Abstract
Introduction
Alcohol use disorder symptoms frequently occur in adolescents and younger adults who seldom acknowledge a need for help. We identified sociodemographic, clinical, and familial predictors of alcohol problem recognition and help seeking in an offspring of twins sample.
Method
We analyzed longitudinal data from the Children of Alcoholics and Twins as Parents studies, which are combinable longitudinal data sources due to their equivalent design. We analyzed respondents (n=1,073, 56.0% of the total sample) with alcohol use disorder symptoms at the baseline interview. Familial characteristics included perceptions of alcohol problems and help seeking for alcohol problems within the immediate family and a categorical variable indicating genetic and environmental risk. We used logistic regression to examine predictors of alcohol problem recognition and help seeking.
Results
Approximately 25.9% recognized their alcohol problems and 26.7% sought help for drinking. In covariate-adjusted analyses, help seeking among family members predicted problem recognition, several clinical characteristics predicted both problem recognition and help seeking, and familial risk predicted help seeking. Alcohol problem recognition mediated the association between alcohol use disorder symptoms and incident help seeking.
Conclusions
Facilitating the self-recognition of alcohol use disorder symptoms, and perhaps the awareness of family members’ help seeking for alcohol problems, may be potentially promising methods to facilitate help seeking.
Keywords: Alcohol use disorders, help seeking, treatment utilization, alcohol problem recognition, adolescents, young adults
1. INTRODUCTION
Among people who experience alcohol problems, alcohol use disorder (AUD) symptoms usually first appear in young adulthood (Bucholz et al., 1992; Schuckit et al., 1995). Despite evidence that obtaining alcohol-related services increases one’s likelihood of recovering from alcohol problems (Dawson et al., 2006; Finney et al., 2007), individuals often delay seeking help until they have experienced a decade of psychological, medical, and/or social harms owing to their drinking (Bucholz et al., 1992; Schuckit et al., 1995). This lack of help seeking has been attributed to the fact that 86–91% of those with AUD in a given year do not think that they need help (Edlund et al., 2009, 2006; Mojtabai et al., 2002). In 2013, only 3% of adolescents or adults with untreated substance use disorders believed that they needed help for their substance use (Substance Abuse and Mental Health Services Administration, 2014).
Studies of adults have explored factors that facilitate or interfere with alcohol problem recognition, beliefs about needing help, and help seeking (Edlund et al., 2009, 2006; Glass et al., 2010; Small et al., 2012). Compared to their middle-aged and older counterparts, young adults with AUD have a particularly elevated risk for denying need for help (Edlund et al., 2009; Oleski et al., 2010). Adults with mental health comorbidities such as mood or anxiety disorder symptoms were more likely to recognize their alcohol problems or to believe that they needed treatment than those without such comorbidity (Edlund et al., 2009, 2006; Grella et al., 2009; Oleski et al., 2010; Small et al., 2012). Having a greater number of AUD symptoms was positively associated with perceived need or with help seeking, but having co-morbid drug use disorders was not. While the comorbidity between alcohol and nicotine disorders is very high (Dawson et al., 2011), we are unaware of studies that have examined the association between nicotine problems and help seeking.
One potentially promising line of investigation is to examine the association between specific AUD symptoms and help seeking (Edlund et al., 2009). The conceptual and empirical literature suggests that recognizing one’s own addiction problems may be a first step in deciding what to do about them (Oser et al., 2010; Redko et al., 2007; Saunders et al., 2006; Sexton et al., 2008). Prevention programs (van Gemert et al., 2011), brief alcohol interventions (Dimeff, 1999), and motivational enhancement therapies (Miller, 1995) educate people about AUD symptoms, such as pharmacologic tolerance, as an effort to elucidate their patterns of problematic use. Knowledge about specific AUD symptoms that heighten concern in younger persons could inform these programs, yet attention has not been directed at the role of specific AUD symptoms in promoting problem recognition, which in turn likely promotes help seeking. Mediation analysis may be better suited to understand such relationships.
Twin studies and prospective cohort studies have found that latent familial factors and family history of alcohol dependence, respectively, are associated with healthcare utilization (Milne et al., 2009; True et al., 1997, 1996). In a study of twin adult male veterans, genetic and shared environmental influences explained 41% and 40% of the variance in help seeking for alcohol problems (True et al., 1996). To our knowledge, research on measurable familial factors, such as family history of alcohol problems, family member’s treatment seeking, or perceived alcohol problems within the family have not been adequately explored in the literature on help seeking. One study of adults in the U.S. general population with past-year substance dependence found no association between self-reported family history of substance use problems and help seeking (Grella et al., 2009), but other studies on help seeking have not considered family history (Cohen et al., 2007; Dawson et al., 2012; Edlund et al., 2012; Glass et al., 2010; Ilgen et al., 2011; Oleski et al., 2010). Familial characteristics may be particularly germane to studying adolescents and young adults because of the recency in which they have experienced their family environment.
In the current study, we examined sociodemographic, clinical, and familial predictors of lifetime alcohol problem recognition and help seeking in a sample of adolescents and young adults at varying levels of genetic and environmental risk. Many younger individuals who experience AUD symptoms would be eligible for intervention and prevention programs due to their high risk of developing full criteria for an AUD. An offspring of twins design allowed us to assess the contributions of genetic and environmental risk to problem recognition and help seeking. A longitudinal design allowed estimation of the extent that alcohol problem recognition mediated the association between AUD symptoms and incident help seeking over a four-year follow-up period.
2. METHOD
2.1 Sample
We analyzed data from two longitudinal studies consisting of children born to twin fathers with or without substance use disorder: the Twins as Parents (TAP) and Children of Alcoholics (COA) studies (combined n = 1,919; mean age 21.4 years at the baseline interview) (Duncan et al., 2006; Jacob et al., 2003; Scherrer et al., 2008; Xian et al., 2010). TAP and COA were designed to analyze the degree to which offspring outcomes (substance-related and others) are influenced by genetic and environmental effects, and their interaction. In 2001–2002, children of twin fathers from the Vietnam Era Twin Registry who had been well characterized by a psychiatric assessment in 1992 (Eisen et al., 1989; Tsuang et al., 1996) were recruited for two studies. Eligibility for each study was based on the father’s history and his co-twin’s history of alcohol (for COA) and drug dependence (for TAP). Zygosity status of the twins was used to construct four familial vulnerability groups representing combinations of genetic and environmental risks (see Table 1). Briefly, one risk group was composed of offspring of men with either alcohol or drug dependence. These offspring were at both high genetic and high environmental risk (“HG-HE”) for developing substance dependence, by virtue of having an affected biological father (genetic risk) and being reared by an affected father (environmental risk). Offspring whose unaffected father was an identical co-twin of an affected individual were also at high genetic risk for substance dependence, because their father shared all his genes with his affected co-twin, but at low environmental risk because they were not reared by an affected father (“HG-LE”). Offspring of an unaffected father with an affected dizygotic twin were at moderate genetic risk for developing substance dependence (since their father shared half his genetic make-up on average with his affected brother), but at low environmental risk because they were not brought up in a household with an affected father (“MG-LE”). Finally, offspring of unaffected fathers whose co-twins were also unaffected had low risks for both genetic and environmental influences on development of substance dependence (“LG-LE”).
Table 1.
Familial risk ascertained from the offspring of twins design
| Offspring risk group | Zygosity of offspring’s father and father’s co- twin | Substance dependence status of father | Substance dependence status of father’s co-twin |
|---|---|---|---|
| High genetic/high environmental (HG/HE) | Monozygotic1 or dizygotic2 | + | + or − |
| High genetic/low environmental (HG/LE) | Monozygotic | − | + |
| Moderate genetic/low environmental (MG/LE) | Dizygotic | − | + |
| Low genetic/low environmental (LG/LE) – control group | Monozygotic or dizygotic | − | − |
Identical, with the father and his co-twin sharing all of their genes, and
fraternal, sharing half of their genes.
Multiple offspring were interviewed for each father when available. TAP and COA had similar recruitment and interview procedures, allowing datasets to be combined. Offspring and maternal interviews used a modified telephone adaptation of the Semi-Structured Assessment for the Genetics of Alcoholism, Version II to assess DSM-IV diagnoses (Bucholz et al., 1994).
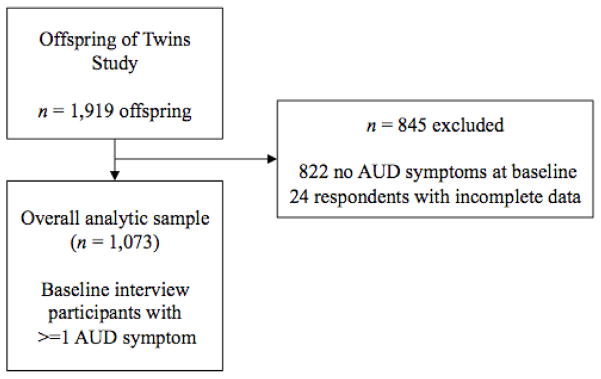
Included in analyses for this study were 1,073 offspring with >=1 DSM-IV AUD symptoms at baseline (see Figure 1) from 782 families. We excluded 845 with no baseline AUD symptoms and 24 with incomplete data. Respondents were re-interviewed twice at 2-year intervals. Response rates at the second and third time points were 73.6% and 64.4%, respectively. Parent interviews were used to define maternal AUD and help seeking for alcohol problems among fathers and mothers. All biological fathers and 87.2% of biological mothers of offspring were interviewed.
Figure 1.
Defining the overall analytic sample
Note: AUD=alcohol use disorder
2.2 Measures
2.2.1 Alcohol problem recognition
At each time point, alcohol problem recognition was assessed with the question, “Have you ever thought you had a drinking problem?”
2.2.2 Sought help for drinking
At each time point, treatment from medical professionals, other clinical professionals, or religious leaders was assessed with the question, “have you ever discussed your drinking with a psychiatrist, other doctor, psychologist, counselor, social worker, priest, rabbi, religious leader or other professional?” Inpatient and residential treatment was assessed with the question, “Have you ever been treated for drinking in a hospital or residential program where you stayed overnight?” Alcoholics Anonymous was assessed by asking, “because of your drinking, have you ever attended an Alcoholics Anonymous meeting?” These were combined to reflect help seeking.
2.2.3 AUD symptoms
Dichotomous variables were created from baseline reports of lifetime criteria for each of the 11 symptoms of DSM-IV AUD (abuse or dependence). We also created a lifetime DSM-IV symptom count (range 1–11).
2.2.4 Years since first AUD symptom
We calculated the number of years that respondents had experienced AUD symptoms by subtracting the age of first AUD symptom from baseline age.
2.2.5 Nicotine use disorder symptoms
A binary variable was used to indicate the presence of any lifetime DSM-IV nicotine use disorder symptoms at baseline (0=no symptoms, 1=one or more).
2.2.6 Alcohol consumption factor score (ACFS)
We created an ACFS (See Supplement 11) which was a latent representation of four past-year alcohol consumption indices: Typical consumption, maximum drinks in a day, frequency of binge drinking, and frequency of intoxication (Agrawal et al., 2009; Grant et al., 2009).
2.2.7 Mood/anxiety disorders
A dichotomous variable indicated the presence of any DSM-IV lifetime mood or anxiety disorders (major depression, social phobia, panic disorder, agoraphobia, and generalized anxiety) reported at baseline.
2.2.8 Cannabis use disorder
We created a binary variable indicated lifetime DSM-IV cannabis use disorder (abuse or dependence) at baseline.
2.2.9 Drug use
A binary variable indicated the lifetime use of drugs at baseline other than cannabis including cocaine, stimulants, opiate, hallucinogens, PCP, inhalants, or solvents, or sedatives.
2.2.10 Familial risk group
We used a four-category variable indicating the combination of low vs. high genetic and environmental risk (see Section 2.1).
2.2.11 Perception of drinking problems in first-degree relatives
Offspring reported at baseline if they thought their mother, father, or siblings were excessive drinkers or had alcohol problems. These dichotomous variables were summed to indicate number of family members perceived to have alcohol problems.
2.2.12 Help seeking among family members
Paternal interviews assessed help seeking with the question, “Did you seek or receive any help for your drinking during this period, including going to self help groups like AA?” Maternal interviews assessed help seeking by asking, “Have you ever been treated for a drinking problem or joined a self-help group, such as AA, for alcohol problems?” Sibling help seeking for drinking was ascertained from their own interview. We summed these variables to indicate the number of family members who sought help for drinking.
2.2.13 Baseline sociodemographic characteristics
We used a continuous variable for age and dichotomous variables for marital status (0=never married or previously married, 1=currently married), employment (0=not currently employed, 1=employed), and ancestry (0=reported ancestry from non-European countries, 1=reported only European ancestry). Education was coded with four hierarchical categories, with 4-year baccalaureate program completion taking precedence.
2.3 Analysis
Data analyses were conducted with Stata version 13 (StataCorp, 2013). We used the Huber-White robust variance estimator (Williams, 2000) to adjust for clustering of offspring within fathers (see Section 2.1). The data file contained one row per offspring.
To address panel attrition and missing responses, we analyzed 20 imputed datasets created with multiple imputation with chained equations. All variables that were significantly associated with loss to follow-up (gender, ancestry, marital status, risk groups, lifetime AUD symptoms, nicotine symptoms, maternal AUD, and parent help seeking) were included in the imputation model.
2.3.1 Descriptive statistics and bivariate analyses
We calculated means or prevalences of baseline characteristics from the raw data and used logistic regression to calculate their association with lifetime alcohol problem recognition and help seeking at any time point from the imputed data.
2.3.2 Covariate-adjusted predictors of lifetime problem recognition and help seeking
We used logistic regression to identify baseline characteristics associated with lifetime alcohol problem recognition and help seeking at any time point. Our first model included sociodemographic, familial, and clinical characteristics. A second series of 11 additional models (one for each AUD symptom) were estimated to examine the association between individual AUD symptoms and the outcomes. These models included the particular symptom and total AUD count minus that symptom. For sensitivity analysis, we compared the results of the fully imputed sample (n = 1,073), which imputed all responses regardless of response to follow-up, with a sample (n = 609) that discarded respondents who did not respond to the third interview or did not have mother interview data but imputed responses for missing survey questions.
2.3.3 Alcohol problem recognition as a mediator of the relationship between AUD symptoms and new help seeking over follow up
These analyses excluded respondents (n = 148) who had at baseline reported a history of seeking help to examine incident help seeking, leaving n = 925 respondents. We examined problem recognition at baseline and incident help seeking in the four years between the baseline and third interview to establish temporal ordering. We were less concerned that AUD symptoms and problem recognition were measured concurrently because theoretically, symptoms would need to be present in order for one to recognize their alcohol problems. Mediation analyses was conducted in Mplus 7.3 with the product of coefficients approach (Muthén and Muthén, 1998). Help seeking and problem recognition were regressed on AUD symptoms and baseline characteristics, and help seeking was regressed on problem recognition. We calculated the statistical significance of the indirect effect of AUD symptoms on help seeking through problem recognition with the delta method (MacKinnon et al., 2007) and used the bias-corrected bootstrap method to calculate its 95% confidence interval, which cannot currently adjust for clustering (Mackinnon et al., 2004). We calculated mediation ratios as an approximate measure of effect size, which represented the ratio of the indirect effect to the total effect (Preacher and Kelley, 2011).
3. RESULTS
3.1 Descriptive statistics and bivariate analyses
At baseline offspring were on average 22.7 years old (range 13–32) and 54.7% were male (see Table 2). Respondents had experienced AUD symptoms for an average of 4.8 years at baseline (SD=3.6). By the third interview, 25.9% had alcohol problem recognition and 26.7% sought help in their lifetime (13.2% and 13.8%, respectively, by the baseline interview). Of those who sought help, 40.7% attended Alcoholics Anonymous, 82.1% sought help from a medical professional, other clinical professional, or religious leader, 10.5% received treatment in a residential or inpatient setting, and 32.7% sought help from more than one source.
Table 2.
Respondent characteristics and their association with lifetime alcohol problem recognition and help seeking (n = 1,073 respondents with alcohol use disorder symptoms at the baseline interview). Outcomes were measured at the third time point.
| Variable | Overall
|
Recognized problems in (25.9% of sample)lifetime alcohol
|
Sought help in (26.7% of sample)lifetime
|
|||
|---|---|---|---|---|---|---|
| N (%) or Mean (SD) | OR (95% CI) | OR (95% CI) | ||||
| Offspring baseline characteristics | ||||||
| Age -- M (SD) | 23 | 3.6 | 1.0 | (1.0–1.1) | 1.0 | (0.9–1.0) |
| Male | 588 | 54.7 | 2.3 | (1.6–3.3) | 1.3 | (0.9–1.7) |
| European ancestry | 917 | 85.4 | 1.7 | (1.0–2.9) | 1.8 | (1.1–2.9) |
| Education | ||||||
| Currently in high school | 100 | 9.3 | 0.9 | (0.5–1.6) | 1.0 | (0.6–1.8) |
| Did not complete high school | 34 | 3.2 | 1.2 | (0.5–2.8) | 2.0 | (0.7–5.2) |
| High school graduate or some college | 690 | 64.2 | 1.0 | (ref) | 1.0 | (ref) |
| 4-year baccalaureate program and above | 247 | 23.0 | 0.7 | (0.5–1.1) | 0.7 | (0.5–1.1) |
| Married (14 missing) | 223 | 21.3 | 0.6 | (0.4–1.0) | 0.7 | (0.4–1.0) |
| Employed | 871 | 81.1 | 1.3 | (0.8–2.0) | 1.0 | (0.7–1.4) |
| Familial risk | ||||||
| Dad had dependence | 499 | 46.5 | 1.2 | (0.8–1.8) | 1.9 | (1.3–2.9) |
| Dad unaffected, MZ cotwin had dependence | 150 | 14.0 | 1.0 | (0.6–1.8) | 1.3 | (0.7–2.2) |
| Dad unaffected, DZ cotwin had dependence | 127 | 11.8 | 0.9 | (0.5–1.7) | 1.5 | (0.8–2.9) |
| Dad unaffected, cotwin unaffected | 297 | 27.7 | 1.0 | (ref) | 1.0 | (ref) |
| Number of family members with perceived drinking problems -- M (SD) | 0.6 | 0.6 | 1.4 | (1.1–1.7) | 1.4 | (1.2–1.8) |
| Perceived drinking problems in father | 284 | 26.4 | 1.3 | (0.9–1.9) | 1.4 | (1.0–2.0) |
| Perceived drinking problems in mother | 75 | 7.0 | 1.4 | (0.8–2.6) | 1.9 | (1.1–3.3) |
| Perceived drinking problems in siblings | 304 | 28.3 | 1.7 | (1.2–2.4) | 1.6 | (1.1–2.2) |
| Number of lifetime AUD symptoms -- M (SD) | 3.3 | 2.5 | 1.5 | (1.4–1.6) | 1.4 | (1.3–1.4) |
| Years since first AUD symptom -- M (SD) | 4.8 | 3.6 | 1.1 | (1.1–1.2) | 1.1 | (1.0–1.1) |
| Lifetime nicotine dependence symptoms | 622 | 57.9 | 2.6 | (1.8–3.9) | 3.0 | (2.1–4.4) |
| Cannabis use disorder (3 missing) | 254 | 23.9 | 2.3 | (1.5–3.3) | 3.2 | (2.2–4.4) |
| Other illicit drug use (11 missing) | 464 | 44.2 | 3.1 | (2.1–4.4) | 2.9 | (2.0–4.1) |
| Lifetime mood/anxiety disorder | 555 | 51.7 | 1.3 | (0.9–1.8) | 1.5 | (1.1–2.1) |
| Major depression | 218 | 20.3 | 1.5 | (1.1–2.2) | 1.7 | (1.2–2.5) |
| Social phobia | 395 | 36.8 | 1.2 | (0.9–1.7) | 1.3 | (1.0–1.9) |
| Panic disorder | 134 | 12.5 | 1.8 | (1.1–2.8) | 1.6 | (1.0–2.6) |
| Agoraphobia | 61 | 5.7 | 2.1 | (1.2–3.9) | 2.6 | (1.5–4.8) |
| Generalized anxiety disorder | 56 | 5.2 | 1.7 | (0.9–3.2) | 2.3 | (1.3–4.0) |
| Family members’ interview data | ||||||
| Mother had AUD (84 missing) | 154 | 16.5 | 1.6 | (1.0–2.5) | 1.9 | (1.2–2.9) |
| Number of family members who sought help for drinking -- M (SD) | 0.3 | 0.5 | 1.5 | (1.1–2.0) | 1.6 | (1.1–2.1) |
| Father sought help (49 missing) | 128 | 12.8 | 1.1 | (0.7–1.8) | 1.4 | (0.9–2.3) |
| Mother sought help (81 missing) | 20 | 2.1 | 1.9 | (0.6–5.9) | 0.7 | (0.2–2.4) |
| Number of siblings who sought help -- M (SD) | 0.1 | 0.1 | 1.7 | (1.1–2.5) | 1.9 | (1.2–2.9) |
Means and prevalences are calculated from the raw data. Bivariate odds ratios were derived from cluster-adjusted logistic regression using 20 datasets created using multiple imputation.
In bivariate analyses, male gender, European ancestry, the number of family members with perceived drinking problems, major depression, panic disorder, agoraphobia, all offspring substance use variables, and the number of help-seeking family members were positively associated with alcohol problem recognition (see Table 2). European ancestry, the number of family members with perceived drinking problems, all substance use and psychiatric variables (except social phobia), maternal AUD, and the number help-seeking family members were positively associated with seeking help. Offspring in the HG-HE group (i.e., those with an affected father) were more likely to obtain help than those in the control group (LG-LE).
3.2 Covariate-adjusted predictors of lifetime problem recognition and help seeking
Any nicotine dependence symptoms and AUD symptom counts predicted both alcohol problem recognition and help seeking (see Table 3). Male gender and number of help-seeking family members were positively associated with problem recognition. Compared to offspring at lowest overall risk (LG-LE), offspring with the highest risk (HG-HE) were more likely to seek help. No other significant differences were observed among the familial risk groups. Two AUD criteria (physical/psychological problems, social problems) were associated with both outcomes, 3 others with problem recognition only and 1 with help seeking only. Sensitivity analyses of models without full imputation produced coefficients with the same direction and similar magnitude. The statistical significance of several coefficients changed, which could be due to an association between respondent characteristics and loss to follow-up (results available from first author upon request).
Table 3.
Adjusted associations of baseline characteristics with lifetime alcohol problem recognition and help seeking (n = 1,073)
| Variable | Recognized alcohol problems in lifetime
|
Sought help in lifetime
|
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Baseline characteristics1 | ||||
| Age | 1.0 | (1.0–1.1) | 1.0 | (0.9–1.0) |
| Male | 2.4 | (1.6–3.5) | 1.2 | (0.8–1.7) |
| European ancestry | 1.4 | (0.7–2.5) | 1.5 | (0.9–2.5) |
| Education | ||||
| Currently in high school | 1.4 | (0.6–3.2) | 1.2 | (0.6–2.3) |
| Did not complete high school | 0.9 | (0.3–2.7) | 1.6 | (0.6–4.9) |
| High school graduate or some college | 1.0 | (ref) | 1.0 | (ref) |
| 4-year baccalaureate program and above | 0.9 | (0.6–1.5) | 1.2 | (0.7–1.9) |
| Married | 0.9 | (0.5–1.5) | 0.9 | (0.5–1.5) |
| Employed | 1.1 | (0.7–1.9) | 1.0 | (0.6–1.6) |
| Family risk | ||||
| Dad had dependence | 1.1 | (0.7–1.7) | 1.6 | (1.0–2.6) |
| Dad unaffected, MZ cotwin had dependence | 1.0 | (0.5–1.9) | 1.4 | (0.8–2.6) |
| Dad unaffected, DZ cotwin had dependence | 1.1 | (0.6–2.3) | 1.9 | (0.9–3.8) |
| Dad unaffected, cotwin unaffected | 1.0 | (ref) | 1.0 | (ref) |
| Number of family members with perceived drinking problems | 1.1 | (0.9–1.4) | 1.0 | (0.8–1.3) |
| Any lifetime nicotine dependence symptoms | 1.7 | (1.1–2.7) | 2.0 | (1.3–3.0) |
| Lifetime cannabis use disorder | 0.9 | (0.5–1.4) | 1.5 | (1.0–2.3) |
| Lifetime other illicit drug use | 1.3 | (0.9–2.0) | 1.3 | (0.8–2.0) |
| Lifetime mood/anxiety disorder | 1.0 | (0.7–1.5) | 1.2 | (0.8–1.7) |
| Count of DSM-IV AUD symptoms | 1.5 | (1.4–1.7) | 1.3 | (1.2–1.4) |
| Alcohol consumption factor score | 1.1 | (0.9–1.2) | 1.1 | (1.0–1.2) |
| Biological mother had AUD | 1.1 | (0.7–1.9) | 1.4 | (0.9–2.4) |
| Number of family members who sought help for drinking | 1.7 | (1.2–2.6) | 1.3 | (0.9–2.0) |
| Individual AUD symptoms1 | ||||
| Tolerance | 1.0 | (0.5–2.0) | 0.9 | (0.5–1.6) |
| Withdrawal | 2.4 | (1.2–4.5) | 1.0 | (0.5–1.9) |
| Used larger amount/longer | 1.0 | (0.6–1.7) | 0.7 | (0.4–1.0) |
| Repeated attempts to quit/control use | 3.1 | (2.0–4.8) | 1.4 | (0.9–2.2) |
| Much time spent using | 1.7 | (1.1–2.7) | 1.2 | (0.8–1.8) |
| Activities given up to use | 1.2 | (0.7–2.1) | 1.0 | (0.6–1.7) |
| Physical/psychological problems | 2.0 | (1.3–3.1) | 2.3 | (1.5–3.5) |
| Neglected major roles to use | 1.0 | (0.7–1.7) | 1.0 | (0.7–1.7) |
| Hazardous use | 1.3 | (0.8–2.1) | 1.7 | (1.1–2.7) |
| Legal problems | 1.1 | (0.4–3.4) | 2.1 | (0.6–6.8) |
| Social/interpersonal problems | 1.8 | (1.2–2.8) | 2.2 | (1.5–3.4) |
OR=Odds ratio, CI=confidence interval, AD=alcohol dependence, MZ=monozygotic, DZ=dizygotic, AUD=alcohol use disorder. Results are from 20 imputed datasets. Model fit statistics: For problem recognition, F (21)=9.2, p <0.0001, average pseudo R2=0.29. For treatment utilization, F (21)=7.0, p <0.0001, average pseudo R2=0.19. Bolded values are statistically significant (p < 0.05).
Individual AUD symptoms were evaluated in separate models due to their collinearity.
3.3 Alcohol problem recognition as a mediator of the relationship between AUD symptoms and incident help seeking
Among those without a baseline history of help seeking (n = 925), 14.9% sought help between baseline and follow-up. Analyses indicated that the association between baseline AUD symptoms and help seeking at follow-up was mediated through alcohol problem recognition (see Table 4). The confidence interval generated by the bias-corrected bootstrap method did not include zero (b = 0.12 95%, CI = 0.01–0.27; not shown), which supported the robustness of the results. Alcohol problem recognition mediated approximately 97.6% of the total relationship between AUD symptoms and help seeking. This final model indicated that only problem recognition, lifetime AUD symptoms, and any nicotine dependence symptoms were associated with incident help seeking.
Table 4.
Effects decomposition of the test for alcohol problem recognition as a mediator of the relationship between alcohol use disorder (AUD) symptoms and incident help seeking (n=926)
| b | SE | p | |
|---|---|---|---|
AUD symptoms
 Problem recognition (path a) Problem recognition (path a) |
0.4 | 0.0 | 0.0 |
AUD symptoms
 Help seeking (path c’) Help seeking (path c’) |
0.0 | 0.1 | 1.0 |
Alcohol problem recognition
 Help seeking (path b) Help seeking (path b) |
0.4 | 0.2 | 0.0 |
| Indirect effect (path a * b) | 0.1 | 0.1 | 0.0 |
| Total effecta | 0.1 | 0.1 | 0.0 |
|
| |||
| Mediation ratio (%) | 97.6 | ||
b values are probit coefficients calculated in Mplus with the WLSMV estimator. Covariates included all sociodemographic, clinical, and familial predictors. Bolded values are statistically significant (p < 0.05). The total effect is calculated as the sum of the total indirect effect and the indirect effect. Mediation ratios are the ratio of the indirect effect to the total effect.
4. DISCUSSION
These results indicate that a history of help seeking for alcohol problems among family members of offspring was associated with the offspring’s own alcohol problem recognition. Familial risk for substance dependence was associated with help seeking, but not problem recognition. With regard to clinical characteristics, any symptoms of nicotine dependence and higher levels of AUD severity were associated with both alcohol problem recognition and help seeking. The recognition of one’s own alcohol problems mediated a large proportion of the relationship between experiencing AUD symptoms and seeking help. These findings provide important insights for research on correlates of help seeking, and have several important implications for intervention research.
While prior research has investigated the association between parental substance use problems and treatment seeking (Grella et al., 2009; True et al., 1996), we are not aware of research that has estimated the independent influence of help seeking within the family. Current findings suggest that the presence or lack of help seeking for alcohol problems within one’s family may play a role in the evaluation of one’s own alcohol problems. It is possible that knowledge of treatment seeking for drinking among family members may bring an otherwise stigmatized issue (Glass et al., 2013a, 2013b; Keyes et al., 2010) out in the open, allowing younger persons to acknowledge their own problem drinking. Because our assessments of help seeking were based on each family member’s self-report, offspring may not have been aware of their family member’s history. It could be that a common familial factor (environmental or genetic) promotes problem recognition or help seeking, as discussed by others (True et al., 1996). It was intriguing that familial help seeking was associated only with problem recognition, but not help seeking. This may be because decisions to seek help involves practical issues, such as transportation, access, and money (Fortney et al., 2011; Pfeiffer et al., 2011), and social issues, such as making oneself vulnerable to stigmatization from society by revealing one’s alcohol problems (Fortney et al., 2004; Glass et al., 2013b; Goffman, 1963).
Offspring at high genetic and high environmental risk were more likely to seek help than those at low genetic and environmental risk. This finding indicates that being raised in a high-risk family environment contributed additionally to help seeking above and beyond having genetic vulnerability for alcohol problems. However, we did not observe differences between HG-HE offspring and other risk groups, including the HG-LE risk group, in supplemental analyses. This could indicate a lack of power to detect differences between other groups and controls. Alternatively, unmeasured influences may play a role in those findings, (e.g., maternal attributes, family functioning, economic resources). Prior twin research has suggested that familial influences on help seeking for alcohol problems are partially distinct from influences of disorder severity (True et al., 1996). Perhaps, an offspring of twins design discordant for help seeking status, rather than substance dependence status, would be better optimized to disentangle genetic and environmental influences of help seeking.
Consistent with prior studies (Edlund et al., 2009), having more AUD symptoms predicted problem recognition and help seeking, which suggests that more pervasive alcohol problems are more easily recognized, and/or that the presence of multiple problems necessitates an increased need for treatment. A novel finding was that any nicotine symptoms were positively associated with alcohol problem recognition and help seeking, in both lifetime and incident analyses. The increasingly negative social attitudes toward smoking, along with mounting evidence of harmful effects on oneself and others (e.g., second hand smoke) may lead to health care consultations in which alcohol problems are addressed as well. Alcohol consumption severity and the presence of any mood/anxiety disorders were not associated with problem recognition or help seeking in adjusted analyses, which conflicts with findings from studies (Edlund et al., 2009; Glass et al., 2010). Perhaps, familial risk that was measured in the present study but not included in prior work may be a proxy for other mental health conditions, which led to the negative results. It was also surprising that perceived alcohol problems within the family were associated in unadjusted, but not adjusted, analyses, which likely was captured in the parental risk group measures.
It is notable that all AUD symptoms associated with problem recognition in the current study were also associated with perceived need for treatment in two nationally representative samples (Edlund et al., 2009). Withdrawal, repeated attempts to quit/control use, having spent much time using alcohol, continued use despite physical/psychological problems, and social/interpersonal problems may be particularly concerning to individuals. A fruitful strategy for intervention and prevention programs aimed at increasing alcohol problem recognition may be to target these particular consequences that may be seen as more problematic. In contrast, we did not observe associations with many of the symptoms that had been identified in other studies, although we did find, as have others, that hazardous use and continued use despite social/interpersonal problems were positively associated with help seeking (Edlund et al., 2009). Evaluations in other samples should be conducted to improve understanding of the association between specific AUD symptoms and help seeking.
A novel finding was nearly all of the effect of AUD symptom severity on help seeking was mediated through problem recognition. The experience of alcohol problems may shape the way that people perceive their alcohol consumption as problematic that may, in turn, influence decisions to seek care. Traditional conceptual frameworks of health services utilization have considered illness-related symptoms as broad measures that indicate a need for treatment (Andersen, 1995), For alcohol treatment utilization, the findings of the current study, in concert with other studies, point to the importance of focusing on the individual’s perception of their problems and treatment need (Edlund et al., 2006; Mojtabai et al., 2002). In particular, prospective studies that examine perceived need for alcohol treatment are scarce (Mojtabai et al., 2012), and more are needed.
We found that men were more likely than women to recognize their alcohol problems. Associations between sociodemographic characteristics and help seeking have been inconsistent (Glass et al., 2010; Ilgen et al., 2011; Mojtabai et al., 2012; Oleski et al., 2010). This may reflect that sociocultural predispositions to treatment seeking may be less important than illness-related factors (e.g., symptomatology) and the self-appraisal of one’s own illness.
4.1 Limitations
Findings must be considered in light of several limitations. Court-mandated treatment and availability/types of health insurance were not measured (Booth et al., 2013; Ilgen et al., 2011). Because of the relatively low rate of help seeking in our sample, we were unable to examine differences in specific sources of care. The longitudinal data permitted prospective analyses, but the four year follow-up may have been too short. Such brief follow-up periods may not allow enough time for participants to utilize treatment, although longer follow-up periods may miss important fluctuations in both predictor and outcome variables. Our sample was predominantly European, which prevents generalization to other ethnic groups. Revisions (DSM-5) to the AUD diagnosis added the criterion of craving (Hasin et al., 2013), which was not assessed in this study and which may have relevance for treatment seeking. Sibling help seeking was only available for those who were interviewed.
4.2 Conclusions
In adolescents and young adults at varying levels of genetic and environmental risk who were experiencing symptoms of DSM-IV AUD, approximately 25.9% recognized their alcohol problems and 26.7% sought help for drinking. Facilitating the self-recognition of AUD symptoms, and the awareness of family members’ help seeking for alcohol problems, may be potentially promising methods to increase the likelihood of help seeking for alcohol problems.
Supplementary Material
Highlights.
Symptoms of alcohol use disorder occur in younger persons but treatment is often delayed or never sought
We examined predictors of alcohol problem recognition and help seeking in a younger sample
Family members help seeking predicted help seeking in adolescents and young adults
Alcohol problem recognition mediated the association between symptoms help seeking
Acknowledgments
Role of Funding Sources. Dr. Glass received support for this project from the University of Wisconsin-Madison Graduate School with funding from the Wisconsin Alumni Research Foundation (PRJ74CB). Dr. Bucholz received support from the National Institutes of Health (DA14363 and AA11998). The funders had no role in the study design, collection, analysis or interpretation of the data, writing or approval of the manuscript, or decision to submit the manuscript for publication.
We would like to acknowledge the Department of Veterans Affairs (VA) Cooperative Studies Program (CSP) for the development and maintenance of the VET Registry, including the management of CSP Study #256, Vietnam Era Twin Registry. Statements, opinions, or views are solely of the author(s) and do not reflect official views of VA. We are most grateful for the participation of members of the VET Registry and their families, who ultimately made this research possible.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Conflict of Interest. All authors declare that they have no conflicts of interest.
Contributors. JEG conceptualized the study’s design, supervised the statistical analyses, and prepared drafts of the manuscript. HYY conducted the statistical analyses. JDG and KKB provided methodological consultation, substantive guidance about the data and selection of constructs for analysis, interpretation of the results and critical revision of the manuscript. All authors approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
J.E. Glass, Email: jglass2@wisc.edu.
J.D. Grant, Email: grantj@psychiatry.wustl.edu.
H.Y. Yoon, Email: hyoon43@wisc.edu.
K.K. Bucholz, Email: kkb@wustl.edu.
References
- Agrawal A, Grant JD, Littlefield A, Waldron M, Pergadia ML, Lynskey MT, Madden PA, Todorov A, Trull T, Bucholz KK, Todd RD, Sher K, Heath AC. Developing a quantitative measure of alcohol consumption for genomic studies on prospective cohorts. J Stud Alcohol Drugs. 2009;70:157–168. doi: 10.15288/jsad.2009.70.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- Booth BM, Curran GM, Han X, Edlund MJ. Criminal justice and alcohol treatment: results from a national sample. J Subst Abuse Treat. 2013;44:249–255. doi: 10.1016/j.jsat.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Homan SM, Helzer JE. When do alcoholics first discuss drinking problems? J Stud Alcohol. 1992;53:582–589. doi: 10.15288/jsa.1992.53.582. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Factors associated with first utilization of different types of care for alcohol problems. J Stud Alcohol Drugs. 2012;73:647–656. doi: 10.15288/jsad.2012.73.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006;101:824–834. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Hingson RW, Grant BF. Epidemiology of alcohol use, abuse and dependence. In: Tsuang MT, Tohen M, Jones PB, editors. Textbook of Psychiatric Epidemiology. John Wiley & Sons, Ltd; Chichester, UK: 2011. pp. 361–379. [Google Scholar]
- Dimeff LA. Brief Alcohol Screening And Intervention For College Students (BASICS): A Harm Reduction Approach. Guilford Press; New York: 1999. [Google Scholar]
- Duncan AE, Scherrer J, Fu Q, Bucholz KK, Heath AC, True WR, Haber JR, Howell D, Jacob T. Exposure to paternal alcoholism does not predict development of alcohol-use disorders in offspring: evidence from an offspring-of-twins study. J Stud Alcohol. 2006;67:649–656. doi: 10.15288/jsa.2006.67.649. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Feldman ZL. Perceived need for treatment for alcohol use disorders: results from two national surveys. Psychiatr Serv. 2009;60:1618–1628. doi: 10.1176/appi.ps.60.12.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Han X. Who seeks care where? utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J Stud Alcohol Drugs. 2012;73:635. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Unutzer J, Curran GM. Perceived need for alcohol, drug, and mental health treatment. Soc Psychiatry Psychiatric Epidemiol. 2006;41:480–487. doi: 10.1007/s00127-006-0047-1. [DOI] [PubMed] [Google Scholar]
- Eisen S, Neuman R, Goldberg J, Rice J, True W. Determining zygosity in the Vietnam Era Twin Registry: an approach using questionnaires. Clin Genet. 1989;35:423–432. doi: 10.1111/j.1399-0004.1989.tb02967.x. [DOI] [PubMed] [Google Scholar]
- Finney JW, Wilbourne PL, Moos RH. A Guide to Treatments That Work. Oxford University Press; New York: 2007. Psychosocial treatments for substance use disorders; pp. 179–202. [Google Scholar]
- Fortney JC, Burgess JF, Jr, Bosworth HB, Booth BM, Kaboli PJ. A re-conceptualization of access for 21st century healthcare. J Gen Intern Med. 2011;26(Suppl 2):639–647. doi: 10.1007/s11606-011-1806-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. J Behav Health Serv Res. 2004;31:418–429. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- Glass JE, Kristjansson SD, Bucholz KK. Perceived alcohol stigma: factor structure and construct validation. Alcohol Clin Exp Res. 2013a;37(Suppl 1):E237–246. doi: 10.1111/j.1530-0277.2012.01887.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Mowbray OP, Link BG, Kristjansson SD, Bucholz KK. Alcohol stigma and persistence of alcohol and other psychiatric disorders: a modified labeling theory approach. Drug Alcohol Depend. 2013b;133:685–692. doi: 10.1016/j.drugalcdep.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Perron BE, Ilgen MA, Chermack ST, Ratliff S, Zivin K. Prevalence and correlates of specialty substance use disorder treatment for Department of Veterans Affairs Healthcare System patients with high alcohol consumption. Drug Alcohol Depend. 2010;112:150–155. doi: 10.1016/j.drugalcdep.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes On The Management Of Spoiled Identity. Prentice-Hall; Englewood Cliffs, N.J: 1963. [Google Scholar]
- Grant JD, Agrawal A, Bucholz KK, Madden PA, Pergadia ML, Nelson EC, Lynskey MT, Todd RD, Todorov AA, Hansell NK, Whitfield JB, Martin NG, Heath AC. Alcohol consumption indices of genetic risk for alcohol dependence. Biol Psychiatry. 2009;66:795–800. doi: 10.1016/j.biopsych.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Moore AA, Niv N. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatr Serv. 2009;60:1068–1074. doi: 10.1176/appi.ps.60.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, Grant BF. DSM-5 Criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170:834–851. doi: 10.1176/appi.ajp.2013.12060782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Price AM, Burnett-Zeigler I, Perron B, Islam K, Bohnert AS, Zivin K. Longitudinal predictors of addictions treatment utilization in treatment-naïve adults with alcohol use disorders. Drug Alcohol Depend. 2011;113:215–221. doi: 10.1016/j.drugalcdep.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Waterman B, Heath A, True W, Bucholz KK, Haber R, Scherrer J, Fu Q. Genetic and environmental effects on offspring alcoholism: new insights using an offspring-of-twins design. Arch Gen Psychiatry. 2003;60:1265–1272. doi: 10.1001/archpsyc.60.12.1265. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, McLaughlin KA, Link BG, Olfson M, Grant BF, Hasin DS. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol. 2010;172:1364–1372. doi: 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Brown CH, Wang W, Hoffman JM. The intermediate endpoint effect in logistic and probit regression. Clin Trials. 2007;4:499–513. doi: 10.1177/1740774507083434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res. 2004;39:99. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Motivational Enhancement Therapy Manual: A Clinical Research Guide For Therapists Treating Individuals With Alcohol Abuse And Dependence. DIANE Publishing; Los Angeles: 1995. [Google Scholar]
- Milne BJ, Caspi A, Harrington H, Poulton R, Rutter M, Moffitt TE. Predictive value of family history on severity of illness: the case for depression, anxiety, alcohol dependence, and drug dependence. Arch Gen Psychiatry. 2009;66:738. doi: 10.1001/archgenpsychiatry.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: results from a longitudinal study. Drug Alcohol Depend. 2012;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: 1998. [Google Scholar]
- Oleski J, Mota N, Cox BJ, Sareen J. Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatr Serv. 2010;61:1223–1231. doi: 10.1176/ps.2010.61.12.1223. [DOI] [PubMed] [Google Scholar]
- Oser ML, McKellar J, Moos BS, Moos RH. Changes in ambivalence mediate the relation between entering treatment and change in alcohol use and problems. Addict Behav. 2010;35:367–369. doi: 10.1016/j.addbeh.2009.10.024. [DOI] [PubMed] [Google Scholar]
- Pfeiffer PN, Glass JE, Austin K, Valenstein M, McCarthy JF, Zivin K. Impact of distance and facility of initial diagnosis on depression treatment. Health Serv Res. 2011;46:768–786. doi: 10.1111/j.1475-6773.2010.01228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16:93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Redko C, Carlson RG, Rapp RC. A Folk model of treatment readiness among drug users in Ohio. J Ethn Subst Abuse. 2007;6:15–40. doi: 10.1300/J233v06n02_03. [DOI] [PubMed] [Google Scholar]
- Saunders SM, Zygowicz KM, D’Angelo BR. Person-related and treatment-related barriers to alcohol treatment. J Subst Abuse Treat. 2006;30:261–270. doi: 10.1016/j.jsat.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Scherrer JF, Grant JD, Duncan AE, Pan H, Waterman B, Jacob T, Haber JR, True WR, Heath AC, Bucholz KK. Measured environmental contributions to cannabis abuse/dependence in an offspring of twins design. Addict Behav. 2008;33:1255–1266. doi: 10.1016/j.addbeh.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Anthenelli RM, Bucholz KK, Hesselbrock VM, Tipp J. The time course of development of alcohol-related problems in men and women. J Stud Alcohol. 1995;56:218–225. doi: 10.15288/jsa.1995.56.218. [DOI] [PubMed] [Google Scholar]
- Sexton RL, Carlson RG, Leukefeld CG, Booth BM. Barriers to formal drug abuse treatment in the rural south: a preliminary ethnographic assessment. J Psychoactive Drugs. 2008;40:121–129. doi: 10.1080/02791072.2008.10400621. [DOI] [PubMed] [Google Scholar]
- Small J, Ounpraseuth S, Curran GM, Booth BM. Motivation to change as a mediator for the longitudinal relationships of gender and alcohol severity with one-year drinking outcome. J Stud Alcohol Drugs. 2012;73:504. doi: 10.15288/jsad.2012.73.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. StataCorp, LP; College Station, TX: 2013. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health (NSDUH): Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. (No. HHS Publication No. (SMA) 14-4863), NSDUH Series H-48. [Google Scholar]
- True WR, Heath AC, Bucholz K, Slutske W, Romeis JC, Scherrer JF, Lin N, Eisen SA, Goldberg J, Lyons MJ, Tsuang MT. Models of treatment seeking for alcoholism: the role of genes and environment. Alcohol Clin Exp Res. 1996;20:1577–1581. doi: 10.1111/j.1530-0277.1996.tb01702.x. [DOI] [PubMed] [Google Scholar]
- True WR, Romeis JC, Heath AC, Flick LH, Shaw L, Eisen SA, Goldberg J, Lyons MJ. Genetic and environmental contributions to healthcare need and utilization: a twin analysis. Health Serv Res. 1997;32:37–53. [PMC free article] [PubMed] [Google Scholar]
- Tsuang MT, Lyons MJ, Eisen SA, Goldberg J, True W, Lin N, Meyer JM, Toomey R, Faraone SV, Eaves L. Genetic influences on DSM-III-R drug abuse and dependence: A study of 3,372 twin pairs. Am J Med Genet. 1996;67:473–477. doi: 10.1002/(SICI)1096-8628(19960920)67:5<473::AID-AJMG6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Van Gemert C, Dietze P, Gold J, Sacks-Davis R, Stoové M, Vally H, Hellard M. The Australian national binge drinking campaign: campaign recognition among young people at a music festival who report risky drinking. BMC Public Health. 2011;11:482. doi: 10.1186/1471-2458-11-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- Xian H, Scherrer JF, Pergadia ML, Madden PAF, Grant JD, Sartor CE, Haber JR, Jacob T, Bucholz KK. Contribution of parental psychopathology to offspring smoking and nicotine dependence in a genetically informative design. J Stud Alcohol Drugs. 2010;71:664–673. doi: 10.15288/jsad.2010.71.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.