Abstract
Background
Prescription opioid abuse and overdose has steadily increased in the United States (U.S.) over the past two decades and current research has shown a dramatic increase in hospitalizations resulting from opioid poisonings. Still, much is unknown about the clinical and demographic features of patients presenting to emergency departments for poisoning from prescription drugs.
Objective
We sought to evaluate ED visits by adults for prescription opioids.
Methods
This was a retrospective cohort study utilizing 2006 – 2011 data from the Nationwide Emergency Department Sample (NEDS). Total number of admissions (weighted), disposition, gender, age, expected payer, income, geographic region, charges, and procedures performed were examined.
Results
From 2006 – 2010, there were 259,093 ED visits by adults for poisoning by opioids and 53.50% of these were unintentional. The overall mean age of patients was 45.5 with more visits made by females (52.37%). Patients who unintentionally overdosed were more likely to have Medicare (36.54%), whereas those who intentionally overdosed had private insurance (29.41%). The majority of patients reside in the South (40.93%) and come from lower-income neighborhoods. Approximately 108,504 patients were discharged and 140,395 were admitted.
Conclusions
There were over 250,000 visits to U.S. EDs from 2006 – 2011 with a primary diagnosis of poisoning by a prescription opioid. The majority of visits were made by females and over half were admitted to the hospital, resulting in over $4 billion in charges. Future studies should examine preventative measures, optimal screening and intervention programs for these patients.
INTRODUCTION
Opioid abuse and overdose has steadily increased in the United States (U.S.) for over two decades. Opioid overdose-related deaths have quadrupled between 1990 and 20101 and it is estimated that roughly 100 people die each day from opioid-related overdoses.2,3 Unintentional poisoning now represents the leading cause of injury death in the U.S for adults ages 25–64.4,5 Of unintentional poisonings, the vast majority are related to prescription and illicit opioid overdoses.2,3,6 In particular, prescription opioid medications seem to confer a major risk to those affected by opioid dependency. These prescriptions, which are often written legitimately for pain control, may be stolen by family members, sold on the street, or taken in excess quantities by the patient themselves.2
In the mid-1990’s, the American Pain Society and the American Academy of Anesthesiologists developed position statements supporting increased use of opioids to treat pain and laws were enacted to protect physicians prescribing such medications. A general movement towards adequate and appropriate pain control management for patients occurred when the Joint Commission created pain management standards in 2001.7 After these policies went into effect, there was a 300% increase in the sale of prescription opioids in the U.S., with enough prescription painkillers to medicate every American adult for one month in 2010.2
Though prescribed painkillers are intended for treatment and pain control,5 the repercussions of the aforementioned policies and position statements have shown to be associated with increased opioid medication addiction, abuse and unintentional poisoning.8,9,10 In 2010, the National Institute of Drug Abuse (NIDA) revealed that approximately seven million Americans reported of prescription drug abuse within 30 days,11 with opioids outranking stimulants and sedatives by five- and two-fold, respectively.12
A recent paper by Coben et al. showed a dramatic increase in hospitalizations resulting from poisoning by prescription opioids, sedatives and tranquilizers between 1999 and 2006.3 However, less information exists about emergency department (ED) visits for poisonings from these substances. Further insight into the unique features of this population may shed light on which populations are most at risk for opioid abuse and provide critical information about the magnitude of the problem. The objective of the current study was to examine the number of ED visits related to poisoning by prescription opioids and describe the sociodemographic and clinical features of this population.
METHODS
This was retrospective cohort study using five years of data (2006 – 2011) from the Nationwide Emergency Department Sample (NEDS)—a database that is part of the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.13 The NEDS is a 20% stratified, multi-stage sample designed to represent national estimates of U.S. ED visits each year. It contains over 26 million records from ED visits from 950 hospitals in the U.S. and is the largest U.S. all-payer ED database.13 Hospital-based EDs that are selected to contribute data to the NEDS is determined by HCUP to represent all of the U.S.13 The NEDS The current study was deemed “not human subjects research” by our institutions’ IRB since information contained in the NEDS is de-identified.
The following ICD-9-CM codes for prescription opioids were included: 965.02 (methadone); 965.09 (other narcotics including codeine, meperidine, morphine). These ICD-9 codes cover poisoning by a prescription opioid medications and do not include heroine. Intentionality was determined by the presence of an External Cause of Injury Code (e-code) in the E850–E858 range (accidental poisonings by drugs, medicinal substances, and biologicals). These cases represent ED visits where prescription drug poisoning was listed as the primary diagnosis.
We also examined the number of admissions, disposition, gender, age, expected payer, income, geographic region, mean and total charges, and procedures performed. SAS-Callable SUDAAN software was used to create unbiased standard errors and to produce weighted estimates. Differences were considered statistically significant (p<.05) if confidence intervals did not overlap.
RESULTS
Demographics
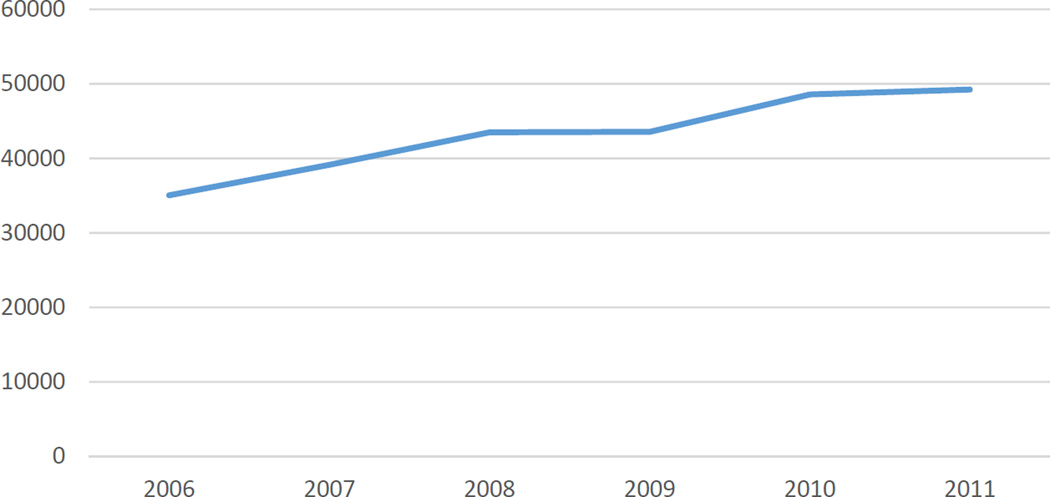
From 2006 – 2011, there were an estimated 259,093 ED adult visits for poisoning by opioids, with 53.50% being unintentional. The number of ED visits by year is represented in Figure 1, representing a steady increase annually. The mean age of the sample was 45.5 (SE=0.12) (Table 1). On average, females were significantly older (47.6; 47.3 – 47.9; SE=0.14 versus 43.2; 42.9 – 43.5; SE=0.14) and accounted for more of the visits (52.36% versus 47.63%) (Table 1). ED visits for opioid poisoning by patients in the 18 – 30 age group was significantly higher than all other age categories (Table 2). Additionally, significantly more patients were admitted to the same hospital (54.19%). The lowest number of ED visits for opioid poisoning was from patients living in the highest quartile neighborhoods (≥ $63,000) (16.41%) and overall, significantly more visits were made by patients with Medicare (29.60%) (Table 1). The majority of visits occurred in the South (40.93%) compared to all other regions.
Figure 1.
Table 1.
Demographic characteristics of adult patients presenting to U.S. EDs for prescription opioid poisonings from 2006 – 2011
| Characteristic | N% |
|---|---|
| Total Number | 259,093 |
| Age, years | 45.5 |
| Gender | |
| Male | 123,399 (47.63) |
| Female | 135,654 (52.36)↑ |
| Payer | |
| Medicare | 76,700 (29.60)↑ |
| Medicaid | 54,569 (21.06) |
| Private insurance | 62,453 (24.10) |
| Self-pay | 49,116 (18.96) |
| Other/No charge | 15,300 (5.91) |
| Income‡ | |
| 1st quartile | 73,876 (28.51) |
| 2nd quartile | 74,126 (28.61) |
| 3rd quartile | 60,628 (23.40) |
| 4th quartile | 42,510 (16.41)↓ |
| Region of Hospital | |
| Northeast | 36,477 (14.08) |
| Midwest | 53,976 (20.83) |
| South | 106,048 (40.93)↑ |
| West | 62,591 (24.16) |
| Type of ED Event | |
| Treated and Released | 108,504 (41.88) |
| Admitted | 140,395 (54.19)↑ |
ED = emergency department
Estimates are weighted numbers of visits
Percentages are column percentages
Numbers may not add to 100% due to missing data
Significantly higher (p < .05) than all other categories
Significantly lower (p < .05) than all other categories
Estimated median household income of residents in the patient's ZIP Code; 1st quartile = ≤ $38,999; 2nd quartile =$39,000–$47,999; 3rd quartile $48,000–$62,999; 4th quartile ≥$63,000.
Table 2.
Intentionality for prescription drug poisonings by age category (N = 259,093)
| Age Category | Total | Unintentional† n (%) |
Intentional n (%) |
Undetermined n (%) |
|---|---|---|---|---|
| 18 – 30 | 60,709* | 26,269 (43.27) | 20,935 (34.48) | 13,505 (22.24) |
| 31 – 40 | 42,197 | 18,508 (43.86) | 14,490 (34.34) | 9,199 (21.80) |
| 41 – 50 | 56,900 | 28,257 (49.66) | 16,824 (29.57) | 11,819 (20.77) |
| 51 – 60 | 52,548 | 31,284 (59.53) | 11,109 (21.14) | 10,154 (19.32) |
| 61 – 70 | 26,146 | 18,492 (70.72) | 3,368 (12.88) | 4,286 (16.39) |
| 71 – 80 | 12,640 | 9,537 (75.46) | 1,189 (9.41) | 1,913 (15.13) |
| 81 – 90 | 6,886 | 5,385 (78.21) | 665 (9.65) | 836 (12.14) |
| 91 – 100 | 1,046 | 862 (82.40) | 60 (5.72) | 124 (11.85) |
Estimates are weighted numbers of visits
Percentages are row percentages
Numbers may not add to 100% due to missing data
Age category was significantly higher than all other categories
All percentages in category are significantly higher
Intentionality
Poisonings were classified from this data as either “unintentional,” “intentional,” or “undetermined.” Of the 259,093 ED visits for poisonings between 2006 and 2011, 26.5% were intentional, whereas 53.50% were unintentional and 20.0% undetermined (Table 3). Significantly more females were classified as both unintentional (52.67%) and intentional (54.95%). When comparing payment source, Medicare was significantly higher for unintentional overdoses (36.41%) and private insurance was higher for intentional overdoses (29.29%). Additionally, the 4th quartile income level remained significantly lower and admission rates remained higher for both unintentional and intentional poisonings.
Table 3.
Demographic characteristics of adult patients by intentionality for prescription opioid poisonings from 2006 – 2011 (N = 259,093)
| Characteristic | Unintentional n (%) |
Intentional n (%) |
Undetermined n (%) |
|---|---|---|---|
| Total | 138,603 (53.50) | 68,641 (26.5) | 51,849 (20.0) |
| Gender | |||
| Male | 65,574 (47.31) | 30,916 (45.04) | 26,908 (51.90) |
| Female | 73,005 (52.67)↑ | 37,717 (54.95)↑ | 24,932 (48.09) |
| Payer | |||
| Medicare | 50,463 (36.41)↑ | 12,733 (18.55) | 13,504 (26.04) |
| Medicaid | 27,734 (20.01) | 14,771 (21.52) | 12,064 (23.27) |
| Private insurance | 31,261 (22.55) | 20,106 (29.29)↑ | 11,086 (21.38) |
| Self-pay | 21,462 (15.48) | 15,921 (23.19) | 11,732 (22.63) |
| Other/No charge | 7,182 (5.18) | 4,838 (7.05) | 3,282 (6.33) |
| Income ‡ | |||
| 1st quartile | 38,567 (27.83) | 18,996 (27.67) | 16,312 (3.15) |
| 2nd quartile | 39,149 (28.25) | 19,871 (28.95) | 15,105 (29.13) |
| 3rd quartile | 32,937 (23.76) | 16,242 (23.66) | 11,449 (22.08) |
| 4th quartile | 23,552 (16.99)↓ | 11,513 (16.77)↓ | 7,445 (14.36) |
| Type of ED Event | |||
| Treated & Released | 57,049 (41.16) | 27,768 (40.45) | 23,687 (45.68) |
| Admitted | 79,109 (57.08)↑ | 35,829 (52.20)↑ | 25,458 (49.10) |
Estimates are weighted numbers of visits
Percentages are column percentages
Numbers may not add to 100% due to missing data
Significantly higher (p < .05) than all other categories
Significantly lower (p < .05) than all other categories
Estimated median household income of residents in the patient's ZIP Code; 1st quartile = ≤ $38,999; 2nd quartile = $39,000–$47,999; 3rd quartile $48,000–$62,999; 4th quartile ≥ $63,000.
Age categories, ranging from 18 to 100 years, were compared with all three classifications of intentionality. Although unintentional poisonings were significantly higher in all age categories compared to intentional and undetermined, the number of these poisonings increased with age (Table 2) Likewise, the total number of intentional poisonings decreased with increasing age.
Charges, Diagnoses and Procedures
The average charge per visit was $3,515.27 for those discharged and $27,491.87 for those admitted. The total charges over the entire five year period for visits resulting in discharge from the ED $381,420,856.08 and $3,859,721,088.65 for admissions.
Poisoning by psychotropic agents or other medications and drugs, as well as substance-related disorders, were the top primary diagnoses of ED visits (Table 4). The top 10 primary procedures included an indwelling catheter, intubation and head CT (Table 4).
Table 4.
Primary procedures and diagnoses for adult patients by prescription opioid poisonings 2006 – 2011 (N = 259,093).
| 95% CI | ||||
|---|---|---|---|---|
| Top Primary Procedures | Rank | Estimate (%) |
Lower | Upper |
| Other therapeutic procedures | 1 | 35.39 | 30.43 | 40.68 |
| Other diagnostic procedures (interview; evaluation; consultation) | 2 | 19.20 | 15.57 | 23.43 |
| Indwelling catheter | 3 | 14.86 | 12.66 | 17.36 |
| Respiratory intubation and mechanical ventilation | 4 | 6.03 | 4.88 | 7.43 |
| Electrocardiogram | 5 | 3.91 | 2.44 | 6.21 |
| Computerized axial tomography (CT) scan head | 6 | 2.75 | 1.91 | 3.94 |
| Routine chest X-ray | 7 | 2.91 | 1.57 | 5.32 |
| Microscopic examination (bacterial smear/culture/toxicology) | 8 | 1.84 | 1.10 | 3.04 |
| Other vascular catheterization; not heart | 9 | 1.78 | 0.94 | 3.37 |
| Suture of skin and subcutaneous tissue | 10 | 1.19 | 0.85 | 1.67 |
| Top Primary Diagnoses | ||||
| Substance-related disorders | 1 | 87.24 | 86.13 | 88.27 |
| Poisoning by other mediations/drugs | 2 | 12.76 | 11.73 | 13.87 |
DISCUSSION
Our data show more than 250,000 visits to U.S. EDs between 2006 and 2011 for poisoning by prescribed opioids. A previous landmark study by Coben et al. using the Nationwide Inpatient Sample (NIS) found a 65% increase in U.S. hospitalizations for opioids as well as sedatives and tranquilizers between 1999 and 2006.3 Similarly, our findings revealed the number of ED visits in the U.S. due to prescription opioids jumped from 35,053 in 2006 to 49,227 in 2011. The current study complements the important work by Coben et al. by providing national data on ED visits due to prescription poisonings.
Research suggests that for every one person who dies from prescription opioid poisoning, there are 26 ED visits nationwide due to opioid misuse and another 733 people in the population not seeking medical attention for their abuse.14 Therefore, even large, national databases may underestimate the vast magnitude of national prescription opioid abuse.14 In 2008, approximately 20,044 deaths were attributed to prescription drug overdose, of which 14,800 (73.8%) resulted from prescribed opioids. This is far greater than the number of overdose deaths due to heroin and cocaine combined.14 Between 1999 and 2008, overdose deaths from opioid pain medications increased almost four-fold.15 Shockingly, Americans constitute only 4.6% of the world's overall population, but use 80% of the global opioid supply.16
Opioid abuse in the U.S. represents a growing public health threat. Elevated prevalence and risk factors associated with opioid abuse have been observed in some socioeconomic groups, specifically low income individuals and those living in rural areas of the U.S.2 While studies evaluating demographics of this population may help in targeting certain at-risk groups, a more unified effort, including changing the paradigm of opioid prescribing, is necessary to fully address this nationwide problem.2 For instance, it is possible that there were higher unintentional opioid poisonings among those who used Medicare, due to therapeutic misadventures as opposed to recreational abuse. Future programs may consider gender-specific interventions, as research has shown that women are more likely to be prescribed medications that have abuse potential and use such drugs for coping more so than men.17–18
Analysis of large-scale databases has revealed the growing problem of prescription drug abuse in the U.S. Our study adds additional information about the magnitude of this issue as well as healthcare utilization patterns and exorbitant costs of this public health crisis. The CDC currently recommends the development of state-wide electronic tracking systems to monitor distribution of prescription drugs in healthcare settings.2 This may hold medical providers accountable for prescribing beyond the necessary treatment level.2 Laws to prevent doctor shopping and drug diversion coupled with better access to treatment resources for patients is needed.2 Furthermore, the increase in the number of opioid treatment centers provides an ideal opportunity to conduct qualitative research with recovering opioid users to provide insight into the factors contributing to the start of their addictions.
LIMITATIONS
Because the ED visit is the unit of analysis in the NEDS as opposed to the individual patient, it is possible that patients were represented multiple times in our sample if they visited the hospital more than once for prescription overdose. Furthermore, the de-identified nature of the data precluded us from examining valuable information specific to the ED visit, such as provider notes and medications that the patients were currently prescribed. The reasons for unintentional visits were also unknown to us. For example, it was unclear from this data if an unintentional poisoning represented a recreational mishap or an over sedation from a prescribed pain medication, which may occur among cancer patients. This information would be valuable in further establishing a risk profile for patients who overdose from prescription drugs.
The classification of “undetermined intentionality” was assumed to be considered missing data or visits that were not coded as either “unintentional” or “intentional.” Outcomes of this study may have been different if there were less reports of undetermined classifications from the NEDS analysis. One of the limitations of using the NEDS database, is that this is a retrospective study and data was not originally collected for the purposes of this particular study, along with the possibility of miscoded data. Additionally, there is a possibility that the e-codes used were underutilized or incorrectly coded for these patients. This study only considered poisonings coded as being the first-listed diagnosis, so it is possible that these results may not reflect visits in which opioid poisonings were listed as secondary diagnosis.19 Also, the estimated charge data may not equal the actual costs of these visits, as the NEDS only provides charge data.19
CONCLUSION
There were over 250,000 visits to EDs in the U.S. from 2006–2011 with a primary diagnosis of poisoning by a prescription opioid. The majority of the patients were female and over half were admitted to the hospital. The charges for ED visits and subsequent hospitalizations totaled $4 billion during the five-year period. One-half of cases were unintentional. This information can be used for focused behavioral and withdrawal support programs that may be gender-specific, along with targeted anti-drug campaigns. Future studies should examine how to best prevent such poisonings and determine optimal screening and intervention programs for these patients. Likewise, further research is suggested for physician opioid prescribing patterns, opioid abuse risk factors beyond general demographics, and interventions for those already afflicted by opioid dependence.
ARTICLE SUMMARY.
1. Why is this topic important?
It is estimated that roughly 100 people die each day from opioid-related overdoses.2 A recent study has shown dramatic increase in hospitalizations resulting from opioid and sedative poisonings between 1999 and 2006, however there is little information known today regarding the clinical and demographic features of this patient population.
2. What does this study attempt to show?
This retrospective cohort study sought to evaluate demographic and clinical outcomes data from the 2006–2011 Nationwide Emergency Department Sample (NEDS).
3. What are they key findings?
From 2006–2011, there were 259,093 ED visits by adults for poisoning by opioids and 53.50% were unintentional. Although the sample mean age was 45.5 years, significantly more visits were made by patients between the ages of 18–30. Patients were also more likely to be female, use Medicare for unintentional poisonings (36.41%) and private insurance for intentional (29.29%). A significant amount of patients from this sample reside in the South (40.93%) and come from lower-income households. Average charge per visit was $3,515 for those discharged and $27,491for admissions, with total charges over the 5-year period amounting to over $4 billion.
4. How is patient care impacted?
More information on this population will possibly increase prescriber awareness of the magnitude of this problem and future behavioral and withdrawal support programs can be established, along with targeted anti-drug campaigns.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Opioids drive continued increase in drug overdose deaths. [Last accessed 02/28/2014]; Available at http://www.cdc.gov/media/releases/2013/p0220_drug_overdose_deaths.html.
- 2.Centers for Disease Control and Prevention (CDC) Policy impact: Prescription painkiller overdoses. [Last accessed 03/20/2014]; Available at http://www.cdc.gov/homeandrecreationalsafety/rxbrief/.
- 3.Coben JH, Davis SM, Furbee PM, et al. Hospitalizations for poisoning by prescription opioids, sedatives, and tranquilizers. Am J Prev Med. 2010;38:517–524. doi: 10.1016/j.amepre.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics, National Vital Statistics System. 10 Leading causes of injury deaths by age group highlighting unintentional injury deaths, United States-2010. [Last accessed 02/28/2014]; Available at http://www.cdc.gov/injury/wisqars/pdf/10LCID_Unintentional_Deaths_2010-a.pdf.
- 5.Centers for Disease Control and Prevention. Drug poisoning deaths in the United States, 1980–2008. [Last accessed 02/28/2014]; Available at http://www.cdc.gov/nchs/data/databriefs/db81.htm.
- 6.National Institute on Drug Abuse. Prescription Drugs: Abuse and Addiction. [Last accessed 03/20/2014]; Available at http://www.drugabuse.gov/sites/default/files/rrprescription.pdf.
- 7.The Joint Commission. Facts about pain management. [Last accessed 03/20/2014]; Available at http://www.jointcommission.org/assets/1/18/pain_management.pdf. [Google Scholar]
- 8.Department of Veterans Affairs. VA/DoD clinical practice guideline for management of opioid therapy for chronic pain. [Last accessed 03/20/2014]; Available at http://www.va.gov/PAINMANAGEMENT/docs/CPG_opioidtherapy_summary.pdf.
- 9.Centers for Disease Control and Prevention (CDC) Unintentional poisoning deaths—United States, 1999–2004. MMWR Morb Mortal Wkly Rep. 2007;56(5):93–96. [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2007 National Survey on Drug Use and Health: National Findings. [Last accessed 02/28/2014]; Available at http://www.samhsa.gov/data/nsduh/2k7nsduh/2k7Results.htm.
- 11.Manchikanti L, Singh A. Therapeutic opioids: a ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician. 2008;11(2 Suppl):S63–S88. [PubMed] [Google Scholar]
- 12.National Institute on Drug Abuse. Topics in Brief: Prescription Drug Abuse. [Last accessed 02/28/2014]; Available at http://www.drugabuse.gov/publications/topics-in-brief/prescription-drug-abuse.
- 13.Rockville, MD: Agency for Healthcare Research and Quality; [Accessed 02/28/2014]. Overview of the Nationwide Emergency Department Sample (NEDS). Healthcare Cost and Utilization Project (HCUP) Available at http://www.hcup-us.ahrq.gov/nedsoverview.jsp. [Google Scholar]
- 14.Centers for Disease Control and Prevention. Prescription drug abuse and overdose: public health perspective. [Last accessed 02/28/2014]; Available at http://www.cdc.gov/primarycare/materials/opoidabuse/docs/pda-phperspective-508.pdf.
- 15.Chakravarthy B, Shah S, Lotfipour S. Prescription Drug Monitoring Programs and Other Interventions to Combat Prescription Opioid Abuse. West J Emerg Med. 2012;13:422–425. doi: 10.5811/westjem.2012.7.12936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manchikanti L, Fellows B. Therapeutic use, abuse and nonmedical use of opioids: a ten225 year perspective. Pain Physician. 2010;13(5):401–435. [PubMed] [Google Scholar]
- 17.Green TC, Grimes Serrano JM, Licari A, Budman SH, Butler SF. Women who abuse prescription opioids: findings from the Addiction Severity Index-Multimedia Version Connect prescription opioid database. Drug Alcohol Depend. 2009;103(1–2):65–73. doi: 10.1016/j.drugalcdep.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manchikanti L. Prescription drug abuse: what is being done to address this new drug epidemic? Testimony before the Subcommittee on Criminal Justice, Drug Policy and Human Resources. Pain Physician. 2006;9(4):287–321. [PubMed] [Google Scholar]
- 19.Xiang Y, Zhao W, Xiang H, Smith GA. ED visits for drug-related poisoning in the United States, 2007. Am J Emerg Med. 2012;30(2):293–301. doi: 10.1016/j.ajem.2010.11.031. [DOI] [PubMed] [Google Scholar]