Abstract
Purpose
to determine if asymmetry between hips in pain or radiographic osteoarthritis (RHOA) is associated with worse pain and joint space narrowing (JSN) at baseline and longitudinally in knees contralateral to more affected hips.
Methods
We studied 279 participants in the Osteoarthritis Initiative with baseline asymmetry between hips in pain and 483 with asymmetry in RHOA none of whom had a hip replacement for ≥4 years after baseline. RHOA assessed from pelvis radiographs was categorized as none, possible or definite and hip pain on most days of a month in the past year as present/absent. Knee pain (WOMAC scale) and JSN (fixed flexion radiographs) were categorized as none, mild and moderate-severe. We compared knees contralateral and ipsilateral to more affected hips on baseline knee pain and JSN using clustered multinomial regression and on change in knee pain and JSN over 4–5 years using generalized linear and logistic estimating equations.
Results
Knees contralateral to painful hips had less baseline pain (“moderate-severe” vs. “none”, relative risk ratio [RRR]: 0.39, 95% CI = 0.27–0.57), but greater baseline JSN (“moderate-severe” vs. “none”, RRR: 1.62, 95% CI = 1.09–2.38) and greater worsening of pain during follow-up (p = 0.001). Knees contralateral to hips with worse RHOA had nonsignificant trends for greater baseline JSN (p = 0.10) and JSN progression (p = 0.17).
Conclusion
These findings provide limited support for the hypothesis that early asymmetry in hip pain and RHOA is associated with worse pain and structural outcomes in knees contralateral to the more affected hip.
Introduction
Osteoarthritis (OA) is a common and debilitating disease, and the most frequent reason for hip and knee replacement.[1] While OA in the hip and knee often occur together,[2, 3] few studies have investigated how disease in one lower extremity joint affects OA in other lower extremity joints.[3, 4] Lower extremity biomechanical abnormalities are risk factors for OA in both the hip and knee.[5–8] It is possible that OA or pain in either joint can alter the hip-knee-ankle kinetic chain in a way that influences the risk of both symptoms and structural changes in the other lower extremity joints.[9–17]
Individuals undergoing total hip replacement (THR) for advanced hip OA have an increased risk of subsequent total knee replacement (TKR) in the knee contralateral to the replaced hip,[18] which may result from asymmetric movement adaptations that increase mechanical loading in the contralateral knee both before and after a unilateral THR.[13, 19] We recently reported that a prevalent unilateral THR is associated with greater severity and increased progression of knee symptoms and structural damage assessed by MRI in the knee contralateral to the replaced hip[20]. Thus unilateral advanced hip OA requiring joint replacement is associated with an increased risk of poor knee OA structural and clinical outcomes in the opposite limb, and this may have potentially modifiable biomechanical causes. To our knowledge, no studies have examined whether asymmetries in symptoms and structural damage between native hips with less advanced OA well prior to THR are associated with a greater risk of pain and structural damage in knees contralateral to the more affected hip joint compared with the ipsilateral knee. Such studies could help determine the need for preventive interventions in persons who are in the earlier stages of developing hip OA that manifests asymmetrically.
This study evaluates data from the Osteoarthritis Initiative (OAI) to determine if individuals at a relatively early stage of disease with asymmetry in hip pain or RHOA between hips had worse pain and structural outcomes at baseline and longitudinally in the knee contralateral to the more affected hip compared to the ipsilateral knee.
Methods
Subjects
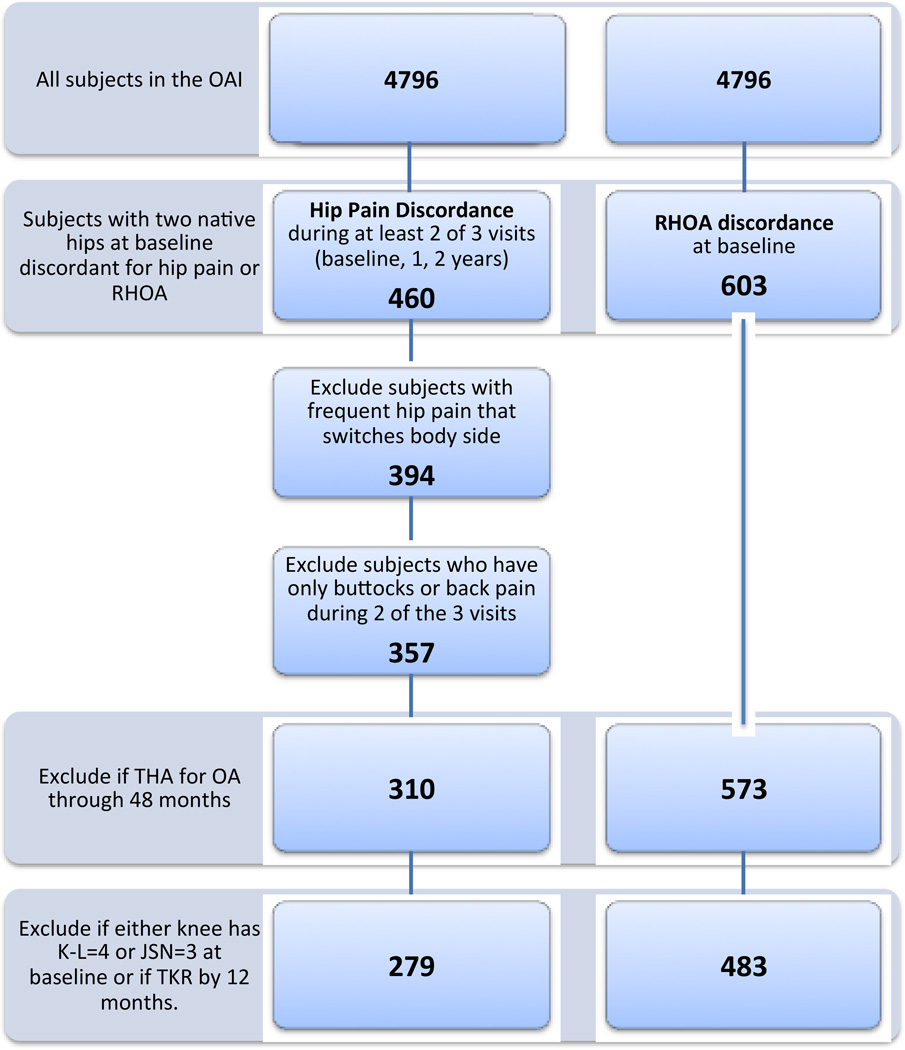
Subjects were participants in the OAI, a multi-center longitudinal study of the natural history, risk factors and biomarkers for hip and knee OA with yearly clinic visits and interviews (http://www.oai.ucsf.edu/). The study was approved by the institutional review boards at the four participating clinical centers and all participants gave written informed consent. Using a paired-limb design, we studied subjects with two native hips that had different degrees of radiographic OA at baseline and subjects who had unilateral frequent hip pain from baseline through 24 months. In order to focus on less advanced hip disease well prior to joint replacement, we excluded those who had a THR for any reason from baseline through 48 months. We also excluded those who already had advanced radiographic knee OA at baseline (K-L grade 4 OA or JSN grade 3) or a TKR at baseline or 12 months in either knee. A flowchart of the subject selection is shown in Figure 1.
Figure 1. Subject selection flowchart.
Note that hip pain is defined as “hip pain on more than half the days of the month in the past 12 months”. K-L grade = Kellgren Lawrence grade.
Radiographic Hip OA Assessment
Hip and knee radiographs were acquired as part of the OAI using standardized acquisition and quality assurance protocols, which are available at www.oai.ucsf.edu. Participants had weight-bearing pelvis radiographs at baseline and 48 months at a 40-inch film-to-focus distance with feet placed in 20 degrees internal rotation using a positioning frame. Radiographs were assessed for individual radiographic features (IRF) of OA using the OARSI atlas and grades[21] by two musculoskeletal radiologists (TML, PMJ) and a rheumatologist (NEL). Prior to reading, baseline, and when available, 48 month radiographs of 4,761 participants were screened by one reader for the presence of hip osteophytes or JSN. Those without either finding were categorized as “negative screen” and viewed by a second reader. If confirmed negative by the second reader radiographs were not evaluated further. The radiographs of 1,441 (30%) participants who screened positive for hip OA findings were independently scored for IRFs by two readers. Disagreements between readers for the presence of superolateral or supermedial JSN, femoral or acetabular osteophytes, cysts, sclerosis or femoral head deformity were adjudicated by agreement of at least 2 of the 3 readers.
Femoral and acetabular osteophytes and superolateral and superomedial JSN with grade ≥2 were considered definite. Hips were classified as “definite RHOA” when: a) the modified Croft grade was ≥2 (presence of two or more of definite osteophytes, definite JSN, sclerosis, cysts or deformity); b) there were grade ≥1 femoral or grade ≥2 acetabular osteophytes plus definite JSN; c) there were grade ≥2 femoral osteophytes regardless of other features; or d) when there was superolateral JSN ≥2 or superomedial JSN≥3 regardless of other features. Hips were classified as “possible RHOA” when other individual, or combinations of, indefinite IRFs were present (e.g. grade 1 osteophytes or grade 1 JSN), and otherwise considered “normal”. [22, 23]
RHOA asymmetry was defined as having a different grade of RHOA (“definite,” “possible” or “normal”) in each hip at baseline.
Radiographs of 140 randomly selected hips that were screened negative for RHOA were blindly read for IRFs using the study protocol. The specificity of screening for the absence of definite RHOA was 99.2%, and the estimated sensitivity for definite RHOA was 93%. Radiographs of a random sample of 197 participants were blindly fed back to the readers for a repeat IRF reading. Test-retest reliability was generally good for medial and lateral JSN (weighted kappas: 0.74 to 0.77), superior and inferior femoral osteophytes (0.74 to 0.79), acetabular osteophytes (0.51 to 0.64), cysts, sclerosis or deformity (0.53 to 0.55), the 3 level summary classification (0.72) and definite OA vs not definite (kappa: 0.73).
Hip Pain and THR Assessment
Hip pain was assessed at annual clinic visits and mailed questionnaires from baseline through 60 months. Participants viewed a diagram showing the usual locations of OA-related hip pain[24, 25] and asked whether they had “pain, aching or stiffness in the hip on most days of a month” during the past year.[26] Those who said ‘Yes’ were considered to have frequent hip pain and asked to indicate on the diagram where the pain occurred: groin, front of the leg (anterior), outside of leg (lateral), low back or buttocks. We excluded subjects with pain in either hip that was only in the low back/buttocks, since this may be misclassified as emanating from structures in the hip region.[27, 28]
Hip pain asymmetry was defined as having unilateral frequent hip pain at baseline. Because OA pain fluctuates over time, persistent pain asymmetry required that one hip had frequent pain for at least two of three time-points from baseline through 24 months and the other hip did not have frequent pain. Participants whose painful side alternated between visits were excluded.
THRs were self-reported annually and confirmed from medical records and study radiographs.
Knee JSN and Knee Symptoms
Fixed flexion knee radiographs were obtained at baseline and yearly follow-up visits and read for progression of JSN from baseline to year 4 with good reliability, as previously described. [29, 30] Test-retest reliability for JSN progression was good to excellent (medial JSN progression, κ=0.0.72 (0.63–0.82); lateral JSN progression, κ=0.83(0.70–0.96). Knee pain was assessed at baseline and yearly using the WOMAC knee pain subscale [31]
Statistical Analysis
Contralateral knees were defined as opposite the hip with unilateral frequent pain and separately as opposite the hip with a higher grade of RHOA. For cross-sectional analyses, baseline WOMAC knee pain and JSN were grouped into 3 levels of severity. Due to the large proportion of knees with baseline WOMAC pain scores of 0, knee pain scores were categorized based on the overall distribution, with 0 as “none” and the remaining knees subdivided into "mild" and "moderate - severe" categories at the 50th percentile score of the remaining knees. Knee pain scores of 1–3 were classified as mild and scores ≥4 classified as moderate-severe. Baseline JSN groups were defined as grades 0, 1 and 2. We compared knee pain and JSN (outcomes) in contralateral vs. ipsilateral knees (predictor) using clustered multinomial regression models, since proportional odds assumptions were not met for pain and JSN outcomes.
For longitudinal analyses, we compared knees for change in WOMAC pain score as a continuous variable and change in JSN as a dichotomous variable (yes/no). We categorized JSN as progressing if either the medial or lateral compartment increased in score (including within grade changes) [29] at any timepoint up to 48 months compared to baseline. If a knee was replaced after 24 months JSN was categorized as progressing, while pain scores were treated as missing from that point on. We used generalized linear models to compare annual pain data from baseline to 60 months between knees. To analyze JSN progression we used logistic regression with generalized estimating equations. To evaluate whether the degree of contrast in RHOA grades between limbs (normal/possible; possible/definite, normal/definite) was associated with knee outcomes, we used clustered multinomial logistic regression.
Comparisons between knees are within-subject, so all statistical models account for paired and correlated limbs within an individual and do not include subject-level covariates. When unilateral hip pain defined the sample, we included baseline RHOA status (normal/possible/definite) and 12-month knee K-L grade as limb-specific covariates. When RHOA asymmetry defined the sample, we included baseline hip pain (yes/ no) and baseline knee K-L grade as limb-specific covariates. For baseline knee JSN outcomes we did not adjust for baseline knee K-L grade due to the collinearity between these variables.
In cross-sectional and longitudinal sensitivity analyses we excluded a small number of subjects with advanced RHOA at baseline, as indicated by a baseline hip JSN grade of 3 (n=8 for pain asymmetry and n=6 for RHOA asymmetry). Separately, we excluded subjects with extreme baseline asymmetry between knees in OA severity (i.e. a K-L grade of 0–1 in one knee and grade 3 in the other knee; n=23 for pain and n=35 for RHOA asymmetry). Finally, we performed two additional sensitivity analyses. First, we repeated our main analyses limited to those with definite OA in one hip and normal or possible in the other, excluding those with one normal hip and the other with possible RHOA. Second, to test whether a more extreme contrast in pain between hips would show larger differences in outcomes between ipsilateral and contralateral knees, we repeated our analyses for unilateral hip pain excluding subjects (n=55) in the unilateral hip pain sample who reported “any” pain in their contralateral hip at ≥2 of the first 3 visits. Our results and conclusions were materially unchanged in these analyses.
Results
Subject Characteristics
There were 279 individuals with unilateral hip pain and 483 with asymmetric RHOA. Those with asymmetric RHOA had the following combinations: Normal/Possible (n=262); Possible/Definite (n=147); and Normal/Definite (n=74). In the unilateral hip pain sample, baseline RHOA status did not differ between contralateral and ipsilateral limbs, and among those with RHOA asymmetry the prevalence of hip pain at baseline was similar between limbs (Table 1). Only 42 persons had asymmetry in both RHOA and hip pain; of these 25 had pain in the hip with worse RHOA compared to 17 with pain in the hip with less severe RHOA (odds ratio: 1.47; (95% CI: 0.76, 2.90)).
Table 1.
Subject Characteristics and Hip and Knee Characteristics of Participants with Unilateral Hip Pain and Participants with Asymmetric Radiographic Hip OA (RHOA)
| Baseline&
Subject Characteristic |
Unilateral Hip Pain (n=279) |
Asymmetric RHOA (n=483) | ||
| Age yrs, median(IQR) # | 61 (54–70) | 63 (54–70) | ||
| BMI, mean (IQR) kg/m2 | 27.7 (24.3–31.1) | 27.7 (24.6–30.8) | ||
| Female, n (%) | 195 (69.9) | 232 (48.0) | ||
| Baseline&
Hip and Knee Characteristic |
Limbs with Hip Pain |
Contralateral Limbs* |
Limbs with worse RHOA |
Contralateral Limbs** |
| Radiographic hip OA, n (%) | ||||
| Normal | 198 (77.7) | 194 (76.1) | 0 (0.0) | 336 (69.6) |
| Possible | 35 (13.7) | 38 (14.9) | 262 (54.2) | 147 (30.4) |
| Definite | 22 (8.63) | 23 (9.0) | 221 (45.8) | 0 (0) |
| Hip pain on most days of month, n (%) | 279(100.0) | 0 (0.0) | 88 (18.3) | 79 (16.4) |
| Knee pain (WOMAC 0–20), median (IQR) | 1 (0–4) | 2 (0–5) | 1 (0–4) | 1 (0–4) |
| Knee K-L grade, n (%) | ||||
| 0 | 129 (46.2) | 126 (45.2) | 185 (38.3) | 178 (36.9) |
| 1 | 41 (14.7) | 51 (18.3) | 92 (19.1) | 93 (19.3) |
| 2 | 63 (22.6) | 62 (22.2) | 141 (29.2) | 133 (27.5) |
| 3 | 46 (16.5) | 40 (14.3) | 65 (13.5) | 79 (16.4) |
| Knee JSN (maximum of medial and lateral) | ||||
| 0 | 167 (59.9) | 178 (63.8%) | 276 (57.1%) | 265 (54.8%) |
| 1 | 70 (25.1%) | 66 (23.7%) | 142 (29.4%) | 139 (28.8%) |
| 2 | 42 (15.1% | 35 (12.5%) | 65 (13.5%) | 79 (16.4%) |
Baseline characteristics for the unilateral hip pain sample are from 12-month contacts since pain asymmetry was defined over 3 visits from baseline to 24 months
IQR – interquartile range; BMI = body mass index; JSN = joint space narrowing
An individual’s contralateral knee and hip are opposite the side with hip pain.
An individual’s contralateral knee and hip are opposite the side with worse RHOA.
Baseline Cross-sectional Comparison between Contralateral and Ipsilateral Knees
Unilateral baseline hip pain
Unilateral hip pain was associated with significantly less moderate-severe baseline pain in the contralateral compared to the ipsilateral knee (Table 3). The adjusted relative risk ratio (RRR) [32] for moderate-severe pain in the contralateral knee was 0.39 (95% CI: 0.27, 0.57). In contrast, the contralateral knee had a greater risk of moderate (grade 2) vs. no baseline JSN than the ipsilateral knee, with an adjusted RRR of 1.62 (1.09, 2.38) (Table 3).
Table 3.
Cross-sectional Association of Asymmetric Radiographic Hip OA (RHOA) with Baseline Knee Pain and Knee Joint Space Narrowing (JSN) in the Contralateral vs. Ipsilateral Knee.
| Outcome | RRR* (95% CI) [p-value] for outcome in the Contralateral vs. Ipsilateral Knee** |
|
|---|---|---|
| WOMAC Knee Pain | Unadjusted | Adjusted for hip pain and knee K-L Grade |
| Mild vs. No Pain | 1.28 (0.98, 1.67) [0.06] |
1.28 (0.98, 1.67) [0.07] |
| Severe vs. No Pain | 1.12 (0.90, 1.40) [0.28] |
1.15 (0.89, 1.48) [0.26] |
| Knee JSN | Unadjusted | Adjusted for hip pain |
| Mild (1) vs. No JSN (0) | 1.02 (0.82, 1.26) [0.86] |
1.03 (0.82, 1.27) [0.82] |
| Moderate [52] vs. No JSN (0) | 1.27 (0.95, 1.68) [0.11] |
1.27 (0.95, 1.68) [0.10] |
Relative risk ratios [32] and 95% confidence intervals (CI) estimated from clustered multinomial regression models.
An individual’s contralateral and ipsilateral knees are identified in relation to the limb with more severe RHOA.
Asymmetric baseline RHOA
There were no significant association between asymmetric baseline RHOA and baseline WOMAC knee pain categories (Table 2). There was a nonsignificant trend (p=0.07) for mild vs. no pain in the contralateral knee, but no similar trend was observed for moderate-severe pain vs. no pain. There were also no significant differences in baseline JSN severity between contralateral and ipsilateral knees (Table 2), although there was a nonsignificant trend (p=0.10) for an increased risk of moderate (grade 2) vs. no JSN in the contralateral knee. Overall, the degree of RHOA asymmetry between hips (normal vs. possible, possible vs. definite, normal vs. definite) was not associated with differences in pain severity (p = 0.27) or JSN severity (p = 0.23) between knees (data not shown).
Table 2.
Cross-sectional Association of Unilateral Hip Pain with Baseline Knee Pain and Joint Space Narrowing (JSN) in the Contralateral vs. Ipsilateral Knee.
| Outcome | RRR* (95% CI) [p-value] for outcome in the Contralateral vs. Ipsilateral Knee** |
|
|---|---|---|
| WOMAC Knee Pain | Unadjusted | Adjusted for RHOA and knee K-L Grade |
| Mild vs. No Pain | 0.70 (0.49, 1.02) [0.068] |
0.69 (0.46, 1.02) [0.064] |
| Severe vs. No Pain | 0.40 (0.28, 0.56) [<0.0001) |
0.39 (0.27, 0.57) [< 0.0001] |
| Knee JSN | Unadjusted | Adjusted for RHOA |
| Mild (1) vs. No JSN (0) | 1.13 (0.85, 1.50) [0.398] |
1.15 (0.85, 1.55) [0.340] |
| Moderate [52] vs. No JSN (0) |
1.27 (0.90, 1.80) [0.163] |
1.62 (1.09, 2.38) [0.015] |
Relative risk ratios [32] and 95% confidence intervals (CI) estimated from clustered multinomial regression models.
An individual’s contralateral and ipsilateral limbs are identified in relation to the limb with hip pain.
Longitudinal Comparison between Contralateral and Ipsilateral Knees
Unilateral baseline hip pain
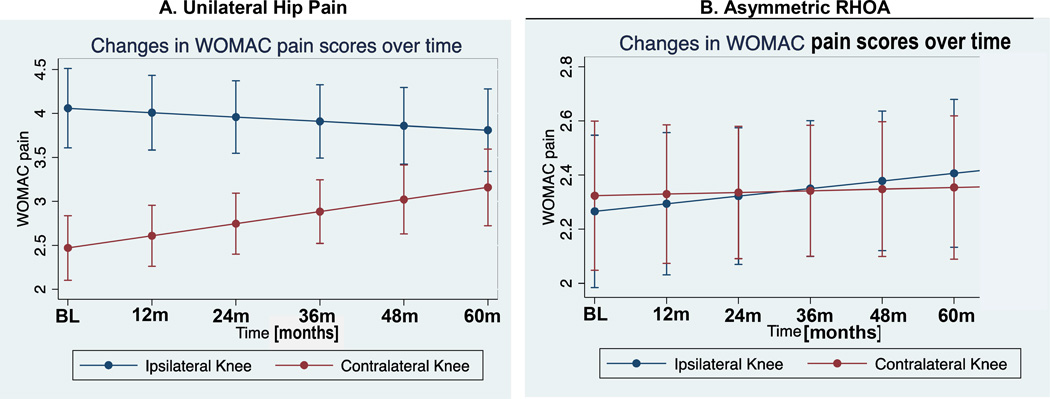
Among those with unilateral hip pain, worsening of WOMAC knee pain during follow-up was significantly greater (p = 0.001) in the contralateral knee (Figure 2). WOMAC pain scores were significantly higher in the ipsilateral knee at baseline. The adjusted rates of change for WOMAC pain were an increase of 0.148/year in the contralateral knee and a decrease of 0.032/year in the ipsilateral knee. Nevertheless, after 60 months of follow-up pain scores remained higher in the ipsilateral knee (adjusted regression coefficient 0.650, p=0.008). There were no significant differences in JSN progression between the contralateral and ipsilateral knees, with an adjusted OR of 1.24 (95% CI: 0.77–1.99, p = 0.36) (Table 4).
Figure 2. Longitudinal changes in WOMAC knee pain scores in subjects with A. Unilateral Hip Pain and B. Asymmetric RHOA.
The graphs illustrate the unadjusted results. A. Unilateral Hip Pain: The rates of change for WOMAC pain (unadjusted) in the contralateral knee were 0.137/year and were −0.049/year in the ipsilateral knee. The adjusted difference in annual rate of change between knees was 0.18 (0.07, 0.28) (p=0.001). At baseline the WOMAC knee pain score was significantly greater in the ipsilateral knee compared to the contralateral knee (adjusted regression coefficient = 1.59; p = <0.0001). B. Discordant RHOA: The rates of change in WOMAC pain scores (unadjusted) in the contralateral knee were 0.006/year and were 0.028/year in the ipsilateral knee. The adjusted difference in rate of change between knees was −0.02 (−0.07, 0.03) (p=0.474). At baseline the WOMAC knee pain score was no different in the ipsilateral knee compared to the contralateal knee (adjusted regression coefficient = −0.036; p = 0.738)..
Table 4.
Association of Unilateral Hip Pain and Discordant Radiographic Hip OA (RHOA) with Knee Joint Space Narrowing (JSN) Progression in the Contralateral vs. Ipsilateral Knee.
| Outcome | Odds Ratio* (95% CI) [p-value] for Outcomes in the Contralateral vs. Ipsilateral Knee* |
|
|---|---|---|
| Unilateral Hip Pain | ||
| Knee JSN Progression# | Unadjusted | Adjusted for RHOA and knee K-L Grade |
| 1.23 (0.93, 1.63) [0.140] |
1.23 (0.92, 1.64) [0.167] |
|
| Discordant for RHOA | ||
| Knee JSN Progression# | Unadjusted | Adjusted for hip pain and knee K-L grade |
| 0.97 (0.63, 0.149) [0.889] |
1.24 (0.77, 1.99) [0.361] |
|
Odds ratios and 95% confidence intervals (CI) estimated from logistic regression models.
An individual’s contralateral and ipsilateral limbs are identified in relation to the limb with more severe RHOA or presence of hip pain.
Any increase in medial or lateral JSN score (including within grade increases) from baseline to 48 months.
Asymmetric baseline RHOA
RHOA asymmetry was not associated with differences between knees in the rate of change in WOMAC knee pain over up to 6 years (Figure 2). Nor did the knee contralateral to the more severely affected hip have a significantly increased risk of JSN progression adjusted odds ratio of 1.23 (95% CI: 0.92–1.64; p = 0.17). Overall, the degree of RHOA discordance (normal vs. possible, possible vs. definite, normal vs. definite) was not associated with change in knee pain (p = 0.83) nor with progression of JSN (p = 0.23) between the knees (data not shown).
Discussion
Our results provide limited support for the hypothesis that asymmetry between limbs in hip pain or RHOA relatively early in the course of disease and well prior to THR is associated with worse pain and structural outcomes in knees contralateral to the more affected hip compared with the ipsilateral knee. Unilateral hip pain “on most days of a month” was associated with significantly less baseline contralateral knee pain, or stated inversely, with greater ipsilateral knee pain. In contrast, knees contralateral to a painful hip had more severe baseline JSN and greater worsening of pain during follow-up but not significantly greater progression of JSN. Knees contralateral to the hip with worse RHOA showed nonsignificant trends for greater baseline JSN and JSN progression, but there was no association of asymmetric RHOA with baseline knee pain or pain change.
Individuals with OA in one lower extremity joint have an increased risk of OA in the same ("cognate") joint in the opposite (contralateral) lower extremity (e.g. knee-knee and hip-hip).[3, 33] There is also an increased risk for endstage OA leading to joint replacement in the hip (or knee) contralateral to that of a replaced hip (or knee).[34, 35] Shakoor et al. [18] extended these observations to include a greater risk of subsequent replacement of a "non-cognate" joint in the lower extremity contralateral to a replaced joint (e.g. a knee contralateral to a replaced hip). Consistent with these cross-limb patterns of joint replacement, we recently reported that during four years of follow-up a prevalent unilateral THR was associated with greater worsening of pain and progression of structural damage assessed by MRI in the knee contralateral to the replaced hip.[20]
These patterns could reflect the existence of a generalized OA phenotype that predisposes to multijoint involvement. [5, 36] However, they also raise the possibility that a potentially modifiable cause of the "spread" of OA among lower extremity joints is related to symptom and neuromuscular control adaptations by persons with OA in one joint who alter movement strategies in a way that results in asymmetric loading and an increased risk of damage in other lower extremity joints.[13, 17, 19] [37] In persons with unilateral severe hip OA leading to joint replacement, increased loading occurs in the unaffected or less affected limb both before and after surgery, [37–42] including significantly higher peak external knee adduction moments and peak medial compartment loads in the contralateral knee.[13] [19] Changes in lower extremity joint loading have also been observed in symptomatic hip OA prior to the development of endstage disease.15,39 Clinic patients with unilateral mild to moderate symptomatic hip OA and not specifically waiting to undergo joint replacement in the near-term have increased loading in the contralateral limb during ambulation[14] and during sit-to-stand postural change,[16] but whether these biomechanical changes are associated with asymmetry in knee pain and structural outcomes is not known.
To our knowledge, this is the first study to directly address the questions of whether asymmetry in symptoms or structural damage between native hips in individuals relatively early in the course of hip disease (hips included in this study did not undergo THR for more than four years after the baseline assessment and 98% had not been replaced by eight years) is associated with asymmetry in the prevalence and progression of symptoms and structural damage in the knee. Our findings of inconsistent and modest differences in contralateral and ipsilateral knee outcomes only partially confirm the cross-limb patterns of knee outcomes seen in previous studies of asymmetric endstage hip OA. One possible explanation is that the degree of asymmetry between hips is not sufficient early in the disease process to lead to biomechanical consequences. It is also possible that that while asymmetric knee loading may occur relatively early in the development of asymmetric hip disease, the immediate effects on clinical and structural knee outcomes are modest. Factors leading to a poor outcome in contralateral knees therefore likely unfold over an extended period, possibly accelerating during the more advanced stages of hip OA along with the development of asymmetric lower extremity strength deficits.[43] It also suggests that a window of opportunity may exist for addressing modifiable causes of lower limb loading asymmetries that could reduce the risk of a poor outcome in the contralateral knee.
Importantly, we found that unilateral hip pain was associated with significantly greater baseline ipsilateral knee pain. While contrary to our hypothesis, this is consistent with a population study in which persons with both unilateral hip pain and unilateral knee pain were over 3 times as likely to have hip and knee pain in the same limb as in the opposite limb.[2] In the study by Shakoor, et al. [14] unilateral clinical symptomatic hip OA was also associated with greater ipsilateral knee pain. The co-occurrence of pain in a hip and knee of the same limb may be due to referred pain from the hip to the knee, [44–46] poorly localized leg pain from non-articular structures such as iliotibial band syndrome, [47] or heightened regional pain sensitivity.[48] It is also possible that neuromuscular adaptations to pain in one lower extremity joint may have adverse effects on joint biomechanics that results in pain in other lower extremity joints of the same limb.[15, 37, 39] On the other hand, we found that pain worsened significantly more over 4–5 years in knees contralateral to a painful hip. Of interest, the contralateral knees also showed elevated baseline JSN in the contralateral knee. While worse baseline JSN may not necessarily be a cause for increasing symptoms over time, there is good evidence that baseline severity of radiographic knee OA predicts clinical progression.[49]. We therefore speculate that while several factors can result in hip and knee pain occurring initially in the same limb, this could magnify asymmetric contralateral loading and be a factor in worse long-term outcomes in the contralateral limb.[18, 34, 50]
Unilateral hip pain showed somewhat stronger associations with knee outcomes than did asymmetric RHOA. This is not surprising given that pain is more likely than structural damage, per se, to trigger movement adaptations that alter lower limb biomechanics, and the fact pain and structural changes of OA in the hip are poorly correlated,[51] in part due to multiple extra321 articular causes hip pain.[44–47] Therefore, the possibility that effective treatment of all causes of hip pain could have beneficial effects on knee outcome is worthy of further consideration.
Our study has several strengths, including within-in person between-limb comparisons that eliminate possible confounding by person-level characteristics including age, gender, obesity and physical activity.[53] Covariates in multivariate models were limited to limb-specific factors that could confound the between knee comparisons, and these adjustments had minimal effects on the associations of interest. We focused on hip pain and RHOA prior to endstage clinical disease by studying only persons who did not undergo a hip replacement at 4 years or longer after the baseline assessments, thus specifically targeting individuals relatively early in the course of hip OA. Further, sensitivity analyses excluding subjects with severe baseline JSN in the hip did not alter our results. Because joint pain typically fluctuates over time, in order to identify subjects with persistent discordance in hip pain we required unilateral frequent pain in at least 2 of 3 consecutive years.
Several limitations of our study deserve consideration. Consistent with our focus on the earlier stages of hip disease and the modest correlation of hip symptoms with structural changes, only 38 individuals in our study had unilateral symptomatic hip OA, defined as pain and definite RHOA in the same hip on one side but not the other side, a number too small to include in our analyses. Thus our study differs from previous ones, which have focused on asymmetry at moderate (i.e. unilateral symptomatic clinical hip OA) [14] or advanced (i.e. unilateral endstage OA before and after hip replacement) stages of disease.[20, 34, 35] Many of our subjects had only subtle degrees of RHOA asymmetry (i.e., a normal hip and a hip with possible RHOA), and the number of participants with the greater degree of discordance between hips in RHOA (i.e. definite vs normal) was limited. However, we also performed analyses that looked at the effect of different degrees of RHOA asymmetry on contralateral vs ipsilateral knee outcomes and found that the associations did not differ significantly by degree of RHOA discordance. In addition, a sensitivity analysis excluding subjects with the most subtle RHOA asymmetry did not change our results. We did not have data on hip pain severity at baseline, so we were unable to use severity differences in defining hip pain asymmetry; results could differ for greater extremes of asymmetry defined in terms of pain severity.
We cannot exclude the possibility that pre-existing asymmetric knee OA preceded, and influenced, the development of asymmetries in the hip. However, to reduce this possibility we excluded subjects with endstage knee OA at baseline (K-L = 4, JSN = 3 and TKR by 12 months). In a sensitivity analyses we also excluded those who already had extreme disparities between knees in the severity of knee OA (baseline KL grade of 0–1 in one knee and 3 in the other), which did not alter our findings. Further studies are needed of persons who develop unilateral hip OA and have bilateral normal knees at baseline.
In conclusion, our results provide limited support for the hypothesis that asymmetry between limbs in hip pain or RHOA at a relatively early point in the development of hip disease is associated with worse pain or structural outcomes in the knee contralateral to the more affected hip. Poor contralateral knee OA outcomes seen in previous studies of unilateral endstage hip OA leading to joint replacement may have their origin in joint loading asymmetries that occur early in the development of hip disease, but likely unfold over an extended period and accelerate in the later stages of hip OA. This suggests a potential window of opportunity for ameliorating biomechanical abnormalities before poor knee outcomes occur.
Acknowledgments
Role of funding source
The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. This project was also funded in whole or part with federal funds from the National Institute of Arthritis and Musculoskeletal and Skin Diseases, NIH under Contract No. HHSN268201000019C.
Other contributions
We would like to thank Lorenzo Nardo, MD, Department of Radiology and Biomedical Imaging at UCSF, for participating in the screening assessment of pelvis radiographs for evidence of radiographic hip OA prior to the reading for individual radiographic features.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors’ contributions
- Substantial contributions to the conception and design, or acquisition of the data, or analysis and interpretation of the data: G.B. Joseph, J.F. Hilton, P.M. Jungmann, J.A. Lynch, N. E. Lane, F. Liu, C.E. McCulloch, I. Tolsktyk, T.M. Link, M. Nevitt.
- Drafting of the article or revising it for important intellectual content: G.B. Joseph, J.F. Hilton, P.M. Jungmann, J.A. Lynch, N. E. Lane, F. Liu, C.E. McCulloch, I. Tolsktyk, T.M. Link, M. Nevitt.
- Final approval of the version to be published: G.B. Joseph, J.F. Hilton, P.M. Jungmann, J.A. Lynch, N. E. Lane, F. Liu, C.E. McCulloch, I. Tolsktyk, T.M. Link, M. Nevitt.
Conflict of interest
No authors declare financial or personal relationships with other people or organizations that could potentially influence their work and conclusions.
References
- 1.Kim S. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997–2004. Arthritis Rheum. 2008;59:481–488. doi: 10.1002/art.23525. [DOI] [PubMed] [Google Scholar]
- 2.Dawson J, Linsell L, Zondervan K, Rose P, Randall T, Carr A, et al. Epidemiology of hip and knee pain and its impact on overall health status in older adults. Rheumatology (Oxford) 2004;43:497–504. doi: 10.1093/rheumatology/keh086. [DOI] [PubMed] [Google Scholar]
- 3.Sayre EC, Jordan JM, Cibere J, Murphy L, Schwartz TA, Helmick CG, et al. Quantifying the association of radiographic osteoarthritis in knee or hip joints with other knees or hips: the Johnston County Osteoarthritis Project. J Rheumatol. 2010;37:1260–1265. doi: 10.3899/jrheum.091154. [DOI] [PubMed] [Google Scholar]
- 4.Kraus VB, Worrell TW, Renner JB, Coleman RE, Pieper CF. High prevalence of contralateral ankle abnormalities in association with knee osteoarthritis and malalignment. Osteoarthritis Cartilage. 2013;21:1693–1699. doi: 10.1016/j.joca.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 6.Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009;91(Suppl 1):95–101. doi: 10.2106/JBJS.H.01408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma L, Chmiel JS, Almagor O, Felson D, Guermazi A, Roemer F, et al. The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis. 2013;72:235–240. doi: 10.1136/annrheumdis-2011-201070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas GE, Palmer AJ, Batra RN, Kiran A, Hart D, Spector T, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women. A 20 year longitudinal cohort study. Osteoarthritis Cartilage. 2014;22:1504–1510. doi: 10.1016/j.joca.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 9.Khashan M, Mor A, Beer Y, Rath E, Morgensteren DR, Debi R, et al. Gait metric profile and gender differences in hip osteoarthritis patients. A case-controlled study. Hip Int. 2014;24:270–276. doi: 10.5301/hipint.5000111. [DOI] [PubMed] [Google Scholar]
- 10.Baert IA, Jonkers I, Staes F, Luyten FP, Truijen S, Verschueren SM. Gait characteristics and lower limb muscle strength in women with early and established knee osteoarthritis. Clin Biomech (Bristol, Avon) 2013;28:40–47. doi: 10.1016/j.clinbiomech.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Kubota M, Shimada S, Kobayashi S, Sasaki S, Kitade I, Matsumura M, et al. Quantitative gait analysis of patients with bilateral hip osteoarthritis excluding the influence of walking speed. J Orthop Sci. 2007;12:451–457. doi: 10.1007/s00776-007-1160-z. [DOI] [PubMed] [Google Scholar]
- 12.Boissonneault A, Lynch JA, Wise BL, Segal NA, Gross KD, Murray DW, et al. Association of hip and pelvic geometry with tibiofemoral osteoarthritis: Multicenter Osteoarthritis Study (MOST) Osteoarthritis Cartilage. 2014;22:1129–1135. doi: 10.1016/j.joca.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shakoor N, Hurwitz DE, Block JA, Shott S, Case JP. Asymmetric knee loading in advanced unilateral hip osteoarthritis. Arthritis Rheum. 2003;48:1556–1561. doi: 10.1002/art.11034. [DOI] [PubMed] [Google Scholar]
- 14.Shakoor N, Dua A, Thorp LE, Mikolaitis RA, Wimmer MA, Foucher KC, et al. Asymmetric loading and bone mineral density at the asymptomatic knees of patients with unilateral hip osteoarthritis. Arthritis Rheum. 2011;63:3853–3858. doi: 10.1002/art.30626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eitzen I, Fernandes L, Nordsletten L, Risberg MA. Sagittal plane gait characteristics in hip osteoarthritis patients with mild to moderate symptoms compared to healthy controls: a cross-sectional study. BMC Musculoskelet Disord. 2012;13:258. doi: 10.1186/1471-2474-13-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eitzen I, Fernandes L, Nordsletten L, Snyder-Mackler L, Risberg MA. Weight-bearing asymmetries during Sit-To-Stand in patients with mild-to-moderate hip osteoarthritis. Gait Posture. 2014;39:683–688. doi: 10.1016/j.gaitpost.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Pozzi F, Snyder-Mackler L, Zeni J., Jr Relationship between biomechanical asymmetries during a step up and over task and stair climbing after total knee arthroplasty. Clin Biomech (Bristol, Avon) 2015;30:78–85. doi: 10.1016/j.clinbiomech.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002;46:3185–3189. doi: 10.1002/art.10649. [DOI] [PubMed] [Google Scholar]
- 19.Foucher KC, Wimmer MA. Contralateral hip and knee gait biomechanics are unchanged by total hip replacement for unilateral hip osteoarthritis. Gait Posture. 2012;35:61–65. doi: 10.1016/j.gaitpost.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Jungmann PMNM, Baum T, Liebl H, Nardo L, Liu F, Lane MC, McCulloch CE, Link TM. Relationship of Unilateral Total Hip Arthroplasty (THA) to Contralateral and Ipsilateral Knee Joint Degeneration: A Longitudinal 3T MRI Study from the Osteoarthritis Initiative (OAI) Osteoarthritis Cart. 2015 doi: 10.1016/j.joca.2015.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Croft P, Cooper C, Coggon D. Case definition of hip osteoarthritis in epidemiologic studies. J Rheumatol. 1994;21:591–592. [PubMed] [Google Scholar]
- 23.Arden NK, Lane NE, Parimi N, Javaid KM, Lui LY, Hochberg MC, et al. Defining incident radiographic hip osteoarthritis for epidemiologic studies in women. Arthritis Rheum. 2009;60:1052–1059. doi: 10.1002/art.24382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Birrell F, Croft P, Cooper C, Hosie G, Macfarlane G, Silman A. Health Impact of pain in the hip region with and without radiographic evidence of osteoarthritis: a study of new attenders to primary care. Ann Rheum Dis. 2000;59:857–863. doi: 10.1136/ard.59.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Birrell F, Lunt M, Macfarlane G, Silman A. Association between pain in the hip region and radiographic changes of osteoarthritis: results from a population-based study. Rheumatology (Oxford) 2005;44:337–341. doi: 10.1093/rheumatology/keh458. [DOI] [PubMed] [Google Scholar]
- 26.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 27.Roberts WN, Williams RB. Hip pain. Prim Care. 1988;15:783–793. [PubMed] [Google Scholar]
- 28.Birrell F, Lunt M, Macfarlane GJ, Silman AJ. Defining hip pain for population studies. Ann Rheum Dis. 2005;64:95–98. doi: 10.1136/ard.2003.018788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35:2047–2054. [PMC free article] [PubMed] [Google Scholar]
- 30.Felson D, Niu J, Sack B, Aliabadi P, McCullough C, Nevitt MC. Progression of osteoarthritis as a state of inertia. Ann Rheum Dis. 2013;72:924–929. doi: 10.1136/annrheumdis-2012-201575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bellamy N, Buchanan Ww, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 32.Harrrell F. Regression modeling strategies, Springer, New York, 2001. New York: Springer; 2001. [Google Scholar]
- 33.Spector TD, Hart DJ, Doyle DV. Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Ann Rheum Dis. 1994;53:565–568. doi: 10.1136/ard.53.9.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Husted H, Overgaard S, Laursen JO, Hindso K, Hansen LN, Knudsen HM, et al. Need for bilateral arthroplasty for coxarthrosis. 1,477 replacements in 1,199 patients followed for 0–14 years. Acta Orthop Scand. 1996;67:421–423. doi: 10.3109/17453679608996660. [DOI] [PubMed] [Google Scholar]
- 35.Sayeed SA, Sayeed YA, Barnes SA, Pagnano MW, Trousdale RT. The risk of subsequent joint arthroplasty after primary unilateral total knee arthroplasty, a 10-year study. J Arthroplasty. 2011;26:842–846. doi: 10.1016/j.arth.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Spector TD, MacGregor AJ. Risk factors for osteoarthritis: genetics. Osteoarthritis Cartilage. 2004;12(Suppl A):S39–S44. doi: 10.1016/j.joca.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 37.Metcalfe A, Stewart C, Postans N, Barlow D, Dodds A, Holt C, et al. Abnormal loading of the major joints in knee osteoarthritis and the response to knee replacement. Gait Posture. 2013;37:32–36. doi: 10.1016/j.gaitpost.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 38.Talis VL, Grishin AA, Solopova IA, Oskanyan TL, Belenky VE, Ivanenko YP. Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin Biomech (Bristol, Avon) 2008;23:424–433. doi: 10.1016/j.clinbiomech.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 39.Metcalfe AJ, Stewart C, Postans N, Dodds AL, Holt CA, Roberts AP. The effect of osteoarthritis of the knee on the biomechanics of other joints in the lower limbs. Bone Joint J. 2013;95-B:348–353. doi: 10.1302/0301-620X.95B3.30850. [DOI] [PubMed] [Google Scholar]
- 40.Martinez-Ramirez A, Weenk D, Lecumberri P, Verdonschot N, Pakvis D, Veltink PH. Pre-operative ambulatory measurement of asymmetric lower limb loading during walking in total hip arthroplasty patients. J Neuroeng Rehabil. 2013;10:41. doi: 10.1186/1743-0003-10-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinez-Ramirez A, Weenk D, Lecumberri P, Verdonschot N, Pakvis D, Veltink PH. Assessment of asymmetric leg loading before and after total hip arthroplasty using instrumented shoes. J Neuroeng Rehabil. 2014;11:20. doi: 10.1186/1743-0003-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Turcot K, Armand S, Fritschy D, Hoffmeyer P, Suva D. Sit-to-stand alterations in advanced knee osteoarthritis. Gait Posture. 2012;36:68–72. doi: 10.1016/j.gaitpost.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 43.Zeni JA, Jr, Snyder-Mackler L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther. 2010;90:43–54. doi: 10.2522/ptj.20090089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khan AM, McLoughlin E, Giannakas K, Hutchinson C, Andrew JG. Hip osteoarthritis: where is the pain? Ann R Coll Surg Engl. 2004;86:119–121. doi: 10.1308/003588404322827518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sakamoto J, Morimoto Y, Ishii S, Nakano J, Manabe Y, Okita M, et al. Investigation and macroscopic anatomical study of referred pain in patients with hip disease. J Phys Ther Sci. 2014;26:203–208. doi: 10.1589/jpts.26.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tipton JS. Obturator neuropathy. Curr Rev Musculoskelet Med. 2008;1:234–237. doi: 10.1007/s12178-008-9030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24:1407–1421. doi: 10.1016/j.arthro.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 48.Lee YC, Lu B, Bathon JM, Haythornthwaite JA, Smith MT, Page GG, et al. Pain sensitivity and pain reactivity in osteoarthritis. Arthritis Care Res (Hoboken) 2011;63:320–327. doi: 10.1002/acr.20373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bastick AN, Runhaar J, Belo JN, Bierma-Zeinstra SM. Prognostic factors for progression of clinical osteoarthritis of the knee: a systematic review of observational studies. Arthritis Res Ther. 2015;17:152. doi: 10.1186/s13075-015-0670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sayeed SA, Trousdale RT, Barnes SA, Kaufman KR, Pagnano MW. Joint arthroplasty within 10 years after primary charnley total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2009;38:E141–E143. [PubMed] [Google Scholar]
- 51.Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. doi: 10.1186/1471-2474-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48:241–249. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 53.Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ. 2009;21:339–345. doi: 10.1136/bmj.b2844. [DOI] [PMC free article] [PubMed] [Google Scholar]