Abstract
Background
Shoulder humeral resurfacing is being performed in increasing numbers. We report the long-term outcome of patients with the Copeland mark III humeral resurfacing hemi-arthroplasty.
Methods
Ninety-five shoulder hemi-arthroplasties were performed in 85 patients, from 1994 to 2003. Oxford Shoulder Score (OSS) and short form 12 (SF-12) questionnaires were administered.
Results
At 12-year follow-up, 49 patients were alive. The OSS was 35.2 and SF-12 score was 83. There were 3 revision operations and 95% survivorship at 18 years.
Conclusion
This prosthesis has a low revision rate with few post-operative complications and good patient-reported outcome in an elderly population.
Keywords: Shoulder, Arthroplasty, Hemi-arthroplasty, Replacement, Functional outcome
1. Introduction
Arthritis of the shoulder is associated with significant morbidity and loss of function. While conservative management has a role, arthroplasty can provide significant pain relief and functional improvement.6, 7, 10, 14, 19, 23 With increasing number of patients undergoing primary shoulder arthroplasty5 and with an ageing population, long-term functional outcome is even more important.
Shoulder arthroplasty has evolved over the last 50 years since Neer introduced a stemmed prosthesis for four-part fractures in 1955.18 One of the more recent developments is resurfacing, which has the advantages of minimal bone resection, avoidance of humeral canal penetration and low risk of peri-prosthetic fracture. Resurfacing has been shown to be at least comparable to stemmed prostheses in terms of function.12, 13, 14 These replacements more accurately approximate the native shoulder geometry compared with stemmed options.9, 11
The Copeland hemi-arthroplasty (Biomet, Warsaw, Indiana) is a resurfacing prosthesis, which has itself evolved over the last 25 years undergoing two major improvements. The first prosthesis, developed in 1986, was the mark I, which had a central pegged metal humeral component and a polyethylene glenoid component with a finned peg. In 1990, this was superseded by the mark II prosthesis, which had a metal backed glenoid component, with both components having a fluted taper fit peg. The implant investigated in this report is the mark III, which was introduced in 1993. This most recent design features a cruciform tapered peg with porous titanium and hydroxyapatite coating.14
The majority of existing outcome studies14, 16, 17 have been reported by the group who developed the Copeland prosthesis. The purpose of this study is to evaluate the long-term outcome of the Copeland mark III humeral resurfacing replacement in a District General Hospital, and previous studies have included patients with total shoulder resurfacing; however, we provide the largest study group and the longest follow-up till date of shoulder resurfacing hemi-arthroplasty.
2. Materials and methods
There were 95 Copeland hemi-arthroplasty operations performed in 85 patients at our institution over a ten-year period (1994–2003). We obtained details of these patients from the hospital theatre register. Case-notes of the cohort were examined and details of each operation, complications and re-operations noted. The surviving patients were sent an Oxford Shoulder Score (OSS) questionnaire, a Short Form 12 (SF-12) questionnaire and a short questionnaire asking about satisfaction and any further surgery. Ethics committee approval was obtained prior to the commencement of the study.
The OSS was devised in 1996 as a patient-reported outcome measure.8 It comprises two sections, the first assessing pain and the second assessing function. The original scoring has been revised recently21 and now ranges from 0 to 48, with 48 being the best outcome. The functional score ranges from 0 to 32, and the pain score from 0 to 16. The OSS has the advantages of being short, with low respondent burden and is specific to shoulder pathology. It is also highly responsive to detecting change.3 The SF-12 score is an abbreviated version of the SF-36 score, which is used to assess physical and mental function. It is scored with the norm-based method, where the population mean is always 50 and a standard deviation 10. Using this system, an individual's score of less than 45 or a group score of less than 47 is considered below the average range.24
Statistics were performed in Microsoft Excel version 2007 (Microsoft, New York, NY, USA) and Statistical Package for the Social Sciences (SPSS) version 19.0 (SPSS Inc., Chicago, IL, USA). Data are given as means with standard deviations (SD) unless stated otherwise.
3. Surgical technique
The deltopectoral approach was used in order to preserve deltoid function. The patients were positioned in a “deck chair” position. A vertical incision was used, one centimetre lateral to the coracoid process. The Cephalic vein was identified in the deltopectoral interval. The conjoint tendon was partially divided to improve exposure. Subscapularis was then divided with capsule just medial to the insertion to the lesser tuberosity. The capsule was entered and the humeral head was dislocated and marginal osteophytes removed. The entry point was found by identifying the margins of the humeral articular surface, inserting a guide-wire and selecting the implant size.
After reaming, a trial prosthesis was reduced. The final prosthesis was inserted without cement, unless the bone stock was poor, in which case, Palacos cement (Heraeus, Hanau, Germany) was used. During closure, subscapularis and the partially divided conjoint tendon were repaired and the deltopectoral groove reconstructed.
4. Results
Of the 85 patients (95 shoulders), 36 patients (38 shoulders) had died and 40 patients (46 shoulders) responded with functional outcome information. 9 patients (11 shoulders) were still alive but were lost to follow-up. Therefore, there was an 80.7% response rate.
Of the deceased patients, 36 shoulders had osteoarthritis (OA) and 2 shoulders had rheumatoid arthritis. None of the deaths were directly related to shoulder surgery. The deceased patients accounted for 42.4% (36 shoulders) of the cohort. 10 were male and 26 were female. They had a mean age of 73 years (8) at operation and a mean age of 81 years (9.3) at death. Of those lost to follow-up, 8 were female, 1 was male and none had any complications reported in the case-notes.
Of the 40 patients that responded, 6 had bilateral operations resulting in 46 shoulders. In this group, there were 40 shoulders with osteoarthritis, 2 with rheumatoid arthritis, 1 with instability, 2 with rotator cuff disease and 1 with avascular necrosis. There were 9 male respondents and 31 female respondents. The mean age was 67 years (SD: 11; range: 35–82). Mean follow-up length was 12 years (SD: 3; range: 8.7–18.0).
4.1. Satisfaction
The mean overall satisfaction score from our questionnaire was 1.5 (SD: 0.81), where 1 is very satisfied and 4 is very dissatisfied.
4.2. Oxford Shoulder Score
The mean OSS was 35.2 (SD: 8.54; range: 17–48). The mean functional score was 24.3 (6.0) and the mean pain score was 11.3 (3.8). The scores were good for all pathologies except for rotator cuff disease, which had a mean OSS of 23.0 (0). The OA group had a mean score of 35.8 (9) (Table 1). The numbers in the individual groups were too small to provide statistical comparison; however, there was no significant difference between OA and non-OA groups (p = 0.4). The male sub-group had a mean OSS of 38.9 (5.56) and the female sub-group had a mean OSS of 33.5 (9.01). The difference was not statistically significant (p = 0.11).
Table 1.
Oxford Shoulder Scores by primary pathology (values are means and standard deviations).
| Pathology | Number of shoulders | Oxford Shoulder Score |
||
|---|---|---|---|---|
| Function | Pain | Overall | ||
| Osteoarthritis | 40 | 24.6 (6) | 11.3 (4) | 35.8 (9) |
| Rheumatoid arthritis | 2 | 19.5 (2.1) | 14.0 (1.4) | 33.5 (2.5) |
| Rotator cuff pathology | 2 | 16.0 (0) | 7.0 (0) | 23.0 (0) |
| Instability | 1 | 25.0 (0) | 9.0 (0) | 34.0 (0) |
| Avascular necrosis | 1 | 27.0 (0) | 10.0 (0) | 37.0 (0) |
4.3. General health and satisfaction
The mean SF-12 score was 83 (15.5). The mean physical score was 33.2 (11.8) and the mean mental score was 49.8 (10.1). Overall, 88% were very satisfied with their shoulder outcome, with 88% able to do housework or gardening and 85% able to do recreational activities.
4.4. Revision
There were three revision operations during the study period. Patient one, a 70-year-old female, 11 years after her index procedure developed an atraumatic peri-prosthetic fracture. Two months later, she underwent a revision to a reversed geometry total shoulder replacement. Patient two was a 52-year-old man who sustained a peri-prosthetic fracture after trauma 12 years and 2 months after his index operation and underwent a revision procedure. Patient three, who was lost to follow-up, fell 2 years and 3 months after her Copeland hemi-arthroplasty and suffered a fracture of her greater tuberosity. This failed to unite with conservative management and after 10 months was revised to a total shoulder replacement.
4.5. Complications
Excluding the three revision patients, there was one other complication. This patient, now deceased, suffered a peri-prosthetic fracture after a fall, 3 years and 11 months after her original surgery. This fracture successfully healed after fixation with a humeral locking plate. There were no nerve injuries, infections or dislocations in this cohort.
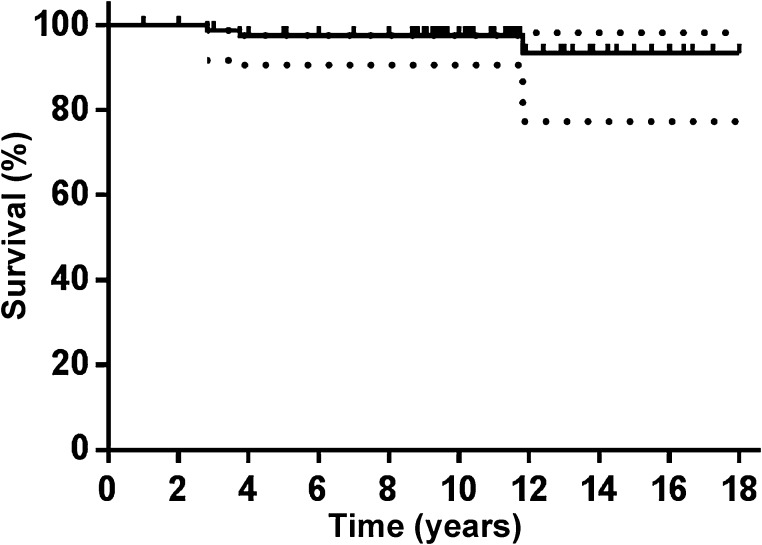
4.6. Survivorship
A Kaplan–Meier survival analysis was undertaken to estimate implant survivorship (Fig. 1). It showed a 10-year survival of 97.5% (90.5–99.4, 95% CI), a 15-year survival of 95.0% (84.0–98.5, 95% CI) and an 18-year survival of 95.0% (84.0–98.5, 95% CI).
Fig. 1.
Kaplan–Meier survival curve with revision as the endpoint (dotted lines represent 95% confidence limits).
5. Discussion
We have shown a good long-term outcome with the mark III Copeland prosthesis. While it is crucial to distinguish between different prostheses when discussing outcome, it is also important to distinguish between different versions of a prosthesis, since even a small change in design can have a significant influence on outcome. In the case of the Copeland prosthesis, there have been 4 versions (mark I–mark IV), with this study examining the mark III. Since there are only three previous studies specific to the mark III prosthesis,1, 17, 22 we also discuss reports on other versions, although direct comparison needs to be considered with caution.
The OSS in our group is 35.2 (8.54) at 12 years, which is lower than the 42 (range: 18–48) reported by Al-Hadithy et al.,1 who also examined the mark III Copeland prosthesis but this was after a shorter follow-up of 4.2 years. Al-Hadithy also reported the mean Constant score, which was 62.5. The only other study to use the OSS was that by Alizadehkhaiyat et al.,2 who investigated the mark IV Copeland prosthesis in a population with a mean age of 66.5 years and reported an OSS of 28 at mean follow-up of 4.0 years. Our patient group had a mean physical score (PCS) on SF-12 of 33.2 (SD: 11.8) and a mean mental score (MCS) on SF-12 of 49.8 (SD: 10.1). This represents a similar general health of our patients to those studied by Alizadehkhaiyet et al.,2 who reported a PCS of 29.5 (SD: 10) and a MCS of 54.7 (SD: 13.3).
The work of others4, 14, 15, 17, 22 is more difficult to compare directly to the current study due to their use of Constant scores rather than OSS to describe functional outcome. These studies reported a mean Constant score ranging from 52 to 63.4, 14, 15, 17, 22
While the majority of studies report results of a single version of the Copeland prosthesis, Levy and Copeland15 reported a cohort of patients, which included the mark I, II and III prostheses, with the exact breakdown not being evident from the paper. They do, however, differentiate those patients receiving a hemi-arthroplasty from those receiving a total shoulder arthroplasty. The 37 hemi-arthroplasty patients, with a mean age of 73.4 years, had a mean Constant score of 58.1 at 4.4 years, while the 42 patients with a total shoulder replacement, with a mean age of 71.5 years, reported a Constant score of 61.9 at 7.6 years.
Our patient cohort comprises predominantly patients with osteoarthritis but also includes patients with rheumatoid arthritis, cuff arthropathy, avascular necrosis and arthropathy from instability. While patients with differing pathologies are likely to have different outcomes, our numbers in the various categories are too small to make meaningful comparison, but instead reflect the case mix present in our practice. It is worth noting that Levy and Copeland14 reported better results with primary osteoarthritis compared to patients with cuff arthropathy or those with arthropathy following septic arthritis. Mullet et al.17 also reported better outcome in patients with primary osteoarthritis than cuff arthropathy.
In terms of functional outcome, 88% of patients in our study group could manage household work and 85% maintained recreational activity at follow-up. There was good pain relief, with 94% of patients satisfied with pain relief from surgery using our own questionnaire and a mean pain score (on the OSS) of 11.0 out of 16 (scale of 0 to 16, with 16 being the least painful). This compares to Levy and Copeland14 who reported a mean score of 13.7 (scale of 3–15, where 15 is the least painful) in patients who had the Copeland mark I prosthesis implanted for osteoarthritis.
There was an overall satisfaction of 88% at 12 years in the current study, which is comparable to the 97.2% (35 out of 36 patients) at 2 years reported by Bailie et al.4 and the 95% at 20 years in the study by Pritchett20 who reported on 33 Depuy (Warsaw, Indiana) and Howmedica (Rutherford, New Jersey) resurfacing hemi-arthroplasty operations in 2011 in a younger cohort of patients (mean age: 58 years). However, it is worth noting that revision patients were excluded in calculations of satisfaction in Pritchett's study. Alizadehkhaiyat et al.2 reported an 85% satisfaction rate, based on those scoring more than 5 out of 10, on a visual analogue scale. Mullet et al.,17 reporting on the Copeland mark III resurfacing, did not report the percentage of patients satisfied, but did report a mean satisfaction of 8.4 out of 10 (range: 6.3–10).
In the current study, there was a 4% (3 of 84 shoulders) revision rate, with one additional patient requiring open reduction and internal fixation of a humeral fracture. There has been a 2–3% revision rate reported for the mark III prosthesis by non-originator centres1, 17, 22 and a higher 5–6% revision rate reported by the originator centre.14, 15 While a high rate of revision of 26% was reported by Alizadehkhaiyat et al.2 for the mark IV prosthesis. The low revision rate in the current study may in part be due to adverse radiological features not being as readily identified as in other studies. Complications recorded in the current study were low, especially when compared to Levy and Copeland,14, 15 which may reflect closer monitoring of patients following surgery from the originator centre, and possibly a lower threshold for diagnostic surgery to investigate pain and a lower revision threshold. Furthermore, the retrospective nature of the current study is likely to under-report transient and minor complications.
Additional limitations of the current study may be considered to be the absence of radiological follow-up. However, usage of patient-reported outcome measures is of more relevance in an elderly population, since the primary concern in this demographic is patient satisfaction, pain relief, function and requirement for further surgery. After a follow-up of 12 years, these patients are often resident in nursing homes with poor general health. Inviting them back for radiological and clinical assessment is often not feasible, and indeed can be difficult to justify. Such a problem has been noted by previous authors.14, 17 If patients are satisfied with their prosthesis and quality-of-life, then the arthroplasty has served its purpose. With this rationale in mind, recording specific values for range of movement are of less value in these patients.
Overall, the long-term outcome of our shoulder resurfacing hemi-arthroplasties is good in terms of relieving pain and restoring function, with few serious complications and infrequent need for revision surgery. While it has been suggested that an older population would have a much greater risk of medical complications, problems with instability and poor healing,17 this study does not support this. No significant medical morbidity associated with surgery was found in this group and there was a low rate of complications compared to previous studies. For the group that did need revision surgery, this was on the whole easily achieved due to the preservation of bone stock and outcome was good with their OSS ranging from 36 to 48.
6. Conclusion
The present study provides long-term follow-up of the mark III Copeland resurfacing hemi-arthroplasty, showing good results in an elderly population, with few complications and a low revision rate. While we cannot comment on the use of the prosthesis in a young population, we do recommend it in an elderly patient group.
Conflicts of interest
The authors have none to declare.
References
- 1.Al-Hadithy N., Domos P., Sewell M.D., Naleem A., Papanna M.C., Pandit R. Cementless surface replacement arthroplasty of the shoulder for osteoarthritis: results of fifty Mark III Copeland prosthesis from an independent center with four-year mean follow-up. J Shoulder Elbow Surg. 2012;21:1776–1781. doi: 10.1016/j.jse.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 2.Alizadehkhaiyat O., Kyriakos A., Singer M.S., Frostick S.P. Outcome of Copeland shoulder resurfacing arthroplasty with a 4-year mean follow-up. J Shoulder Elbow Surg. 2013;22:1352–1358. doi: 10.1016/j.jse.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 3.Angst F., Schwyzer H., Aeschlimann A., Simmen B., Goldhahn J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and Its Short Version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society Standardized Shoulder Assessment Form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI) Arthritis Care Res. 2011;63(suppl 11):S174–S188. doi: 10.1002/acr.20630. [DOI] [PubMed] [Google Scholar]
- 4.Bailie D.S., Llinas P.J., Ellenbecker T.S. Cementless humeral resurfacing arthroplasty in active patients less than fifty-five years of age. J Bone Joint Surg Am. 2008;90:110–117. doi: 10.2106/JBJS.F.01552. [DOI] [PubMed] [Google Scholar]
- 5.Bergen H. Department of Orthopaedic Surgery, Haukeland University Hospital; 2010. The Norwegian Arthroplasty Register Report 2010. [Google Scholar]
- 6.Boileau P., Walch G., Noel E., Liotard J.P. Neer's shoulder prosthesis: results according to etiology. Rev Rhum Ed Fr. 1994;61:607–618. [in French] [PubMed] [Google Scholar]
- 7.Cofield R.H. Total shoulder arthroplasty with the Neer prosthesis. J Bone Joint Surg Am. 1984;66A:899–906. doi: 10.2106/00004623-198466060-00010. [DOI] [PubMed] [Google Scholar]
- 8.Dawson J., Fitzpatrick R., Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78:593–600. [PubMed] [Google Scholar]
- 9.Deladerriere J.Y., Szymanski C., Vervoort T., Budzik J.F., Maynou C. Geometrical analysis results of 42 resurfacing shoulder prostheses: a CT scan study. Orthop Traumatol Surg Res. 2012;98:520–527. doi: 10.1016/j.otsr.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Haines J.F., Trail I.A., Nuttall D., Birch A., Barrow A. The results of arthroplasty in osteoarthritis of the shoulder. J Bone Joint Surg Br. 2006;88B:496–501. doi: 10.1302/0301-620X.88B4.16604. [DOI] [PubMed] [Google Scholar]
- 11.Hammond G., Tibone J.E., McGarry M.H., Jun B.J., Lee T.Q. Biomechanical comparison of anatomic humeral head resurfacing and hemiarthroplasty in functional glenohumeral positions. J Bone Joint Surg Am. 2012;94:68–76. doi: 10.2106/JBJS.I.00171. [DOI] [PubMed] [Google Scholar]
- 12.Jensen K.L. Humeral resurfacing arthroplasty: rationale, indications, technique, and results. Am J Orthop. 2007;36(suppl 1):4–8. [PubMed] [Google Scholar]
- 13.Levy O. Shoulder resurfacing: is it really as good as total shoulder replacement? Curr Orthop Pract. 2012;23:2–9. [Google Scholar]
- 14.Levy O., Copeland S.A. Cementless surface replacement arthroplasty of the shoulder: 5- to 10-year results with the Copeland mark-2 prosthesis. J Bone Joint Surg Br. 2001;83B:213–221. doi: 10.1302/0301-620x.83b2.11238. [DOI] [PubMed] [Google Scholar]
- 15.Levy O., Copeland S.A. Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg. 2004;13:266–271. doi: 10.1016/j.jse.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Levy O., Funk L., Sforza G., Copeland S.A. Copeland surface replacement arthroplasty of the shoulder in rheumatoid arthritis. J Bone Joint Surg Am. 2004;86A:512–518. doi: 10.2106/00004623-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Mullett H., Levy O., Raj D., Even T., Abraham R., Copeland S.A. Copeland surface replacement of the shoulder: results of an hydroxyapatite-coated cementless implant in patients over 80 years of age. J Bone Joint Surg Br. 2007;89B:1466–1469. doi: 10.1302/0301-620X.89B11.18850. [DOI] [PubMed] [Google Scholar]
- 18.Neer C.S. Articular replacement for the humeral head. J Bone Joint Surg Am. 1955;37A:215–228. [PubMed] [Google Scholar]
- 19.Neer C.S., Watson K.C., Stanton F.J. Recent experiences in total shoulder replacement. J Bone Joint Surg Am. 1982;64A:319–337. [PubMed] [Google Scholar]
- 20.Pritchett J.W. Long-term results and patient satisfaction after shoulder resurfacing. J Shoulder Elbow Surg. 2011;20:771–777. doi: 10.1016/j.jse.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 21.Rees J.L., Dawson J., Hand G.C. The use of patient-reported outcome measures and patient satisfaction ratings to assess outcome in hemiarthroplasty of the shoulder. J Bone Joint Surg Br. 2010;92:1107–1111. doi: 10.1302/0301-620X.92B8.22860. [DOI] [PubMed] [Google Scholar]
- 22.Thomas S.R., Wilson A.J., Chambler A., Harding I., Thomas M. Outcome of Copeland surface replacement shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14:485–491. doi: 10.1016/j.jse.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Torchia M.E., Cofield R.H., Settergren C.R. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6:495–505. doi: 10.1016/s1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 24.Ware J., Kosinski M., Keller S.D. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]