Abstract
Background and Objectives
Statin-induced changes in high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) are unrelated. Many patients initiated on statins experience a paradoxical decrease in HDL-C. The aim of this study was to evaluate the association between a decrease in HDL-C and risk of major adverse cardiovascular events (MACE).
Methods
Data from 15,357 primary care patients initiated on statins during 2004–2009 were linked with data from mandatory national hospital, drug-dispensing, and cause-of-death registers, and were grouped according to HDL-C change: decreased ≥0.1 mmol/L, unchanged ±0.1 or ≥0.1 mmol/L increased. To evaluate the association between decrease in HDL-C and risk of MACE, a sample of propensity score-matched patients from the decreased and unchanged groups was created, using the latter group as reference. MACE was defined as myocardial infarction, unstable angina pectoris, ischaemic stroke, or cardiovascular mortality. Cox proportional hazards models were used to estimate relative risks.
Results
HDL-C decreased in 20 %, was unchanged in 58%, and increased in 22 % of patients initiated on statin treatment (96 % treated with simvastatin). The propensity score-matched sample comprised 5950 patients with mean baseline HDL-C and LDL-C of 1.69 and 4.53 mmol/L, respectively. HDL-C decrease was associated with 56 % higher MACE risk (hazard ratio 1.56; 95 % confidence interval 1.12–2.16; p < 0.01) compared with the unchanged HDL-C group.
Conclusions
Paradoxical statin-induced reduction in HDL-C was relatively common and was associated with increased risk of MACE.
Electronic supplementary material
The online version of this article (doi:10.1007/s40261-015-0372-9) contains supplementary material, which is available to authorized users.
Key Points
| Of patients newly initiated on statin treatment, one-fifth experienced a decrease in HDL-C. |
| This HDL-C decrease was associated with higher risk of major adverse cardiovascular events compared with unchanged HDL-C. |
| Statin induced HDL-C decrease might be more hazardous than previously recognised and patients should be monitored closely regarding potential cardiovascular risk. |
Introduction
The role of high-density lipoprotein cholesterol (HDL-C) as a potential risk factor in the development of cardiovascular disease (CVD) is not fully understood. Epidemiological studies have reported an association between HDL-C single point measurements and risk of coronary heart disease (which forms a large proportion of CVD) [1–3]. Some guidelines recommend an HDL-C target above 1.0 mmol/L for men and above 1.2 mmol/L for women, [4] but such goals have also been questioned [5, 6]. Recent studies with novel HDL-C-raising therapies have not shown a clear preventive effect of increasing HDL-C on risk of CVD. Treatment with one such agent, torcetrapib, resulted in an increased risk of mortality and morbidity of unknown mechanism, whereas potential favourable effects of another agent, dalcetrapib, with respect to HDL-C were possibly offset by other unfavourable effects [7, 8].
Statins show various degrees of low-density lipoprotein cholesterol (LDL-C)-lowering and HDL-C-raising effects, [9] where the action on HDL-C is independent of the reduction in LDL-C [10]. Is has been indicated from a meta-analysis that among statin-treated patients, HDL-C levels are strongly and inversely associated with the risk of major cardiovascular events [11]. Notably, a large proportion of patients experienced a paradoxical decrease in HDL-C following statin treatment initiation [10]. A recent study reported an inverse association between the paradoxical HDL-C decrease after initiation of statin therapy and major adverse cardiovascular events in patients with acute myocardial infarction [12]. It is possible that a reduction in HDL-C is associated with suboptimal protection against cardiovascular events [13].
The aim of this observational study was to investigate the association between paradoxical HDL-C decrease after initiation of statin therapy and major adverse cardiovascular events in a general primary care patient population.
Methods
The study protocol was reviewed and approved by the regional research ethics committee in Uppsala, Sweden (Reference number 2012/007) and registered at ClinicalTrials.gov (clinical trial identifier NCT01551784).
This study linked data from electronic patient records to hospital, drug-dispensing, and cause-of-death registers. Information on blood lipids and patient characteristics was extracted from primary care medical records [e.g. date of birth, gender, body weight, blood pressure, number of primary healthcare centre contacts, and diagnosis according to International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) codes) using an established software system [14].
Data regarding morbidity and mortality were collected from the Swedish National Patient Register, inpatient (admission and discharge dates, and main and secondary diagnoses) and outpatient hospital care (number of contacts and diagnosis according to ICD-10-CM codes) registers, and the Swedish National Cause-of-Death Register (date and cause of death) [15]. Drug-dispensing data were collected from the Swedish Prescribed Drug Register.
Data linkage was performed by the Swedish National Board of Health and Welfare. The linked study database is owned and managed by the Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden. Personal identification numbers used to identify included patients in all healthcare contacts and were anonymised prior to further data processing.
The study population consisted of statin-naïve patients initiating a first statin treatment at 76 primary care centres in Sweden. To facilitate a representative selection of primary care centres in Sweden, a mix of rural and urban areas, public and private care providers, and small, mid-sized, and large primary care centres (all using the same electronic patient journal system) was included, corresponding to approximately 7 % of the Swedish primary care centres. Men and women were eligible for inclusion if they were aged 18–85 years and were prescribed statins [Anatomical Therapeutic Chemical (ATC): C10A A] between 1 January 2004 and 31 December 2009. Patients had to have HDL-C and LDL-C measurements recorded within 12 months prior to the start of statin treatment as well as a measurement after 10 days and within 12 months on treatment; patients with cardiovascular events before the first HDL-measurement on statin treatment were excluded. Patients with an LDL-C lowering of no more than 0.5 mmol/L were also excluded due to insufficient statin effect or indication of low compliance to statin treatment. Further exclusion criteria were prior history of alcoholism and on-going malignancy.
The date of first known statin dispense was defined as start of statin treatment. The start of the observation period for collecting endpoints was date of first HDL-C measurement on statin treatment. The end of the study observation was 31 December 2011, the end of statin treatment, or death. If a gap of more than 90 days was observed, based on available dispensed drug data, the end of statin treatment was defined as calculated days on last available dispensed drug package plus an additional 25 % of days based on the last dispensed drug pack size.
Two HDL-C groups were defined based on change in between last HDL-C measurement prior statin treatment and first HDL-C measurement on at least 14 days of statin treatment: HDL-C decrease: more than 0.1 mmol/L and HDL-C unchanged group: ±0.1 mmol/L. In addition, a group with more than 0.1 mmol/L increase in HDL-C was defined to explore the effect of HDL-C increase.
The analysis was performed in two patient samples; the matched sample, which included HDL-C decrease and unchanged HDL-C patients who fulfilled the inclusion and exclusion criteria and who could be propensity score matched for baseline characteristics regarding propensity of HDL-C decrease. The unmatched population used for sub-group analyses comprised all patients who fulfilled the inclusion and exclusion criteria.
The major adverse cardiovascular event (MACE) endpoint was a composite of hospitalisation for a primary diagnosis for myocardial infarction (ICD-10, I21), unstable angina pectoris (ICD-10, I20.0), ischaemic stroke (ICD-10, I63), or cardiovascular death (all primary causes of death diagnosed with ICD-10 codes I00–I99).
Differences in baseline data between the two HDL-C groups were tested by one-way ANOVA and Pearson’s chi-square test according to the type of data. Differences between groups were considered statistically significant when p was less than 0.05.
Propensity score matching provides an alternative means to balance study groups in order to reduce confounding when randomisation is not possible [16–20]. Logistic regression models were included to estimate the propensity scores between the decreased and unchanged HDL-C groups, with the HDL-C decrease as the response variable and the following covariates: age, gender, baseline HDL-C, baseline LDL-C, LDL-C change on statin treatment, antihypertensive therapy, diagnosis of diabetes, heart failure, hypertension, angina pectoris, peripheral artery disease (PAD), and stroke.
The propensity scores were matched pairwise, with exact matching for prior myocardial infarction and use of calipers of width equal to 0.1 of the standard deviation of the propensity score. The matching procedure was performed using the Match function in the R package Matching [21]. The primary endpoint was analysed by a Cox proportional hazards model, using a grouped jack-knife estimation of the variance to take the correlation within pairs into account.
The association between HDL-C change and the primary endpoint in the decreased and increased HDL-C groups was studied in the following sub groups: gender (men/women), primary/secondary prevention, with/without diabetes, and in patients above 75 years of age versus younger patients. In the sub-group analyses, Cox regression with adjustment for age, gender, baseline HDL-C, baseline LDL-C, LDL-C change on statin treatment, antihypertensive therapy, diagnoses of diabetes, heart failure, hypertension, angina pectoris, PAD, and stroke was used.
An additional analysis was performed comparing the separate outcome of cardiovascular death or all-cause death, as well as a sensitivity analysis including patients with a LDL-C reduction of <0.5 mmol/L.
Results
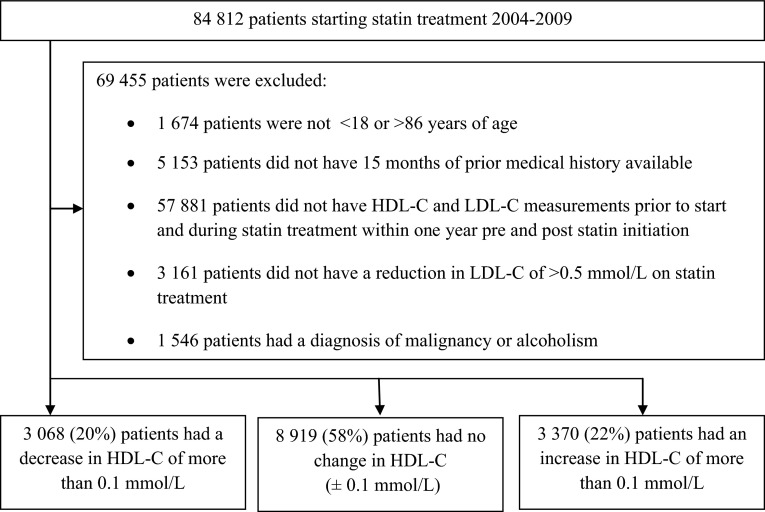
In all, 84,812 patients were initiated on statin treatment during the observation period, of whom 15,357 (18 %) were eligible (Fig. 1). The main reason for exclusion was lack of recorded lipid measurements before and during statin treatment. Compared with the study population, the excluded patients were more often men, were older, and fewer had diabetes/more had CVD before statin treatment initiation (Table S1).
Fig. 1.
Patient flow. HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol
In the full eligible study cohort, baseline mean age was 62.7 years (range 19–85 years) and mean HDL-C was 1.48 mmol/L. The majority of patients (96 %) were initiated on simvastatin, with a mean dose of 20 mg/day (median 20 mg/day). Of these patients, 20 % had a decrease in HDL-C during the observation period, 58 % were unchanged, and 22 % showed an increase (Fig. 1). The patient group with a decrease in HDL-C comprised more women, had a higher HDL-C at baseline (1.69 mmol/L), less diabetes, compared with the unchanged HDL-C group (Table 1). The groups were similar regarding presence of cardiovascular diagnoses; myocardial infarction, angina pectoris, PAD, stroke or heart failure. The changes in HDL-C and LDL-C did not show any correlation (Fig. S1) [10].
Table 1.
Baseline characteristics for patients with a decrease in HDL-C (≥0.1 mmol/L), an increase in HDL-C (≥0.1 mmol/L), or no change in HDL-C (±0.1 mmol/L) (unmatched and propensity score-matched populations)
| Variable | Unmatched population | Propensity score-matched population | ||||
|---|---|---|---|---|---|---|
| Decreased (n = 3068) | Unchanged (n = 8919) | Increased (n = 3370) | Decreased (n = 2975) | Unchanged (n = 2975) | p valuea | |
| Women, n (%) | 1872 (61.0) | 4840 (54.3) | 1997 (59.3) | 1803 (60.6) | 1798 (60.4) | 0.92 |
| Age (years) | 62.3 (10.2) | 62.6 (10.2) | 63.0 (9.8) | 62.2 (10.1) | 62.3 (10.2) | 0.64 |
| Simvastatin, n (%) | 2925 (95.3) | 8510 (95.4) | 3244 (96.3) | 2835 (95.3) | 2823 (94.9) | 0.09 |
| Dose (mg) | 20.8 (9.7) | 19.7 (8.7) | 20.2 (8.8) | 20.8 (9.7) | 19.7 (8.4) | <0.01 |
| Hospitalisations, number/year prior to statin start | 0.2 (0.6) | 0.2 (0.6) | 0.19 (0.6) | 0.2 (0.6) | 0.2 (0.6) | 0.16 |
| Systolic blood pressure (mmHg) | 144.6 (19.8) | 143.6 (18.6) | 144.0 (18.9) | 144.6 (19.8) | 143.3 (19.0) | 0.02 |
| Diastolic blood pressure (mmHg) | 82.6 (10.4) | 82.0 (10.1) | 82.0 (10.4) | 82.7 (10.4) | 81.9 (10.2) | 0.01 |
| Body mass index (kg/cm2) | 28.6 (5.0) | 29.4 (5.0) | 28.8 (4.9) | 28.7 (5.0) | 28.6 (5.2) | 0.67 |
| HbA1c (%) | 5.5 (1.3) | 5.7 (1.3) | 5.64 (1.4) | 5.6 (1.3) | 5.6 (1.4) | 0.77 |
| HDL-C (mol/L) | 1.69 (0.47) | 1.41 (0.40) | 1.44 (0.42) | 1.66 (0.43) | 1.66 (0.45) | 0.95 |
| LDL-C (mmol/L) | 4.53 (1.00) | 4.45 (0.95) | 4.52 (0.97) | 4.53 (0.99) | 4.52 (0.96) | 0.71 |
| Change in LDL-C (mmol/L) | −1.96 (0.81) | −1.84 (0.70) | −1.86 (0.75) | −1.95 (0.80) | −1.96 (0.73) | 0.92 |
| Total cholesterol (mmol/L) | 6.88 (1.10) | 6.66 (1.04) | 6.77 (1.07) | 6.86 (1.09) | 6.86 (1.05) | 0.86 |
| Triglycerides (mmol/L) | 1.61 (0.45) | 1.37 (0.38) | 1.40 (0.40) | 1.53 (0.75) | 1.55 (0.75) | 0.23 |
| Antihypertensives (hypertension), n (%) | 1426 (46.5) | 4320 (48.4) | 1530 (45.4) | 1379 (46.4) | 1410 (47.4) | 0.44 |
| Diabetes, n (%) | 691 (22.5) | 2433 (27.3) | 834 (24.8) | 678 (22.8) | 680 (22.9) | 0.98 |
| Myocardial infarction, n (%) | 107 (3.5) | 254 (2.9) | 81 (2.4) | 93 (3.1) | 93 (3.1) | 1.00 |
| Unstable angina pectoris, n (%) | 45 (1.5) | 129 (1.5) | 46 (1.4) | 44 (1.5) | 43 (1.5) | 1.00 |
| Heart failure, n (%) | 75 (2.4) | 237 (2.7) | 75 (2.2) | 73 (2.5) | 72 (2.4) | 1.00 |
| Arrhythmia, n (%) | 182 (5.9) | 480 (5.4) | 175 (5.2) | 177 (6.0) | 180 (6.1) | 0.64 |
| Peripheral arterial disease, n (%) | 54 (1.8) | 130 (1.5) | 56 (1.7) | 52 (1.8) | 44 (1.5) | 0.47 |
| Cerebrovascular disease, n (%) | 242 (7.9) | 665 (7.5) | 208 (6.2) | 181 (6.1) | 172 (5.8) | 0.66 |
Values are expressed as mean (SD) unless specified otherwise
HbA1c glycated haemoglobin, HDL high-density lipoprotein cholesterol, LDL low-density lipoprotein cholesterol
a T test for continuous variables and Chi-square test for categorical variable
The decreased and unchanged HDL-C groups showed a large degree of propensity score overlap (71 %), indicating that these groups were similar prior to the start of statin treatment. After matching, the decreased and unchanged HDL-C groups had similar baseline characteristics and LDL-C changes, with the exception of a higher simvastatin dose and lower triglyceride level in the decreased HDL-C group (Table 1). The mean baseline HDL-C was 1.69 mmol/L and mean LDL-C was 4.53 mmol/L, respectively. The median time from HDL-C measurement to the start of statin treatment was 12 days [interquartile range (IQR) 7–31 days], and the mean time from the start of statin treatment to the second HDL-C measurement was 84 days (IQR 48–148 days). Patients were followed for up to 7 years, with a median follow-up of 2 years, including 14,198 patient-years. In the group with decreased HDL-C, the mean HDL-C reduction was 0.27 mmol/L. The primary endpoint incidence rates (per 1000 patient-years) were 12.8 and 8.2 in the decreased and unchanged HDL-C groups, respectively.
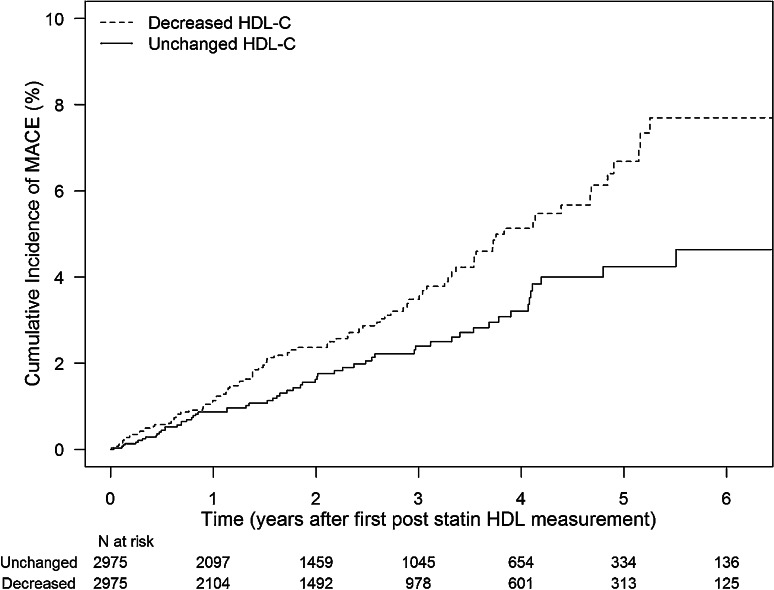
The risk of major cardiovascular events was 56 % higher in the decreased HDL-C group compared with the unchanged HDL-C group [hazard ratio (HR), 1.56; 95 % confidence interval (CI), 1.12–2.16; p < 0.01; Table 2; Fig. 2]. The difference between the two groups was due to ischaemic stroke (HR, 1.74; 95 % CI, 1.00–3.03; p = 0.05), but was also driven by cardiovascular death (HR, 1.72; 95 % CI, 0.86–3.42; p = 0.12).
Table 2.
Exposure time (years) in the propensity score-matched populations
| Unchanged HDL-C | Decreased HDL-C | Total | |
|---|---|---|---|
| Maximum follow-up time | 6.9 | 6.9 | 6.9 |
| Median follow-up time | 1.9 | 2.0 | 2.0 |
| Total patient-years | 7157 | 7041 | 14,198 |
| Total number of events | 59 | 90 | 149 |
Fig. 2.
Kaplan-Meier plot of time to first major cardiovascular events for the decreased and unchanged HDL-C propensity score-matched populations. MACE major adverse cardiovascular events
Subgroup Analyses
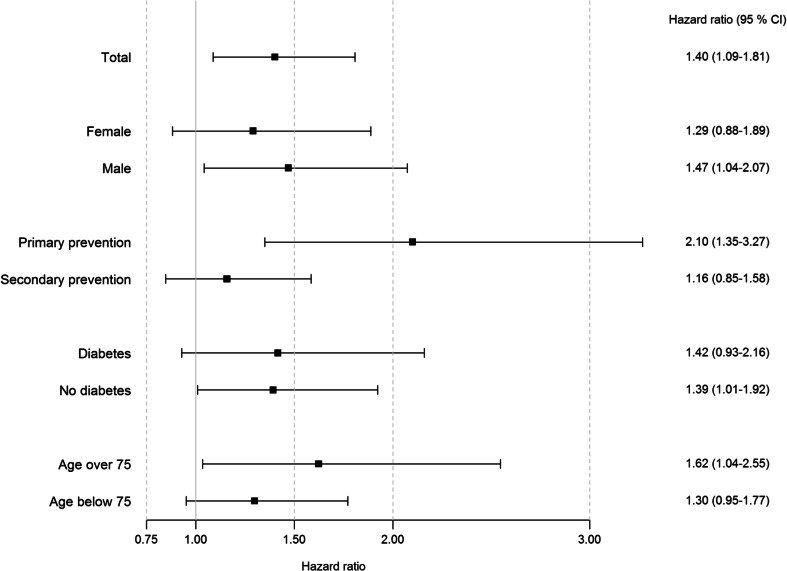
The association between HDL-C change and the primary endpoint in the decreased and increased HDL-C groups showed consistent results in the sub-group analyses: gender, primary/secondary prevention, with/without diabetes, and in patients aged >75 years of age versus younger patients (Fig. 3; Table 3).
Fig. 3.
Hazard ratio forest plot of major cardiovascular events in different sub-groups
Table 3.
Events and events rates for forest plot (Fig. 3)
| Unchanged HDL-C No of patients |
Decreased HDL-C No of patients |
Unchanged HDL-C No of events |
Decreased HDL-C No of events |
Unchanged HDL-C Events/1000 patient-years |
Decreased HDL-C Events/1000 patient-years |
|
|---|---|---|---|---|---|---|
| Total | 8919 | 3068 | 236 | 93 | 11.3 | 12.8 |
| Female | 4840 | 1872 | 98 | 43 | 8.5 | 9.7 |
| Male | 4079 | 1196 | 138 | 50 | 14.6 | 17.5 |
| Primary prevention | 5063 | 1838 | 62 | 34 | 5.3 | 8.1 |
| Secondary prevention | 3856 | 1230 | 174 | 59 | 18.8 | 19.0 |
| Diabetes | 2433 | 691 | 93 | 36 | 16.3 | 20.4 |
| No diabetes | 6486 | 2377 | 143 | 57 | 9.4 | 10.3 |
| Age over 75 years | 959 | 303 | 72 | 32 | 31.8 | 48.7 |
| Age below 75 years | 7960 | 2765 | 164 | 61 | 8.8 | 9.2 |
No difference in risk of major cardiovascular events was observed between the HDL-C increase group compared with the unchanged HDL-C group (HR, 1.05; 95 % CI, 0.82–1.34; p = 0.72).
Sensitivity Analyses
The separate outcome of cardiovascular death (HR, 1.61; 95 % CI, 0.94–2.75; p = 0.09) and all-cause death (HR, 1.30; 95 % CI, 0.92–1.85; p = 0.14) showed similar results. To assess the impact of the 3161 patients with an LDL-C reduction of <0.5 mmol/L, they were included in the analyses which showed a similar risk (HR, 1.56; 95 % CI, 1.25–1.95; p < 0.01).
Discussion
In this study, two-thirds of eligible patients initiating statin treatment had a change in their HDL-C level, and the degree of change was similar to that observed in randomised clinical trials [10]. A paradoxical decrease in HDL-C of >0.1 mmol/L was associated with a 56 % increase in major adverse cardiovascular events compared with unchanged HDL-C levels. The results were consistent across subgroups based on age, gender, presence of diabetes, primary and secondary prevention. No association between increased HDL-C levels and risk of major adverse cardiovascular events could be observed.
Results from a recent meta-analysis did not demonstrate an association between statin treatment, HDL-C change, and CVD risk [11]. Our patients had a relatively high untreated HDL-C level (1.48 mmol/L), in line with observations of untreated HDL-C levels in other Scandinavian studies, but in contrast with the recent publications [11, 21–23]. We observed a greater reduction in HDL-C (−0.27 mmol/L) compared with the meta-analysis (−0.13 mmol/L), and the relatively small HDL-C reduction in the meta-analysis might not have been sufficient to detect CVD risk associations. Furthermore, our findings are supported by a recent study which shows that a paradoxical decrease in plasma HDL-C levels after statin therapy is an important risk factor predicting long-term adverse cardiac events in patients with acute myocardial infarction [12].
Low single point measurements of HDL-C levels in patients receiving statin treatment have been reported to be associated with increased CVD risk, irrespective of the low LDL-C levels achieved [13]. We have shown that patients with a relatively high HDL-C (mean 1.48 mmol/L) newly initiated on cholesterol-modifying treatment (statin) and who experienced a consecutive HDL-C reduction have an increased cardiovascular risk, independently of baseline LDL-C and LDL-C change on statin treatment. Our findings are in line with previous observational data where a threshold for increased cardiovascular risk for HDL-C values below 1.3–4 mmol/L was observed [4]. Since the untreated HDL-C is relatively high in our material, this is the likely explanation for why we do not observe a reduced cardiovascular risk with increased HDL-C values. A major decrease in HDL-C level, independent of the size of the LDL-C reduction, might cause a shift in cholesterol transport. Indeed, the one-third of patients initiated on statin therapy who had a paradoxical reduction in HDL-C level [10] may have a suboptimal balance of cholesterol in/out transport to/from the inner arterial wall. Other important cardiovascular risk-lowering properties of HDL-C include antioxidant, anti-apoptotic, anti-inflammatory, antithrombotic, and anti-proteolytic properties, which account for the direct protective action on endothelial cells [24]. The decrease in HDL-C might consequently negatively impact these protective actions. However, we believe that reduction of HDL-C per se is associated with increased cardiovascular risk and not necessarily a statin-specific effect. Thus, we would highlight the importance of non-pharmacological efforts that will prevent HDL-C reductions, such as avoiding weight gain and/or maintaining physical activity levels.
The endpoint was a composite of hospitalisation with a primary diagnose of myocardial infarction, unstable angina pectoris, or ischaemic stroke, or cardiovascular death. An analysis of the separate endpoint components showed that risk of ischaemic stroke was statistically significant. The risks of coronary events and cardiovascular death were not significant, although the trends showed indication of similar directions/patterns. This finding might be somewhat surprising, as a predominant effect of statin treatment on coronary disease would be expected. However, as more patients in Sweden die outside hospital owing to coronary disease than owing to stroke, and a proportion of fatal coronary events occur in the out-of-hospital setting, stroke events were more likely to be a classified event in our study because more of these patients survived to hospitals [25, 26]. Similar results were observed when comparing outcome of separate analysis of cardiovascular death with all-cause death. Interestingly, the recent study which showed that a paradoxical decrease in plasma HDL-C levels after statin therapy initiation also had results driven by significantly higher incidence of stroke in the decreased HDL-C group [12].
Eighteen percent of patients initiated on statin treatment during the observation period were included in the study. The main reason for exclusion was lack of laboratory data, as only laboratory measurements from primary care were available. This favoured the inclusion of patients with regular healthcare controls (hypertension, diabetes, atrial fibrillation) in primary care. A considerable proportion of secondary prevention patients with initiation of statin treatment in hospital did not have a pre-treatment HDL-C measurement available to us and were therefore not included (Table S1).
The exclusion of a significant proportion of patients might call into question the generalisability of the results. However, we found consistent results in all subgroup analyses, with a numerically higher risk of reaching the composite endpoint with decreased HDL-C levels for all subgroups (older vs. younger patients, men vs. women, primary vs. secondary prevention patients, and presence of diabetes). However, among secondary preventive patients, a smaller numerical difference in cardiovascular risk between unchanged and decreased HDL-C groups was observed. Secondary prevention, for patients recently experiencing a myocardial infarction or a stroke, might potentially a have an initial increased thrombotic risk, which is more critical than the long-term effect caused by the atherosclerosis process. Altogether, this indicates that the study findings might be valid for a broad statin-treated population.
A further potential limitation regarding generalisability is the fact that the absolute majority of patients in Sweden are treated with relatively low doses of simvastatin. The frequent use of low-dose simvastatin might be the result of a stringent reimbursement regime, only allowing the use of high-potency statins in patients who do not reach treatment goals or in individuals who do not tolerate simvastatin. The effect on HDL-C change achieved by statins in general is reported to be independent of the reduction in LDL-C [10].
The present study is observational and unmeasured confounders may have influenced our results. Patients with malignancy or history of alcoholism were not included in the study. Changes in body weight, smoking pattern, or physical activity might influence levels of HDL-C, the latter two of which are not systematically recorded in primary care records. Since smoking previously was reported to be associated with generally low HDL-C levels, it is likely that smokers would be in the unchanged group or increase group due to the regression to the mean effect in our study [10, 27]. Furthermore, if the increase in HDL-C was due to cessation of smoking, a decrease in HDL-C should be found more frequently in smokers. In Sweden, not only is the overall smoking practice low (<15 %) but the likelihood of patients starting smoking during initiation of statin therapy can also be considered to be low. Furthermore, the effect of smoking cessation programmes in primary care is modest [28, 29]. The inverse correlation between physical activity and HDL-C change is low and can therefore be considered to be of minor importance [30]. We did not observe a marked percentage increase in body mass index in patients with a reduction in HDL-C, when compared with patients with unchanged HDL-C levels.
Low compliance to statin treatment could potentially be a possible explanation for our findings. However, patients were only included in the analyses while on statin treatment, and only if the reported LDL-C reduction was >0.5 mmol/L. The risk of the results being due to low compliance and/or statin response can therefore also be considered to be low.
The statin prescription pattern might be a source of confounding by indication. We found that patients with high cardiovascular risk in general had a lower untreated LDL-C, and vice versa. This correlation between LDL levels and CVD risk has been reported previously in a real-life clinical setting [31]. However, we found no correlation between LDL-C change and HDL-C change, as also supported by a previous report [10]. A prescription bias based on low HDL-C levels might also be a source of explanation for our findings. As low HDL-C is not a reason for initiation of statin treatment in Sweden, though, it is not likely that HDL-C should be affected by confounding by indication. Furthermore, we observed a mean difference of 1.1 mg of simvastatin between the decrease and unchanged groups after propensity score matching. We do not think this minimal difference in dosing had any impact on the results.
Laboratory data were only available from primary care records. Biological and analytical variation of HDL-C values may be a potential source of misclassification into the different HDL-C change groups. However, we observed similar associations with baseline cholesterol parts [HDL-C, plasma triglycerides (TG), and LDL-C] on HDL-C change pattern in our study compared to those reported in randomized clinical trials [10]. Thus, in our study, patients with high HDL-C had higher likelihood of HDL-C reduction and patients with low HDL-C and higher associated cardiovascular risk at baseline would more likely be identified for the HDL-C decrease group. In Sweden, HDL-C samples are generally analysed at regional central laboratories, all of which have participated in national quality and standardisation programmes since the end of the 1980s [32]. The analytical variation for HDL-C in the Swedish external quality assurance programme is between 3 % and 4 % (at the level of 1.68 mmol/L) [31], while the biological variation of HDL-C is approximately 7 %. Patients in our study had to have a decrease in HDL-C of >0.1 mmol/L, and the average HDL-C decrease was 0.27 mmol/L. Our conservative estimations of the HDL-C variation support the notion that the magnitude of the observed HDL-C decrease was sufficient.
The present study also has several important strengths. First, the composite endpoint has been validated previously in Swedish studies [19]. Second, only statin-naïve patients were included in order to increase the likelihood of analysing the actual treatment effect on HDL-C levels. The observed HDL-C change pattern is similar to that observed in randomised clinical trials [10]. Third, our analyses carefully matched the patients for numerous cardiovascular diagnoses, risk factors, including baseline LDL-C, and LDL-C change on treatment, thus increasing the likelihood of similar baseline risk. Finally, using Swedish national health registers the follow-up was performed with basically no loss of events.
Conclusions
A marked proportion of patients newly initiated on statin treatment experienced a decrease in HDL-C. This decrease was associated with a higher risk of major adverse cardiovascular events compared with patients in whom HDL-C levels were unchanged. Statin-induced increase in HDL-C was not associated with lower risk of major adverse cardiovascular events.
Electronic supplementary material
Acknowledgments
Editorial support was provided by Oxford PharmaGenesis Ltd, funded by AstraZeneca.
Contributors’ statements
P Hasvold, M. Thuresson, G. Johansson, and J. Bodegård participated equally in the study conception, design, and statistical analysis planning. M. Thuresson was responsible for the statistical analyses, P. Hasvold for the manuscript draft and finalization, and G. Johansson for handling of data and the study database. All authors had access to study data, and had authority over manuscript preparation, approval of the final version, and the decision to submit for publication.
Compliance with Ethical Standards
Role of the funding source
Project management was provided by AstraZeneca. Data collection was performed by Pygargus AB, Stockholm, Sweden, and was funded by AstraZeneca. The statistical analysis was agreed on by the study steering committee, and data analysis was performed by the study database owner in collaboration with AstraZeneca. As members of the study steering committee, AstraZeneca took part in the interpretation of the data and the drafting of the manuscript. Editorial support was provided by Oxford PharmaGenesis Ltd, funded by AstraZeneca.
Disclosures
Pål Hasvold is enrolled at the PhD School of the University of Oslo, Department of Medicine.
Pål Hasvold, Johan Bodegård, and Niklas Hammar are employed by AstraZeneca.
Marcus Thuresson is employed by an independent statistical consultant company, Statisticon AB, for which AstraZeneca is a client.
Gunnar Johansson has served on an advisory board arranged by AstraZeneca.
Johan Sundström serves on an advisory board for Itrim.
Sverre E. Kjeldsen has received honoraria for lecturing/consulting and other research support from AstraZeneca, Bayer, Hemo Sapiens, Medtronic, MSD, Novartis, Pronova, Serodus, and Takeda.
Ingar Holme has received honoraria for research consulting from AstraZeneca.
References
- 1.Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79:8–15. doi: 10.1161/01.CIR.79.1.8. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs DR, Jr, Mebane IL, Bangdiwala SI, Criqui MH, Tyroler HA. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32–47. doi: 10.1093/oxfordjournals.aje.a115483. [DOI] [PubMed] [Google Scholar]
- 3.Collaboration Emerging Risk Factors, Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chapman MJ, Ginsberg HN, Amarenco P, Andreotti F, Borén J, Catapano AL, et al. European Atherosclerosis Society Consensus Panel. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J. 2011;32:1345–1361. doi: 10.1093/eurheartj/ehr112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, European Association for Cardiovascular Prevention and Rehabilitation (EACPR) ESC Committee for Practice Guidelines. CPG European guidelines on cardiovascular disease prevention in clinical practice (version 2012) et al. The Fifth Joint Task Force of the European Society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2012;2012(33):1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 6.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 7.Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, et al. ILLUMINATE Investigators. Effects of torcertrapib in patients at high risk for coronary events. N Engl J Med. 2007;357:2109–2122. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. dal-OUTCOMES Investigators. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367:2089−99. [DOI] [PubMed]
- 9.Jones PH, Davidson MH, Stein EA, Bays HE, McKenney JM, Miller E, et al. STELLAR Study Group. Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR* Trial) Am J Cardiol. 2003;92:152–160. doi: 10.1016/S0002-9149(03)00530-7. [DOI] [PubMed] [Google Scholar]
- 10.Barter PJ, Brandrup-Wognsen G, Palmer MK, Nicholls SJ. Effect of statins on HDL-C: a complex process unrelated to changes in LDL-C: analysis of the VOYAGER database. J Lipid Res. 2010;51:1546–1553. doi: 10.1194/jlr.P002816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boekholdt SM, Arsenault BJ, Hovingh GK, Mora S, Pedersen TR, Larosa JC, et al. Levels and changes of HDL cholesterol and apolipoprotein A-I in relation to risk of cardiovascular events among statin-treated patients: a meta-analysis. Circulation. 2013;128:1504–1512. doi: 10.1161/CIRCULATIONAHA.113.002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ota T, Ishii H, Suzuki S, Tanaka A, Shibata Y, Tatami Y, Harata S, Shimbo Y, Takayama Y, Kawamura Y, Osugi N, Maeda K, Kondo T, Murohara T. Relation between paradoxical decrease in high-density lipoprotein cholesterol levels after statin therapy and adverse cardiovascular events in patients with acute myocardial infarction. Am J Cardiol. 2015;115:411–416. doi: 10.1016/j.amjcard.2014.11.043. [DOI] [PubMed] [Google Scholar]
- 13.Acharjee S, Boden WE, Hartigan PM, Teo KK, Maron DJ, Sedlis SP, et al. Low levels of high density lipoprotein cholesterol and increased risk of cardiovascular events in stable ischemic heart disease patients: a post hoc analysis from the COURAGE trial. J Am Coll Cardiol. 2013;62:1826–1833. doi: 10.1016/j.jacc.2013.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martinell M, Stalhammar J, Hallqvist J. Automated data extraction—a feasible way to construct patient registers of primary care utilization. Ups J Med Sci. 2012;117:52–56. doi: 10.3109/03009734.2011.653015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janson C, Larsson K, Lisspers KH, Ställberg B, Stratelis G, Goike H, et al. Pneumonia and pneumonia related mortality in patients with COPD treated with fixed combinations of inhaled corticosteroid and long acting β2 agonist: observational matched cohort study (PATHOS) BMJ. 2013;346:f3306. doi: 10.1136/bmj.f3306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eklind-Cervenka M, Benson L, Dahlstrom U, Edner M, Rosenqvist M, Lund LH. Association of candesartan vs losartan with all-cause mortality in patients with heart failure. JAMA. 2011;305:175–182. doi: 10.1001/jama.2010.1949. [DOI] [PubMed] [Google Scholar]
- 18.Varenhorst C, Jensevik K, Jernberg T, Sundström A, Hasvold P, Held C, et al. Duration of dual antiplatelet treatment with clopidogrel and aspirin in patients with acute coronary syndrome. Eur Heart J. 2014;35:969–978. doi: 10.1093/eurheartj/eht438. [DOI] [PubMed] [Google Scholar]
- 19.Brookhart MA, Wyss R, Layton JB, Stürmer T. Propensity score methods for confounding control in non experimental research. Circ Cardiovasc Qual Outcomes. 2013;6:604–611. doi: 10.1161/CIRCOUTCOMES.113.000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sekhon JS. Multivariate and propensity score matching software with automated balance optimization. J Stat Softw. 2011;42:1–52. doi: 10.18637/jss.v042.i07. [DOI] [Google Scholar]
- 21.Van Hemelrijck M, Harari D, Garmo H, Hammar N, Walldius G, Lambe M, et al. Biomarker-based score to predict mortality in persons aged 50 years and older: a new approach in the Swedish AMORIS study. Int J Mol Epidemiol Genet. 2012;3:66–76. [PMC free article] [PubMed] [Google Scholar]
- 22.Langsted A, Nordestgaard BG. Nonfasting lipids, lipoproteins, and apolipoproteins in individuals with and without diabetes: 58,434 individuals from the Copenhagen General Population Study. Clin Chem. 2011;3:482–489. doi: 10.1373/clinchem.2010.157164. [DOI] [PubMed] [Google Scholar]
- 23.Hambraeus K, Lindhagen L, Tydén P, Lindahl B, Lagerqvist B. Target-attainment rates of low-density lipoprotein cholesterol using lipid-lowering drugs one year after acute myocardial infarction in Sweden. Am J Cardiol. 2014;113:17–22. doi: 10.1016/j.amjcard.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Tran-Dinh A, Diallo D, Delbosc S, Varela-Perez LM, Dang QB, Lapergue B, et al. HDL and endothelial protection. Br J Pharmacol. 2013;169:493–511. doi: 10.1111/bph.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilhelmsen L, Köster M, Harmsen P, Lappas G. Differences between coronary disease and stroke in incidence, case fatality, and risk factors, but few differences in risk factors for fatal and non-fatal events. Eur Heart J. 2005;26:1916–1922. doi: 10.1093/eurheartj/ehi412. [DOI] [PubMed] [Google Scholar]
- 26.Dudas K, Lappas G, Stewart S, Rosengren A. Trends in out-of-hospital deaths due to coronary heart disease in Sweden (1991 to 2006) Circulation. 2011;123:46–52. doi: 10.1161/CIRCULATIONAHA.110.964999. [DOI] [PubMed] [Google Scholar]
- 27.Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: an analysis of published data. BMJ. 1989;298:784–788. doi: 10.1136/bmj.298.6676.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.OECD. OECD Factbook 2011−2012: Economic, Environmental and Social Statistics. Adult population smoking daily. Available at: http://www.oecd-ilibrary.org/sites/factbook-2011-en/12/02/01/12-02-01g1.html?contentType=/ns/StatisticalPublication,/ns/Chapter&itemId=/content/chapter/factbook-2011-107en&containerItemId=/content/serial/18147364&accessItemIds=&mimeType=text/html&_csp_=db2b28696cd26bcfce3036cbd611c6ac. Accessed 14 Oct 2014.
- 29.Persson LG, Hjalmarson A. Smoking cessation in patients with diabetes mellitus: results from a controlled study of an intervention programme in primary healthcare in Sweden. Scand J Prim Health Care. 2006;24:75–80. doi: 10.1080/02813430500439395. [DOI] [PubMed] [Google Scholar]
- 30.Skretteberg PT, Grundvold I, Kjeldsen SE, Erikssen JE, Sandvik L, Liestøl K, et al. HDL-cholesterol and prediction of coronary heart disease: modified by physical fitness? A 28-year follow-up of apparently healthy men. Atherosclerosis. 2012;220:250–256. doi: 10.1016/j.atherosclerosis.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 31.Heintjes EM, Penning-van Beest FJ, Johansson S, Stalenhoef AF, Herings RM. Comparison of incidences of cardiovascular events among new users of different statins: a retrospective observational cohort study. Curr Med Res Opin. 2009;25:2621–2629. doi: 10.1185/03007990903269112. [DOI] [PubMed] [Google Scholar]
- 32.http://www.equalis.se/media/41723/u040_kvalitetsmål_equalis_1.2.pdf. Accessed 21 May 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.