth R.L., Spencer K., Thirstrup S., Walsh E.E., Whitley R.J. Challenges and opportunities in developing respiratory syncytial virus therapeutics. J. Infect. Dis. 2015;211(Suppl. 1):S1–S20. doi: 10.1093/infdis/jiu828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yang K., Varga S.M. Mucosal vaccines against respiratory syncytial virus. Curr. Opin. Virol. 2014;6:78–84. doi: 10.1016/j.coviro.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Warfel J.M., Beren J., Kelly V.K., Lee G., Merkel T.J. Nonhuman primate model of pertussis. Infect. Immun. 2012;80:1530–1536. doi: 10.1128/IAI.06310-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Subbarao K., Roberts A. Is there an ideal animal model for SARS? Trends Microbiol. 2006;14:299–303. doi: 10.1016/j.tim.2006.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zumbrun E.E. Mission critical: mobilization of essential animal models for Ebola, nipah, and machupo virus infections. Vet. Pathol. 2015;52:18–20. doi: 10.1177/0300985814556781. [DOI] [PubMed] [Google Scholar]
- 155.Henning L.N., Comer J.E., Stark G.V., Ray B.D., Tordoff K.P., Knostman K.A., Meister G.T. Development of an inhalational Bacillus anthracis exposure therapeutic model in cynomolgus macaques. Clin. Vaccine Immunol. 2012;19:1765–1775. doi: 10.1128/CVI.00288-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mett V., Lyons J., Musiychuk K., Chichester J.A., Brasil T. A plant produced plague vaccine candidate confers protection to monkeys. Vaccine. 2007;25:3014–3017. doi: 10.1016/j.vaccine.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 157.Pitt M.L. Public Workshop on Animal Models and Correlates of Protection for Plague Vaccines. Department of Health and Human Resources, Food and Drug Administration, and Center for Biologics Evlauation and Research; 2004. Non-human primates as a model for pneumonic plague. ( http://www.fda.gov/downloads/BiologicsBloodVaccines/NewsEvents/WorkshopsMeetingsConferences/TranscriptsMinutes/UCM054438.pdf) [Google Scholar]
- 158.Dhondt K.P., Horvat B. Henipavirus infections: lessons from animal models. Pathogens. 2013;2:264–287. doi: 10.3390/pathogens2020264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Niewiesk S. Current animal models: cotton rat animal model. Curr. Top. Microbiol. Immunol. 2009;330:89–110. doi: 10.1007/978-3-540-70617-5_5. [DOI] [PubMed] [Google Scholar]
- 160.Zhang Y., Niewiesk S., Li J. Small animal models for human metapneumovirus: cotton rat is more permissive than hamster and mouse. Pathogens. 2014;3:633–655. doi: 10.3390/pathogens3030633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Guvenel A.K., Chiu C., Openshaw P.J. Current concepts and progress in rsv vaccine development. Expert Rev. Vaccines. 2014;13:333–344. doi: 10.1586/14760584.2014.878653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Rockx B. Recent developments in experimental animal models of henipavirus infection. Pathog. Dis. 2014;71:199–206. doi: 10.1111/2049-632X.12149. [DOI] [PubMed] [Google Scholar]
- 163.Zhang N., Tang J., Lu L., Jiang S., Du L. Receptor-binding domain-based subunit vaccines against MERS–CoV. Virus Res. 2015;202:151–159. doi: 10.1016/j.virusres.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Oscherwitz J., Yu F., Jacobs J.L., Cease K.B. Recombinant vaccine displaying the loop-neutralizing determinant from protective antigen completely protects rabbits from experimental inhalation anthrax. Clin. Vaccine Immunol. 2013;20:341–349. doi: 10.1128/CVI.00612-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Gutting B.W., Marchette D., Sherwood R., Andrews G.A., Director-Myska A., Channel S.R., Wolfe D., Berger A.E., Mackie R.S., Watson B.J., Rukhin A. Modeling low-dose mortality and disease incubation period of inhalational anthrax in the rabbit. J. Theor. Biol. 2013;329:20–31. doi: 10.1016/j.jtbi.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 166.Enkirch T., von Messling V. Ferret models of viral pathogenesis. Virology. 2015;479-480C:259–270. doi: 10.1016/j.virol.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Margine I., Krammer F. Animal models for influenza viruses: implications for universal vaccine development. Pathogens. 2014;3:845–874. doi: 10.3390/pathogens3040845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xu L., Bao L., Deng W., Zhu H., Chen T., Lv Q., Li F., Yuan J., Xiang Z., Gao K., Xu Y., Huang L., Li Y., Liu J., Yao Y., Yu P., Yong W., Wei Q., Zhang L., Qin C. The mouse and ferret models for studying the novel avian-origin human influenza a (h7n9) virus. Virol. J. 2013;10:253. doi: 10.1186/1743-422X-10-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sutton T.C., Finch C., Shao H., Angel M., Chen H., Capua I., Cattoli G., Monne I., Perez D.R. Airborne transmission of highly pathogenic h7n1 influenza virus in ferrets. J. Virol. 2014;88:6623–6635. doi: 10.1128/JVI.02765-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Zhu H., Wang D., Kelvin D.J., Li L., Zheng Z., Yoon S.W., Wong S.S., Farooqui A., Wang J., Banner D., Chen R., Zheng R., Zhou J., Zhang Y., Hong W., Dong W., Cai Q., Roehrl M.H., Huang S.S., Kelvin A.A., Yao T., Zhou B., Chen X., Leung G.M., Poon L.L., Webster R.G., Webby R.J., Peiris J.S., Guan Y., Shu Y. Infectivity, transmission, and pathology of human-isolated h7n9 influenza virus in ferrets and pigs. Science. 2013;341:183–186. doi: 10.1126/science.1239844. [DOI] [PubMed] [Google Scholar]
- 171.Yen H.L., Liang C.H., Wu C.Y., Forrest H.L., Ferguson A., Choy K.T., Jones J., Wong D.D., Cheung P.P., Hsu C.H., Li O.T., Yuen K.M., Chan R.W., Poon L.L., Chan M.C., Nicholls J.M., Krauss S., Wong C.H., Guan Y., Webster R.G., Webby R.J., Peiris M. Hemagglutinin–neuraminidase balance confers respiratory–droplet transmissibility of the pandemic h1n1 influenza virus in ferrets. Proc. Natl. Acad. Sci. U. S. A. 2011;108:14264–14269. doi: 10.1073/pnas.1111000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Houser K.V., Pearce M.B., Katz J.M., Tumpey T.M. Impact of prior seasonal h3n2 influenza vaccination or infection on protection and transmission of emerging variants of influenza a(h3n2)v virus in ferrets. J. Virol. 2013;87:13480–13489. doi: 10.1128/JVI.02434-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kreijtz J.H., Kroeze E.J., Stittelaar K.J., de Waal L., van Amerongen G., van Trierum S., van Run P., Bestebroer T., Kuiken T., Fouchier R.A., Rimmelzwaan G.F., Osterhaus A.D. Low pathogenic avian influenza a(h7n9) virus causes high mortality in ferrets upon intratracheal challenge: a model to study intervention strategies. Vaccine. 2013;31:4995–4999. doi: 10.1016/j.vaccine.2013.06.071. [DOI] [PubMed] [Google Scholar]
- 174.Van Riel D., Munster V.J., de Wit E., Rimmelzwaan G.F., Fouchier R.A., Osterhaus A.D., Kuiken T. H5n1 virus attachment to lower respiratory tract. Science. 2006;312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 175.Paquette S.G., Huang S.S., Banner D., Xu L., Leomicronn A., Kelvin A.A., Kelvin D.J. Impaired heterologous immunity in aged ferrets during sequential influenza a h1n1 infection. Virology. 2014;464–465:177–183. doi: 10.1016/j.virol.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bossart K.N., Zhu G., Middleton D. A neutralizing human monoclonal antibody protects against lethal disease in a ferret model of acute nipah virus infection. PLoS Pathog. 2009;5:e1000642. doi: 10.1371/journal.ppat.1000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Chu Y.K., Ali G.D., Jia F., Li Q., Kelvin D., Couch R.C., Harrod K.S., Hutt J.A., Cameron C., Weiss S.R., Jonsson C.B. The SARS–CoV ferret model in an infection challenge study. Virology. 2008;374:151–163. doi: 10.1016/j.virol.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Weingartl H., Czub M., Czub S., Neufeld J., Marszal P., Gren J., Smith G., Jones S., Proulx R., Deschambault Y., Grudeski E., Andonov A., He R., Li Y., Copps J., Grolla A., Dick D., Berry J., Ganske S., Manning L., Cao J. Immunization with modified vaccinia virus Ankara-based recombinant vaccine against severe acute respiratory syndrome is associated with enhanced hepatitis in ferrets. J. Virol. 2004;78:12672–12676. doi: 10.1128/JVI.78.22.12672-12676.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronoavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 180.Czerkinsky C., Holmgren J. Topical immunization strategies. Mucosal Immunol. 2010;3:545–555. doi: 10.1038/mi.2010.55. [DOI] [PubMed] [Google Scholar]
- 181.Bailey M., Christoforidou Z., Lewis M.C. The evolutionary basis for differences between the immune systems of man, mouse, pig and ruminants. Vet. Immunol. Immunopathol. 2013;152:13–19. doi: 10.1016/j.vetimm.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 182.Wernersson R., Schierup M.H., Jorgensen F.G., Gorodkin J., Panitz F., Staerfeldt H.H., Christensen O.F., Mailund T., Hornshoj H., Klein A., Wang J., Liu B., Hu S.N., Dong W., Li W., Wong G.K.S., Yu J., Bendixen C., Fredholm M., Brunak S., Yang H.M., Bolund L. Pigs in sequence space: A 0.66 × coverage pig genome survey based on shotgun sequencing. BMC Genomics. 2005;6 doi: 10.1186/1471-2164-6-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Groenen M.A., Archibald A.L., Uenishi H., Tuggle C.K., Takeuchi Y., Rothschild M.F., Rogel-Gaillard C., Park C., Milan D., Megens H.J., Li S., Larkin D.M., Kim H., Frantz L.A., Caccamo M., Ahn H., Aken B.L., Anselmo A., Anthon C., Auvil L., Badaoui B., Beattie C.W., Bendixen C., Berman D., Blecha F., Blomberg J., Bolund L., Bosse M., Botti S., Bujie Z., Bystrom M., Capitanu B., Carvalho-Silva D., Chardon P., Chen C., Cheng R., Choi S.H., Chow W., Clark R.C., Clee C., Crooijmans R.P., Dawson H.D., Dehais P., De Sapio F., Dibbits B., Drou N., Du Z.Q., Eversole K., Fadista J., Fairley S., Faraut T., Faulkner G.J., Fowler K.E., Fredholm M., Fritz E., Gilbert J.G., Giuffra E., Gorodkin J., Griffin D.K., Harrow J.L., Hayward A., Howe K., Hu Z.L., Humphray S.J., Hunt T., Hornshoj H., Jeon J.T., Jern P., Jones M., Jurka J., Kanamori H., Kapetanovic R., Kim J., Kim J.H., Kim K.W., Kim T.H., Larson G., Lee K., Lee K.T., Leggett R., Lewin H.A., Li Y., Liu W., Loveland J.E., Lu Y., Lunney J.K., Ma J., Madsen O., Mann K., Matthews L., McLaren S., Morozumi T., Murtaugh M.P., Narayan J., Nguyen D.T., Ni P., Oh S.J., Onteru S., Panitz F., Park E.W., Park H.S., Pascal G., Paudel Y., Perez-Enciso M., Ramirez-Gonzalez R., Reecy J.M., Rodriguez-Zas S., Rohrer G.A., Rund L., Sang Y., Schachtschneider K., Schraiber J.G., Schwartz J., Scobie L., Scott C., Searle S., Servin B., Southey B.R., Sperber G., Stadler P., Sweedler J.V., Tafer H., Thomsen B., Wali R., Wang J., Wang J., White S., Xu X., Yerle M., Zhang G., Zhang J., Zhang J., Zhao S., Rogers J., Churcher C., Schook L.B. Analyses of pig genomes provide insight into porcine demography and evolution. Nature. 2012;491:393–398. doi: 10.1038/nature11622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Mendicino M., Ramsoondar J., Phelps C., Vaught T., Ball S., LeRoith T., Monahan J., Chen S., Dandro A., Boone J., Jobst P., Vance A., Wertz N., Bergman Z., Sun X.Z., Polejaeva I., Butler J., Dai Y., Ayares D., Wells K. Generation of antibody- and b cell-deficient pigs by targeted disruption of the j-region gene segment of the heavy chain locus. Transgenic Res. 2011;20:625–641. doi: 10.1007/s11248-010-9444-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Phelps C.J., Ball S.F., Vaught T.D., Vance A.M., Mendicino M., Monahan J.A., Walters A.H., Wells K.D., Dandro A.S., Ramsoondar J.J., Cooper D.K., Ayares D.L. Production and characterization of transgenic pigs expressing porcine ctla4-ig. Xenotransplantation. 2009;16:477–485. doi: 10.1111/j.1399-3089.2009.00533.x. [DOI] [PubMed] [Google Scholar]
- 186.Luo Y., Lin L., Bolund L., Jensen T.G., Sorensen C.B. Genetically modified pigs for biomedical research. J. Inherit. Metab. Dis. 2012;35:695–713. doi: 10.1007/s10545-012-9475-0. [DOI] [PubMed] [Google Scholar]
- 187.Suzuki S., Iwamoto M., Saito Y., Fuchimoto D., Sembon S., Suzuki M., Mikawa S., Hashimoto M., Aoki Y., Najima Y., Takagi S., Suzuki N., Suzuki E., Kubo M., Mimuro J., Kashiwakura Y., Madoiwa S., Sakata Y., Perry A.C., Ishikawa F., Onishi A. Il2rg gene-targeted severe combined immunodeficiency pigs. Cell Stem Cell. 2012;10:753–758. doi: 10.1016/j.stem.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 188.Yang G., Artiaga B.L., Hackmann T.J., Samuel M.S., Walters E.M., Salek-Ardakani S., Driver J.P. Targeted disruption of cd1d prevents nkt cell development in pigs. Mamm. Genome. 2015;26:264–270. doi: 10.1007/s00335-015-9564-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Satyananda V., Hara H., Ezzelarab M.B., Phelps C., Ayares D., Cooper D.K. New concepts of immune modulation in xenotransplantation. Transplantation. 2013;96:937–945. doi: 10.1097/TP.0b013e31829bbcb2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kuzmuck K., Schook L. Pigs as a model for biomedical sciences. In: Rothschild M., Ruvinsky A., editors. The Genetics of the Pig. 2nd ed. AB International; Oxfordshire, UK: 2011. pp. 426–444. [Google Scholar]
- 191.Lunney J.K. Advances in swine biomedical model genomics. Int. J. Biol. Sci. 2007;3:179–184. doi: 10.7150/ijbs.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kuzmuck K., Schook L. Pigs as a model for biomedical sciences. In: Rothschild M., Ruvinsky A., editors. The Genetics of the Pig. 2nd ed. CAB International; Oxfordshire, UK: 2011. pp. 426–444. [Google Scholar]
- 193.Humphray S.J., Scott C.E., Clark R., Marron B., Bender C., Camm N., Davis J., Jenks A., Noon A., Patel M., Sehra H., Yang F., Rogatcheva M.B., Milan D., Chardon P., Rohrer G., Nonneman D., de Jong P., Meyers S.N., Archibald A., Beever J.E., Schook L.B., Rogers J. A high utility integrated map of the pig genome. Genome Biol. 2007;8:R139. doi: 10.1186/gb-2007-8-7-r139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Mair K.H., Sedlak C., Kaser T., Pasternak A., Levast B., Gerner W., Saalmuller A., Summerfield A., Gerdts V., Wilson H.L., Meurens F. The porcine innate immune system: an update. Dev. Comp. Immunol. 2014;45:321–343. doi: 10.1016/j.dci.2014.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Choi H.K., Finkbeiner W.E., Widdicombe J.H. A comparative study of mammalian tracheal mucous glands. J. Anat. 2000;197(Pt 3):361–372. doi: 10.1046/j.1469-7580.2000.19730361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Cunningham S., Meng Q.H., Klein N., McAnulty R.J., Hart S.L. Evaluation of a porcine model for pulmonary gene transfer using a novel synthetic vector. J. Gene Med. 2002;4:438–446. doi: 10.1002/jgm.270. [DOI] [PubMed] [Google Scholar]
- 197.Hayden F.G., Fritz R., Lobo M.C., Alvord W., Strober W., Straus S.E. Local and systemic cytokine responses during experimental human influenza a virus infection. Relation to symptom formation and host defense. J. Clin. Invest. 1998;101:643–649. [Google Scholar]
- 198.Ballard S.T., Trout L., Garrison J., Inglis S.K. Ionic mechanism of forskolin-induced liquid secretion by porcine bronchi. Am. J. Physiol. Lung Cell. Mol. Physiol. 2006;290:L97–104. doi: 10.1152/ajplung.00159.2005. [DOI] [PubMed] [Google Scholar]
- 199.Ballard S.T., Inglis S.K. Liquid secretion properties of airway submucosal glands. J. Physiol. 2004;556:1–10. doi: 10.1113/jphysiol.2003.052779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Inglis S.K., Corboz M.R., Taylor A.E., Ballard S.T. Regulation of ion transport across porcine distal bronchi. Am. J. Physiol. 1996;270:L289–L297. doi: 10.1152/ajplung.1996.270.2.L289. [DOI] [PubMed] [Google Scholar]
- 201.Baskerville A. Development of the early lesions in experimental enzootic pneumonia of pigs: an ultrastructural and histological study. Res. Vet. Sci. 1972;13:570–578. [PubMed] [Google Scholar]
- 202.Rogers C.S., Stoltz D.A., Meyerholz D.K., Ostedgaard L.S., Rokhlina T., Taft P.J., Rogan M.P., Pezzulo A.A., Karp P.H., Itani O.A., Kabel A.C., Wohlford-Lenane C.L., Davis G.J., Hanfland R.A., Smith T.L., Samuel M., Wax D., Murphy C.N., Rieke A., Whitworth K., Uc A., Starner T.D., Brogden K.A., Shilyansky J., McCray P.B., Jr., Zabner J., Prather R.S., Welsh M.J. Disruption of the cftr gene produces a model of cystic fibrosis in newborn pigs. Science. 2008;321:1837–1841. doi: 10.1126/science.1163600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Dee S.A., Joo H.S., Park B.K., Molitor T.W., Bruna G. Attempted elimination of porcine reproductive and respiratory syndrome virus from a seedstock farm by vaccination of the breeding herd and nursery depopulation. Vet. Rec. 1998;142:569–572. doi: 10.1136/vr.142.21.569. [DOI] [PubMed] [Google Scholar]
- 204.Qi X., Lu C. Swine influenza virus: evolution mechanism and epidemic characterization–a review. Wei Sheng Wu Xue Bao. 2009;49:1138–1145. [PubMed] [Google Scholar]
- 205.Yassine H.M., Lee C.W., Gourapura R., Saif Y.M. Interspecies and intraspecies transmission of influenza a viruses: viral, host and environmental factors. Anim. Health Res. Rev. 2010;11:53–72. doi: 10.1017/S1466252310000137. [DOI] [PubMed] [Google Scholar]
- 206.Van Reeth K., Van Gucht S., Pensaert M. Correlations between lung proinflammatory cytokine levels, virus replication, and disease after swine influenza virus challenge of vaccination-immune pigs. Viral Immunol. 2002;15:583–594. doi: 10.1089/088282402320914520. [DOI] [PubMed] [Google Scholar]
- 207.Khatri M., Dwivedi V., Krakowka S., Manickam C., Ali A., Wang L., Qin Z., Renukaradhya G.J., Lee C.W. Swine influenza h1n1 virus induces acute inflammatory immune responses in pig lungs: a potential animal model for human h1n1 influenza virus. J. Virol. 2010;84:11210–11218. doi: 10.1128/JVI.01211-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Hirschberg H.J., van Riet E., Oosterhoff D., Bouwstra J.A., Kersten G.F. Animal models for cutaneous vaccine delivery. Eur. J. Pharm. Sci. 2015;71:112–122. doi: 10.1016/j.ejps.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 209.Rajao D.S., Vincent A.L. Swine as a model for influenza a virus infection and immunity. ILAR J. 2015;56:44–52. doi: 10.1093/ilar/ilv002. [DOI] [PubMed] [Google Scholar]
- 210.Hein W.R., Griebel P.J. A road less travelled: large animal models in immunological research. Nat. Rev. Immunol. 2003;3:79–84. doi: 10.1038/nri977. [DOI] [PubMed] [Google Scholar]
- 211.Dwivedi V., Manickam C., Binjawadagi B., Joyappa D., Renukaradhya G.J. Biodegradable nanoparticle-entrapped vaccine induces cross-protective immune response against a virulent heterologous respiratory viral infection in pigs. PLoS One. 2012;7:e51794. doi: 10.1371/journal.pone.0051794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Miyake A., Akagi T., Enose Y., Ueno M., Kawamura M., Horiuchi R., Hiraishi K., Adachi M., Serizawa T., Narayan O., Akashi M., Baba M., Hayami M. Induction of hiv-specific antibody response and protection against vaginal shiv transmission by intranasal immunization with inactivated shiv-capturing nanospheres in macaques. J. Med. Virol. 2004;73:368–377. doi: 10.1002/jmv.20100. [DOI] [PubMed] [Google Scholar]
- 213.Renukaradhya G.J., Meng X.J., Calvert J.G., Roof M., Lager K.M. Inactivated and subunit vaccines against porcine reproductive and respiratory syndrome: current status and future direction. Vaccine. 2015 doi: 10.1016/j.vaccine.2015.04.102. [DOI] [PubMed] [Google Scholar]
- 214.Dwivedi V., Manickam C., Binjawadagi B., Renukaradhya G.J. Plga nanoparticle entrapped killed porcine reproductive and respiratory syndrome virus vaccine helps in viral clearance in pigs. Vet. Microbiol. 2013;166:47–58. doi: 10.1016/j.vetmic.2013.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Dwivedi V., Manickam C., Patterson R., Dodson K., Murtaugh M., Torrelles J.B., Schlesinger L.S., Renukaradhya G.J. Cross-protective immunity to porcine reproductive and respiratory syndrome virus by intranasal delivery of a live virus vaccine with a potent adjuvant. Vaccine. 2011;29:4058–4066. doi: 10.1016/j.vaccine.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Ren J., Lu H., Wen S., Sun W., Yan F., Chen X., Jing J., Liu H., Liu C., Xue F., Xiao P., Xin S., Jin N. Enhanced immune responses in pigs by DNA vaccine coexpressing gp3 and gp5 of European type porcine reproductive and respiratory syndrome virus. J. Virol. Methods. 2014;206:27–37. doi: 10.1016/j.jviromet.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 217.Diaz I., Darwich L., Pappaterra G., Pujols J., Mateu E. Immune responses of pigs after experimental infection with a European strain of porcine reproductive and respiratory syndrome virus. J. Gen. Virol. 2005;86:1943–1951. doi: 10.1099/vir.0.80959-0. [DOI] [PubMed] [Google Scholar]
- 218.Takikawa N., Kobayashi S., Ide S., Yamane Y., Tanaka Y., Yamagishi H. Detection of antibodies against porcine reproductive and respiratory syndrome (prrs) virus in swine sera by enzyme-linked immunosorbent assay. J. Vet. Med. Sci. 1996;58:355–357. doi: 10.1292/jvms.58.355. [DOI] [PubMed] [Google Scholar]
- 219.Spellberg B., Edwards J.E., Jr. Type 1/type 2 immunity in infectious diseases. Clin. Infect. Dis. 2001;32:76–102. doi: 10.1086/317537. [DOI] [PubMed] [Google Scholar]
- 220.Taylor G. Bovine model of respiratory syncytial virus infection. Curr. Top. Microbiol. Immunol. 2013;372:327–345. doi: 10.1007/978-3-642-38919-1_16. [DOI] [PubMed] [Google Scholar]
- 221.Ackermann M.R. Lamb model of respiratory syncytial virus-associated lung disease: insights to pathogenesis and novel treatments. ILAR J. 2014;55:4–15. doi: 10.1093/ilar/ilu003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Kroeze E.J., Kuiken T., Osterhaus A.D. Animal models. Methods Mol. Biol. 2012;865:127–146. doi: 10.1007/978-1-61779-621-0_8. [DOI] [PubMed] [Google Scholar]