Abstract
Background
Cardiopulmonary resuscitation (CPR) video self-instruction (VSI) materials have been promoted as a scalable approach to increase the prevalence of CPR skills among the lay public, in part due to the opportunity for secondary training (i.e., sharing of training materials). However, the motivations for, and barriers to, disseminating VSI materials to secondary trainees is poorly understood.
Methods
This work represents an ancillary investigation of a prospective hospital-based CPR education trial in which family members of cardiac patients were trained using VSI. Mixed-methods surveys were administered to primary trainees six months after initial enrollment. Surveys were designed to capture motivations for, and barriers to, sharing VSI materials, the number of secondary trainees with whom materials were shared, and the settings, timing, and recipients of trainings.
Results
Between 07/2012–05/2015, 653 study participants completed a six-month follow-up interview. Of those, 345 reported sharing VSI materials with 1455 secondary trainees. Materials were shared most commonly with family members. In a logistic regression analysis, participants in the oldest quartile (age > 63 years) were less likely to share materials compared to those in the youngest quartile (age ≤ 44 years, OR 0.58, CI 0.37–0.90, p=0.02). Among the 308 participants who did not share their materials, time constraints was the most commonly cited barrier for not sharing.
Conclusions
VSI materials represent a strategy for secondary dissemination of CPR training, yet older individuals have a lower likelihood of sharing relative to younger individuals. Further work is warranted to remedy perceived barriers to CPR dissemination among the lay public using VSI approaches.
Keywords: cardiopulmonary resuscitation, education, basic life support, cardiac arrest
Introduction
The provision of bystander cardiopulmonary resuscitation (CPR) has been associated with greater odds of survival from out-of-hospital cardiac arrest (OHCA),1 yet rates of bystander CPR remain low, with less than one-third of victims of OHCA receiving bystander CPR prior to EMS arrival in some communities.2 Studies suggest that previous receipt of CPR training may increase a bystander’s likelihood of initiating CPR.3–5 For example, in one study that interviewed witnesses of cardiac arrest events, investigators found that previously trained bystanders were more likely to initiate CPR compared to their untrained counterparts.5 To broaden the reach of CPR training—and thereby increase rates of bystander CPR provision—emerging research has underscored the need to employ innovative strategies to maximize dissemination of CPR training, especially among populations at high risk of witnessing a cardiac arrest.6–8
Despite efforts to increase CPR training rates among the lay public, barriers to learning CPR persist. One commonly cited obstacle is the perceived complexity of training materials; another is the high monetary and time costs associated with formal certification.9 In an attempt to mitigate these barriers, researchers have promoted the use of CPR video self-instruction (VSI) materials: low-cost, validated alternatives to traditional classroom instruction that increase the ease and retention of CPR training,10–12 and allow trainees to disseminate materials among their personal networks, a phenomenon known as “secondary training.”13,14 While numerous studies have examined the utility of these materials in terms of cost, ease of instruction, and degree of skills retention, relatively little research has explored secondary training after CPR training using the VSI approach, and—specifically—the motivations and barriers associated with secondary training activity among the lay public.
To address this knowledge gap, the objectives of the current study were twofold: (1) to identify the characteristics of the individuals most likely to share VSI materials; and (2) to characterize the motivations for, and barriers to, sharing VSI materials among individuals receiving primary CPR VSI training.
Methods
Study context
As an ancillary investigation associated with a multicenter, hospital-based CPR education trial, participants were surveyed regarding their use and dissemination of CPR VSI materials. The parent randomized prospective trial, formally known as the CPR Hospital-Initiated Project (CHIP) Study, trained adult family members of hospitalized patients with known cardiac disease or significant risk factors in hands-only CPR using a validated VSI kit (Family & Friends CPR Anytime, Laerdal Medical, Wappinger Falls, NY). Preliminary details of this trial are described elsewhere.13,14 In the trial protocol, participants were enrolled by student volunteers and hospital nursing staff on cardiac care units across eight hospitals in Southeastern Pennsylvania, and received VSI training before hospital discharge. Subsequent to this training, participants were encouraged to share their VSI materials with others. Six months after the initial training, participants were contacted to complete a short survey to solicit their perspectives on the study. Collection of these data and subsequent analyses were approved by the institutional review boards of the participating institutions in the multicenter trial (University of Pennsylvania, Albert Einstein Health Network, Temple University, Crozer-Keystone Health System, and the Chester County Hospital and Health System).
Data collection
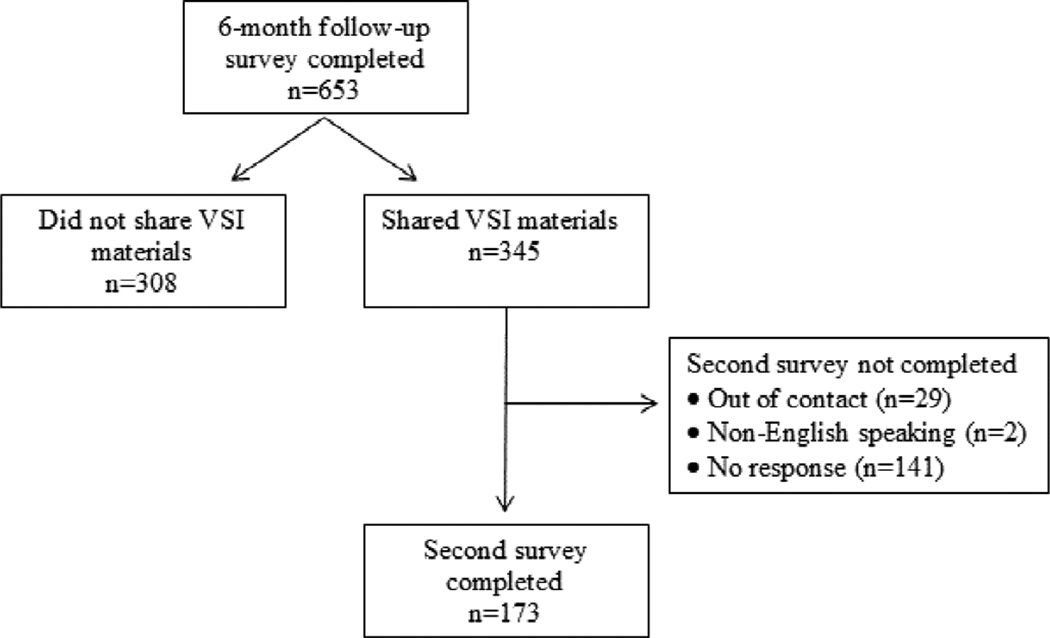
Participants that completed a six-month follow-up survey between 07/2012 and 05/2015 as part of the parent trial were eligible for inclusion in this ancillary investigation. Of the 653 participants successfully completing this follow-up survey, 345 reported sharing their VSI materials, while 308 reported not sharing (Figure 1). Demographics of those eligible for inclusion in this ancillary study were statistically indistinguishable from those of participants who were initially enrolled in the parent trial (data not shown). Following completion of the six-month survey, participants who reported sharing their materials were re-contacted by research assistants to complete a second survey over the telephone; of these, non-English speaking participants (n=2), and subjects with invalid or defunct contact information (n=29) were excluded. Among the 314 participants meeting these inclusion criteria, 173 (55%) successfully completed a second survey. The survey instrument used Likert-scale, multiple-choice, and open-response questions to capture participants’ motivations for, and perceived barriers to, sharing their VSI materials, the locations in which trainings were held, and the timing of trainings. Survey questions also queried the total number of individuals trained, and questions commonly received by participants from secondary trainees. Once collected, all data were stored and managed using a secure, internet-based application (REDCap Software Version 5.2.1, Vanderbilt University, Nashville, TN).
Figure 1.
Diagram of the subject inclusion criteria and survey completion.
Statistical approach and analysis
All Likert-scale and multiple-choice survey data were reported as proportions. Open-response data were independently coded in a computer spreadsheet program (Microsoft Excel 2010, Microsoft Corporation, Redmond, WA) by two members of the research team (DJI and DGB) using a grounded-theory approach,15 and presented according to underlying theme. Descriptive statistics of demographic covariates were tabulated and reported as number and frequency. Age was summarized as a mean with standard deviation (SD) and grouped into quartiles in subsequent regression analysis. The secondary training multiplier factor, defined as the number of secondary trainees instructed per VSI kit distributed, was calculated by dividing the total number of secondary trainees by the number of initial trainees, and reported as a cohort-wide (n=653) mean with SD. This approach is consistent with previous work on secondary training after CPR education.13,14,16–18 Student’s t and Pearson’s chi-squared tests were used to compare the prevalence of secondary training according to demographic covariates. Logistic regression analysis was then used to identify and quantify predictors of sharing, and results were reported as odds ratios (OR) with 95% confidence intervals (95% CI). All tests for significance were two-tailed, and an alpha level of 0.05 was used. All analyses were performed using Stata 12 (StataCorp, College Station, TX).
Results
Multiplier factor and likelihood of sharing
In our sample, 345 participants shared their materials with 1455 secondary trainees, corresponding to a cohort-wide average multiplier rate of 2.1 ± 4.9 (Table 1). The prevalence of secondary training did not vary significantly according to participants’ gender, race, level of education, previous CPR training, or relationship to the hospitalized patient. The average age of participants who shared, however, was significantly lower than those that did not share (51 ± 14 vs. 54 ± 14 years, p<0.01). In logistic regression analysis (Table 2), age quartile was a significant predictor of sharing, with participants in the oldest quartile (age > 63 years) having a decreased likelihood of sharing (OR 0.58, CI 0.37–0.90, p=0.02) compared to participants in the youngest quartile (age ≤ 44 years).
Table 1.
Demographics of six-month follow-up participants by sharing status
| Demographics | Shared? | p-value* | Surveyed (n=173) |
p-value† | |
|---|---|---|---|---|---|
| Yes (n=345) |
No (n=308) |
||||
| Average age ± SD, years | 51 ± 14 | 54 ± 14 | <0.01a | 52 ± 14 | 0.47a |
| Female gender, n (%) | 263 (76) | 226 (73) | 0.40b | 133 (77) | 0.82b |
| Race, n (%) | 0.43b | 0.46b | |||
| White | 181 (52) | 182 (59) | 97 (56) | ||
| Black | 137 (40) | 103 (33) | 64 (37) | ||
| Hispanic/Latino | 13 (4) | 12 (4) | 4 (2) | ||
| Other | 11 (3) | 7 (3) | 6 (4) | ||
| No response | 3 (1) | 4 (1) | 2 (1) | ||
| Highest education, n (%) | 0.19b | 0.02b | |||
| High school or less | 131 (38) | 95 (31) | 73 (42) | ||
| Some college | 83 (24) | 81 (26) | 47 (27) | ||
| College | 85 (25) | 82 (27) | 35 (20) | ||
| Graduate school | 44 (13) | 50 (16) | 16 (10) | ||
| No response | 2 (0) | 0 (0) | 2 (1) | ||
| Relationship to patient, n (%) | 0.32b | 0.67b | |||
| Spouse | 118 (34) | 121 (39) | 60 (34) | ||
| Immediate family | 151 (44) | 135 (44) | 72 (42) | ||
| Other | 72 (21) | 50 (16) | 38 (22) | ||
| No response | 4 (1) | 2 (1) | 3 (2) | ||
| Previous CPR training, n (%) | 0.27b | 0.94b | |||
| No | 158 (46) | 143 (46) | 80 (46) | ||
| Yes – within prior 2 years | 36 (10) | 18 (6) | 19 (10) | ||
| Yes – 2–5 years | 47 (14) | 36 (12) | 22 (13) | ||
| Yes – 6–10 years | 31 (9) | 33 (11) | 15 (9) | ||
| Yes – more than 10 years | 72 (21) | 77 (25) | 37 (22) | ||
| No response | 1 (0) | 1 (0) | 0 (0) | ||
| Average multiplier rate ± SD | 2.1 ± 4.9 | —— | —— | —— | |
SD, standard deviation;
Student’s t test;
Pearson’s chi-squared test;
yes shared vs. no shared;
yes shared vs. surveyed
Table 2.
Logistic regression results showing effects of age quartile on sharing status
| Variable | Unadjusted OR (95% CI) |
p-value |
|---|---|---|
| Age (years) | ||
| 18–44 | 1.00 (reference) | — |
| 44–54 | 0.76 (0.49–1.18) | 0.22 |
| 54–63 | 0.78 (0.50–1.19) | 0.25 |
| 63–89 | 0.58 (0.37–0.90) | 0.02 |
OR, odds ratio; CI, confidence interval
Motivations for sharing and not sharing
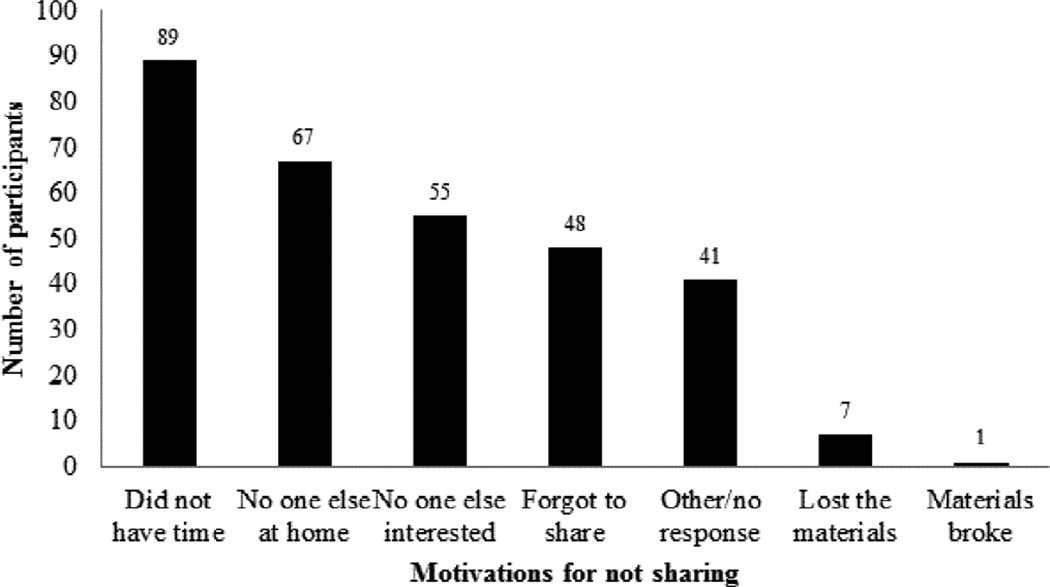
Among participants who shared, 96% reported feeling either “comfortable” or “very comfortable” sharing their VSI materials. Thematic analysis of answers to open-response survey questions revealed that the participants who shared VSI materials were motivated by “The power to save a life,” “The ability to help family members and friends with cardiac conditions,” and “The simplicity and portability of VSI materials” (Table 3). To assess why participants did not share their materials, we tabulated responses to the multiple-choice question, “If you did not share the CPR Anytime kit/DVD, what was the main reason?” Among the 308 participants who did not report sharing, the most common reasons for not sharing included perceived time constraints (89/308, 29%), the absence of any individuals with whom to share (67/308, 22%), and a lack of interest among potential secondary trainees (55/308, 18%) (Figure 2). No significant differences in the distribution of motivations for not sharing were found when stratified according to demographic covariates (data not shown).
Table 3.
Representative quotations regarding motivations for sharing (n=173)
| Theme | In your words, what motivated you to share the VSI materials with others? |
|---|---|
| The power to save a life | “Being able to say that you could do something and not be helpless. It was eye-opening to know all you had to do was keep the heart moving even if you didn’t know to do the breathing. It can save lives.” |
| “I wanted people to know that training was available and that they could help people.” | |
| “The idea that I could help save a life and figured that the more people who know, the better.” | |
| The ability to help a family member or friend with cardiac conditions | “My wife had just recently got a diagnosis of cardiac issues and there was the possibility I’d have to use it.” |
| “I trained the people in my house so I wouldn’t be the only one to know what to do in case something were to happen to my dad.” | |
| “I have a 12 year-old daughter and I want her to know how to be calm in case of emergency and how to help me if something happened to me. She’d be the one in charge after me so I also wanted her to know how to help her little brother.” | |
| The simplicity and portability of VSI materials | “It seemed very simple; everyone should know how to do it.” |
| “The materials were small, easy to transport, different from other CPR trainings.” | |
| “It’s very easy to take out and show people.” |
VSI, video self-instruction; CPR, cardiopulmonary resuscitation
Figure 2.
Graph displaying subject’s motivations for not sharing the CPR training materials.
Characteristics of secondary trainings
Among the sample (n=173) of participants who completed a second survey (Table 4), the majority reported that the most common recipients of their VSI materials were family members, although some reported sharing their materials with groups as diverse as friends, coworkers, and fellow congregants. The majority of secondary trainings occurred in the home (85%), with 7% of trainings occurring in the workplace, and a combined 8% of trainings occurring elsewhere. Educational materials were most commonly shared by participants within 4 weeks of the initial in-hospital training (70%). 100 (58%) participants reported receiving questions about CPR from secondary trainees. The most common questions reported by participants in response to the prompt, “Please describe the questions you received,” included “Why are there no breaths?” (27% of participants), “How hard does one compress?” (20%), and “How fast does one compress?” (17%).
Table 4.
Characteristics of secondary trainings (n=173)
| Characteristics* | |
|---|---|
| Location of trainings, n (%)† | |
| School | 2/181 (1) |
| Church/place of worship | 4/181 (2) |
| Community/civic center | 4/181 (2) |
| Home | 153/181 (85) |
| Assisted living facility | 5/181 (3) |
| Work | 12/181 (7) |
| Other | 1/181 (0) |
| Secondary trainees, n (%) | |
| Family | 151/173 (88) |
| Friends | 10/173 (6) |
| Coworkers | 10/173 (6) |
| Other | 2/173 (0) |
| Time of sharing after initial enrollment, n (%)‡ | |
| 0–1 months | 124/177 (70) |
| 1–2 months | 28/177 (16) |
| 3–6 months | 17/177 (10) |
| 7–12 months | 6/177 (3) |
| >12 months | 2/177 (1) |
| Questions received by trainers, n (%) | |
| “Why no breaths?” | 27/100 (27) |
| “How hard to press?” | 20/100 (20) |
| “How fast to press?” | 17/100 (17) |
| “Where to place hands?” | 11/100 (11) |
| “Will it hurt victim/will I be sued?” | 7/100 (7) |
| “How long to continue?” | 6/100 (6) |
| “Difference between adult and child or infant?” | 6/100 (6) |
| Don’t remember | 6/100 (6) |
Denominators included to represent missing data;
Some participants reported more than one training location;
Some participants reported more than one time of sharing
Discussion
In this ancillary investigation of a hospital-based multicenter trial of VSI education, we examined the phenomenon of secondary training in a cohort of family members of high-risk cardiac patients. In particular, we found that 345 participants shared their VSI materials with a total of 1455 secondary trainees, corresponding to a cohort-wide average multiplier rate of 2.1 ± 4.9. Older age was the only demographic characteristic found to be predictive of sharing in this cohort, with participants in the oldest quartile having a significantly lower likelihood of sharing relative to those in the youngest quartile. Participants who shared their VSI materials were most commonly motivated by “the power to save a life,” while participants who did not share were most commonly deterred by perceived time constraints. Compared to previous VSI dissemination studies that have examined largely homogenous samples using quantitative evaluative frameworks, the current work extends the generalizability of these studies in its application of a mixed-methods approach to a heterogeneous sample and is, to our knowledge, the first such study to do so.
The results of the current study confirm findings from previous work that have shown the relative ease with which VSI materials—and, by extension, CPR skills—can be disseminated among the lay public.13,14,16–22 Our finding of a 2.1 ± 4.9 average multiplier rate is in line with estimates from similar studies that have calculated rates as low as 1.8 in a sample of Italian secondary school students,19 and as high as 3.1 in a sample of American caregivers of high-risk infants.21 That these materials have been shown, in diverse contexts, to be highly disseminable further reinforces their import in population-level initiatives to increase the prevalence of CPR training among the lay public, with initial trainees acting comfortably as “ambassadors” of layperson CPR training in their personal networks.17 However, given our finding that perceived time constraints constitutes a common barrier to VSI dissemination among primary trainees, additional work is needed to explore how novel CPR training modalities—such as mobile applications23–25 and so-called “ultrabrief” curricula26—may lessen this barrier and encourage wider VSI dissemination among layperson trainees. In contrast to a related study that assessed skills proficiency among secondary trainees and deemed it “very satisfactory,”17 this study does not offer an “objective” assessment of participants’ competency as trainers. That questions about CPR commonly arose among trainees even after receipt of secondary training in our cohort further suggests that refinement of VSI may be indicated to provide laypersons the adequate tools—and infrastructure—to effectively address secondary trainees’ concerns without need for certified instructors.
Although existing evidence has shown that many of the barriers associated with CPR training and the willingness to perform bystander CPR are lessened through provision of VSI materials, critical uncertainties still remain. For example, given the relatively brief follow-up period of the parent trial, we could not assess the association of rates of VSI dissemination with rates of bystander CPR delivery among secondary trainees. Although a landmark study by Isbye et al. found that the dissemination of 35,000 CPR VSI materials in Denmark did not significantly improve rates of bystander CPR delivery,22 it is important to note that investigators distributed materials to schoolchildren between the ages of 12 and 14, a population that is not at particularly high risk of witnessing a cardiac arrest. Because VSI materials in this study were distributed to family members of cardiac patients—and, in turn, shared with additional family members of these patients—it is not unreasonable to hypothesize that a “saturation” of high-risk cardiac patients’ immediate networks with CPR training may have led to a higher than expected prevalence of bystander CPR in this cohort. Future work with adequate statistical power and long-term follow up will be needed to test the veracity of this hypothesis.
Previous research has explored the cost-effectiveness of formal certification courses.27,28 To our knowledge, however, no systematic work to date has explored whether the phenomenon of secondary training—with its well-documented multiplier effect and lack of need for credentialed, often paid instructors—confers further cost savings. Results from our previous work suggest that provision of chest compression-only CPR curricula—in contrast to standard CPR curricula—is associated with higher rates of secondary training and may, correlatively, be associated with lower costs.14 Though no formal analysis is included here, it is therefore plausible that dissemination of CPR VSI materials to family members and friends of high-risk patients represents a highly cost-effective means by which to maximize CPR awareness and skills among the general population.27 Further work is needed to assess the validity of this proposition and its public health implications on a broader scale.
That older participants in this cohort were less likely to share their VSI materials with additional individuals compared to younger participants is a significant finding of the current work, and suggests that CPR VSI materials may require further tailoring to appeal to older individuals. It is well understood that individuals in the seventh decade of life constitute the demographic most likely to suffer a cardiac arrest,2 and that, for most of these individuals, a spouse of similar age is the individual most likely to witness the arrest.29 Despite its comparatively high risk of witnessing a cardiac arrest, however, this population is also one of the least likely to be trained in CPR, thus creating a “mismatch” between those individuals who are most often targeted for training, and those individuals who would be most likely to use the training.17 Therefore, it is important to examine not only this population’s attitudes and self-efficacy regarding CPR and VSI, but additionally how educational initiatives and materials may be further refined to reach this high-risk group.30
Limitations
As a survey study, this investigation has several noteworthy limitations. First, because all surveys were administered at least six months after subjects’ initial enrollment, it is possible that our results—especially those obtained through open-response questions—were attenuated by recall bias. Second, as the parent trial employed a relatively brief follow-up period, the association of secondary training with bystander CPR delivery could not be rigorously assessed. Third, as participants in the parent trial were all family members of cardiac patients, data regarding their motivations and perceived barriers to VSI dissemination may not be generalizable to all laypersons that are trained in CPR using VSI approaches. Fourth, it is plausible that our results—owing to self-selection bias subsequent to non-random sampling—are not representative of all participants of the parent study who shared their materials. Based on our analysis of participants’ demographics, however, we find that our sample is, with the exception of education, approximately representative of the parent cohort.
Conclusion
Secondary training using VSI constitutes a phenomenon that was highly prevalent, and comfortably facilitated, among laypersons participating in a hospital-based CPR education trial. As older individuals are less likely to share these materials relative to younger individuals, further work is needed to understand how VSI approaches—and barriers to their dissemination—can be addressed to increase CPR training prevalence among this population, as well as others at high risk of witnessing a cardiac arrest.
Acknowledgments
Ms. Leary has received research support from the Laerdal Foundation and the American Heart Association, as well as in-kind support from Laerdal Medical and Physio-Control. Dr. Abella has received research support and honoraria from Philips Healthcare, in-kind research support from Laerdal Medical, and research support from the Medtronic Foundation. Ms. Blewer has received research support from the American Heart Association.
The authors wish to thank the student volunteers and nurses whose dedication to, and insights surrounding, cardiac patients and their families were integral to the completion of this study. This work was supported by a grant from the National Institutes of Health (R18HL107217).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
None of the remaining authors report conflicts of interest.
References
- 1.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 2.Chan PS, McNally B, Tang F, Kellermann A CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;130:1876–1882. doi: 10.1161/CIRCULATIONAHA.114.009711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coons SJ, Guy MC. Performing bystander CPR for sudden cardiac arrest: behavioral intentions among the general adult population in Arizona. Resuscitation. 2009;80:334–340. doi: 10.1016/j.resuscitation.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 4.Dwyer T. Psychological factors inhibit family members' confidence to initiate CPR. Prehosp Emerg Care. 2008;12:157–161. doi: 10.1080/10903120801907216. [DOI] [PubMed] [Google Scholar]
- 5.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13:596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 6.Sasson C, Meischke H, Abella BS, Berg RA, Bobrow BJ, Chan PS, Root ED, Heisler M, Levy JH, Link M, Masoudi F, Ong M, Sayre MR, Rumsfeld JS, Rea TD American Heart Association Council on Quality of Care and Outcomes Research, Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Clinical Cardiology, and Council on Cardiovascular Surgery and Anesthesia. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–1350. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 7.Anderson ML, Cox M, Al-Khatib SM, Nichol G, Thomas KL, Chan PS, Saha-Chaudhuri P, Fosbol EL, Eigel B, Clendenen B, Peterson ED. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhanji F, Mancini ME, Sinz E, Rodgers DL, McNeil MA, Hoadley TA, Meeks RA, Hamilton MF, Meaney PA, Hunt EA, Nadkarni VM, Hazinski MF. Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S920–S933. doi: 10.1161/CIRCULATIONAHA.110.971135. [DOI] [PubMed] [Google Scholar]
- 9.Abella BS, Aufderheide TP, Eigel B, Hickey RW, Longstreth WT, Jr, Nadkarni V, Nichol G, Sayre MR, Sommargren CE, Hazinski MF American Heart Association. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–709. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 10.Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30-min video self-training: a controlled randomized study. Resuscitation. 2007;74:476–486. doi: 10.1016/j.resuscitation.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 11.Lynch B, Einspruch EL, Nichol G, Becker LB, Aufderheide TP, Idris A. Effectiveness of a 30-min CPR self-instruction program for lay responders: a controlled randomized study. Resuscitation. 2005;67:31–43. doi: 10.1016/j.resuscitation.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 12.Potts J, Lynch B. The American Heart Association CPR Anytime Program: the potential impact of highly accessible training in cardiopulmonary resuscitation. J Cardiopulm Rehabil. 2006;26:346–354. doi: 10.1097/00008483-200611000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Blewer AL, Leary M, Decker CS, Andersen JC, Fredericks AC, Bobrow BJ, Abella BS. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: a feasibility trial. J Hosp Med. 2011;6:428–432. doi: 10.1002/jhm.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blewer AL, Leary M, Esposito EC, Gonzalez M, Riegel B, Bobrow BJ, Abella BS. Continuous chest compression cardiopulmonary resuscitation training promotes rescuer self-confidence and increased secondary training: a hospital-based randomized controlled trial*. Crit Care Med. 2012;40:787–792. doi: 10.1097/CCM.0b013e318236f2ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Starks H, Trinidad SB. Choose your method: a comparison of phenomenology, discourse analysis, and grounded theory. Qual Health Res. 2007;17:1372–1380. doi: 10.1177/1049732307307031. [DOI] [PubMed] [Google Scholar]
- 16.Pierick TA, Van Waning N, Patel SS, Atkins DL. Self-instructional CPR training for parents of high risk infants. Resuscitation. 2012;83:1140–1144. doi: 10.1016/j.resuscitation.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Lorem T, Steen PA, Wik L. High school students as ambassadors of CPR--a model for reaching the most appropriate target population? Resuscitation. 2010;81:78–81. doi: 10.1016/j.resuscitation.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 18.Lorem T, Palm A, Wik L. Impact of a self-instruction CPR kit on 7th graders' and adults' skills and CPR performance. Resuscitation. 2008;79:103–108. doi: 10.1016/j.resuscitation.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 19.Corrado G, Rovelli E, Beretta S, Santarone M, Ferrari G. Cardiopulmonary resuscitation training in high-school adolescents by distributing personal manikins. The Como-Cuore experience in the area of Como, Italy. J Cardiovasc Med (Hagerstown) 2011;12:249–254. doi: 10.2459/JCM.0b013e328341027d. [DOI] [PubMed] [Google Scholar]
- 20.de Paiva EF, Padilha Rde Q, Sgobero JK, Ganem F, Cardoso LF. Disseminating cardiopulmonary resuscitation training by distributing 9,200 personal manikins. Acad Emerg Med. 2014;21:886–891. doi: 10.1111/acem.12423. [DOI] [PubMed] [Google Scholar]
- 21.Knight LJ, Wintch S, Nichols A, Arnolde V, Schroeder AR. Saving a life after discharge: CPR training for parents of high-risk children. J Healthc Qual. 2013;35:9–16. doi: 10.1111/j.1945-1474.2012.00221.x. quiz17. [DOI] [PubMed] [Google Scholar]
- 22.Isbye DL, Rasmussen LS, Ringsted C, Lippert FK. Disseminating cardiopulmonary resuscitation training by distributing 35,000 personal manikins among school children. Circulation. 2007;116:1380–1385. doi: 10.1161/CIRCULATIONAHA.107.710616. [DOI] [PubMed] [Google Scholar]
- 23.Semeraro F, Taggi F, Tammaro G, Imbriaco G, Marchetti L, Cerchiari EL. iCPR: a new application of high-quality cardiopulmonary resuscitation training. Resuscitation. 2011;82:436–441. doi: 10.1016/j.resuscitation.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 24.Lee JS, Jeon WC, Ahn JH, Cho YJ, Jung YS, Kim GW. The effect of a cellular-phone video demonstration to improve the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation as compared with audio coaching. Resuscitation. 2011;82:64–68. doi: 10.1016/j.resuscitation.2010.09.467. [DOI] [PubMed] [Google Scholar]
- 25.Ahn JY, Cho GC, Shon YD, Park SM, Kang KH. Effect of a reminder video using a mobile phone on the retention of CPR and AED skills in lay responders. Resuscitation. 2011;82:1543–1547. doi: 10.1016/j.resuscitation.2011.08.029. [DOI] [PubMed] [Google Scholar]
- 26.Bobrow BJ, Vadeboncoeur TF, Spaite DW, Potts J, Denninghoff K, Chikani V, Brazil PR, Ramsey B, Abella BS. The effectiveness of ultrabrief and brief educational videos for training lay responders in hands-only cardiopulmonary resuscitation: implications for the future of citizen cardiopulmonary resuscitation training. Circ Cardiovasc Qual Outcomes. 2011;4:220–226. doi: 10.1161/CIRCOUTCOMES.110.959353. [DOI] [PubMed] [Google Scholar]
- 27.Groeneveld PW, Owens DK. Cost-effectiveness of training unselected laypersons in cardiopulmonary resuscitation and defibrillation. Am J Med. 2005;118:58–67. doi: 10.1016/j.amjmed.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Bouland AJ, Risko N, Lawner BJ, Seaman KG, Godar CM, Levy MJ. The Price of a Helping Hand: Modeling the Outcomes and Costs of Bystander CPR. Prehosp Emerg Care. 2015;19:524–534. doi: 10.3109/10903127.2014.995844. [DOI] [PubMed] [Google Scholar]
- 29.Swor RA, Jackson RE, Walters BL, Rivera EJ, Chu KH. Impact of lay responder actions on out-of-hospital cardiac arrest outcome. Prehosp Emerg Care. 2000;4:38–42. doi: 10.1080/10903120090941623. [DOI] [PubMed] [Google Scholar]
- 30.Panchal AR, Fishman J, Camp-Rogers T, Starodub R, Merchant RM. An "Intention-Focused" paradigm for improving bystander CPR performance. Resuscitation. 2015;88:48–51. doi: 10.1016/j.resuscitation.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]