ABSTRACT
OBJECTIVE
To analyze oral health work changes in primary health care after Brazil’s National Oral Health Policy Guidelines were released.
METHODS
A literature review was conducted on Medline, LILACS, Embase, SciELO, Biblioteca Virtual em Saúde, and The Cochrane Library databases, from 2000 to 2013, on elements to analyze work changes. The descriptors used included: primary health care, family health care, work, health care policy, oral health care services, dentistry, oral health, and Brazil. Thirty-two studies were selected and analyzed, with a predominance of qualitative studies from the Northeast region with workers, especially dentists, focusing on completeness and quality of care.
RESULTS
Observed advances focused on educational and permanent education actions; on welcoming, bonding, and accountability. The main challenges were related to completeness; extension and improvement of care; integrated teamwork; working conditions; planning, monitoring, and evaluation of actions; stimulating people’s participation and social control; and intersectorial actions.
CONCLUSIONS
Despite the new regulatory environment, there are very few changes in oral health work. Professionals tend to reproduce the dominant biomedical model. Continuing efforts will be required in work management, training, and permanent education fields. Among the possibilities are the increased engagement of managers and professionals in a process to understand work dynamics and training in the perspective of building significant changes for local realities.
Keywords: Dental Health Services, organization and administration; Public Health Dentistry, Manpower; Primary Health Care; Dentist’s Practice Patterns; Working Conditions; Public Health Policy; Review
INTRODUCTION
Brazil has made advancements with its Unified Health System (SUS) by establishing universal and full care as its principles and by increasing the coverage of its Primary Health Care (PHC), through Family Health Care Strategy (FHCS). However, the biomedical health care model prevails, and it guides all professional practices, including dentistry. 4 , 13 , 35 , 48 , 50 , 54 , 55
According to its last epidemiological survey, Brazil shifted its prevalence of caries from medium to low. 59 Although results are nationally satisfactory, some factors call our attention: (a) regional differences in the prevalence and seriousness of caries are distinctive, which indicates a need for policies focused on equal care; (b) small reduction of caries in deciduous dentition (18.0%) and 80.0% of affected teeth remaining untreated; (c) significant deficit for older adults, despite adolescents’ and adults’ need for prosthetics having been decreased; and (d) prevalence of malocclusion requiring treatment in 10.0% of adolescents, which suggests a need for resizing the supply of dental procedures in secondary care. 32 , 33 These results are associated with the profile of dental practice, characterized by the conduction of eminently clinical actions emphasizing restoring activities and preventive actions focusing on students, which were shown to be insufficient to meet the needs of the population. 31
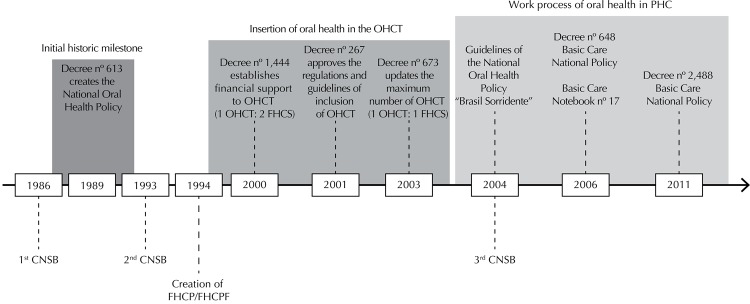
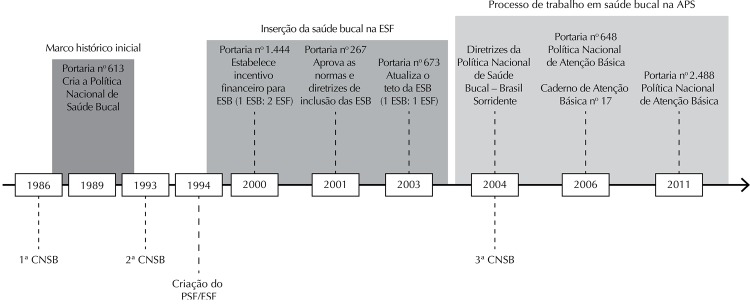
The Brazilian path to shift the direction of its oral health care model in PHC has found milestones that have a potential to drive work changes: (a) first ConferênciaNacional de Saúde Bucal (CNSB – National Oral Health Conference) in 1986, followed by the creation of Brazil’s National Oral Health Policy in 1989, a and by the second CNSB in 1993; 9 (b) inclusion of dental professionals in FHCS in 2000, 17 facing the historical restriction of dealing with mother and their children and established a federal financial incentive; creation of new national syllabus guidelines for undergraduate courses in the health care field; 3 and approval of rules and guidelines to include oral health care teams in FHCS in 2001; (c) release of the Programa Brasil Sorridente (“Smiling Brazil” Program) in 2004 23 and the third CNSB, which contributed to democratic and forward-looking production on the topic; (d) common and specific responsibilities of oral health care professionals in Brazil’s National Basic Health Care Policy in 2006, b which were restated in 2011. c
The recent path of oral health care signals that a new model is being built in the country (Figure 1).
Figure 1. Timeline identifying the moments and regulations that mark the incentive to changes in the oral health work process in Primary Health Care in Brazil.
CNSB: Conferência Nacional de Saúde Bucal (National Oral Health Conference); FHCP: Family Health Care Program; FHCS: Family Health Care Strategy; OHCT: Oral Health Care Team
The “Smiling Brazil” Program, as a guideline of Brazil’s National Oral Health Policy (PNSB), d is the largest public oral health care program in the world and it has turned a decade old in 2014. 28 Changes were made to the work of oral health care teams in PHC over that period, in a way to meet the goals for readjusting the health care model. 20
The PHC is a potential space for innovation in the management and organization of the work process, one of the central axes for rearranging SUS’s health care.
This article intended to analyze the oral health work changes in primary health care after Brazil’s National Oral Health Policy Guidelines were released.
METHODS
The literature review was guided by analyzing elements of work changes in oral health in PHC, according to regulations in effect, 27 , c , d and from the publication of the Guidelines of PNSB. The following elements were used to analyze the changes in oral health in PHC: welcoming, bonding, and accountability; extension and improvement of care; intersectorial actions; educational actions; permanent education; fostering of popular participation and social control; completeness; planning, monitoring, and evaluation of actions; integrated teamwork; and working conditions. The guiding questions were: “Which analyzing elements are mentioned?”, “Are reports of work changes, advances, or difficulties present?”, “Are recommendations, complaints, or suggestions for oral health work in PHC present?”.
Studies were collected in Medline (via PubMed), LILACS, Embase, SciELO, Biblioteca Virtual em Saúde (BVS), and The Cochrane Library (via Bireme) databases. Publications from 2000 to 2013 were included (until November 3, 2013). A period prior to 2004 was included, when the Guidelines of PNSB were released, after experiences and agreements among the several players involved in the discussion and that may have been research topics in published scientific journals.
The descriptors used in the search on PubMed were: (“primary health care” OR “family health” OR “work” OR “health policy”) AND (“dental health services” OR “dentistry” OR “oral health”) AND (“Brazil”). The descriptors were used in English and Portuguese in the remaining databases. The combination was conducted with the use of boolean operators “AND” and “OR”, as well as terms from the Medical Subject Headings (MeSH) or analogous ones available in each surveyed database.
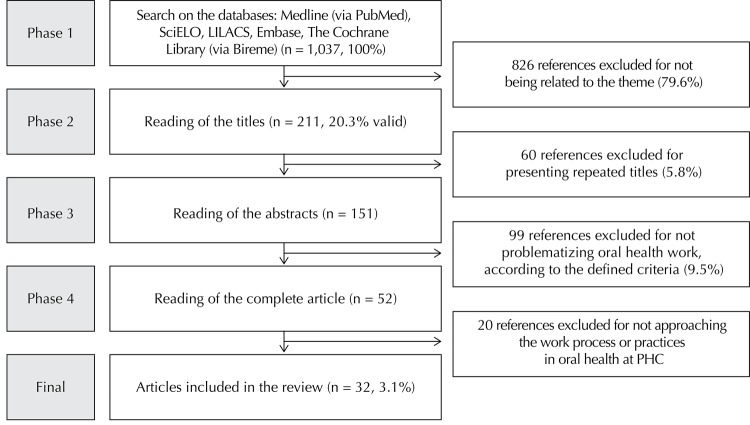
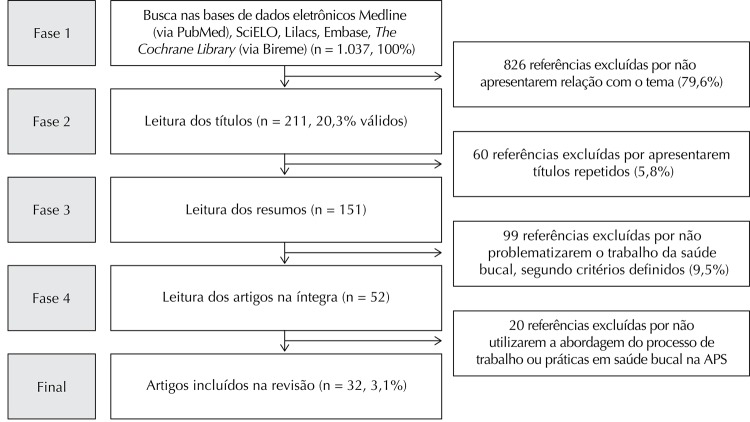
Data were collected by one of the authors, whereas the other two, who were familiar with the topic and the method, undertook the selection and evaluation of studies. A total of 77 articles were found on Medline, 538 on LILACS, four on Embase, 67 on SciELO, 338 on BVS, and 13 on The Cochrane Library, which totaled 1,037 articles.
We included the articles that concerned the work, practices, or change of model in oral health in PHC, selected by title. The selected articles were those that discussed the organization and management of work processes in oral health, especially about teamwork in PHC, a central element of the rearrangement of SUS’ health care. Studies of theoretical reflection, essays, and theses were excluded.
We selected 211 articles. Sixty of them were excluded for being repeated in the bases, which resulted in 151 studies whose abstracts should be read and 52 to be fully read. At the end, 32 articles were included in the final analysis (Figure 2).
Figure 2. Search, selection, inclusion, and exclusion of studies on the work process in oral health in Primary Health Care.
PHC: Primary Health Care
General publication aspects, methodological characteristics, and main results were identified and analyzed based on their elements (Table 1). Information screening was independently conducted by the researchers and compared in a meeting for consensus. Agreed items were considered proper and included in the description of results. These were grouped according to their previous topic categories (elements for analysis) and analyzed in a descriptive manner.
Table 1. General aspects of selected studies, methodological characteristics, and study subjects.
| Year | Location | Author | Journal | Title | Study type and methodology | Study subjects | |
|---|---|---|---|---|---|---|---|
| 2013 | SP | Pezzato LM, L’Abbate S, and Botazzo C | Ciência & Saúde Coletiva, 18(7):2095-104 | A produção de micropolíticas no processo de trabalho em saúde bucal: uma abordagem sócio-analítica (The production of micro-policies in the work process in oral health care: a socioanalytical approach) | Qualitative | Socioanalytical approach | Workers (OHCT) and users |
| 2013 | MG | Sanglard-Oliveira CA, Werneck MAF, Lucas SD, and Abreu MHNG | Ciência & Saúde Coletiva, 18(8):2453-60 | Atribuições dos Técnicos em Saúde Bucal na Estratégia Saúde da Família em Minas Gerais, Brasil (Attributions of oral health technicians in the Family health care strategy in Minas Gerais, Brazil) | Qualitative | Cross-sectional, descriptive study Telephone interview | Workers (DS) |
| 2013 | PI | Moura MS, et al | Ciência & Saúde Coletiva, 18(2):471-80 | Saúde bucal na estratégia de saúde da família em um colegiado gestor regional do estado do Piauí (Oral Health in the strategy of family health care in a managing regional collegiate of Piauí state) | Qualitative | Cross-sectional study Questionnaire | Workers (DS) |
| 2012 | ES | Esposti CDD, Oliveira AE, Santos Neto ET, and Zandonade E | Saúde Soc. São Paulo, 21(2):372-85 | O processo de trabalho do técnico em saúde bucal e suas relações com a equipe de saúde bucal na Região Metropolitana da Grande Vitória, Espírito Santo, Brasil (The work process of oral health care technicians and their relationships with oral health care teams in the metropolitan region of Grande Vitória, Espírito Santo, Brazil) | Qualitative | Semi-structured interview | Workers (DS) |
| 2012 | PE | Pimentel FC, et al | Cad. Saúde Pública, 28 Sup:S146-S157 | Caracterização do processo de trabalho das equipes de saúde bucal em municípios do Estado de Pernambuco, Brasil, de acordo com o tamanho da população: a partir de links da comunidade para a organização dos cuidados clínicos. (Characterization of the work process of oral health care teams in municipalities in the state of Pernambuco, Brazil, according to the population size: from community links for the organization of clinical care). | Qualitative | Structured questionnaire | Workers (OHCT) |
| 2011 | SP | Cunha BAT, Marques RAA, Castro CGJ, and Narvai PC | Saúde Soc, 20(4):1033-45 | Saúde bucal em Diadema: da odontologia escolar à estratégia saúde da família (Oral health in Diadema: from school dentistry to the family health care strategy) | Qualitative | Semi-structured interview and document analysis | Managers and worker (Mayors, MHCO, OHC, and CD) |
| 2011 | SP | Mialhe FL, Lefèvre F, Lefèvre AMC | Ciência & Saúde Coletiva, 16(11):4425-32 | O agente comunitário de saúde e suas práticas educativas em saúde bucal: uma avaliação qualiquantitativa (Community health care agents and their oral health-related educational practices: a qualitative and quantitative evaluation) | Qualitative and quantitative | Semi-structured interview | Workers (CHCA) |
| 2011 | PE | Silva SF et al | Ciência & Saúde Coletiva, 16(1):211-20 | Análise do avanço das equipes de saúde bucal inseridas na Estratégia Saúde da Família em Pernambuco, região Nordeste, Brasil, 2002 a 2005 (Analysis of the advancement of oral health care teams in the family health care strategy in Pernambuco, Northeast region, Brazil, 2002 to 2005) | Quantitative | Descriptive exploratory study | Secondary data (SIA-SUS) |
| 2011 | BA | Rodrigues AAAO, Nascimento MAA, Fonsêca GS, and Siqueira DVS | Rev. Baiana Saúde Pública, 35(3):695-709 | Saúde bucal na estratégia saúde da família em um município do semiárido baiano (Oral health in the family health care strategy in a municipality in Bahia’s semi-arid zone) | Qualitative | Semi-structured interview and observation | Workers (FHCT and OHCT) |
| 2010 | PE | Pimentel FC, et al | Ciência & Saúde Coletiva, 15(4):2189-96 | Análise da atenção à saúde bucal na Estratégia de Saúde da Família do Distrito Sanitário VI, Recife - PE (Analysis of oral health care in the Family Health Care Strategy in Sanitary District VI, Recife - PE) | Qualitative | Descriptive study Semi-structured interview and secondary data | Managers and workers (OHC, DS, and nurse) |
| 2010 | BA | Rodrigues AAAO, Santos AM, and Assis MMA | Ciência & Saúde Coletiva, 15(3):907-15 | Agente comunitário de saúde: sujeito da prática em saúde bucal em Alagoinhas, Bahia (Community health care agent: subject of the oral health care practice in Alagoinhas, Bahia) | Qualitative | Semi-structured interview, observation, and document analysis | Workers (CHCA and OHCT) |
| 2010 | CE | Nuto SAS, Oliveira GC, Andrade, JV, and Maia MCG | Rev. APS, 13(4):505-9 | O acolhimento em saúde bucal na estratégia de saúde da família, Fortaleza-CE: um relato de experiência (Welcoming in oral health in the family health care strategy, Fortaleza-CE: an account of an experiment) | Qualitative | Experiment report | Workers (OHCT and CHCA), users, and scholars |
| 2010 | PI | Moura MS, et al | Ciência & Saúde Coletiva, 15(supl.1): 1487-95 | Perfil e práticas de saúde bucal do agente comunitário de saúde em municípios piauienses de pequeno porte (Oral health profile and practices of community health care agents in small-sized municipalities in Piaúi) | Qualitative | Cross-sectional, observational, descriptive study Questionnaire | Workers (CHCA) |
| 2010 | PE | Martelli PJL, et al | Ciência & Saúde Coletiva, 15(Supl. 2):3243-8 | Perfil do cirurgião dentista inserido na Estratégia de Saúde da Família em municípios do estado de Pernambuco, Brasil (Profile of dentist surgeons in the Family Health Care Strategy in municipalities in Pernambuco state, Brazil) | Qualitative | Descriptive, exploratory, and cross-sectional case study Questionnaire | Workers (DS) |
| 2010 | SC | Faccin D, Sebold R, and Carcereri DL | Ciência & Saúde Coletiva, 15(Supl. 1):1643-52 | Processo de trabalho em saúde bucal: em busca de diferentes olhares para compreender e transformar a realidade (Work process in oral health care: searching for different opinions in order to understand and transform reality) | Qualitative | Semi-structured interview | Workers (FHCT and OHCT) |
| 2009 | MG | Lourenço EC, Silva ACB, Meneghin MC, and Pereira AC | Ciência & Saúde Coletiva, 14(Supl. 1):1367-77 | A inserção dos serviços de saúde bucal no Programa Saúde da Família no Estado de Minas Gerais (The inclusion of oral health care services in the family health care program in Minas Gerais state) | Qualitative and quantitative | Questionnaires | Workers (FHCT and OHCT) |
| 2009 | PR/SP | Nascimento AC, Moysés ST, Bisinelli JC, and Moysés SJ | Rev. Saúde Pública, 43(3):455-62 | Oral health in the family health strategy: a change of practices or semantics diversionism | Qualitative | Focal Group | Workers (DS) |
| 2009 | BA | Rodrigues AAAO, Gallotti AP, Pena SFA, and Ledo CAS | Rev. Baiana Saúde Pública, 33(4):582-94 | Saúde bucal no programa de saúde da família na cidade de Feira de Santana (BA): o perfil do cirurgião-dentista (Oral health in the family health care program in the city of Feira de Santana - BA - the profile of a dentist surgeon) | Quantitative | Questionnaire | Workers (DS) |
| 2009 | RN | Rocha ECA and Araújo MAD | Rev. Adm. Pública, 43(2): 481-517 | Condições de trabalho das equipes de saúde bucal no Programa Saúde da Família: o caso do Distrito Sanitário Norte em Natal, RN (Working conditions of oral health care teams in the family health care program: the case of North Sanitary District in Natal, RN) | Qualitative and quantitative | Descriptive exploratory study Questionnaire | Workers (DS) |
| 2009 | RN | Holanda ALF, Barbosa AAA, and Brito EWG | Ciência & Saúde Coletiva, 14(Supl. 1):1507-12 | Reflexões acerca da atuação do agente comunitário de saúde nas ações de saúde bucal (Reflections regarding the performance of community health care agents in oral health actions) | Qualitative | Experiment report | Workers (DS) |
| 2008 | PR | Koyashiki GAK, Alves-Souza RA, and Garanhani ML | Ciência & Saúde Coletiva, 13(4):1343-54 | O trabalho em saúde bucal do Agente Comunitário de Saúde em Unidades de Saúde da Família (The oral health work of Community Health care Agents in Family Health Care Units) | Qualitative | Interview | Workers (CHCA) |
| 2008 | BA | Dos Santos AM, Assis MMA, Nascimento, MAA, and Jorge, MSB | Rev. Saúde Pública 2008;42(3):464-70 | Vínculo e autonomia na prática de saúde bucal no Programa Saúde da Família (Bonding and autonomy in the oral health practice in the family health care program) | Qualitative | Critical-reflexive approach Semi-structured interview and observation | Workers (FHCT and OHCT) and users |
| 2008 | BA | Chaves SCL and Vieira-da-Silva LM | Health Policy 86(1):119-28 | Inequalities in oral health practices and social space: an exploratory qualitative study | Qualitative | Exploratory study Semi-structured interview | Workers and managers (DS and OHC) and users |
| 2008 | PE | Martelli PJL, et al | Ciência & Saúde Coletiva, 13(5):1669-74 | Análise do modelo de atenção à saúde bucal em municípios do estado de Pernambuco (Analysis of the oral health care model in municipalities in Pernambuco state) | Qualitative | Semi-structured interview | Managers (OHC) |
| 2008 | PE | Pimentel FC, et al | Rev. Baiana Saúde Pública, 32(2): 253-64 | Evolução da assistência em saúde bucal na estratégia de saúde da família do município do Recife (PE) no período de 2001 a 2007 (Evolution of the oral health care in the family health care strategy in the municipality of Recife - PE - from 2001 to 2007) | Quantitative | Descriptive study | Secondary data (SIA-SUS) |
| 2008 | RN | Almeida GC and Ferreira MA | Cad. Saúde Pública, 24(9):2131-40 | Saúde bucal no contexto do Programa de Saúde da Família: práticas de prevenção orientadas a saúde individual e pública (Oral health in the context of the Family Health Care Program: prevention practices focusing on individual and public health) | Qualitative and quantitative | Descriptive exploratory study Structured interview Document analysis | Workers (DS) Secondary data (SIAB and SIA-SUS) |
| 2008 | PA | Emmi DT and Barroso RFF | Ciência & Saúde Coletiva, 13(1):35-41 | Avaliação das ações de saúde bucal no Programa Saúde da Família no distrito de Mosqueiro, Pará (Evaluation of oral health actions in the family health care program in the district of Mosqueiro, Pará state) | Qualitative | Descriptive study Questionnaire | Users |
| 2007 | BA | Dos Santos AM, et al | Cad. Saúde Pública, 23(1):75-85 | Linhas de tensões no processo de acolhimento das equipes de saúde bucal do Programa Saúde da Família: o caso de Alagoinhas, Bahia, Brasil (Tension lines in the process of receiving oral health care teams of the family health care program: the case of Alagoinhas, Bahia, Brazil) | Qualitative | Semi-structured interview and observation | Workers (FHCT and OHCT) and users |
| 2007 | BA | Chaves SCL and Silva LMV | Ciência & Saúde Coletiva, 12(6):1697-710 | As práticas profissionais no campo público de atenção à saúde bucal: o caso de dois municípios da Bahia (Professional practices in the public oral health care: the case of two municipalities in Bahia) | Qualitative | Semi-structured interview | Workers (DS) |
| 2007 | RN | Souza TM and Roncalli AG | Cad. Saúde Pública, 23(11):2727-39 | Saúde bucal no Programa Saúde da Família: uma avaliação do modelo assistencial (Oral health in the family health care program: an evaluation of the care model) | Qualitative | Structured interview, observation, and document analysis | Managers (OHC or person in charge) and workers (DS) |
| 2005 | PR | Baldani MH, Fadel CB, Possamai T, and Queiroz MGS | Cad. Saúde Pública, 21(4):1026-35 | Inclusão de serviços de saúde bucal no Programa Saúde da Família no Estado do Paraná (Inclusion of oral health care services in the family health care program in Paraná State) | Qualitative and quantitative | Questionnaires | Managers (OHC or MHCO) and workers (DS) |
| 2005 | BA | Rodrigues AAAO and Assis MMA | Rev. Baiana Saúde Pública, 29(2):273-85 | Oferta e demanda na atenção à saúde bucal: o processo de trabalho no Programa Saúde da Família em Alagoinhas – Bahia (Supply and demand in oral health care: the work process of the family health care program in Alagoinhas - Bahia) | Qualitative | Semi-structured interview, observation, and document analysis | Managers (Mayor, MHCO, and OHC) and workers (FHCT and OHCT + CHCA) |
CHCA: community health care agent; DS: Dental Surgeon; OHC: Oral Health Coordinator; OHCT: Oral Health Care Team; FHCT: Family Health Care Team; SIA-SUS: Sistema de Informações Ambulatoriais (System of Ambulatorial Information) of SUS; SIAB: Sistema de Informação de Atenção Básica (Basic Health Care Information System); MHCO: Municipal Health Care Officer
RESULTS
Most studies were from the Northeast (n = 21; 65.6%), Southeast (n = 6; 18.7%) and South regions (n = 3; 9.3%) (Table 1). We identified qualitative (n = 24; 75.0%) and quantitative studies (n = 3; 9.3%). A combination of quantitative and qualitative methods was used in 15.6% of the articles (Table 2). In general, the main subjects were FHCT workers, dental surgeons (DS) being highlighted. Around a third of them included managers and users (Table 1). All studies (n = 32) mentioned one or more work-analyzing elements, but none included all of them (Table 2).
Table 2. Selected studies on the analyzing elements of oral health work in Primary Health Care in Brazil pointing out challenges and changes.
| Region | State | Year | Author | Analyzing elements in the studies | |
|---|---|---|---|---|---|
|
| |||||
| Indicating challenges | Pointing out changes | ||||
| South | PR | 2005 | Baldani MH, Fadel CB, Possamai T, and Queiroz MGS | 1, 7, 9, and 10 | 4 |
| PR | 2008 | Koyashiki GAK, Alves-Souza RA, and Garanhani ML | 5 and 9 | 7 | |
| SC | 2010 | Faccin D, Sebold R, and Carcereri DL | 1, 3, 7, 9, and 10 | 2 | |
| Southeast | MG | 2009 | Lourenço EC, Silva ACB, Meneghin MC, and Pereira AC | 5, 8, 9, and 10 | 1 |
| SP | 2010 | Cunha BAT, Marques RAA, Castro CGJ, and Narvai PC | 1 and 7 | 4 and 5 | |
| SP | 2011 | Mialhe FL, Lefèvre F, Lefèvre AMC | 2 and 5 | 0 | |
| ES | 2012 | Esposti CDD, Oliveira AE, Santos Neto ET, and Zandonade E | 9 | 5 and 10 | |
| SP | 2013 | Pezzato LM, L’Abbate S, and Botazzo C | 6 | 1 and 7 | |
| MG | 2013 | Sanglard-Oliveira CA, Werneck MAF, Lucas SD, and Abreu MHNG | 0 | 2, 4, and 7 | |
| South and Southeast | PR | 2009 | Nascimento AC, Moysés ST, Bisinelli JC, and Moysés SJ | 1, 9 | 4, 7 |
| SP | 1 | 0 | |||
| Northeast | BA | 2005 | Rodrigues AAAO and Assis MMA | 7 and 9 | 0 |
| BA | 2007 | Santos AM, Assis MMA, Rodrigues AAAO, Nascimento MAA, Jorge MSB | 4 | 0 | |
| BA | 2007 | Chaves SCL and Silva LMV | 7 | 0 | |
| RN | 2007 | Souza TM and Roncalli AG | 1, 8, 9, and 10 | 3 | |
| BA | 2008 | Santos AM, Assis MMA, Nascimento MAA, and Jorge MSB | 1 and 10 | 4 | |
| BA | 2008 | Chaves SCL and Vieira-da-Silva LM | 2 and 7 | 0 | |
| PE | 2008 | Martelli PJL, et al | 1, 5, 8, and 10 | 9 | |
| PE | 2008 | Pimentel FC, et al | 7 and 8 | 1 | |
| RN | 2008 | Almeida GC and Ferreira MA | 1 and 8 | 2 | |
| BA | 2009 | Rodrigues AAAO, Gallotti AP, Pena SFA, and Ledo CAS | 10 | 2 and 5 | |
| RN | 2009 | Rocha ECA and Araújo MAD | 1 and 10 | 0 | |
| RN | 2009 | Holanda ALF, Barbosa AAA, and Brito EWG | 7 and 9 | 5 | |
| PE | 2010 | Pimentel FC, et al | 1, 6, 7, 8, 9 | 2 | |
| BA | 2010 | Rodrigues AAAO, Santos AM, and Assis MMA | 9 | 7 | |
| CE | 2010 | Nuto SAS, Oliveira GC, Andrade JV, and Maia MCG | 1 | 4 and 5 | |
| PI | 2010 | Moura MS, et al | 7 | 5 | |
| PE | 2010 | Martelli PJL, et al | 1, 5, and 10 | 2 | |
| PE | 2011 | Silva SF, et al | 7 | 1 and 5 | |
| BA | 2011 | Rodrigues AAAO, Nascimento MAA, Fonsêca GS, and Siqueira DVS | 5, 7, 8, and 10 | 0 | |
| PE | 2012 | Pimentel FC, et al | 1, 5, 6, 7, and 8 | 9 | |
| PI | 2013 | Moura MS, et al | 5, 7, 9, and 10 | 0 | |
| North | PA | 2008 | Emmi DT and Barroso RFF | 0 | 1 and 2 |
1: extension and improvement of care; 2: educational actions; 3: intersectorial actions; 4: welcoming, bonding, and accountability; 5: permanent education in health; 6: fostering of popular participation and social control; 7: completeness; 8: planning, monitoring, and evaluation of actions; 9: integrated teamwork; 10: working conditions; 0: Absence of analyzing elements in the study; States: PR: Parana; SC: Santa Catarina; MG: Minas Gerais; SP: Sao Paulo; ES: Espirito Santo; BA: Bahia; PE: Pernambuco; RN: Rio Grande do Norte; PI: Piaui; PA: Para
The few advances in oral health work focused on educational actions; permanent education actions; welcoming, bonding, and accountability. The main challenges related to completeness; extension and improvement of care; teamwork; planning, monitoring, and evaluation of actions; and working conditions. Few studies 14 , 36 , 38 , 39 , 57 included fostering of popular participation and social control and intersectorial actions.
Among the 32 studies analyzed, 19 of them mentioned the topic of completeness. Fourteen of those 5 , 7 , 8 , 10 , 14 , 16 , 29 , 30 , 37 , 38 , 41 , 44 , 53 pointed out difficulties to restructure oral health in PHC, overcome the practices in the traditional school dentistry model and create new possibilities, such as the family approach and diagnosis of the health care situation. 1 , 10 , 14 , 34 , 39 Actions focusing on clinical care and excess emphasis on technique and specialty persisted, and traditional preventive and educational practices prevailed. 7 , 14 , 41 The oral health care teams found difficulties in practices related to FHCT, such as house calls by dentists, actions to prevent illnesses and promote health, as well as meetings and actions for articulation with the community. 5 , 39
Insufficient changes related to completeness were presented in five studies 18 , 32 , 36 , 43 , 45 (26.3%), which reported the introduction of care focused on the user, with a space for dialog and for the bringing together knowledge encompassing oral health. Unlike individual actions, the group actions and the advances in the preventive view and the practice of health education of professionals were expressive in FHCT. 1 , 14 , 38 Another change regards to the oral health technicians, who spent more of their time in preventive and collective activities than in care activities. 45
Two studies mentioned teamwork and showed that most DS reported integration with their teams, but only a few took part in meetings or used single records. 5 , 19 The work of a DS was rarely inserted in shared practices with professionals of other fields, as their actions were autonomously, independently, and individually developed. 39
We observed obstacles for teamwork also among dental professionals. 13 The DS recognized their relationship with oral health technicians was damaged by the lack of information on the work process, due to being uncertain of how liable they were regarding the activities of technicians, and also due to being afraid of technicians becoming practical dentists and taking their space in the job market. On the other hand, the DS appreciated the participation of technicians in the reorganization of dental work and in the construction of a relationship of partnership and cooperation.
Intersectorial actions were mentioned in two of the 32 studies, 14 , 57 related to oral health prevention and education actions developed in the community or at schools. 57 We observed intersectorial actions to be volunteer practices in some of the teams, not reaching the expected impacts. Such circumstance may lead professionals to disbelief regarding FHCT, considering the inability of the health sector to deal with social determining factors of the health-disease process in an isolated manner.
Educational actions were present in nine studies, 1 , 8 , 11 , 14 , 22 , 26 , 38 , 42 , 45 of which seven pointed out advances in the practices of professionals concerning what is recommended by the guidelines of PNSB. According to Martelli et al, 22 92.3% of the DS considered them relevant. Among those, 89.6% reported conducting them. Rodrigues et al 42 identified that all DS conducted health education activities, at their health care units or schools, nursing homes, churches, and daycare facilities. The actions that were most reported were the ones of prevention and promotion in groups, 1 , 14 highlighting oral health technicians as the ones responsible for them. 45 The ones of education in health were more present in the daily lives of FHCT professionals. 38 , 42
According to Mialhe et al, 26 the educational activities in oral health were conducted sporadically and mainly focused on pregnant women, mothers, and their children, in a vertical model of transmission of information, targeting changes in individual behaviors and incorporation of healthy habits. That vision was shared by the population, which considered oral hygiene instructions as one of the most important improvements. 11
Eight studies 1 , 19 , 21 , 37 - 44 , 57 reported that planning, monitoring, and evaluation of actions were insufficient practices, and indicated difficulties in the conduction of surveys to recognize population needs, considering social and epidemiological characteristics. 38 , 44 Despite the advances, oral health needs much investment, besides the control and evaluation of its actions through information systems, which strengthen planning and decision-making. 37
Fostering of popular participation and social control was mentioned in three studies 36 , 38 , 39 as an action to be stimulated by teams. Pezatto et al 36 pointed out that the appropriation of oral health topics by social control spaces is one of the challenges in implementing oral health care services in SUS.
The extension and improvement of oral health care were mentioned in 19 of the 32 studies. Among those, five 11 , 19 , 36 , 37 , 53 mentioned advances, but difficulties prevailed (73.6%) regarding meeting the needs of the related population. 5 Excessive demand was highlighted as a negative aspect, with predominance of healing actions by the DS. 19 Even with the extended access to oral health care services, organizing the demand was a critical bottleneck, as there are several gateways, large repressed demand, and little supply. 19 , 32 , 34 Increasing and improving care requires facing challenges related to insufficient public investments; to the difficulties in referring patients to specialty services; the actions focusing on clinical care with excess emphasis on technique and specialty; and the rising demand for services by the population, focused on healing actions. 34 Despite the difficulties, we observed positive aspects in the studies: limiting of clients, enabling better supervision; changes in the profile of dental procedures conducted; and population-based coverage according to the minimum limit as per the Ministry of Health. 11 , 37 , 53
Establishing welcoming, bonding, and accountability allows negotiating with users and professionals of full health care, which helps the therapeutic act to be focused on the professional, however being conducted according to the user’s wishes. These elements were mentioned by seven studies. 5 , 10 , 32 , 34 , 45 - 47 Among those, six pointed out changes: the influence of new national syllabus guidelines in the more humanized practice of dentists, reinforcing the bond, the extended look at the territory and the community; and the potential work of community health care agent in the establishment of bonding, welcoming, and autonomy of users. 5 , 47
We identified 11 studies 5 , 14 , 19 , 21 , 22 , 30 , 40 , 42 , 46 , 47 , 56 out of the 12 that mentioned difficulties regarding the working conditions of SUS. Some critical bottlenecks were poor labor relationships, with small wages and unstable employment, 5 , 1 9 , 22 with probable effects on turnover and professional satisfaction, which jeopardizes the quality of health care; 5 , 22 DS having double shifts in public and private health care units; and the lack of compliance with the weekly workload of 40 hours in FHCT, as something agreed to by managers and workers. 42 , 44 The lack of financial, structural, physical, and human resources also influenced the working conditions. 5 , 30
Among the 15 studies on permanent education in health, eight 18 , 19 , 21 , 22 , 26 , 30 , 39 , 44 showed that professionals working in FHCT were not trained before starting their position, 44 and that no training processes focusing on professional oral health training was available, to make care more complete. 18 , 19 , 26 , 30 , 38 However, seven studies 10 , 13 , 16 , 29 , 34 , 39 , 42 , 45 pointed changes: over 90.0% of the DS from a study 5 reported taking part in training courses – the ones who did not had just been hired; another study 22 showed that 67.8% of the DS had been trained to FHCT and felt the need to specialize in public health care, to be able to work in FHCT.
DISCUSSION
Most of the analyzed studies were published from 2008, which indicates a recent interest in the field. The increased number of qualitative studies over the last few years adds an important dimension to the evaluation of actions in oral health, by producing knowledge from the experiences of professionals.
There was a predominance of studies from the Northeast region, which indicates that the results characterize a region, and not Brazil as a whole. According to Soares et al, 54 as the Northeast region is the one with the highest number of family health care teams in the country, that might explain the predominance of studies in the region.
The most investigated work-analyzing elements in oral health in PHC were completeness, extension, and improvement of care. The literature suggests these are two of the most commonly analyzed elements, which may positively contribute to improving and orienting public policies (in overcoming inequalities in the access to health care services, in reaching equity in the system, and in achieving completeness regarding practices and teamwork). 5 , 52
Despite the significant extension of coverage in oral health in PHC over the last decade, there are barriers that keep Brazilians from accessing the services. 24 The advances in the extension and improvement of care to the population are few and the work process in oral health care may be damaged by the permanent excess demand and predominance of healing actions.
Among the principles and guidelines of SUS, completeness may be the least visible one in the path of the health care system and its practices. 24 The study pointed out that completeness is insufficient, with weak points to be dealt with the work of FHCT teams. These analyses may be associated with the polysemy and coverage of the concept of completeness. To be effective, they require extended clinic, integration of individual and collective practices, and ability to solve problems with ensured access and articulation with other levels of care. 24 , 52
Teamwork directly influences completeness. 58 For oral health care professionals, integration in the work of family health care teams is limited by the historical isolation of these two professional categories, associated with the late introduction of oral health in FHCT and to the individualist and technicist training of professionals. That jeopardizes the full integration of the human being. 5 , 45
Professionals will be required to learn and re-learn through their individual experiences in collective work situations. Work is the result of a debate over rules and values of a worker with themselves, about how to be able to manage the complexity of issues regarding collective work. e In that sense, permanent education in health arises as a fundamental device. However, the review of the literature showed that training is focused on qualifying, 18 which is generally distant from work routines and restricted to professional centers.
The intersectorial actions and fostering of popular participation and social control were not investigated to a great extent, which corroborates the literature. 54 , 55 The volunteer nature of some teams or professionals may be partially explained by the fact that acting pursuant to the intersectoriality principle requires availability for periods that are not established in employment contracts. 15 Despite the existence of a consensus regarding the need for intersectoriality in PHC, it is a process being built in FHCT. 48 One of the challenges to implement it is the training of professionals, which is guided according to the perception of complexity of problems, and to the recognition of the need for intersectorial actions to intervene in such problems. 51
The planning, monitoring, and evaluation of actions are far from the everyday routines of oral health care teams. 54 It is a challenge that requires mobilization, engagement, and decision by managers and professionals.
Improving working conditions in SUS is directly related to improving the quality of care, but that is not a linear relationship. In contexts that are considered favorable to work, according to the principles of FHCT, teams focus their practices on treating occasional or scheduled patients. 25 At the same time, in adverse contexts, professionals seek alternatives to be efficient. 6 It is hard to define to which extent working conditions influence the change in professional practices.
The literature shows that, after a decade since the “Smiling Brazil” Program was implemented, the main problems and difficulties in the work of oral health care teams are not exclusive to dentistry. Strictly speaking, they follow the reality of FHCT teams, pursuant to what has been established by recent studies on the work of family health care teams. 2 , 49 , 56
The advances are concentrated in educational and permanent education actions, in welcoming, bonding, and accountability. The main challenges are related to completeness; extension and improvement of care; integrated teamwork; working conditions; planning, monitoring, and evaluation of actions; stimulating people’s participation and social control; and intersectorial actions.
Despite the new regulatory environment, there are very few changes in oral health work. Professionals tend to reproduce the dominant biomedical model. Continuing efforts will be required in the management of work, training, and permanent education. Increasing the engagement of managers and professionals in the process to understand the dynamics of work and training in the perspective of building significant changes for local realities is one of the possibilities to enable the substitution of traditional practices and a new way to provide health care services.
Ministério da Saúde. Portaria nº 613, de 13 de junho de 1989. Aprova a Política Nacional de Saúde Bucal. Diario Oficial Uniao. 13 jun 1989; Seção I: 42607.
Ministério da Saúde. Portaria nº 648, de 28 de março de 2006. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes e normas para a organização da Atenção Básica para o Programa Saúde da Família (FHCP) e o Programa Agentes Comunitários de Saúde (PACS). Diario Oficial Uniao. 29 mar 2006; Seção I: 71.
Ministério da Saúde. Portaria nº 2.488, de 21 de outubro de 2011. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes e normas para a organização da Atenção Básica, para a Estratégia Saúde da Família (FHCT) e o Programa de Agentes Comunitários de Saúde (PACS). Diario Oficial Uniao. 24 out 2011; Seção I: 48.
Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Atenção Básica, Coordenação Nacional de Saúde Bucal. Diretrizes da Política Nacional de Saúde Bucal. Brasília (DF); 2004. Available from: http://dab.saude.gov.br/portaldab/biblioteca.php?conteudo=publicacoes/pnsb
Schwartz Y. Trabalho e uso de si. Pro-Posições. 2000;1(5)(32):34-50, jul. 2000. Available from: http://www.proposicoes.fe.unicamp.br/proposicoes/textos/32-artigos-schwartzy.pdf
Based on the thesis of Charleni Inês Scherer, titled: “O trabalho em saúde bucal na Estratégia Saúde da Família: revisão da literatura e estudo qualitativo no Distrito Federal”, presented to the Postgraduate Program in Collective Health of Universidade de Brasília in 2014.
Research supported by the Ministry of Science, Technology, and Innovation, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq – Ministry of Health - Science, Technology and Strategic Inputs Secretariat – Department of Science and Technology (MCTI/CNPq/MS - SCTIE - DECIT – Process 10/2012 - Oral health Research – Process 403367/2012-3).
REFERENCES
- 1.Almeida GCM, Ferreira MAF. Saúde bucal no contexto do Programa Saúde da Família: práticas de prevenção orientadas ao indivíduo e ao coletivo. 10.1590/S0102-311X2008000900019Cad Saude Publica. 2008;24(9):2131–2140. doi: 10.1590/s0102-311x2008000900019. [DOI] [PubMed] [Google Scholar]
- 2.Anjos FS, Mestriner SF, Bulgarelli AF, Pinto IC, Mestriner W., Jr Equipes de saúde bucal no Brasil: avanços e desafios. 10.4025/cienccuidsaude.v10i3.10921Cienc Cuid Saude. 2011;10(3):601–607. [Google Scholar]
- 3.Antunes JLF, Narvai PC. Políticas de saúde bucal no Brasil e seu impacto sobre as desigualdades em saúde. 10.1590/S0034-89102010005000002Rev Saude Publica. 2010;44(2):360–365. [Google Scholar]
- 4.Ardenghi TM, Piovesan C, Antunes JLF. Desigualdades na prevalência de cárie dentária não tratada em crianças pré-escolares no Brasil. 10.1590/S0034-8910.2013047004352Rev Saude Publica. 2013;47(Suppl 3):129–137. doi: 10.1590/s0034-8910.2013047004352. [DOI] [PubMed] [Google Scholar]
- 5.Baldani MH, Fadel CB, Possamai T, Queiroz MGS. A inclusão da odontologia no Programa Saúde da Família no Estado do Paraná. 10.1590/S0102-311X2005000400005Cad Saude Publica. 2005;21(4):1026–1035. doi: 10.1590/s0102-311x2005000400005. [DOI] [PubMed] [Google Scholar]
- 6.Bertoncini JH, Pires DEP, Scherer MDA. Condições de trabalho e renormalizações nas atividades das enfermeiras na saúde da família. 10.1590/S1981-77462011000400008Trab Educ Saude. 2011;9(Suppl 1):157–173. [Google Scholar]
- 7.Chaves SCL, Silva LMV. As práticas profissionais no campo público de atenção à saúde bucal: o caso de dois municípios da Bahia. 10.1590/S1413-81232007000600031Cienc Saude Coletiva. 2007;12(6):1697–1710. doi: 10.1590/s1413-81232007000600031. [DOI] [PubMed] [Google Scholar]
- 8.Chaves SCL, Vieira-da-Silva LM. Inequalities in oral health practices and social space: an exploratory qualitative study. 10.1016/j.healthpol.2007.10.001Health Policy. 2008;86(1):119–128. doi: 10.1016/j.healthpol.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Costa JFR, Chagas LD, Silvestre RM.organizadores . A política nacional de saúde bucal do Brasil: registro de uma conquista histórica. Brasília (DF): Organização Pan-Americana da Saúde; 2006. [cited 2014 May 11]. (Série Técnica Desenvolvimento de Sistemas e Serviços de Saúde, 11). http://189.28.128.100/dab/docs/publicacoes/geral/serie_tecnica_11_port.pdf. [Google Scholar]
- 10.Cunha BAT, Marques RAA, Castro CGJ, Narvai PC. Saúde bucal em Diadema: da odontologia escolar à Estratégia Saúde da Família. 10.1590/S0104-12902011000400019Saude Soc. 2011;20(4):1033–1045. [Google Scholar]
- 11.Emmi DT, Barroso RFF. Avaliação das ações de saúde bucal no Programa Saúde da Família no distrito de Mosqueiro, Pará. 10.1590/S1413-81232008000100008Cienc Saude Coletiva. 2008;13(1):35–41. doi: 10.1590/s1413-81232008000100008. [DOI] [PubMed] [Google Scholar]
- 12.Esposti CDD, Oliveira AE, Silva MZ, Lima RCD. Perspectivas da saúde bucal na Estratégia Saúde da Família: dificuldades e avanços. UFES Rev Odontol. 2006;8(3):49–54. [Google Scholar]
- 13.Esposti CDD, Oliveira AE, Santos ET, Neto, Zandonade E. O processo de trabalho do técnico em saúde bucal e suas relações com a equipe de saúde bucal na Região Metropolitana da Grande Vitória, Espírito Santo, Brasil. 10.1590/S0104-12902012000200011Saude Soc. 2012;21(2):372–385. [Google Scholar]
- 14.Faccin D, Sebold R, Carcereri DL. Processo de trabalho em saúde bucal: em busca de diferentes olhares para compreender e transformar a realidade. 10.1590/S1413-81232010000700076Cienc Saude Coletiva. 2010;15(Supl 1):1643–1652. doi: 10.1590/s1413-81232010000700076. [DOI] [PubMed] [Google Scholar]
- 15.Gonçalves RJ, Soares RA, Troll T, Cyrino EG. Ser médico no PSF: formação acadêmica, perspectivas e trabalho cotidiano. 10.1590/S0100-55022009000300009Rev Bras Educ Med. 2009;33(3):382–392. [Google Scholar]
- 16.Holanda ALF, Barbosa AAA, Brito EWG. Reflexões acerca da atuação do agente comunitário de saúde nas ações de saúde bucal. 10.1590/S1413-81232009000800024Cienc Saude Coletiva. 2009;14(Supl 1):1507–1512. doi: 10.1590/s1413-81232009000800024. [DOI] [PubMed] [Google Scholar]
- 17.Jatrana S, Crampton P, Filoche S. The case for integrating oral health into primary health care. N Z Med J. 2009;122(1301):43–52. [PubMed] [Google Scholar]
- 18.Koyashiki GAK, Alves-Souza RA, Garanhani ML. O trabalho em saúde bucal do agente comunitário de saúde em unidades de Saúde da Família. 10.1590/S1413-81232008000400032Cienc Saude Coletiva. 2008;13(4):1343–1354. doi: 10.1590/s1413-81232008000400032. [DOI] [PubMed] [Google Scholar]
- 19.Lourenço EC, Silva ACB, Meneghin MC, Pereira AC. A inserção dos serviços de saúde bucal no Programa Saúde da Família no Estado de Minas Gerais. 10.1590/S1413-81232009000800009Cienc Saude Coletiva. 2009;14(Supl 1):1367–1377. doi: 10.1590/s1413-81232009000800009. [DOI] [PubMed] [Google Scholar]
- 20.Lucena EHG, Pucca JR GA, Sousa MF. A Política Nacional de Saúde Bucal no Brasil no contexto do Sistema Único de Saúde. [cited 2015 May 11];Tempus Actas Saude Coletiva [Internet] 2011 5(3):53–63. http://www.tempus.unb.br/index.php/tempus/article/view/1042/951. [Google Scholar]
- 21.Martelli PJL, Cabral APS, Pimentel FC, Macedo CLSV, Monteiro IS, Silva SF. Análise do modelo de atenção à saúde bucal em municípios do estado de Pernambuco. 10.1590/S1413-81232008000500030Cienc Saude Coletiva. 2008;13(5):1669–1674. doi: 10.1590/s1413-81232008000500030. [DOI] [PubMed] [Google Scholar]
- 22.Martelli PJL, Macedo CLSV, Medeiros KR, Silva SF, Cabral APS, Pimentel FC, et al. Perfil do cirurgião-dentista inserido na Estratégia de Saúde da Família em municípios do estado de Pernambuco, Brasil. 10.1590/S1413-81232010000800029Cienc Saude Coletiva. 2010;15(Supl 2):3243–3248. doi: 10.1590/s1413-81232010000800029. [DOI] [PubMed] [Google Scholar]
- 23.Matos PES, Tomita NE. A inserção da saúde bucal no Programa Saúde da Família: da universidade aos pólos de capacitação. 10.1590/S0102-311X2004000600011Cad Saude Publica. 2004;20(6):1538–1544. doi: 10.1590/s0102-311x2004000600011. [DOI] [PubMed] [Google Scholar]
- 24.Mattos RA. A integralidade na prática (ou sobre a prática da integralidade) 10.1590/S0102-311X2004000500037Cad Saude Publica. 2004;20(5):1411–1416. doi: 10.1590/s0102-311x2004000500037. [DOI] [PubMed] [Google Scholar]
- 25.Mendonça MHM, Martins MIC, Giovanella L, Escorel S. Desafios para gestão do trabalho a partir de experiências exitosas de expansão da Estratégia de Saúde da Família. 10.1590/S1413-81232010000500011Cienc Saude Coletiva. 2010;15(5):2355–2365. doi: 10.1590/s1413-81232010000500011. [DOI] [PubMed] [Google Scholar]
- 26.Mialhe FL, Lefèvre F, Lefèvre AMC. O agente comunitário de saúde e suas práticas educativas em saúde bucal: uma avaliação qualiquantitativa. 10.1590/S1413-81232011001200015Cienc Saude Coletiva. 2011;16(11):4425–4432. doi: 10.1590/s1413-81232011001200015. [DOI] [PubMed] [Google Scholar]
- 27.Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica . Saúde bucal. Brasília (DF): 2006. (Cadernos de Atenção Básica, n. 17). http://bvsms.saude.gov.br/bvs/publicacoes/abcad17.pdf. [Google Scholar]
- 28.Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica 10 anos de Brasil Sorridente: milhões de sorrisos. Rev Bras Saude Familia. 2012;1(1):74–77. http://dab.saude.gov.br/portaldab/biblioteca.php?conteudo=publicacoes/revista_saude_familia35_36. [Google Scholar]
- 29.Moura MS, Carvalho CJ, Amorim JTC, Marques MFSS, Moura LFAD, Mendes RF. Perfil e práticas de saúde bucal do agente comunitário de saúde em municípios piauienses de pequeno porte. 10.1590/S1413-81232010000700061Cienc Saude Coletiva. 2010;15(Supl 1):1487–1495. doi: 10.1590/s1413-81232010000700061. [DOI] [PubMed] [Google Scholar]
- 30.Moura MS, Ferro FEFD, Cunha NL, Nétto OBS, Lima MDM, Moura LFAD. Saúde bucal na Estratégia de Saúde da Família em um colegiado gestor regional do estado do Piauí. 10.1590/S1413-81232013000200018Cienc Saude Coletiva. 2013;18(2):471–480. doi: 10.1590/s1413-81232013000200018. [DOI] [PubMed] [Google Scholar]
- 31.Moysés SJ, Pucca GA, Junior, Paludetto M, Junior, Moura L. Avanços e desafios à Política de Vigilância à Saúde Bucal no Brasil. 10.1590/S0034-8910.2013047004329Rev Saude Publica. 2013;47(Suppl 3):161–167. doi: 10.1590/s0034-8910.2013047004329. [DOI] [PubMed] [Google Scholar]
- 32.Nascimento AC, Moysés ST, Bisinelli JC, Moysés SJ. Oral health in the family health strategy: a change of practices or semantics diversionism. 10.1590/S0034-89102009005000015Rev Saude Publica. 2009;43(3):455–462. doi: 10.1590/s0034-89102009000300009. [DOI] [PubMed] [Google Scholar]
- 33.Nascimento AC, Moyses ST, Werneck RI, Moyses SJ. Oral health in the context of primary care in Brazil. 10.1111/idj.12039Int Dent J. 2013;63(5):237–243. doi: 10.1111/idj.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nuto SAS, Oliveira GC, Andrade JV, Maia MCG. O acolhimento em saúde bucal na Estratégia de Saúde da Família, Fortaleza-CE: um relato de experiência. Rev APS. 2010;13(4):505–509. [Google Scholar]
- 35.Pereira DQ, Pereira JCM, Assis MMA. A prática odontológica em Unidades Básicas de Saúde em Feira de Santana (BA) no processo de municipalização da saúde: individual, curativa, autônoma e tecnicista. 10.1590/S1413-81232003000200020Cienc Saude Coletiva. 2003;8(2):599–609. [Google Scholar]
- 36.Pezzato LM, L’Abbate S, Botazzo C. Produção de micropolíticas no processo de trabalho em saúde bucal: uma abordagem sócioanalítica. 10.1590/S1413-81232013000700025Cienc Saude Coletiva. 2013;18(7):2095–2104. doi: 10.1590/s1413-81232013000700025. [DOI] [PubMed] [Google Scholar]
- 37.Pimentel FC, Martelli PJL, Araújo JLAC, Júnior, Lima AS, Santana VGD, Macedo CLSV. Evolução da assistência em saúde bucal na Estratégia de Saúde da Família do município do Recife (PE) no período de 2001 a 2007. Rev Baiana Saude Publica. 2008;32(2):253–264. [Google Scholar]
- 38.Pimentel FC, Martelli PJL, Araújo JLAC, Junior, Aciolli RML, Macedo CLSV. Análise da atenção à saúde bucal na Estratégia de Saúde da Família do Distrito Sanitário VI, Recife (PE) 10.1590/S1413-81232010000400033Cienc Saude Coletiva. 2010;15(4):2189–2196. doi: 10.1590/s1413-81232010000400033. [DOI] [PubMed] [Google Scholar]
- 39.Pimentel FC, Albuquerque PC, Martelli PJL, Souza WV, Acioli RML. Caracterização do processo de trabalho das equipes de saúde bucal em municípios do Estado de Pernambuco, Brasil, segundo porte populacional: da articulação comunitária à organização do atendimento clínico. 10.1590/S0102-311X2012001300015Cad Saude Publica. 2012;28(Suppl):s146–s157. doi: 10.1590/s0102-311x2012001300015. [DOI] [PubMed] [Google Scholar]
- 40.Rocha ECA, Araújo MAD. Condições de trabalho das equipes de saúde bucal no Programa Saúde da Família: o caso do Distrito Sanitário Norte em Natal, RN. 10.1590/S0034-76122009000200010Rev Adm Publica. 2009;43(2):481–517. [Google Scholar]
- 41.Rodrigues AAAO, Assis MMA. Oferta e demanda na atenção à saúde bucal: o processo de trabalho no Programa Saúde da Família em Alagoinhas – Bahia. Rev Baiana Saude Publica. 2005;29(2):273–285. [Google Scholar]
- 42.Rodrigues AAAO, Gallotti AP, Pena SFA, Ledo CAS. Saúde bucal no programa de saúde da família na cidade de Feira de Santana (BA): o perfil do cirurgião-dentista. Rev Baiana Saude Publica. 2009;33(4):582–594. [Google Scholar]
- 43.Rodrigues AAAO, Santos AM, Assis MMA. Agente comunitário de saúde: sujeito da prática em saúde bucal em Alagoinhas, Bahia. 10.1590/S1413-81232010000300034Cienc Saude Coletiva. 2010;15(3):907–915. doi: 10.1590/s1413-81232010000300034. [DOI] [PubMed] [Google Scholar]
- 44.Rodrigues AAAO, Assis MMA, Nascimento MAA, Fonsêca GS, Siqueira DVS. Saúde bucal na Estratégia Saúde da Família em um município do semiárido baiano. Rev Baiana Saude Publica. 2011;35(3):695–709. [Google Scholar]
- 45.Sanglard-Oliveira CA, Werneck MAF, Lucas SD, Abreu MHNG. Atribuições dos técnicos em saúde bucal na Estratégia Saúde da Família em Minas Gerais, Brasil. 10.1590/S1413-81232013000800030Cienc Saude Coletiva. 2013;18(8):2453–2460. doi: 10.1590/s1413-81232013000800030. [DOI] [PubMed] [Google Scholar]
- 46.Santos AM, Assis MMA, Rodrigues AAAO, Nascimento MAA, Jorge MSB. Linhas de tensões no processo de acolhimento das equipes de saúde bucal do Programa Saúde da Família: o caso de Alagoinhas, Bahia, Brasil. 10.1590/S0102-311X2007000100009Cad Saude Publica. 2007;23(1):75–85. doi: 10.1590/s0102-311x2007000100009. [DOI] [PubMed] [Google Scholar]
- 47.Santos AM, Assis MMA, Nascimento MAA, Jorge MSB. Vínculo e autonomia na prática de saúde bucal no Programa Saúde da Família. 10.1590/S0034-89102008005000025Rev Saude Publica. 2008;42(3):464–470. doi: 10.1590/s0034-89102008005000025. [DOI] [PubMed] [Google Scholar]
- 48.Scherer MDA, Marino SRA, Ramos FRS. Rupturas e resoluções no modelo de atenção à saúde: reflexões sobre a Estratégia Saúde da Família com base nas categorias kuhnianas. 10.1590/S1414-32832005000100005Interface (Botucatu) 2005;9(6):53–66. [Google Scholar]
- 49.Scherer MDA, Pires DEP, Soratto J. Sousa MF, Franco MS, Mendonça AVM.organizadores . Saúde da Família nos municípios brasileiros: os reflexos dos 20 anos do espelho do futuro. Campinas: Saberes; 2014. O trabalho na Estratégia Saúde da Família; pp. 521–571. [Google Scholar]
- 50.Silva JM, Caldeira AP. Modelo assistencial e indicadores de qualidade da assistência: percepção dos profissionais da atenção primária à saúde. 10.1590/S0102-311X2010000600012Cad Saude Publica. 2010;26(6):1187–1193. doi: 10.1590/s0102-311x2010000600012. [DOI] [PubMed] [Google Scholar]
- 51.Silva KL, Rodrigues AT. Ações intersetoriais para promoção da saúde na Estratégia Saúde da Família: experiências, desafios e possibilidades. 10.1590/S0034-71672010000500011Rev Bras Enferm. 2010;63(5):762–769. doi: 10.1590/s0034-71672010000500011. [DOI] [PubMed] [Google Scholar]
- 52.Silva LA, Casotti CA, Chaves SCL. A produção científica brasileira sobre a Estratégia Saúde da Família e a mudança no modelo de atenção. 10.1590/S1413-81232013000100023Cienc Saude Coletiva. 2013;18(1):221–232. doi: 10.1590/s1413-81232013000100023. [DOI] [PubMed] [Google Scholar]
- 53.Silva SF, Martelli PJL, Sá DA, Cabral AP, Pimentel FC, Monteiro IS, et al. Análise do avanço das equipes de saúde bucal inseridas na Estratégia Saúde da Família em Pernambuco, região Nordeste, Brasil, 2002 a 2005. 10.1590/S1413-81232011000100024Cienc Saude Coletiva. 2011;16(1):211–220. doi: 10.1590/s1413-81232011000100024. [DOI] [PubMed] [Google Scholar]
- 54.Soares FF, Figueiredo CRV, Borges NCM, Jordão RA, Freire MCM. Atuação da equipe de saúde bucal na Estratégia Saúde da Família: análise dos estudos publicados no período 2001-2008. 10.1590/S1413-81232011000800017Cienc Saude Coletiva. 2011;16(7):3169–3180. doi: 10.1590/s1413-81232011000800017. [DOI] [PubMed] [Google Scholar]
- 55.Sousa MF, Hamann EM. Programa Saúde da Família no Brasil: uma agenda incompleta? 10.1590/S1413-81232009000800002Cienc Saude Coletiva. 2009;14(Supl 1):1325–1335. doi: 10.1590/s1413-81232009000800002. [DOI] [PubMed] [Google Scholar]
- 56.Souza LGS, Menandro MCS. Atenção primária à saúde: diretrizes, desafios e recomendações: revisão de bibliografia internacional. 10.1590/S0103-73312011000200010Physis Rev Saude Coletiva. 2011;21(2):517–539. [Google Scholar]
- 57.Souza TMS, Roncalli AG. Saúde bucal no Programa Saúde da Família: uma avaliação do modelo assistencial. 10.1590/S0102-311X2007001100020Cad Saude Publica. 2007;23(11):2727–2739. doi: 10.1590/s0102-311x2007001100020. [DOI] [PubMed] [Google Scholar]
- 58.Viegas SMF, Penna CMM. A construção da integralidade no trabalho cotidiano da equipe saúde da família. 10.1590/S1414-81452013000100019Esc Anna Nery. 2013;17(1):133–141. [Google Scholar]
- 59.World Health Organization, Collaborating Centre for Education, Training and Research in Oral Health . WHO Global Oral Health Database. Malmö: 2011. [cited 2012 Apr 15]. http://www.mah.se/CAPP/ [Google Scholar]