Significance
Influenza pandemics occur several times per century, causing millions of deaths. For one of the myriad of zoonotic influenza viruses to do so, a virus containing a hemagglutinin (HA) surface antigen previously unseen by most humans must evolve the necessary, albeit largely unknown, properties for sustained respiratory spread between people. During entry, the prototypic viral fusion protein HA binds receptors and is triggered irreversibly by low pH in endosomes to cause membrane fusion. These studies link a fundamental property, activation energy of a fusion protein measured as its pH of activation (acid stability), to the ability of zoonotic influenza viruses to cause a human pandemic. Monitoring HA stability is expected to enhance prepandemic surveillance and control of emerging influenza viruses.
Keywords: influenza virus, pandemic, transmission, membrane fusion, fusion glycoprotein
Abstract
Influenza pandemics require that a virus containing a hemagglutinin (HA) surface antigen previously unseen by a majority of the population becomes airborne-transmissible between humans. Although the HA protein is central to the emergence of a pandemic influenza virus, its required molecular properties for sustained transmission between humans are poorly defined. During virus entry, the HA protein binds receptors and is triggered by low pH in the endosome to cause membrane fusion; during egress, HA contributes to virus assembly and morphology. In 2009, a swine influenza virus (pH1N1) jumped to humans and spread globally. Here we link the pandemic potential of pH1N1 to its HA acid stability, or the pH at which this one-time-use nanomachine is either triggered to cause fusion or becomes inactivated in the absence of a target membrane. In surveillance isolates, our data show HA activation pH values decreased during the evolution of H1N1 from precursors in swine (pH 5.5–6.0), to early 2009 human cases (pH 5.5), and then to later human isolates (pH 5.2–5.4). A loss-of-function pH1N1 virus with a destabilizing HA1-Y17H mutation (pH 6.0) was less pathogenic in mice and ferrets, less transmissible by contact, and no longer airborne-transmissible. A ferret-adapted revertant (HA1-H17Y/HA2-R106K) regained airborne transmissibility by stabilizing HA to an activation pH of 5.3, similar to that of human-adapted isolates from late 2009–2014. Overall, these studies reveal that a stable HA (activation pH ≤ 5.5) is necessary for pH1N1 influenza virus pathogenicity and airborne transmissibility in ferrets and is associated with pandemic potential in humans.
Wild aquatic birds are thought to be the natural reservoir of influenza A viruses (1). Influenza pandemics occur every few decades, and swine are widely believed to be a key factor in the genesis of pandemics by facilitating reassortment of the eight viral gene segments and replacing avian-like (α-2,3-linked) hemagglutinin (HA) sialic acid receptor-binding specificity with human-like (α-2,6-linked) (2). If the molecular adaptations that allow efficient human-to-human transmissibility are understood, then circulating viruses undergoing these changes (i.e., those with the greatest pandemic potential) could be identified.
In 2009, pandemic (p) H1N1 emerged from swine and swiftly infected more than 60 million people, causing 12,000 US deaths in the first year (3). The pandemic strain originated by reassortment in swine, combining five genes (PB1, PB2, PA, NP, and NS) from North American triple-reassortant swine (TRS) viruses, two genes (NA and M) from Eurasian avian-like swine viruses, and an HA gene closely related to that of the classical swine lineage (4). pH1N1 viruses continue to circulate as seasonal H1N1 viruses. They retain several known pandemic traits, including α-2,6-linked sialic acid receptor-binding specificity of the HA, functional balance of HA and NA activity, and a polymerase adapted to the mammalian upper airway (5). Although these traits appear to be necessary for airborne transmissibility of influenza viruses, they do not appear to be sufficient. For example, H5N1 viruses engineered to have these traits were not air-transmissible among ferrets until a mutation increased HA thermostability and lowered the HA activation pH (6–8). The importance of HA stabilization in supporting the adaptation of influenza viruses to humans or enabling a human pandemic is not completely understood.
After receptor binding and endocytosis, low pH triggers irreversible structural changes in the HA protein that fuse the viral envelope and host endosomal membrane (9). Measured HA activation pH values across all subtypes and species range from ∼5.0 to 6.0, trending higher in avian viruses (pH 5.6–6.0) and lower in human viruses (pH 5.0–5.5) (10).
The goal of this study was to define the role of HA acid stability in pH1N1 pandemic capability. Our data show that HA activation pH decreased as H1N1 adapted from swine to humans. Complementary experiments in ferrets recapitulated this evolution, as we observed a loss-of-function pH1N1 virus acquired airborne transmissibility via stabilizing mutations. Overall, these studies link a fundamental molecular property, the barrier for activation of a membrane fusion protein (for influenza virus HA, its acid stability), to the interspecies adaptation of a ubiquitous respiratory virus.
Results
HA Activation pH of Swine H1 Viruses.
To investigate the contribution of HA acid stability in the emergence of pH1N1, we first measured the HA activation pH values of 38 antecedent H1 swine viruses representing classical swine, North American TRS, and Eurasian avian-like lineages (SI Appendix, Table S1 and Fig. S1 A and B). Syncytia assays were performed after infecting Vero cells with influenza viruses. Classical swine and North American TRS H1 viruses had HA activation pH values ranging from 5.5 to 5.9 and from 5.4 to 5.8, respectively (Fig. 1). Eurasian avian-like swine viruses had a mean activation pH of 5.8–6.0 (Fig. 1), overlapping the values from classical swine and TRS lineages, but trending higher. The relatively high HA activation pH values for the avian-like swine viruses is consistent with their greater similarity to avian H1 viruses (SI Appendix, Fig. S1B), which we found to have a high, albeit broad, range of HA activation pH (5.5–6.2). Human pH1N1 viruses A/CA/04/2009 and A/TN/1–560/2009, which were isolated at the start of the pandemic, had mean an HA activation pH of 5.6 and 5.5, respectively (Fig. 1), which is moderately higher than the activation values (pH 5.0–5.3) of early pandemic viruses from the three 20th-century pandemics (10). Later pH1N1 viruses isolated from 2010 to 2012 were lower (pH 5.2–5.4), which is more in line with the 20th-century pandemic viruses. Before the emergence of TRS viruses, few human infections with classical swine viruses were reported. To determine whether HA acid stability could have contributed to dead-end outcomes of classical swine virus infections in humans, we measured the activation pH of two such viruses recovered from humans (A/Wisconsin/301/1976, A/Ohio/3559/1988). These pH values were 5.8 and 5.6, respectively, which is higher than values in human-adapted viruses. Overall, these data suggest that the H1 viruses have a preferred HA activation pH of 5.5–6.0 in swine, a tolerable range of 5.5–5.6 in humans early during a pandemic, and a preferred range of 5.0–5.4 in humans after sustained circulation.
Fig. 1.
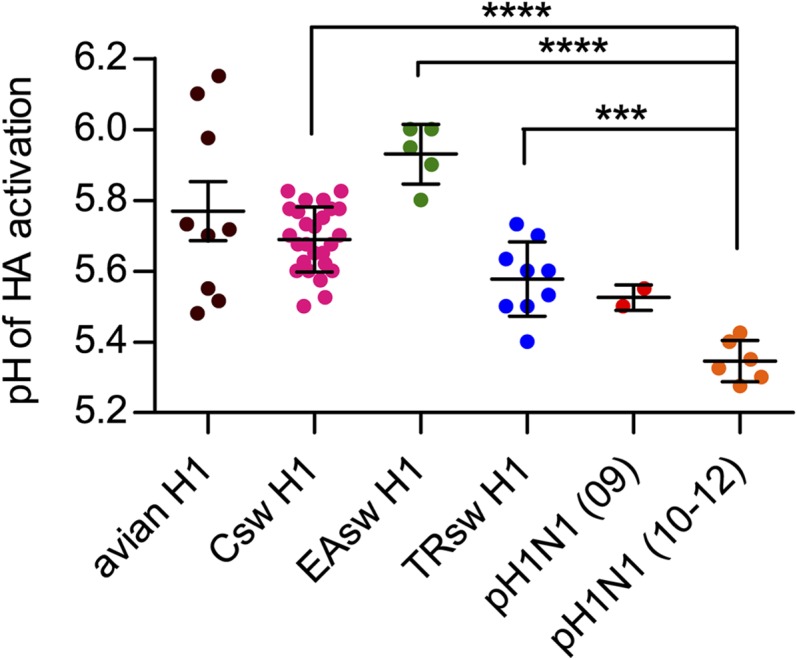
HA activation pH values for pH1N1 influenza viruses and potential H1 swine precursors. HA activation pH was determined by syncytia assays in virus-infected Vero cells. Each dot represents HA activation pH of an individual virus. Swine viruses are from classical (Csw), Eurasian avian-like (EAsw), and North American triple-reassortant (TRsw) lineages. Human isolates are pH1N1. Avian isolates are H1N1 duck and shorebird viruses. Mean (±SD) of two to three independent experiments with duplicates is shown. Virus abbreviations are described in SI Appendix, Fig. S1. **P < 0.01, ***P < 0.001, ****P < 0.0001, Student t test.
In Vitro Properties of an HA-Destabilized pH1N1 Virus.
To examine how HA acid stability influences virus fitness, we engineered an HA-destabilizing HA1-Y17H mutation into the fusion peptide pocket of the HA stalk of A/Tennessee/1–560/2009, an early pH1N1 isolate. Residue 17 in H3 numbering is residue 24, starting from the initiating methionine in the H1 HA protein. Y17 allows a direct hydrogen bond to the fusion peptide, but H17 does not, thereby destabilizing the HA protein (SI Appendix, Fig. S2). H17 occurs rarely in swine H1 viruses (2 of 9,574), which have group 1 HA proteins. However, H17 is nearly universally conserved in the group 2 HA proteins of the H3, H4, H7, H10, H14, and H15 subtypes. A loss-of-function approach was used because of the current suspension of gain-of-function research on influenza viruses.
The destabilizing Y17H mutation increased both the pH of activation and the pH of inactivation of the HA protein from 5.5 (WT) to 6.0 (Y17H) (SI Appendix, Fig. S3 A–C). This relatively high activation pH is common in avian and some swine viruses (10), and we wished to determine its effect on replication in mammals. As HA receptor-binding specificity contributes to H1 influenza virulence and transmissibility in mammals (11), we first analyzed the receptor preference of the mutant. The Y17H mutation did not alter the binding preference of the pH1N1 HA protein for α-2,6-linked glycans (SI Appendix, Fig. S3D). WT and Y17H HA proteins were comparably expressed and cleaved in infected cells (SI Appendix, Fig. S3E), suggesting the mutation does not alter HA protein folding and processing. The WT and Y17H pH1N1 had similar replication kinetics in MDCK, A549, and primary normal human bronchial epithelial cells (SI Appendix, Fig. S3 F–H), suggesting virus packaging and infectivity are not affected by the mutation.
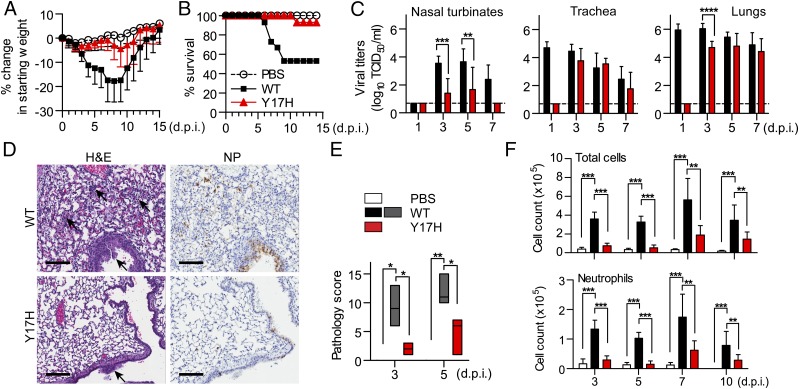
An HA-Destabilizing Mutation Attenuates pH1N1 Replication and Pathogenicity in Mice.
We next investigated in vivo whether HA acid stability affects pathogenicity. We inoculated DBA2/J mice intranasally with 750 plaque-forming units (PFU) of WT or Y17H pH1N1 virus. WT virus caused ∼20% weight loss and 50% mortality, whereas Y17H virus caused minimal weight loss and <10% mortality (Fig. 2 A and B). Peak titers of Y17H virus were delayed ∼2 d and were reduced ∼10- to 100-fold in the nasal turbinates, trachea, and lungs (Fig. 2C and SI Appendix, Table S2).
Fig. 2.
Pathogenicity in mice. DBA/2J mice were inoculated with 750 PFU of virus or with vehicle (PBS). Mean (±SD) percentage weight change (A) and survival (B) are reported at the indicated d.p.i. in groups of 15 mice. (C) Mean (±SD) virus titers in nasal turbinates, trachea, and lungs in groups of eight mice. Dashed line shows limit of detection. (D) Histology slides were stained with hematoxylin and eosin (H&E) or polyclonal anti-NP antisera. Representative lung sections at 3 d.p.i. Black arrows show lesions, including alveoli thickening, inflammatory cell infiltration of the airway, and epithelial necrosis of bronchi/bronchioles causing cell debris in the lumen. Numerous bronchiolar epithelial cells expressed viral NP proteins in WT virus-infected mice, but only a few in Y17H virus-infected mice. The control group showed no damage or NP staining. (Scale bar, 100 μm.) (E) Median (range) pathology scores for lung histology. (F) Mean (±SD) total number of cells (Top) and neutrophils (Bottom) in bronchoalveolar lavage fluid at the indicated d.p.i. in groups of five to six mice. For the Student test (C and E) and one-way ANOVA followed by Tukey post hoc test (F), significance is as follows: *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001.
pH1N1 infection in humans can cause acute lung injury and acute respiratory distress syndrome (12). In the DBA2/J mice, viral NP staining revealed that both viruses infected epithelial cells of the bronchi/bronchioles and pneumocytes in the alveoli (Fig. 2D). However, the WT virus spread more extensively in the epithelial cells of the airways and alveoli, causing severe bronchiolitis (with greater necrosis of epithelial cells, edema, and perivasculitis) and diffuse alveolar damage (including greater interstitial septal thickening, infiltration of mixed inflammatory cells, and regenerative pneumocyte hyperplasia) (Fig. 2D). Pathology scores for Y17H virus were significantly less (P < 0.05) at 3 and 5 d postinoculation (d.p.i.) than those of WT virus (Fig. 2E). We probed inflammation by assessing cell infiltration and cytokine/chemokine release in bronchoalveolar lavage fluid. The total cells and neutrophils, which help trigger lung repair and recruit adaptive effector cells, were 1.6–6.7 times lower in mice infected with Y17H pH1N1 than in mice infected with WT (P < 0.001 on days 3 and 5 p.i. and P < 0.01 on days 7 and 10 p.i.; Fig. 2F), consistent with minimal pathology. Y17H virus also caused less induction of proinflammatory cytokines and chemokines involved in the recruitment of immune cells or lung repair than WT pH1N1 (SI Appendix, Fig. S4A). The levels of those proinflammatory mediators remained significantly lower on days 5 (P < 0.05, P < 0.01, P < 0.001, and P < 0.0001) and 7 (P < 0.05 and P < 0.01) p.i. Y17H-infected mice also had minimal pulmonary vascular permeability and 2.5–3.3 times less extravasation of high-molecular-weight proteins in bronchoalveolar lavage fluid on days 5 (P < 0.01) and 7 (P < 0.001) p.i. (SI Appendix, Fig. S4 B and C). Overall, the data show that a destabilizing HA mutation (activation pH, 6.0) substantially reduces pH1N1 replication and pathogenesis in mice.
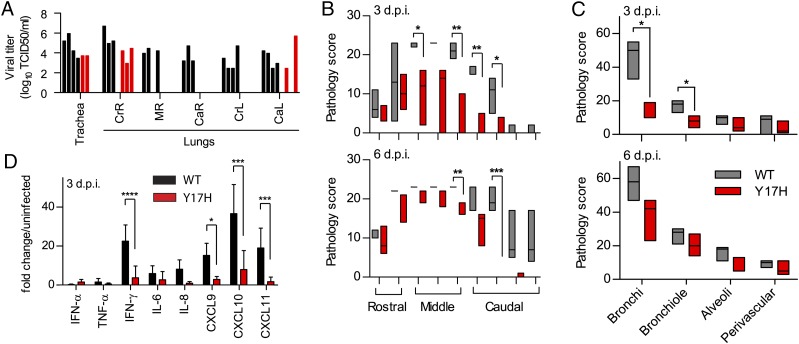
pH1N1 Pathogenicity and Airborne Transmissibility in Ferrets Require a Stable HA.
Ferrets are a well-established model for studies of influenza pathogenicity and transmissibility. Their lung physiology, receptor expression patterns, clinical signs, and transmission phenotypes resemble those in humans (13). We intranasally inoculated 5-mo-old female ferrets with 106 PFU of WT or Y17H pH1N1 virus and collected tissues 3 and 6 d.p.i. Whereas WT virus was recovered from the tracheas and three to five lung lobes in all four ferrets, the Y17H mutant was recovered from only two tracheas and one to two lung lobes (Fig. 3A). Peak titers of Y17H virus in nasal washes occurred 2 d later and were lower by a factor of 100 than those of WT virus (Fig. 4A). Both WT and Y17H viruses infected the submucosal glands and the epithelial cells of the nasal turbinates, bronchi/bronchioles, and alveoli (SI Appendix, Fig. S5 A and B). However, Y17H pH1N1 spread less efficiently early in infection (SI Appendix, Table S2 and Fig. S5A). The overall blinded histopathology score in Y17H virus–infected ferrets of the nasal turbinates and lungs was significantly lower than in WT-infected ferrets (Fig. 3 B and C). The lesions showed alveolar septal thickening, infiltration of inflammatory cells including monocytes/macrophages in the alveoli, pneumocyte hyperplasia, and bronchial and bronchiolar epithelial necrosis (SI Appendix, Fig. S5 A and C). In addition, the Y17H group also showed significantly less damage in the nasal turbinates and lower induction of proinflammatory cytokines (Fig. 3 B and D).
Fig. 3.
Pathogenicity in ferrets. Ferrets were inoculated intranasally with 106 PFU of virus or PBS. Nasal turbinates, trachea, and lung lobes were harvested from four ferrets at 3 and 6 d.p.i. (A) Virus titers in the trachea and cranial right (CrR), middle right (MR), caudal right (CaR), cranial left (CrL), and caudal left (CaL) lung lobes at 3 d.p.i. Each bar represents an individual animal. No virus was detected at 6 d.p.i. (B and C) Pathology scores. Median (range) pathology scores correspond to lesions in the front, middle, and anterior nasal cavity (B) and bronchi, bronchioles, alveoli, and perivascular areas (C). (D) Mean (±SD) fold change of cytokine and chemokine concentration in the lungs by RT-PCR at 3 and 6 d.p.i. *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001; Student test.
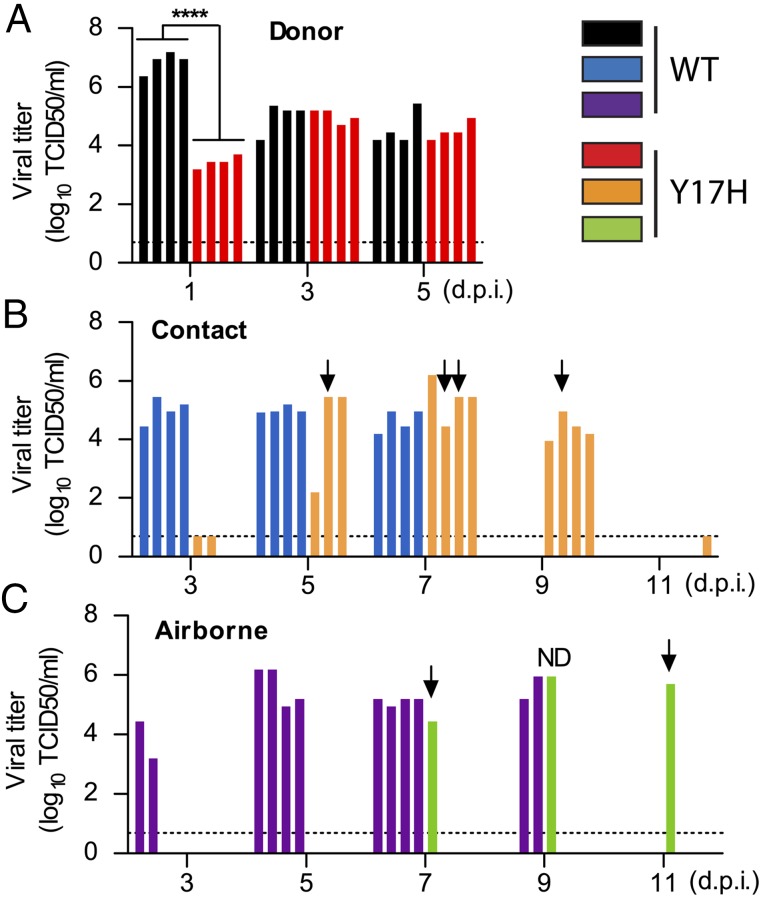
Fig. 4.
Influenza virus transmission in ferrets by contact and airborne routes. Four donor ferrets were inoculated intranasally with 106 PFU of WT (black bars) or Y17H-mutant (red bars) virus and were caged separately. The next day, one naive contact ferret was introduced into each cage (Contact: WT, blue bars; Y17H, orange bars), and another was placed in an adjacent cage that permitted only airborne contact. (Airborne: WT, purple bars; Y17H, green bars). (A–C) Titers of infectious virus in nasal washes of donor ferrets (A), contact ferrets (B), and airborne-contact ferrets (C). Downward arrows indicate subpopulations in the Y17H contact and airborne-contact ferrets with stabilized HA proteins (pH < 5.6). Each bar shows an individual animal. ****P < 0.0001; Student test. ND, not determined because there was insufficient sample for phenotypic testing from the airborne-contact ferret on day 9 p.i.
We next investigated the effect of a destabilized HA protein on direct contact and airborne transmission between ferrets. For each of four caging units per virus, one donor ferret was intranasally inoculated with 106 PFU virus. One day later, one naive ferret was moved into the same cage and one was moved into an adjacent cage, permitting only airborne transmission. Virus in nasal washes was titrated every other day. Both viruses transmitted by contact with 100% efficiency (four of four) (Fig. 4B). However, contact transmission of Y17H was delayed by 2 d, consistent with the 2-d delay in Y17H donors’ peak nasal virus titers. As expected for a human pandemic virus, WT pH1N1 was airborne-transmitted with 100% efficiency (four of four) by day 5 p.i. (Fig. 4C). Only one of four ferrets in the Y17H group transmitted by the airborne route, and transmission was detected 4 d later than in the WT group. All ferrets with nasal wash virus titers became seropositive (HI titer range, 320–2,560), whereas the three negative animals remained seronegative (SI Appendix, Fig. S6A). Further, WT- and Y17H-infected ferrets had similar neutralizing antibody and total IgG levels (SI Appendix, Fig. S6 A and B).
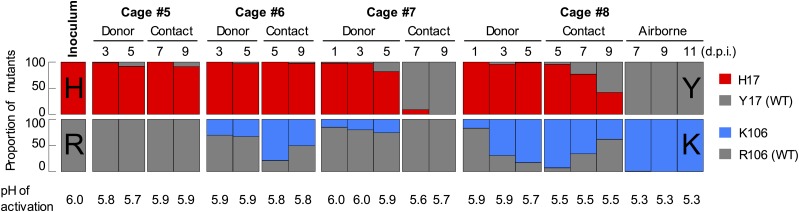
As direct contact transmission in the Y17H group was delayed and airborne transmission was relatively inefficient, we sought to identify potential adaptive mutations in the recipient hosts. From recipient animal nasal virus isolates, we measured the HA activation pH and sequenced the HA, NA, and M genes. The WT sequence and HA activation pH were maintained in the WT-infected group (SI Appendix, Table S3), consistent with its high fitness and airborne transmissibility in ferrets. In contrast, in donor and contact ferrets in the Y17H group, subpopulations of viruses developed with one or more HA sequence variations, including HA1-H17Y (reversion), HA1-T290A, HA1-S291N, HA2-R106K, and others (SI Appendix, Table S3). As a result, the HA activation pH values of virus isolates from Y17H-inoculated donors were reduced from 6.0 to 5.7–5.9, and those of their contact cage mates were reduced to 5.5–5.8.
In the case of airborne transmission of Y17H virus, the donor ferret in cage 8 retained the Y17H mutation (except for small proportion of reversion near the limit of detection of next-generation sequencing on day 3) and had an increasing subpopulation of HA2-R106K variants on days 1, 3, and 5 of 17%, 69%, and 83%, respectively (Fig. 5). In cage 8, virus first isolated from the contact ferret on day 5 contained 93% HA2-R106K and 5% HA1-H17Y. In the prefusion conformation, HA2 residue 106 resides at the core of the central triple-stranded coiled coil, at the hinge region between helices C and D that opens out after low-pH-induced activation (SI Appendix, Fig. S2). Mutations to residue 106 were previously found to alter HA acid stability in H2N2 and H3N2 influenza subtypes (14, 15). To study the effect of an HA2-R106K mutation, we used reverse genetics to rescue an A/TN/1–560/09 (pH1N1) virus containing HA2-R106K. The R106K mutation decreased the HA activation pH from 5.5 to 5.3 (SI Appendix, Fig. S7). All three virus samples collected on days 7, 9, and 11 from the cage 8 airborne recipient contained HA1-H17Y (revertant) and HA2-R106K within the limit of detection of next-generation sequencing (5%), and all had HA activation pH values of 5.3 (Fig. 5), similar to the reverse-genetics R106K mutant (SI Appendix, Fig. S7). The HA activation pH of 5.3 for the airborne-transmitted virus is within the range we had measured in natural pH1N1 viruses circulating in humans between 2010 and 2012 (5.2–5.4) (Fig. 1). We analyzed pH1N1 sequences and found that the HA2-K106 polymorphism was present in eight of 21,102 WT pH1N1 viruses recovered from humans in North America, Europe, Africa, and the Middle East between late 2009 and 2014 (GenBank accession numbers ACR15758, ADC32410, AFK14341, AFK14358, AGR50262, AHY84609, AGB13360, AHV83800).
Fig. 5.
Evolution of loss-of-function Y17H mutant after acquiring enhanced transmissibility in ferrets. Viruses from the Y17H group in the experiment described in Fig. 4 were isolated so that their HA genes could be sequenced and HA activation pH values measured. Bar charts for each of the four cages (5–8) show the proportion of mutations with each residue at positions HA1-17 and HA2-106 over the course of infection. Proportions were determined by next-generation sequencing. At HA1 position 17, red bars correspond to H17 (inoculated virus) and gray bars to Y17 (stabilized revertant). At HA2 position 106, gray bars correspond to R106 (inoculated virus) and blue bars to K106 (stabilized mutant). The isolated viruses were then propagated for measurement of the pH of HA activation by syncytia assay (mean of two independent assays, each performed in duplicate). Airborne transmission was only detected in cage 8. For the cage 5 and cage 6 donors on day 1 and the cage 5 contact recipient on day 5, sufficient sample was not available for next-generation sequencing, but Sanger sequencing showed no difference from the inoculated virus (HA1-H17 and HA2-R106).
Discussion
The HA protein plays a central role in human influenza pandemics, yet the HA molecular properties required for pandemic potential remain largely undefined. Influenza virus pathogenicity has been clearly linked to its HA cleavage site sequence, which helps determine in which tissues the HA protein can be activated to cause membrane fusion and enter cells (16). Influenza virus transmissibility in humans, and in ferret and guinea pig animal models, has been linked to the specificity of the HA protein to bind sialic acid-containing receptors that are abundant in the upper respiratory tract (2, 5). Human pandemic viruses have also been loosely associated with a functional balance between HA receptor-binding avidity and NA receptor-destroying activities (17). Here we showed that a relatively stable HA protein (activation pH ≤ 5.5) is necessary for the pandemic capacity of 2009 pH1N1 influenza virus. The HA activation pH was 5.5–6.0 in swine influenza virus precursors, ∼5.5 in human pH1N1 isolates at the start of the pandemic, and 5.2–5.4 in subsequent human-adapted pH1N1 isolates. Thus, the pH1N1 HA protein has become more acid-stable as it has evolved from swine to human hosts. In mice and ferrets, the growth of our prototypic early pandemic 2009 virus engineered to have a higher activation pH (by virtue of an HA1-Y17H mutation) was delayed and reduced, thus reducing pathogenicity. The destabilized HA protein also eliminated airborne transmissibility in ferrets. Adaptation of the loss-of-function virus to ferrets resulted in an HA-stabilizing HA2-R106K mutation followed by HA1-H17Y reversion. These two mutations collectively lowered the activation pH to 5.3 and restored airborne transmission. HA stabilization would allow a human-adapted virus to avoid inactivation in the mildly acidic upper respiratory tract. Although several recent studies of highly pathogenic avian influenza (HPAI) viruses in animal models support the role of HA acid stability as a molecular “switch” for avian–ferret adaptation (18), our data directly link HA acid stability with a human H1N1 influenza pandemic. Overall, our ferret experiment recapitulated the natural phenotypic evolution of the pH1N1 HA in humans, at least with respect to HA acid stability.
H5 and H7 HPAI viruses have HA proteins that are cleaved intracellularly, which is necessary for systemic virus dissemination. Relatively unstable HA proteins from HPAI viruses are protected from inactivation while trafficking through the secretory pathway by M2 ion channel activity, which neutralizes the mildly acidic trans-Golgi compartment (19). In avian-like H5N1 viruses, relatively high HA activation pH values (5.6–6.0) were associated with greater growth and pathogenicity in chickens (20, 21) and greater growth and transmission in mallard ducks (22). A stabilizing mutation that reduced H5N1 HA activation pH from 5.9 to 5.4 attenuated growth and eliminated transmission in ducks but enhanced growth in the upper (but not lower) respiratory tracts of mice and ferrets (22–24). Here, stabilizing mutations that reduced pH1N1 HA activation pH from 6.0 to 5.3 enhanced upper respiratory growth and airborne transmissibility in ferrets. Similarly, two independent studies showed that adaptation of H5 viruses to the upper respiratory tracts of ferrets and the acquisition of airborne transmissibility required a mutation that lowered the HA activation pH from 5.6 to 5.2–5.4 (7, 8). In addition, α-2,6 sialic acid receptor specificity and efficient polymerase activity at 33 °C (the temperature of mammalian upper airways) were also required (8, 23, 25). In contrast to the upper respiratory tract, in the lungs, a lower HA activation pH has been associated with reduced virus growth and reduced or delayed pathogenicity for H5N1 viruses (23, 26). An opposite effect is reported here for pH1N1, for which a lower HA activation pH has been linked to increased growth in the lungs and increased pathogenicity. Further studies are needed to determine the extent to which differential HA cleavage and receptor binding specificity contribute to the apparent differences between HPAI and human seasonal influenza viruses in the lungs.
A mechanism by which HA acid stability regulates interspecies adaptation of influenza viruses is partially defined. When exposed to sufficiently low pH, the HA protein either is triggered to cause membrane fusion in the endosome or is inactivated by exposure to an acidic environment in the secretory pathway or outside the cell or host. An unstable HA protein is more prone to inactivation, whereas a very stable HA is more susceptible to lysosomal degradation. A higher HA activation pH (5.6–6.0) enhances replication of HPAI viruses in the enteric and respiratory tracts of ducks and chickens by facilitating membrane fusion (20, 22). Such facile activation of the HA protein leads to virion inactivation in mildly acidic pH environments, such as the mammalian upper respiratory tract (7, 8, 23, 25). The airways of mammals are mildly acidic (pH 5.5–6.9) (27) and become more acidic (pH 5.2) during influenza virus infection (28).
Surveillance reports after the 2009 pandemic identified another HA-stabilizing mutation (HA2-E47K) that may have played a role in adaptation of pH1N1 to humans (29, 30). Other viral genes may also contribute to pandemic capacity. Balanced HA and NA activity is reported in human pandemic viruses (17) and was shown to be required for pH1N1 airborne transmissibility in ferrets (31). NA enzymatic activity promotes release of influenza virions by preventing aggregation and enhancing penetration of the mucous layer (32). However, increased NA activity can also increase the HA activation pH of viruses (22). When introduced into pH1N1 virus, both the NA and M genes of a TRS virus reduced airborne transmissibility in ferrets (33). Conversely, introduction of pH1N1 NA and M genes into a swine virus enhanced transmission in swine (34). Introduction of the pH1N1 M gene alone into PR8 or a swine H3N2 virus allowed efficient airborne transmission in guinea pigs (35). The M gene encodes both the M1 matrix protein and the M2 ion channel. The HA destabilizing property of the M gene in the live attenuated vaccine backbone A/Ann Arbor/60 (H2N2) has been linked to M2 ion channel activity (36), which is required to prevent HA inactivation during trafficking in the mildly acidic secretory pathway (19). The M1 matrix protein contributes to virus assembly, budding, and morphology (37), which may also affect transmissibility (38).
At the heart of pandemic prevention is identification of emerging viruses that pose the greatest risk of adaptation to humans, so that infections can be contained and vaccine seed stocks can be produced. In some cases, swine may serve as a mixing vessel that allows avian-origin HA genes to evolve α-2,6 receptor-binding specificity and to acquire other properties through mutation and/or reassortment of gene segments. Our findings suggest that one of the molecular requirements for a pandemic influenza A virus is a stabilized HA protein with an activation pH of 5.5 or less, a value sufficiently low to allow airborne human-to-human transmission at the start of the 2009 pH1N1 pandemic. HA stabilization could occur in swine, other animal hosts, or directly in humans. Although swine influenza viruses only occasionally infect humans and rarely cause pandemics (39), they appear to pose an increasing risk. TRS viruses with human-like HA and NA proteins are airborne-transmissible in ferrets (40, 41). Moreover, diverse swine viruses to which humans lack immunity are emerging through reassortment with the pH1N1 viruses (42). This work and other recent studies suggest that the HA acid stability of emerging viruses is an important factor in their pandemic potential.
Materials and Methods
Cells and Viruses.
Cells, viruses, and in vitro experiments in this study are described in SI Appendix, Materials and Methods.
Animal Experiments.
Animal experiments were conducted in an ABSL2+ facility in compliance with the NIH and the Animal Welfare Act and with approval by the St. Jude Animal Care and Use Committee. Six-week-old female DBA/2J mice (Jackson Laboratories) and 5-mo-old male ferrets (Triple F farms) were anesthetized with isoflurane and intranasally inoculated with virus. Clinical signs, temperature, and weight were recorded daily. Details are in SI Appendix, Materials and Methods.
Statistical Analysis.
Student t test and one-way analysis of variance followed by the Tukey post hoc test were used to compare groups. P values < 0.05 were considered statistically significant. All statistical analyses were performed with GraphPad Prism5 software.
Supplementary Material
Acknowledgments
Paul Thomas, Sun Woo Yoon, and Zeynep Kocer provided viruses. The St. Jude Animal Resources Center, Hartwell Center for Bioinformatics and Biotechnology, Veterinary Pathology Core Laboratory, and Sharon Naron of Scientific Editing provided assistance. This work was supported by the NIH, National Institute of Allergy and Infectious Diseases (NIAID), Centers of Excellence for Influenza Research and Surveillance (Contract HHSN272201400006C), St. Jude Children's Research Hospital, and American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1524384113/-/DCSupplemental.
References
- 1.Krauss S, Webster RG. Avian influenza virus surveillance and wild birds: Past and present. Avian Dis. 2010;54(1) Suppl:394–398. doi: 10.1637/8703-031609-Review.1. [DOI] [PubMed] [Google Scholar]
- 2.Elderfield R, Barclay W. 2011. Influenza pandemics. Adv Exp Med Biol 719:81–103.
- 3.Neumann G, Noda T, Kawaoka Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature. 2009;459(7249):931–939. doi: 10.1038/nature08157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith GJ, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459(7250):1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 5.Belser JA, Maines TR, Tumpey TM, Katz JM. Influenza A virus transmission: Contributing factors and clinical implications. Expert Rev Mol Med. 2010;12:e39. doi: 10.1017/S1462399410001705. [DOI] [PubMed] [Google Scholar]
- 6.Chen LM, et al. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology. 2012;422(1):105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imai M, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486(7403):420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linster M, et al. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell. 2014;157(2):329–339. doi: 10.1016/j.cell.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: The influenza hemagglutinin. Annu Rev Biochem. 2000;69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 10.Galloway SE, Reed ML, Russell CJ, Steinhauer DA. Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: Implications for host range and adaptation. PLoS Pathog. 2013;9(2):e1003151. doi: 10.1371/journal.ppat.1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tumpey TM, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315(5812):655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Padilla R, et al. INER Working Group on Influenza Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361(7):680–689. doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 13.Belser JA, Katz JM, Tumpey TM. The ferret as a model organism to study influenza A virus infection. Dis Model Mech. 2011;4(5):575–579. doi: 10.1242/dmm.007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thoennes S, et al. Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology. 2008;370(2):403–414. doi: 10.1016/j.virol.2007.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu R, Wilson IA. Structural characterization of an early fusion intermediate of influenza virus hemagglutinin. J Virol. 2011;85(10):5172–5182. doi: 10.1128/JVI.02430-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bosch FX, Garten W, Klenk HD, Rott R. Proteolytic cleavage of influenza virus hemagglutinins: Primary structure of the connecting peptide between HA1 and HA2 determines proteolytic cleavability and pathogenicity of Avian influenza viruses. Virology. 1981;113(2):725–735. doi: 10.1016/0042-6822(81)90201-4. [DOI] [PubMed] [Google Scholar]
- 17.Xu R, et al. Functional balance of the hemagglutinin and neuraminidase activities accompanies the emergence of the 2009 H1N1 influenza pandemic. J Virol. 2012;86(17):9221–9232. doi: 10.1128/JVI.00697-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russell CJ. Acid-induced membrane fusion by the hemagglutinin protein and its role in influenza virus biology. Curr Top Microbiol Immunol. 2014;385:93–116. doi: 10.1007/82_2014_393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takeuchi K, Lamb RA. Influenza virus M2 protein ion channel activity stabilizes the native form of fowl plague virus hemagglutinin during intracellular transport. J Virol. 1994;68(2):911–919. doi: 10.1128/jvi.68.2.911-919.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DuBois RM, et al. Acid stability of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity. PLoS Pathog. 2011;7(12):e1002398. doi: 10.1371/journal.ppat.1002398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hulse DJ, Webster RG, Russell RJ, Perez DR. Molecular determinants within the surface proteins involved in the pathogenicity of H5N1 influenza viruses in chickens. J Virol. 2004;78(18):9954–9964. doi: 10.1128/JVI.78.18.9954-9964.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reed ML, et al. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity and transmissibility in ducks. J Virol. 2010;84(3):1527–1535. doi: 10.1128/JVI.02069-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zaraket H, et al. Increased acid stability of the hemagglutinin protein enhances H5N1 influenza virus growth in the upper respiratory tract but is insufficient for transmission in ferrets. J Virol. 2013;87(17):9911–9922. doi: 10.1128/JVI.01175-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zaraket H, Bridges OA, Russell CJ. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus replication and pathogenesis in mice. J Virol. 2013;87(9):4826–4834. doi: 10.1128/JVI.03110-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shelton H, Roberts KL, Molesti E, Temperton N, Barclay WS. Mutations in haemagglutinin that affect receptor binding and pH stability increase replication of a PR8 influenza virus with H5 HA in the upper respiratory tract of ferrets and may contribute to transmissibility. J Gen Virol. 2013;94(Pt 6):1220–1229. doi: 10.1099/vir.0.050526-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herfst S, et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336(6088):1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fischer H, Widdicombe JH. Mechanisms of acid and base secretion by the airway epithelium. J Membr Biol. 2006;211(3):139–150. doi: 10.1007/s00232-006-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacoby DB, Tamaoki J, Borson DB, Nadel JA. 1988. Influenza infection causes airway hyperresponsiveness by decreasing enkephalinase. J Appl Physiol (1985) 64(6):2653–2658. [DOI] [PubMed]
- 29.Cotter CR, Jin H, Chen Z. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog. 2014;10(1):e1003831. doi: 10.1371/journal.ppat.1003831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maurer-Stroh S, et al. A new common mutation in the hemagglutinin of the 2009 (H1N1) influenza A virus. PLoS Curr. 2010;2:RRN1162. doi: 10.1371/currents.RRN1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yen HL, et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc Natl Acad Sci USA. 2011;108(34):14264–14269. doi: 10.1073/pnas.1111000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wagner R, Matrosovich M, Klenk HD. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol. 2002;12(3):159–166. doi: 10.1002/rmv.352. [DOI] [PubMed] [Google Scholar]
- 33.Lakdawala SS, et al. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog. 2011;7(12):e1002443. doi: 10.1371/journal.ppat.1002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma W, et al. The neuraminidase and matrix genes of the 2009 pandemic influenza H1N1 virus cooperate functionally to facilitate efficient replication and transmissibility in pigs. J Gen Virol. 2012;93(Pt 6):1261–1268. doi: 10.1099/vir.0.040535-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chou YY, et al. The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J Virol. 2011;85(21):11235–11241. doi: 10.1128/JVI.05794-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Donnell CD, Vogel L, Matsuoka Y, Jin H, Subbarao K. The matrix gene segment destabilizes the acid and thermal stability of the hemagglutinin of pandemic live attenuated influenza virus vaccines. J Virol. 2014;88(21):12374–12384. doi: 10.1128/JVI.01107-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rossman JS, Lamb RA. Influenza virus assembly and budding. Virology. 2011;411(2):229–236. doi: 10.1016/j.virol.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Campbell PJ, et al. The M segment of the 2009 pandemic influenza virus confers increased neuraminidase activity, filamentous morphology, and efficient contact transmissibility to A/Puerto Rico/8/1934-based reassortant viruses. J Virol. 2014;88(7):3802–3814. doi: 10.1128/JVI.03607-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vincent A, et al. Review of influenza A virus in swine worldwide: A call for increased surveillance and research. Zoonoses Public Health. 2014;61(1):4–17. doi: 10.1111/zph.12049. [DOI] [PubMed] [Google Scholar]
- 40.Belser JA, et al. Pathogenesis and transmission of triple-reassortant swine H1N1 influenza viruses isolated before the 2009 H1N1 pandemic. J Virol. 2011;85(4):1563–1572. doi: 10.1128/JVI.02231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pascua PN, et al. Virulence and transmissibility of H1N2 influenza virus in ferrets imply the continuing threat of triple-reassortant swine viruses. Proc Natl Acad Sci USA. 2012;109(39):15900–15905. doi: 10.1073/pnas.1205576109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vijaykrishna D, et al. Reassortment of pandemic H1N1/2009 influenza A virus in swine. Science. 2010;328(5985):1529. doi: 10.1126/science.1189132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.