Abstract
Purpose
To compare short and mid-term results in the treatment of chronic elbow tendinosis with platelet-rich plasma (PRP) or Nirschl surgical technique.
Method
A retrospective study was conducted on patients with chronic lateral epicondylitis, treated by Nirschl surgical technique (50 elbows) or PRP (60 elbows). Outcome was evaluated with Visual Analog Score (VAS), Mayo Elbow Scores and grip strength measurements.
Results
VAS and Mayo Elbow Scores of the PRP group had improved as a mean of 83% (p = 0.0001), 74% (p = 0.0001) over baseline and 34.2 pounds gain of grip strength.
Conclusion
The PRP seems to be better for pain relief and functionality in the short and mid-term periods.
Keywords: Nirschl surgical technique, Platelet rich plasma (PRP), Chronic elbow tendinosis
1. Introduction
Elbow epicondylar tendinosis is a common problem for patients, whose activities require strong gripping or repetitive wrist movements. Histologic specimens from chronic cases confirm that tendinosis is not an acute inflammatory condition but rather a failure of the normal tendon repair mechanism associated with angiofibroblastic degeneration.1 The cause of elbow tendinosis is most likely a combination of mechanical overloading and abnormal microvascular responses.2, 3 Nirschl and Pettrone identified the primary pathologic alteration in the extensor carpi radialis brevis (ECRB), termed histologically as angiofibroblastic hyperplasia. The term was subsequently modified to angiofibroblastic tendinosis and has been theorized to be a degenerative process, as no inflammatory cells are identified histologically.4 Nirschl and Pettrone reported on 1213 clinical elbow cases with 88 surgical interventions. At surgery, identification and excision of the tendinosis tissue within the ECRB were undertaken, with anatomical repair of the normal tissues: extensor carpi radialis longus (ECRL) and extensor digitorum communis (EDC).5
Numerous methods have been advocated for treating elbow tendinosis, including rest, nonsteroidal anti-inflammatory medication, bracing, physical therapy, iontophoresis, extracorporeal shock wave therapy, and botulism toxin.6, 7 Injections of corticosteroids or whole blood and various types of surgical procedures have also been recommended.8 The utility of several of these treatments has recently come into question. Recently, platelet-rich plasma (PRP) is promoted as an ideal autologous biological blood-derived product that can be exogenously applied to various tissues, where it releases high concentrations of platelet-derived growth factors that enhance wound healing, bone healing, and tendon healing.9 In addition, PRP possesses antimicrobial properties that may contribute to the prevention of infections.10, 11 When platelets become activated, growth factors are released and initiate the body's natural healing response. The use of PRP for healing purposes was first popularized in maxillofacial and plastic surgery in the 1990s.4 Its use in orthopedics started later and it is increasing.6 Laboratory and clinical studies of PRP use on tendons, ligaments, muscle, bone, and cartilage are already published.5 A further research into the precise cause of tendinosis is, however, still needed.
Our hypothesis was that the PRP technique is better than open surgical release of the ECRB for lateral epicondylitis. Therefore, the purpose of this study was to review and compare the short and mid-term results of the Nirschl surgical technique for lateral epicondylitis by resection of tendinosis tissue within the ECRB with repair of the ECRL-EDC interface with PRP as a potential new treatment for chronic severe elbow tendinosis.
2. Materials and methods
This study is a third level of evidence, retrospective cohort study, was conducted on patients with chronic lateral epicondylitis whom were treated by open surgical Nirschl technique (44 patients, 55 elbows) or PRP (36 patients, 60 elbows) from February 2011 to December 2012. Patients with bilateral lateral epicondylitis were operated or treated with PRP injection one by one with a 3 months interval. Inclusion criteria were as follows: patients with suggestive symptoms of lateral epicondylitis (point tenderness, decreased grip strength and pain with resisted wrist extension), of at least twelve months of duration and unresponsive to a course of at least six months of conservative treatment including non-steroidal anti-inflammatory drugs, physical therapy modalities, corticosteroid injections and splints. The ethics committee of the hospital approved this study. Written informed consent was obtained from each patient before enrollment.
3. Surgical technique
All procedures were performed on an out-patient basis and carried out by the same investigator (MA) by means of lateral release technique as previously described by Nirschl.4 The visualization of the ECRB origin was facilitated by horizontal dissection of the ECRL off the ECRB. The tendinosis tissue within the ECRB was identified by its gray, edematous, and friable nature. All tendinosis tissue was resected sharply. A scratch maneuver was then performed using the scalpel to scrape away any remaining tendinosis tissue while leaving the normal tendon intact. If present, tendinosis tissue within the anterior edge of the EDC is resected as well. To enhance the vascular supply, a single drill hole was placed into the anterior lateral condyle but not into the lateral epicondyle. The extensor aponeurosis was then repaired to the ECRL using interrupted buried no. 1 polydioxanone suture. Postoperatively, an elbow immobilizer in 90° of flexion with the forearm in neutral rotation was applied for 48 h. Light activities of daily living and office work were resumed in 3–5 days. Strengthening with lightweights was allowed at 3 weeks. A counterforce brace was used while exercising. Gradual return to sports such as tennis was initiated 5–6 weeks from surgery.
4. PRP technique
By using a centrifuge type system (Biomet Biologics GPS III, Warsaw, IN), PRP injections were done by the same investigator (MK). This method requires drawing 54 mL of whole blood with 6 mL of anticoagulant from a peripheral vein. The blood was then placed in a plastic cylinder inside a centrifuge for 15 min at 3200 rpm. This action separates the blood into platelet-poor plasma, red blood cells, and PRP. It is a simple and reproducible method of producing at least 5 times baseline platelets in an office, surgery center, or hospital. With the use of these methods, 6 mL of PRP was obtained and then buffered to physiologic pH with the use of sodium bicarbonate. The lateral epicondylar region was sterilely prepared and injected with a local anesthetic, and 5–6 mL of PRP was then injected into and around echographically identified extensor tendon with inflammatory findings by use of a peppering technique. Approximately 0.5 mL was placed deep to the extensor tendon, 1–2 mL was placed into and around the tendon, and an additional 0.5 mL can be placed in the dermal layer. After the injection, the patient was kept in the supine position for 15 min to allow for binding of the PRP to the tendon. The patient was then given a home-based stretching and strengthening program to begin 48 h after the injection. No anti-inflammatory medication was allowed for 4 weeks. The patient was then followed at monthly intervals and allowed to return to activities as tolerated.
The subjects were evaluated five times. They were first evaluated just before the procedure and than follow-up examinations were carried out at outpatient clinic at first month, second month, 6th month and one year follow-ups. The evaluation included the following components: Visual Analog Scale (VAS) from 0 mm (no symptoms) to 100 mm (the most intense symptoms), a modified Mayo Elbow Score (best score, 100 points) and grip strength gain measurement (0–200 Ib) (using a hydraulic hand dynamometer according to the American Society of Hand Therapists guidelines).12 Baseline® HiRes Hydraulic Hand Dynamometer (Fabrication Enterprises Inc., NY, USA) was used for grip strength measurement.
During follow-up examinations, all patients reported complete compliance with the recommended post-procedure exercise program. All patients’ rehabilitations were done by the same physical therapist according to the same rehabilitation protocol.
4.1. Statistical analysis
Using SPSS 15.0 software, we compared the following parameters: VAS Scores and Mayo Elbow Scores of patients treated with PRP and Nirschl technique, respectively. The outcome measures for severity of complaints, and the change scores (difference between baseline and follow-up) were calculated for each elbow separately. Statistical analysis was performed using the paired Student-t test with two-tailed distribution and the nonparametric χ2 test with the significance level set at p < 0.05.
5. Results
Of the 88 subjects who met the inclusion criteria, 8 were lost to follow-up and excluded from the study. Characteristics of the remaining 80 subjects are presented in Table 1. There were no significant differences between groups in terms of age, gender, hand dominance, intervention on dominant extremity, preoperative VAS, Mayo Elbow Scores and baseline grip strength measurements and duration of follow-up (p > 0.05). No complications were noted in either group at the treatment period. Specifically, there were no infections, neurovascular complications, or worsening of the patients’ lateral elbow pain.
Table 1.
Comparative demographics of PRP and surgery groups.
| No. or average (range) |
||
|---|---|---|
| PRP | Surgery | |
| No. of patients | 36 | 44 |
| No. of elbows | 60 | 50 |
| Sex | ||
| M | 22 | 28 |
| F | 14 | 16 |
| Age | 63.7 (58–72) | 65.2 (60–78) |
| Dominance | ||
| Right hand | 24 | 26 |
| Left hand | 8 | 10 |
| Ambidextrous | 4 | 8 |
| Intervention on dominant extremity | ||
| Yes | 22 | 32 |
| No | 12 | 8 |
| Ambidextrous | 2 | 4 |
| Initial Visual Analog Pain Score | 70.3 (60–100) | 75.3 (80–100) |
| Initial Mayo Elbow Score | 50.3 (38–68) | 50 (43–53) |
| Initial Grip Strength (pounds) | 52.7 (20–76) | 54.6 (24–76) |
| Follow-up duration, weeks | 56.7 (54–62) | 55.7 (54–58) |
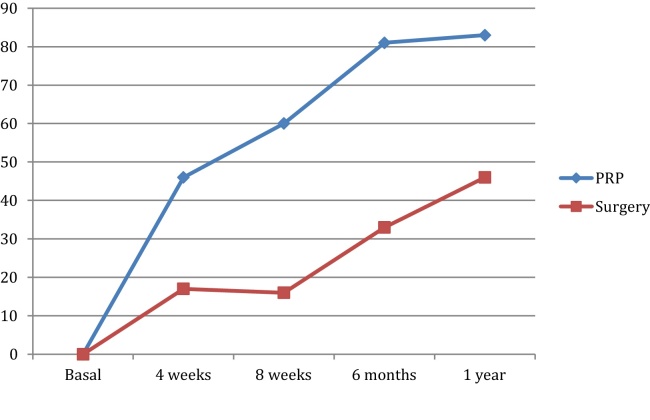
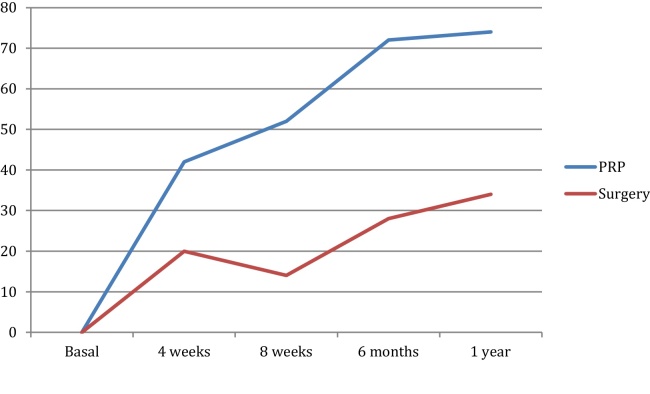
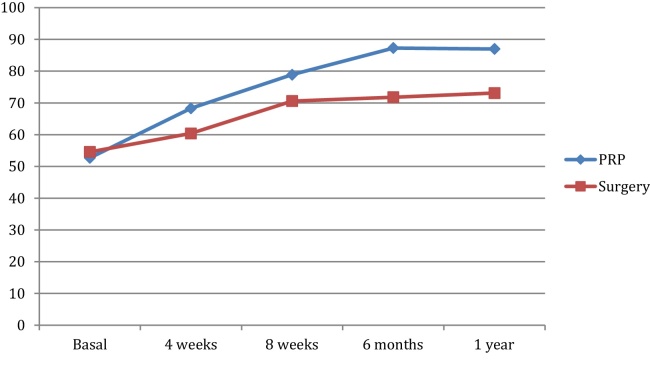
Results of outcome measures are presented in Fig. 1, Fig. 2, Fig. 3. Four weeks after these procedures, PRP group reported a mean of 46% improvement (70.3–37.9) in their VAS and Nirschl group reported 17% improvement (75.3–62.5); (p = 0.028). Also, after 4 weeks, Mayo Elbow Scores had improved 42% (50.3–71.3) in PRP group versus a 20% improvement (49.5–59.5) in Nirschl group patients (p = 0.120). Grip strength gain measurements were 15.6 pounds in PRP group, 5.8 pounds in surgery group after 4 weeks. Two months and six months after the treatment, PRP group reported a better improvement than Nirschl group in both their mean VAS and Mayo Elbow Scores (60%, 81% and 52%, 72% vs. 16%, 33% and 14%, 28%; p < 0.05, p < 0.05, respectively). Two and six months follow-up grip strength gain measurements were respectively: 26.2, 34.6 pounds for PRP group and 16, 17.2 pounds for Nirschl group (p < 0.05). At the last follow-up as one year after treatment, VAS and Mayo Elbow Scores of the PRP group had continued to improve a mean of 83% (p = 0.0001) and 74% (p = 0.0001) over baseline grip strength gain was 34.3 pounds. However, functional assessment of the Nirschl group at the last follow-up demonstrated 46% and 34% improvement in their VAS and Mayo Elbow Scores respectively, and 18.5 pounds for gain of grip strength.
Fig. 1.
Visual Analog Score improvement of PRP and surgery groups (%).
Fig. 2.
Mayo Elbow Score improvement of PRP and surgery groups (%).
Fig. 3.
Grip strength measurement improvement of PRP and surgery groups (pounds).
6. Discussion
During the last decade, there has been a transition to use of PRP injection for treatment of various tendinopathies.13, 14 PRP injection has advantages, including being a bioactive component of whole blood that composed of many growth factors and safe because of its autologues nature. Increasing the local regenerative stimulus for tendon healing is thought to be the main advantage of PRP application, but this has not been substantiated.10, 15, 16 Because of controversy regarding release and debridement with pain relief, we wished to compare surgical release or PRP injection in patients with lateral epicondylitis regarding (1) residual pain at the end of follow-up; and (2) functional improvement like grip strength.
Our study has limitations including lack of randomization, lack of anatomic data, and small sample size. First, there were two different surgeons who performed these two kinds of procedures. Our senior surgeon performed surgical treatment and it is difficult to know what influence this might have had in this analysis. It is possible that surgeon selection bias could have influenced patients’ early postoperative pain experience but could not effect grip strength measurements. However, also there were no differences between groups in the influential preoperative variables that we measured. Finally, our patient cohort was relatively small and a short and mid-term follow-up analysis was performed. Pain analysis, a subjective outcome, also has significant variability between individuals and requiring large sample sizes to detect differences. Despite these limitations, our results indicate that surgical method influenced early postoperative pain scores and PRP injection provided a rapid improvement in both pain scores and grip strength measurements.
The main findings of this study are that PRP injection resulted in better pain control and that the functional improvement was stable and maintained up to a mid-term follow-up. Functional improvement was significantly insensible and late in operated patients. Elbow epicondylar tendinosis is a common problem with many possible treatments. Quick cessation of symptoms is important to patients and is economically advantageous. If neither rest nor simple treatments do not provide a satisfactory remedy, a patient may pursue several other options. The most commonly recommended treatment is physical therapy. A recent meta-analysis of physical therapy, however, noted that there is insufficient evidence to conclude that it has any lasting value.17 Corticosteroid injections have also been used extensively for this problem, but studies showed that there is conflicting evidence about their efficacy.1, 18 Jobe and Ciccotti1 also concluded that superficial injection of corticosteroid may result in subcutaneous atrophy and that intratendinous injection may lead to permanent adverse changes within the ultrastructure of the tendon. Despite these issues, corticosteroid is still widely in use. Hill et al. surveyed 400 members of the American Academy of Orthopaedic Surgeons and found that 93% had given a corticosteroid injection for elbow epicondylitis. Extracorporeal shock wave therapy also has recently gained popularity. A recent randomized double-blind study, however, showed that this treatment is no better than placebo.19
The data supporting the use of PRP autograft procedure (instead of corticosteroid injection) for chronic tendinosis are just beginning to emerge. There is, however, a prospective randomized trial that provides evidence that PRP is better than corticosteroid injection.13 Although both treatments provide relief of pain, corticosteroid injection provided only transient improvement. PRP therapy, however, has been shown to produce lasting improvement. Mechanistically, this is likely the result of improvement in the tendon tissue quality as has been shown by in vitro and animal studies.4, 8 PRP contains many growth factors and therefore induces angiogenesis, dilatation of choke vessels, and regeneration of injured tissues. To improve the absorption and increase the efficacy of PRP, we injected the PRP directly into the peppered tendon. In clinical practice, surgeons commonly have used activated platelets pretreated with thrombin and/or calcium to induce an immediate and full release of soluble factors. As Scherer et al.20 showed the nonactivated platelets is better in tissue healing, we used nonactivated PRP direct injection with a fine needle and even distribution were possible.
There was a trend for increased early postoperative pain in patients in the first week, who had an open debridement, and this condition can be explained by the natural result of the technique itself, but the pain relief at the PRP injection group was nearly 3-fold better at the end of first month. While this difference reached statistical significance in the first week and remained till the last visit, the differences in this analysis met the threshold of a clinically important difference. This suggests that the PRP therapy seems to be better for pain relief in the short and mid-term periods, quicker improvement in grip strength and this amelioration likely will continue in the long term.
7. Conclusion
Although it is an invasive method, it has many advantages in that. It is less time consuming and has an autologous nature with easy application. We believe that PRP injection should be offered to all patients with lateral epicondylitis. Further comparative studies are required to evaluate the long-term outcomes.
Ethical approval
Details: 122012/186, 09/January/2013, Ankara Kecioren TRH.
Conflicts of interest
The authors have none to declare.
Acknowledgements
The authors recognize the help of Bilge Duran Karaduman, M.D., for the statistical analysis. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Jobe F., Ciccotti M. Lateral and medial epicondylitis of the elbow. J Am Acad Orthop Surg. 1994;2:1–8. doi: 10.5435/00124635-199401000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Wang J., Iosifidis M., Fu F. Biomechanical basis for tendinopathy. Clin Orthop Relat Res. 2006;443:320–332. doi: 10.1097/01.blo.0000195927.81845.46. [DOI] [PubMed] [Google Scholar]
- 3.Smith R., Papadopolous E., Mani R., Cowley M.I. Abnormal microvascular responses in lateral epicondylitis. Br J Rheumatol. 1994;33:1166–1168. doi: 10.1093/rheumatology/33.12.1166. [DOI] [PubMed] [Google Scholar]
- 4.Nirschl R.P., Pettrone F. Tennis elbow: the surgical treatment of lateral epicondylitis. J Bone Jt Surg. 1979;61:832–841. [PubMed] [Google Scholar]
- 5.Regan W., Wold L.E., Coonrad R., Morrey B.F. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med. 1992;20:746–749. doi: 10.1177/036354659202000618. [DOI] [PubMed] [Google Scholar]
- 6.Nirschl R., Rodin D., Ochiai D., Maartmann-Moe C. Iontophoretic administration of dexamethasone sodium phosphate for acute epicondylitis: a randomized, double-blinded, placebo-controlled study. Am J Sports Med. 2003;31:189–195. doi: 10.1177/03635465030310020601. [DOI] [PubMed] [Google Scholar]
- 7.Keizer S., Rutten H., Pilot P., Morré H.H., v Os J.J., Verburg A.D. Botulinum toxin injection versus surgical treatment for tennis elbow. Clin Orthop Relat Res. 2002;401:125–131. doi: 10.1097/00003086-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Hill J., Trapp R., Colliver J. Survey on the use of corticosteroid injections by orthopedists. Contemp Orthop J. 1989;18:39–45. [Google Scholar]
- 9.Samson S., Gerhardt M., Mandelbaum B. Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskelet Med. 2008;1:165–174. doi: 10.1007/s12178-008-9032-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Everts P.A., Overdevest E.P., Jakimowicz J.J. The use of autologous platelet-leukocyte gels in enhancing the healing process in surgery: a review. Surg Endosc. 2007;21:2063–2068. doi: 10.1007/s00464-007-9293-x. [DOI] [PubMed] [Google Scholar]
- 11.Foster T.E., Puskas B.L., Mandelbaum B.R., Gerhardt M.B., Rodeo S.A. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37:2259–2271. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 12.Fess E.E. Grip strength. In: Casanova J.S., editor. Clinical Assessment Recommendations. 2nd ed. American Society of Hand Therapists; Chicago: 1992. pp. 41–45. [Google Scholar]
- 13.Tonk G., Kumar A., Gupta A. Platelet rich plasma versus laser therapy in lateral epicondylitis of elbow. Indian J Orthop. 2014;48:390–393. doi: 10.4103/0019-5413.136260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zargar Baboldashti N., Poulsen R.C., Franklin S.L., Thompson M.S., Hulley P.A. Platelet-rich plasma protects tenocytes from adverse side effects of dexamethasone and ciprofloxacin. Am J Sports Med. 2014;39:1929–1935. doi: 10.1177/0363546511407283. [DOI] [PubMed] [Google Scholar]
- 15.Boswell S.G., Cole B.J., Sundman E.A., Karas V., Fortier L.A. Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy. 2012;28:429–439. doi: 10.1016/j.arthro.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 16.Hsu W.K., Mishra A., Rodeo S.R. Platelet-rich plasma in orthopaedic applications: evidence-based recommendations for treatment. J Am Acad Orthop Surg. 2013;21:739–748. doi: 10.5435/JAAOS-21-12-739. [DOI] [PubMed] [Google Scholar]
- 17.Kon E., Filardo G., Delcogliano M. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper's knee. Injury. 2009;40:598–603. doi: 10.1016/j.injury.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 18.Filardo G., Kon E., Di Matteo B. Platelet-rich plasma injections for the treatment of refractory Achilles tendinopathy: results at 4 years. Blood Transfus. 2014;12:533–540. doi: 10.2450/2014.0289-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeong D.U., Lee C.R., Lee J.H. Clinical applications of platelet-rich plasma in patellar tendinopathy. BioMed Res Int. 2014:249498. doi: 10.1155/2014/249498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scherer S.S., Tobalem M., Vigato E. Nonactivated versus thrombin-activated platelets on wound healing and fibroblast-to-myofibroblast differentiation in vivo and in vitro. Plast Reconstr Surg. 2012;29:46e–54e. doi: 10.1097/PRS.0b013e3182362010. [DOI] [PubMed] [Google Scholar]