Abstract
Objective
Spirituality is favorably related to depression, quality of life, hospitalizations, and other important outcomes in congestive heart failure (CHF) patients but has not been examined as a predictor of mortality risk in this population. Given the well-known difficulties in managing CHF, we hypothesized that spirituality would be associated with lower mortality risk, controlling for baseline demographics, functional status, health behaviors, and religiousness.
Method
Participants were 191 CHF patients (64% male; Mage = 68.6 years, SD = 10.1) who completed a baseline survey and were then followed for five years.
Results
Nearly one third of the sample (32%) died during the study period. Controlling for demographics and health status, smoking more than doubled the risk of mortality, while alcohol consumption was associated with slightly lower risk of mortality. Importantly, adherence to healthy lifestyle recommendations was associated with halved mortality risk. While both religion and spirituality were associated with better health behaviors at baseline in bivariate analyses, a proportional hazard model showed that only spirituality was significantly associated with reduced mortality risk (by 20%), controlling for demographics, health status, and health behaviors.
Conclusions
Experiencing spiritual peace, along with adherence to a healthy lifestyle, were better predictors of mortality risk in this sample of CHF patients than were physical health indicators such as functional status and comorbidity. Future research might profitably examine the efficacy of attending to spiritual issues along with standard lifestyle interventions.
Keywords: Religiousness, Spirituality, Health, Self-Regulation, Mortality, Heart Failure
Research linking religiousness to physical health, including mortality, has been accumulating for decades. These links have been shown in many prospective studies of the general population, including for cardiovascular deaths (for reviews, see Chida, Steptoe, & Powell, 2009; Hill, Burdette, & Idler, 2011). Most of the research examining the religiousness-mortality link has focused on attendance at worship services (Chida et al., 2009), a core indicator of religiousness and typically the one with the strongest relationships with health variables (Hill et al., 2011; McCullough Hoyt, Larson, Koenig, & Thoresen, 2000).
Recently, increased research interest has been directed at spirituality, which is related to but distinct from religiousness (Oman, 2013). Spirituality is sometimes used to refer to manifestations of the divine or experiences imbued with divine-like qualities, such as transcendence, immanence, and ultimacy (Aldwin, Park, Jeong, & Nath, 2014), but in the context of health research, spirituality typically refers more generally to a sense of peace and meaning (Canada, Murphy, Fitchett, Peterman, & Schover, 2008). To date, little research attention has been directed at spirituality as a predictor of mortality, although some preliminary results are promising. A study of end-stage renal disease patients found that spirituality predicted survival over several years (Spinale et al., 2008), and a study of hospitalized older adults showed that lower levels of spiritual struggle predicted subsequent survival (Pargament, Koenig, Tarakeshwar, & Hahn, 2001). In a study of people with AIDS, several aspects of spirituality independently predicted long-term survival, with a sense of peace exerting the strongest effects (Ironson et al., 2002). The purpose of the present study is to examine spirituality as a predictor of mortality in congestive heart failure patients.
Congestive Health Failure
Congestive heart failure (CHF) is a progressive syndrome resulting from an impaired ability of the heart to maintain normal blood circulation. Common symptoms include difficult and painful breathing even during rest, fluid retention and swelling of the lower extremities, and general weakness and fatigue (Whang, 2013). Quality of life in CHF is usually increasingly impaired as the disease progresses and functioning becomes more and more compromised (Rector, Anand, & Cohn, 2006). CHF has high mortality rates: approximately 50% of people diagnosed with heart failure die within 5 years (American Heart Association, 2014).
CHF is among the most prevalent chronic diseases in the US, with over 5 million people estimated to be living with CHF in the US (American Heart Association, 2014). CHF is also the only cardiovascular disorder that is increasing in both incidence and prevalence, likely due to the aging of the US population, reduced myocardial infarction death rates, and more effective CHF treatments that improve longevity, but at the cost of a weakened heart (Galbreath et al., 2004). CHF is also one of the most expensive chronic diseases in the US; health care services, medications, and lost productivity due to CHF were estimated at $34 billion in 2010 (CDC, 2010).
Surprisingly few studies have examined psychosocial factors and mortality outcomes in CHF patients. Health behaviors such as cigarette smoking, poor diet, and alcohol consumption (e.g., Chamberlain et al., 2013; Levitan et al., 2013; Mozaffarian, Nye, & Levy, 2004) have been associated with increased risk of mortality for CHF patients. Social support has been shown to be related to lower mortality risk (e.g., Murberg & Bru, 2001) while depressive mood is related to higher mortality risk (e.g., Adams et al., 2012; Jiang et al., 2001).
Congestive Heart Failure and Spirituality
Issues of spirituality are very important to many CHF patients (Koenig, 2002; Murray, Kendall, Boyd, Worth, & Benton, 2004), particularly as their disease worsens (e.g., Murray et al., 2007). Several cross-sectional studies have demonstrated that positive aspects of spirituality are related to lower levels of depression and better psychological well-being and quality of life for those living with CHF (e.g., Bekelman, Dy, Becker et al., 2007; Bekelman et al., 2010).
We focused specifically on the spiritual component of deep peacefulness, which has been shown to be critically important to individuals with serious and life-limiting illnesses (Canada et al., 2008; Ironson et al., 2002; Steinhauser et al., 2006; Whitford & Olver, 2012). A sense of peacefulness refers to the affective aspects of spiritual-wellbeing (Canada et al., 2008), a ‘state of tranquility or serenity’ (Whitford & Olver, 2012, p. 608). Peacefulness is a subjective sense that may refer to feeling at peace with God or to a non-religious sense of tranquility. Peacefulness may reflect a sense of resolution regarding interpersonal conflicts, acceptance of one’s illness, a lack of struggle, and a sense of comfort and meaningful connection (Ironson et al., 2002; Steinhauser et al., 2006; Whitford & Olver, 2012).
Present Study
This study examined the association of spirituality with mortality risk in CHF patients, defining spirituality in terms of a sense of inner peace and harmony. We hypothesized that spirituality would be inversely associated with mortality risk, and that this association would remain when controlling for medical and psychosocial variables shown to relate to mortality in CHF patients and when controlling for religiousness, which, while not examined heretofore in the context of CHF, has been associated with lower mortality risk in many studies.
As control variables, we included both variables associated with increased risk of mortality and those shown to be associated with decreased risk in previous research. Thus, we included (and controlled for, as necessary), demographics as well as a variety of indicators of health status, including severity of symptoms based on the NYHA Classification (Jiang et al., 2001) and comorbidities (e.g., Chamberlain et al., 2013). For health behaviors, we included adherence to a healthy lifestyle (Park, Moehl, Fenster, Suresh, & Bliss, 2008; Sherbourne, Hays, Ordway, Dimatteo, & Kravitz, 1992), as well as cigarette smoking and alcohol consumption, which have been found to increase the risk of mortality in this group (e.g., Gargiulo et al., 2013; Mozaffarian et al., 2004). We also examined psychosocial factors that had been shown in previous studies to predict mortality in CHF patients: marital status and social support, which have been associated with a lower mortality risk (e.g., Murberg & Bru, 2001) and depressive symptoms, which have been associated with a higher mortality risk (e.g., Jiang et al., 2001). Finally, we included religious service attendance, which has not been examined explicitly in the context of CHF but has been shown to be associated with reduced mortality risk in many general population studies (Chida et al., 2009).
Methods
Procedure
Participants were recruited from a multicardiologist practice (Comprehensive Cardiology Consultants, Inc.), located in the greater Cincinnati, Ohio, and Northern Kentucky region. Eligibility requirements for the study were as follows: having diagnosed left-sided, systolic congestive heart failure of at least moderate severity as documented in their medical records by echocardiogram, Multi Gated Acquisition Scan (MUGA) or other nuclear tests of ventricular function, with the ejection fraction (EF) < 45; being ineligible for transplantation; speaking and reading English; being over age 45; and having no evident psychosis or severe cognitive impairment. CHF patients meeting eligibility criteria were informed by research staff about the study during their office visit. Interested participants were provided more information and an appointment was scheduled to conduct the consent process and complete the survey packet. Participants were given $10 for their participation in the study. Patient recruitment and data collection occurred in 2007. Data collection for mortality began approximately four years later at the end of 2011 and was completed in mid-2013.
Sample Characteristics
The sample consisted of 191 CHF patients. The sample was 64% male and the mean age was 68.6 years (SD = 10.1, range = 46 - 92). Fifty-nine percent of participants were married, 18% were widowed, and 11% were divorced. Racial composition of the sample was 83.2% Caucasian, 10.8% African American, 5.4% Native American, and 0.5% other. Income levels were fairly low: 38% had a family income of less than $25,000, 38% were between $25,000 and $50,000, and the remaining participants had a family income of more than $50,000. Nearly a quarter of the sample (23%) had not finished high school, 35% had a high school degree, and the remaining participants had some college education or more. Median time since CHF diagnosis was 48 months.
Measures
New York Heart Association (NYHA) functional classification
CHF patients are commonly assigned a classification according to the severity of their symptoms (i.e., how much they are limited during physical activity) by their physicians. Classification ranges from I (no limitation of physical activity) to II (Slight limitation in physical activity; comfortable at rest but ordinary physical activity results in fatigue, palpitations, and dyspnea) to III (marked limitation of physical activity; symptoms are caused by less than ordinary physical activity) to IV (unable to carry on any physical activity without discomfort) (Bennett, Riegel, Bittner, & Nichols, 2012). The NYHA classification was recorded from participants’ medical record at baseline. Most of the patients in this study had moderate NYHA symptom severity ratings, ranging from I (12%) to II (63%); only 25% were at Stage III or IV. Because only one patient was classified as level IV, we collapsed this category with III for analyses.
Health conditions
Comorbidity was assessed with endorsement of 14 health conditions based on respondent self-report of a physician diagnosis. These include chronic lung disease (11%), blindness or trouble seeing (14%), deafness or trouble hearing (15%), diabetes (31%), asthma (10%), ulcer or gastritis (11%), arthritis or rheumatism (38%), sciatica or chronic back pain (21%), hypertension (high blood pressure) (64%), angina (15%), heart attack or myocardial infarction (60%), stroke (10%), kidney or liver disease (8%), and cancer (18%). Health conditions were scored by summing the number of positive responses to the conditions (M = 3.5, SD = 2.1, range = 0 - 10).
Current smoking status
A dichotomous variable assessed current smoking status by self-report. About 15% (n = 28) of the sample reported being current smokers.
Alcohol consumption
Individuals were asked how many drinks (drink = one beer, one glass of wine, or one shot of liquor) on average they consumed (M = 0.5, SD = 1.1, range = 0 - 8) and the number of days they consumed alcohol during the past week (M = 0.7, SD = 1.7, range = 0 -7). Alcohol consumption was calculated by multiplying average drinks by number of days per week alcohol was consumed.
Adherence to healthy lifestyles
To assess the degree to which participants engaged in salutary health behaviors, a 7-item scale was adapted from the adherence scale used by Sherbourne et al. (1992). (We omitted the eighth item, alcohol consumption, from this scale, as it was separately measured.) Participants rated the degree to which they engaged in seven positive health behaviors relevant to CHF patients on a 5-point scale ranging from none of the time (0) to all of the time (4). The items asked about behaviors such as following a heart-healthy diet, taking prescribed medications, scheduling appropriate medical visits, maintaining weight, following doctor’s advice, and taking specific actions or activities to reduce stress level. A mean score was computed using all seven items (α = .63).
Depressive symptoms during the past week were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). The CES-D is a widely-used instrument in both clinical and epidemiological studies of depression symptoms (Haley et al., 1995). Response categories of for each of 20 items were rarely or none of the time (0) to most or all the time (3). We calculated a mean score for the 20 items (α = .91).
Social support was measured by the 6-item ENRICHD Social Support Instrument (ESSI; Mitchell et al., 2003), which was validated in a sample of myocardial infarction patients. Sample items on the ESSI include "Is there someone available to you who shows you love and affection?" and "Is there someone available to help you with daily chores?”. Six items were rated on a 5-point scale ranging from none of the time (1) to all of the time (5). We calculated a mean score for all six items (α = .91).
Service attendance was evaluated by a single item from the Brief Multidimensional Measure of Religiousness and Spirituality (BMMRS; Fetzer/NIA, 1999; Idler et al., 2003), “How often do you attend religious services?” Participants could select responses from never (0) to several times a week (4).
Spiritual peace was assessed by a single item from the BMMRS (Fetzer/NIA, 1999; Idler et al., 2003) that assesses inner peace and harmony, a central component of spirituality (Underwood & Teresi, p. 25). The item, "I feel deep inner peace or harmony," was rated on a 6-point scale in terms of how frequently the respondent experiences this state, ranging from never or almost never (1) to many times a day (6).
Survival time was calculated for each participant based on the number of days between the date on which the baseline (Time 1) survey was completed and their corresponding date of death. For those participants who were not deceased, the last day of Time 2 data collection (6/27/2013) was used to calculate the number of days between Time 1 participation and the study end date. Thus, for deceased participants, the survival variable represented the number of days until they died; for the non-deceased participants, it represented the number of days until the end of data collection (right censored).
Vital status
Patients’ medical charts were used to collect mortality information. As the medical records did not have mortality information for all participants (as patients may have moved or discontinued treatment at this practice), the Social Security Administration's publicly available Social Security Death Index (SSDI) was used to collect data on the remaining participants. Participants' names were searched on the SSDI to identify those who were deceased. After identifying those who were deceased, death certificates were requested for all deceased participants. Using these death certificates, data regarding mortality status, cause of death, and date of death were recorded.
Statistical Analysis
We used hierarchical Cox proportional hazards models to predict risk of death. Because we had a relatively small sample and a large number of variables, we used a correlation matrix to identify variables that were not related to survival or mortality and omitted them from the multivariate analyses. The only exceptions were smoking and alcohol consumption, given their established importance as mortality risk factors in CHF (Gargiulo et al., 2013; Mozaffarian et al., 2004).
We used a hierarchical procedure in which blocks of variables were entered step by step (Cleves, Gould, Guterrez, & Marchenko, 2010). The first step contained demographics and the health status variables; the second the health behavior habits; and the third focused on religion and spirituality. This effectively controls for the demographics, measures of health status, health behaviors and other study variables.
Proportional hazards models yield hazard ratios (HRs), which are the probability of an event occurring, such as mortality, over time. HRs above 1 signify an increased probability of mortality (e.g., HR = 1.3 indicates that higher scores on the predictive value increases the risk of mortality by 30%). HRs below 1 indicate that the predictive variable is a protective factor that decreases the risk of mortality, by 1 - HR. For example, an HR of .7 indicates a 30% lower risk of mortality.
All analyses were conducted using Stata 13.1 (Stata, 2014). We used the stcox command for proportional hazard models and nestreg command for hierarchical (nested) regression where we added blocks of variables in a sequence (Cleves et al., 2010). To evaluate models, the adequacy of model fit to the data was assessed by χ2, likelihood (−2LL), and Akaike Information Criterion (AIC).
Missing data percentages ranged from 0.5 to 4%. While the missing data percentages were fairly low, our sample size was only 191; therefore, we decided to use multiple imputation (Stata, 2014). This technique permits the analysis of complete data sets in which missing values are filled in based on regression-predicted values by generating multiple complete data sets (Hofer & Hoffman, 2007). The Stata manual recommends at least 20 iterations; therefore, we examined 20 to 50 iterations for imputed data sets. There were only minor differences between these solutions, so we used the 50 iteration solution.
Results
In this sample, 61 out of the 191 participants (31.94%) were deceased by the five year follow-up. The median survival time for the deceased participants was 828.6 days, and for the non-deceased participants, it was 1889 days, t(189) = 22.691, p < .001. We were able to locate cause of death for 59 of the deceased, most of whom died from CHF or other cardiopulmonary disease (61%). The second most frequent cause was cancer-related deaths (n = 9; 15%). The rest died from diverse problems such as septic shock (n = 4; 7%) and renal failure (n = 4; 7%).
Correlations among Study Variables
Table 1 presents zero-order correlations among the study variables, along with their means and standard deviations. Not surprisingly, demographics were related to various health indicators. Age was positively associated with the number of comorbidities and greater risk of mortality. However, older adults were also more likely to adhere to healthy lifestyle recommendations, have higher levels of social support, and attend religious services. They were also less likely to smoke and reported lower levels of depressive symptoms. Interestingly, gender was not significantly associated with other study variables with the exception of marital status and alcohol consumption; women were less likely to be married and consumed less alcohol. Marital status was positively associated with social support and service attendance. Married individuals were less likely to adhere to healthy lifestyles and had higher NYHA ratings. However, neither marital status nor gender predicted survival or mortality and thus were omitted from the multivariate models.
Table 1.
Correlations, Means, and Standard Deviations for Study Variables (N = 191)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | ||||||||||||||
| 2. Gendera | .00 | |||||||||||||
| 3. Marital Statusb | −.06 | −.25*** | ||||||||||||
| 4. NYHAc | .08 | .11 | .16* | |||||||||||
| 5. Health Conditions | .15* | .04 | .05 | .22** | ||||||||||
| 6. Depressive Symptoms | −.19** | .07 | −.13 | .23** | .14* | |||||||||
| 7. Social Support | .14* | −.08 | .35*** | .04 | .05 | −.36*** | ||||||||
| 8. Adherenced | .29*** | .09 | −.08 | .02 | −.07 | −.34*** | .26*** | |||||||
| 9. Smokinge | −.30*** | .00 | −.08 | −.04 | −.08 | .20** | −.08 | −.12 | ||||||
| 10. Alcohol Consumption | .06 | −.15* | −.01 | −.08 | −.13 | −.06 | −.02 | −.06 | −.08 | |||||
| 11. Spiritual Peace | .09 | .03 | .08 | −.06 | −.03 | −.31*** | .38*** | .21** | −.11 | −.17* | ||||
| 12. Service Attendance | .25** | .05 | .21** | −.03 | −.01 | −.22** | .23** | .23** | −.18* | −.09 | .33*** | |||
| 13. Survival Time | −.11 | .02 | −.05 | −.18* | −.23** | −.13 | .13 | .17* | −.14 | .12 | .14 | .08 | ||
| 14. Vital Statusf | .16* | −.06 | .03 | .13 | .20** | .14* | −.11 | −.18* | .13 | −.13 | −.18* | −.07 | −.86*** | |
|
| ||||||||||||||
| Mean | 68.65 | .36 | .59 | 2.13 | 3.50 | 15.31 | 4.01 | 2.87 | .15 | 1.56 | 4.48 | 2.34 | 1550.34 | .32 |
| SD | 10.14 | .48 | .49 | .60 | 2.14 | 11.22 | .94 | .55 | .36 | 4.09 | 1.43 | 1.66 | 579.6 | .47 |
Note.
Gender (Male = 0, Female = 1);
Marital Status (Not married = 0, Married = 1);
NYHA = New York Heart Association (NYHA) functional classification;
Adherence = Adherence to healthy lifestyle;
Smoking = Current smoking status (Not smoking = 0, Smoking = 1);
Vital Status (Alive = 0, Deceased = 1).
p < .05;
p < .01;
p < .001.
Indicators of health status were also predictors of survival/mortality outcomes. Individuals with lower NYHA classifications reported fewer depressive symptoms and less co-morbidity, and had longer survival time. Co-morbidity was related to higher depressive symptoms, shorter survival times, and higher rates of mortality. Depressive symptoms were positively associated with current smoking status and higher risk of mortality. Adhering to healthy lifestyle recommendations was associated with better survival time and lower mortality rates.
Finally, the religious (attendance) and spirituality (peace) variables were, in general, related to better health and health behaviors. Both were inversely associated with depressive symptoms and positively with better adherence to healthy lifestyle recommendations. Religious attendance was inversely related to smoking, but inner peace was related to less alcohol consumption. However, religious attendance was unrelated to either survival or mortality in this study, so it was dropped from further consideration. However, inner peace was related to lower risk of mortality, and so became the focus of the multivariate analyses.
Predicting Mortality
Table 2 presents the results of the hierarchical Cox proportional hazards models predicting risk of death. In Step 1, age, health conditions, and depressive symptoms were significantly associated with mortality. Age significantly increased the risk of mortality by 3%, HR = 1.029, p < .05, while depressive symptoms were only marginally related to higher risk of mortality by 2%, HR = 1.019, p = .09. Comorbidity, the number of health conditions, was significantly associated with increased risk of mortality, by 13%, HR = 1.134, p < .05; however, NYHA severity ratings were not significantly predictive of mortality risk in this multivariate model.
Table 2.
Hierarchical Cox Proportional Hazard Models Predicting Mortality (N = 191)
|
Step 1
|
Step 2
|
Step 3
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | HR | SE | z | p | 95% | CI | HR | SE | z | p | 95% | CI | HR | SE | z | p | 95% | CI |
| Age | 1.029 | .01 | 2.18 | 0.03 | 1.00 | 1.06 | 1.055 | .02 | 3.50 | 0.00 | 1.02 | 1.09 | 1.060 | .02 | 3.70 | 0.00 | 1.03 | 1.09 |
| NYHA | 1.237 | .28 | 0.93 | 0.35 | 0.79 | 1.94 | 1.437 | .32 | 1.62 | 0.11 | 0.93 | 2.23 | 1.443 | .33 | 1.62 | 0.11 | 0.93 | 2.25 |
| Health Conditions | 1.134 | .06 | 2.19 | 0.03 | 1.01 | 1.27 | 1.127 | .07 | 1.98 | 0.05 | 1.00 | 1.02 | 1.123 | .07 | 1.92 | 0.06 | 1.00 | 1.27 |
| Depressive Symptoms | 1.019 | .01 | 1.72 | 0.09 | 1.00 | 1.04 | 1.000 | .01 | 0.03 | 0.98 | 0.98 | 0.98 | 0.988 | .01 | −0.86 | 0.39 | 0.96 | 1.01 |
| Adherence | - | - | - | - | - | - | 0.423 | .11 | −3.24 | 0.00 | 0.25 | 0.71 | 0.402 | .11 | −3.36 | 0.00 | 0.24 | 0.68 |
| Smoking | - | - | - | - | - | - | 2.679 | .95 | 2.78 | 0.01 | 1.34 | 5.37 | 2.643 | .97 | 2.64 | 0.01 | 1.29 | 5.43 |
| Alcohol Consumption | - | - | - | - | - | - | 0.921 | .05 | −1.53 | 0.13 | 0.83 | 1.02 | 0.894 | .97 | −1.94 | 0.05 | 0.80 | 1.00 |
| Spiritual Peace | - | - | - | - | - | - | - | - | - | - | - | - | 0.795 | .07 | −2.56 | 0.01 | 0.67 | 0.95 |
|
| ||||||||||||||||||
| χ2(df) | 16.80**(4) | 36.27***(7) | 42.66***(8) | |||||||||||||||
| Δχ2(df) | - | 19.46***(3) | 6.40*(1) | |||||||||||||||
| −2LL | 600.6354 | 581.1712 | 574.7748 | |||||||||||||||
| Δ−2LL | - | 19.4642 | 6.3964 | |||||||||||||||
| AIC | 608.6354 | 595.1712 | 590.7748 | |||||||||||||||
Note. HR = Hazard Ratio; aNYHA = New York Heart Association (NYHA) functional classification; bAdherence = Adherence to healthy lifestyle; cSmoking = Current smoking status (Not smoking = 0, Smoking = 1).
p < .05;
p < .01;
p < .001.
In Step 2, health behaviors were added. Among the health behaviors, smoking was significantly associated with a nearly three-fold increased mortality risk, HR = 2.679, p < .01, but alcohol consumption was not significantly associated. Adherence to healthy lifestyle recommendations more than halved the risk of mortality, HR = 0.423, p < .001. Adding the health behaviors to the model rendered the associations of depressive symptoms with mortality risk nonsignificant. The difference in χ2 distribution, Δχ2 (3) = 19.46, p < .001, showed that the model in Step 2 provided a better fit to the data than did the model in Step 1.
In Step 3, only one predictor, spiritual peace, was added. (Ancillary analyses confirmed that neither social support nor religious attendance were significant predictors in a multivariate model.) Spiritual peace was significantly associated with decreased risk of mortality, by 20%, HR = 0.795, p = .01. Interestingly, alcohol consumption now emerged as a significant predictive factor, associated with lower risk of mortality, by 11%, HR = 0.894, p = .05. The difference in χ2 distribution, Δχ2 (1) = 6.40, p < .05, and the smaller values of the −2LL and AIC, indicated that the model in Step 3 was a better fit to the data than were the other models.
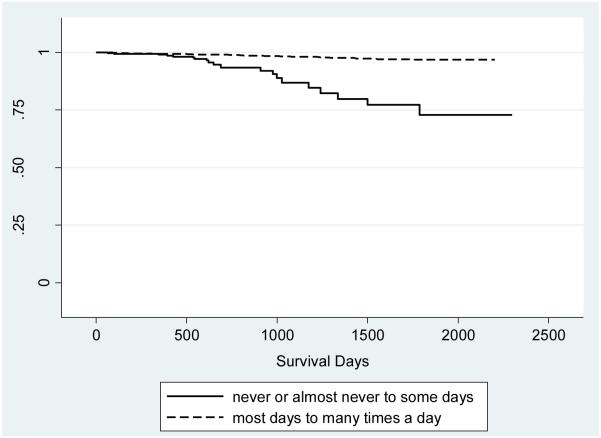
Figure 1 plots the survival curves for individuals with high and low levels of spiritual peace, controlling for all of the other variables in the model. For illustrative purposes, we dichotomized spiritual peace (1 = never or almost never to some days; 2 = most days to many times a day). Very few of those with high levels (i.e., feeling inner peace and harmony most days to many times a day) had died by the end of the study period, compared to about 25% of those with low levels of spiritual peace.
Figure 1.
Impact of spiritual peace on survival, controlling for demographics, health, and adherence to health behaviors.
Discussion
Congestive heart failure (CHF) is a very difficult illness to manage, and has a high mortality rate, yet there is a surprising lack of studies examining psychosocial predictors of mortality in CHF patients. In the literature on aging, there is particular interest in how older adults can maintain well-being in the face of chronic illness, which is so often accompanied by pain, discomfort, disability, and mortality threats (Fortinsky, Tennen, & Steffens, 2013; Kahana, Kelley-Moore, & Kahana, 2012). However, whether maintenance of well-being in chronic illness – especially CHF-- decreases the risk of mortality remains an open question.
For many people, religiousness and spirituality are important aspects of adapting to chronic illness. In our sample, levels of both service attendance and spirituality were fairly high at baseline. While religiousness has long been shown to be a factor associated with reduced mortality risk in general population studies (Chida et al., 2009), much less is known about associations of spirituality with mortality risk. In this relatively small sample of CHF patients, we found that a sense of inner peace and harmony predicted lower mortality risk -- specifically, feelings of inner peace were related to a lower mortality risk of about 20%, controlling for demographics, measures of physical health status, and other psychosocial factors. In contrast, religiousness, assessed as service attendance, was unrelated to mortality even at the bivariate level, although it was related to other health-related variables.
The lack of relationship between religiousness and mortality was not entirely unexpected. Although there is a robust literature demonstrating associations between religiousness, particularly service attendance, and reduced risk of mortality in healthy samples, these effects are often not found for samples already diagnosed with a serious disease (see Chida et al., 2009, for a review). Chida and her colleagues noted that religiousness may be more important in resisting disease than in helping people already diagnosed and in treatment, a conclusion that echoed one drawn earlier by Powell and her colleagues in an influential review (Powell, Shahabi, & Thoresen, 2003).
Yet spirituality was indeed related to lower mortality risk, even after taking into account many other variables. This finding is consistent with those of studies that have been conducted with people with AIDS, in which a sense of peace exerted the strongest protective effects on mortality risk (Ironson et al., 2002), and with cancer patients, which had similar findings (Whiford & Olver, 2012). Clearly, future research should examine not only the standard measures of religiousness (service attendance as well as private religious practices such as prayer), but the more experiential aspects of spirituality such as assessed in the present study.
Consistent with these other studies linking spirituality and mortality in those with serious illness, our results suggest that this inner experience that may matter most in terms of survival. Perhaps some people achieve this inner state of peace and harmony through religious involvement, but others may achieve it in other ways (Oman, 2013). Previous research using a similar one-item measure (Are you at peace?) (Steinhauser et al., 2006) in patients with CHF, cancer, and other life-threatening illnesses found that it was substantially correlated with the widely-used FACIT-Sp spirituality subscales of both faith (r = .51) and meaning/peace (r = .47). Extrapolating from these results, our one-item measure of inner peace and harmony may be tapping into a broad spirituality factor. This sense of inner peace and harmony appears to reflect a core sense of comfort and meaningful connection (Ironson et al., 2002; Steinhauser et al., 2006; Whitford & Olver, 2012). This speculative interpretation of our findings awaits further research.
Interestingly, the bivariate relations between physical functioning and mortality outcomes disappeared once age was controlled in the multivariate model. Given the importance of comorbidity in predicting mortality, it would be a mistake to conclude that having multiple health problems did not affect mortality; rather, one reason that age might be a good predictor – increases of 5% with each year of age – was that it was associated with multiple medical conditions.
Not surprisingly, smoking was associated with nearly a three-fold risk of mortality; however, very few individuals in this sample still smoked (15%). Although the role of alcohol in heart disease tends to show a favorable effect (e.g., Jayasekara, English, Room, & MacInnis, 2014), moderate alcohol consumption has been related to increased mortality risk in CHF patients (e.g., Gargiulo et al., 2013). In our study, alcohol consumption was associated with a 10% decreased risk of mortality. In contrast, adherence to healthy lifestyle physician recommendations was related to substantially reduced risk of mortality, about 50%. These findings suggest that interventions that help CHF patients adhere to healthy lifestyle recommendations would be a promising approach to improve their mortality risk. Research has especially noted links between diet and disease progression in CHF (e.g., Levitan et al., 2013), so increased attention to dietary improvements may also facilitate greater health and longevity in CHF patients.
In bivariate relations, depressive symptoms were associated with mortality; however, in the multivariate analyses, they were no longer significant. Depressive symptoms may impair health status in CHF patients in part due to poorer lifestyle behaviors (e.g., Murberg & Bru, 2001). However, in this sample, social support and marital status, while associated with one another, were unrelated to mortality or survival time even at the bivariate level.
Limitations and Future Studies
Our sample size was relatively small in terms of studies that examine mortality; a number of the expected effects approached significance, and it is possible that a larger study might find more statistically significant predictors. Our measure of spirituality was a single item; although not without precedent (e.g., Steinhauser et al., 2006), a more comprehensive measure of spirituality may have revealed more nuanced findings. For example, Ironson and her colleagues (2002) developed the Ironson–Woods Spirituality/Religiousness Index through interviews and surveys with people with a variety of diagnosed illnesses. They identified seven dimensions of spirituality that were meaningful in these samples, such as feeling connected and feeling compassion for others; future research should include multiple dimensions of spirituality.
An additional limitation of our study was that, for a CHF sample, the average NYHA classification level was relatively good, limiting the generalizability of our findings to more impaired samples. As we noted earlier, mortality rates are typically 50% over a five year period (American Heart Association, 2014), but our mortality rate was only 32%. Future research should conduct tests in larger samples with a broader range of health statuses. Further, biomarker pathways should be included to more directly examine the pathways between spirituality and health outcomes.
Nonetheless, it is encouraging to see that both adherence to healthy lifestyles and spiritual peace are associated with reduced risks of mortality in CHF patients. Such information should inform future interventions with this group to increase the life expectancy as well as quality of life. Given the very large projected increases in the incidence and prevalence in CHF as the Baby Boomers age (Norton, Georgiopoulou, Kalogeropoulos, & Butler, 2011), such interventions may substantially improve the lives and well-being of a large segment of the population. Already, interventions to promote better adherence to health behaviors are being tested in CHF patients (e.g., Jaarsma et al., 2000). However, virtually no interventions have been tested that include a spiritual component; such interventions would, of course, need to be carefully designed and implemented, but might also be an important aspect of patient-centered care (Park & Paloutzian, 2013).
Acknowledgments
The study was supported by grant #21733 from the Templeton Foundation and grant 1R03AG023883-01A2 from the National Institute of Aging. We would like to thank Paula Casson and Valeri Cook for their assistance in data collection.
References
- Adams J, Kuchibhatla M, Christopher EJ, Alexander JD, Clary GL, Cuffe MS, Jiang W. Association of depression and survival in patients with chronic heart failure over 12 years. Psychosomatics. 2012;53:339–346. doi: 10.1016/j.psym.2011.12.002. doi:10.1016/j.psym.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldwin CM, Park CL, Jeong Y-J, Nath R. Differing pathways between religiousness, spirituality, and health: A self-regulation perspective. Psychology of Religion and Spirituality. 2014;6:9–21. doi: 10.1037/a0034416. [Google Scholar]
- American Heart Association Heart disease and stroke statistics--2014 update: A report from the American Heart Association. Circulation. 2014 doi: 10.1161/01.cir.0000441139.02102.80. published online December 18, 2013. doi:10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekelman DB, Parry C, Curlin FA, Yamashita TE, Fairclough DL, Wamboldt FS. A comparison of two spirituality instruments and their relationship with depression and quality of life in chronic heart failure. Journal of Pain and Symptom Management. 2010;39:515–526. doi: 10.1016/j.jpainsymman.2009.08.005. doi:10.1016/j.jpainsymman.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekelman D, Dy S, Becker D, Wittstein I, Hendricks D, Yamashita T, Gottlieb SH. Spiritual well-being and depression in patients with heart failure. Journal of General Internal Medicine. 2007;22:470–477. doi: 10.1007/s11606-006-0044-9. doi: 10.1007/s11606-006-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett JA, Riegel B, Bittner V, Nichols J. Validity and reliability of the NYHA classes for measuring research outcomes in patients with cardiac disease. Heart & Lung: The Journal of Acute and Critical Care. 2002;31:262–270. doi: 10.1067/mhl.2002.124554. doi:10.1067/mhl.2002.124554. [DOI] [PubMed] [Google Scholar]
- Canada AL, Murphy PE, Fitchett G, Peterman AH, Schover LR. A 3-factor model for the FACIT-Sp. Psycho-Oncology. 2008;17:908–916. doi: 10.1002/pon.1307. doi: 10.1002/pon.1307. [DOI] [PubMed] [Google Scholar]
- CDC Estimated direct and indirect costs of major cardiovascular diseases, United States. 20102010 Retrieved from http://www.cdc.gov/chronicdisease/resources/publications/AAG/dhdsp.htm. [Google Scholar]
- Chamberlain AM, McNallan SM, Dunlay SM, Spertus JA, Redfield MM, Moser DK, Roger VL. Physical health status measures predict all-cause mortality in patients with heart failure. Circulation: Heart Failure. 2013;6:669–675. doi: 10.1161/CIRCHEARTFAILURE.112.000291. doi: 10.1161/CIRCHEARTFAILURE.112.000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, Steptoe A, Powell LH. Religiosity/spirituality and mortality. A systematic quantitative review. Psychotherapy and Psychosomatics. 2009;78:81–90. doi: 10.1159/000190791. doi:10.1159/000190791. [DOI] [PubMed] [Google Scholar]
- Cleves M, Gould W, Guterrez R, Marchenko Y. An introduction to survival analysis using Stata. 3rd Stata Press; College Station, TX: 2010. [Google Scholar]
- Curtis JP, Sokol SI, Wang Y, Rathore SS, Ko DT, Jadbabaie F, Krumholz HM. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. Journal of the American College of Cardiology. 2003;42:736–742. doi: 10.1016/s0735-1097(03)00789-7. doi:10.1016/S0735-1097(03)00789-7. [DOI] [PubMed] [Google Scholar]
- Fetzer Institute/National Institute on Aging Working Group . Multidimensional measurement of religiousness/spirituality for use in health research. John E. Fetzer Institute; Kalamazoo, MI: 1999. [Google Scholar]
- Fortinsky RH, Tennen H, Steffens DC. Resilience in the face of chronic illness and family caregiving in middle and later life. Psychiatric Annals. 2013;43:549–554. doi: 10.3928/00485713-20131206-07. [Google Scholar]
- Galbreath A, Krasuski R, Smith B, Stajduhar K, Kwan M, Ellis R, Freeman GL. Long-term healthcare and cost outcomes of disease management in a large, randomized, community-based population with heart failure. Circulation. 2004;110:3518–3526. doi: 10.1161/01.CIR.0000148957.62328.89. doi:10.1161/01.CIR.0000148957.62328.89. [DOI] [PubMed] [Google Scholar]
- Gargiulo G, Testa G, Cacciatore F, Mazzella F, Galizia G, Della-Morte D, Abete P. Moderate alcohol consumption predicts long-term mortality in elderly subjects with chronic heart failure. The Journal of Nutrition, Health & Aging. 2013;17:480–485. doi: 10.1007/s12603-012-0430-4. doi: 10.1007/s12603-012-0430-4. [DOI] [PubMed] [Google Scholar]
- Haley WE, West CAC, Wadley VG, Ford G, White FA, Roth DL. Psychological, social, and health impact of caregiving: A comparison of black and white dementia family caregivers and noncaregivers. Psychology and Aging. 1995;10:540–552. doi: 10.1037/0882-7974.10.4.540. [PubMed] [Google Scholar]
- Hill TD, Burdette AM, Idler EL. Religious involvement, health status, and mortality risk. In: Settersten RA, Angel JL, editors. Handbook of sociology of aging. Springer; New York: 2011. pp. 533–546. [Google Scholar]
- Hofer SM, Hoffman L. Statistical analysis with incomplete data: A developmental perspective. In: Little TD, Bovaird JA, Card NA, editors. Modeling developmental processes in ecological context. LEA; Mahwah, NJ: 2007. pp. 13–32. [Google Scholar]
- Horowitz A. Family caregiving to the frail elderly. Annual Review of Gerontology and Geriatrics. 1985;5:194–246. [PubMed] [Google Scholar]
- Idler EL, Musick MA, Ellison CG, George LK, Krause N, Ory MG, Williams DR. Measuring multiple dimensions of religion and spirituality for health research: Conceptual background and findings from the 1998 General Social Survey. Research on Aging. 2003;25:327–365. doi: 10.1177/0164027503252749. [Google Scholar]
- Ironson G, Solomon GF, Balbin EG, O’Cleirigh C, George A, Kumar M, Woods TE. The Ironson-Woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine. 2002;24:34–48. doi: 10.1207/S15324796ABM2401_05. doi: 10.1207/S15324796ABM2401_05. [DOI] [PubMed] [Google Scholar]
- Jaarsma T, Halfens R, Tan F, Abu-Saad HH, Dracup K, Diederiks J. Self-care and quality of life in patients with advanced heart failure: the effect of a supportive educational intervention. Heart & Lung: The Journal of Acute and Critical Care. 2000;29:319–330. doi: 10.1067/mhl.2000.108323. doi: 10.1067/mhl.2000.108323. [DOI] [PubMed] [Google Scholar]
- Jayasekara H, English DR, Room R, MacInnis RJ. Alcohol consumption over time and risk of death: A systematic review and meta-analysis. American Journal of Epidemiology. 2014;179:1049–1059. doi: 10.1093/aje/kwu028. doi: 10.1093/aje/kwu028. [DOI] [PubMed] [Google Scholar]
- Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, O'Connor CM. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Archives of Internal Medicine. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. doi:10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- Kahana E, Kelley-Moore J, Kahana B. Proactive aging: A longitudinal study of stress, resources, agency and well-being in later life. Aging & Mental Health. 2012;16:438–451. doi: 10.1080/13607863.2011.644519. doi: 10.1080/13607863.2011.644519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandala J, Uthamalingam S, Daley M, Baribeau Y, Ballari S, Capodilupo R. Left ventricle ejection fraction versus NYHA functional classification in predicting postoperative outcomes. Journal of Cardiac Failure. 2009;15:S99–S100. doi:10.1016/j.cardfail.2009.06.116. [Google Scholar]
- Koenig HG. Religion, congestive heart failure, and chronic pulmonary disease. Journal of Religion & Health. 2002;41:263–278. doi: 10.1023/A:1020241004572. [Google Scholar]
- Levitan EB, Lewis CE, Tinker LF, Eaton CB, Ahmed A, Manson JE, Shikany JM. Mediterranean and DASH diet scores and mortality in women with Heart failure: The Women’s Health Initiative. Circulation: Heart Failure. 2013;6:1116–1123. doi: 10.1161/CIRCHEARTFAILURE.113.000495. doi: 10.1161/CIRCHEARTFAILURE.113.000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough ME, Hoyt WT, Larson DB, Koenig HG, Thoresen C. Religious involvement and mortality: A meta-analytic review. Health Psychology. 2000;19:211–222. doi: 10.1037//0278-6133.19.3.211. doi: 10.1037/0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- Mitchell P, Powell L, Blumenthal J, Norten J, Ironson G, Pitula C, Berkman L. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. Journal of Cardiopulmonary Rehabilitation. 2003;23:398–403. doi: 10.1097/00008483-200311000-00001. doi: 00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Nye R, Levy WC. Statin therapy is associated with lower mortality among patients with severe heart failure. The American Journal of Cardiology. 2004;93:1124–1129. doi: 10.1016/j.amjcard.2004.01.039. doi:10.1016/j.amjcard.2004.01.039. [DOI] [PubMed] [Google Scholar]
- Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. Journal of Psychosomatic Research. 2001;51:521–527. doi: 10.1016/s0022-3999(01)00226-4. doi: 10.1016/S0022-3999(01)00226-4. [DOI] [PubMed] [Google Scholar]
- Murray SA, Kendall M, Boyd K, Worth A, Benton TF. Exploring the spiritual needs of people dying of lung cancer or heart failure: A prospective qualitative interview study of patients and their carers. Palliative Medicine. 2004;18:39–45. doi: 10.1191/0269216304pm837oa. doi:10.1191/0269216304pm837oa. [DOI] [PubMed] [Google Scholar]
- Murray SA, Kendall M, Grant E, Boyd K, Barclay S, Sheikh A. Patterns of social, psychological, and spiritual decline toward the end of life in lung cancer and heart failure. Journal of Pain and Symptom Management. 2007;34:393–402. doi: 10.1016/j.jpainsymman.2006.12.009. doi:10.1016/j.jpainsymman.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Norton C, Georgiopoulou VV, Kalogeropoulos AP, Butler J. Epidemiology and cost of advanced heart failure. Progress in Cardiovascular Diseases. 2011;54:78–85. doi: 10.1016/j.pcad.2011.04.002. doi:10.1016/j.pcad.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Oman D. Religious and spirituality: Evolving meanings. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. 2nd Guilford Press; New York: 2013. pp. 23–47. [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients: A 2-year longitudinal study. Archives of Internal Medicine. 2001;161:1881–1885. doi: 10.1001/archinte.161.15.1881. doi:10.1001/archinte.161.15.1881. [DOI] [PubMed] [Google Scholar]
- Park CL, Moehl B, Fenster JR, Suresh DP, Bliss D. Religiousness and treatment adherence in congestive heart failure patients. Journal of Religion, Spirituality, & Aging. 2008;20:249–266. doi:10.1080/15528030802232270. [Google Scholar]
- Park CL, Paloutzian RF. Directions for the future of the psychology of religion and spirituality: Research advances in methodology and meaning systems. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. 2nd Guilford; New York: 2013. pp. 651–665. [Google Scholar]
- Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: Linkages to physical health. American Psychologist. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. doi:10.1037/0003-066X.58.1.36. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Rector TS, Anand IS, Cohn JN. Relationships between clinical assessments and patients' perceptions of the effects of heart failure on their quality of life. Journal of Cardiac Failure. 2006;12:87–92. doi: 10.1016/j.cardfail.2005.10.002. doi:10.1016/j.cardfail.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Spinale J, Cohen SD, Khetpal P, Peterson RA, Clougherty B, Puchalski CM, Kimmel PL. Spirituality, social support, and survival in hemodialysis patients. Clinical Journal of the American Society of Nephrology. 2008;3:1620–1627. doi: 10.2215/CJN.01790408. doi:10.2215/CJN.01790408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Hays R,D, Ordway L, DiMatteo MR, Kravitz RL. Antecedents of adherence to medical recommendations: Results from the Medical Outcomes Study. Journal of Behavioral Medicine. 1992;15:447–468. doi: 10.1007/BF00844941. doi:10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- Stata . Stata survival analysis and epidemiological tables reference manual release. Vol. 13. Stata Press; College Station, TX: 2014. [Google Scholar]
- Steinhauser KE, Voils CI, Clipp EC, Bosworth HB, Christakis NA, Tulsky JA. “Are you at peace?”: One item to probe spiritual concerns at the end of life. Archives of Internal Medicine. 2006;166:101–105. doi: 10.1001/archinte.166.1.101. doi:10.1001/archinte.166.1.101. [DOI] [PubMed] [Google Scholar]
- Underwood LG, Teresi JA. The Daily Spiritual Experience Scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Annals of Behavioral Medicine. 2002;24:22–33. doi: 10.1207/S15324796ABM2401_04. doi:10.1207/S15324796ABM2401_04. [DOI] [PubMed] [Google Scholar]
- Whitford HS, Olver IN. The multidimensionality of spiritual wellbeing: Peace, meaning, and faith and their association with quality of life and coping in oncology. Psycho-Oncology. 2012;21:602–610. doi: 10.1002/pon.1937. doi: 10.1002/pon.1937. [DOI] [PubMed] [Google Scholar]
- Whang W. Congestive heart failure. In: Gellman MD, Turner JR, editors. Encyclopedia of behavioral medicine. Springer; New York: 2013. pp. 485–486. doi:10.1007/978-1-4419-1005-9_1255. [Google Scholar]