Abstract
Objective
Given the overlap among depressive symptoms, disordered eating, and overweight, identifying shared risk factors for these conditions may inform public health interventions. This study aimed to examine cross-sectional and prospective relationships among these three conditions, and identify potential shared eating-related and psychosocial variable risk factors (i.e., body dissatisfaction, dieting, teasing experiences).
Methods
A population-based sample (n=1,902) self-reported depressive symptoms, disordered eating (binge eating, extreme weight control behaviors), weight status, and several putative risk factors (body satisfaction, dieting frequency, weight-related teasing) at 5-year intervals spanning early/middle adolescence, late adolescence/early young adulthood, and early/middle young adulthood.
Results
There was moderate overlap among depressive symptoms, disordered eating, and overweight at each timepoint, and moderate stability in each condition over time. Body dissatisfaction and dieting were the most potent shared risk factors for later depressive symptoms, disordered eating, and overweight among males and females (ps<.05).
Conclusions
Depressive symptoms, disordered eating, and overweight share several risk factors, including dieting and body dissatisfaction, which may be effective targets for interventions aiming to simultaneously prevent these three conditions.
Keywords: Depression, disordered eating, overweight, risk factors
Depression, disordered eating, and excess weight status are major public health concerns associated with impairment, morbidity, and mortality (Fabricatore & Wadden, 2006; Goldschmidt, Fitzsimmons-Craft, & Le Grange, in press; National Institute for Health and Clinical Excellence, 2009). There is substantial overlap in the prevalence of these conditions (Faith et al., 2011; Green et al., 2009; Haines, Kleinman, Rifas-Shiman, Field, & Austin, 2010) and given the likelihood of common pathways to onset, researchers have called for public health interventions to target shared risk factors for these overlapping health conditions (Becker, Plasencia, Kilpela, Briggs, & Stewart, 2014; Haines & Neumark-Sztainer, 2006). Importantly, to date, shared risk for these three conditions largely has been inferred by comparing across studies using divergent methodologies and populations, thus limiting the precision of the existing research. Our group has identified specific personal and socio-environmental shared risk factors for excess weight status and disordered eating (Neumark-Sztainer et al., 2007); these data, however, could further inform prevention research by additional consideration of depressive symptoms, which frequently co-occur with both excess weight status and disordered eating.
Several pathways to the co-occurrence of depression, disordered eating, and elevated weight status are plausible. For example, support exists for a model whereby binge eating (i.e., overeating accompanied by a sense of loss of control; American Psychiatric Association, 2013) leads to both excess weight status and depressive symptoms (Sonneville et al., 2013), perhaps due to the socially isolating nature of the behavior (Ranzenhofer et al., 2012). Alternatively, binge eating and other disordered eating behaviors may develop as a means of coping with antecedent depressive symptoms (Haedt-Matt & Keel, 2011) and thereby lead to later overweight onset (Goldschmidt, Wall, Choo, Larson, & Neumark-Sztainer, 2015). It also is possible that being overweight in adolescence results in negative interpersonal experiences, which promote the development of both disordered eating (Puhl & Luedicke, 2012) and depressive symptoms (Faith et al., 2011). Although one pathway is unlikely to account for all cases, and there may be significant variability in the timing of symptom onset (Presnell, Stice, Seidel, & Madeley, 2009; Reas & Grilo, 2007), the co-occurrence of these three conditions may present a significant challenge to treatment providers. Thus, there is a need to better understand the etiology of these overlapping conditions in order to inform the development of comprehensive, empirically-driven preventive interventions.
Body dissatisfaction, dieting, and weight-related teasing all have received empirical support as variable risk factors for mood- (Presnell et al., 2009), eating- (Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004), and weight-related problems (Quick, Wall, Larson, Haines, & Neumark-Sztainer, 2013). Several models have been proposed to explain these associations, including the cognitive-behavioral and dual pathway models. The former posits that dissatisfaction with one’s current shape/weight promotes dieting behaviors and related cognitions (e.g., attempts to follow dietary rules) intended to alter one’s appearance (Fairburn, Cooper, & Shafran, 2003), which in turn stimulate binge eating when dieting efforts are interrupted (Polivy & Herman, 1993). The latter posits that both body dissatisfaction and negative affect promote disordered eating, and offers proposed mechanisms for the associations among risk factors (Stice & Agras, 1998). The model suggests, for example, that perceived pressure to adhere to the thin ideal fosters body dissatisfaction (which may manifest in direct appearance-related criticism; Jacobi et al., 2011), which in turn contributes to depressive symptoms due to the emphasis on appearance as an evaluative construct in Western culture. Dieting is also proposed to increase depressive symptoms by means of both failures at weight control, and direct effects of caloric deprivation on mood (Stice, 2001). Both models have received support in the literature (Allen, Byrne, & McLean, 2012). To date, however, no studies have investigated the proposed risk factors in relation to the overlapping outcomes of depressive symptoms, disordered eating, and excess weight status.
The current study aimed to examine, within a population-based sample followed over 10 years from adolescence to young adulthood, the co-occurrence of depressive symptoms, disordered eating, and excess weight status, and identify shared variable risk factors, so as to inform the development of interventions aiming to simultaneously prevent all three conditions. We predicted that there would be substantial co-occurrence of depressive symptoms, disordered eating, and excess weight status across adolescence and young adulthood, and that each condition would increase risk for the other two conditions at 5-year and 10-year follow-up. We further hypothesized that body dissatisfaction, dieting behaviors, and weight-related teasing during early/middle adolescence and middle adolescence/early young adulthood would be shared risk factors for depressive symptoms, disordered eating, and excess weight status at 5-year and 10-year follow-up. We focused on behavioral, psychological, and interpersonal risk factors (e.g., as opposed to familial or biological risk factors) because these are among the most compelling modifiable risk factors to date as reviewed in the literature (Becker et al., 2014). As such, they have the potential to serve as key targets for future public health interventions aimed at reducing risk for all three outcomes.
Methods
Study Design and Population
Participants were involved in Project EAT (Eating Among Teens and Young Adults), a 10-year longitudinal study of eating, activity, and weight-related outcomes, and relevant psychosocial factors, among young people (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). Public schools and school districts serving socioeconomically and racially/ethnically diverse communities in and around Minneapolis, Minnesota were invited to participate in the study. Data were collected during middle/late adolescence (Time 1; TI: 1998–1999) in health, physical education, and science classrooms; and at 5-year (Time 2; T2: 2003–2004; late adolescence/early young adulthood) and 10-year follow-up (Time 3; T3: 2008–2009; early/middle young adulthood) by mail or online. All study protocols were approved by the University of Minnesota's Institutional Review Board.
Of the original 4,746 EAT-I participants, 1,902 (40.1%) had data available at all three timepoints. Attrition was primarily due to inability to contact participants (e.g., missing or outdated address information). Participants were 56.9% female (n=1,083), 66.5% Caucasian, and 14.9±1.6 years old, on average, at T1 (see Table 1); 54.9% of participants fell in the middle and middle-high socioeconomic categories, with the remainder being categorized as low/low-middle (27.0%) or high (18.1%). Overall, participants with complete follow-up data were more likely to be female, Caucasian, and from a higher socioeconomic category (ps<.05).
Table 1.
Sample characteristics (N=1,902), M±SD unless otherwise indicated
|
|
|||
|---|---|---|---|
| Time 1 | Time 2 | Time 3 | |
|
Demographic and Anthropometric Variables
| |||
| Age | 14.9±1.6 | 19.4±1.6 | 25.2±1.6 |
| Caucasian | 66.5 (1,264) | See Time 1 | See Time 1 |
| Asian | 15.4 (293) | See Time 1 | See Time 1 |
| Race/ethnicity, % (n) | |||
| Black | 8.9 (170) | See Time 1 | See Time 1 |
| Hispanic | 3.4 (65) | See Time 1 | See Time 1 |
| Other | 5.8 (110) | See Time 1 | See Time 1 |
| Overweight, % (n) | 25.9 (436) | 26.7 (443) | 50.5 (843) |
|
| |||
|
Psychological, Behavioral, and Interpersonal Variables
| |||
| Depressive symptoms | 10.5±2.8 | 11.2±2.9 | 11.1±3.0 |
| Disordered eating, % (n ) | 15.0 (244) | 19.0 (353) | 21.7 (402) |
| Body satisfaction | 33.9±9.4 | 33.1±9.5 | 31.6±9.6 |
| Dieting, % (n) | 43.3 (788) | 43.3 (820) | 47.8 (882) |
| Weight-related teasing | 1.8±1.2 | 1.8±1.1 | 1.8±1.1 |
Note: Time 1=early/middle adolescence; Time 2=middle adolescence/early young adulthood; Time 3=early/middle young adulthood. Disordered eating=reported binge eating and/or self-induced vomiting, laxative use, or diuretic use for weight control. Dieting=reporting ever changing the way that one eats for weight loss during the last year. Depressive symptoms range=6–18; body satisfaction range=10–50; weight-related teasing range=1–5.
Measures
Key items used in this paper were consistent across the three study waves to facilitate examination of data longitudinally. A subsample of EAT-I participants (n=161) completed identical versions of the survey approximately two weeks apart in order to calculate test-retest reliability.
Anthropometric and demographic factors
Self-reported height and weight were used to determine body mass index (BMI; kg/m2) percentiles, based on age- and sex-specific Centers for Disease Control and Prevention normative data (Kuczmarski et al., 2000). Overweight referred to a BMI≥85th percentile (Kuczmarski et al., 2000) at T1 and T2, and a BMI≥25 at T3. Self-reported height and weight were validated in a subsample of 125 EAT-III (T3) participants for whom height and weight were measured by trained research staff. Results showed very high correlations between self-reported and measured BMI in males (r=.95) and females (r=.98). Age, sex, and race/ethnicity (Eaton, Brener, Kann, & Pittman, 2007) were based on self-report. Five levels of socioeconomic status (SES) were based on the highest educational attainment by either parent, which appears to be a valid proxy for most adolescents and emerging young adults (Lien, Friestad, & Klepp, 2001). Where this information was missing, eligibility for public assistance, eligibility for free/reduced cost school meals, and parental employment status were used to infer SES (Neumark-Sztainer, Story, Hannan, & Croll, 2002).
Behavioral factors
Binge eating was ascertained as follows: “In the past year, have you ever eaten so much food in a short period of time that you would be embarrassed if others saw you?”; “During the times when you ate this way, did you feel you couldn’t stop eating or control what or how much you were eating?” These items have good concurrent validity and test-retest reliability (Nangle, Johnson, Carr-Nangle, & Engler, 1994; present study test-retest agreement=92% for overeating, 84% for loss of control). A positive response to both questions was classified as binge eating. Extreme weight control behaviors were assessed with the question, “Have you done any of the following things in order to lose weight or keep from gaining weight during the past year? (yes or no for each behavior).” Weight control behaviors categorized as “extreme” included “made myself vomit,” “used laxatives,” “used diuretics,” and “took diet pills” [percent agreement (yes vs. no) for test-retest data=98%). Disordered eating was considered to be present if binge eating and/or extreme weight control behaviors were endorsed. Dieting was assessed with the question, “How often have you gone on a diet during the last year? By ‘diet’ we mean changing the way you eat so you can lose weight.” Responses included “never;” “one to four times;” “five to 10 times;” “more than 10 times;” and “I am always dieting” [Spearman’s r for test-retest data=.71; percent agreement (never vs. ever dieted) for test-retest data=76%].
Psychosocial factors
Depressive symptoms were assessed via Kandel and Davies’ six-item scale for adolescents (Kandel & Davies, 1982), which inquires about the frequency of dysphoric mood, tension/nervousness, fatigue, worry, sleep disturbance, and hopelessness during the past year. Scores range from 6–18, with higher scores indicating greater depressive symptoms (present study α=.84). Body satisfaction was measured using a modified version of the Body Shape Satisfaction Scale (Pingitore, Spring, & Garfield, 1997), in which respondents rate their satisfaction with 10 aspects of their body (e.g., height, weight, body shape, thighs). Scores range from 10–50 with higher scores reflecting greater satisfaction (present study α=.92). Teasing experiences were assessed via two items: “How often did any of the following things happen to you: 1) You were teased about your weight; 2) You were teased about your appearance.” Responses ranged from “never” to “at least once a week” (Spearman’s r for test-retest data=.47). These questions were combined to form a mean teasing index; higher scores indicate more frequent teasing experiences. Teasing questions were based on a previously validated questionnaire (Thompson, Cattarin, Fowler, & Fisher, 1995).
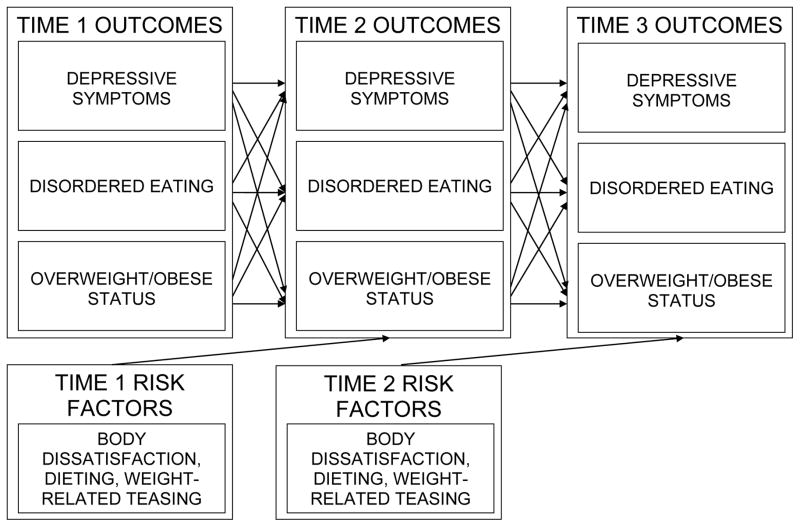
Statistical Analysis
All analyses were stratified by gender. Correlations were used to examine cross-sectional and prospective associations among the categorical and continuous outcomes at each timepoint, and cross-tabulated frequencies summarized the percentage of overlap among the dichotomized outcomes of depressive symptoms (above vs. below the minimum value of the upper quartile of depressive symptoms within the full EAT-I sample), disordered eating (present vs. absent), and weight status (overweight vs. non-overweight). Structural equation modeling was used to examine T1 psychological (body satisfaction), behavioral (dieting), and social (weight-related teasing) risk factors as simultaneous longitudinal predictors of T2 depressive symptoms, disordered eating, and weight status, and, separately, to examine T2 risk factors as longitudinal predictors of T3 outcomes (see Figure 1). All models controlled for age, race/ethnicity, and SES. Also included as covariates were the outcome variables as measured at the previous timepoint (i.e., analyses examining T1 predictors of T2 depressive symptoms, disordered eating, and weight status controlled for T1 depressive symptoms, disordered eating, and weight status). In these models, depressive symptoms, body satisfaction, and teasing were treated as continuous, while disordered eating and dieting were binary (according to whether the subjects endorsed binge eating and/or extreme weight control behaviors, or reported “never” or “ever” dieting in the past year, respectively). Weight status was categorized ordinally (non-overweight, overweight, obese). Because attrition from the T1 sample was not random, data were weighted with the inverse of the estimated probability that an individual responded at all three timepoints. The use of non-response sampling weights generates estimates that represent the demographic composition of the EAT-I sample corresponding to the analytic subgroup. MPlus 7.1 was used for the structural equation models utilizing the weighted least squares estimation, which appropriately accommodates categorical outcome variables.
Figure 1.
Theoretical model of the relationships among psychological, behavioral, and interpersonal risk factors, and mood-, eating-, and weight-related outcomes
Results
Overlap Among Health Outcomes
The percentage of males with any combination of two or more of the mood-, eating-, and weight-related health outcomes was 11.2%, 15.5%, and 25.7% at T1, T2, and T3, respectively (see Table 2). The percentage of females with any combination of two or more of these health-related outcomes was 21.5%, 29.9%, and 38.7% at T1, T2, and T3, respectively.
Table 2.
Cross-tabulations for depressive symptoms, disordered eating, and excess weight status among males and females
| Combination of conditions | Frequency of combination patterns (%) | ||||
|---|---|---|---|---|---|
|
| |||||
| Depressive symptoms | Disordered eating | Excess weight status | |||
| Males | Time 1 | Time 2 | Time 3 | ||
|
| |||||
| Yes | Yes | Yes | 8 (1.0) | 19 (2.4) | 43 (5.3) |
| Yes | No | Yes | 48 (6.2) | 66 (8.5) | 124 (15.3) |
| No | Yes | Yes | 10 (1.3) | 17 (2.3) | 33 (4.1) |
| No | No | Yes | 148 (19.0) | 99 (12.6) | 249 (30.8) |
| Yes | Yes | No | 21 (2.7) | 18 (2.3) | 8 (1.0) |
| Yes | No | No | 111 (14.2) | 171 (21.8) | 108 (13.4) |
| No | Yes | No | 13 (1.7) | 13 (1.7) | 11 (1.4) |
| No | No | No | 421 (54.0) | 380 (48.5) | 232 (28.7) |
|
| |||||
|
Females
| |||||
| Yes | Yes | Yes | 43 (4.2) | 61 (6.2) | 137 (13.9) |
| Yes | No | Yes | 62 (6.1) | 92 (9.3) | 131 (13.2) |
| No | Yes | Yes | 37 (3.6) | 36 (3.6) | 55 (5.6) |
| No | No | Yes | 119 (11.7) | 84 (8.5) | 134 (13.5) |
| Yes | Yes | No | 77 (7.6) | 107 (10.8) | 59 (6.0) |
| Yes | No | No | 238 (23.4) | 247 (24.9) | 171 (17.3) |
| No | Yes | No | 53 (5.2) | 59 (6.0) | 42 (4.2) |
| No | No | No | 389 (38.2) | 304 (30.7) | 260 (26.3) |
Note: Time 1=early/middle adolescence; Time 2=middle adolescence/early young adulthood; Time 3=early/middle young adulthood. Depressive symptoms=above the minimum value of the upper quartile of depressive symptoms within the full EAT-I sample; disordered eating=reported binge eating and/or self-induced vomiting, laxative use, or diuretic use for weight control; excess weight status=overweight/obese.
Shared and Independent Risk Factors for Depressive Symptoms, Disordered Eating, and Excess Weight Status
T1 to T2 Predictors
From the structural equation models (see Table 3), we found that in males, after adjusting for T1 demographics, T1 depressive symptomatology was a risk factor for both T2 depressive symptoms (p<.001) and disordered eating (p=.017); T1 disordered eating predicted T2 depressive symptoms (p=.001); and T1 excess weight status was predictive of T2 excess weight status (p<.001). After controlling for demographics, depressive symptoms, disordered eating, and weight status, T1 dieting and teasing were risk factors for T2 excess weight status (p<.001 and p=.040, respectively), and T1 body dissatisfaction was a risk factor for T2 depressive symptoms (p=.045). There were no shared T1 risk factors for any of the T2 outcomes among males.
Table 3.
Time 1 risk factors for Time 2 depression symptoms, disordered eating, and excess weight status among males and females
|
|
|||||
|---|---|---|---|---|---|
| Males | Females | ||||
| Time 2 Outcome | Time 1 Predictor | Estimate | p-Value | Estimate | p-Value |
| Depressive symptoms | Depressive symptoms | 0.383 | <.001 | 0.396 | <.001 |
| Disordered eating | 0.092 | 0.001 | 0.021 | 0.545 | |
| Excess weight status | −0.058 | 0.105 | 0.005 | 0.882 | |
| Body satisfaction | −0.099 | 0.045 | −0.128 | 0.005 | |
| Dieting | −0.056 | 0.203 | −0.080 | 0.063 | |
| Weight-related teasing | −0.051 | 0.329 | 0.028 | 0.569 | |
|
| |||||
| Disordered eating | Depressive symptoms | 0.143 | 0.017 | 0.033 | 0.463 |
| Disordered eating | 0.097 | 0.113 | 0.138 | 0.002 | |
| Excess weight status | 0.080 | 0.215 | 0.018 | 0.723 | |
| Body satisfaction | −0.031 | 0.760 | −0.210 | 0.002 | |
| Dieting | 0.085 | 0.345 | 0.055 | 0.344 | |
| Weight-related teasing | −0.034 | 0.704 | −0.030 | 0.662 | |
|
| |||||
| Excess weight status | Depressive symptoms | −0.057 | 0.157 | −0.094 | 0.013 |
| Disordered eating | −0.036 | 0.301 | −0.058 | 0.096 | |
| Excess weight status | 0.522 | <.001 | 0.484 | <.001 | |
| Body satisfaction | −0.005 | 0.941 | −0.152 | 0.007 | |
| Dieting | 0.290 | <.001 | 0.104 | 0.039 | |
| Weight-related teasing | 0.119 | 0.040 | 0.172 | 0.002 | |
Note: Time 1=early/middle adolescence; Time 2=middle adolescence/early young adulthood. Disordered eating=reported binge eating and/or self-induced vomiting, laxative use, or diuretic use for weight control; excess weight status=overweight/obese; dieting=reporting ever changing the way that one eats for weight loss during the last year. Significant differences are in bold font.
In females, after controlling for T1 demographics, T1 depressive symptomatology was a risk factor for both T2 depressive symptoms (p<.001) and excess weight status (p=.013); T1 disordered eating predicted T2 disordered eating (p=.002); and T1 excess weight status was predictive of T2 excess weight status (p<.001). After controlling for demographics, depressive symptoms, disordered eating, and weight status, T1 body dissatisfaction was a shared risk factor T2 depressive symptoms (p=.005), disordered eating (p=.002), and excess weight status (p=.007). T1 dieting and teasing were non-shared risk factors for T2 excess weight status (p=.039 and p=.002, respectively).
T2 to T3 Predictors
In males, after adjusting for T2 demographics, T2 depressive symptoms predicted T3 depressive symptoms (p<.001) and disordered eating (p=.036); T2 disordered eating predicted T3 disordered eating (p=.001); and T2 excess weight status predicted T3 excess weight status (p<.001; see Table 4). After adjusting for T2 demographics and outcome variables, T2 dieting was a shared risk factor for T3 disordered eating (p<.001) and excess weight status (p<.001), and T2 body dissatisfaction was a shared risk factor for T3 depressive symptoms (p<.001), disordered eating (p<.001), and excess weight status (p=.010). T2 teasing was a non-shared risk factor for T3 depressive symptoms (p=.004).
Table 4.
Time 2 risk factors for Time 3 depression symptoms, disordered eating, and excess weight status among males and females
|
|
|||||
|---|---|---|---|---|---|
| Males | Females | ||||
| Time 3 Outcome | Time 2 Predictor | Estimate | p-Value | Estimate | p-Value |
| Depressive symptoms | Depressive symptoms | 0.321 | <.001 | 0.359 | <.001 |
| Disordered eating | 0.147 | 0.022 | -0.080 | 0.113 | |
| Excess weight status | −0.059 | 0.264 | 0.110 | 0.017 | |
| Body satisfaction | −0.212 | <.001 | −0.183 | <.001 | |
| Dieting | 0.064 | 0.147 | 0.014 | 0.720 | |
| Weight-related teasing | 0.138 | 0.004 | 0.126 | 0.001 | |
|
| |||||
| Disordered eating | Depressive symptoms | 0.157 | 0.036 | 0.096 | 0.043 |
| Disordered eating | 0.367 | 0.001 | 0.413 | <.001 | |
| Excess weight status | 0.112 | 0.177 | 0.087 | 0.146 | |
| Body satisfaction | −0.187 | 0.036 | −0.125 | 0.066 | |
| Dieting | 0.278 | <.001 | 0.273 | <.001 | |
| Weight-related teasing | 0.048 | 0.588 | 0.097 | 0.071 | |
|
| |||||
| Excess weight status | Depressive symptoms | 0.024 | 0.531 | 0.116 | 0.002 |
| Disordered eating | 0.053 | 0.423 | 0.039 | 0.447 | |
| Excess weight status | 0.679 | <.001 | 0.735 | <.001 | |
| Body satisfaction | −0.130 | 0.010 | −0.211 | <.001 | |
| Dieting | 0.246 | <.001 | 0.092 | 0.048 | |
| Weight-related teasing | −0.052 | 0.284 | 0.039 | 0.399 | |
Note: Time 2=middle adolescence/early young adulthood; Time 3=early/middle young adulthood. Disordered eating=reported binge eating and/or self-induced vomiting, laxative use, or diuretic use for weight control; excess weight status=overweight/obese; dieting=reporting ever changing the way that one eats for weight loss during the last year. Significant differences are in bold font.
In females, after adjusting for T2 demographics, T2 depressive symptomatology was a risk factor for T3 depressive symptoms (p<.001), disordered eating (p=.043), and excess weight status (p=.002); T2 disordered eating predicted T3 disordered eating (p<.001); and T2 excess weight status predicted T3 excess weight status (p<.001) and depressive symptoms (p=.017). After controlling for T2 demographics and outcome variables, T2 dieting was a shared risk factor for disordered eating (p<.001) and excess weight status (p=.048). T2 body dissatisfaction was a shared risk factor for T3 depressive symptoms (p<.001) and excess weight status (p<.001). Finally, T2 teasing was a risk factor for T3 depressive symptoms (p=.001).
Discussion
In the current study, we found that depressive symptoms, disordered eating, and excess weight status were relatively stable across three timepoints during adolescence and young adulthood, and that there was moderate overlap among the conditions within and across timepoints. In males, body dissatisfaction in middle adolescence/early young adulthood was a shared risk factor for depressive symptoms, disordered eating, and overweight in early/middle young adulthood, and dieting in middle adolescence/early young adult was a shared risk factor for disordered eating and overweight in early/middle young adulthood. In females, early/middle adolescent body dissatisfaction was a shared risk factor depressive symptoms, disordered eating, and overweight in middle adolescence/early young adulthood, while body dissatisfaction in middle adolescence/early young adulthood was a shared risk factor for depressive symptoms and overweight in early/middle young adulthood. Dieting in middle adolescence/early young adulthood was a shared risk factor for disordered eating and overweight in early/middle young adulthood. Thus, body dissatisfaction and dieting appear to be critical constructs to consider in developing preventive interventions targeting shared risk for these conditions.
Prevention programs targeting depression, disordered eating, and overweight have shown demonstrable improvements in reducing risk factors for and incidence of the target condition (Stice, Becker, & Yokum, 2013; Stice, Shaw, Bohon, Marti, & Rohde, 2009; Waters et al., 2011). Given the overlap in these health conditions, outcomes (and cost-effectiveness) of preventive interventions could be improved further by addressing shared risk factors (Rodgers & Paxton, 2014). The current data suggest that body dissatisfaction and dieting are viable treatment targets for such shared prevention programs. Indeed, prevention programs addressing these risk factors often result in improvements across multiple outcomes (Stice, Shaw, Burton, & Wade, 2006; Wilksch & Wade, 2009), suggesting that addressing shared risk is both expeditious and efficacious. Leaders in healthcare are increasingly calling for cost-effective, scalable interventions that reach large numbers of individuals to reduce the burden of mental illness and conditions like obesity (Austin, 2012; Kazdin & Blase, 2011; Kazdin & Rabbitt, 2013; Patel, Chowdhary, Rahman, & Verdeli, 2011). Preventive interventions that have the potential to successfully impact multiple targets by modifying shared risk factors are a viable method for answering these calls to action. To facilitate the development and refinement of such interventions, future clinical trials should assess a range of potential outcomes (including, but not limited to, depressive symptoms, disordered eating, and body weight) so as to enhance knowledge about the inter-relationships among risk factors and their response to various treatment options.
Strengths of the current study include the prospective design and the diverse, community-based sample. However, several limitations should be noted. First, because data were collected within a large epidemiological study, the use of “gold standard” measures was not feasible, and brief self-report measures were instead used to assess anthropometric, psychosocial, and behavioral variables (although self-reported and measured height and weight had good concordance in this sample at Time 3; Himes, Hannan, Wall, & Neumark-Sztainer, 2005). In particular, some multidimensional constructs (e.g., dieting) were measured using one or two indicators, highlighting the need for more comprehensive assessments in future replication studies. On a related note, outcomes were continuous or sub-syndromal variants of depression and eating disorders, respectively, rather than full-threshold diagnostic states. Indeed, the sample generally reported low-to-moderate impairment across both outcome and risk factor variables (although notably, prevalence rates of disordered eating and dieting were slightly higher than in other community-based samples, perhaps due to the use of different measures; Haines et al., 2010), which makes it difficult to infer whether the findings could apply to those with higher levels of impairment (e.g., clinical populations). However, this approach facilitated the examination of a spectrum of impairment, which potentially aids in generalizability and the development of population-based, non-clinical interventions. Second, attrition between T1 and Time 2 was significant and non-random, however, there was minimal attrition from Time 2 to Time 3, and the sample was weighted to maintain consistency with the original EAT sample.
In summary, there is a need for preventive interventions to address shared risk factors for overlapping health conditions in order to promote efficacy, generalizability, and conservative allocation of limited resources. The current study suggests that there is considerable overlap in both prevalence of and risk factors for depressive symptoms, disordered eating, and excess weight status; hence, prevention programs could conceivably target all three conditions via shared pathways to onset (e.g., reducing dieting behaviors, improving body satisfaction). Future research should identify shared risk factors for the full-syndrome variants of these symptom profiles, and should incorporate findings into the development of novel prevention programs.
Acknowledgments
This work was support by grant R01-HL084064 from the National Heart, Lung, and Blood Institute (DNS). ABG’s time was supported by KL2-RR025000 from the National Center for Research Resources.
Footnotes
Author Note: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
The study sponsors were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. MMW had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors have no conflicts of interest to report.
References
- Allen KL, Byrne SM, McLean NJ. The dual-pathway and cognitive- behavioural models of binge eating: prospective evaluation and comparison. European Child and Adolescent Psychiatry. 2012;21:51–62. doi: 10.1007/s00787-011-0231-z. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, D.C: 2013. [Google Scholar]
- Austin SB. A public health approach to eating disorders prevention: it's time for public health professionals to take a seat at the table. BMC Public Health. 2012;12:854. doi: 10.1186/1471-2458-12-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker CB, Plasencia M, Kilpela LS, Briggs M, Stewart T. Changing the course of comorbid eating disorders and depression: what is the role of public health interventions in targeting shared risk factors? J Eat Disord. 2014;2:15. doi: 10.1186/2050-2974-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Brener ND, Kann L, Pittman V. High school student responses to different question formats assessing race/ethnicity. Journal of Adolescent Health. 2007;41:488–494. doi: 10.1016/j.jadohealth.2007.05.017. [DOI] [PubMed] [Google Scholar]
- Fabricatore AN, Wadden TA. Obesity. Annual Review of Clinical Psychology. 2006;2:357–377. doi: 10.1146/annurev.clinpsy.2.022305.095249. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A "transdiagnostic" theory and treatment. Behaviour Research and Therapy. 2003;41:509–528. doi: 10.1016/S0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Faith MS, Butryn M, Wadden TA, Fabricatore A, Nguyen AM, Heymsfield SB. Evidence for prospective associations among depression and obesity in population-based studies. Obesity Reviews. 2011;12:e438–e453. doi: 10.1111/j.1467-789X.2010.00843.x. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Fitzsimmons-Craft EE, Le Grange D. Eating disorders. In: Friedman HS, editor. Encyclopedia of Mental Health. 2. New York, NY: Elsevier; (in press) [Google Scholar]
- Goldschmidt AB, Wall MM, Choo TJ, Larson N, Neumark-Sztainer D. Mediators involved in the relation between depressive symptoms and obesity in female adolescents and young adults. International Journal of Obesity. 2015;39:1027–1029. doi: 10.1038/ijo.2015.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MA, Scott NA, Cross SE, Liao KY, Hallengren JJ, Davids CM, Jepson AJ. Eating disorder behaviors and depression: a minimal relationship beyond social comparison, self-esteem, and body dissatisfaction. Journal of Clinical Psychology. 2009;65:989–999. doi: 10.1002/jclp.20586. [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines J, Kleinman KP, Rifas-Shiman SL, Field AE, Austin SB. Examination of shared risk and protective factors for overweight and disordered eating among adolescents. Archives of Pediatrics and Adolescent Medicine. 2010;164:336–343. doi: 10.1001/archpediatrics.2010.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Education Research. 2006;21:770–782. doi: 10.1093/her/cyl094. [DOI] [PubMed] [Google Scholar]
- Himes JH, Hannan P, Wall M, Neumark-Sztainer D. Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Annals of Epidemiology. 2005;15:272–278. doi: 10.1016/j.annepidem.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Fittig E, Bryson SW, Wilfley D, Kraemer HC, Taylor CB. Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high-risk sample. Psychological Medicine. 2011;41:1939–1949. doi: 10.1017/S0033291710002631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Kandel D, Davies M. Epidemiology of depressive mood in adolescents. Archives of General Psychiatry. 1982;39:1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science. 2011;6:21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science. 2013;1:170–191. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Johnson CL. CDC growth charts: United States. Advance Data. 2000;314:1–27. [PubMed] [Google Scholar]
- Lien N, Friestad C, Klepp KI. Adolescents' proxy reports of parents' socioeconomic status: How valid are they? Journal of Epidemiology and Community Health. 2001;55:731–737. doi: 10.1136/jech.55.10.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nangle DW, Johnson WG, Carr-Nangle RE, Engler LB. Binge eating disorder and the proposed DSM-IV criteria: Psychometric analysis of the Questionnaire of Eating and Weight Patterns. International Journal of Eating Disorders. 1994;16:147–157. doi: 10.1002/1098-108X(199409)16:2<147::AID-EAT2260160206>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. Depression in adults: The treatment and management of depression in adults. London, UK: National Collaborating Centre for Mental Health; 2009. [Google Scholar]
- Neumark-Sztainer D, Story M, Hannan PJ, Croll J. Overweight status and eating patterns among adolescents: Where do youths stand in comparison with the healthy people 2010 objectives? American Journal of Public Health. 2002;92:844–851. doi: 10.2105/AJPH.92.5.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association. 2011;111:1004–1011. doi: 10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall MM, Haines JI, Story MT, Sherwood NE, van den Berg PA. Shared risk and protective factors for overweight and disordered eating in adolescents. American Journal of Preventive Medicine. 2007;33:359–369. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- Patel V, Chowdhary N, Rahman A, Verdeli H. Improving access to psychological treatments: lessons from developing countries. Behaviour Research and Therapy. 2011;49:523–528. doi: 10.1016/j.brat.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pingitore R, Spring B, Garfield D. Gender differences in body satisfaction. Obesity Research. 1997;5:402–409. doi: 10.1002/j.1550-8528.1997.tb00662.x. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Etiology of binge eating: Psychological mechanisms. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. New York, NY: Guilford Press; 1993. pp. 173–205. [Google Scholar]
- Presnell K, Stice E, Seidel A, Madeley MC. Depression and eating pathology: prospective reciprocal relations in adolescents. Clinical Psychology & Psychotherapy. 2009;16:357–365. doi: 10.1002/cpp.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Luedicke J. Weight-based victimization among adolescents in the school setting: emotional reactions and coping behaviors. J Youth Adolesc. 2012;41:27–40. doi: 10.1007/s10964-011-9713-z. [DOI] [PubMed] [Google Scholar]
- Quick V, Wall M, Larson N, Haines J, Neumark-Sztainer D. Personal, behavioral and socio-environmental predictors of overweight incidence in young adults: 10-yr longitudinal findings. Int J Behav Nutr Phys Act. 2013;10:37. doi: 10.1186/1479-5868-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranzenhofer LM, Columbo KM, Tanofsky-Kraff M, Shomaker LB, Cassidy O, Matheson BE, Yanovski JA. Binge eating and weight-related quality of life in obese adolescents. Nutrients. 2012;4:167–180. doi: 10.3390/nu4030167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas DL, Grilo CM. Timing and sequence of the onset of overweight, dieting, and binge eating in overweight patients with binge eating disorder. International Journal of Eating Disorders. 2007;40:165–170. doi: 10.1002/eat.20353. [DOI] [PubMed] [Google Scholar]
- Rodgers RF, Paxton SJ. The impact of indicated prevention and early intervention on co-morbid eating disorder and depressive symptoms: a systematic review. J Eat Disord. 2014;2:30. doi: 10.1186/s40337-014-0030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, Field AE. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: Does loss of control matter? JAMA Pediatr. 2013;167:149–155. doi: 10.1001/2013.jamapediatrics.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Agras WS. Predicting onset and cessation bulimic behaviors during adolescence: A longitudinal grouping analysis. Behavior Therapy. 1998;29:257–276. [Google Scholar]
- Stice E, Becker CB, Yokum S. Eating disorder prevention: current evidence-base and future directions. International Journal of Eating Disorders. 2013;46:478–485. doi: 10.1002/eat.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006x.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JK, Cattarin J, Fowler B, Fisher E. The Perception of Teasing Scale (POTS): A revision and extension of the Physical Appearance Related Teasing Scale (PARTS) Journal of Personality Assessment. 1995;65:146–157. doi: 10.1207/s15327752jpa6501_11. [DOI] [PubMed] [Google Scholar]
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- Wilksch SM, Wade TD. Reduction of shape and weight concern in young adolescents: a 30-month controlled evaluation of a media literacy program. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:652– 661. doi: 10.1097/CHI.0b013e3181a1f559. [DOI] [PubMed] [Google Scholar]