Abstract
Objective
To examine longitudinal changes in perceptions of barriers to healthy eating and its impact on dietary intake and weight loss in a 24-month trial.
Methods
A secondary analysis was conducted using data from a behavioral weight loss trial (N=210). The Barriers to Healthy Eating (BHE) Scale was used to measure perceived barriers to healthy eating. Weight, total energy and fat intake were measured. Longitudinal mixed regression modeling was used for data analysis.
Results
The BHE total score decreased from baseline to 6 months, and slightly increased from 6 to 24 months (P < .001). The changes in the BHE total and subscale scores were positively associated with the changes in total energy and fat intake (P < .05) as well as weight (P < .01).
Conclusions and Implications
Reducing barriers could lead to improved short-term dietary changes and weight loss. Innovative strategies need to be developed to prevent barriers from increasing when intervention intensity begins to decrease.
Keywords: eating barriers, weight loss, dietary intake, behavioral intervention, behavior change, health belief
Introduction
Prevalence of overweight and obesity remains high at approximately 66% among U.S. adults.1 Even though behavioral intervention studies focusing on healthy eating and physical activity have demonstrated that individuals can achieve an average weight loss of 10.4 kg at 6 months and maintain a weight loss of 8.1 kg at 18 months,2 a re-evaluation of current efforts to tackle obesity is essential to improve the long-term effect of such behavioral intervention approach.3 Perceived barriers is one of the most studied concepts and important predictors of behavior change.4 However, most of the studies in obesity and/or healthy eating have used qualitative inquiry or cross sectional designs to examine perceived barriers to healthy eating,5-9 which limits the ability to evaluate how individuals’ perceptions of barriers to healthy eating change over the course of a behavioral intervention.
Several researchers have studied perceptions of barriers to healthy eating and identified multiple barriers. A qualitative study revealed four key factors that can lead to adolescents’ perception of barriers to healthy eating: physical and psychological reinforcement of eating behaviors, perceptions of food and eating behaviors, perceptions of contradictory food-related social pressures, and perceptions of the concept of healthy eating itself.9 A cross sectional study of African American adults (mean age: 50 years) found that participants reported that the high price of healthy foods was the biggest barrier to healthy eating, other barriers included healthy food being less palatable, not being able to find and/or cook healthy foods, and absence of social support for having healthy foods available.5
Very few studies have reported the changes in barriers to healthy eating over time along with the association with dietary intake and weight change. Turk et al. found that increases in barriers to healthy eating predicted weight gain among black and white adults.10 Another behavioral weight loss clinical trial reported declines in perceived barriers to healthy eating, e.g. reduced perception of lack of control and lack of time were significantly associated with greater weight loss over 12 months in an adult sample that was predominantly White.11 However, neither of these two studies examined the trend of how individuals’ perceptions of barriers to healthy eating change over the duration of a 24-month behavioral intervention, and how such changes in individuals’ perceived barriers to healthy eating contribute to changes in weight and individuals’ dietary habits. Filling this gap of knowledge will help researchers examine long-term effectiveness of counseling strategies to overcome barriers to healthy eating in a behavioral intervention for overweight and obesity, thus, this study aimed to examine changes in perceptions of barriers to healthy eating and its associations with changes in dietary intake and weight loss over 24 months in a behavioral weight loss trial.
Methods
The design of this study is a secondary analysis using data from a behavioral weight loss trial – the Self-Monitoring and Recording using Technology (SMART) Trial.12 The SMART trial was a 24-month, 3-group randomized clinical trial that tested the efficacy of a behavioral weight loss intervention with three different approaches to self-monitoring of diet and physical activity: 1) using a paper diary, or 2) using a personal digital assistant (PDA) or 3) using a PDA and receiving a daily tailored feedback message delivered via the PDA at random times. Regardless of treatment assignment, all study participants received a standard group-based behavioral weight loss intervention based on social cognitive theory.12
Group meetings were held in the evening and lasted approximately 45 to 90 minutes. They were held weekly for the first 4 months, biweekly for months 5-12, and monthly for months 13-18; one maintenance session was held at 21 months, totaling 39 group sessions. Participants were prescribed a calorie goal between 1200 and 1800 depending on their gender and baseline weight and were asked to limit their fat intake to 25% of their daily calories. They also received exercise goals given as weekly minutes which increased throughout the study, e.g., to achieve 150 minutes of physical activity by the third month and 180 minutes by the sixth month. All participants were instructed to self-monitor their daily energy and fat intake and physical activity using a paper diary or PDA as described above.12 Barriers related to healthy eating were addressed in the context of the group counseling sessions.
Participants were eligible if they were 21-59 years old and had a body mass index (BMI) between 27 and 43 kg/m2. Individuals who had a major medical condition requiring dietary and exercise supervision or a psychiatric condition that might interfere with their completing the study, participated in a weight loss program in the previous 6 months, or planned a pregnancy in the next 24 months were excluded.12 A total of 704 individuals were screened over the phone, 210 eligible participants were randomized. The sample size of 210 was chosen to have at least 0.80 power for two-sided hypothesis testing at a significance level of 0.05. Retention was 84.7% with no differential attrition at 24 months.
Socio-demographic data including age, gender, race (white/black), education, marital status (currently married, never married, widowed), employment status (full time, not full time), and income levels were collected using the Socio-demographic and Lifestyle Questionnaire, which is a self-administered, standardized questionnaire. The questionnaire was developed by the research staff at the University of Pittsburgh School of Nursing Center for Research in Chronic Disorders and has been used extensively for over 15 years in an array of populations. Participants’ perceived barriers to healthy eating were measured by the Barriers to Healthy Eating (BHE) Scale, which was the first scale designed to systematically measure perceptions of various barriers to healthy eating among individuals undergoing weight loss treatment. The BHE is a 22-item questionnaire asking individuals to rate various feelings or situations related to following the calorie- and fat-restricted diet, e.g., feelings of deprivation or cost of the recommended eating plan. It has 3 subscales: Emotions (11 items), Daily Mechanics of Following a Healthy Eating Plan (8 items), and Social Support (3 items). The potential range for the BHE total score is from 22 to110, and the potential range for each of the subscales is as follows: Emotions subscale 11-55, the Daily Mechanics subscale 8-40, and the Social Support subscale 3-15. A higher score indicates higher perceived barriers. It has good internal consistency reliability with a Cronbach's alpha of 0.7 in this study and predictive validity with weight loss at 6 months (r=0.28) in a previous study.13
Total energy intake and total fat intake was assessed using data extracted from two unannounced 24-hour dietary recalls guided by the Five-Step Automated Multiple-Pass Method14,15 and the Nutrition Data System for Research software program.16 One recall was conducted for a weekday and another for a weekend day. The average of the total energy and total fat intake from the two recalls was used to summarize participants’ daily dietary intake. Weight was measured by research staff using a digital scale (Tanita Corporation of America, Inc., Arlington Heights, IL, USA) following an overnight fast and participants wearing light clothing and no shoes. All measures were completed every 6 months (baseline, 6, 12, 18, and 24 months). The study was approved by the University of Pittsburgh Institutional Review Board.
Statistical analyses were conducted using SAS version 9.2 (SAS institute, Cary, NC). Significance was set at 0.05 for two-sided hypothesis testing. Summary statistics were reported as mean (SD) or frequency count (%) as appropriate. Linear mixed modeling was used to examine the main effects of treatment groups and time (baseline, 6, 12, 18, and 24 months) on the weight, dietary intake, BHE total score and subscale sores. Because there was no significant treatment group effect on the weight, dietary intake, BHE total score and subscale sores (P >0.05 for all variables), we merged the data from the three groups and used the full sample to examine the associations between BHE scores and weight as well as dietary intake. Missing data were handled by the linear mixed model assuming data missing at random.
Results
The majority of participants were White (78.1%) and female (84.8%); they had a mean (±SD) age of 46.8±9.0 years and BMI of 34.0 ± 4.5. Demographic characteristics of the sample are described in Table 1 and the descriptive data of BHE total score, three BHE subscale scores, weight, and total energy and fat intake are reported in Table 2. Time effect on participants’ overall perceptions of barriers to healthy eating through the BHE total score were examined and presented in Table 2. The BHE total score decreased from baseline to 6 months and increased slightly from 6 to 24 months (P < .001); a similar profile was observed in both barriers related to Emotions (P < .001) and Daily Mechanics of following a healthy eating plan (P < .001). There was no significant time effect on Social Support (P = .064); except for the BHE Social Support subscale score, all values at 24 months were below the baseline values.
Table 1.
Demographic Characteristics of the Sample (N=210)
| Characteristics | M±SD or % (n) |
|---|---|
| Age (years) | 46.8 ± 9.0 |
| Education (years) | 15.6 ± 3.0 |
| BMI (kg/m2) | 34.0 ± 4.5 |
| Gender | |
| Female | 84.8 (178) |
| Male | 15.2 (32) |
| Ethnicity | |
| White | 78.1 (164) |
| Non white | 21.9 (46) |
| Marital status | |
| Currently married | 68.6 (144) |
| Never married | 13.8 (29) |
| Formerly married (divorced or separated) | 17.6 (37) |
| Employment status | |
| Employed full time | 82.9 (174) |
| Employed not full time | 17.1 (36) |
| Gross household income | |
| >$50,000 | 60 (123) |
| $30,000-$50,000 | 23.9 (49) |
| ≤$30,000 | 16.1 (33) |
BMI= Body Mass Index; M±SD= Mean±Standard Deviation
Table 2.
Description of Study Variables Over Time (N=210)
| Outcomes | Baseline | 6 month | 12 month | 18 month | 24 month | P values |
|---|---|---|---|---|---|---|
| Weight (kg) | 93.8±15.2 | 87.9±15.8 | 87.5±16.9 | 89.5±17.1 | 90.6±17.0 | <.001 |
| Energy intake (calories) | 2089.8±682.3 | 1592.5±506.0 | 1646.3±522.1 | 1641.8±505.4 | 1641.7±507.5 | <.001 |
| Fat intake (grams) | 82.1±36.8 | 53.8±25.0 | 58.9±28.6 | 59.2±28.8 | 59.3±26.3 | <.001 |
| BHE total | 61.3±14.0 | 54.0±13.3 | 54.9±14.5 | 56.3±14.7 | 55.8±14.4 | <.001 |
| Emotions | 34.5±8.1 | 30.9±8.6 | 31.3±9.0 | 32.3±9.0 | 32.0±8.5 | <.001 |
| Daily mechanics | 20.4±6.3 | 16.9±5.1 | 17.1±5.2 | 17.5±5.6 | 17.2±5.5 | <.001 |
| Social support | 6.4±2.5 | 6.1±2.2 | 6.4±2.7 | 6.5±2.7 | 6.5±2.7 | .064 |
BHE total indicates Barriers to Healthy Eating Scale total score.
Note: No group difference was found for all of the study variables, P> .05; The score ranges: BHE total (22-110), Emotions subscale (11-55), Daily Mechanics subscale (8-40), Social Support subscale (3-15).
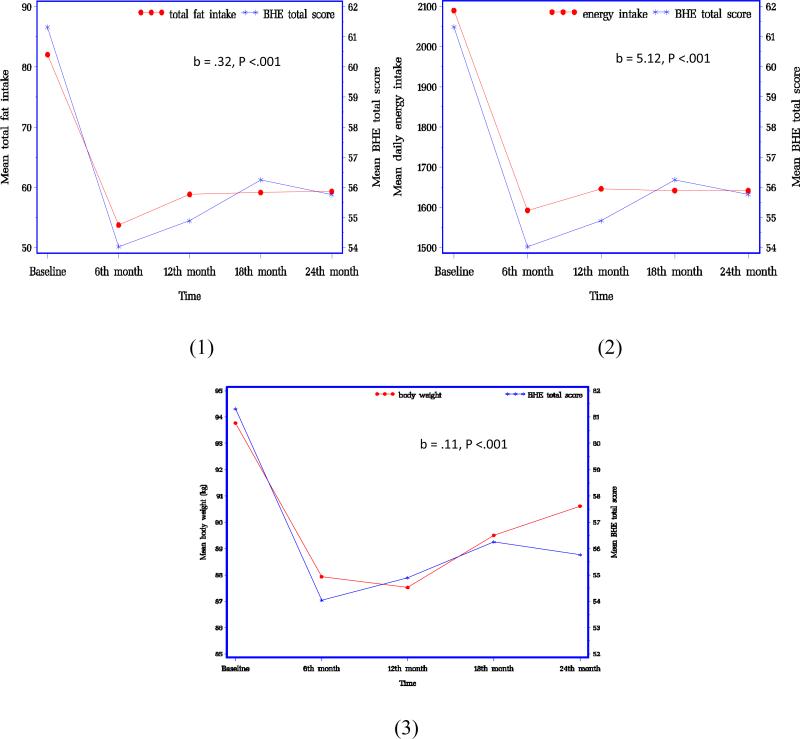
The associations between BHE total score and subscale scores and dietary intake and weight from baseline to 24 months were examined. The BHE total score (b= 5.12, P < .001; b= .32, P < .001), and the three sub-scale scores —Emotions (b= 8.01, P < .001; b=0.47, P < .001), Daily Mechanics (b= 9.63, P = .01; b= .68, P < .001), and Social Support (b= 16.66, P = .033; b= 1.01, P = .016) — were positively associated with both the total energy and fat intake changes, respectively. The BHE total score (b= .11, P < .001), as well as the scores on the Emotions subscale (b= .19, P < .001), the Daily Mechanics subscale (b= .19, P < .001), and Social Support subscale (b= .16, P = .01) were significantly associated with weight over the 24 months.
Discussion
The longitudinal changes in participants’ perceptions of barriers to healthy eating and its impact on changes in weight and dietary intake were examined. Significant improvements were found in perceptions of eating barriers during the course of a 24-month behavioral weight loss intervention. Participants’ perceptions of barriers to healthy eating decreased from baseline to 6 months and increased slightly from 6 to 24 months; their total energy intake, fat intake, and weight revealed similar patterns of initial decline and then slight increase from 6 to 24 months.
The greatest reductions in weight, perceived barriers to healthy eating, and energy and fat intake occurred from baseline to 6 months, with slight increases from 6 to 24 months. This slight increases may be partially explained by these changes being concurrent with the change in intervention intensity. For example, the intensive intervention phase ended and sessions decreased in frequency from weekly to biweekly to monthly and subsequently only one contact in the last 6 months. Previous studies showed that regression of behavior change occurred as the frequency of contact declines.10
The decreases in individuals’ perceptions of barriers to healthy eating were concurrent with reductions in their energy and fat intake, as well as weight loss over 24 months of the study; however, while the BHE scores began a slight upturn at 6 months, the increase in fat and energy intake revealed a lag with weight regain not occuring until after 12 months. In a weight maintenance study, Turk et al. found that increases in barriers to healthy eating predicted weight gain at 18 months after an intensive behavioral treatment.10 Welsh et al. reported declines in perceived barriers to healthy eating over a 12-month behavioral weight loss study, and such declines were significantly associated with greater weight loss at 12 months.11 This study is the only study reporting the association of perceptions of barriers to healthy eating and individuals’ dietary changes and weight loss over a 24-month behavioral intervention demonstrating the immediate impact of perceptions of barriers to healthy eating on changes in dietary intake and weight loss within 12 months. The impact became weaker when the intervention sessions were less frequent in the later phase of the intervention.
There are some limitations to the study. First, the sample was predominantly white and female and participants were generally well educated. Thus, study findings may not be applicable to adults with lower levels of attained education, lower socioeconomic status, or ethnic minorities. Second, barriers captured in the BHE scale may not have covered all of the barriers to healthy eating perceived by this study's sample of overweight or obese individuals, however, the barriers mentioned in the existing literature6-8 were covered in the BHE scale used in this study. These limitations emphasize the need to assess barriers to healthy eating in more diverse populations and determine if the findings are similar.
Implications for Research and Practice
Numerous studies have demonstrated the phenomena of declining adherence to healthy lifestyle habits as the support of an intervention is reduced or withdrawn.17,18 Innovative strategies that are adaptive and tailored to the individuals’ need to be developed to prevent the regression in adherence to a healthy diet, which may result from the perception that the barriers to eating a healthy diet are increasing when intervention intensity and support declines. Using ongoing contact for supportive messages or boosters, which current technology facilitates, can be one example of an approach that can provide ongoing support. Also, future studies need to examine the longitudinal changes in barriers to healthy eating in association with changes in diet and weight in samples that are more diverse in racial, gender, and age composition. The science could benefit from the use of advanced methods such as mediation analysis and factorial intervention designs to examine the efficacy of each component of behavioral interventions and thus adapt the intervention to improve outcomes related to perceived barriers to a sustained healthy eating plan.
Figure.
Association between Barriers to Healthy Eating, Fat and Energy Intake, and Body Weight over Time
Note: BHE total score indicates Barriers to Healthy Eating Scale total score
Acknowledgement
The parent study was supported by NIH/NIDDK # R01 DK071817. The conduct of the parent study was also supported by the Data Management Core of the Center for Research in Chronic Disorders NIH-NINR #P30-NR03924, the General Clinical Research Center, NIH-NCRR-GCRC #5M01-RR000056 and the Clinical Translational Research Center, NIH/NCRR/CTSA Grant UL1 RR024153 at the University of Pittsburgh. This work was also supported by NIH/NINR K24-NR010742 for LE Burke and Robert Wood Johnson Foundation Nurse Faculty Scholars Program for J Wang.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jing Wang, University of Texas Health Science Center at Houston School of Nursing, 6901 Bertner Avenue, SON 614, Houston, TX 77030. Phone: 713-500-9022. Fax: 713-500-2142. jing.wang@uth.tmc.edu.
Lei Ye, University of Pittsburgh Center for Aging and Population Health, 130 N. Bellefield Ave. Room 520, Pittsburgh, PA 15213. Phone: 412-383-1024, Fax: 412-383-1308. ley9@pitt.edu.
Yaguang Zheng, Graduate Student Researcher, University of Pittsburgh School of Nursing, 415 Victoria Building, 3500 Victoria St, Pittsburgh, PA 15261. Phone: 412-624-2305. Fax: 412-383-7293. yaz40@pitt.edu.
Lora E. Burke, University of Pittsburgh School of Nursing, 415 Victoria Building, 3500 Victoria St, Pittsburgh, PA 15261..
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014 Feb 26;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bourchard C, James WPT, editors. Handbook of obesity: Clinical applications. 2nd ed. Marcel Dekker; New York: 2004. pp. 147–167. [Google Scholar]
- 3.Burke LE, Wang J. Treatment strategies for overweight and obesity. J Nurs Scholarsh. 2011 Dec;43(4):368–375. doi: 10.1111/j.1547-5069.2011.01424.x. [DOI] [PubMed] [Google Scholar]
- 4.Rosenstock IM. Historical origins of the health belief model. Health Educ Q. 1974;2:328–335. [Google Scholar]
- 5.Pawlak R, Colby S. Nutr Res Pract. 1. Vol. 3. Spring; 2009. Benefits, barriers, self-efficacy and knowledge regarding healthy foods; perception of African Americans living in eastern North Carolina. pp. 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baruth M, Sharpe PA, Parra-Medina D, Wilcox S. Perceived barriers to exercise and healthy eating among women from disadvantaged neighborhoods: results from a focus groups assessment. Women Health. 2014 Mar 11;54(4):336–353. doi: 10.1080/03630242.2014.896443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fukuoka Y, Lindgren TG, Bonnet K, Kamitani E. Perception and Sense of Control Over Eating Behaviors Among a Diverse Sample of Adults at Risk for Type 2 Diabetes. Diabetes Educ. 2014 Feb 13;40(3):308–318. doi: 10.1177/0145721714522717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Musaiger AO, Al-Mannai M, Tayyem R, et al. Perceived barriers to healthy eating and physical activity among adolescents in seven Arab countries: a cross-cultural study. ScientificWorldJournal. 2013:232164. doi: 10.1155/2013/232164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stevenson C, Doherty G, Barnett J, Muldoon OT, Trew K. Adolescents' views of food and eating: identifying barriers to healthy eating. J Adolesc. 2007 Jun;30(3):417–434. doi: 10.1016/j.adolescence.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Turk MW, Sereika SM, Yang K, Ewing LJ, Hravnak M, Burke LE. Psychosocial correlates of weight maintenance among black & white adults. Am J Health Behav. 2012 Mar;36(3):395–407. doi: 10.5993/AJHB.36.3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Welsh EM, Jeffery RW, Levy RL, et al. Measuring perceived barriers to healthful eating in obese, treatment-seeking adults. J Nutr Educ Behav. 2012 Nov-Dec;44(6):507–512. doi: 10.1016/j.jneb.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burke LE, Styn MA, Glanz K, et al. SMART trial: A randomized clinical trial of self-monitoring in behavioral weight management-design and baseline findings. Contemp Clin Trials. 2009 Nov;30(6):540–551. doi: 10.1016/j.cct.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burke LE, Kim Y, Music E. The barriers to healthy eating scale: Psychometric report. Ann Behav Med. 2004;27(Supp):S101. [Google Scholar]
- 14.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr. 2006 Oct;136(10):2594–2599. doi: 10.1093/jn/136.10.2594. [DOI] [PubMed] [Google Scholar]
- 15.Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003 May;77(5):1171–1178. doi: 10.1093/ajcn/77.5.1171. [DOI] [PubMed] [Google Scholar]
- 16.Buzzard I, Schakel S, Ditter-Johnson J. Quality and Accessibility of Food-Related Data. AOAC International; Arlington, VA: 1995. Quality control in the use of food and nutrient databases for epidemiologic studies. pp. 241–252. [Google Scholar]
- 17.Acharya SD, Elci OU, Sereika SM, et al. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer Adherence. 2009;3:151–160. doi: 10.2147/ppa.s5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang J, Sereika SM, Chasens ER, Ewing LE, Matthews JT, Burke LE. Effect of Adherence to Self-Monitoring of Diet and Physical Activity on Weight Loss in a Technology-Supported Behavioral Intervention. Patient Prefer Adherence. 2012;6:221–226. doi: 10.2147/PPA.S28889. [DOI] [PMC free article] [PubMed] [Google Scholar]