Abstract
Background
The purpose of this study was to determine if capsular repair used in conjunction with the Latarjet procedure results in significant alterations in glenohumeral rotational range of motion and translation.
Methods
Glenohumeral rotational range of motion and translation were measured in eight cadaveric shoulders in 90° of abduction in both the scapular and coronal planes under the following four conditions: intact glenoid, 20% bony Bankart lesion, modified Latarjet without capsular repair, and modified Latarjet with capsular repair.
Results
Creation of a 20% bony Bankart lesion led to significant increases in anterior and inferior glenohumeral translation and rotational range of motion (p < 0.005). The Latarjet procedure restored anterior and inferior stability compared to the bony Bankart condition. It also led to significant increases in glenohumeral internal and external rotational range of motion relative to both the intact and bony Bankart conditions (p < 0.05). The capsular repair from the coracoacromial ligament stump to the native capsule did not significantly affect translations relative to the Latarjet condition; however it did cause a significant decrease in external rotation in both the scapular and coronal planes (p < 0.005).
Conclusions
The Latarjet procedure is effective in restoring anteroinferior glenohumeral stability. The addition of a capsular repair does not result in significant added stability; however, it does appear to have the effect of restricting glenohumeral external rotational range of motion relative to the Latarjet procedure performed without capsular repair.
Keywords: Shoulder, Instability, Bone loss, Dislocation
Shoulder instability is a common occurrence in young, physically active individuals. The majority of shoulders dislocate in an anteroinferior direction, resulting in damage to the anteroinferior labrum and glenohumeral ligament. 1,2) Repair of the Bankart lesion by both open and arthroscopic methods has shown favorable outcomes regarding stability and the incidence of recurrence.3,4,5) However, in the setting of significant glenoid bone loss (> 20%), soft tissue reconstructions are universally associated with poor outcomes and unacceptably high recurrence rates.6,7,8,9)
In 1954, Latarjet10) described transferring the coracoid process with an intact conjoint tendon to the anterior neck of the glenoid in cases of recalcitrant instability due to glenoid bone loss. The stabilizing mechanism of the Latarjet procedure is thought to be provided by both the "bone block" derived from transfer of the coracoid process, which increases the surface area of the anteroinferior glenoid, and the "sling effect" produced by the conjoint tendon and intact subscapularis.11,12,13) The "sling effect" is especially important in positions of mid to end-range shoulder abduction.13)
Another possible stabilizing mechanism of the Latarjet includes the capsular repair from the transferred portion of the coracoacromial ligament to the native capsule after fixation of the coracoid. Several studies show an added benefit to the capsular repair,12,14) while other reports of coracoid transfers not incorporating capsular repair have also shown excellent results and low rates of recurrence.15,16) Furthermore, it is unclear if the capsular repair has any harmful effects, such as restricting the range of motion.
The purpose of this study was to evaluate the effects of the Latarjet procedure with and without capsular repair on anteroinferior translation, glenohumeral kinematics and rotational range of motion. We hypothesized that repair of the capsule would result in altered glenohumeral kinematics and reduced range of motion without adding significant resistance to glenohumeral translations.
METHODS
Eight cadaveric shoulders (five left and three right shoulders from two male and six female cadavers; average age, 58 years; standard deviation, 4.3 years) were prepared by removing the clavicle and superficial muscles of the shoulder. The rotator cuff, capsule, coracoacromial ligament, and conjoined tendon were left intact. Three small screws were placed in the anterolateral edge of the acromion and the proximal humerus as reference points for measuring glenohumeral kinematics. The methods used in this study are similar to those in a previous study evaluating glenohumeral translations of a Bristow compared to a conjoint tendon-only transfer.17)
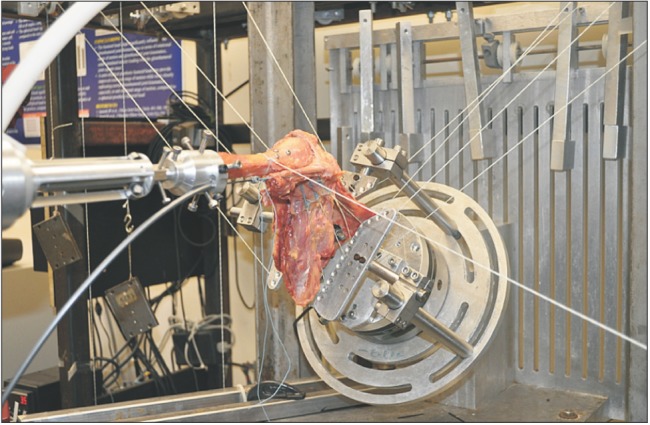
The scapula was secured to a mounting bracket, and the humerus was secured to an intramedullary rod for mounting. The scapula plate was mounted on a custom testing system with 20° of anterior tilt to simulate average in vivo position of the shoulder18) (Fig. 1). The humeral rod was inserted through a hollow-shaft angle potentiometer (Novotechnik US Inc., Southborough, MA, USA) for measuring humeral rotation. The potentiometer was attached to an arc with a custom device that allows for compression/distraction as well as anterior/posterior and medial/lateral glenohumeral translation while fixing the degree of shoulder abduction.
Fig. 1. Photograph of a right shoulder mounted on the custom testing system at 60° of glenohumeral abduction.
The rotator cuff and conjoined tendons were loaded based on physiological cross-sectional area with multiple lines of pull. Two lines of pull were used for the supraspinatus, three for the subscapularis, two for the infraspinatus, one for the teres minor, and one for the conjoined tendon. Five N were loaded on each line of pull, for a total of 40 N. The conjoined tendon was sutured in Krackow fashion and loaded with 10 N.
Ninety degrees of external rotation was defined as the position at which the bicipital groove was aligned with the anterolateral aspect of the acromion.19,20) A string was attached to the humerus at the proximal pectoralis major insertion for application of an anteroinferior translation force. The string passed through a pulley positioned perpendicular and anterior to the humerus with a 20°-inferior pull. Three anteroinferior loads were applied to simulate an anteroinferior dislocation force. Weights measuring 20, 30, and 40 N were applied and glenohumeral translation was measured using a MicroScribe 3DLX (Revware, Raleigh, NC, USA).
Specimens were tested in 60° of glenohumeral abduction simulating 90° of shoulder abduction. Glenohumeral kinematics were measured throughout the rotational range of motion at maximum internal rotation; 0°, 30°, 60°, 90°, and maximum external rotation by digitizing the three reference screws on the acromion and the humerus at each position with the MicroScribe. Maximum rotation was defined as the amount of rotation reached with 1.5 N·m of torque. This torque was adequate to provide a consistent endpoint for measuring humeral rotation while not resulting in soft-tissue damage. Anteroinferior translation was measured with the humerus locked in 60° of abduction and 60° of external rotation by adding 20, 30, and 40 N loads incrementally through the pulley. Translation was measured in the scapular and coronal planes. The four experimental conditions of testing comprised: (1) intact glenohumeral joint; (2) Bankart lesion with 20% glenoid bone loss; (3) Latarjet procedure; and (4) Latarjet procedure with capsular repair. All tests conditions were performed on each cadaver.
After intact testing, a Bankart lesion was created through a split in the subscapularis. All Bankart lesions were created and surgical procedures performed by the primary author. All tendons were unloaded temporarily by removing the attached weights, and lateral traction was placed on the proximal humerus to expose the glenoid face. The capsule was split vertically to the glenoid and then the labrum and capsule were released from the anterior glenoid from the 12- to 6-o'clock position. The widest part of the glenoid was measured twice with a depth gauge and averaged. A mark was made on the face of the glenoid at the calculated distance required to produce a 20% osseous glenoid defect. An osteotome was used to remove 20% of the anterior glenoid in line with the longitudinal axis. A glenoid lesion of 20% was chosen based on a similar study by Kephart et al.17)
After testing the Bankart condition, the Latarjet procedure was performed by cutting the coracoacromial ligament 1 cm lateral to the coracoid process. The surgical technique utilized during testing was that described by Walch and Boileau.21) A reciprocating saw and osteotome were used to cut the coracoid process at its base and remove it. The coracoid was then transferred to the anterior neck of the glenoid by drilling a 3.5 mm hole in the inferior aspect of the coracoid. Next, using a 2.5-mm drill, a hole was made at the 5:30 position of the anterior neck of the glenoid, drilling from anterior to posterior. A 3.5 mm fully threaded cortical screw was placed in the coracoid and fed into the glenoid at the 5:30 position for adequate compression of the bone block to the glenoid neck. Next, a 3.5 mm drill was used to drill a second hole in the coracoid corresponding to the 4:30 position on the glenoid. A second hole was drilled through the glenoid neck using the 2.5 mm-drill. A second 3.5 mm fully threaded cortical screw was placed into the coracoid bone block and glenoid from anterior to posterior using lag technique. The holes drilled in the glenoid were made such that the coracoid block sat flush with the glenoid articular surface.
Next, a capsular repair was performed by placing two figure-of-eight sutures with a #2 FiberWire (Arthrex Inc., Naples, FL, USA) from the stump of the coracoacromial ligament to the cut free edge of the native capsule. The repair was performed with the specimen in 90° of external rotation as described by Young et al.22) Care was taken not to imbricate the capsular tissue. A third figure-of-eight suture was placed superior to the bone block to re-approximate native capsular tissue. Again, all conditions were tested.
Following biomechanical testing of the four conditions, the specimens were disarticulated and the glenoid and humeral head articular surfaces were digitized using the MicroScribe 3DLX (Revware) relative to the three reference screws on each bone. Using these geometric relationships, the humeral head apex position, defined as the highest point on the articular surface of the humeral head relative to the plane of the articular margin, was tracked relative to the geometric center of the glenoid.23) The geometric center of the glenoid was defined as the point bisecting the superoinferior and anteroposterior axes of the glenoid at the articular surface.
Based on expected differences and standard deviations in a previous study in our laboratory, a power analysis was conducted using a power of 0.8 and alpha of 0.5. It was determined that six specimens were needed to show a statistically significant difference in range of motion and eight specimens were needed to show a difference in translation; therefore we chose to test eight specimens. All data were collected for two trials. If the points were not repeatable within 1.0 mm, a third trial was carried out. The average value for the two most repeatable trials was used. A repeated-measures analysis of variance with a significance level of 0.5 was used. If significance was shown, a Tukey post hoc test was used to determine the areas where significance occurred.
RESULTS
Rotational Range of Motion
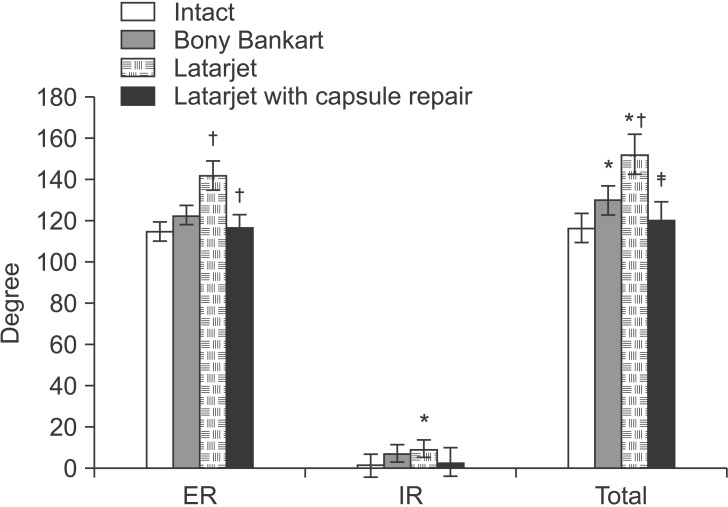
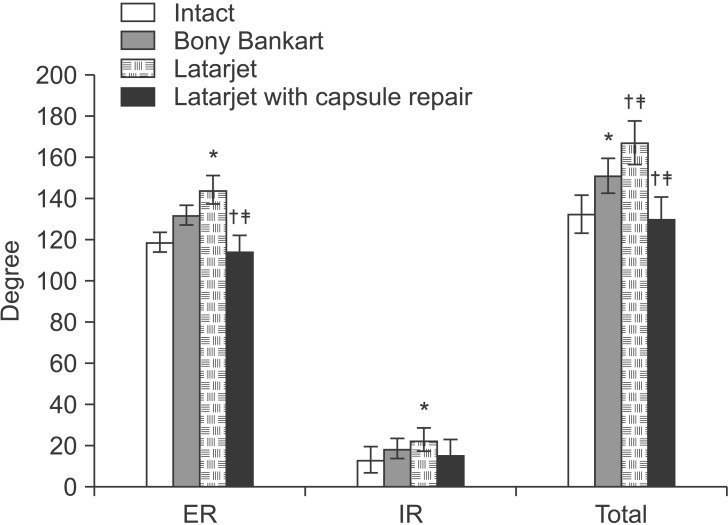
In the scapular and coronal planes, creation of a 20% bony Bankart lesion led to insignificant increases in internal and external rotation compared to the intact condition (Figs. 2 and 3). However, total range of motion for the bony Bankart condition was significantly increased (p = 0.039 and p = 0.016, respectively) compared to the intact condition. The Latarjet condition resulted in significant increases in internal and external rotational range of motion as well as total range of motion in both the scapular and coronal planes (p < 0.05). The addition of a capsular repair to the Latarjet condition resulted in close restoration of range of motion to the intact condition with significant decreases in external rotation and total range of motion compared to the Latarjet condition in both the scapular and coronal planes (p < 0.001 for both the scapular and coronal planes).
Fig. 2. Rotational range of motion in the coronal plane for external rotation, internal rotation and total range of motion for all four conditions tested (p < 0.05). ER: external rotation, IR: internal rotation. *vs. intact. †vs. bony Bankart. ‡vs. Latarjet.
Fig. 3. Rotational range of motion in the scapular plane for external rotation, internal rotation and total range of motion for all four conditions tested (p < 0.05). ER: external rotation, IR: internal rotation. *vs. intact. †vs. bony Bankart. ‡vs. Latarjet.
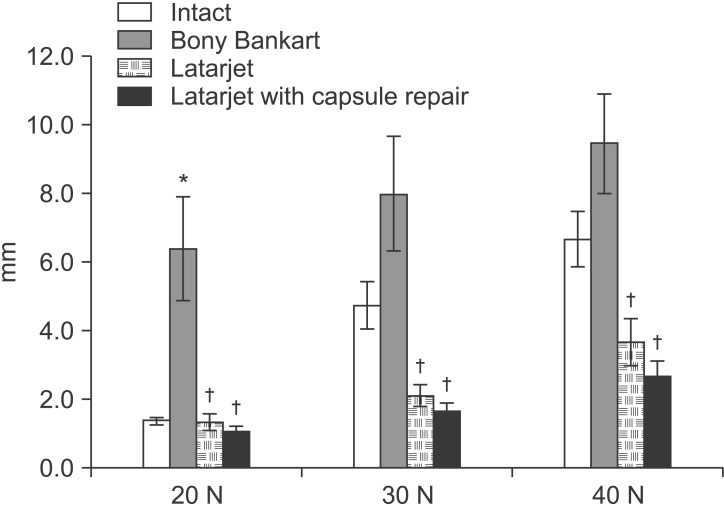
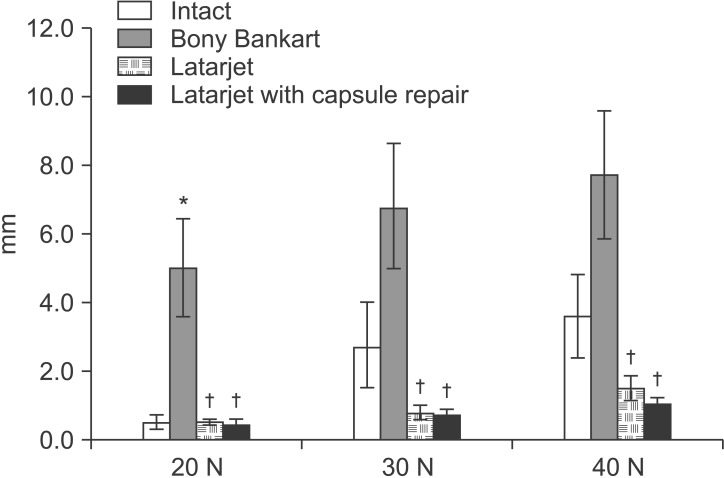
Glenohumeral Translation in the Scapular Plane
A 20% bony Bankart lesion increased anterior translation in the scapular plane by 5, 3.3, and 2.8 mm when 20, 30, and 40 N loads were applied (Fig. 4). Only the 20 N load resulted in a significant increase in translation relative to the intact condition (p = 0.0009). Inferior translation increased by 4.5, 4.1, and 4.1 mm when 20, 30, and 40 N loads were applied (Fig. 5). Again, only the 20 N load resulted in a statistically significant increase in inferior translation (p = 0.001). The Latarjet condition restored both anterior and inferior translation to the intact condition. The addition of a capsular repair did not result in significant added stability compared to the Latarjet condition alone at all loads applied.
Fig. 4. Anterior glenohumeral translation for 20, 30, and 40 N loads in the scapular plane (p < 0.05). *vs. intact. †vs. bony Bankart.
Fig. 5. Inferior glenohumeral translation for 20, 30, and 40 N loads in the scapular plane (p < 0.05). *vs. intact. †vs. bony Bankart.
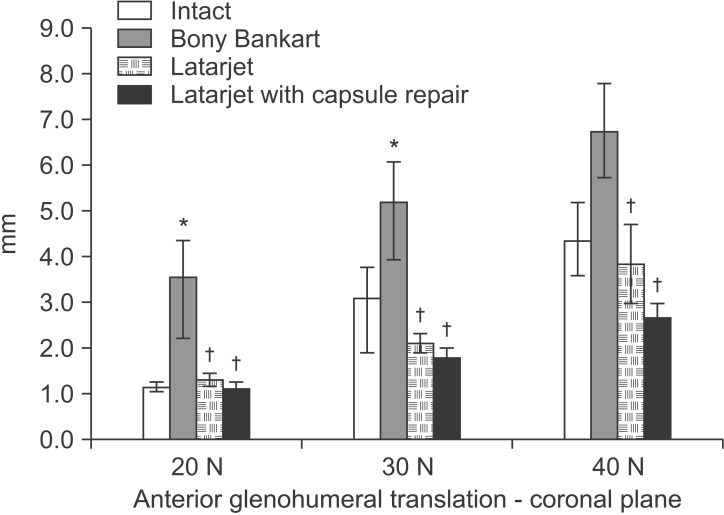
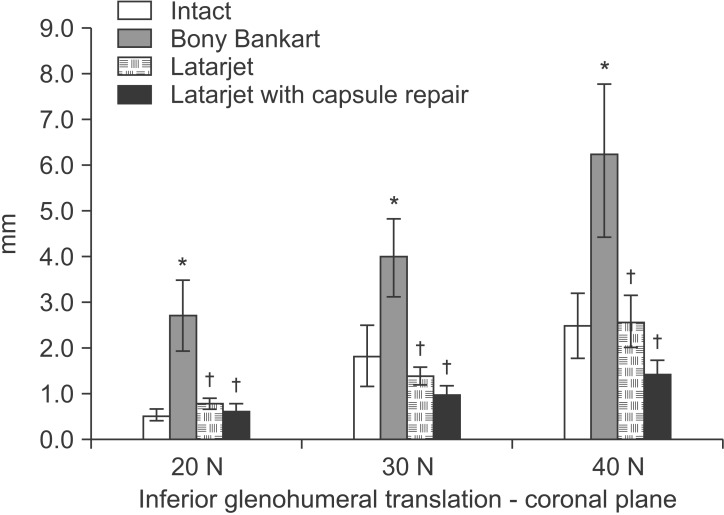
Glenohumeral Translation in the Coronal Plane
After creation of the bony Bankart lesion, anterior translation increased by 2.4, 2.2, and 2.4 mm when 20, 30, and 40 N loads were applied, respectively (Fig. 6). The increase in translation was significant for the 20 and 30 N loads (p = 0.0009 and p = 0.008, respectively) but not for the 40 N load (p = 0.11). Inferior translation increased by 2.2, 2.2, and 3.7 mm for the 20, 30, and 40 N loads. (Fig. 7) All of these values reached statistical significance (p = 0.0008, p = 0.007, and p = 0.03, respectively). The Latarjet procedure restored both anterior and inferior translation with all applied loads. The addition of the capsular repair did not significantly improve anterior or inferior translations relative to the Latarjet procedure alone.
Fig. 6. Anterior glenohumeral translation for 20, 30, and 40 N loads in the coronal plane (p < 0.05). *vs. intact. †vs. bony Bankart.
Fig. 7. Inferior glenohumeral translation for 20, 30, and 40 N loads in the coronal plane (p < 0.05). *vs. intact. †vs. bony Bankart.
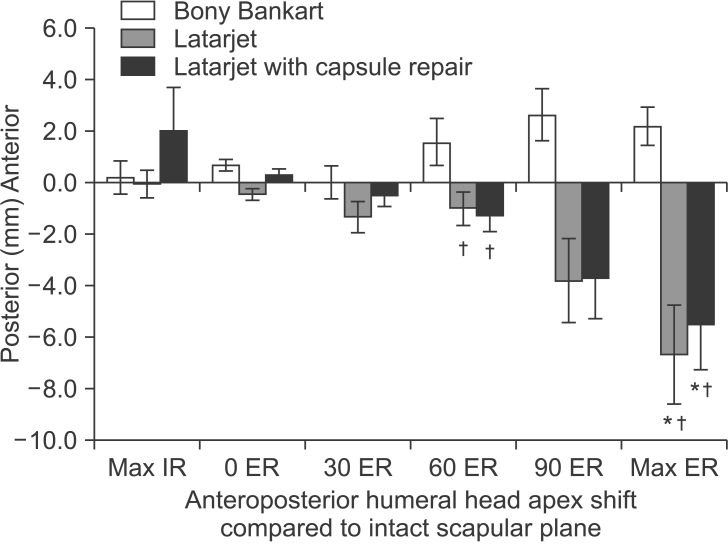
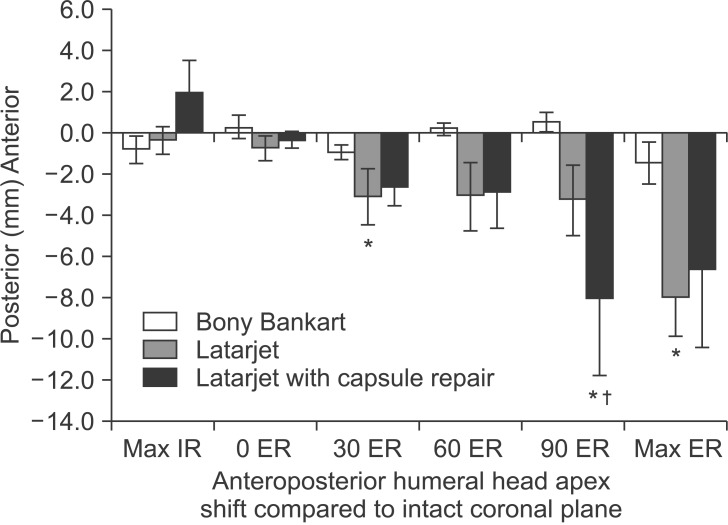
Humeral Head Apex Position
The Latarjet procedure resulted in a significant increase in posterior translation relative to the intact state at 90° external rotation and maximum external rotation in both the scapular and coronal planes (p < 0.05) (Figs. 8 and 9). The capsular repair did not lead to any significant changes in humeral head apex position relative to the Latarjet procedure alone. There was no significant change in the superoinferior humeral head apex position in either the scapular or coronal plane. There was one significant mediolateral change in humeral head apex position in the scapular plane at 60° of external rotation after completion of the Latarjet with capsular repair (p = 0.048). The implications of this particular value are likely negligible.
Fig. 8. Change in anteroposterior humeral head apex position in the scapular plane compared with the intact position throughout the range of motion from maximum internal rotation (Max IR) to maximum external rotation (Max ER) (p < 0.05). *vs. intact. †vs. bony Bankart.
Fig. 9. Change in anteroposterior humeral head apex position in the coronal plane compared with the intact position throughout the range of motion from maximum internal rotation (Max IR) to maximum external rotation (Max ER) (p < 0.05). *vs. intact. †vs. bony Bankart.
DISCUSSION
In this biomechanical model, the Latarjet procedure effectively decreased anteroinferior glenohumeral translation relative to the 20% bony Bankart condition. The capsular repair showed a trend toward increasing anteroinferior translational stability compared to the Latarjet procedure, but this did not reach statistical significance. The primary modes of stability in this model arise from the stabilizing mechanisms of the bone block and sling effect. Therefore, according to these results the capsular repair may not be necessary for restoration of stability when performing a Latarjet procedure.
While our study did not find a significant improvement in glenohumeral stability with Latarjet augmented with capsular repair, other investigations have found that capsular repair contributes significant stability to the procedure. A recent biomechanical study conducted by Yamamoto et al.13) showed that the suturing of the capsule to the coracoacromial ligament contributed 23% to the resistance of translational force in the end-range arm position, with the remaining 77% provided by the sling effect. The main key difference in the methodology between the two studies is that Yamamoto et al.13) evaluated the effect of the capsule repair to the coracoacromial ligament after removing the sling effect of the subscapularis and conjoint tendon. In our model the sling effect remained before and after removing the capsule repair by loading of the subscapularis and conjoint tendon. Since removal of this sling effect significantly decreased stability, the effect of capsule repair may have been exaggerated. Yamamoto et al.13) also do not mention the contribution of the bone block in the end range position even though the translational force required to translate 10 mm significantly increases after performing Latarjet, even with an unloaded subscapularis and conjoint tendon.
Another biomechanical study performed by stepwise dissection of an open Latarjet reconstruction with a capsular repair with coracoacromial ligament transfer to the native capsule demonstrated significant increases in anterior and inferior glenohumeral translations when the coracoacromial ligament transfer was removed from the Latarjet reconstruction.12) Finally, a clinical study of 319 shoulders treated with Bristow-Latarjet procedures found that a horizontal capsular shift decreased the overall rate of dislocation from 18% to 4%, resulting in improved subjective patient outcomes as well as decreased rates of recurrence.14) Therefore, controversy remains regarding the efficacy of capsular repair in terms of its contribution to stability after the Latarjet procedure. However, our study denotes a lesser role for capsular repair compared to previously reported studies.
In our study, we found that the addition of a capsular repair resulted in a significant loss of motion compared to the Latarjet procedure. However, the capsular repair was determined to result in glenohumeral range of motion that simulated values seen in the intact shoulder. Several clinical studies have shown a decreased range of motion after coracoid transfer procedures for glenoid bone loss.12,15,24) It should be acknowledged that a procedure that restores motion to that of the intact condition, namely capsular repair, should be looked upon favorably. However, it is difficult to extrapolate the clinical consequences of the capsular repair.
The Latarjet procedure with and without the capsular repair resulted in a posterior shift in the humeral head apex position. This effect became more apparent with increasing amounts of external rotation. This phenomenon has similarly been reported in other biomechanical studies examining the effects of the modified Bristow procedure.17) While the clinical relevance of this posterior shift is unknown, it may serve as a protective mechanism against anterior subluxation or dislocation of the humeral head in positions of increased abduction and external rotation.
There are certain limitations to this study inherent to a biomechanical cadaveric study. The data do not account for natural healing responses that occur after surgical procedures. Scarring and contracture are natural phenomena after surgical procedures that can alter range of motion. There was no statistically significant increase in glenohumeral translation for the higher loads following Bankart lesion. Translation with the 30 and 40 N loads resulted in anterior subluxation or dislocation in the intact shoulder in some but not all specimens, making the changes seen with Bankart lesion relatively small since the shoulder was already subluxation. This also made the standard deviation relatively large for the 30 and 40 N loads. Despite this however, a post hoc power analysis of the translation data revealed a power of greater than 0.83 to detect differences between the groups. Therefore we feel the study was adequately powered to detect these differences. While we chose to perform our capsular repair at 90° of external rotation, consistent with the technique described by Young et al.,22) others may perform this repair in maximum external rotation, leading to less restriction of rotation relative to the Latarjet procedure performed without capsular repair. It is also worth noting that some surgeons perform the capsular repair by reattaching the capsule to the native glenoid, effectively creating an extraarticular bone block and possibly altering the stabilizing properties of the capsular repair.
In conclusion, the Latarjet procedure is effective in terms of restoring anteroinferior glenohumeral stability. The addition of a capsular repair does not result in significant added stability; however, it does appear to have the effect of restricting glenohumeral external rotational range of motion relative to the Latarjet procedure performed without capsular repair.
Acknowledgments
Partial funding was provided by VA Rehabilitation Research and Development Merit Review and the John C. Griswold Foundation. The funding source did not play a role in the investigation.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Bankart AS, Cantab MC. Recurrent or habitual dislocation of the shoulder-joint: 1923. Clin Orthop Relat Res. 1993;(291):3–6. [PubMed] [Google Scholar]
- 2.Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994;76(12):1819–1826. doi: 10.2106/00004623-199412000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Kim SH, Ha KI, Cho YB, Ryu BD, Oh I. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003;85(8):1511–1518. [PubMed] [Google Scholar]
- 4.Petrera M, Patella V, Patella S, Theodoropoulos J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1742–1747. doi: 10.1007/s00167-010-1093-5. [DOI] [PubMed] [Google Scholar]
- 5.Tjoumakaris FP, Abboud JA, Hasan SA, Ramsey ML, Williams GR. Arthroscopic and open Bankart repairs provide similar outcomes. Clin Orthop Relat Res. 2006;446:227–232. doi: 10.1097/01.blo.0000205883.73705.19. [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 8.Porcellini G, Campi F, Pegreffi F, Castagna A, Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am. 2009;91(11):2537–2542. doi: 10.2106/JBJS.H.01126. [DOI] [PubMed] [Google Scholar]
- 9.Tauber M, Resch H, Forstner R, Raffl M, Schauer J. Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg. 2004;13(3):279–285. doi: 10.1016/j.jse.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49(8):994–997. [PubMed] [Google Scholar]
- 11.Giles JW, Boons HW, Elkinson I, et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22(6):821–827. doi: 10.1016/j.jse.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Wellmann M, de Ferrari H, Smith T, et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure. Arch Orthop Trauma Surg. 2012;132(3):377–386. doi: 10.1007/s00402-011-1425-z. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95(15):1390–1397. doi: 10.2106/JBJS.L.00777. [DOI] [PubMed] [Google Scholar]
- 14.Hovelius L, Sandstrom B, Olofsson A, Svensson O, Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg. 2012;21(5):647–660. doi: 10.1016/j.jse.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Barry TP, Lombardo SJ, Kerlan RK, et al. The coracoid transfer for recurrent anterior instability of the shoulder in adolescents. J Bone Joint Surg Am. 1985;67(3):383–387. [PubMed] [Google Scholar]
- 16.Schroder DT, Provencher MT, Mologne TS, Muldoon MP, Cox JS. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen. Am J Sports Med. 2006;34(5):778–786. doi: 10.1177/0363546505282618. [DOI] [PubMed] [Google Scholar]
- 17.Kephart CJ, Abdulian MH, McGarry MH, Tibone JE, Lee TQ. Biomechanical analysis of the modified Bristow procedure for anterior shoulder instability: is the bone block necessary? J Shoulder Elbow Surg. 2014;23(12):1792–1799. doi: 10.1016/j.jse.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Itoi E, Morrey BF, An KN. Biomechanics of the shoulder. In: Rockwood CA Jr, Matsen FA III, editors. The shoulder. 4th ed. Philadelphia: Saunders; 2009. pp. 223–268. [Google Scholar]
- 19.Lee TQ, Black AD, Tibone JE, McMahon PJ. Release of the coracoacromial ligament can lead to glenohumeral laxity: a biomechanical study. J Shoulder Elbow Surg. 2001;10(1):68–72. doi: 10.1067/mse.2001.111138. [DOI] [PubMed] [Google Scholar]
- 20.Tibone JE, McMahon PJ, Shrader TA, Sandusky MD, Lee TQ. Glenohumeral joint translation after arthroscopic, nonablative, thermal capsuloplasty with a laser. Am J Sports Med. 1998;26(4):495–498. doi: 10.1177/03635465980260040301. [DOI] [PubMed] [Google Scholar]
- 21.Walch G, Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg. 2000;1(4):256–261. [Google Scholar]
- 22.Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg. 2011;20(2 Suppl):S61–S69. doi: 10.1016/j.jse.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 23.Lee YS, Lee TQ. Specimen-specific method for quantifying glenohumeral joint kinematics. Ann Biomed Eng. 2010;38(10):3226–3236. doi: 10.1007/s10439-010-0074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hovelius L, Vikerfors O, Olofsson A, Svensson O, Rahme H. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J Shoulder Elbow Surg. 2011;20(7):1095–1101. doi: 10.1016/j.jse.2011.02.005. [DOI] [PubMed] [Google Scholar]