Abstract
Objectives
We sought to describe the effect of alterations in hip morphology with respect to worsening hip OA in a community-based sample including African American (AA) and white men and women.
Methods
This nested case-control study defined case hips as Kellgren Lawrence grade (KLG)<3 on baseline supine pelvis radiographs and KLG≥3 or THR for OA at the 1st or 2nd follow-up visit (mean 6 and 13 years, respectively); control hips had KLG<3 at both visits, with gender/race distribution similar to cases. Hip morphology was assessed using HipMorf software (Oxford, UK). Descriptive means and standard errors were obtained from generalized estimating equation (GEE) models. Sex-stratified GEE regression models (accounting for within-person correlation), adjusted for age, race, BMI, and side were then employed.
Results
A total of 120 individuals (239 hips; 71 case/168 control) were included (25% male, 26% AA, mean age 62 years, BMI 30 kg/m2). Case hips tended to have greater baseline AP alpha angles, smaller minimum joint space width (mJSW) and more frequent triangular index signs. Adjusted results among men revealed that higher AP alpha angle, Gosvig ratio, and acetabular index were positively associated with case hips; coxa profunda was negatively associated. Among women, greater AP alpha angle, smaller mJSW, protrusio acetabuli, and triangular index sign were associated with case hips.
Conclusions
We confirmed an increased risk of worsening hip OA due to baseline features of cam deformity among men and women, as well as protrusio acetabuli among women, and provide the first estimates of these measures in AAs.
Keywords: hip morphology, femoroacetabular impingement, race/sex differences
Femoroacetabular impingement (FAI) describes pathologic contact at the hip joint resulting from abnormal variations in hip morphology related to the proximal femur (cam), acetabulum (pincer), or both (mixed)1, 2. Reported FAI prevalence rates vary based on the population and diagnostic criteria used, ranging from 10%-39%3. There is a well-documented and growing body of evidence supporting the connection between FAI morphology and increased risk for osteoarthritis (OA), the most common form of arthritis and a leading cause of disability. For example, Gosvig et al. found that the presence of either a pistol grip deformity (cam) or deep acetabular socket (pincer) conferred an increased risk of hip OA4. Evidence suggests a greater risk for hip OA in the presence of a cam-type compared with pincer-type impingement5, 6, and there is conflicting evidence for an independent association between pincer impingement and risk for hip OA4, 7, 8. There is also an association between FAI features and severe hip OA resulting in total hip replacement (THR)8, 9.
FAI morphology has been studied in various geographic populations including Japan10, 11, China12, Denmark4, the Netherlands5, 7, and the UK8, 13, and in specific athletic populations (e.g., ballet14, soccer15, football16, hockey17). One study demonstrated a higher prevalence of abnormal hip morphology and OA among Caucasian compared with Asian women12. Gender differences have also been explored, with hip dysplasia much more common among women18, 19, and a greater tendency toward cam-type morphology (higher mean radiographic anteroposterior [AP] alpha angle, triangular index sign) in men20, 21. Despite research among these and other populations, no research has been conducted to assess FAI and variations in hip morphology among African Americans (AA) and very few studies have utilized a community-based sample. Therefore, this study aims to describe variations in hip morphology with respect to worsening hip OA in a large community-based cohort including AA and Caucasian men and women using a nested case-control study design.
PARTICIPANTS AND METHODS
This case-control study was nested within the Johnston County OA Project. Details of the parent project, which has been continuously approved by the Institutional Review Boards of the University of North Carolina (UNC) and the Centers for Disease Control and Prevention have been reported elsewhere22, 23; this study was specifically approved by the UNC IRB (#11-1021).
We utilized the baseline visit (1991-7), first follow-up (mean 6 years, 1999-2004) and second follow-up (mean 12.7 years, 2006-10). As part of the parent study, all men, and women over 50 years of age, underwent standardized supine AP pelvic radiography with feet in 15 degrees of internal rotation at each clinic visit. All hips were read for Kellgren Lawrence grade (KLG) by a single, experienced musculoskeletal radiologist (JBR) with high reliability (inter-reader k 0.859, intra-reader [comparison with another expert reader] 0.886)24. Radiographs were scored as KLG=0 in the absence of radiographic OA features; KLG=1 in the presence of a small osteophyte of doubtful significance; KLG=2 with an osteophyte but no joint space narrowing; KLG=3 if there was moderate joint space narrowing; and KLG=4 if severe joint space narrowing was present, along with subchondral bone sclerosis25.
Age and race were self-reported, while height and weight were measured in clinic; body mass index (BMI) was calculated as weight (kg)/height (m2). Participants also completed detailed interviewer-administered questionnaires including assessment of hip symptoms (“on most days, do you have pain, aching, or stiffness in your right|left hip?”), history of hip injury, and groin pain.
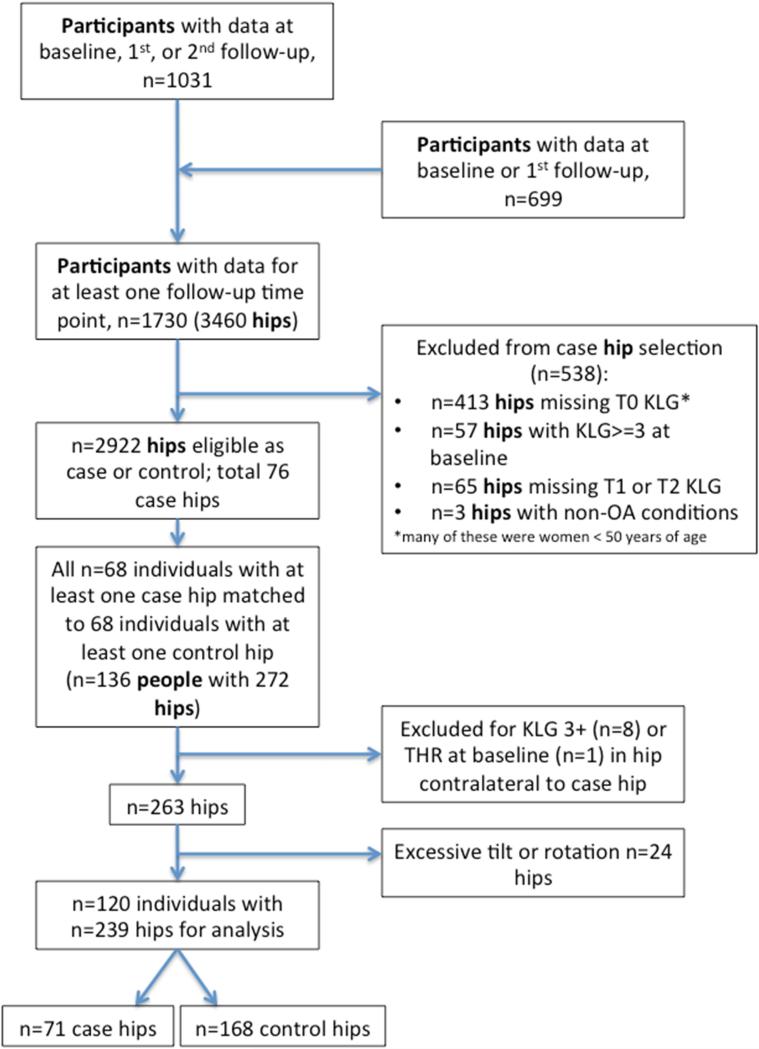
Case hips were conservatively defined as those with a KLG <3 at baseline, and KLG ≥ 3 (or THR for OA) at follow-up. This threshold was chosen as it more closely approximates a modified Croft grade of 3 or more, which has been used and validated in other studies26, 27. Control hips had KLG <3 at both baseline and follow-up. For this analysis, we selected all individuals (person-level) with radiographs from at least 2 time-points with at least one hip meeting our case definition of worsening hip OA. We considered the distribution of case individuals across 4 strata (white women, white men, AA women, and AA men) and randomly selected control individuals in an equal distribution, with at least one hip meeting the control definition (Figure).
Figure 1.
Flowchart of hip selection
Sixty-eight individuals with at least one case hip were selected along with 68 controls with a similar race and sex distribution, for a total of 136 individuals. Of these participants, 25% were men, 29% were AA, with a mean age of 62 ± 9 years and mean BMI 30 ± 6 kg/m2. Hips with KLG ≥ 3 or THR at baseline were excluded (n=9), such that hip morphology was assessed for all 263 hips with a KLG <3 at baseline; or 76 case and 187 control hips. An additional 13 individuals (24 hips) were excluded due to excessive tilt or rotation, resulting in a total of 120 individuals with 239 hips for hip-based analyses, with 71 case and 168 control hips (Figure). The demographics of this group did not differ significantly from the original 136 individuals (data not shown).
OxMorf morphology software, which includes HipMorf, developed by the University of Oxford, was used to assess 23 aspects of hip morphology on the baseline hip films. HipMorf measurements have previously been shown to have high reproducibility as well as predictive validity for both radiographic OA progression and future hip replacement in a population-based cohort 8, 13. One reader read all films (AEN); intra-reader reliability (AEN) was assessed on 20 films read twice 2 weeks apart, while inter-reader reliability was assessed on 20 films read by two readers (AEN/KML, supplemental table). For crossover sign and deep acetabulum only, intra-reader reliability (AEN) was assessed on 30 films read twice 4 weeks apart, and inter-reader reliability was assessed on 10 films read by two readers (AEN/JBR, supplemental table). Hip morphology measures included (supplemental figure) assessments of acetabular orientation (depth, width, depth:width ratio, crossover sign 28), acetabular coverage (acetabular index [aka Toit angle, angle of the sourcil relative to the teardrop axis], extrusion index, lateral center edge angle [LCEA], protrusio acetabula, coxa profunda), cam deformity (AP alpha angle, triangular index sign29, Gosvig ratio [continuous version of the triangular index sign], and modified triangular index height 8), femoral angles (proximal femoral angle [angle between the femoral shaft and a line joining the greater trochanter and center of femoral head] and femoral shaft angle [angle between the femoral shaft and femoral neck]), and anatomic distance (femoral head and neck, interacetabular edge, distance between femoral heads and teardrops, sacroiliac [SI] joint to pubic symphysis). Prior to the final analysis, hips with excessive tilt (sacrococcygeal [SC] joint to pubic symphysis distance >50 mm in men or >80 mm in women 30) or pelvic rotation (obturator index <0.6 or >1.4 29) were excluded.
Statistical Analysis
All analyses were hip-based, except as noted. Intra-class correlation coefficients were used to assess reliability of morphologic assessments. Baseline characteristics were generated for the sample by case/control status (Table 1). For descriptive purposes, we stratified the sample by sex and race separately (Tables 2 and 3, respectively) and obtained model-estimated means (or percentages as appropriate) with corresponding standard errors for each of the morphologic variables, using generalized estimating equations (GEE) to account for the correlation between hips in the same subject. These models were used only to generate means and standard errors; no demographic adjustment was included and no inferential p-values are reported. Consistent with our descriptive focus, the goal of this work is to provide means and measures of variability in this population to allow comparison to the literature; subsequent discussion of these findings is intended as strictly qualitative without necessarily implying statistical significance.
Table 1.
Hip (n=239) Characteristics at Baseline by Case/Control Status
| Characteristic | Case (n=71) n(%) or mean (SD) | Control (n=168) n(%) or mean (SD) |
|---|---|---|
| Sex* | ||
| Women | 54 (76%) | 126 (75%) |
| Men | 17 (24%) | 42 (25%) |
| Race* | ||
| White | 51 (72%) | 125 (74%) |
| African American | 20 (28%) | 43 (26%) |
| Side | ||
| Right | 47 (66%) | 73 (43%) |
| Left | 24 (34%) | 95 (57%) |
| Age (years) | 63 (8) | 62 (9) |
| BMI (kg/m2) | 30 (6) | 30 (5) |
| Height (cm) | 165 (9) | 166 (9) |
| Baseline KL grade | ||
| 0 | 4 (6%) | 26 (15%) |
| 1 | 22 (31%) | 94 (56%) |
| 2 | 45 (63%) | 48 (29%) |
| Groin pain present | 17 (24%) | 12 (7%) |
| Hip Symptoms present | 20 (28%) | 38 (23%) |
| History of Hip Injury | 2 (3%) | 3 (2%) |
groups selected to be comparable for sex and race
For BMI, n=237; for height, n=237; for hip symptoms, n=238
Table 2.
Morphologic variables by case/control status, stratified by sex (n=239)*
| Variable | Women (n=180) | Men (n=59) | ||
|---|---|---|---|---|
| Cases (n=54) | Controls (n=126) | Cases (n=17) | Controls (n=42) | |
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |
| MORPHOLOGY | ||||
| Acetabular depth (mm) | 35.85 (0.45) | 35.40 (0.35) | 39.62 (0.83) | 39.15 (0.66) |
| Acetabular width (mm) | 62.15 (0.54) | 61.50 (0.49) | 72.75 (1.17) | 72.26 (0.77) |
| Acetabular depth:width | 0.59 (0.01) | 0.57 (0.01) | 0.55 (0.02) | 0.54 (0.01) |
| AP alpha angle (°) | 64.58 (3.33) | 51.27 (1.54) | 67.34 (4.61) | 59.54 (2.79) |
| AP alpha angle >60° (categorical) | 47% (0.07) | 18% (0.04) | 59% (0.12) | 40% (0.09) |
| Minimum JSW (mm) | 3.17 (0.11) | 3.56 (0.08) | 3.43 (0.21) | 4.06 (0.13) |
| Extrusion index | 0.19 (0.01) | 0.18 (0.01) | 0.23 (0.02) | 0.21 (0.01) |
| Femoral shaft angle (°) | 132.27 (0.77) | 131.86 (0.65) | 130.10 (1.27) | 130.52 (1.09) |
| Gosvig ratio | 0.93 (0.01) | 0.93 (0.01) | 1.00 (0.01) | 0.99 (0.01) |
| Acetabular index (°) | 2.90 (1.18) | 1.08 (0.69) | 6.99 (2.68) | 3.28 (1.03) |
| LCEA (°) | 32.77 (1.20) | 33.04 (0.79) | 28.62 (2.57) | 30.01 (1.13) |
| LCEA <=25° | 17% (0.05) | 15% (0.04) | 34% (0.13) | 17% (0.06) |
| LCEA >40° | 24% (0.05) | 17% (0.04) | 10% (0.07) | 6% (0.04) |
| Proximal femoral angle (°) | 80.16 (0.79) | 80.67 (0.61) | 76.81 (2.21) | 81.88 (1.11) |
| Triangular index height (mm) | 21.19 (0.35) | 21.06 (0.24) | 27.39 (0.50) | 27.02 (0.47) |
| Crossover sign (categorical) | 28% (0.06) | 29% (0.04) | 46% (0.12) | 51% (0.09) |
| Deep acetabulum (categorical) | ||||
| Protrusio | 18% (0.06) | 4% (0.02) | 0% | 0% |
| Profunda | 68% (0.07) | 82% (0.04) | 29% (0.11) | 62% (0.09) |
| Triangular Index Sign (categorical) | 9% (0.04) | 2% (0.01) | 18% (0.09) | 8% (0.05) |
| DISTANCE | ||||
| Femoral head diameter (mm) | 54.34 (0.43) | 53.90 (0.40) | 63.90 (0.94) | 62.88 (0.65) |
| Femoral neck length (mm) | 57.13 (0.72) | 58.29 (0.62) | 60.28 (2.06) | 61.68 (1.75) |
| Minimum neck width (mm) | 36.50 (0.38) | 36.55 (0.33) | 43.96 (0.72) | 44.05 (0.65) |
| Interacetabular edge distance (mm) | 142.64 (1.28) | 142.64 (1.28) | 136.83 (1.86) | 136.82 (1.86) |
| Interhead center distance (mm) | 213.49 (1.74) | 213.49 (1.74) | 221.96 (2.56) | 221.96 (2.56) |
| Interteardrop distance (mm) | 141.82 (1.15) | 141.82 (1.15) | 134.65 (1.87) | 134.65 (1.87) |
| SI to symphysis (mm) | 104.49 (1.52) | 104.49 (1.52) | 81.57 (2.55) | 81.57 (2.55) |
| TILT | ||||
| Obturator foramen ratio | 1.02 (0.01) | 1.02 (0.01) | 1.07 (0.03) | 1.07 (0.03) |
| SC to symphysis (mm) | 48.18 (1.73) | 48.18 (1.73) | 18.23 (3.05) | 18.23 (3.05) |
Data are model-estimated means/percentages (standard errors) from GEE models unadjusted for covariates, accounting for correlation between hips in the same subject.
For femoral shaft angle, n=237; for Gosvig ratio, n=238; for deep acetabulum, n=234; for triangular index, n=238; for minimum neck width, n=238; for femoral neck length, n=238, for SC to symphysis, n=237.
Table 3.
Morphologic variables by case/control status, stratified by race (n=239)*
| Variable | White (n=176) | African American (n=63) | ||
|---|---|---|---|---|
| Cases (n=51) | Controls (n=125) | Cases (n=20) | Controls (n=43) | |
| MORPHOLOGY | ||||
| Acetabular depth (mm) | 36.70 (0.45) | 36.40 (0.38) | 37.00 (0.97) | 36.13 (0.74) |
| Acetabular width (mm) | 65.28 (0.79) | 64.59 (0.69) | 63.47 (1.05) | 62.70 (1.09) |
| Acetabular depth:width | 0.57 (0.01) | 0.56 (0.01) | 0.59 (0.02) | 0.57 (0.01) |
| AP alpha angle (°) | 65.36 (3.19) | 54.30 (1.73) | 64.79 (5.41) | 50.43 (1.85) |
| AP alpha angle >60° (categorical) | 48% (0.07) | 26% (0.04) | 55% (0.12) | 15% (0.06) |
| Minimum JSW (mm) | 3.22 (0.11) | 3.70 (0.09) | 3.20 (0.20) | 3.66 (0.11) |
| Extrusion index | 0.20 (0.01) | 0.19 (0.01) | 0.18 (0.02) | 0.17 (0.01) |
| Femoral shaft angle (°) | 131.85 (0.83) | 131.03 (0.67) | 131.46 (1.04) | 132.93 (0.92) |
| Gosvig ratio | 0.95 (0.01) | 0.94 (0.01) | 0.95 (0.02) | 0.94 (0.01) |
| Acetabular index (°) | 4.39 (1.32) | 2.29 (0.70) | 1.05 (2.34) | 0.68 (1.16) |
| LCEA (°) | 31.50 (1.29) | 31.61 (0.79) | 33.81 (2.48) | 33.58 (1.33) |
| LCEA <=25° | 24% (0.06) | 16% (0.04) | 10% (0.08) | 15% (0.06) |
| LCEA >40° | 20% (0.05) | 11% (0.03) | 23% (0.08) | 25% (0.07) |
| Proximal femoral angle (°) | 79.10 (1.14) | 81.07 (0.63) | 79.21 (1.43) | 80.98 (0.98) |
| Triangular index height (mm) | 22.89 (0.46) | 22.79 (0.37) | 22.17 (0.64) | 21.74 (0.59) |
| Crossover sign (categorical) | 41% (0.07) | 38% (0.05) | 9% (0.06) | 24% (0.07) |
| Deep acetabulum (categorical) | ||||
| Protrusio | 10% (0.05) | 2% (0.02) | 14% (0.11) | 11% (0.06) |
| Profunda | 61% (0.07) | 74% (0.04) | 71% (0.12) | 76% (0.08) |
| Triangular Index Sign (categorical) | 12% (0.04) | 4% (0.02) | 10% | 0% |
| DISTANCE | ||||
| Femoral head diameter (mm) | 57.16 (0.66) | 56.56 (0.56) | 55.51 (0.98) | 54.69 (0.94) |
| Femoral neck length (mm) | 58.25 (0.86) | 59.01 (0.79) | 56.84 (1.48) | 59.49 (1.08) |
| Minimum neck width (mm) | 38.31 (0.52) | 38.49 (0.48) | 38.45 (0.81) | 38.01 (0.83) |
| Interacetabular edge distance (mm) | 142.62 (1.22) | 142.62 (1.22) | 137.39 (2.23) | 137.39 (2.23) |
| Interhead center distance (mm) | 218.23 (1.60) | 218.23 (1.60) | 208.28 (3.09) | 208.28 (3.09) |
| Interteardrop distance (mm) | 141.43 (1.17) | 141.43 (1.17) | 136.36 (1.91) | 136.36 (1.91) |
| SI to symphysis (mm) | 98.64 (1.90) | 98.64 (1.90) | 100.00 (2.79) | 100.00 (2.79) |
| TILT | ||||
| Obturator foramen ratio | 1.04 (0.01) | 1.04 (0.01) | 1.02 (0.02) | 1.02 (0.02) |
| SC to symphysis (mm) | 38.87 (2.35) | 38.87 (2.35) | 46.98 (2.75) | 46.98 (2.75) |
Data are model-estimated means/percentages (standard errors) from GEE models unadjusted for covariates, accounting for correlation between hips in the same subject.
For femoral shaft angle, n=237; for Gosvig ratio, n=238; for deep acetabulum, n=234; for triangular index, n=238; for minimum neck width, n=238; for femoral neck length, n=238, for SC to symphysis, n=237.
Given a priori knowledge of likely sex differences 31-36 and the fact that most measures were substantially different by sex, all further analyses were Sex-stratified. Race stratified results are reported for descriptive purposes.
Logistic regression via a generalized estimating equations approach was employed to assess the associations between case/control status and each morphologic variable, accounting for within-person correlation (between hips in one individual, Table 4). These models were adjusted for age, race, BMI, and side (left/right hip), and adjusted odds ratios with 95% confidence intervals were obtained. Additional adjustment for baseline KLG did not affect the estimates and was not included in the final models. Control variables of age and BMI were used in these models as continuous variables while race and side were binary variables. Missing data were treated as missing completely at random. Person-based sensitivity analyses were conducted using one randomly selected case or control hip for each selected individual.
Table 4.
Associations between morphologic variables and case/control status stratified by sex
| Variable | Men (n=59) aOR (95% CI) | Women (n=180) aOR (95% CI) |
|---|---|---|
| MORPHOLOGY | ||
| Acetabular depth (mm) | 0.91 (0.78, 1.07) | 1.04 (0.93, 1.15) |
| Acetabular width (mm) | 1.01 (0.88, 1.15) | 0.98 (0.91, 1.05) |
| Acetabular depth:width* | 0.65 (0.17, 2.47) | 1.49 (0.77, 2.88) |
| AP alpha angle (°) | 1.04 (1.01, 1.07) | 1.04 (1.02, 1.05) |
| AP alpha angle >60 | 3.57(1.17, 10.90) | 4.61 (2.09, 10.16) |
| Minimum JSW (mm) | 0.46 (0.21, 1.04) | 0.32 (0.19, 0.54) |
| Extrusion index* | 2.40 (0.68, 8.51) | 0.86 (0.51, 1.45) |
| Femoral shaft angle (°) | 0.95 (0.87, 1.03) | 0.98 (0.92, 1.04) |
| Gosvig ratio* | 2.46 (1.08, 5.63) | 1.48 (0.90, 2.46) |
| Acetabular index (°) | 1.17 (1.02, 1.34) | 1.01 (0.97, 1.06) |
| LCEA (°) | 0.95 (0.84, 1.07) | 1.02 (0.98, 1.06) |
| LCEA <=25° | 3.63 (0.76, 17.29) | 1.31 (0.54, 3.18) |
| LCEA >40° | 0.84 (0.04, 17.57) | 1.73 (0.79, 3.77) |
| Proximal femoral angle (°) | 0.90 (0.81, 0.99) | 0.97 (0.91, 1.03) |
| Triangular index height (mm) | 1.17 (0.95, 1.44) | 1.05 (0.91, 1.21) |
| Crossover sign | 0.56 (0.18, 1.74) | 1.02 (0.47, 2.21) |
| Deep acetabulum | ||
| Protrusio | nd | 4.10 (1.00, 16.79) |
| Profunda | 0.22 (0.07, 0.69) | 0.87 (0.34, 2.20) |
| Triangular Index | 2.73(0.51, 14.58) | 6.17 (1.85, 20.53) |
| DISTANCE | ||
| Femoral head diameter (mm) | 1.03 (0.87, 1.22) | 0.96 (0.88, 1.06) |
| Femoral neck length (mm) | 0.95 (0.88, 1.02) | 0.96 (0.90, 1.02) |
| Minimum neck width (mm) | 1.02 (0.85, 1.22) | 0.94 (0.83, 1.07) |
| Interacetabular edge distance (mm) | 1.04 (0.98, 1.10) | 0.97 (0.95, 1.00) |
| Interhead center distance (mm) | 1.02 (0.98, 1.06) | 0.98 (0.96, 1.00) |
| Interteardrop distance (mm) | 1.02 (0.96, 1.07) | 0.98 (0.95, 1.01) |
| SI to symphysis (mm) | 0.98 (0.93, 1.02) | 0.99 (0.97, 1.02) |
Acetabular depth:width, Extrusion index, and Gosvig ratio given as OR per 0.1 change in unit.
Nd=not defined, no men with protrusion; adjusted for age, race, BMI, and side.
Measures with accepted cutoffs were analyzed as both continuous and categorical variables: for AP alpha angle we compared ≤60 to 60 degrees or more 37, and for LCEA we compared ≤25, >25-40 (referent), and >40 degrees 7. Where appropriate, the two-sided significance level was set at 0.05. All statistical computations were performed using SAS Version 9.3 software (SAS Institute, Cary, NC).
RESULTS
Characteristics of the 239 included hips are shown in Table 1.
Due to the selection process, case and control hips were similar by sex and race. Case hips were more often right hips and more often had baseline KLG=2. There were no apparent differences between cases and controls by age, BMI, height, waist/hip circumference, hip symptoms or injury. Cases were more likely to report baseline groin pain (24% vs. 7%), although infrequent in both groups (n=29 hips).
Reliability for all measures was acceptable (intra-reader ICC 0.7-1.00; inter-reader ICC 0.5-1.00, supplemental table).
Descriptive analyses were obtained from GEE models comparing case and control hips, (Table 2 and Table 3), with stratification by sex and race respectively, and are summarized here. As shown in Table 2, nearly all measures were qualitatively different by sex.
Male hips tended to have greater acetabular depth and width, higher AP alpha angles, greater mJSW, greater extrusion indices, higher Gosvig angles, acetabular indices, and modified triangular index height, as well as more frequent triangular index sign. Female hips tended to have greater LCEA and more frequent protrusio acetabuli and coxa profunda. Pelvic distance varied by sex as expected.
Racial differences were less marked than sex differences (Table 3).
Hips of AAs compared with Whites had qualitatively lower acetabular width, smaller extrusion indices, smaller acetabular indices, larger LCEA, and less frequent crossover signs. The femoral head diameter, interacetabular edge distance, interhead center distance, and interteardrop distance all appeared to be smaller in AAs, suggesting a narrower pelvis compared with whites.
As shown in Tables 2 and 3, regardless of sex or race stratification, compared with control hips, case hips tended toward greater AP alpha angles and acetabular indices, and smaller minimum joint space width, while other continuous measures did not appear to be substantially different. Case hips more often had AP alpha angles >60°. Protrusio acetabuli was present only in women and was more frequently seen among cases, while coxa profunda was more commonly present in controls. The triangular index sign was more frequently seen among cases.
Adjusted results: Men
As shown in Table 4, among men (left), no statistically significant associations were seen between case/control status and acetabular depth, acetabular width, depth:width ratio, femoral shaft angle, lateral center edge angle (continuous or categorized), mJSW, or crossover sign. There were also no associations between case/control status and geometric measures of distance. The odds of being a case hip were more than doubled with higher extrusion index or the presence of the triangular index sign, although not statistically significant. The odds of being a case hip were increased 4% for every one degree increase in AP alpha angle, and 17% for every one unit increase in acetabular index and modified triangular index height. The odds of being a case hip were more than three times as high for hips with a baseline AP alpha angle >60° (aOR 3.6 [95% CI 1.2-10.9]) and increased with increasing Gosvig ratio. Higher proximal femoral angle and the presence of coxa profunda were protective.
Adjusted results: Women
Among women (Table 4, right), there were no statistically significant associations between case status and acetabular depth, width or depth:width ratio, femoral shaft angle, proximal femoral angle, or crossover sign, or with any of the geometric measures of distance. There was also no association with extrusion index, Gosvig ratio, or modified triangular index height. Every degree of increase in AP alpha angle was associated with 4% increased odds of being a case hip; having an alpha angle >60 degrees (compared with ≤60 degrees) conferred more than 4 times the odds of being a case hip (OR 4.6, 95% CI [2.1-10.2]). The presence of protrusio acetabula, but not coxa profunda, was associated with 4 times the odds of being a case hip. The presence of the triangular index sign was associated with 6 times the odds of being a case hip. A greater baseline joint space width was protective.
Person-based sensitivity analyses using one randomly selected case or control hip for each individual provided similar results to the hip-based analyses, although some associations were no longer statistically significant due to smaller sample size (n=123 persons and hips after exclusion of 13 with excessive tilt or rotation; data not shown).
DISCUSSION
In this unique community-based sample of AA and white men and women assessed for hip morphology using a standardized method, we found that case hips tended to have higher AP alpha angles and acetabular indices, smaller mJSW, and more frequent protrusio acetabula and triangular index signs. This is in agreement with prior work showing that cam deformities (increased AP alpha angle and triangular index sign) are associated with incident hip OA, and is supportive of an association between acetabular overcoverage (protrusio acetabula but not coxa profunda) and hip OA, which has been less universally identified. We identified numerous qualitative differences in hip morphology between sexes. Differences by race were less marked, but are of interest and have not been previously reported for AAs.
In Sex-stratified analyses among men, higher extrusion index and Gosvig ratio, presence of the triangular index sign, and increased acetabular index, modified triangular index height, and AP alpha angle were seen in case hips. Coxa profunda was negatively associated with case hips, but given the unclear association between coxa profunda and hip pathology, the meaning of this finding (seen in men only) is unclear 38, 39. To date, no large prospective community-based studies with OA outcomes have reported on all of these measures specifically among men for comparison. A limited subset of three hip morphology measures was assessed in a recent cross-sectional study in asymptomatic older men, which reported an association between prevalent radiographic OA (Croft grade ≥2) and LCEA > 39 degrees, and between symptomatic OA (Croft grade ≥2 with symptoms) and femoral shaft angle < 125 degrees (termed CCD by the authors).40
Among women in our study, the indicators of cam-type deformity: higher AP alpha angle and the triangular index sign, were more frequent in case hips after adjustment for age, race, BMI, and side. In the Chingford cohort, a community-based study of white women aged 44-67, using the same software 8 and a similar radiographic protocol, AP alpha angle and triangular index sign and height were associated with progression to THR over 20 years in crude analyses, although triangular index was no longer statistically significantly associated after adjustment for age and BMI. This group also identified an independent association between smaller LCEA and THR, indicative of a tendency toward acetabular dysplasia. While extrusion index was associated with THA in Chingford, no statistically significant association was seen with worsening hip OA in our study 8. Protrusio acetabula, consistent with overcoverage 41, was associated with worsening hip OA in the current study but not in Chingford.
The Cohort Hip and Cohort Knee study, which recruited men and women with hip or knee pain or stiffness aged 45-65 years, and obtained weight-bearing AP pelvis and false profile hip films, also reported an association between AP alpha angle >60 degrees and the development of incident hip OA (KLG 2 or more, OR 2.4, positive predictive value 12%) but did not stratify by sex 5. They also found an association between mild acetabular dysplasia (LCEA < 25 degrees), but not pincer deformity (LCEA > 40 degrees), and incident hip OA 7.
In the current analysis, interactions between the morphologic measures and age, race, BMI, baseline KLG, and groin pain were explored, but none was significant at a p value ≤0.05. However, due to the preponderance of right hip cases, we performed some exploratory analyses including interactions between side and the morphology measures. In these exploratory analyses that would be expected to be underpowered, we found that among men, associations of AP alpha angle, mJSW, and Gosvig ratio were stronger on the right (p for interactions ≤ 0.04), while among women mJSW and LCEA were more strongly associated with case status on the left (p for interactions ≤ 0.1). Sidedness has been infrequently assessed in hip OA and in the FAI literature. More than 20 years ago, THR was reportedly more frequent in the right hip42 and a higher frequency of hip OA on the right side versus the left was noted 43, 44, also confirmed in a more recent study 45. Studies using various imaging methods in young adults have identified slightly higher alpha angles in right vs. left hips 20, 46, 47. In two radiographic studies of acetabular dysplasia, CEA was smaller on the right compared with the left 48, 49. Differences by side should be explored in other populations and larger samples, and if confirmed, underlying biomechanical explanations (e.g. leg dominance) should be sought.
This study has many strengths, including the stringent definition of worsening hip OA using a KLG of 3 or more determined by a single, highly reliable reader, standardized pelvis films with reliable FAI assessment using validated software, use of a community-based sample and inclusion of /presentation of morphologic values for AA and white men and women. The limitations of this work include the relatively small number of cases available and small numbers with certain features (e.g. groin pain), which reduced our power to detect interactions; for this reason we chose a more descriptive approach. Like other large epidemiological studies, we have 2D radiographs and lack specialized 3D imaging optimized for FAI assessment. However, plain radiography is still the accepted initial diagnostic imaging modality for FAI due to ease of acquisition, low cost, and low risk, and has adequate sensitivity 50.
CONCLUSION
This case control study nested in a large, well-characterized prospective community-based cohort provides sex-stratifed, and the first race-stratified values for a number of commonly assessed hip morphology variables, supporting the association between cam deformity and worsening hip OA. These data also support an association between acetabular overcoverage (protrusio acetabuli) and worsening hip OA among women.
Supplementary Material
Acknowledgments
We would like to thank: the participants and staff of the Johnston County Osteoarthritis Project, Oxford NIHR Musculoskeletal BRU for the support of Professor Nigel Arden and Dr M Kassim Javaid; Professor Cyrus Cooper, D Murray, R Gill, David Hunter, Sion Glyn-Jones, Geraint Thomas, and Antony Palmer for the development of OxMorf.
Role of the Funding Source
Funding was provided in part by: NIAMS K23 AR061406 (Nelson); NIH/NIAMS P60AR30701 (Jordan/Renner/Schwartz); CDC/ASPH S043 and S3486 (Jordan/Renner); Arthritis Research UK supporting the Centre for Sport, Exercise and Osteoarthritis (Leyland/Arden); evelopment of OxMorf was supported by NIH contract BAA-NHLBI-AR-10-06 (Contract No. HHSN268201000019C) to the University of California San Francisco and the University of Oxford. The funding sources had no role in design, analysis, interpretation or decision to publish this work.
Abbreviations
- OA
osteoarthritis
- THR
total hip replacement
- AA
African American
- KLG
Kellgren-Lawrence grade
- BMI
body mass index
- AP
anteroposterior
- mJSW
minimum joint space width
- FAI
femoroacetabular impingement
- LCEA
lateral center edge angle
- ICC
Intra-class correlation
- OR
odds ratio
- aOR
adjusted odds ratio
- CI
confidence interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions
Conception and design: AEN, NKA, JMJ; Acquisition of data: AEN, JLS, KML, JBR, JMJ; Analysis and interpretation of data: AEN, XAS, TAS, NKA, JMJ; Drafting of article: AEN, JLS; Reviewing for important intellectual content: all authors; Final approval of submitted version: all authors.
Competing Interest Statement
The authors declare no conflicts in relation to this work.
References
- 1.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Wright AA, Naze GS, Kavchak AE, Paul D, Kenison B, Hegedus EJ. Radiological variables associated with progression of femoroacetabular impingement of the hip: a systematic review. J Sci Med Sport. 2015;18:122–127. doi: 10.1016/j.jsams.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162–1169. doi: 10.2106/JBJS.H.01674. [DOI] [PubMed] [Google Scholar]
- 5.Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72:918–923. doi: 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 6.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agricola R, Heijboer MP, Roze RH, Reijman M, Bierma-Zeinstra SM, Verhaar JA, et al. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthritis Cartilage. 2013;21:1514–1521. doi: 10.1016/j.joca.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Nicholls AS, Kiran A, Pollard TC, Hart DJ, Arden CP, Spector T, et al. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: a nested case-control study. Arthritis Rheum. 2011;63:3392–3400. doi: 10.1002/art.30523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agricola R, Reijman M, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Total hip replacement but not clinical osteoarthritis can be predicted by the shape of the hip: a prospective cohort study (CHECK). Osteoarthritis Cartilage. 2013;21:559–564. doi: 10.1016/j.joca.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Fukushima K, Uchiyama K, Takahira N, Moriya M, Yamamoto T, Itoman M, et al. Prevalence of radiographic findings of femoroacetabular impingement in the Japanese population. J Orthop Surg Res. 2014;9:25. doi: 10.1186/1749-799X-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hashimoto S, Fujishiro T, Hayashi S, Kanzaki N, Nishiyama T, Kurosaka M. Clinical importance of impingement deformities for hip osteoarthritis progression in a Japanese population. Int Orthop. 2014;38:1609–1614. doi: 10.1007/s00264-014-2393-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dudda M, Kim YJ, Zhang Y, Nevitt MC, Xu L, Niu J, et al. Morphologic differences between the hips of Chinese women and white women: could they account for the ethnic difference in the prevalence of hip osteoarthritis? Arthritis Rheum. 2011;63:2992–2999. doi: 10.1002/art.30472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas GE, Palmer AJ, Batra RN, Kiran A, Hart D, Spector T, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthritis Cartilage. 2014;22:1504–1510. doi: 10.1016/j.joca.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 14.Duthon VB, Charbonnier C, Kolo FC, Magnenat-Thalmann N, Becker CD, Bouvet C, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29:411–419. doi: 10.1016/j.arthro.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Agricola R, Heijboer MP, Ginai AZ, Roels P, Zadpoor AA, Verhaar JA, et al. A cam deformity is gradually acquired during skeletal maturation in adolescent and young male soccer players: a prospective study with minimum 2-year follow-up. Am J Sports Med. 2014;42:798–806. doi: 10.1177/0363546514524364. [DOI] [PubMed] [Google Scholar]
- 16.Kapron AL, Anderson AE, Aoki SK, Phillips LG, Petron DJ, Toth R, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93:e111(111–110). doi: 10.2106/JBJS.K.00544. [DOI] [PubMed] [Google Scholar]
- 17.Siebenrock KA, Kaschka I, Frauchiger L, Werlen S, Schwab JM. Prevalence of cam-type deformity and hip pain in elite ice hockey players before and after the end of growth. Am J Sports Med. 2013;41:2308–2313. doi: 10.1177/0363546513497564. [DOI] [PubMed] [Google Scholar]
- 18.de Hundt M, Vlemmix F, Bais JM, Hutton EK, de Groot CJ, Mol BW, et al. Risk factors for developmental dysplasia of the hip: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2012;165:8–17. doi: 10.1016/j.ejogrb.2012.06.030. [DOI] [PubMed] [Google Scholar]
- 19.Hartofilakidis G, Karachalios T, Stamos KG. Epidemiology, demographics, and natural history of congenital hip disease in adults. Orthopedics. 2000;23:823–827. doi: 10.3928/0147-7447-20000801-16. [DOI] [PubMed] [Google Scholar]
- 20.Laborie LB, Lehmann TG, Engesaeter IO, Sera F, Engesaeter LB, Rosendahl K. The alpha angle in cam-type femoroacetabular impingement: new reference intervals based on 2038 healthy young adults. Bone Joint J. 2014;96-B:449–454. doi: 10.1302/0301-620X.96B4.32194. [DOI] [PubMed] [Google Scholar]
- 21.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49:436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 22.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–180. [PubMed] [Google Scholar]
- 23.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009;36:809–815. doi: 10.3899/jrheum.080677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8:242–250. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 25.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lane NE, Nevitt MC, Hochberg MC, Hung YY, Palermo L. Progression of radiographic hip osteoarthritis over eight years in a community sample of elderly white women. Arthritis Rheum. 2004;50:1477–1486. doi: 10.1002/art.20213. [DOI] [PubMed] [Google Scholar]
- 27.Arden NK, Lane NE, Parimi N, Javaid KM, Lui LY, Hochberg MC, et al. Defining incident radiographic hip osteoarthritis for epidemiologic studies in women. Arthritis Rheum. 2009;60:1052–1059. doi: 10.1002/art.24382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 29.Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89:1309–1316. doi: 10.1302/0301-620X.89B10.19405. [DOI] [PubMed] [Google Scholar]
- 30.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 31.Maillefert JF, Gueguen A, Monreal M, Nguyen M, Berdah L, Lequesne M, et al. Sex differences in hip osteoarthritis: results of a longitudinal study in 508 patients. Ann Rheum Dis. 2003;62:931–934. doi: 10.1136/ard.62.10.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nelson AE, Braga L, Renner JB, Atashili J, Woodard J, Hochberg MC, et al. Characterization of individual radiographic features of hip osteoarthritis in African American and White women and men: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2010;62:190–197. doi: 10.1002/acr.20067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, et al. Radiological progression of hip osteoarthritis: definition, risk factors and correlations with clinical status. Ann Rheum Dis. 1996;55:356. doi: 10.1136/ard.55.6.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. Factors influencing hip joint space in asymptomatic subjects. A survey of 4151 subjects of the Copenhagen City Heart Study: the Osteoarthritis Substudy. Osteoarthritis Cartilage. 2004;12:698–703. doi: 10.1016/j.joca.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Nelson AE, Liu F, Lynch JA, Renner JB, Schwartz TA, Lane NE, et al. Association of incident symptomatic hip osteoarthritis with differences in hip shape by active shape modeling: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2014;66:74–81. doi: 10.1002/acr.22094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nepple JJ, Riggs CN, Ross JR, Clohisy JC. Clinical presentation and disease characteristics of femoroacetabular impingement are sex-dependent. J Bone Joint Surg Am. 2014;96:1683–1689. doi: 10.2106/JBJS.M.01320. [DOI] [PubMed] [Google Scholar]
- 37.Agricola R, Waarsing JH, Thomas GE, Carr AJ, Reijman M, Bierma-Zeinstra SM, et al. Cam impingement: defining the presence of a cam deformity by the alpha angle: data from the CHECK cohort and Chingford cohort. Osteoarthritis Cartilage. 2014;22:218–225. doi: 10.1016/j.joca.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 38.Anderson LA, Kapron AL, Aoki SK, Peters CL. Coxa profunda: is the deep acetabulum overcovered? Clin Orthop Relat Res. 2012;470:3375–3382. doi: 10.1007/s11999-012-2509-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nepple JJ, Lehmann CL, Ross JR, Schoenecker PL, Clohisy JC. Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Joint Surg Am. 2013;95:417–423. doi: 10.2106/JBJS.K.01664. [DOI] [PubMed] [Google Scholar]
- 40.Nardo L, Parimi N, Liu F, Lee S, Jungmann PM, Nevitt MC, et al. Femoroacetabular Impingement: Prevalent and Often Asymptomatic in Older Men: The Osteoporotic Fractures in Men Study. Clin Orthop Relat Res. 2015 doi: 10.1007/s11999-015-4222-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015;473:1234–1246. doi: 10.1007/s11999-014-4038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Newton J, Seagroatt V. Why is osteoarthritis of the hip more common on the right? Lancet. 1993;341:179. doi: 10.1016/0140-6736(93)90045-i. [DOI] [PubMed] [Google Scholar]
- 43.Lederman R. An epidemiological and therapeutic multicenter study involving 3,309 patients with osteoarthritis. Eur J Rheumatol Inflamm. 1983;6:90–98. [PubMed] [Google Scholar]
- 44.van Saase JL, van Romunde LK, Cats A, Vandenbroucke JP, Valkenburg HA. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum Dis. 1989;48:271–280. doi: 10.1136/ard.48.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stea S, Bordini B, Viceconti M, Traina F, Cervini A, Toni A. Is laterality associated with a higher rate of hip arthroplasty on the dominant side? Artif Organs. 2008;32:73–77. doi: 10.1111/j.1525-1594.2007.00457.x. [DOI] [PubMed] [Google Scholar]
- 46.Tsitskaris K, Sharif K, Meacock LM, Bansal M, Ayis S, Li PL, et al. The prevalence of cam-type femoroacetabular morphology in young adults and its effect on functional hip scores. Hip Int. 2012;22:68–74. doi: 10.5301/HIP.2012.9074. [DOI] [PubMed] [Google Scholar]
- 47.Hack K, Di Primio G, Rakhra K, Beaule PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 48.McWilliams DF, Doherty SA, Jenkins WD, Maciewicz RA, Muir KR, Zhang W, et al. Mild acetabular dysplasia and risk of osteoarthritis of the hip: a case-control study. Ann Rheum Dis. 2010;69:1774–1778. doi: 10.1136/ard.2009.127076. [DOI] [PubMed] [Google Scholar]
- 49.Morvan J, Bouttier R, Mazieres B, Verrouil E, Pouchot J, Rat AC, et al. Relationship between hip dysplasia, pain, and osteoarthritis in a cohort of patients with hip symptoms. J Rheumatol. 2013;40:1583–1589. doi: 10.3899/jrheum.121544. [DOI] [PubMed] [Google Scholar]
- 50.Nepple JJ, Martel JM, Kim YJ, Zaltz I, Clohisy JC. Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clin Orthop Relat Res. 2012;470:3313–3320. doi: 10.1007/s11999-012-2510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.