Abstract
Myalgic Encephalomyelitis (ME) continues to cause significant morbidity worldwide with an estimated one million cases in the United States. Hurdles to establishing consensus to achieve accurate evaluation of patients with ME continue, fueled by poor agreement about case definitions, slow progress in development of standardized diagnostic approaches, and issues surrounding research priorities. Because there are other medical problems, such as early MS and Parkinson’s Disease, which have some similar clinical presentations, it is critical to accurately diagnose ME to make a differential diagnosis. In this article, we explore and summarize advances in the physiological and neurological approaches to understanding, diagnosing, and treating ME. We identify key areas and approaches to elucidate the core and secondary symptom clusters in ME so as to provide some practical suggestions in evaluation of ME for clinicians and researchers. This review, therefore, represents a synthesis of key discussions in the literature, and has important implications for a better understanding of ME, its biological markers, and diagnostic criteria. There is a clear need for more longitudinal studies in this area with larger data sets, which correct for multiple testing.
Keywords: Biomarkers, case definitions, chronic fatigue syndrome, myalgic encephalomyelitis, neurocognitive, LORETA, post exertional malaise.
1. INTRODUCTION
Consensus-based case definitions, constructed by agreement among experts, are necessary when diagnostic tests for a disease have not been developed. However, consensus-based definitions may encounter problems with construct and external validity [1, 2]. To date, chronic fatigue syndrome (CFS), Myalgic Encephalomyelitis (ME), or a combination of both (ME/CFS) has largely been diagnosed using consensus-based case definitions. Even though the exact mechanisms which underlie ME have not been fully elucidated, we now have more empirical evidence, making it possible to begin to develop a more empirically based case definition. As such, there is a need to identify critical features of these illnesses [3] in order to reduce criterion variance [4], a major source of diagnostic unreliability. For example, we do know that in contrast to the Fukuda CFS criteria [5], both the Canadian ME/CFS criteria [6] and the ME-ICC criteria [7] identify a smaller subset of patients with more severe symptoms and greater physical functioning impairments [8] than Fukuda. However, these latter criteria require a larger set of symptoms for a diagnosis1, and as patients with higher numbers of somatic symptoms tend to have higher rates of psychiatric disorders [9], difficulties with differential diagnoses become more prominent. Along these lines, case definitions with more somatic symptoms might inadvertently increase rates of psychiatric co-morbidity [10].
Recently, the Institute of Medicine [11] issued a report that proposed a new name (Systemic Exertion Intolerance Disease, SEID) and case definition that included the following 4 symptoms: substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social or personal activities; post-exertional malaise, unrefreshing sleep; and at least one of the two following symptoms: cognitive impairment or orthostatic intolerance. Whereas the Fukuda criteria [5], the ME/CFS Canadian criteria [6] and the ME-ICC criteria [7] excluded other medical and psychiatric conditions that might have produced the fatigue, the new SEID criteria [11] had a different position regarding exclusionary conditions. More details about exclusions are provided within the IOM’s SEID Report Guide for Clinicians [11] (p. 4), where it states: “The presence of other illnesses should not preclude patients from receiving a diagnosis of ME/CFS (SEID) except in the unlikely event that all symptoms can be accounted for by these other illnesses.”
With the addition of SEID, there are now multiple case definitions [12, 13], and it is critical to determine whether these criteria identify patients with different characteristics. More importantly, to reduce criterion variance, in this article, we will try to identify defining features of ME2. We review the most recent literature to explore what might be essential for an empirical ME2case definition (Fig. 1).
Fig. (1).
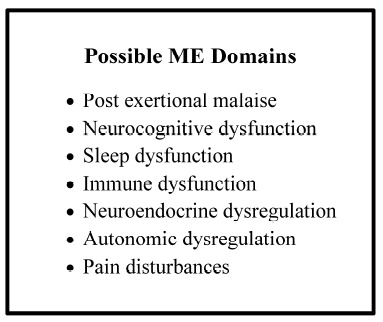
ME criteria to be evaluated.
The past 3 decades have seen a growth in research involving clinical aspects of ME [14, 15]. With this growing literature come new ideas for identifying core symptoms. Progress in this area has come from expert clinical observations and empirical findings, and has been presented within case definitions, review articles and research reports. One example, King and Jason [12], suggest that ME diagnosis could be improved by using pre-identified core symptoms, with severity ratings, alongside standardized measures to collect clinical information. These suggestions have now been incorporated in a number of studies, such as the work of Jason and colleagues [8], which found that three types of core symptoms, post-exertional malaise (PEM), neurocognitive dysfunction and unrefreshing sleep occur in nearly all patients with ME. In the same study, using data mining, the authors found that a few core symptom-clusters could correctly classify 95.3% of participants as ME or control. Furthermore, factor analytic studies have supported the identification of these critical primary domains of the illness [15].
In this article, we will argue that secondary symptoms of ME might include symptoms within immune [16-19], neuro-endocrine [20-22], autonomic [23-26], and pain domains [23, 24, 26, 27]. Despite the reported lower prevalence of these domains, these secondary symptoms are nonetheless found with enough frequency in the literature to utilize them for patient subtyping, such as, ME-immune, ME-autonomic, ME-neuroendocrine, ME-pain, or ME-combination. With this conceptual framework, we now review the biological evidence for ME biomarkers that could be used in a ME case definition.
Therefore, it is the purpose of the present article to build upon previous work to illustrate that the domains identified here are likely indicative of ME diagnosis. We recognize the variability inherent in each domain category (such as not all types of cognitive performance are impaired) and anticipate that the variances will be reduced by more focused research in the future. Furthermore, the features of ME do appear to be modulated by biological findings and will be diagnosable as symptoms of ME.
2. CORE SYMPTOM DOMAINS
2.1. Post-Exertional Malaise (PEM)
PEM is the extreme exhaustion, pain, cognitive deficits and other symptoms present after exertion in patients with ME, accompanied by an unusually slow return to baseline after exertion, not explained by deconditioning, sedentary lifestyle or malingering [28-30]. This return to baseline has been shown to last days, weeks or even months. One aspect of PEM is that the onset sometimes occurs about 24-hours post-exertion. This onset delay might help establish a differential diagnosis between ME and other diseases (e.g. Multiple Sclerosis, lupus, etc.), all of which have severe fatigue and malaise but no delay has been reported.
Every ME case definition, as well as factor analytic studies, concludes that PEM is an essential feature of this illness [31]. Exercise testing [28, 29] suggests that PEM can be prompted even by mild exercise with subjective patient reports of PEM generally describing a worsening of the entire ME symptom constellation as a result of the exercise [30]. In the laboratory, PEM has been characterized in a variety of ways such as increased symptoms of fatigue and pain [32-34], abnormal cardiopulmonary responses [35], increased oxidative stress [36], changes in cognitive function [32], and upregulation of several biological variables including complement C4a levels [28], cytokines [32] and various leukocyte markers [32-34]. Some of these studies [35, 37] await replication, though they provide evidence that a core feature of this illness is PEM.
Hypotheses about the nature of PEM include vascular dysfunction, peripheral nervous system deregulation, or spinal cord dysfunction [38-42]. PEM may be due to mitochondrial dysfunction [43, 44] secondary to mitochondrial damage and/or inhibition of the oxidative metabolism as a consequence of excessive and prolonged oxidative stress after exertion [36, 45]. Low oxygen uptake by muscle cells caused exercise intolerance in a majority, indicating insufficient metabolic adaptation to incremental exercise [46, 47].
Maes, Twisk, and Johnson [46] found that self-reported PEM was significantly related to inflammatory and cell-mediated immune biomarkers; patients with ME displayed more severe clinical symptoms and immune abnormalities compared to patients with CFS; whereas, both ME and CFS displayed more severe symptoms and immune disorders than patients with chronic fatigue. Biological measures and self-report items may therefore aid in discrimination between ME, CFS, and chronic fatigue.
2.1.1. Channelopathies
There is a small but compelling literature showing that PEM may involve channelopathies [3, 47-49]. Involving at least 29 ion channel genes, channelopathies are now known to underpin a variety of neurological diseases such as migraine (especially hemiplegic migraine), epilepsy, episodic ataxia, periodic paralysis or myotonia [50, 51], and congenital myasthenic syndrome [50, 52]. The central features of channelopathies in these diseases involve paroxysmal presentation, triggered by environmental events such as toxins, viruses or stressful life events [50]. Chaudhuri and colleagues [47, 48, 53-55] indicate that the mutations of ion channels [56] have only recently been implicated in ME [48]. Because stable ion-channel functioning is necessary for stable neural excitability, generation of action potentials and neurotransmitter release [57], it appears that PEM may be a channelopathy or related to one.
Regardless of source, the abnormal ion channel function in ME may be a result of a shift of membrane potential in voltage-gated potassium channels of the cell to a state of hyperpolarization and accompanying reduction of neuro-transmitter availability [47, 48]. For example, Snell, Vanness, Strayer, and Stevens [58] found disrupted immune status associated with exercise intolerance associated with oxidative stress and nitric oxide-related channelopathies. This converging evidence has therefore been used by some authors to argue for channelopathies in the etiology and maintenance of ME symptoms such as PEM [48, 59]. A summary of PEM studies are listed in Table 1.
Table 1.
Studies investigating Post exertional malaise in ME.1
| Author/Year | N | Case Def. | Investigation | Key Findings |
|---|---|---|---|---|
| LaManca et al. (1998) [32] | 19 patients 20 controls |
Dx done by others | Cognitive test battery, Stroop, Symbol Digit Modalities Test (processing speed), Trails, Serial 13’s, BDI, NAART, fatigue scale; treadmill test. | After demanding exercise (24 hours post), patients demonstrated significantly impaired cognitive processing when compared to controls. |
| VanNess, et al. (2003) [35] | 189 patients, no controls (repeated measures design) | Unknown | Treadmill test to subclassify patients. | Found three groups of patients and called for classifiers based on cardiopulmonary testing. |
| Siemionow et al. (2004) [78] | 8 patients 8 controls |
CDC Holmes criteria | Used 58-channel EEG data collection, performed handgrip tests. | Patients displayed significantly less motor strength, altered EEG theta findings. |
| Snell et al. (2005) [58] | 35 male patients 71 female patients |
Holmes and Fukuda | Exercise capacity as measured by graded exercise; peak VO2, peak HR, BMI, exertion, respiratory quotient. | ↓No gender effects but found immune effects consistent with mutated ion channels. |
| VanNess, et. al.(2007) [37] | 6 patients 6 controls |
Fukuda | Repeated measures design, with exercise as the repeated variable; VO2 peak, Peak HR, VO2 anaerobic | Differences not sig. at baseline but wide sig. differences at time 2 in peak oxygen consumption; HR not different. |
| Neary et al. (2008) [79] | 6 patients 8 controls |
Unknown | Incremental cycle test to exhaustion to look for prefrontal cortex hypoxia during exercise. | Cerebral oxygenation (HbO2), deoxy-hemoglobin, oxygen saturation and total blood volume found; reduced brain oxygenation and blood volume indicative of patients. |
| Nijs et al. (2008) [80] | 24 patients | Unknown | SF-36, symptom list, activities and participation questionnaire, all done 24 hours post exercise. |
↑after test, return to baseline 24 hours post ↑in pain overall. |
| Light et al. (2009) [33] | Unknown | Unknown | Post exercise, ME and ME-FMS patients show enhanced gene expression for receptors detecting muscle metabolites and for SNS and IS, which correlate with these symptoms. | Groups highly correlated with symptoms of physical fatigue, mental fatigue, and pain suggesting dysregulation of metabolite detecting receptors as well as SNS and IS in ME and ME-FMS. |
| Nijs et al. (2010) [28] | 22 patients 22 controls |
CDC criteria | Participants did submaximal exercise and a self-paced, physiologically limited exercise 8 days later. | Both resulted in PEM but IL-1B not altered. |
| VanNess et al. (2010) [30] | 25 patients 23 matched controls |
Fukuda | Maximal cardiopulmonary exercise test. | Within 24 hours posttest, 85% of controls fully recovered, 0% of patients fully recovered. Other 15% of controls recovered 48 hours post, only 1 patient recovered 48 hours post. |
| White et al. (2010) [81] | 19 patients 17 controls |
Not known | Looked at circulating cytokines post exercise | Used exercise protocol, cytokine analysis, found cytokines appear to vary with symptom flare (PEM). |
| Van Oosterwijck et al. (2010) [82] | 22 patients 22 controls |
CDC criteria | Cardiorespiratory tests, health status questionnaires. | ↑Pain post exercise patients, ↓pain post controls. |
| Maes et al. (2012) [46] | 144 patients | Fukuda and CF | Used PEM rating scale | Argues for stratification of patients. |
| Vermeulen et al. (2014) [83] | 3 Groups: 203 patients 223 chronic fatigue 18 controls |
Fukuda | Maximal exercise capacity measured. | ↓ max exercise capacity peak VO2 for the patient and CF groups, higher in controls. Low exercise capacity associated with metabolic problems. |
| Lengert et al. (2015) [84] | None | NA | This article presents a model to measure and demonstrate reduced mitochondrial capacity in ME exercise intolerance. | |
This list is not exhaustive.
2.1.2. Kindling
The kindling hypothesis has been proposed as an explanation for the etiology of many aspects of ME, as well as a mechanism to understand PEM [14, 60]. The electro-physiological kindling hypothesis posits that repeated intermittent exposure to excess neural activity, which is initially sub-threshold, can eventually cause that neural activity to exceed threshold limits, resulting in persistent hypersensitivity to that stimulus, and ultimately, spontaneous seizure-like activity [61-64]. According to the kindling model, using seizures as an example, repeated stimulation lowers the threshold for seizures to occur spontaneously after repetitive sub-threshold stimuli [65]. According to the CNS seizure kindling model, seizure activity can then spread to adjacent structures in the brain [63], which could, in part, explain the fluctuating nature of symptoms in patients with ME. Seizure activity is implicated in epilepsy and migraine. For infectious disease, chronically repeated, low-intensity stimulation due to an infectious illness may cause similar CNS kindling, which likewise involves neuronal cell populations that continue to fire after the initiating stimulation has ceased [66]. Available evidence suggests that kindling may play a part in the maintenance of PEM, possibly through both CNS and infectious diseases routes.
Exercise may also exacerbate kindling for individuals with underlying inflammatory states [67, 68], producing PEM. Arnett, Alleva, Korossy-Horwood, and Clark [69] hypothesize that exercise is pro-inflammatory for those with high circulating cytokine concentrations, whereas the same exercise may be anti-inflammatory for those with less severe persistent peripheral inflammation. These hypotheses suggest that non-pharmacologic interventions which attempt to increase exercise and activity may have negative effects for many patients with high circulating cytokine concentrations who are already exhausted due to limited energy levels and stamina.
In a clinical treatment trial, Jason, Benton, Torres-Harding, and Muldowney [70] found that patients who exerted more energy than they had available did not improve over time, whereas those patients who were able to stay within their energy boundaries made significant improvements over time. According to Energy Envelope Theory [71], when an individual with ME avoids overexertion and maintains an optimal level of activity over time, it may be associated with some improvements in physical functioning and fatigue, which might be due to reducing PEM. Alternatively, kindling may explain why going beyond energy reserves can elicit PEM (which results in a very slow return to baseline), and which can actually be an impediment to improving functionality and fatigue levels. The kindling hypothesis suggests that once this system is charged or elevated, either by high-intensity stimulation or by chronically repeated low-intensity stimulation, activities that involve going beyond energy reserves may enhance an already high level of arousal.
Autonomic nervous system findings from Light, White, Hughen, and Light [33] could also be used in support of a kindling model. Light et al. [33] found that exercise sends a continuous signal of muscle sensory fatigue to the sympathetic nervous system branch of the autonomic nervous system, causing dysregulation of sympathetic nervous system reflexes and ultimately producing the recognition of enhanced fatigue. Light’s group found that after exercise, patients with ME in comparison to controls demonstrated increases in mRNA in gene receptors that detect muscle-produced metabolites, genes that are essential for sympathetic nervous system processes, and immune function genes. The researchers concluded that patients may have an enhanced sensory signal for fatigue that is increased after exercise. Within this paradigm, kindling could cause excessive arousal that leads to an increase in excitatory postsynaptic receptors and a decrease in inhibitory presynaptic receptors. There are anecdotal reports of Light and his colleagues having some success using propranolol, a beta blocker that blocks activity of both epinephrine and norepinephrine and reduces excitation of the sympathetic nervous system. The researchers used low doses of propranolol (1/5 to 1/10 the dose prescribed for blood pressure control) to block the sensory receptors, thereby reducing sympathetic nervous system responsivity [72].
2.1.3. Measuring PEM
Standardized assessment of post-exertional malaise is necessary due to the variability in assessment strategies across studies. For example, Jason, King, Richman, Taylor, and Torres [73] found that PEM for individuals with ME ranged from 41-94% depending on how the self-report question was worded, calling attention to the need to develop standardized assessment tools. Biological assessments of PEM include the work of Light et al. [33], documenting increases in the expression for sensory, adrenergic, and immune genes following moderate exercise. The types of challenges reviewed above document impairments in sensory, adrenergic, and immune systems. Other efforts to document PEM might include pain threshold before and after exercise [55, 74], neuropsychological and cognitive tests before and after a treadmill test [32] and repeated exercise tests [30]. Neu, Mairesse, Verbanck, and Linkowski [75] had patients with ME and controls use an electronic handgrip dynamometer to measure muscular hand grip strength. While sitting and using the dominant hand, in the “tonic” condition, participants gripped the handle as strongly as possible and maintained the grip as long as possible. This condition was performed four times, and the measured variable was the time elapsed before grip force decreased by 50%. In the “phasic” condition, participants gripped the handle as strongly as possible and relaxed immediately during ten successive trials. Cytokine levels were increased for IL-1b, IL-8, IL-10 and TNF-α and fatigue intensity was correlated to grip strength and IL-8. The gap between the controls over the people with ME increased with almost every trial, suggesting this might be a useful test to measure or test for fatigability in ME.
Another important issue in PEM measurement is the timing of the testing. The significance of second-day testing in exercise challenges was evident in VanNess, et al. [35], who recruited 6 female patients and 6 sedentary matched control subjects and all achieved maximal exertion. During day 1 of exercise test, patients with ME had a slightly lower V02 max (maximum capacity of an individual's body to transport and use oxygen) than controls (26.2 ml/kg/min vs. 28.4 ml/kg/min) and lower oxygen utilization at anaerobic threshold (15.0 ml/kg/min vs. 17.6 mg/kg/min). However, these values for patients versus controls at day 1 were not significantly different, but on day 2, prominent effects of exercise emerged. On day 2 of the exercise test, sedentary controls improved in VO2 max (28.4 to 28.9 ml/kg/min) and oxygen utilization at anaerobic threshold (17.6 to 18.0 ml/kg/min) whereas patients worsened in VO2 max (26.2 to 20.5 ml/kg/min) and in oxygen utilization at anaerobic threshold (15.0 to 11.0 ml/kg/min). ME values were in the severe disability range [76], and the decline in function from day 1 to day 2 could not be explained by inactivity. The fall in oxygen consumption on day 2 of the exercise test among patients compared to controls suggests metabolic dysfunction [77]. Therefore, it is critical to assess PEM with a challenge over a two day period of time.
3. Neurocognitive Domain
Neurocognitive impairment is frequently reported in ME both through self-reported by 85% of patients [85] and over 90% in clinical and anecdotal reports [86] with a number of studies using objective testing [31, 87]. Studies of neurocognitive impairment typically use neuropsychological assessment, surveys, paper-and-pencil tests, and others using some of these assessments combined with neuroimaging. With these modalities, earlier studies (prior to 2001) primarily found impairments in information processing speed, working memory and incidental learning [88]. More recently, these results have been replicated and extended, indicating a variety of neurocognitive impairments in ME such as sustained and divided attention, concentration, memory and metamemory, working memory, slowed information processing speed, slowed verbal fluency including word-finding problems, learning complex information, cognitive slowing, impaired concentration problems, fine motor speed, reaction time and abstract thinking [89-95]. Neurocognitive studies in ME are also notable for the wide range of findings between studies but overall, demonstrate the neurocognitive impairment in ME. The limitations appear to be primarily in variations of study design, as well as which actual assessments are used. For example, one study, to address some limitations for genetic and environmental influences, used twins reared together for matching (a powerful study design). In that study, Claypoole, Noonan, Mahurin, Goldberg, Erickson, and Buchwald [96] found decreases in overall executive functioning in ME. Another commonly cited ME research problem is issues in diagnosis as well as exclusion criteria for the study, which can lead to contamination. Currently, disparate findings can be explained by the variety of designs and design issues (such as small sample size), and/or to the differences between the tests themselves.
It should be noted that several studies have found the neurocognitive deficits to be independent of psychopathology [97, 98] and medication effects [94, 95, 99]. For children with ME, neurocognitive impairment is the single most problematic symptom resulting in long term school absence and inability to complete school work, which has been shown to be independent of depression and anxiety [100-102].
There are many theories proposed about the cause of the neurocognitive abnormalities in ME. The following points capture some of the theories surrounding the abnormalities:
Nieoullon [103] postulated that disruption in dopamine function might lead to some of the cognitive dysfunction experienced by many patients with ME.
Arnett and colleagues [69] proposed that ME is the result of a long-term inflammatory process within the brain, which could impact cognitive functioning. These long term processes are very similar to that of critical care patients, since both ME and critical/non-critical illnesses are associated with steeper declines in cognition as a function of more infections and inflammation [69, 104-109].
Widespread neuroinflammation has been found in the brain of patients with ME, which has been associated with the severity of neuropsychological symptoms [24]. More specifically, activation of microglia or astrocytes was found through [11C-ide] (11C-(R)-PK11195) a ligand of PET for a translocator protein that is related to neuroinflammation. Binding potential, a measure of the density of the receptors for the translocator protein, was higher in patients with ME than controls. The binding potential in the amygdala, thalamus and midbrain was significantly and positively correlated with cognitive impairment. Pain scores were positively correlated with binding potential in the cingulate cortex and thalamus, and depression scores were likewise positively correlated with binding potential in the hippocampus.
In a recent microglia study, Fuku, Hossain, Noda, and Katafuchi [110] found 5-HTT astrocyte expression resulted in immunologically induced fatigue in rats. These studies are important as they are addressing the core issues of ME symptomology at the gene level, creating a better understanding of the array of symptoms in this illness.
Overall, neuroinflammation is present in the CNS in all neurological diseases, CNS injury or infection, peripheral infection and stress, and most often the inflammation presents as one or more types of neurocognitive impairment [105]. Since neurocognitive impairment without dementia due to chronic medical conditions overall accounts for about 25% of all neurocognitive impairment [111, 112], it may be that the course of neurocognitive impairment in ME could parallel that of other types of neurocognitive disorders and have similar etiologies, informing clinicians and researchers alike about etiology and prognosis.
3.1. The Immune Activation Hypothesis
Kuratsune and Watanabe [109, 113] demonstrated that brain dysfunction among patients with ME is caused by reactivation of various herpes viral infections and/or chronic mycoplasma that may cause infection and abnormal production of cytokines. In support of immune activation, Natelson, Weaver, Tseng, and Ottenweller [114] indicated that IL-8 and IL-10 have been found to be significantly elevated in the cerebrospinal fluid of patients with ME (both of the cytokines are elevated after an acute inflammatory event). Sorenson and colleagues [115] also found increased expression of pro-inflammatory cytokine IL-8 in patients. Still another indicator of chronic immune activation is the up-regulated amyloid beta precursor protein (APP) in the cerebrospinal fluid of patients with ME [116], and APP-1 expression is driven by tumor necrosis factor.
Free radicals in moderate amounts are normal in that they play a key role in metabolism and immunity. However, significantly large amounts of free radicals have been implicated in ME [117]. Baraniuk and colleagues [116] found that patients with ME have a longer rather than shorter version of the gene CNDP1 (carnosine dipeptidase) and the longer version of this gene impairs the ability of the brain to protect itself from free radicals. CNDP1 degrades carnosine, which is a free radical scavenger and increases corticosterone levels. In this manner, low carnosine levels may contribute to increased oxidative stress.
Oxidative stress has also been shown to be associated with neuroinflammation [118]. de Lange and colleagues [119] observed significant reductions in grey matter volume in patients with ME, which appeared to be due to neuro-inflammation. This finding appears to be similar to the grey matter loss in Alzheimer’s Disease which is, in turn, hypothesized to be related to chronic inflammatory cytokine production in the brain [120]. Kindling may also be what is responsible for the high levels of oxidative stress in patients with ME due to the dysfunction of ion channels in conjunction with ion transport [120-122]. Nitric Oxide, a free radical and an important biological regulator that plays a key hypothesis in the pathogenesis of ME [18, 19], is another source of oxidative stress in this disease [123].
Martin Pall’s [124] Nitric Oxide hypothesis states that when a virus, bacteria, mold, toxin, microbe or allergy activates the immune system--and this can occur with patients with ME who are fighting these viruses and bacterial infections--the immune system reacts by producing excessive amounts of nitric oxide. Furthermore, Paul Cheney [125] states when NMDA (N-methyl-D-aspartate) receptors on neurons are activated, they likewise trigger nitric oxide production, introducing more free radicals into the ME patient. Superoxide, another free radical, is produced in the mitochondria of the cell and is produced during energy production; that is, for every molecule of ATP (energy) generated, one molecule of superoxide is generated. Enzymes embedded in the mitochondria can break superoxide down to hydrogen peroxide and then to water. This enzyme cannot do its job without proper amounts of selenium and glutathione. If superoxide leaks out of the mitochondria, it combines with nitric oxide (found outside the mitochondria), nitric oxide then combines with superoxide in a 1:1 relationship to produce one molecule of peroxynitrite. Peroxynitrite is an oxidant which, like nitric oxide and superoxide, also creates free radicals, causing oxidative damage. In addition, peroxynitrite increases the levels of both nitric oxide and superoxide which then react to produce more peroxynitrite. Once peroxynitrite levels are elevated, they continue the elevation, thus producing a self-sustaining cycle. These pathways lead to high amounts of free radicals in patients with ME, and when taken together with the events described above, all contribute to oxidative stress damage seen in the CNS of these patients. To ameliorate these effects, coenzyme Q10, which some patients have found to be helpful in dealing with ME symptoms [126], binds to excess superoxide so that it cannot couple with nitric oxide to produce peroxynitrite.
3.2. Neuroimaging in ME
3.2.1. Structural Neuroimaging
Preliminary studies relying on visual inspection methods for investigating abnormalities on MRI scans revealed small, punctate white matter hyperintensities [131, 134] in patients with ME. An early MRI study involving 144 patients from the Incline Village Nevada outbreak reported 78% of those patients showed white matter hyperintensities predominantly in subcortical regions [125]. Greco and colleagues [138] observed white matter abnormalities were greater in patients with ME without co-morbid depression or psychiatric disorders. However, two other studies [119, 147] using voxel-based morphometry and found no differences in white matter volume, but instead both studies found markedly reduced grey matter volume in patients with ME. Okada et al. [147] reported the prefrontal cortex in patients had 16.9% less grey matter volume, while de Lange et al. [119] reported that patients had an overall reduction (8%) of global gray matter volume. In another voxel-based morphometry study involving 25 patients with ME and 25 age/gender-matched controls, Barnden et al. [162] found that white matter volume decreases in the midbrain were associated with increasing fatigue duration and grey matter atrophy in the brainstem was positively associated with seated pulse pressure measures. Barnden speculated that astrocyte dysfunction could account from some of the observed changes. Additionally, among 26 patients with ME and 26 age/gender-matched controls, Puri et al. [130] found patients with ME had reduced grey matter volume in the occipital lobes, the right angular gyrus and the posterior division of the left parahippocampal gyrus, and reduced white matter volume in the left occipital lobe. Finally, in a recent study using MRI and diffusion tract imaging, Zeineh et al. (2015) found decreased global white matter in patients as well as higher fractional anisotropy values in the right posterior arcuate fasciculus, a white fiber tract connecting brain areas primarily involved in language and speech production. Taken together, these studies indicate structural changes may be occurring in patients and those changes might be causing alterations in functional connectivity and contributing to fatigue. While further replication is needed, these findings are promising in establishing the basis of impaired cognitive function in patients.
3.2.2. Functional Neuroimaging
Use of functional magnetic resonance imaging, single-proton magnetic resonance spectroscopy (SPECT) and positron emission tomography (PET) have also been used to study cognitive dysfunction in ME (see Table 2). In addition to the white and grey matter abnormalities mentioned earlier, reduced cerebral blood flow has been reported globally as well as in the frontal and occipital lobes of ME patients. Neary and colleagues [79] found that, in addition to significant exercise intolerance, patients had reduced prefrontal oxygenation in comparison to controls, suggesting altered cerebral oxygenation (hypoxia) and blood volume in the brain. Early SPECT found hypoperfusion in varying regions of the cerebral hemispheres and brainstems of patients with ME [135, 137]. Deficits in ME cerebral flow and perfusion have also been found using near-infrared spectroscopy [167], Xenon gas diffusion computerized tomography [154], and magnetic resonance arterial spin labeling [163]. Shungu and colleagues [164] found increased ventricular lactate and decreased cortical glutathione, as well as lower regional cerebral blood flow in the left anterior cingulate cortex and the right lingual gyrus in patients with ME. However, work by Fischler et al. [168] and MacHale et al. [169] could not confirm any deficits in ME cerebral perfusion. SPECT, CT, and MRI-based methods are limited as they cannot be used during tilt table tests.
Table 2.
Observational case-control studies using neuroimaging methods to investigate ME.*
| Author/Year | N | Imaging Method | Investigation | Key Findings |
|---|---|---|---|---|
| Ichise et al. (1992) [133] | 60 patients 14 controls |
SPECT | Regional cerebral perfusion | ↓ rCBF ratios in frontal, temporal, parietal, occipital lobes, and basal ganglia. |
| Natelson et al. (1993) [134] | 52 patients 52 controls |
MRI | White matter hyperintensities in patients screened for depression with BDI. | Majority of white matter lesions found were located in subcortical regions. |
| Schwartz et al. (1994) [135] | 16 patients 15 controls |
MRI SPECT |
Intracranial functional and structural abnormalities | Abnormalities on SPECT scans in patients > controls. Patient abnormalities in SPECT scans > MRI scans. |
| Cope et al. (1995) [136] | 11 patients + MDD 15 patients 18 controls 13 MDD |
MRI | Neuropsychological test battery Psychiatric assessments White matter abnormalities |
No significant differences in test performance were found between sample groups. Psychiatric assessment scores correlated with subjective measures of cognitive dysfunction. White matter lesions found in all 3 groups. |
| Costa et al. (1995) [137] | 40 patients 13 patients + MDD 14 patients + Psych 60 controls |
SPECT | Brain perfusion | Generalized brain hypoperfusion, particularly in brainstem and bi-lateral frontal cortex. Brainstem hypoperfusion differentiated patients with ME from depressed patients. |
| Greco et al. (1997) [138] | 15 patients 14 patients + MDD 14 patients + Psych |
MRI | White matter | Statistical trend of greater white matter abnormalities in the ME subgroup without depression or psychiatric disorder. |
| Tirelli et al. (1998) [139] | 18 patients 6 MDD 6 controls |
FDG-PET | Brain metabolism | Hypometabolism in brain stem differentiated patients from those with depression. |
| Lange et al (1999) [131] | 21 patients 18 patients + Psych 18 controls |
MRI | White matter | ↑ small, punctuate, subcortical white matter hyperintensities in frontal lobes. |
| Brooks et al. (2000) [140] | 7 patients 10 controls |
1H MRSI | Hippocampal volume and cerebral metabolites including markers of neuronal density (NAA), cellular bioenergetics, cell membranes and glial cells | No significant difference in hippocampal volume was found. ↓ amounts of N-acetylasparate (NAA) concentrations in patients indicating neuronal damage in right hippocampus. |
| Lange et al. (2001) [141] | 28 patients 15 controls |
MRI | Lateral ventricular volumes; Left-right hemisphere subcomponents | Larger ventricular volumes in patients at near significance level. |
| Lewis et al. (2001) [142] | 22 monozygotic twins discordant for patients | SPECT | Regional cerebral blood flow | No significant differences in regional cerebral blood flow were found. |
| Kuratsune et al. (2002) [143] | 8 patients 8 controls |
PET | Cerebral uptake of acetylcarnitine | ↓ acetylcarnitine in prefrontal cortex (BAs 9, 46), temporal lobe (BAs 21, 41), anterior cingulate (BAs 24, 32), and cerebellum. |
| Chadhuri et al. (2003) [54] | 8 patients 8 controls |
1H MRSI | Metabolic functioning of left basal ganglia in patients |
↑ choline containing compounds in patients suggesting functional changes occurring in the neuron membrane of the basal ganglia. |
| Schmaling et al. (2003) [144] | 15 patients 15 controls |
SPECT | Differences in CBF during rest and during the PASAT cognitive task of auditory working memory. | Perfusion incontrols > patients in the anterior cingulate during baseline and experimental conditions. Patients’ anterior cingulate perfusion approached control group levels during cognitive task, on the contralateral side. |
| Siessmeier et al. (2003) [145] | 26 patients 18 controls |
FDG-PET | Cerebral glucose metabolism | Metabolic abnormalities detected in half of patients, mainly in the orbital frontal lobe. No relationship found between fatigue and glucose metabolism. |
| de Lange et al. (2004) [146] | 16 patients 16 controls |
fMRI | Anterior cingulate, visual regions | Increased activation in visual areas in response to motor imagery task. Ventral anterior cingulate inactive in patients during error trials. |
| Okada et al. (2004) [147] | 16 patients 49 controls |
MRI | Grey & white matter VBM and association with fatigue severity scores. | ↓ grey-matter volume in bilateral prefrontal cortex. Fatigue severity associated atrophy in the right dorsolateral prefrontal cortex. No differences in white matter volume. |
| Yamamoto et al. (2004) [148] | 10 patients 10 controls |
PET | Density of serotonin transporters (5-HTTs) | ↓ 5-HTTs found in rostral anterior cingulate in patients. 5-HTT alterations associated with increased pain ratings. |
| Cleare et al. (2005) [149] | 10 patients 10 controls |
PET | 5-HT1A Receptor Binding in patients | ↓ 5-HT1A binding potential in patients is widespread and particularlyfound in the hippocampus. |
| de Lange et al. (2005) [150] | 28 patients 28 controls |
MRI | Grey matter, white matter using voxel-based morphometry | ↓ global grey matter volume in patients. |
| Lange et al. (2005) [151] | 25 patients 22 controls |
fMRI | Verbal working memory during a complex auditory processing task | ↑ effort expenditure in patients associated with activation in more extensive regions of the working memory system. |
| Caseras et al. (2006) [152] | 17 patients 12 controls |
bold fMRI | Verbal working memory using n-back task to measure task load effects. | ↑ activity during low task load in bilateral medial prefrontal regions, rostral anterior cingulate. When task load increased, major nodes of WM system (dorsolateral prefrontal, parietal) became less active while inferior temporal gyrus were more active. |
| Tanaka et al. (2006) [153] | 6 patients 7 controls |
fMRI | Auditory responsiveness while performing a fatiguing visual search task. | ↓ responsiveness in patients with fatigue-inducing task. Rate of task responsiveness associated with subjective fatigue sensation. |
| Yoshiuchi et al. (2006) [154] | 16 patients 9 patients + Psych 7 controls |
Xenon-CT | Absolute cerebral blood flow | ↓ absolute CBF in left and right middle cerebral artery areas in the entire patient sample. Patients-No Psych group had more regions of reduced cerebral blood flow than patients-Psych group. |
| Cook et al. (2007) [155] | 9 patients 11 controls |
bold fMRI | Mental fatigue using auditory fatigue inducing tasks | ↑ reaction times and errors in patient associated with increasing mental fatigue. ↑ activation in frontal, temporal, cingulate and cerebellar regions associated with mental fatigue. ↓ activation in the left posterior parietal cortex in response to mental fatigue. |
| Sherlin et al. (2007) [156] | 17 twin pairs discordant. | LORETA | Spatial locations in the brain associated with patient twins. | ↑ current source density for delta band in left uncus and parahippocampal gyrus found in patient co-twins. ↑ current source density for theta band in cingulate gyrus and right precentral gyrus found in patient co-twins. |
| Caseras et al. (2008) [157] | 12 patients 11 controls |
bold fMRI | Imaginal experience of fatigue using a fatigue provocation task | Patient ratings to fatiguing video clips were higher than controls. ↑ activity in medial parietal cortex and precuneus, posterior cingulate gyrus, and parahippocampal gyrus. ↓ activity in prefrontal cortex. Fatigue was predicted by increased activity in the caudate nucleus for both groups. |
| de Lange et al. (2008) [158] | 22 patients 22 controls |
MRI | Gray matter volume using voxel-based morphometry | ↓ grey matter in patients at baseline and follow-up. Grey matter volume was modestly reversed by graded exercise therapy intervention in some but not all patients. |
| Mathew et al. (2009) [159] | 16 patients 14 GAD 15 controls |
1H MRSI | Lactate concentrations in lateral ventricular cerebrospinal fluid | ↑ mean lateral ventricular lactate concentrations in patients differentiated from GAD and control groups. Patients’diagnoses accounted for 43% of the variance. |
| Flor-Henry et al. (2010) [160] |
61 patients 80 controls |
BK-Beamformer EEG Source Analysis | Spatial patterns of EEG and their associated source cortical distributions in alpha and beta. | Significant differences in spatial patterns and source distributions between groups in alpha and beta bands across all conditions and resulting high classification rates separating both groups. |
| Murrough et al. (2010) [161] | 17 patients 21 MDD 19 controls |
1H MRSI | Ventricular cerebrospinal fluid lactate levels | ↑ cerebrospinal fluid lactate levels in 13 patients compared to controls and were related to severity of mental fatigue. |
| Barnden et al. (2011) [162] | 25 patients 25 controls |
MRI, fMRI | Grey/white matter VBM regressed against clinical scores | ↓ white matter in the midbrain associated with increasing years in fatigue duration. ↓ grey matter in brainstem predicted by seated pulse pressure measures. |
| Biswal et al. (2011) [163] | 11 patients 10 controls |
ASL | Absolute cerebral blood flow. | ↓ absolute global CBF in 9 patients while 2 patients demonstrated the opposite result. |
| Puri et al. (2012) [130] | 26 patients 26 controls |
MRI | Grey/white matter VBM | ↓ grey matter volume in patients found in bi-lateral occipital region, left parahippocampal gyrus, and right angular gyrus. |
| Shungu et al. (2012) [164] | 15 patients 15 MDD 15 controls |
1H MRSI ASL MRI P MRSI |
Oxidative stress, cerebral hypoperfusion, mitochondrial dysfunction: - Ventricular cerebrospinal fluid (CSF) lactate - Cortical glutathione (GSH) to measure antioxidant capacity - Regional cerebral blood flow, high-energy phosphate assessment of mitochondrial dysfunction |
↑ ventricular CSF lactate and ↓ GSH in ME, MDD groups compared to controls. ↓ regional cerebral blood flow in left anterior cingulate and right lingual gyrus compared to controls, but no statistical differences between ME and MDD were found. No differences in high-energy phosphate metabolites. |
| Yamamoto et al. (2012) [165] | 11 patients 11 controls |
PET | Neurotransmitter receptor binding potential and associated serum autoantibody levels | ↑ serum antibodies and ↓ neurotransmitter receptor binding levels in a subset of patient sample suggesting penetration into the brain following BBB impairment in those patients. |
| Zinn et al. (2014) [94] | 50 patients 50 controls |
eLORETA | Spatial locations and temporal patterns of current source densities within the neocortex and their association with scores on two subjective fatigue measurements | ↑ current source density in delta band predominately in bi-lateral frontal/limbic areas. ↑ current source density in beta band bi-laterally, in superior parietal and sensorimotor areas. Maximal current source densities for delta band in left Broca’s area predicted by higher scores on the Multidimensional Fatigue Inventory (MFI-20), reduced motivation subscale. |
| Zeineh et al. (2015) [132] | 15 patients 14 controls |
DTI, ASL | Fractional anisotropy in white fiber tracks Cerebral blood flow |
↑ fractional anisotropy in the right posterior arcuate fasciculus and right inferior longitudinal fasciculus in right handed patients. ↓ bi-lateral white matter present in patients. No differences were found in cerebral blood flow. |
| Barnden et al. (2015) [166] | 25 patients 25 controls |
MRI, fMRI | Voxel-based quantitative analysis of T1w and T2w MRI signal level. Behavioral measures of anxiety and depression. |
↑ myelination in prefrontal cortex, related to disease severity. ↓ white matter volume found in the midbrain in patients. Severity effects were independent of anxiety and depression. |
ASL = arterial spin labeling; CT = computerized tomography; bold fMRI = blood oxygen dependent functional magnetic resonance imaging; MRI = magnetic resonance imaging; 1H MRSI = proton magnetic resonance spectroscopy imaging; PET = positron emission tomography; FDG-PET = 18-flourodeoxyglucose positron emission tomography; SPECT = single-photon emission computerized tomography; XeCT = xenon enhanced computed tomography; LORETA = low resolution electromagnetic tomography; eLORETA = exact low resolution electromagnetic tomography, DTI = diffusion tensor imaging. *Studies without a control group were omitted.
While examining autonomic dysregulation, cerebral impairments have been found during orthostatic challenges. For example, Ocon, Medow, Taneja, Clarke, and Stewart [170] studied a subset of subjects with Postural Orthostatic Tachycardia Syndrome (POTS) who, after being placed upright during tilt-table testing, had decreased cerebral blood flow. Additionally, there are discrepant findings regarding cerebral blood flow may be due to the differing ways of measuring the response of cerebral blood flow velocity to arterial pressure or due to the fact that these symptoms occur with less frequency among patients with ME.
Contrary to the aforementioned functional imaging evidence showing CNS hypofunction, Wyller, Eriksen, and Malterud [171] hypothesize that sustained arousal is the primary mechanism of ME. Wyller et al. suggest clonidine may effectively reduce this arousal. Morriss, Robson, and Deakin [172] have found that low doses of clonidine act pre-synaptically at alpha-2 adrenoceptors to inhibit noradrenaline function, and using this drug with patients with ME enhances growth hormone and cortisol release, and increases speed in the initial stage of a planning task. Accordingly, Nijs and colleagues [173] suggest that acetaminophen, serotonin-reuptake inhibitor drugs, selective and balanced serotonin and norepinephrine-reuptake inhibitor drugs, the serotonin precursor tryptophan, opioids, NMDA-receptor antagonists, calcium-channel alpha(2)delta (a2δ) ligands, transcranial magnetic stimulation, transcutaneous electric nerve stimulation (TENS), manual therapy and stress management could theoretically be used to desensitize the central nervous system in patients.
Finally, an intriguing set of experiments by Hilty and colleagues [174-176] found that nerve impulses from the muscle inhibit the primary motoric area (M1) during an energy-demanding exercise; but after narcotization of the spinal cord, the corresponding fatigue-related inhibition processes become significantly weaker. The thalamus and the insular cortex exhibited an increase in activity shortly before the interruption of a tiring, energy-demanding activity, while the inhibitory influences on motoric activity were actually mediated via the insular cortex. As the fatigued progressed, communication between the insular cortex and the primary motor area became more intensive. These findings further indicate that the brain plays a major role in muscle fatigue.
Linking brain abnormalities with cognitive function, studies of brain rhythms have consistently demonstrated the relationship between quantitative electroencephalography (qEEG) and ME. Oscillatory patterns, which reflect underlying differences in the speed and timing of neuronal communication within local and long distance networks [57], appear to be deregulated primarily in the lower frequencies in ME.
It appears that brain rhythm studies [78, 95, 177, 178] likewise demonstrate a connection between cortical dysfunction and cognitive impairment in ME. qEEG abnormalities include spike and sharp waves, which have been associated with seizure activity in the cortex [179, 180]. In Donati and colleagues [179] spikes were found to be most common in the temporal region, which contains the hippocampus, thus implicating memory disturbance. It is known that the temporal lobes have a predilection for infection by the herpes virus in acute herpes encephalopathy and encephalitis [181]; therefore, the findings may be related to post-viral mild encephalopathy which could cause the self-reported memory and attention problems. Another use of qEEG is connectivity analysis; Duffy, McAnulty, McCreary, Cuchural, and Komaroff [182] found that qEEG connectivity measures were able to discriminate patients with ME from healthy controls and from those with major depression with nearly 90% accuracy.
Another measure of cerebral activity, based on qEEG data, is source analysis [183-188]. Three studies using qEEG source analysis [94, 156, 160] found evidence of brain dysregulation which indicates reduced efficiency of information processing in patients with ME. This type of analysis allows measurement of the limbic system as well as the cortex, and the finding by Sherlin [156] of increased delta sources in the left uncus and parahippocampal gyrus of affected twins with ME is associated with blunted affect, apathy, and reduced motivation. Sherlin’s findings were similar to Nickl-Jockschat et al. [189] who conducted a meta-analysis of MRI studies involving 917 patients with mild cognitive impairment which showed that cognitive decline was associated with a pattern of grey matter atrophy in deeper limbic structures including the parahippocampal gyrus. Interestingly, two recent sleep studies found lower delta in subjects with ME; Le Bon and colleagues [190] found that ME was associated with lower ultra-slow (0.5-0.8Hz) delta power and Decker et al. (2009) also observed varying delta abnormalities in patients. Taken together, these studies suggest that delta slow-wave activity could be a key factor in differentiating between patients with ME and controls.
In a different method of source analysis, Flor-Henry, Lind, and Koles [160, 191] found significantly greater current source density in the left frontal-temporal-parietal regions of the cortex among the patients with ME, which would account for executive functioning deficits as well as perceptual reasoning problems.
M. A. Zinn et al. [94] performed a source analysis using exact low-resolution electromagnetic tomography (eLORETA) and found widespread cortical hypoactivation among patients with ME, with elevated delta sources in 50% of the frontal lobe and 19% of limbic lobe regions of interest including the anterior cingulate and orbital frontal gyrus. A co-occurrence of beta-2 sources was also found bilaterally in 18% of the parietal lobe regions of interest including the paracentral lobule (sensorimotor cortex), posterior cingulate, and precuneus, indicating compensatory activation. Furthermore, portions of the left frontal lobe and left limbic lobe were positively associated with scores on a fatigue measure (MFI-20) with reduced motivation as the only predictive factor. This study found objective quantification of central nervous system dysregulation providing evidence of specific nodes within brain networks that might be involved in producing ME symptoms of cognitive impairment or “brain fog”.
3.3. Measuring Neurocognitive Dysfunction
Central nervous system dysfunction can be measured in vivo and functional imaging data, as indicated by the array of biological measures above. Objective testing can also occur using the neuropsychological and cognitive tests such as the Cambridge Neuropsychological Test Automated Battery (CANTAB) [192]. Alternatively, Gudrun Lange (personal communication, 2/29/2012) suggests that a staged approach for cognitive assessment can last from 1.5–2 hours, and would include a WAIS IV abbreviated version, Repeatable Battery for the Assessment of Neuropsychological Status (RBANS™) Form A or B (working memory supplement), Digit Span forward and backward, Computerized Continuous Performance Test [Processing speed, Simple reaction time and Vigilance, and Executive Function], Computerized Category Test, and effort measures can be derived from Digit Span and RBANS™.
4. Sleep Dysfunction Domain
Unrefreshing sleep, or reduced sleep efficiency, is one of the most commonly-reported symptoms of ME [193]. Landis [194] hypothesizes that sleep dysfunction may be a consequence of the neurological dysfunction of ME. The Carruthers ME-ICC diagnostic criteria [7] places sleep disturbance within the neurological impairments domain and several studies hypothesize that sleep disturbance may reflect the neurological dysfunction of ME. The particular disturbances reported are difficulty falling asleep, staying asleep and early morning awakening [194] as well as non-restorative sleep which can be seen in the deregulated brain rhythms overall including an increase in slow waves and a shift in alpha rhythms [195].
Some investigations (see Table 3) report problems with delta slow-wave sleep and others with alpha intrusion into deep sleep [196]. Kishi et al. [197] found that after exercise, those with ME were significantly more likely to wake than controls, and had a disrupted rate of transition from REM to wakefulness than controls. Because the probability of transition from REM to wake correlated significantly with increases in subjective fatigue, pain, and sleepiness overnight in ME, it is possible that these transitions may relate to patient complaints of unrefreshing sleep. Decker, Tabassum, Lin, and Reeves [198] found that the homeostatic function of sleep is disrupted in patients with ME, which could be one causal factor for the failure of sleep to resolve fatigue. Decker investigated delta (slow wave) power and found impaired sleep homeostasis. Delta waves have been associated with prolonged hypopolarization in the thalamo-cortical circuit and inhibit cortical neurons, “turning off the neurons,” disconnecting the cortex from the lower brain centers and causing the person to fall asleep [180, 199, 200]. Using polysomnography and psychometric assessment, Neu, Mairesse, Verbanck, Linkowski, and Le Bon [75] found that patients with ME presented with highest fatigue and those with sleep apnea-hypopnea syndrome with highest sleepiness levels. During non-REM sleep, there is a pattern of power exchange in higher frequency bands at the expense of central ultra-slow (delta) power.
Table 3.
EEG polysomnography observational case-control studies investigating sleep abnormalities in ME.1
| Author/Year of Study | N | Investigation | Key Findings |
|---|---|---|---|
| Whelton et al. (1992) [206] | 14 patients 12 controls |
Sleep physiology, viral serology, linkage to patient symptoms | ↑ Alpha in patients during non-REM sleep related to unrefreshing sleep symptom. |
| Morriss et al. (1993) [207] | 12 patients 12 controls |
nighttime sleep disturbance with relationship to daytime fatigue. |
Did not find significant alpha/delta sleep differences. 7 patients met criteria for a sleep disorder (initiation & maintenance). |
| Krupp et al. (1993) [208] | 72 patients 57 multiple sclerosis 40 controls |
Sleep assessment, relationship between sleep, fatigue, and depressive symptoms. Polysomnography in a subgroup of 16 patients with ME. |
↑ sleep disturbances reported by patients with ME compared to MS and controls. 2 of 16 patients in ME subgroup had alpha intrusions during delta sleep stages. 10 of 16 patients in ME subgroup had sleep abnormalities. |
| Fischler et al. (1997) [209] | 49 patients 20 controls |
Compare polysomnographic variables between groups for possible sleep disturbances. | ↓ percentage of stage 4 sleep in ME. ↑ problems with sleep initiation and maintenance in ME. |
| Neu et al. (2007) [210] | 28 patients (female) 12 controls (female) |
Examine relationships in sleep efficiency parameters and subjective measures of sleep quality. | Poor subjective sleep quality in ME. No differences found in sleep efficiency index or slow wave sleep patterns. |
| Armitage et al. (2007) [211] | 13 pairs of monozygotic twins discordant for ME | Power spectral analysis of response to sleep regulatory challenge. | Patient co-twins had a blunted slow wave activity response to sleep challenge. |
| Kishi et al. (2008) [212] | 22 patients (female) 22 controls (female) |
Dynamic transition analysis of sleep stage patterns. | ↑ time in non-REM & stage 1, much less time in stages 2, 3 and 4. |
| Togo et al (2008) [213] | 12 patients 12 patients + fibromyalgia 26 controls |
Polysomnographic relationships in sleep-disrupted breathing or periodic leg movement disorder. | ↓ Total sleep time, sleep efficiency, and REM sleep in ME. ↓ Length of uninterrupted sleep time in patients with sustained levels of pain and fatigue after sleep. |
| Decker et al. (2009) [198] | 35 patients 40 controls |
Sleep homeostasis in patients using EEG power spectral analysis. | ↓ delta power in patients during slow wave stages ↑ delta during stage 1 and REM. ↓ alpha power in patients in stage 2, slow wave sleep and REM. ↓ lower theta, sigma (12-14), beta in patients during stage 2, slow wave sleep and REM. |
| Armitage et al. (2009) [214] | 13 pairs of monozygotic twins discordant for ME | Polysomnography analysis, EEG power spectral analysis, alpha-delta relationships | No differences in Polysomnographic measures were found. No differences in EEG power during REM and all other sleep stages. |
| Kishi et al. (2011) [215] | 14 patients 12 patients + fibromyalgia 26 controls |
Sleep stage transition probabilities and rates, sleep continuity. | ↑ probability of REM to waking transition in patients with ME. ↑ rates of transitions in patients+FM ↓ continuity of stage 2 sleep in patients+FM |
| Le Bon et al. (2012) [190] | 10 patients 10 controls |
EEG power spectral analysis including ultra-slow (0.5-0.8 Hz) delta power. | ↓ Ultra-slow delta absolute power was 1/5 that of controls |
| Kishi et al. (2013) [197] | 17 patients 16 controls |
Effects of exercise on sleep dynamics: transition probabilities and rates, sleep continuity with relationship to subjective fatigue, pain, sleepiness, depression, and anxiety. |
↑ disruption of REM sleep in patients related to increased subjective fatigue levels. ↑ quality of sleep in both groups after exercise, but patients reported greater subjective fatigue. Patients did not fully normalize sleep dynamics with exercise. |
Studies without a control group were omitted from this table.
Also earlier mentioned, using quantitative EEG data, Donati et al. [179] found temporal-lobe spiking, consistent with seizure activity, which are typically found after traumatic brain injury and extreme sleep deprivation. Using a multiple sleep latency test, in which patients were given the opportunity to fall asleep during five 20-minute nap periods, Spitzer and Broadman [201] found that 80% of patients with FM and ME fell asleep in under eight minutes, an indication of excessive daytime sleepiness. In addition, DQB1*0602, an immunological marker that is present in about half of people with narcolepsy, was present in 43% of patients, five times higher than in healthy people. People
with narcolepsy sleep poorly at night and have excessive daytime sleepiness. Spitzer and Broadman [201] believe that patients with ME and FM have a lesion in the ventral-lateral preoptic nucleus of the hypothalamus, which is critical to initiating and maintaining sleep.
Stress can trigger mast cells, which are heavily populated in the thalamus (located next to the sleep/wake center in the hypothalamus), to release the stimulant histamine. Excessive mast cells and their release of stimulants could be one of the reasons that sleep is interrupted in patients with ME and FM. Mast cells act as an immunologic defense against external pathogens, and there are 5 to 14 fold increases of these cells in the top layer of the skin in 100% of patients with FM [202]. Kindling may impact mast cells and the release of histamine in the thalamus, resulting in disrupted sleep patterns among patients with ME.
4.1. Measuring Sleep Dysfunction
Unrefreshing sleep, disturbance of sleep quantity, or rhythm disturbance have been documented by polysomno-graphy [203]. However, Togo and Natelson [204] found that standard polysomnographic methods did not differ between ME and healthy control groups, but patients with ME who reported more sleepiness after a night’s sleep showed significantly higher fractal scaling exponent (a1) of beat-to-beat RR interval dynamics in heart-rate variability analysis during non-rapid eye movement sleep than healthy controls.
Sleep dysfunction can also be assessed by using the Pittsburg Sleep Quality Index [205], which measures sleep disruptions and sleep quality. Using qualitative interviews, Gotts [216] first found that sleep disturbances experienced were highly unpredictable and variable over time among ME patients. Next, using self-reported sleep diaries, Gotts found that afternoon-evening napping was associated with greater impairment in daytime cognitive functioning in patients with ME. Gotts’ next study revealed four sleep-specific phenotypes that are amenable to different treatment approaches. Using single-night polysomnography, 30% had a primary sleep disorder. Gotts also found that sleep duration, wake duration, sleep efficiency, sleep stages were consistent across two nights of assessment. Gotts’ work provides excellent methods for documenting the disturbed sleep, which is a major problem for patients with ME, but is highly variable between and within individuals.
5. Secondary Symptom Subtypes
5.1. Immune Subtype
Exploring viral causes in ME has generated considerable interest with regard to their role in ME over the past several years [217, 218]. The consensus among ME case definitions is that immune manifestations may be related to the type of onset. However, many individuals who initially had an active viral onset, may, at a later time, have lower titers of the same viruses (became dormant). If this occurs, at this later time, immune symptoms might not be a distinguishable feature of the illness [31]. This view is supported by the lower prevalence of viral-like symptoms when compared to the three primary domains discussed earlier [8, 193]. Therefore, immune manifestations might be a subtype of ME, but not a cardinal symptom. Nonetheless, immune symptoms are important, as Hardcastle and colleagues [219] grouped individuals into healthy controls, moderate/mobile ME, or severe/bedridden ME; and immune deregulation correlated positively with patient reports of severity.
5.1.1. Kindling and Infection
The kindling effect is hypothesized to be one possible mechanism which continues to exacerbate symptoms long after the initial infection has cleared, thereby possibly playing a role in the etiology of the illness. For example, Elfaitouri et al. [220] evaluated patients with ME and non-ME (including blood donors, Multiple Sclerosis, Systemic Lupus Erythematosus), and found a peptide from Chlamydia pneumonia HSP60 detected IgM in 15 of 61 (24%) within the ME group, but only 1 of 399 (.25%) within the non-ME group, suggesting that a subset of the ME group had infection-induced autoimmunity. It is important to remember that pro-inflammatory cytokines are produced within the central nervous system in response to infection and that the presence of viruses increase activation of macrophages, which produce a release of interleukin-1 beta (IL-1β), a pro-inflammatory cytokine, causing an alteration in the electrical activity of the brain (altered the EEG) [221]. This sequence of events could occur with kindling.
Another pro-inflammatory cytokine, interleukin-six (IL-6), is produced by cells within the brain after exposure to viral infections contributing to the development of seizure activity [222]. It is well known that among patients with ME, the production of pro-inflammatory cytokines (IL-1β and IL-6) is correlated with acute sickness behavior (i.e., fever, malaise, pain, fatigue, and poor concentration) and that levels of pro-inflammatory cytokines may also be correlated with ME symptom severity. Some studies have found increases in both pro- and anti-inflammatory immune responses, while others found an attenuated inflammatory response when ME cultures were exposed to lipopolysaccharide (LPS) mitogen [223]. Thus, prolonged exposure to these cytokines may actually induce a state of chronic activation and kindling [224] along with pre-existent kindling which can also induce the production of pro- and anti-inflammatory cytokines, in turn worsening subthreshold kindling through a process of prolonged activation [225].
Administering the pro-inflammatory cytokine tumor necrosis factor alpha (TNF-α) has been shown to increase seizure activity in animals [226] and seizure activity has known kindling involvement [226-228]. TNF-α is a cytokine involved in systemic inflammation, and it stimulates the release of corticotropin-releasing hormone (CRH), therefore stimulating the hypothalamus-pituitary-adrenal (HPA) axis, placing individuals who have higher levels of these pro-inflammatory cytokines at greater risk of developing ME. In support of this proposition, Vollmer-Conna et al. [224] found that severe illness following an infection was more likely to occur among individuals with high levels of IFN-γ (a pro-inflammatory cytokine) and low levels of IL-10 (an anti-inflammatory cytokine). In addition, elevated levels of pro-inflammatory cytokines can lead to increases in levels of nitric oxide, and as described earlier, this nitric oxide can, in turn, react with superoxide to form the powerful oxidant peroxynitrite, resulting in oxidative stress.
Morris and Maes [229] speculate that initial infection and immune activation leads to a state of chronic peripheral immune activation driven by activated oxidative and nitrosative stress pathways. Raised levels of oxidative and nitrosative stress cause progressive elevation of autoimmune activity, and these processes provoke central nervous system activation in an attempt to restore immune homeostasis. In support of this theory, Maes, Mihaylova, et al. [230] found greater autoimmune responses directed against anchorage molecules and oxidatively-modified neo-epitopes discriminated patients with ME from those with depression. Maes, Twisk, and Ringel [231] compared inflammatory and cell-mediated immune responses between depression and ME. They found plasma proinflammatory cytokines were significantly higher in ME than a depression patient group.
Fletcher et al. [232] have suggested that the VN receptor vasoactive intestinal peptide receptor 2 (VPACR2) may induce an anti-inflammatory IL-10 response and could account for the suppression of cell-mediated cellular cytotoxicity. Although expressed in many tissues, the VPACR2 protein is highly expressed on the surface of T cells in patients with ME, which likely reflects the increase in Th2 cytokines [233]. VPACR2 has been shown to modulate the expression of IL-10 and other anti-inflammatory cytokines [233]. Binding of VPACR2 inhibits the expression and release of pro-inflammatory cytokines and acts to increase the secretion of anti-inflammatory factors [234], which further confirms a skewed Th2 immune response.
Along with increases in VPACR2 expression, Brenu et al. [233] and Fletcher, Zeng, et al. [235] found Natural Killer cell function to be low. Brenu, van Driel, et al. [236] examined cytokine secretions measured by stimulation of peripheral blood mononuclear cells. NK cytotoxic activity was significantly decreased in patients with ME, and the authors propose that this could be a biomarker for ME. Brenu, Ashton, et al. [237] found a significant reduction in the expression levels of miR-21, in both the NK and CD8+T cells in patients with ME. The expression of miR-17-5p, miR-10a, miR-103, miR-152, miR-146a, miR-106, miR-223 and miR-191 was significantly decreased in NK cells of patients. The authors conclude that changes in miRNAs in cytotoxic cells may disrupt effective cytotoxic activity along with other immune functions.
A review article by Klimas et al. [21] highlights a number of promising immune biomarkers associated with ME. For example, Dipeptyl peptidase IV/ CD26, a marker for chronic immune activation, is dysregulated in ME [235]. A substrate for this dipeptidase is neuropeptide Y (NPY), which was elevated in patients with ME [232] and correlated with symptom severity, including fatigue.
Going beyond conventional analytic methods that focus on the expression of individual markers, network-based approaches have found promising differences in immune regulatory processes [238-240]. Broderick et al. [238] applied network analysis to cytokines in patients with ME and healthy controls, and outcomes were consistent with a latent viral infection (i.e., attenuated Th1 and Th17 immune responses, an established Th2 inflammatory milieu, and diminished NK cell responsiveness). In another network study, Broderick, Klimas, Fletcher, and Efroni [239] found there were no genes expressed with a 2-fold difference between ME and healthy controls at rest. However, 18 such genes were differentially expressed at rest among patients with Gulf War Illness. Under physiological challenge, individuals with Gulf War Illness and ME showed distinct differences from each other and healthy controls. When moving to peak effort from rest, 166 genes became differentially expressed from rest in healthy controls, 50 genes responded to challenge at peak effort in Gulf War Illness but only one was expressed in ME at peak effort versus rest. So, Gulf War Illness showed a partial early response to maximal exercise challenge, but those with ME were unresponsive. Differences in gene expression implicated 90 documented pathways with the majority being linked to immune metabolism.
A group in Chicago has also used network analysis and found that MS and ME are characterized by a pro-inflammatory connective phenotype. Sorenson, Furst, Mathews, and Jason [241] found that patients with ME had IL-4, IL-5 and IL-13 connective phenotypes consistent with the Th2 phenotype. However, IFN and IL-12 were connected normally and hence the Th1 pathway was untouched by the illness.
Using Neural-Network Classifiers to differentiate ME groups and non-ME control groups, Hanson, Gause, and Natelson [242] found only one cytokine interleukin-4 remained in their final model, suggesting a shift in the ME group to a type 2 cytokine pattern. Another study also compared computational tools with and without feature selection for predicting ME using genetic factors such as single nucleotide polymorphisms [243]. They found a significant association of NR3C1with ME compared to non-fatigued controls, which suggests that NR3C1 may be involved in biological mechanisms with ME (the NR3C1 gene encodes the protein for the glucocorticoid receptor). Others have used machine learning algorithms to show that an inflammatory adipokine leptin could distinguish with 78.3% accuracy high from low fatigue days among a sample of ten women with ME [244].
Lerner and colleagues [245] had treatment success with patients with ME who had EBV, HCMV, and HHV6 in single or multiple infections. They found that 79 of 106 (74.5%) patients experienced significant improvements in functioning after herpes virus subset-directed antiviral treatment. Those with other co-occurring disorders (e.g., Lyme disease) had less favorable outcomes. More recently, they [246] found prolonged elevated antibody levels against the encoded proteins EBV dUTPase and EBV DNA polymerase in a subset of patients with ME but not in controls, suggesting that this antibody panel could be used to identify these patients. Evidence for the persistence of infectious agents has been found by Embers et al. [247], who infected Rhesus macaques with B. burgdorferi and then provided them with aggressive antibiotic therapy. These investigators found that B. burgdorferi can withstand antibiotic treatment, suggesting the same may occur in humans.
Loebel et al. [217] recently found that EBV nuclear antigen (EBNA)-IgG titers were low or absent in 10% of patients with ME, and when analyzing the EBV-specific memory B-cell reservoir, there was a diminished or absent number of EBNA-1- and VCA-antibody secreting cells in up to 76% of patients with ME. This is evidence for a deficient EBV-specific B- and T-cell memory response in patients. The authors suggest that patients might have an impaired ability to control early steps of EBV reactivation.
Tzartos and colleagues [248] provided information that in an active Multiple Sclerosis lesion, a latent Epstein-Barr virus infection can trigger interferon-α production. In other words, while the virus was not actively replicating, it was releasing small RNA molecules in the brain, causing inflammation and damaging nerve cells in the brain, and thereby causing symptoms. This is of particular interest as Capuron et al. [249] found that interferon-α was associated with increases in glucose metabolism in the basal ganglia and cerebellum and decreases in the dorsal prefrontal cortex glucose metabolism, which may be contributing to fatigue in medically ill patients.
In a recent (2015) phase 2 study designed to establish the therapeutic efficacy of Rituximab, Fluge et al. [250] found that infusions of rituximab (Rituxan), which depletes B cells, led to significant and sustained clinical responses in 64% of patients with ME with 11 out of 18 continuing to improve at 3-year follow-up. Nine controls experienced no effect, until they were also infused (at 12 months after study start), at which time they likewise had significant improvement. The results suggest that, for some patients, ME could be an autoimmune disease variant involving B-lymphocytes.
Jason et al. [251] combined their four non-pharmacologic treatment groups into two categories, improvers and non-improvers, based on a measure of physical functioning (as measured by the SF-36, with higher scores indicating better functioning). About half of the participants in each group were improvers and the other half were non-improvers. For these two groups, there were no significant baseline differences in physical functioning. However, at follow-up, physical functioning scores for improvers increased from 43.9 to 66, whereas non-improvers’ scores declined from 50.4 to 42.2. What was most remarkable between these two groups was that improvers had decreased T and B cells and elevated NK percentage numbers at baseline, whereas non-improvers had an elevated humoral immune response (in other words, a dominance of the Type 2 over the Type 1 immune response) at baseline. Those with the most severe immune baseline characteristics tended to be non-improvers. As this illness is associated with a shift toward a Type 2 immune response, those with this pattern at baseline tended not to improve over the course of the trial.
More recently, Falkenberg, Whistler, Murray, Unger, and Rajeevan [252] found perforin expression was normal during rest, but then decreased during a stress test and an hour and a half after the stress test, the levels increased dramatically, suggesting problems regulating functioning in response to stress. Patients with were later subdivided into low and high methylation rates, and those with high methylation rates had significantly lower perforin gene expression just after exercise.
Hornig et al. [253] examined 52 ME patients early in the course of illness (less than or equal to 3 years) with those who were ill longer, and the early patients had activation of both pro- and anti-inflammatory cytokines as well as dissociation of inter cytokine regulatory networks. In a different study, Hornig and colleagues [254] analyzed cerebrospinal fluid from patients with ME (who had been ill for 7.6 years on average), MS and normal subjects. Network analysis indicated immune activation in the central nervous system (i.e., a shift toward T helper type-2 pattern associated with autoimmunity).
5.1.2. Measuring Immune Dysfunction
The presence of immune dysfunction could be measured by elevations in CD5+CD19+ subset and decreased natural killer cell cytotoxicity [255]. Other potential markers include immune activation e.g., elevated cytokine levels, inflammatory markers (elastase, etc.), immune dysfunction (e.g., RNAse L fragmentation, Th1-Th2 cytokine markers), and immunosuppression e.g., IgG subclass deficiencies (IgG1 and IgG3), NK Cell activity including perforin and granzyme levels). The most promising strategies might be those that use network analyses, as suggested by several investigators [238-241]
5.2. Autonomic Subtype
While orthostatic intolerance and other autonomic issues are an important problem for some patients with ME, they do not occur with the high frequency as other symptoms such as PEM, neurocognitive and sleep difficulties [193], and are therefore considered a sub-type rather than primary symptom.
Stress can be defined as any physical or psychological threat that induces chemical and physiological changes in the body when the body detects a challenge to homeostasis and responds to it by activating the stress response [68]. During activation, the stress response triggers a wide variety of hormones and neurotransmitters released through the hypothalamic-pituitary-adrenal (HPA) axis [256]. These hormones and neurotransmitters then have numerous effects on multiple local and remote sites to maintain the immune system, inhibit non-essential processes such as eating and keeping the periphery warm, and later returning the body to homeostasis [257-259].
The stress system is a highly flexible system, designed to keep the body as close to homeostasis as possible despite the wide variety of challenges present in everyday living [260-262]. However, when this system becomes chronically or recurrently hyperactivated or hypoactivated, the ability of the body to utilize the stress response to respond appropriately to physical or psychological challenge becomes compromised. This compromised state is known as “allostatic load,” [261, 271, 349] reflecting the impact of life experiences, genetics, disease, etc., thereby impairing the body’s ability to adapt [68, 257-262]. One aspect of stress-related medical problems can therefore be characterized as a failure of adaptation—a failure of the system to change in accordance with environmental, chemical or physical demands [261, 263]. This cascade of events has been consistently associated with adverse health outcomes [259, 262-264] involving a range of endocrine and inflammatory disorders, and susceptibility to these disorders [259, 262-267] including poorer prognosis in the disorders listed previously, as well as in other medical conditions [268-270]. For example, impairments in the stress system have consistently been associated with abnormal aging [271] and many other disease states [171, 271-274], including ME [171]. Moreover, when the stress system is chronically deregulated, the result is physical changes in neural circuitry becoming hard-wired through neural plasticity [265, 275], which in turn supports a condition of a chronically elevated stress baseline or stress kindling [276-278]. It is this reduced (or lack of) adaptation that is the subject of a large body of research, illustrating the role of the deregulated stress response in health and disease [257, 266, 279] with a smaller but compelling literature regarding the role of deregulated stress system in ME [280].
It is the autonomic nervous system and the neuro-endocrine system which regulate the stress response as primary biological mediators between stress and illness as well as illness and stress [260]. Therefore, a chronically deregulated stress response (dysfunctional autonomic nervous system) can take many forms in that the stress response and the disease itself may display a bi-directional causal relationship [281, 282]. In ME, the notion of deregulated autonomic nervous system involvement in some patients with ME has been proposed [283], with some authors arguing that the deregulated stress response is a product of the illness [281] and others stating that the direction of the relationship cannot be determined [283]. Regardless of the direction of the relationship, the stress system in ME is thought to be unstable through chronic activation [171, 284] or chronic hypoactivation [22, 257, 258, 283-285].
Over the past 2 decades, the stress system in ME has been studied by several investigators using a variety of triggers to study it. Light et al. [33, 34], using exercise as a trigger, found that after moderate exercise, two subtypes of changes occurred within the ME group. In 71% of the ME group, large gene expression occurred for multiple systems, including sensory receptors, adrenergic receptors (SNS), and cytokine receptors, but only 18% of that group had orthostatic intolerance. However, for 29% of the ME group, there was only SNS dysregulation, and 71% of these patients had orthostatic intolerance.
Another system affected by stress system dysregulation in ME is the cardiovascular system. According to Visser [286] cardiovascular irregularities seen in ME can be due to several factors which are associated with the stress system. Due to the association of cardiac problems in ME with the stress system, sympatho-vagal balance (measured in heart rate variability indices—see Malik and Camm) [287] is used in many ME studies involving different stress triggers. For example, patients with ME have been shown to have higher levels of serum catecholamines (stress-related hormones) [204, 288], which can directly contribute to increased heart rate but decreased heart rate variability (HRV) [272]. Heart rate by itself is not a good indicator of stress due to the multiple influences on it. In contrast, HRV analysis has been shown to be a reliable and valid measure of ANS (stress) activity [287]. In HRV analysis, components of the heart beat are assessed by spectral analysis; high frequency power (HF) indicates SNS dominance while low frequency (LF) power indicates PNS dominance [289]. In ME, there is a small but growing literature on HRV being compromised when compared to norms [290-292].
Another measure of stress is blood oxygenation or blood volume. In a study of blood oxygenation, patients with ME demonstrated lower blood volume than normals [79]. Taken together, these studies point to a dysregulated autonomic nervous system which creates symptoms consistent with ME symptoms (lightheadedness, dyspnea). Some have argued that as electrical stimulation to the vagus nerve can block inflammation, the vagus nerve might be infected, which could be contributing to inflammation in the periphery [293].
Hollingsworth, Hodgson, Macgowan, Blamire, and Newton [294] found those with ME had the following cardiac abnormalities: substantially reduced left ventricular mass (reduced by 23%), end-diastolic volume (30%), stroke volume (29%) and cardiac output (25%) and in 2014, Miwa [288] found 35 out of 36 patients with ME had OI and significantly smaller left ventricle sizes than normals. These results suggest that, compared to controls, patients have significant impairments in stroke volume and cardiac output. Beaumont et al. [295] found ME was further characterized by low HRV, greater heart rate reactivity and prolonged heart rate recovery after cognitive challenge. This study suggests that there may be an association between reduced cardiac vagal tone and cognitive impairment in ME. In another study involving HRV analysis, at rest, low frequency heart rate variability (LF-HRV; a measure of SNS dominance) was significantly increased in ME compared to controls, while parasympathetic markers (high frequency heart rate variability or parasympathetic predominance) was significantly reduced [296]. In a study involving blood pressure and HRV to measure autonomic dysfunction, Frith and colleagues [297] suggested that abnormalities of blood pressure variability could serve as a diagnostic tool. Total diastolic blood pressure (DBP) spectral power was increased indicating a shift towards sympathetic and away from parasympathetic systolic blood pressure variability (SBPV). On standing, overall SBPV response was significantly reduced with reductions in both sympathetic and parasympathetic components of SBPV. Using the 85% sensitivity levels, they determined a threshold for three chosen resting BPV parameters of LF DBP >3.185, rest HF DBP >0.86, rest total DBP >7.05. Achieving all of these differentiated between ME and controls with 77% sensitivity and 53% specificity.
Dysregulation of the ANS in ME is also functionally related to cardiac arrhythmia, especially in abnormally fast heart rhythms [297-299]. Cardiac arrhythmias are any variation from a normal rhythm of the heartbeat with the irregularities occurring in either rate, regularity, site of origination or sequence of activation [300]. Arrhythmia can include abnormal irregular heart rhythms and/or loss of rhythm [301] and can originate from the upper chambers of the heart (supraventricular) or lower ones (ventricular). In POTS, the heart rate increases abnormally quickly upon standing. A common complaint of patients with ME is that of skipped, irregular beats (ectopic beats), extra beats, or an abnormally fast heart rate. In the absence of structural heart disease, cardiac arrhythmias can arise from a wide variety of circumstances with the most prevalent explanation being a deregulated stress system [26, 325].
Li et al. [302] found that among patients with POTS, autoantibodies interfere with the system which controls the ability of blood vessels to constrict, and this is needed to prevent a drop of blood pressure when a person stands. The inadequate response to standing leads to a generalized increase of activity in the ANS, which plays a part in normalization of blood pressure. The increased ANS activity in turn increases a prominent symptom in patients with POTS, increased heart rate. Li et al. [302] also found a second group of autoantibodies in some POTS patients which directly increase the heart rate. In this study, the combination of these two autoantibodies played a part in the abnormal heart rate response seen in study participants.
Autonomic dysfunction is common in ME which can also be seen in another measure of heart rate, the QT interval. In normal heart rhythm, the QT interval extends from the onset of the QRS complex to the end of the T wave. Thus, it includes the total duration of ventricular activation and recovery in a heartbeat [295]. Even though QT intervals are difficult to measure accurately, overall, the longer the QT interval the higher the likelihood of having ventricular arrhythmia. However, in recent years, another abnormality found in autonomic dysfunction is short QT intervals, typically seen in patients with hypocalcemia and in some disorders of autonomic failure [303]. Since several studies have demonstrated ANS dysregulation in ME, the QT interval could be a diagnostic marker for ME. Although Scott, Norton, Mabillard, and Newton [304] found no statistically significant difference between the average QT intervals in the ME compared to the non-ME fatigued group, the QT intervals were shorter for those with ME overall, suggesting the short QT interval syndrome may be found in ME.
Lewis, Pairman, Spickett, and Newton [305] conducted a study on a subgroup of patients with ME who had been previously diagnosed with POTS. POTS can be objectively measured by autonomic function analysis or hemodynamic responses upon standing. This study revealed that a combined clinical assessment tool with the Epworth Sleepiness scale and the orthostatic grading scale was able to accurately identify those with ME and POTS with 100% positive and negative predictive values.
Another measure of the ANS is through eye pupil reaction. Badham and Hutchinson [306] found that when patients with ME were asked to accurately tracking a moving object, even for a short time period, dysfunctional eye movement behavior was found. Hutchinson, Maltby, Badham, and Jason [307] found that vision-related symptoms might be particularly discriminative in making the diagnosis of ME. Sensitivity to bright light, inability to focus vision and loss of depth perception may all be neurologically related pupil function, as pupils are mainly controlled by the autonomic nervous system (and the balance between sympathetic and parasympathetic nervous systems effectively controls pupil size and speed of reactivity). These vision-symptoms may be another sensitive marker of autonomic dysfunction.
5.2.1. Measuring Autonomic Dysfunction
Autonomic manifestations can potentially be measured using a tilt table test showing decreased blood pressure and/or increased heart rate [39] or by using HRV measurement. To confirm dysfunction, the Composite Autonomic Symptom Scale has been used [308].
5.3. Neuroendocrine Subtype
Neuroendocrine manifestations have been given secondary prominence within ME case definitions [31, 309], and empirical findings indicate they are less prevalent than other core symptoms [8, 193]. This domain could therefore be referred to as a subtype. Findings spanning over 30 years demonstrate decreased HPA activity in ME [281, 310-316] as well as reductions in peptides such as CRH and ACTH which stimulate the HPA axis, implicating reduced HPA activity in the pathophysiology of ME. Many studies, such as those in a recent review article by Powell, Liossi, Moss-Morris, and Schlotz [317] find consistently that the cortisol-awakening response is deregulated in ME and not necessarily total cortisol. It should be noted here that stress and elevated (or depressed) glucocorticoids (cortisol) do not covary in an equivalent manner, and there are individual differences in HPA function, though it is not well understood, making cortisol measurement of the stress response problematic [318].
5.3.1. How Illness Affects the CNS
It is well known that survivors of critical illness are a high risk to develop permanent and severe cognitive impairment [319]. To the CNS, exposure to illness is an acute injury [104-106, 319-322], which activates the stress response and in turn, triggers a number of hormones that are released and regulated by the HPA axis. These hormones affect numerous sites in the brain and periphery [323] including the immune system [324], influencing CNS’s reaction to the toxic insult of infection [105]. Glucocorticoids (GC), the most common of which is cortisol, are known for their anti-inflammatory effects, but only in the periphery; GCs have been shown to be pro-inflammatory in the CNS [68, 259, 318, 323, 324], which in turn, contribute to neuronal damage through inflammation [259, 325]. It is inflammation which then contributes significantly to the release of cytokines and free radicals [318]. Also, as previously stated, CRH induces neuronal excitability, which can lead to seizure activity [326]. Fevers and trauma can activate CRH receptors in the hippocampus and amygdala to induce seizures in both children and rats, and CRH increases the frequency of spontaneous excitatory postsynaptic currents by as much as 252% [326]. Infections could cause the sub-threshold kindling effects that eventually increase levels of CRH. Once the kindling has occurred, the CRH may play a less critical role in maintaining the kindling, and after time, CRH levels may become depleted.
Cleare et al. [327] has suggested that hypocortisolism could contribute to ME by failing to modulate the immune system. However, Arnett et al. [69] suggest that it is more likely that an immune dysfunction progresses to ME rather than a hypoactive HPA axis dysfunction predisposing someone to ME. Supportive evidence for this is that the length of the illness is positively correlated with HPA axis dysfunction, and efforts to treat ME with corticosteroids have not been effective. It is also of interest that glucocorticoids have a more immunosuppressant effect on men than women [328], and this functional difference in immune systems may result in a higher pro-inflammatory response to infection in females. Accordingly, this may aid to explain why about 75% of patients with ME are female.
As previously reviewed, differences have also been found in the expression of glucocorticoid receptor (GR) (NR3C1, the encoding gene for GR) in individuals with ME when compared to controls [329]. Those with ME may have decreased sensitivity to the effects of cortisol due to a down-regulation of GR [330]. In a pediatric ME sample, Jason et al. [331] found hypocortisolism and the down-regulated expression of NR3C1. It is possible that epigenetic alterations in expression of NR3C1 leads to an inflammatory immunologic profile, which further suppresses cortisol levels through a process of feedback through bidirectional pathways. The reduced expression of NR3C1 provides further evidence for dysfunction of the HPA axis in those with ME. Meyer et al. [332] has also found significant differences for NR3C1 between patients with ME versus controls following a maximal exercise challenge, suggesting that increased glucocorticoid sensitivity may contribute to symptoms of post-exertional malaise for patients.
Histone deacetylases (HDACs) are a group of enzymes that inhibit the process of DNA unwinding [333]. Among an elderly sample with ME, Jason, Sorenson et al. [60] found increased HDAC activity in the context of decreased plasma cortisol concomitant with decreased expression of the encoding gene for the glucocorticoid receptor. Therefore, it is possible that increased HDAC activity may in turn contribute to a chronic pro-inflammatory state that may result in the expression of fatigue, through the inhibition of gene expression.
Chronic cortisol deficiency can cause an overproduction of pro-inflammatory cytokine IL-6, which has been associated with symptoms of ME [334]. Lower cortisol [335], as well as an overactive sympathetic nervous system, could be responsible for the findings of ejection fraction decreases (the fraction of blood pumped out of the ventricles per heartbeat) and lower cardiac output among patients with ME [336].
Jason et al. [251] categorized patients from non-pharmacologic interventions into abnormal versus normal baseline cortisol levels. Readings were categorized as abnormal if cortisol levels continued to rise, was flat, or was abnormally low over five test times during one day. Patients with normal cortisol at baseline had the most improvements over time in activity levels, fatigue severity, depression, anxiety, and immune system markers. Thus, patients with normal baseline cortisol evidenced improvements on a number of immunologic and self-report measures, whereas patients most impaired on hypothalamic-pituitary-adrenal functioning at baseline may be least able to improve when provided non-pharmacologic interventions.
There is also evidence for the existence of a persistent hyperserotonergic state in some patients with ME [337], and this refers to synaptic serotonin concentrations. This state may be related to the inducible form of nitric oxide synthase that is produced during inflammation. As mentioned earlier, high nitric oxide concentrations can activate the NMDA receptor, which antagonizes the serotonin receptor signal transduction pathway. Arnett et al. [69] proposed that, as the pathways of NMDA and serotonin are antagonistic, this hyperserotonergic state may be an attempt to overcome the chronic inhibition of serotonergic pathways due to increased activation of the NMDA pathways.
The serotonin hypothesis links fatigue to increases in serotonin synthesis and elevations of activities of serotonergic neurons. Several investigators have found patients with ME have an abnormally high level of brain serotonin, and this may contribute to the persistent central fatigue [338]. One pilot study found that medications that block serotonin (5-HT3) receptors were followed by at least a 35% improvement in about one-third of patients with ME [339]. Vassallo et al. [340] found evidence of elevated activity of presynaptic serotonin neurons, which could be an area affected by kindling.
Still, there may be subtypes of patients with ME, with some evidencing decreases in serotonin levels. For example, Badawy, Morgan, Llewelyn, Albuquerque, and Farmer [341] found decreased brain serotonin levels in patients with ME. Yamamoto et al. [148], using PET, found that the density of 5-HTT (the serotonin transporter involved in the reuptake of serotonin from the synaptic cleft immediately after its release) of the rostral subdivision of the anterior cingulate cortex was significantly reduced in patients with ME. These findings suggest that an alteration in the serotonergic neurons in the anterior cingulate cortex, specifically a depletion of serotonin, may play a role in the pathophysiology of some patients with ME.
Glass et al. [342] found that healthy individuals with certain biological patterns (i.e., lower cortisol, reduced heart rate variability, and NK attenuated response to stress) developed somatic symptoms when asked to stop exercising for a week. These biological patterns may be some of the other predisposing neuroendocrine and immunologic irregularities of some individuals who are at increased risk for sensitization and kindling, and ultimately, developing ME.
Another possible neuroendocrine problem has recently started gaining momentum in the research community; that is, Multiple Chemical Sensitivities (MCS). MCS is characterized by debilitating chemical sensitivities whereby even small exposures to chemicals found in many common products (paint, laundry products, perfumes, smoke, and building materials). While these exposures make most people ill at high or persistent levels, those with MCS experience symptoms after very small amounts of exposure. Baraniuk and Zheng [343] hypothesize that further research about nonallergic hypersensitivity pathways will elucidate the etiology of MCS.
5.3.2. Measuring Neuroendocrine Dysfunction
Since neuroendocrine manifestations have frequently measured levels or patterns of circulating cortisol [316], our recommendation, based on findings from Powell et al. [317], is to assess the attenuation of the cortisol awakening response increase (e.g., cortisol at awakening minus waking levels). Neuroendocrine manifestations have also been measured with the DePaul Symptom Questionnaire (DSQ) [344] confirming neuroendocrine symptoms (e.g. feeling hot or cold, night sweats).
5.4. Pain Subtype
There is consensus among the current ME case definitions that while pain is experienced by many patients, it is not a core symptom category of ME [31, 309]. Early findings of pain can include: headaches associated with neck rigidity and occipital eye pain, migratory muscle and arthralgia pain, and cutaneous hypersensitivity. Late findings of pain can include any of the early findings and also Fibromyalgia-like pain syndromes [39].
The sensitization theory has been proposed as a possible explanation for the pain and lower pain threshold in patients [123, 345, 346]. In this model, repeated or sustained noxious stimulation can lead to increased neuronal responsiveness or central sensitization [123], and this stimulation can cause the spinal cord to become sensitized, or placed into a “hyperexcitable” state [347]. Martinez-Lavin and Solano [348] speculate that within the dorsal root ganglia, after trauma or inflammation due to infection, sympathetic nervous system neurons gain greater long-term potentiation through up-regulated ion channels, increasing pain synapses in the dorsal root ganglia become hyperexcitable to painful inputs. In other words, patients may have a sensitized central nervous system, and if the pain inhibitory systems are not functioning adequately, the central nervous system may become hyperexcitable.
We are beginning to learn the mechanism for this sensitization. Following an injury, the dorsal root ganglia are in a state of neuropathic pain, and glia prolong this state of neuronal hypersensitization by releasing substances that act on the immune system [349]. Vargus-Alarcon et al. [350] suggest that for some patients with severe FM, the sodium channels of the cell bodies in the dorsal root ganglia act as molecular gatekeepers for pain detection. When NMDA receptors of neurons are activated, calcium enters into the dorsal horn neurons, leading to the synthesis of nitric oxide [351]. Nitric oxide enhances the release of sensory neuropeptides, such as substance P [352], and this substance increases synaptic excitability. When substance P is released into the neurons, the NMDA receptors become hypersensitive to glutamate, which is the chief excitatory neurotransmitter in the brain [353]. High levels of NMDA receptors on a cell indicate that the cell is hypersensitive to glutamate. As a consequence, spinal neurons are sensitized, and individuals have an increased sensitivity to pain. Cooper and Clark [67] also show how an injury can result in a widespread chronic multi-system condition (Complex Regional Pain Syndrome 1), where inflammation spreads throughout the nervous system.
5.4.1. Measuring Pain
Symptoms of pain can be assessed with the DSQ [344] (e.g., feeling pain or aches in muscles, experiencing headaches) or the well validated McGill Pain Questionnaire [354].
6. BIOCHEMISTRY IN ME SYMPTOMOLOGY
With all the studies reviewed above indicating biological abnormalities, many physicians do not have access to these more sophisticated measures. Blood biochemistry in ME (complete blood counts) tends to fall within normal laboratory ranges, but it is important to note that there are discernable differences within the reference ranges. For example, Niblett et al. [355] conducted a case-control comparison of blood cell data which revealed that those with ME had a significant decrease in red cell distribution width but increases in mean platelet volume, neutrophil counts, and the neutrophil-lymphocyte ratio, suggesting alterations in physiologic homeostasis. In the same study, the overnight urine output and rate of amino acid excretion were also both reduced in the ME group, and there were significant decreases in the urinary excretion of asparagine, phenylalanine, the branch-chain amino acids, and succinic acid, as well as increases in 3-methylhistidine and tyrosine.
Of course, more advanced types of testing have found many different types of abnormalities, and we will review just a few more as we end this section. For example, Booth, Myhill, and McLaren-Howard [356] worked with patients diagnosed with ME and normal, healthy controls, and found that all patients had measureable mitochondrial dysfunction, which significantly correlated with the severity of the illness. In another study involving gene expression, Piraino, Vollmer-Conna, and Lloyd’s [107] examined discrete symptom domains which included fatigue and possible genetic associations, the T allele of the IFN-γ +874 T/A SNP was associated with increased fatigue, whereas the C allele of the IL-10 -592 C/A SNP exerted a protective effect on neurocognitive impairment. Using saliva samples to analyze protein profiles, Ciregia et al. [357] found 13 proteins with a different expression in ME versus controls indicating the inflammatory response.
7. FIBROMYALGIA
Comparable findings occur within studies of Fibromyalgia (FM), establishing considerable shared variance between the two medical problems. In a recent study by Keller [358], 46% of patients with FM versus 17% among controls were found to have reduced nerve fiber density in their leg biopsy to below the fifth centile of the predicted value, which is considered evidence of small-fiber polyneuropathy; other investigators have confirmed this observation [359-361]. In a study of autonomic nervous system activity, Chalaye, Lafrenaye, Goffaux, and Marchand [362] found significantly increased heart rate but reduced blood pressure in a sample of patients with FM. The Default Mode Network is a set of brain regions which are functionally active when an individual is focused inward. Brain imaging studies have found reduced functional connectivity in the Default Mode Network in FM [363, 364], providing an objective marker that tracks changes in spontaneous chronic pain in FM while Hargrove et al. [365] found reduced EEG power in the frontal lobes of the cortex, elevated power in the central lobes and widespread reduced functional cortical connectivity in a sample of 85 patients and 85 controls. As cognitive and motor operations are dependent on the frontal and central lobes [366], there is growing evidence for cognitive impairment and impaired motor control in FM.
These and similar studies demonstrate that more fine-tuned investigations are discovering biological abnormalities for individuals with both FM and ME [20, 21], providing evidence for the biological underpinnings of these domains/symptoms and possible biomarkers. In addition, we have provided evidence for the 'kindling hypothesis' [14, 61, 63, 367, 368] as a model for better understanding of the etiology of some ME symptoms.
8. DISCUSSION
In reviewing ME case definitions, it does appear that there is consensus on the requirement for symptoms within the PEM and neurocognitive domains. Given the high prevalence of sleep disturbances, it might also be considered a central symptom of ME. Whereas immune, neuroendocrine, autonomic and pain domains are less prevalent for patients with ME, we propose that these areas might be considered subtypes. A number of secondary symptoms that may fall under different sub-groups, and some individuals may have ME with several subtypes such as both pain and autonomic domains, and there is growing evidence for the importance of subtyping patients [369]. Whereas standard medical tests infrequently identify ME abnormalities, research reviewed in this article suggest there are a number of promising central nervous system, inflammatory, circulatory, neuroendocrine, and pain markers of impairments. These biological findings could be used in demarcating critical domains and subtypes of ME.
In this article, we have recommended reduction of the key symptoms to a minimum followed by identifying sub-groups based on additional symptoms. The case for these ideas would be significantly strengthened if the data were available to show that the proposed key symptom domains accounted for the greater proportion of disability as measured by the physical functioning scale of the SF-36. However, in contrast, it may be that primary symptoms are not present at all stages of the illness. Future studies may be directed toward determining the role of the secondary symptoms in how they contribute to illness burden. For example, pain is the major contributor to incapacity and self-reported symptoms, and some might therefore challenge its relegation to secondary status.
In a recent review article, Johnston, Brenu, Staines, and Marshall-Gradisnik [370] found that differences in method of assessment was possibly due to the heterogeneity in ME prevalence, and they urged researchers to exercise caution for estimates of prevalence determined by the self-reporting of symptoms alone. There is much potential in using more biological methods to confirm differences in diagnostic classifications [371]. For example, Brenu et al. [236] found natural killer cell activity significantly decreased for both the Fukuda [5] and the ME-ICC [7] case definitions, but only those diagnosed with the ME-ICC had significant correlations between physical status and some immune parameters.
We have only touched upon issues of the case definition in this review. Some might feel that the Canadian ME/CFS criteria [6] might suffice as a new case definition of ME. Unfortunately, in Johnston et al. [370, 372] review of 31 CFS prevalence studies, 8 different case definitions, and only one study reported prevalence according to the Canadian Consensus Criteria.
One candidate for an ME case definition is the International Consensus Criteria for Myalgic Encephalomyelitis (ME-ICC) [7]. Jason et al., [10] contrasted the ME-ICC criteria with the Fukuda et al. [5] CFS criteria. Findings indicated that the ME-ICC criteria identified a subset of patients with more functional impairments and physical, mental, and cognitive problems than the larger group of patients who met the Fukuda et al. [5] criteria. However, the patients who met the ME-ICC criteria also had significantly greater rates of psychiatric comorbidity. The ME-ICC criteria requires 8 symptoms, and the Holmes et al. [373] CFS criteria were previously criticized for having a similar number of somatic symptoms, which can increase chances of identifying those with somatization disorder.
Methodological developments, such as the use of network analysis of cytokines and data mining might ultimately aid in this effort to match ME biological markers to a case definition. Machine learning or data mining is one of these techniques which could help compare and contrast case definitions as well as determine the types of symptoms that may be most useful in accurately diagnosing ME. In particular, data mining can uncover patterns in the data that would not be evident to humans because of the size and complexity of the data.
Given the diagnostic complexity of ME, and the multiple case definitions available for clinical and research application, there is a need for comprehensive medical tests to identify dysfunction in core domains, as well as much more sensitive self-report tools to aid in symptomatology assessment, such as the DePaul Symptom Questionnaire [344] which has demonstrated high test-retest reliability. A well validated measure capable of classifying individuals with ME using a variety of case definitions, allows researchers across settings to identify groups with more homogenous phenotypes. Consistent identification of more homogenous patient samples could possibly assist in the pursuit of biomarkers for ME.
Conceptual models influence our research as well as our development of case definitions. Our work in this article has been based on a model that has heuristic appeal, and it posits that neurotropic viral infections could be responsible for the appearance of lesions in the brain and the presence of focal epileptiform seizure activity in patients with ME. It is possible that kindling could play a major role in the promotion of these seizures, given that kindling has been shown to increase brain dysregulation as seen in abnormal significant increases in slow EEG frequencies (i.e., EEG delta (1-4 Hz) and/or theta (5-7 Hz) [66, 374, 375]. EEG slow waves are produced by the thalamus, which receives its input from the amygdala [375, 376] and hippocampus [378] in response to brain damage [379, 380]. Though the exact mechanism is still under investigation, there is an impressive body of literature indicating the components of the effect of kindling on brain rhythms, which in turn, affect cognitive abilities [78]. Reactivation of various herpes viral infections and/or chronic mycoplasma infection causes abnormal production of cytokines, which can lead to increases in levels of CRH [225]. CRH then elevates the frequency of spontaneous excitatory postsynaptic currents by as much as 252% [326] which may be among such routes [377] increasing seizure susceptibility in the hippocampus [381, 382]. Consequently, CRH receptors in the amygdala may induce seizures [326], through limbic eleptogenesis [66] and the stress response [383] which can cause dendrites to more densely populate the amygdala [384]. In some cases, cortical lesions caused by herpes viridae infections fade before MR documentation can take place. Lesions may then reappear under specific conditions of environmental stimuli, a process that fits well with the relapsing and remitting nature of ME. Within the brain, psychological stress can change homeostasis, especially within areas of the prefrontal cortex and anterior cingulate, which in turn influence the limbic system [271, 385, 386], so kindling in these areas may cause continuous sympathetic nervous stimulation that would eventually lead to glandular depletion, affecting the stress response and the limbic system. There are clear non-infection routes into ME, and brain damage can occur from other sources such as chemicals or accidents (symptoms of post-concussion syndrome include PEM and alcohol intolerance) to begin this posited neuro-inflammatory state.
In long-term potentiation, synaptic strength increases between co-firing neurons after brief but repetitive stimulation, and this has many similarities to kindling. LeDoux [387] refers to these cell assemblies as being particularly resistant to extinction; so, for some patients, this hard-wiring may only be regulated rather than extinguished. Gupta [388] believes that activation of the amygdala causes continuous sympathetic stimulation that is a predominantly unconscious process over which patients have little control, but it eventually leads to mental and physical exhaustion as well as glandular depletion. Wyller et al. [171] proposed compatible theories, stating that sustained arousal is the primary mechanism of ME.
However, as an example of the contradictory findings in this area, a recent randomized trial of clonidine [389] found that low-dose clonidine is not clinically useful in pediatric ME, even though low-dose clonidine did attenuate sympathetic outflow and systemic inflammation in ME, and had a negative effect on physical activity. The investigators conclude that sympathetic and inflammatory enhancement may be compensatory mechanisms. In other words, they found that neither sympathetic enhancement nor low-grade systemic inflammation contributes to symptoms and disability in ME, as postulated in the sustained arousal model.
In the future, we might find new proteins that strongly influence the persistence of viruses. For example, Toll-like receptor 7 (TLR7) is a protein encoded by the TLR7 gene. It recognizes infectious agents and mediates the production of cytokines that are needed for immunity. In mice, if this protein is not present, mice are not able to clear infections throughout their lives. This might have implications for people who have persistent viral infections, and particularly for patients with ME [390]. However, Hooper, Hightower, and Hooper [391] proposed that viral infections can induce a deficient cell stress response and thereby impairs stress tolerance and makes tissues vulnerable to damage. If this is true and that ME is due to a nonspecific response to viral infection, Hooper et al. [391] believe that the search for a specific virus may not be worthwhile. In addition, Agliari, Barra, Vidal, and Guerra [392] suggest that the immune system might experience Pavlovian conditioning following exposure to stimulus that lasts a long time (such as what occurs with viral infections such as Epstein-Barr virus).
New classes of drugs are emerging that might have important implications for reducing inflammation and arousal in patients. With animal models, there is research on these new classes of drugs (MW151 and MW189) that address neuroinflammation, which can easily cross the blood-brain barrier [393]. These drugs might reduce brain inflammation in humans that causes progressive neurological damage in Alzheimer’s Disease, Multiple Sclerosis, Parkinson’s Disease, and traumatic brain injury. For example, after a traumatic brain injury, glia cells become hyperactive in the brain and release a cascade of proinflammatory cytokines; the new drugs block glial activation and prevent the flood of proinflammatory cytokines. However, for ME, compelling recent evidence is emerging of a genetic basis for the immune and inflammatory aspects of the disease, further identifying ME as a disorder associated with gene alterations [394].
It should be noted that some theorists believe that ME is not a discrete disease and that it is futile to attempt to rigorously define it. For example, several researchers [19, 24] conclude that ME is a neuroinflammatory illness (resulting in a glutamate/GABA imbalance, oxidative stress and mitochondrial dysfunction), and they suggest that this neuroinflammatory state also underlies a number of psychiatric, neurological and neurodegenerative conditions. In a sense, all of these conditions might involve an abnormal balance between glutamate and GABA, and a wide range of symptom-complexes might be due to glutamate levels being too high in one brain region and too low in another area. Therefore, according to this perspective, ME is not a distinct disease with specific biomarkers. This perspective is not the viewpoint of the authors of the current article.
With the inclusion of such a large number of sources, one criticism of this article is that we have not provided much information of their relative worth. It is of importance to be cautious in reviewing the results of studies in the ME area. Many of the cited studies a cross-sectional, so it is not always clear whether the results reflect biological disturbances associated with the disorder or are concomitants or consequences. Also, a number of studies suffer from other methodological issues such as small sample sizes and not correcting for multiple testing.
In a review of the literature on biomarkers, Fischer et al. [371] found studies have been limited by small sample sizes and differences in methodologies. These authors concluded that neuroanatomical differences (magnetic resonance imaging) were found between some patients with ME and controls, but there is still no unifying explanation for the diversity of neuroanatomical findings. While some individuals with ME exhibit impairments using PET, not all studies have identified neural perfusion abnormalities. Regarding functional neuroscience characteristics. Regarding neurofunctional characteristics, fMRI studies have detected functional differences in neural activity (e.g., heightened activity in several cortical and subcortical brain regions) in some patients. EEG methodologies are currently the only imaging methods which consistently find functional differences in awake-state ME research. Overall, Fischer and colleagues [371] do indicate a number of promising neurocognitive markers that have been subject to mixed results. Regarding neurochemical/endocrine characteristics, findings have included some patients evidencing low basal cortisol levels, increased serotonin function but reduced serotonin receptor binding in some but not all patients. Regarding immunological abnormalities, a number of studies have found an aberrant immune response with a pro-inflammatory cytokine profile, but results have been variable. Studies have also found a shift towards a TH2 response, suggesting a chronic allergic reaction, reduction of NK cell numbers and function, increased active rates of infection (HHV-6). Whereas markers such as elevated pro-inflammatory cytokines (IL1b, IL6, TNF-a) and reduced NK cell cytotoxicity, reduced NK activity, and reduced HRV are all useful, they are far from specific. Still, biomarkers could help characterize patient subgroups in terms of clinical phenotypes and prognosis, and provide justification for a ME case definition. Individually and in combination, they point to systemic low grade inflammation and a system under stress, potentially indicating neuroinflammation and consistent with a neurological core pathology.
In our review article, we have also incorporated a number of references derived from web blogs, conference presentations, manuscripts submitted for publication, and unpublished manuscripts. This is very different from the selection criteria of the recent Institute of Medicine report [11], and we decided to include many peer-reviewed publications that had wide variability in quality (see [395] and [396] for the first author’s views on this case definition). Although there are a number of methods that can be used to evaluate the quality of different types of studies, e.g., observational studies (STROBE), clinical trials (CONSORT), or diagnostic studies (STARD or QUADAS), we decided to provide for a review of promising and heuristic studies that may stimulate further research and conceptual models for understanding ME.
9. CONCLUSION
In summary, having a diagnostic system as illustrated in this article can provide integration of the disparate findings that have been documented with patients having ME. At the present time, many of the findings are based on small samples, may have methodological issues and use varying case definitions. There is currently little agreement on reproducible biomarkers of ME, due in part to ambiguity in how biomarkers are defined and used [371]. Clearly, there is a need to adopt a common ME case definition, and then to use standardized measurement devices to collect both biological and self-report. Larger data sets can also help guide investigators toward identifying cardinal symptoms of ME, and when such data sets are compared with controls, the process of selecting items with good sensitivity and specificity is enhanced. These types of developments, along with sophisticated statistical approaches, could be used to both define ME and specify the ways of measuring it with a high degree of reliability and validity.
ACKNOWLEDGEMENTS
The authors are grateful to Mark Livingstone for providing his thoughtful input.
Footnotes
To meet the ME-ICC criteria, a person must have Post-Exertional Neuroimmune Exhaustion. Within the Neurological Impairment symptom grouping, a patient must have at least one symptom from three of the following four symptom categories (1) neurocognitive impairments (e.g., difficulty processing information, short-term memory loss), (2) pain, (3) sleep disturbance, and (4) neurosensory, perceptual and motor disturbances (e.g. inability to focus vision, sensitivity to light, feeling unsteady on feet). The third category is Immune, Gastro-intestinal and Genitourinary Impairments, and individuals must have at least one symptom from three of the following five symptom categories: (1) flu-like symptoms, (2) susceptibility to viral infections with prolonged recovery periods (3) gastro-intestinal tract symptoms (e.g., nausea, abdominal pain), (4) genitourinary symptoms (e.g., urinary urgency), and (5) sensitivities to food, medications, odors, or chemicals. The final category is Energy Production/Transportation Impairments, and at least one symptom from one of the following four symptom categories must be present: (1) cardiovascular (e.g. orthostatic intolerance), (2) respiratory (e.g. labored breathing), (3) loss of thermostatic stability (e.g. subnormal body temperature), and (4) intolerance of extremes of temperature.
For clarity, in this review article, we use the term ME even though a number of the articles do not use this term to describe their samples.
CONFLICT OF INTEREST
The authors confirm that this article content has no competing interest. Funding was provided by NIAID (grant numbers AI 49720 and AI 055735).
REFERENCES
- 1.Anastasi A., Urbina S. Psychological Testing. Upper Saddle River, NJ: Prentice Hall; 1997. [Google Scholar]
- 2.Kaplan R.M., Saccuzzo D.P. Psychological testing: Principles, applications, and issues. Pacific Grove, CA: Brooks/Cole Publishing Company; 1997. [Google Scholar]
- 3.Johnson C. Puzzle Pieces Coming Together. In: Johnson C., editor. Health Rising: Looking for Answers to Chronic Fatigue Syndrome and Fibromyalgia. Health Rising; 2014. [Google Scholar]
- 4.Lemke E., Wiersma W. Principles of psychological measurement. Chicago: Rand McNally; 1976. [Google Scholar]
- 5.Fukuda K., Straus S.E., Hickie I., Sharpe M.C., Dobbins J.G., Komaroff A., International Chronic Fatigue Syndrome Study Group The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann. Intern. Med. 1994;121(12):953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Carruthers B.M., Jain A.K., De Meirleir K.L., Peterson D.L., Klimas N., Lerner A.M., Bested A.C., Flor-Henry P., Joshi P., Powles A.C., Sherkey J.A., Van de Sande M.I. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical working case definition, diagnostic and treatment protocols. J. Chronic Fatigue Syndr. 2003;11(1):7–115. doi: 10.1300/J092v11n01_02. [DOI] [Google Scholar]
- 7.Carruthers B.M., van de Sande M.I., De Meirleir K.L., Klimas N.G., Broderick G., Mitchell T., Staines D., Powles A.C., Speight N., Vallings R., Bateman L., Baumgarten-Austrheim B., Bell D.S., Carlo-Stella N., Chia J., Darragh A., Jo D., Lewis D., Light A.R., Marshall-Gradisbik S., Mena I., Mikovits J.A., Miwa K., Murovska M., Pall M.L., Stevens S. Myalgic encephalomyelitis: International Consensus Criteria. J. Intern. Med. 2011;270(4):327–338. doi: 10.1111/j.1365-2796.2011.02428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jason L.A., Sunnquist M., Brown A., Evans M., Newton J.L. Are Myalgic Encephalomyelitis and chronic fatigue syndrome different illnesses? A preliminary analysis. J. Health Psychol. 2014. [DOI] [PMC free article] [PubMed]
- 9.Katon W., Russo J. Chronic fatigue syndrome criteria. A critique of the requirement for multiple physical complaints. Arch. Intern. Med. 1992;152(8):1604–1609. doi: 10.1001/archinte.1992.00400200042008. [DOI] [PubMed] [Google Scholar]
- 10.Jason L.A., Brown A., Evans M., Sunnquist M., Newton J.L. Contrasting Chronic Fatigue Syndrome versus Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Fatigue. 2013;1(3):168–183. doi: 10.1080/21641846.2013.774556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute of Medicine . Report Guide for Clinicians. Washington, DC: The National Academies; 2015. Beyond myalgic encephalomyelitis/chronic fatigue syndrome: Redefining an illness. [Google Scholar]
- 12.King C., Jason L.A. Improving the diagnostic criteria and procedures for chronic fatigue syndrome. Biol. Psychol. 2005;68(2):87–106. doi: 10.1016/j.biopsycho.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 13.Brurberg K.G., Fønhus M.S., Larun L., Flottorp S., Malterud K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open. 2014;4(2):e003973. doi: 10.1136/bmjopen-2013-003973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jason L.A., Sorenson M., Evans M., Brown A., Flores S., Sunnquist M., Schafer C. The implications of sensitization and kindling for chronic fatigue syndrome. In: Gotsiridze-Columbus N., editor. Encephalopathies: Symptoms, causes and potential complications. New York: Nova Science; 2013. pp. 73–94. [Google Scholar]
- 15.Brown A.A., Jason L.A. Validating a measure of myalgic encephalomyelitis/chronic fatigue syndrome symptomology. Fatigue. in press. [Google Scholar]
- 16.Brenu E.W., Huth T.K., Hardcastle S.L., Fuller K., Kaur M., Johnston S., Ramos S.B., Staines D.R., Marshall-Gradisnik S.M. Role of adaptive and innate immune cells in chronic fatigue syndrome/myalgic encephalomyelitis. Int. Immunol. 2014;26(4):233–242. doi: 10.1093/intimm/dxt068. [DOI] [PubMed] [Google Scholar]
- 17.Morris G., Berk M., Galecki P., Maes M. The emerging role of autoimmunity in myalgic encephalomyelitis/chronic fatigue syndrome (ME/cfs). Mol. Neurobiol. 2014;49(2):741–756. doi: 10.1007/s12035-013-8553-0. [DOI] [PubMed] [Google Scholar]
- 18.Morris G., Maes M. Oxidative and Nitrosative Stress and Immune-Inflammatory Pathways in Patients with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS). Curr. Neuropharmacol. 2014;12(2):168–185. doi: 10.2174/1570159X11666131120224653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris G., Maes M. Mitochondrial dysfunctions in myalgic encephalomyelitis/chronic fatigue syndrome explained by activated immuno-inflammatory, oxidative and nitrosative stress pathways. Metab. Brain Dis. 2014;29(1):19–36. doi: 10.1007/s11011-013-9435-x. [DOI] [PubMed] [Google Scholar]
- 20.Broderick G., Ben-Hamo R., Vashishtha S., Efroni S., Nathanson L., Barnes Z., Fletcher M.A., Klimas N. Altered immune pathway activity under exercise challenge in Gulf War Illness: an exploratory analysis. Brain Behav. Immun. 2013;28:159–169. doi: 10.1016/j.bbi.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Klimas N.G., Broderick G., Fletcher M.A. Biomarkers for chronic fatigue. Brain Behav. Immun. 2012;26(8):1202–1210. doi: 10.1016/j.bbi.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Den Eede F., Moorkens G. Neuroendocrine correlates of childhood trauma in CFS. Nat. Rev. Endocrinol. 2012;8(8):502. doi: 10.1038/nrendo.2011.153-c1. [DOI] [PubMed] [Google Scholar]
- 23.Ickmans K., Meeus M., De Kooning M., Lambrecht L., Pattyn N., Nijs J. Can recovery of peripheral muscle function predict cognitive task performance in chronic fatigue syndrome with and without fibromyalgia? Phys. Ther. 2014;94(4):511–522. doi: 10.2522/ptj.20130367. [DOI] [PubMed] [Google Scholar]
- 24.Nakatomi Y., Mizuno K., Ishii R., Wada Y., Tanaka M., Tazawa S., Onoe K., Fukuda S., Kawabe J., Takahashi K., Kataoka Y., Shiomi S., Yamkaguti K., Inaba M., Kuratsune H., Watanabe Y. Neuroinflammation in patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: An 11C-(R)-PK11195 PET study. J. Nucl. Med. . 2014;55(6):945–950. doi: 10.2967/jnumed.113.131045. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds G.K., Lewis D.P., Richardson A.M., Lidbury B.A. Comorbidity of postural orthostatic tachycardia syndrome and chronic fatigue syndrome in an Australian cohort. J. Intern. Med. 2014;275(4):409–417. doi: 10.1111/joim.12161. [DOI] [PubMed] [Google Scholar]
- 26.Van Cauwenbergh D., Nijs J., Kos D., Van Weijnen L., Struyf F., Meeus M. Malfunctioning of the autonomic nervous system in patients with chronic fatigue syndrome: a systematic literature review. Eur. J. Clin. Invest. 2014;44(5):516–526. doi: 10.1111/eci.12256. [DOI] [PubMed] [Google Scholar]
- 27.Yasui M., Yoshimura T., Takeuchi S., Tokizane K., Tsuda M., Inoue K., Kiyama H. A chronic fatigue syndrome model demonstrates mechanical allodynia and muscular hyperalgesia via spinal microglial activation. Glia. 2014;62(9):1407–1417. doi: 10.1002/glia.22687. [DOI] [PubMed] [Google Scholar]
- 28.Nijs J., Van Oosterwijck J., Meeus M., Lambrecht L., Metzger K., Frémont M., Paul L. Unravelling the nature of postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: the role of elastase, complement C4a and interleukin-1beta. J. Intern. Med. 2010;267(4):418–435. doi: 10.1111/j.1365-2796.2009.02178.x. [DOI] [PubMed] [Google Scholar]
- 29.Nijs J., van Eupen I., Vandecauter J., Augustinus E., Bleyen G., Moorkens G., Meeus M. Can pacing self-management alter physical behavior and symptom severity in chronic fatigue syndrome? A case series. J. Rehabil. Res. Dev. 2009;46(7):985–996. doi: 10.1682/JRRD.2009.01.0007. [DOI] [PubMed] [Google Scholar]
- 30.VanNess J.M., Stevens S.R., Bateman L., Stiles T.L., Snell C.R. Postexertional malaise in women with chronic fatigue syndrome. J. Womens Health (Larchmt) 2010;19(2):239–244. doi: 10.1089/jwh.2009.1507. [DOI] [PubMed] [Google Scholar]
- 31.Jason L.A., Damrongvachiraphan D., Hunnell J., Bartgis L., Brown A. Myalgic Encephalomyelitis: Case definitions. Autonomic control Physiol. State Function. 2012;1:1–14. [Google Scholar]
- 32.LaManca J.J., Sisto S.A., DeLuca J., Johnson S.K., Lange G., Pareja J., Cook S., Natelson B.H. Influence of exhaustive treadmill exercise on cognitive functioning in chronic fatigue syndrome. Am. J. Med. 1998;105(3A):59S–65S. doi: 10.1016/S0002-9343(98)00171-5. [DOI] [PubMed] [Google Scholar]
- 33.Light A.R., White A.T., Hughen R.W., Light K.C. Moderate exercise increases expression for sensory adrenergic and immune genes in chronic fatigue syndrome patients but not in normal subjects. 2009. [DOI] [PMC free article] [PubMed]
- 34.Light A.R., Bateman L., Jo D., Hughen R.W., Vanhaitsma T.A., White A.T., Light K.C. Gene expression alterations at baseline and following moderate exercise in patients with Chronic Fatigue Syndrome and Fibromyalgia Syndrome. J. Intern. Med. 2012;271(1):64–81. doi: 10.1111/j.1365-2796.2011.02405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vanness J.M., Snell C.R., Strayer D.R., Dempsey L., IV, Stevens S.R. Subclassifying chronic fatigue syndrome through exercise testing. Med. Sci. Sports Exerc. 2003;35(6):908–913. doi: 10.1249/01.MSS.0000069510.58763.E8. [DOI] [PubMed] [Google Scholar]
- 36.Jammes Y., Steinberg J.G., Mambrini O., Brégeon F., Delliaux S. Chronic fatigue syndrome: assessment of increased oxidative stress and altered muscle excitability in response to incremental exercise. J. Intern. Med. 2005;257(3):299–310. doi: 10.1111/j.1365-2796.2005.01452.x. [DOI] [PubMed] [Google Scholar]
- 37.VanNess M., Snell C.R., Stevens S.R. Diminished cardiopulmonary capacity during post-exertional malaise. J. Chronic Fatigue Syndr. 2007;14(2):77–85. doi: 10.1300/J092v14n02_07. [DOI] [Google Scholar]
- 38.He J., Hollingsworth K.G., Newton J.L., Blamire A.M. Cerebral vascular control is associated with skeletal muscle pH in chronic fatigue syndrome patients both at rest and during dynamic stimulation. Neuroimage Clin. 2013;2:168–173. doi: 10.1016/j.nicl.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hyde B.M. The nightingale definition of myalgic encephalomyelitis (M.E.). [Online] 2007. The Nightingale Research Foundation. http://www.hfme.org/Other/DefinitionBooklet_Sept_2011.pdf [Accessed on: 07/07/2014]. 2007.
- 40.Newton D.J., Kennedy G., Chan K.K., Lang C.C., Belch J.J., Khan F. Large and small artery endothelial dysfunction in chronic fatigue syndrome. Int. J. Cardiol. 2012;154(3):335–336. doi: 10.1016/j.ijcard.2011.10.030. [DOI] [PubMed] [Google Scholar]
- 41.Spence V.A., Khan F., Belch J.J. Enhanced sensitivity of the peripheral cholinergic vascular response in patients with chronic fatigue syndrome. Am. J. Med. 2000;108(9):736–739. doi: 10.1016/S0002-9343(00)00407-1. [DOI] [PubMed] [Google Scholar]
- 42.Spence V.A., Khan F., Kennedy G., Abbot N.C., Belch J.J. Acetylcholine mediated vasodilatation in the microcirculation of patients with chronic fatigue syndrome. 2004. [DOI] [PubMed]
- 43.Dowsett E.G., Ramsay A.M., McCartney R.A., Bell E.J. Myalgic encephalomyelitis--a persistent enteroviral infection? Postgrad. Med. J. . 1990;66(777):526–530. doi: 10.1136/pgmj.66.777.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Myhill S., Booth N.E., McLaren-Howard J. Chronic fatigue syndrome and mitochondrial dysfunction. Int. J. Clin. Exp. Med. 2009;2(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- 45.Twisk F.N., Maes M. A review on cognitive behavioral therapy (CBT) and graded exercise therapy (GET): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients with ME/CFS. Neuroendocrinol. Lett. 2009;30:284–299. [PubMed] [Google Scholar]
- 46.Maes M., Twisk F.N., Johnson C. Myalgic Encephalomyelitis (ME), Chronic Fatigue Syndrome (CFS), and Chronic Fatigue (CF) are distinguished accurately: Results of supervised learning techniques applied on clinical and inflammatory data. Psychiatry Res. . 2012;200(2-3):754–760. doi: 10.1016/j.psychres.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 47.Chaudhuri A., Behan P.O., Behan W.M. Ion channel function and chronic fatigue syndrome.; International Conference on Fatigue Science; Karuizawa, Japan. 2005. [Google Scholar]
- 48.Chaudhuri A., Watson W.S., Pearn J., Behan P.O. The symptoms of chronic fatigue syndrome are related to abnormal ion channel function. Med. Hypotheses. 2000;54(1):59–63. doi: 10.1054/mehy.1998.0822. [DOI] [PubMed] [Google Scholar]
- 49.Gow J.W., Cannon C., Behan W.M., Herzyk P., Keir S., Riboldi-Tunnicliffe G. Whole-genome (33,000 genes) affymetrix DNA microarray analysis of gene expression in Chronic Fatigue Syndrome.; Inter. Conf. Fatigue Sci.; Karuizawa, Japan. 2005. [Google Scholar]
- 50.Kullmann D.M., Waxman S.G. Neurological channelopathies: new insights into disease mechanisms and ion channel function. J. Physiol. 2010;588(Pt 11):1823–1827. doi: 10.1113/jphysiol.2010.190652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cannon S.C. Voltage-sensor mutations in channelopathies of skeletal muscle. J. Physiol. 2010;588(Pt 11):1887–1895. doi: 10.1113/jphysiol.2010.186874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eymard B., Stojkovic T., Sternberg D., Richard P., Nicole S., Fournier E., Béhin A., Laforêt P., Servais L., Romero N., Fardeau M., Hantaï D., Membres du réseau national Syndromes Myasthéniques Congénitaux [Congenital myasthenic syndromes: difficulties in the diagnosis, course and prognosis, and therapy--The French National Congenital Myasthenic Syndrome Network experience]. Rev. Neurol. (Paris) 2013;169(Suppl. 1):S45–S55. doi: 10.1016/S0035-3787(13)70060-2. [Congenital myasthenic syndromes: difficulties in the diagnosis, course and prognosis, and therapy--The French National Congenital Myasthenic Syndrome Network experience]. [DOI] [PubMed] [Google Scholar]
- 53.Chaudhuri A., Behan P.O. Fatigue in neurological disorders. Lancet. 2004;363(9413):978–988. doi: 10.1016/S0140-6736(04)15794-2. [DOI] [PubMed] [Google Scholar]
- 54.Chaudhuri A., Condon B.R., Gow J.W., Brennan D., Hadley D.M. Proton magnetic resonance spectroscopy of basal ganglia in chronic fatigue syndrome. Neuroreport. 2003;14(2):225–228. doi: 10.1097/00001756-200302100-00013. [DOI] [PubMed] [Google Scholar]
- 55.Whiteside A., Hansen S., Chaudhuri A. Exercise lowers pain threshold in chronic fatigue syndrome. Pain. 2004;109(3):497–499. doi: 10.1016/j.pain.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 56.Kullmann D.M. Inherited channelopathies of the CNS: Lessons for clinical neurology. In: Waxman S., editor. From Neuroscience to Neurology. Elsevier; 2005. pp. 293–302. [DOI] [Google Scholar]
- 57.Buzsaki G. Rhythms of the Brain. Oxford University Press; 2006. [DOI] [Google Scholar]
- 58.Snell C.R., Vanness J.M., Strayer D.R., Stevens S.R. Exercise capacity and immune function in male and female patients with chronic fatigue syndrome (CFS). In Vivo. 2005;19(2):387–390. [PubMed] [Google Scholar]
- 59.Nijs J.C., McGregor N.R., de Becker P., Verhas M., Engelbienne P. Monitoring a hypothetical channelopathy in Chronic Fatigue Syndrome: Preliminary observations. J. Chronic Fatigue Syndr. 2003;11(1):117–133. doi: 10.1300/J092v11n01_03. [DOI] [Google Scholar]
- 60.Jason L.A., Sorenson M., Porter N., Belkairous N. An Etiological Model for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Neurosci. Med. 2011;2(1):14–27. doi: 10.4236/nm.2011.21003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cardamone L., Salzberg M.R., Koe A.S., Ozturk E., O’Brien T.J., Jones N.C. Chronic antidepressant treatment accelerates kindling epileptogenesis in rats. Neurobiol. Dis. 2014;63:194–200. doi: 10.1016/j.nbd.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 62.Goddard G.V. Development of epileptic seizures through brain stimulation at low intensity. Nature. 1967;214(5092):1020–1021. doi: 10.1038/2141020a0. [DOI] [PubMed] [Google Scholar]
- 63.Jones N.C., Lee H.E., Yang M., Rees S.M., Morris M.J., O’Brien T.J., Salzberg M.R. Repeatedly stressed rats have enhanced vulnerability to amygdala kindling epileptogenesis. Psychoneuroendocrinology. 2013;38(2):263–270. doi: 10.1016/j.psyneuen.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 64.Post R.M. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. 2007. [DOI] [PubMed]
- 65.Mazarati A., Shin D., Auvin S., Caplan R., Sankar R. Kindling epileptogenesis in immature rats leads to persistent depressive behavior. Epilepsy Behav. 2007;10(3):377–383. doi: 10.1016/j.yebeh.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Loscher W., Ebert U. The role of the piriform cortex in kindling. 1996. [DOI] [PubMed]
- 67.Cooper M.S., Clark V.P. Neuroinflammation, neuroautoimmunity, and the co-morbidities of complex regional pain syndrome. J. Neuroimmune Pharmacol. 2013;8(3):452–469. doi: 10.1007/s11481-012-9392-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sorrells S.F., Caso J.R., Munhoz C.D. The stressed CNS: When glucocorticoids aggravate inflammation. Neuron . 2009;64(1):33–39. doi: 10.1016/j.neuron.2009.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arnett S.V., Alleva L.M., Korossy-Horwood R., Clark I.A. Chronic fatigue syndrome: A neuroimmunological model. 2011. [DOI] [PubMed]
- 70.Jason L., Benton M., Torres-Harding S., Muldowney K. The impact of energy modulation on physical functioning and fatigue severity among patients with ME/CFS. Patient Educ. Couns. 2009;77(2):237–241. doi: 10.1016/j.pec.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jason L.A., Brown M., Brown A., Evans M., Flores S., Grant-Holler E., Sunnquist M. Energy Conservation/Envelope Theory Interventions to Help Patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Fatigue. 2013;1(1-2):27–42. doi: 10.1080/21641846.2012.733602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Johnson C. Light on ME/CFS I: Bad reception: A key to ME uncovered? The Light gene expression studies. http://phoenixrising. me/archives/5790 (Accessed May 8, 2015).
- 73.Jason L.A., King C.P., Richman J.A., Taylor R.R., Torres S.R. US case definition of chronic fatigue syndrome: Diagnostic and theoretical issues. J. Chronic Fatigue Syndr. 1999;5:3–33. doi: 10.1300/J092v05n03_02. [DOI] [Google Scholar]
- 74.Meeus M., Roussel N.A., Truijen S., Nijs J. Reduced pressure pain thresholds in response to exercise in chronic fatigue syndrome but not in chronic low back pain: an experimental study. J. Rehabil. Med. 2010;42(9):884–890. doi: 10.2340/16501977-0595. [DOI] [PubMed] [Google Scholar]
- 75.Neu D., Mairesse O., Verbanck P., Linkowski P., Le Bon O. Non-REM sleep EEG power distribution in fatigue and sleepiness. 2014. [DOI] [PubMed]
- 76.American Medical Association American Medical Association. Guides to the evaluation of permanent impairment: Clarifications and corrections. 2008. 2008.
- 77.Snell C.R., Stevens S.R. E., D.T.; VanNess, J.M. Discriminative Validity of metabolic and workload measurements to identify individuals with chronic fatigue syndrome. Phys. Ther. 2013;93(11):1484–1492. doi: 10.2522/ptj.20110368. [DOI] [PubMed] [Google Scholar]
- 78.Siemionow V., Fang Y., Calabrese L., Sahgal V., Yue G.H. Altered central nervous system signal during motor performance in chronic fatigue syndrome. Clin. Neurophysiol. 2004;115(10):2372–2381. doi: 10.1016/j.clinph.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 79.Patrick Neary J., Roberts A.D., Leavins N., Harrison M.F., Croll J.C., Sexsmith J.R. Prefrontal cortex oxygenation during incremental exercise in chronic fatigue syndrome. Clin. Physiol. Funct. Imaging. 2008;28(6):364–372. doi: 10.1111/j.1475-097X.2008.00822.x. [DOI] [PubMed] [Google Scholar]
- 80.Nijs J., Almond F., De Becker P., Truijen S., Paul L. Can exercise limits prevent post-exertional malaise in chronic fatigue syndrome? An uncontrolled clinical trial. Clin. Rehabil. 2008;22(5):426–435. doi: 10.1177/0269215507084410. [DOI] [PubMed] [Google Scholar]
- 81.White A.T., Light A.R., Hughen R.W., Bateman L., Martins T.B., Hill H.R., Light K.C. Severity of symptom flare after moderate exercise is linked to cytokine activity in chronic fatigue syndrome. Psychophysiology. 2010;47(4):615–624. doi: 10.1111/j.1469-8986.2010.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Van Oosterwijck J., Nijs J., Meeus M., Lefever I., Huybrechts L., Lambrecht L., Paul L. Pain inhibition and postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: an experimental study. J. Intern. Med. 2010;268(3):265–278. doi: 10.1111/j.1365-2796.2010.02228.x. [DOI] [PubMed] [Google Scholar]
- 83.Vermeulen R.C. Vermeulen, van Eck, I.W.G. Decreased oxygen extraction during cardiopulmonary exercise test in patients with chronic fatigue syndrome. J. Transl. Med. 2014;12(1) doi: 10.1186/1479-5876-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lengert N., Drossel B. In silico analysis of exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome. Biophys.Chem. . 2015;202:21–31. doi: 10.1016/j.bpc.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 85.Komaroff A.L. Clinical presentation of chronic fatigue syndrome; Chronic Fatigue Syndrome. Ciba Foundation Symposium; Hoboken, NJ. 1993. pp. 43–61. [DOI] [PubMed] [Google Scholar]
- 86.Komaroff A.L., Fagioli L.R., Doolittle T.H., Gandek B., Gleit M.A., Guerriero R.T., Kornish R.J., II, Ware N.C., Ware J.E., Jr, Bates D.W. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. 1996. [DOI] [PubMed]
- 87.Jason L.A., Evans M., Porter N., Brown A., Brown M., Hunnell J., Anderson V., Lerch A., DeMeirleir K., Friedberg F. The development of a revised Canadian myalgic encephalomyelitis-chronic fatigue syndrome case definition. Am. J. Biochem. Biotechnol. 2010;6(2):120–135. doi: 10.3844/ajbbsp.2010.120.135. [DOI] [Google Scholar]
- 88.Michiels V., Cluydts R. Neuropsychological functioning in chronic fatigue syndrome: a review. Acta Psychiatr. Scand. 2001;103(2):84–93. doi: 10.1034/j.1600-0447.2001.00017.x. [DOI] [PubMed] [Google Scholar]
- 89.Cockshell S.J., Mathias J.L. Cognitive functioning in chronic fatigue syndrome: a meta-analysis. Psychol. Med. 2010;40(8):1253–1267. doi: 10.1017/S0033291709992054. [DOI] [PubMed] [Google Scholar]
- 90.Cockshell S.J., Mathias J.L. Test effort in persons with Chronic Fatigue Syndrome when assessed using the Validity Indicator Profile. J. Clin. Exp. Neuropsychol. 2012;34(7):679–687. doi: 10.1080/13803395.2012.668176. [DOI] [PubMed] [Google Scholar]
- 91.Cockshell S.J., Mathias J.L. Cognitive functioning in people with chronic fatigue syndrome: a comparison between subjective and objective measures. Neuropsychology. 2014;28(3):394–405. doi: 10.1037/neu0000025. [DOI] [PubMed] [Google Scholar]
- 92.DeLuca J., Johnson S.K., Natelson B.H. Information processing efficiency in chronic fatigue syndrome and multiple sclerosis. 1993. [DOI] [PubMed]
- 93.Marshall P.S., Forstot M., Callies A., Peterson P.K., Schenck C.H. Cognitive slowing and working memory difficulties in chronic fatigue syndrome. Psychosom. Med. 1997;59(1):58–66. doi: 10.1097/00006842-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 94.Zinn M.A., Zinn M.L., Norris J.L., Valencia I., Montoya J.G., Maldonado J.R. Cortical hypoactivation during resting EEG suggests central nervous system pathology in patients with Chronic Fatigue Syndrome.; Symposium conducted at the meeting of IACFS/ME 2014 Biennial Conference; San Francisco, CA, USA. 2014. [Google Scholar]
- 95.Zinn M.L., Zinn M.A., Norris J.L., Valencia I., Montoya J.G., Maldonado J.R. EEG Peak Alpha Frequency Correlates in Chronic Fatigue Syndrome: A Case-Control Observational Study.; IACFS/ME 2014 Biennial Conference; March 2014; San Francisco, CA, USA. 2014. [Google Scholar]
- 96.Claypoole K.H., Noonan C., Mahurin R.K., Goldberg J., Erickson T., Buchwald D. A twin study of cognitive function in chronic fatigue syndrome: the effects of sudden illness onset. Neuropsychology. 2007;21(4):507–513. doi: 10.1037/0894-4105.21.4.507. [DOI] [PubMed] [Google Scholar]
- 97.Deluca J., Johnson S.K., Natelson B.H. Neuropsychiatric status of patients with chronic fatigue syndrome: an overview. Toxicol. Ind. Health. 1994;10(4-5):513–522. [PubMed] [Google Scholar]
- 98.Thomas M., Smith A. An investigation into the cognitive deficits associated with chronic fatigue syndrome. Open Neurol. J. 2009;3:13–23. doi: 10.2174/1874205X00903010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Majer M., Welberg L.A., Capuron L., Miller A.H., Pagnoni G., Reeves W.C. Neuropsychological performance in persons with chronic fatigue syndrome: results from a population-based study. Psychosom. Med. 2008;70(7):829–836. doi: 10.1097/PSY.0b013e31817b9793. [DOI] [PubMed] [Google Scholar]
- 100.Colby J. Special problems of children with myalgic encephalomyelitis/chronic fatigue syndrome and the enteroviral link. J. Clin. Pathol. 2007;60(2):125–128. doi: 10.1136/jcp.2006.042606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Haywood K.L., Collin S.M., Crawley E. Assessing severity of illness and outcomes of treatment in children with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME): a systematic review of patient-reported outcome measures (PROMs). Child Care Health Dev. 2014;40(6):806–824. doi: 10.1111/cch.12135. [DOI] [PubMed] [Google Scholar]
- 102.Care N.C. National Institute for Health and Clinical Excellence: Guidance. In: Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (or Encephalopathy): Diagnosis and Management of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (or Encephalopathy) in Adults and Children; London: Royal College of General Practitioners:; 2007. [Google Scholar]
- 103.Nieoullon A. Dopamine and the regulation of cognition and attention. Prog. Neurobiol. 2002;67(1):53–83. doi: 10.1016/S0301-0082(02)00011-4. [DOI] [PubMed] [Google Scholar]
- 104.Hopkins R.O. The brain after critical illness: effect of illness and aging on cognitive function. Crit. Care. 2013;17(1):116. doi: 10.1186/cc11913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hopkins R.O., Jackson J.C. Long-term neurocognitive function after critical illness. Chest. 2006;130(3):869–878. doi: 10.1378/chest.130.3.869. [DOI] [PubMed] [Google Scholar]
- 106.Hopkins R.O., Jackson J.C. Neuroimaging after critical illness: implications for neurorehabilitation outcome. NeuroRehabilitation. 2012;31(3):311–318. doi: 10.3233/NRE-2012-0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Piraino B., Vollmer-Conna U., Lloyd A.R. Genetic associations of fatigue and other symptom domains of the acute sickness response to infection. Brain Behav. Immun. 2012;26(4):552–558. doi: 10.1016/j.bbi.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pizzagalli D.A., Oakes T.R., Fox A.S., Chung M.K., Larson C.L., Abercrombie H.C., Schaefer S.M., Benca R.M., Davidson R.J. Functional but not structural subgenual prefrontal cortex abnormalities in melancholia. Mol. Psychiatry. 2004;9(4):325–, 393-405. doi: 10.1038/sj.mp.4001501. [DOI] [PubMed] [Google Scholar]
- 109.Kuratsune H., Nakatomi Y., Mizuno K., Watanabe Y. Neuroinflammation in patients with ME: A positron emission topography study.; 11th Biennial International Association of CFS/ME Conference; San Francisco, CA. 2014. [Google Scholar]
- 110.Fuku M., Hossain S.M., Noda M., Katafuchi T. Induction of interleukin-1β by activated microglia is a prerequisite for immunologically induced fatigue. Eur. J. Neurosci. 2014 doi: 10.1111/ejn.12668. [DOI] [PubMed] [Google Scholar]
- 111.Plassman B.L., Langa K.M., Fisher G.G., Heeringa S.G., Weir D.R., Ofstedal M.B., Burke J.R., Hurd M.D., Potter G.G., Rodgers W.L., Steffens D.C., McArdle J.J., Willis R.J., Wallace R.B. Prevalence of cognitive impairment without dementia in the United States. Ann. Intern. Med. 2008;148(6):427–434. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Plassman B.L., Langa K.M., McCammon R.J., Fisher G.G., Potter G.G., Burke J.R., Steffens D.C., Foster N.L., Giordani B., Unverzagt F.W., Welsh-Bohmer K.A., Heeringa S.G., Weir D.R., Wallace R.B. Incidence of dementia and cognitive impairment, not dementia in the United States. Ann. Neurol. 2011;70(3):418–426. doi: 10.1002/ana.22362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kuratsune H., Watanabe Y. Chronic fatigue syndrome. In: Watanabe Y., Evengard B., Natelson B.H., Jason L.A., Kuratusune H., editors. Fatigue Science for Human Health. Tokyo: Springer; 2007. pp. 67–88. [Google Scholar]
- 114.Natelson B.H., Weaver S.A., Tseng C.L., Ottenweller J.E. Spinal fluid abnormalities in patients with chronic fatigue syndrome. 2005. [DOI] [PMC free article] [PubMed]
- 115.Sorenson M., Porter N., Jason L.A., Lerch A., Matthews H. IL-8 increased in patients with CFS. Unplished manuscript. Chicago, Illinois: Chronic Fatigue Syndrome Project; 2011. [Google Scholar]
- 116.Baraniuk J.N., Casado B., Maibach H., Clauw D.J., Pannell L.K., Hess S S. A Chronic Fatigue Syndrome - related proteome in human cerebrospinal fluid. BMC Neurol. 2005;5:22. doi: 10.1186/1471-2377-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Richards R.S., Roberts T.K., Dunstan R.H., McGregor N.R., Butt H.L. Free radicals in chronic fatigue syndrome: Cause or effect? Redox. Rep. 2000;5(2-3):146–147. doi: 10.1179/135100000101535519. [DOI] [PubMed] [Google Scholar]
- 118.Camps J. Adv. Exp. Med. Biol. Vol. 824. Reus, Spain: Springer; 2014. Oxidative Stress and Inflammation in Non-communicable Diseases - Molecular Mechanisms and Perspectives in Therapeutics. [DOI] [Google Scholar]
- 119.de Lange F.P., Kalkman J.S., Bleijenberg G., Hagoort P., van der Meer J.W., Toni I. Gray matter volume reduction in the chronic fatigue syndrome. Neuroimage. 2005;26(3):777–781. doi: 10.1016/j.neuroimage.2005.02.037. [DOI] [PubMed] [Google Scholar]
- 120.Clark I.A., Alleva L.M., Vissel B. The roles of TNF in brain dysfunction and disease. Pharmacol. Ther. 2010;128(3):519–548. doi: 10.1016/j.pharmthera.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 121.Kennedy G., Spence V.A., McLaren M., Hill A., Underwood C., Belch J. Oxidative stress levels are raised in chronic fatigue syndrome and are associated with clinical symptoms. 2005. [DOI] [PubMed]
- 122.Robinson M., Gray S.R., Watson M.S., Kennedy G., Hill A., Belch J.J. Plasma IL-6, its soluble receptors and F-isoprostanes at rest and during exercise in chronic fatigue syndrome. Scand. J. Med. Sci. Sports. 2009;13:1–9. doi: 10.1177/0363546508322885. [DOI] [PubMed] [Google Scholar]
- 123.Meeus M., Nijs J. Central sensitization: a biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin. Rheumatol. 2007;26(4):465–473. doi: 10.1007/s10067-006-0433-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pall M.L., Satterlee J.D. Elevated nitric oxide/peroxynitrite mechanism for the common etiology of multiple chemical sensitivity, chronic fatigue syndrome, and posttraumatic stress disorder. Ann. N. Y. Acad. Sci. 2001;933:323–329. doi: 10.1111/j.1749-6632.2001.tb05836.x. [DOI] [PubMed] [Google Scholar]
- 125.Buchwald D., Cheney P.R., Peterson D.L., Henry B., Wormsley S.B., Geiger A., Ablashi D.V., Salahuddin S.Z., Saxinger C., Biddle R., et al. A chronic illness characterized by fatigue, neurologic and immunologic disorders, and active human herpesvirus type 6 infection. Ann. Intern. Med. 1992;116(2):103–113. doi: 10.7326/0003-4819-116-2-103. [DOI] [PubMed] [Google Scholar]
- 126.Nicolson G.L. Mitochondrial dysfunction and chronic disease: treatment with natural supplements. Altern. Ther. Health Med. 2014;20(Suppl. 1):18–25. [PubMed] [Google Scholar]
- 127.Kindlon T. Change in grey matter volume cannot be assumed to be due to cognitive behavioural therapy. 2009. [DOI] [PubMed]
- 128.Morris G., Maes M. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. BMC Med. 2013;11:205. doi: 10.1186/1741-7015-11-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rayhan R.U., Stevens B.W., Timbol C.R., Adewuyi O., Walitt B., VanMeter J.W., Baraniuk J.N. Increased brain white matter axial diffusivity associated with fatigue, pain and hyperalgesia in Gulf War illness. PLoS One. 2013;8(3):e58493. doi: 10.1371/journal.pone.0058493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Puri B.K., Jakeman P.M., Agour M., Gunatilake K.D., Fernando K.A., Gurusinghe A.I., Treasaden I.H., Waldman A.D., Gishen P. Regional grey and white matter volumetric changes in myalgic encephalomyelitis (chronic fatigue syndrome): a voxel-based morphometry 3 T MRI study. Br. J. Radiol. 2012;85(1015):e270–e273. doi: 10.1259/bjr/93889091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lange G., DeLuca J., Maldjian J.A., Lee H., Tiersky L.A., Natelson B.H. Brain MRI abnormalities exist in a subset of patients with chronic fatigue syndrome. J. Neurol. Sci. 1999;171(1):3–7. doi: 10.1016/S0022-510X(99)00243-9. [DOI] [PubMed] [Google Scholar]
- 132.Zeineh M.M., Kang J., Atlas S.W., Raman M.M., Reiss A.L., Norris J.L., Valencia I., Montoya J.G. Right arcuate fasciculus abnormality in chronic fatigue syndrome. Radiology. 2015;274(2):517–526. doi: 10.1148/radiol.14141079. [DOI] [PubMed] [Google Scholar]
- 133.Ichise M., Salit I.E., Abbey S.E., Chung D.G., Gray B., Kirsh J.C., Freedman M. Assessment of regional cerebral perfusion by 99Tcm-HMPAO SPECT in chronic fatigue syndrome. Nucl. Med. Commun. 1992;13(10):767–772. doi: 10.1097/00006231-199213100-00011. [DOI] [PubMed] [Google Scholar]
- 134.Natelson B.H., Cohen J.M., Brassloff I., Lee H.J. A controlled study of brain magnetic resonance imaging in patients with the chronic fatigue syndrome. J. Neurol. Sci. 1993;120(2):213–217. doi: 10.1016/0022-510X(93)90276-5. [DOI] [PubMed] [Google Scholar]
- 135.Schwartz R.B., Garada B.M., Komaroff A.L., Tice H.M. ; Schwartz R.B., Garada B.M., Komaroff A.L., Tice H.M., Gleit M., Jolesz F.A., Holman B.L. Detection of intracranial abnormalities in patients with chronic fatigue syndrome: comparison of MR imaging and SPECT. AJR Am. J. Roentgenol. 1994;162(4):935–941. doi: 10.2214/ajr.162.4.8141020. [DOI] [PubMed] [Google Scholar]
- 136.Cope H., Pernet A., Kendall B., David A. Cognitive functioning and magnetic resonance imaging in chronic fatigue. 1995. [DOI] [PubMed]
- 137.Costa D.C., Tannock C., Brostoff J. Brainstem perfusion is impaired in chronic fatigue syndrome. QJM. 1995;88(11):767–773. [PubMed] [Google Scholar]
- 138.Greco A., Tannock C., Brostoff J., Costa D.C. Brain MR in chronic fatigue syndrome. AJNR Am. J. Neuroradiol. 1997;18(7):1265–1269. [PMC free article] [PubMed] [Google Scholar]
- 139.Tirelli U., Chierichetti F., Tavio M., Simonelli C., Bianchin G., Zanco P., Ferlin G. Brain positron emission tomography (PET) in chronic fatigue syndrome: Preliminary data. Am. J. Med. . 1998;105(3A):54S–58S. doi: 10.1016/S0002-9343(98)00179-X. [DOI] [PubMed] [Google Scholar]
- 140.Brooks J.C., Roberts N., Whitehouse G., Majeed T. Proton magnetic resonance spectroscopy and morphometry of the hippocampus in chronic fatigue syndrome. Br. J. Radiol. 2000;73(875):1206–1208. doi: 10.1259/bjr.73.875.11144799. [DOI] [PubMed] [Google Scholar]
- 141.Lange G., Holodny A.I., DeLuca J., Lee H.J., Yan X.H., Steffener J., Natelson B.H. Quantitative assessment of cerebral ventricular volumes in chronic fatigue syndrome. Appl. Neuropsychol. 2001;8(1):23–30. doi: 10.1207/S15324826AN0801_4. [DOI] [PubMed] [Google Scholar]
- 142.Lewis D.H., Mayberg H.S., Fischer M.E., Goldberg J., Ashton S., Graham M.M., Buchwald D. Monozygotic twins discordant for chronic fatigue syndrome: regional cerebral blood flow SPECT. Radiology. 2001;219(3):766–773. doi: 10.1148/radiology.219.3.r01jn18766. [DOI] [PubMed] [Google Scholar]
- 143.Kuratsune H., Yamaguti K., Lindh G., Evengård B., Hagberg G., Matsumura K., Iwase M., Onoe H., Takahashi M., Machii T., Kanakura Y., Kitani T., Långström B., Watanabe Y. Brain regions involved in fatigue sensation: reduced acetylcarnitine uptake into the brain. Neuroimage. 2002;17(3):1256–1265. doi: 10.1006/nimg.2002.1260. [DOI] [PubMed] [Google Scholar]
- 144.Schmaling K.B., Lewis D.H., Fiedelak J.I., Mahurin R., Buchwald D.S. Single-photon emission computerized tomography and neurocognitive function in patients with chronic fatigue syndrome. Psychosom. Med. 2003;65(1):129–136. doi: 10.1097/01.PSY.0000038942.33335.9B. [DOI] [PubMed] [Google Scholar]
- 145.Siessmeier T., Nix W.A., Hardt J., Schreckenberger M., Egle U.T., Bartenstein P. Observer independent analysis of cerebral glucose metabolism in patients with chronic fatigue syndrome. J. Neurol. Neurosurg. Psychiatry. 2003;74(7):922–928. doi: 10.1136/jnnp.74.7.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.de Lange F.P., Kalkman J.S., Bleijenberg G., Hagoort P., van der Werf S.P., van der Meer J.W., Toni I. Neural correlates of the chronic fatigue syndrome--an fMRI study. Brain. 2004;127(Pt 9):1948–1957. doi: 10.1093/brain/awh225. [DOI] [PubMed] [Google Scholar]
- 147.Okada T., Tanaka M., Kuratsune H., Watanabe Y., Sadato N. Mechanisms underlying fatigue: a voxel-based morphometric study of chronic fatigue syndrome. BMC Neurol. 2004;4(1):14. doi: 10.1186/1471-2377-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Yamamoto S., Ouchi Y., Onoe H., Yoshikawa E., Tsukada H., Takahashi H., Iwase M., Yamaguti K., Kuratsune H., Watanabe Y. Reduction of serotonin transporters of patients with chronic fatigue syndrome. Neuroreport. 2004;15(17):2571–2574. doi: 10.1097/00001756-200412030-00002. [DOI] [PubMed] [Google Scholar]
- 149.Cleare A.J., Messa C., Rabiner E.A., Grasby P.M. Brain 5- HT1A receptor binding in chronic fatigue syndrome measured using positron emission tomography and [11C] WAY-100635. Biol Psychiatry, 2005;57(3):239–246. doi: 10.1016/j.biopsych.2004.10.031. [DOI] [PubMed] [Google Scholar]
- 150.de Lange F.P., Kalkman J.S., Bleijenberg G., Hagoort P., van der Meer J.W., Toni I. Gray matter volume reduction in the chronic fatigue syndrome. Neuroimage. 2005;26(3):777–781. doi: 10.1016/j.neuroimage.2005.02.037. [DOI] [PubMed] [Google Scholar]
- 151.Lange G., Steffener J., Cook D.B., Bly B.M., Christodoulou C., Liu W.C., Deluca J., Natelson B.H. Objective evidence of cognitive complaints in Chronic Fatigue Syndrome: a BOLD fMRI study of verbal working memory. Neuroimage. 2005;26(2):513–524. doi: 10.1016/j.neuroimage.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 152.Caseras X., Mataix-Cols D., Giampietro V., Rimes K.A., Brammer M., Zelaya F., Chalder T., Godfrey E.L. Probing the working memory system in chronic fatigue syndrome: a functional magnetic resonance imaging study using the n-back task. Psychosom. Med. 2006;68(6):947–955. doi: 10.1097/01.psy.0000242770.50979.5f. [DOI] [PubMed] [Google Scholar]
- 153.Tanaka M., Sadato N., Okada T., Mizuno K., Sasabe T., Tanabe H.C., Saito D.N., Onoe H., Kuratsune H., Watanabe Y. Reduced responsiveness is an essential feature of chronic fatigue syndrome: a fMRI study. BMC Neurol. 2006;6:9. doi: 10.1186/1471-2377-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Yoshiuchi K., Farkas J., Natelson B.H. Patients with chronic fatigue syndrome have reduced absolute cortical blood flow. 2006. [DOI] [PubMed]
- 155.Cook D.B., O'Connor P.J., Lange G., Steffener J. Functional neuroimaging correlates of mental fatigue induced by cognition among chronic fatigue syndrome patients and controls. 2007. [DOI] [PubMed]
- 156.Sherlin L., Budzynski T., Kogan Budzynski H., Congedo M., Fischer M.E., Buchwald D. Low-resolution electromagnetic brain tomography (LORETA) of monozygotic twins discordant for chronic fatigue syndrome. Neuroimage. 2007;34(4):1438–1442. doi: 10.1016/j.neuroimage.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 157.Caseras X., Mataix-Cols D., Rimes K.A., Giampietro V., Brammer M., Zelaya F., Chalder T., Godfrey E. The neural correlates of fatigue: an exploratory imaginal fatigue provocation study in chronic fatigue syndrome. Psychol. Med. 2008;38(7):941–951. doi: 10.1017/S0033291708003450. [DOI] [PubMed] [Google Scholar]
- 158.de Lange F.P., Koers A., Kalkman J.S., Bleijenberg G., Hagoort P., van der Meer J.W., Toni I. Increase in prefrontal cortical volume following cognitive behavioural therapy in patients with chronic fatigue syndrome. Brain. 2008;131(Pt 8):2172–2180. doi: 10.1093/brain/awn140. [DOI] [PubMed] [Google Scholar]
- 159.Mathew S.J., Mao X., Keegan K.A., Levine S.M., Smith E.L., Heier L.A., Otcheretko V., Coplan J.D., Shungu D.C. Ventricular cerebrospinal fluid lactate is increased in chronic fatigue syndrome compared with generalized anxiety disorder: an in vivo 3.0 T (1)H MRS imaging study. NMR Biomed. 2009;22(3):251–258. doi: 10.1002/nbm.1315. [DOI] [PubMed] [Google Scholar]
- 160.Flor-Henry P., Lind J.C., Koles Z.J. EEG source analysis of chronic fatigue syndrome. Psychiatry Res. 2010;181(2):155–164. doi: 10.1016/j.pscychresns.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 161.Murrough J.W., Mao X., Collins K.A., Kelly C., Andrade G., Nestadt P., Levine S.M., Mathew S.J., Shungu D.C. Increased ventricular lactate in chronic fatigue syndrome measured by 1H MRS imaging at 3.0 T. II: Comparison with major depressive disorder. NMR Biomed. 2010;23(6):643–650. doi: 10.1002/nbm.1512. [DOI] [PubMed] [Google Scholar]
- 162.Barnden L.R., Crouch B., Kwiatek R., Burnet R., Mernone A., Chryssidis S., Scroop G., Del Fante P. A brain MRI study of chronic fatigue syndrome: evidence of brainstem dysfunction and altered homeostasis. NMR Biomed. 2011;24(10):1302–1312. doi: 10.1002/nbm.1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Biswal B., Kunwar P., Natelson B.H. Cerebral blood flow is reduced in chronic fatigue syndrome as assessed by arterial spin labeling. 2011. [DOI] [PMC free article] [PubMed]
- 164.Shungu D.C., Weiduschat N., Murrough J.W., Mao X., Pillemer S., Dyke J.P., Medow M.S., Natelson B.H., Stewart J.M., Mathew S.J. Increased ventricular lactate in chronic fatigue syndrome. III. Relationships to cortical glutathione and clinical symptoms implicate oxidative stress in disorder pathophysiology. NMR Biomed. 2012;25(9):1073–1087. doi: 10.1002/nbm.2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Yamamoto S., Ouchi Y., Nakatsuka D., Tahara T., Mizuno K., Tajima S., Onoe H., Yoshikawa E., Tsukada H., Iwase M., Yamaguti K., Kuratsune H., Watanabe Y. Reduction of [11C] (+)3-MPB binding in brain of chronic fatigue syndrome with serum autoantibody against muscarinic cholinergic receptor. PLoS One. 2012;7(12):e51515. doi: 10.1371/journal.pone.0051515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Barnden L.R., Crouch B., Kwiatek R., Burnet R., Del Fante P. Evidence in chronic fatigue syndrome for severity-dependent upregulation of prefrontal myelination that is independent of anxiety and depression. NMR Biomed. 2015;28(3):404–413. doi: 10.1002/nbm.3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Tanaka H., Matsushima R., Tamai H., Kajimoto Y. Impaired postural cerebral hemodynamics in young patients with chronic fatigue with and without orthostatic intolerance. J. Pediatr. 2002;140(4):412–417. doi: 10.1067/mpd.2002.122725. [DOI] [PubMed] [Google Scholar]
- 168.Fischler B., D’Haenen H., Cluydts R., Michiels V., Demets K., Bossuyt A., Kaufman L., De Meirleir K. Comparison of 99m Tc HMPAO SPECT scan between chronic fatigue syndrome, major depression and healthy controls: an exploratory study of clinical correlates of regional cerebral blood flow. Neuropsychobiology. 1996;34(4):175–183. doi: 10.1159/000119307. [DOI] [PubMed] [Google Scholar]
- 169.MacHale S.M., Lawŕie S.M., Cavanagh J.T., Glabus M.F., Murray C.L., Goodwin G.M., Ebmeier K.P. Cerebral perfusion in chronic fatigue syndrome and depression. Br. J. Psychiatry. 2000;176:550–556. doi: 10.1192/bjp.176.6.550. [DOI] [PubMed] [Google Scholar]
- 170.Ocon A.J., Medow M.S., Taneja I., Clarke D., Stewart J.M. Decreased upright cerebral blood flow and cerebral autoregulation in normocapnic postural tachycardia syndrome. 2009. [DOI] [PMC free article] [PubMed]
- 171.Wyller V.B., Eriksen H.R., Malterud K. Can sustained arousal explain the Chronic Fatigue Syndrome? Behav. Brain Funct. 2009;5:10. doi: 10.1186/1744-9081-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Morriss R.K., Robson M.J., Deakin J.F. Neuropsychological performance and noradrenaline function in chronic fatigue syndrome under conditions of high arousal. Psychopharmacology, (Berl) 2002;163(2):166–173. doi: 10.1007/s00213-002-1129-8. [DOI] [PubMed] [Google Scholar]
- 173.Nijs J., Meeus M., Van Oosterwijck J., Roussel N., De Kooning M., Ickmans K., Matic M. Treatment of central sensitization in patients with ‘unexplained’ chronic pain: what options do we have? Expert Opin. Pharmacother. 2011;12(7):1087–1098. doi: 10.1517/14656566.2011.547475. [DOI] [PubMed] [Google Scholar]
- 174.Hilty L., Jancke L., Luechinger R., Boutellier U., Lutz K. Limitation of physical performance in a muscle fatiguing handgrip exercise is mediated by thalamo-insular activity. 2011. [DOI] [PMC free article] [PubMed]
- 175.Hilty L., Langer N., Pascual-Marqui R., Boutellier U., Lutz K. Fatigue-induced increase in intracortical communication between mid/anterior insular and motor cortex during cycling exercise. Eur. J. Neurosci. 2011;34(12):2035–2042. doi: 10.1111/j.1460-9568.2011.07909.x. [DOI] [PubMed] [Google Scholar]
- 176.Hilty L., Lutz K., Maurer K., Rodenkirch T., Spengler C.M., Boutellier U., Jancke L., Amann M. Spinal opioid receptor-sensitive muscle afferents contribute to the fatigue-induced increase in intracortical inhibition in healthy humans. 2011. [DOI] [PubMed]
- 177.Billiot K.M., Budzynski T.H., Andrasik F. EEG Patterns and CFS. J. Neurother. 1997;2-2(4) [Google Scholar]
- 178.Neu D., Kajosch H., Peigneux P., Verbanck P., Linkowski P., Le Bon O. Cognitive impairment in fatigue and sleepiness associated conditions. Psychiatry Res. 2011;189(1):128–134. doi: 10.1016/j.psychres.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 179.Donati F., Fagioli L.R., Komaroff A., Duffy F.H. Quantified EEG findings in patients with chronic fatigue syndrome. Ft. Lauderdale, FL: American Association for Chronic Fatigue Syndrome; 1994. [Google Scholar]
- 180.Steriade M. Grouping of brain rhythms in corticothalamic systems. Neuroscience. 2006;137(4):1087–1106. doi: 10.1016/j.neuroscience.2005.10.029. [DOI] [PubMed] [Google Scholar]
- 181.Ropper A.H. S.M. Principles Neurol. Chicago, Illinois: McGraw Hill; 2014. p. 1570. [Google Scholar]
- 182.Duffy F.H., McAnulty G.B., McCreary M.C., Cuchural G.J., Komaroff A.L. EEG spectral coherence data distinguish chronic fatigue syndrome patients from healthy controls and depressed patients--a case control study. BMC Neurol. 2011;11:82. doi: 10.1186/1471-2377-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Grech R., Cassar T., Muscat J., Camilleri K.P., Fabri S.G., Zervakis M., Xanthopoulos P., Sakkalis V., Vanrumste B. Review on solving the inverse problem in EEG source analysis. J. Neuroeng. Rehabil. 2008;5:25. doi: 10.1186/1743-0003-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Pascual-Marqui R., Kochi K., Lehmann D., Koukkou M., Kinoshita T. Functional independent components: Revealing cortico-cortical, cross-frequency interactions. Jpn. J. Pharmacol. EEG. 2011;12:53–58. [Google Scholar]
- 185.Pascual-Marqui R.D. Standardized low-resolution brain electromagnetic tomography (sLORETA): technical details. Methods Find Exp. Clin. Pharmacol. . 2002; 24 Suppl D:5–12. [PubMed] [Google Scholar]
- 186.Pascual-Marqui R.D., Biscay R.J., Bosch-Bayard J., Lehmann D., Kochi K., Kinoshita T., Yamada N., Sadato N. Assessing direct paths of intracortical causal information flow of oscillatory activity with the isolated effective coherence (iCoh). Front. Hum. Neurosci. 2014;8:448. doi: 10.3389/fnhum.2014.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Pascual-Marqui R.D., Lehmann D., Koukkou M., Kochi K., Anderer P., Saletu B., Tanaka H., Hirata K., John E.R., Prichep L., Biscay-Lirio R., Kinoshita T. Assessing interactions in the brain with exact low-resolution electromagnetic tomography. Philos. Trans. A Math Phys. Eng. Sci. 1952;2011(369):3768–3784. doi: 10.1098/rsta.2011.0081. [DOI] [PubMed] [Google Scholar]
- 188.Sekihara K., Nagarajan S.S., Poeppel D., Marantz A., Miyashita Y. Reconstructing spatio-temporal activities of neural sources using an MEG vector beamformer technique. IEEE Trans. Biomed. Eng. 2001;48(7):760–771. doi: 10.1109/10.930901. [DOI] [PubMed] [Google Scholar]
- 189.Nickl-Jockschat T., Kleiman A., Schulz J.B., Schneider F., Laird A.R., Fox P.T., Eickhoff S.B., Reetz K. Neuroanatomic changes and their association with cognitive decline in mild cognitive impairment: a meta-analysis. Brain Struct. Funct. 2012;217(1):115–125. doi: 10.1007/s00429-011-0333-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Le Bon O., Neu D., Berquin Y., Lanquart J.P., Hoffmann R., Mairesse O., Armitage R. Ultra-slow delta power in chronic fatigue syndrome. Psychiatry Res. 2012;200(2-3):742–747. doi: 10.1016/j.psychres.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 191.Flor-Henry P., Lind J.C., Koles Z.J. A source-imaging (low-resolution electromagnetic tomography) study of the EEGs from unmedicated males with depression. Psychiatry Res. 2004;130(2):191–207. doi: 10.1016/j.pscychresns.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 192.Fray P.J., Robbins T.W., Sahakian B.J. Neuropsychiatric applications of CANTAB. 1996.
- 193.Jason L.A., Sunnquist M., Brown A., Evans M., Vernon S.D., Furst J., Simonis V. Examining case definition criteria for chronic fatigue syndrome and myalgic encephalomyelitis. Fatigue. 2014;2(1):40–56. doi: 10.1080/21641846.2013.862993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Landis C.A. Sleep, pain, fibromyalgia, and chronic fatigue syndrome. Handb. Clin. Neurol. 2011;98:613–637. doi: 10.1016/B978-0-444-52006-7.00039-3. [DOI] [PubMed] [Google Scholar]
- 195.Thatcher R.W. Handbook of Quantitative Electroencephalography and EEG Biofeedback. St. Petersburg, FL: ANI Publishing; 2012. [Google Scholar]
- 196.Van Hoof E., De Becker P., Lapp C., Cluydts R., De Meirleir K. Defining the occurrence and influence of alpha-delta sleep in chronic fatigue syndrome. Am. J. Med. Sci. 2007;333(2):78–84. doi: 10.1097/00000441-200702000-00003. [DOI] [PubMed] [Google Scholar]
- 197.Kishi A., Togo F., Cook D.B., Klapholz M., Yamamoto Y., Rapoport D.M., Natelson B.H. The effects of exercise on dynamic sleep morphology in healthy controls and patients with chronic fatigue syndrome. Physiol. Rep. 2013;1(6):e00152. doi: 10.1002/phy2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Decker M.J., Tabassum H., Lin J.M., Reeves W.C. Electroencephalographic correlates of Chronic Fatigue Syndrome. Behav. Brain Funct. 2009;5:43. doi: 10.1186/1744-9081-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Thatcher R.W. Neuropsychiatry and quantitative EEG in the 21st Century. Future Med. 2011;1(5):495–514. doi: 10.2217/npy.11.45. [DOI] [Google Scholar]
- 200.Thatcher R.W. Handbook of Quantitattive Electroencephalo- graphy and EEG Biofeedback. ANI Publishing. St. Petersburg: FLA; 2012. [Google Scholar]
- 201.Spitzer A.R., Broadman M. A retrospective review of the sleep characteristics in patients with chronic fatigue syndrome and fibromyalgia. Pain Pract. 2010;10(4):294–300. doi: 10.1111/j.1533-2500.2009.00352.x. [DOI] [PubMed] [Google Scholar]
- 202.Blanco I., Béritze N., Argüelles M., Cárcaba V., Fernández F., Janciauskiene S., Oikonomopoulou K., de Serres F.J., Fernández-Bustillo E., Hollenberg M.D. Abnormal overexpression of mastocytes in skin biopsies of fibromyalgia patients. Clin. Rheumatol. 2010;29(12):1403–1412. doi: 10.1007/s10067-010-1474-7. [DOI] [PubMed] [Google Scholar]
- 203.Shaver J.L. Sleep disorders. In: Jason L.A., Fennell P.A., Taylor R.R., editors. Handbook of Chronic Fatigue Syndrome. New York: Wiley; 2003. pp. 281–303. [Google Scholar]
- 204.Togo F., Natelson B.H. Heart rate variability during sleep and subsequent sleepiness in patients with chronic fatigue syndrome. Auton. Neurosci. 2013;176(1-2):85–90. doi: 10.1016/j.autneu.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 206.Whelton C.L., Salit I., Moldofsky H. Sleep, Epstein-Barr virus infection, musculoskeletal pain, and depressive symptoms in chronic fatigue syndrome. J. Rheumatol. 1992;19(6):939–943. [PubMed] [Google Scholar]
- 207.Morriss R., Sharpe M., Sharpley A.L., Cowen P.J., Hawton K., Morris J. Abnormalities of sleep in patients with the chronic fatigue syndrome. BMJ. 1993;306(6886):1161–1164. doi: 10.1136/bmj.306.6886.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Krupp L.B., Jandorf L., Coyle P.K., Mendelson W.B. Sleep disturbance in chronic fatigue syndrome. J. Psychosom. Res. 1993;37(4):325–331. doi: 10.1016/0022-3999(93)90134-2. [DOI] [PubMed] [Google Scholar]
- 209.Fischler B., Le Bon O., Hoffmann G., Cluydts R., Kaufman L., De Meirleir K. Sleep anomalies in the chronic fatigue syndrome. A comorbidity study. Neuropsychobiology. 1997;35(3):115–122. doi: 10.1159/000119331. [DOI] [PubMed] [Google Scholar]
- 210.Neu D., Mairesse O., Hoffmann G., Dris A., Lambrecht L.J., Linkowski P., Verbanck P., Le Bon O. Sleep quality perception in the chronic fatigue syndrome: correlations with sleep efficiency, affective symptoms and intensity of fatigue. Neuropsychobiology. 2007;56(1):40–46. doi: 10.1159/000110727. [DOI] [PubMed] [Google Scholar]
- 211.Armitage R., Landis C., Hoffmann R., Lentz M., Watson N.F., Goldberg J., Buchwald D. The impact of a 4-hour sleep delay on slow wave activity in twins discordant for chronic fatigue syndrome. Sleep. 2007;30(5):657–662. doi: 10.1093/sleep/30.5.657. [DOI] [PubMed] [Google Scholar]
- 212.Kishi A., Struzik Z.R., Natelson B.H., Togo F., Yamamoto Y. Dynamics of sleep stage transitions in healthy humans and patients with chronic fatigue syndrome. 2008. [DOI] [PMC free article] [PubMed]
- 213.Togo F., Natelson B.H., Cherniack N.S., FitzGibbons J., Garcon C., Rapoport D.M. Sleep structure and sleepiness in chronic fatigue syndrome with or without coexisting fibromyalgia. Arthritis Res. Ther. 2008;10(3):R56. doi: 10.1186/ar2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Armitage R., Landis C., Hoffmann R., Lentz M., Watson N., Goldberg J., Buchwald D. Power spectral analysis of sleep EEG in twins discordant for chronic fatigue syndrome. 2009. [DOI] [PMC free article] [PubMed]
- 215.Kishi A., Natelson B.H., Togo F., Struzik Z.R., Rapoport D.M., Yamamoto Y. Sleep-stage dynamics in patients with chronic fatigue syndrome with or without fibromyalgia. Sleep. 2011;34(11):1551–1560. doi: 10.5665/sleep.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Gotts Z.M. The role of sleep in Chronic Fatigue Syndrome. [Online] 2014, Doctor of Philosophy, 261. Northumbria University. http://nrl.northumbria.ac.uk/21605/. 2014.
- 217.Loebel M., Strohschein K., Giannini C., Koelsch U., Bauer S., Doebis C., Thomas S., Unterwalder N., von Baehr V., Reinke P., Knops M., Hanitsch L.G., Meisel C., Volk H.D., Scheibenbogen C. Deficient EBV-specific B- and T-cell response in patients with chronic fatigue syndrome. PLoS One. 2014;9(1):e85387. doi: 10.1371/journal.pone.0085387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Watt T., Oberfoell S., Balise R., Lunn M.R., Kar A.K., Merrihew L., Bhangoo M.S., Montoya J.G. Response to valganciclovir in chronic fatigue syndrome patients with human herpesvirus 6 and Epstein-Barr virus IgG antibody titers. 2012. [DOI] [PubMed]
- 219.Hardcastle S.L., Brenu E.W., Johnson S., Nguyen T., Huth T., Kaurl M., Ramos S., Salajegheh A., Staines D., Marshall-Gradisbik S. Analysis of the relationship between immune dysfunction and symptom severity in patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. J. Clin. Cel. Immunol. 2014;5 [Google Scholar]
- 220.Elfaitouri A., Herrmann B., Bolin-Wiener A., Wang Y., Gottfries C.G., Zachrisson O., Pipkorn R., Ronnblom L., Blomberg J. Epitopes of microbial and human heat shock protein 60 and their recognition in myalgic encephalomyelitis. 2013. [DOI] [PMC free article] [PubMed]
- 221.Maier S.F., Watkins L.R., Fleshner M. Psychoneuroimmunology. The interface between behavior, brain, and immunity. Am. Psychol. 1994;49(12):1004–1017. doi: 10.1037/0003-066X.49.12.1004. [DOI] [PubMed] [Google Scholar]
- 222.Libbey J.E., Kennett N.J., Wilcox K.S., White H.S., Fujinami R.S. Interleukin-6, produced by resident cells of the central nervous system and infiltrating cells, contributes to the development of seizures following viral infection. J. Virol. 2011;85(14):6913–6922. doi: 10.1128/JVI.00458-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Gaab J., Rohleder N., Heitz V., Engert V., Schad T., Schürmeyer T.H., Ehlert U. Stress-induced changes in LPS-induced pro-inflammatory cytokine production in chronic fatigue syndrome. Psychoneuroendocrinology. 2005;30(2):188–198. doi: 10.1016/j.psyneuen.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 224.Vollmer-Conna U., Piraino B.F., Cameron B., Davenport T., Hickie I., Wakefield D., Lloyd A.R., Dubbo Infection Outcomes Study Group Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection. Clin. Infect. Dis. 2008;47(11):1418–1425. doi: 10.1086/592967. [DOI] [PubMed] [Google Scholar]
- 225.Plata-Salamán C.R., Ilyin S.E., Turrin N.P., Gayle D., Flynn M.C., Romanovitch A.E., Kelly M.E., Bureau Y., Anisman H., McIntyre D.C. Kindling modulates the IL-1beta system, TNF-alpha, TGF-beta1, and neuropeptide mRNAs in specific brain regions. Brain Res. Mol. Brain Res. 2000;75(2):248–258. doi: 10.1016/S0169-328X(99)00306-X. [DOI] [PubMed] [Google Scholar]
- 226.Shandra A.A., Godlevsky L.S., Vastyanov R.S., Oleinik A.A., Konovalenko V.L., Rapoport E.N., Korobka N.N. The role of TNF-alpha in amygdala kindled rats. Neurosci. Res. 2002;42(2):147–153. doi: 10.1016/S0168-0102(01)00309-1. [DOI] [PubMed] [Google Scholar]
- 227.Aalbers M.W., Rijkers K., Majoie H.J., Dings J.T., Schijns O.E., Schipper S., De Baets M.H., Kessels A., Vles J.S., Hoogland G. The influence of neuropathology on brain inflammation in human and experimental temporal lobe epilepsy. J. Neuroimmunol. 2014;271(1-2):36–42. doi: 10.1016/j.jneuroim.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 228.Zhao R.R., Xu X.C., Xu F., Zhang W.L., Zhang W.L., Liu L.M., Wang W.P. Metformin protects against seizures, learning and memory impairments and oxidative damage induced by pentylenetetrazole-induced kindling in mice. Biochem. Biophys. Res. Commun. 2014;448(4):414–417. doi: 10.1016/j.bbrc.2014.04.130. [DOI] [PubMed] [Google Scholar]
- 229.Morris G., Maes M. A neuro-immune model of Myalgic Encephalomyelitis/Chronic fatigue syndrome. Metab. Brain Dis. 2013;28(4):523–540. doi: 10.1007/s11011-012-9324-8. [DOI] [PubMed] [Google Scholar]
- 230.Maes M., Mihaylova I., Kubera M., Leunis J.C., Twisk F.N., Geffard M. IgM-mediated autoimmune responses directed against anchorage epitopes are greater in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) than in major depression. Metab. Brain Dis. 2012;27(4):415–423. doi: 10.1007/s11011-012-9316-8. [DOI] [PubMed] [Google Scholar]
- 231.Maes M., Twisk F.N., Ringel K. Inflammatory and cell-mediated immune biomarkers in myalgic encephalomyelitis/chronic fatigue syndrome and depression: inflammatory markers are higher in myalgic encephalomyelitis/chronic fatigue syndrome than in depression. Psychother. Psychosom. 2012;81(5):286–295. doi: 10.1159/000336803. [DOI] [PubMed] [Google Scholar]
- 232.Fletcher M.A., Rosenthal M., Antoni M., Ironson G., Zeng X.R., Barnes Z., Harvey J.M., Hurwitz B., Levis S., Broderick G., Klimas N.G. Plasma neuropeptide Y: a biomarker for symptom severity in chronic fatigue syndrome. Behav. Brain Funct. 2010;6:76. doi: 10.1186/1744-9081-6-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Brenu E.W., van Driel M.L., Staines D.R., Ashton K.J., Ramos S.B., Keane J., Klimas N.G., Marshall-Gradisnik S.M. Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. J. Transl. Med. 2011;9:81. doi: 10.1186/1479-5876-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Gomariz R.P., Juarranz Y., Abad C., Arranz A., Leceta J., Martinez C. VIP-PACAP system in immunity: new insights for multitarget therapy. Ann. N. Y. Acad. Sci. 2006;1070:51–74. doi: 10.1196/annals.1317.031. [DOI] [PubMed] [Google Scholar]
- 235.Fletcher M.A., Zeng X.R., Maher K., Levis S., Hurwitz B., Antoni M., Broderick G., Klimas N.G. Biomarkers in chronic fatigue syndrome: evaluation of natural killer cell function and dipeptidyl peptidase IV/CD26. PLoS One. 2010;5(5):e10817. doi: 10.1371/journal.pone.0010817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Brenu E.W., van Driel M.L., Staines D.R., Ashton K.J., Hardcastle S.L., Keane J., Tajouri L., Peterson D., Ramos S.B., Marshall-Gradisnik S.M. Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. J. Transl. Med. 2012;10:88. doi: 10.1186/1479-5876-10-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Brenu E.W., Ashton K.J., van Driel M., Staines D.R., Peterson D., Atkinson G.M., Marshall-Gradisnik S.M. Cytotoxic lymphocyte microRNAs as prospective biomarkers for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. J. Affect. Disord. 2012;141(2-3):261–269. doi: 10.1016/j.jad.2012.03.037. [DOI] [PubMed] [Google Scholar]
- 238.Broderick G., Fuite J., Kreitz A., Vernon S.D., Klimas N., Fletcher M.A. A formal analysis of cytokine networks in chronic fatigue syndrome. Brain Behav. Immun. 2010;24(7):1209–1217. doi: 10.1016/j.bbi.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Broderick G., Klimas N., Fletcher M.A., Efroni S. From cytokines to cells to gene expression: An integrative approach to the study of Gulf War Illness systems biology. In: research Advisory Committe on Gulf War Veterans Illnesses: Washington, D. C.: 2011. [Google Scholar]
- 240.Broderick G., Kreitz A., Fuite J., Fletcher M.A., Vernon S.D., Klimas N. A pilot study of immune network remodeling under challenge in Gulf War Illness. Brain Behav. Immun. 2011;25(2):302–313. doi: 10.1016/j.bbi.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 241.Sorenson M., Furst J., Mathews H., Jason L.A. 2014. Disruption of cytokine pathways in Chronic Fatigue Syndrome. [Google Scholar]
- 242.Hanson S.J., Gause W., Natelson B. Detection of immunologically significant factors for chronic fatigue syndrome using neural-network classifiers. Clin. Diagn. Lab. Immunol. 2001;8(3):658–662. doi: 10.1128/cdli.8.3.658-662.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Huang L.C., Hsu S.Y., Lin E. A comparison of classification methods for predicting Chronic Fatigue Syndrome based on genetic data. J. Transl. Med. 2009;7:81. doi: 10.1186/1479-5876-7-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Stringer E.A., Baker K.S., Carroll I.R., Montoya J.G., Chu L., Maecker H.T., Younger J.W. Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: evidence of inflammatory pathology. J. Transl. Med. 2013;11:93. doi: 10.1186/1479-5876-11-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Lerner A.M., Beqaj S., Fitzgerald J.T., Gill K., Gill C., Edington D. Subset-directed antiviral treatment of 142 herpesvirus patients with Chronic Fatigue Syndrome. Virus Adaptation Treat. 2010;2:1–11. [Google Scholar]
- 246.Lerner A.M., Ariza M.E., Williams M., Jason L., Beqaj S., Fitzgerald J.T., Lemeshow S., Glaser R. Antibody to Epstein-Barr virus deoxyuridine triphosphate nucleotidohydrolase and deoxyribonucleotide polymerase in a chronic fatigue syndrome subset. PLoS One. 2012;7(11):e47891. doi: 10.1371/journal.pone.0047891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Embers M.E., Barthold S.W., Borda J.T., Bowers L., Doyle L., Hodzic E., Jacobs M.B., Hasenkampf N.R., Martin D.S., Narasimhan S., Phillippi-Falkenstein K.M., Purcell J.E., Ratterree M.S., Philipp M.T. Persistence of Borrelia burgdorferi in rhesus macaques following antibiotic treatment of disseminated infection. PLoS One. 2012;7(1):e29914. doi: 10.1371/journal.pone.0029914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Tzartos J.S., Khan G., Vossenkamper A., Cruz-Sadaba M., Lonardi S., Sefia E., Meager A., Elia A., Middeldorp J.M., Clemens M., Farrell P.J., Giovannoni G., Meier U.C. Association of innate immune activation with latent Epstein-Barr virus in active MS lesions. Neurology. 2012;78(1):15–23. doi: 10.1212/WNL.0b013e31823ed057. [DOI] [PubMed] [Google Scholar]
- 249.Capuron L., Pagnoni G., Demetrashvili M.F., Lawson D.H., Fornwalt F.B., Woolwine B., Berns G.S., Nemeroff C.B., Miller A.H. Basal ganglia hypermetabolism and symptoms of fatigue during interferon-alpha therapy. Neuropsychopharmacology. 2007;32(11):2384–2392. doi: 10.1038/sj.npp.1301362. [DOI] [PubMed] [Google Scholar]
- 250.Fluge Ø., Risa K., Lunde S., Alme K., Rekeland I.G., Sapkota D., Kristoffersen E.K., Sørland K., Bruland O., Dahl O., Mella O. Lymphocyte depletion in myalgic encephalopathy/ Chronic fatigue syndrome: An open-label Phase II study with Rituximab maintenance treatment. PLoS One. 2015;10(7):e0129898. doi: 10.1371/journal.pone.0129898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Jason L.A., Torres-Harding S., Brown M., Sorenson M., Donalek J., Corradi K., Maher K., Fletcher M.A. Predictors of changes following participation in non-pharmacologic intervention for CFS. 2008. [DOI]
- 252.Falkenberg V.R., Whistler T., Murray J.R., Unger E.R., Rajeevan M.S. Acute psychosocial stress-mediated changes in the expression and methylation of perforin in chronic fatigue syndrome. 2013. [DOI] [PMC free article] [PubMed]
- 253.Hornig M., Montoya J.G., Klimas N.G., Levine S., Felsenstein D., Bateman L., Peterson D.L., Gottschalk C.G., Schultz A.F., Che X., Eddy M.L., Komaroff A.L., Lipkin W.I. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci. Adv. 2015;1:1–10. doi: 10.1126/sciadv.1400121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Hornig M., Gottschalk G., Peterson D.L., Knox K.K., Schultz A.F., Eddy M. L., Che X., Lipkin W.I. Immunology. In: Handbook of Chronic Fatigue Syndrome. New York: Wiley; pp. 124–151. [Google Scholar]
- 255.Maher K.J., Klimas N.G., Fletcher M.A. Immunology. In: Jason L.A., Fennell P.A., Taylor R.R., editors. Handbook of Chronic Fatigue Syndrome. New York: Wiley; 2003. pp. 124–151. [Google Scholar]
- 256.Buijs R.M. The autonomic nervous system: a balancing act. Handb. Clin. Neurol. 2013;117:1–11. doi: 10.1016/B978-0-444-53491-0.00001-8. [DOI] [PubMed] [Google Scholar]
- 257.O'Connor T.M., O'Halloran D.J., Shanahan F. The stress response and the hypothalamic-pituitary-adrenal axis: From molecule to melancholia. QJM, 2000;93(6):323–333. doi: 10.1093/qjmed/93.6.323. [DOI] [PubMed] [Google Scholar]
- 258.Juster R.P., McEwen B.S., Lupien S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. 2010. [DOI] [PubMed]
- 259.McEwen B.S., Morrison J.H. The brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron. 2013;79(1):16–29. doi: 10.1016/j.neuron.2013.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Sorrells S.F., Sapolsky R.M. An inflammatory review of glucocorticoid actions in the CNS. Brain Behav. Immun. 2007;21(3):259–272. doi: 10.1016/j.bbi.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.McEwen B.S., Wingfield J.C. What is in a name? Integrating homeostasis, allostasis and stress. Horm. Behav. 2010;57(2):105–111. doi: 10.1016/j.yhbeh.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Chrousos G.P. Regulation and dysregulation of the hypothalamic-pituitary-adrenal axis. The corticotropin-releasing hormone perspective. Endocrinol. Metab. Clin. North Am. 1992;21(4):833–858. [PubMed] [Google Scholar]
- 263.Sapolsky R.M. Stress and plasticity in the limbic system. 2003. [DOI] [PubMed]
- 264.Sapolsky R.M., Romero L.M., Munck A.U. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr. Rev. 2000;21(1):55–89. doi: 10.1210/er.21.1.55. [DOI] [PubMed] [Google Scholar]
- 265.Maniam J., Antoniadis C., Morris M.J. Early-Life Stress, HPA Axis Adaptation, and Mechanisms Contributing to Later Health Outcomes. Front Endocrinol. 2014;5(73) doi: 10.3389/fendo.2014.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Reynolds R.M., Hii H.L., Pennell C.E., McKeague I.W., de Kloet E.R., Lye S., Stanley F.J., Mattes E., Foster J.K. Analysis of baseline hypothalamic-pituitary-adrenal activity in late adolescence reveals gender specific sensitivity of the stress axis. Psychoneuroendocrinology. 2013;38(8):1271–1280. doi: 10.1016/j.psyneuen.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 267.Reynolds R.M., Walker B.R., Haw S., Newby D.E., Mackay D.F., Cobbe S.M., Pell A.C., Fischbacher C., Pringle S., Murdoch D., Dunn F., Oldroyd K., Macintyre P., O’Rourke B., Pell J.P. Low serum cortisol predicts early death after acute myocardial infarction. Crit. Care Med. 2010;38(3):973–975. doi: 10.1097/CCM.0b013e3181cdf6de. [DOI] [PubMed] [Google Scholar]
- 268.Brouwer M.C., McIntyre P., Prasad K., van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst. Rev. 2013;6:CD004405. doi: 10.1002/14651858.cd004405.pub4. [DOI] [PubMed] [Google Scholar]
- 269.Kern S., Rohleder N., Eisenhofer G., Lange J., Ziemssen T. Time matters - acute stress response and glucocorticoid sensitivity in early multiple sclerosis. Brain Behav. Immun. 2014;41:82–89. doi: 10.1016/j.bbi.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 270.Mo G.L., Li Y., Du R.H., Dai D.Z., Cong X.D., Dai Y. Isoproterenol induced stressful reactions in the brain are characterized by inflammation due to activation of NADPH oxidase and ER stress: attenuated by Apocynin, Rehmannia complex and Triterpene acids. Neurochem. Res. 2014;39(4):719–730. doi: 10.1007/s11064-014-1260-z. [DOI] [PubMed] [Google Scholar]
- 271.Sapolsky R.M., Krey L.C., McEwen B.S. McEwen, B.S. The adrenocortical stress-response in the aged male rat: Impairment of recovery from stress. Exp. Gerontol. 1983;18(1):55–64. doi: 10.1016/0531-5565(83)90051-7. [DOI] [PubMed] [Google Scholar]
- 272.Perini R., Veicsteinas A. Heart rate variability and autonomic activity at rest and during exercise in various physiological conditions. Eur. J. Appl. Physiol. 2003;90(3-4):317–325. doi: 10.1007/s00421-003-0953-9. [DOI] [PubMed] [Google Scholar]
- 273.Robertson D. Primer on the Autonomic Nervous System. New York: Elsevier; 2012. [Google Scholar]
- 274.Tripathi O.N., Ravens U., Sanguinetti M.C. Heart Rate and Rhythms. New York: Springer; 2011. Heart Rate and Rhythm: Molecular Basis, Pharmacological Modulation and Clinical Implications. [DOI] [Google Scholar]
- 275.Rodrigues S.M., LeDoux J.E., Sapolsky R.M. The influence of stress hormones on fear circuitry. Annu. Rev. Neurosci. 2009;32:289–313. doi: 10.1146/annurev.neuro.051508.135620. [DOI] [PubMed] [Google Scholar]
- 276.Pajand P., Elahdadi Salmani M., Shajiee H., Abiri H., Goudarzi I., Abrari K. Stress during first pregnancy increases seizure threshold in adult male offspring. Iran. J. Basic Med. Sci. 2014;17(1):34–40. [PMC free article] [PubMed] [Google Scholar]
- 277.Juruena M.F. Early-life stress and HPA axis trigger recurrent adulthood depression. Epilepsy Behav. 2014;38:148–159. doi: 10.1016/j.yebeh.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 278.Kellett J., Kokkinidis L. Extinction deficit and fear reinstatement after electrical stimulation of the amygdala: implications for kindling-associated fear and anxiety. Neuroscience. 2004;127(2):277–287. doi: 10.1016/j.neuroscience.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 279.Willner P., Scheel-Kruger J., Belzung C. The neurobiology of depression and antidepressant action. 2013. [DOI] [PubMed]
- 280.Maloney E.M., Boneva R., Nater U.M., Reeves W.C. Chronic fatigue syndrome and high allostatic load: Results from a population-based case-control study in Georgia. Psychosom. Med. 2009;71(5):549–556. doi: 10.1097/PSY.0b013e3181a4fea8. [DOI] [PubMed] [Google Scholar]
- 281.Cleare A.J. The HPA axis and the genesis of chronic fatigue syndrome. Trends Endocrinol. Metab. 2004;15(2):55–59. doi: 10.1016/j.tem.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 282.Grippo A.J., Scotti M.L. Stress and Neuroinflammation. In: Halaris A., Leonard B.E., editors. Inflammation in Psychiatry. Vol. 28. Basel, Switzerland: Karger; 2013. pp. 20–32. [DOI] [Google Scholar]
- 283.Van Den Eede F., Moorkens G., Van Houdenhove B., Cosyns P., Claes S.J. Hypothalamic-pituitary-adrenal axis function in chronic fatigue syndrome. Neuropsychobiology. 2007;55(2):112–120. doi: 10.1159/000104468. [DOI] [PubMed] [Google Scholar]
- 284.Naschitz J.E., Yeshurun D., Rosner I. Dysautonomia in chronic fatigue syndrome: Facts, hypotheses, implications. . Med. Hypotheses, 2004;62(2):203–206. doi: 10.1016/S0306-9877(03)00331-1. [DOI] [PubMed] [Google Scholar]
- 285.Martínez-Martínez L.A., Mora T., Vargas A., Fuentes-Iniestra M., Martínez-Lavín M. Sympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis: a review of case-control studies. J. Clin. Rheumatol. 2014;20(3):146–150. doi: 10.1097/RHU.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 286.Visser F.C. Science to patients, Seminar 22: ME/CFS and palpitations. [Online] 2013. ME/CFS Vereniging. [Accessed on: 07/11/2014]. 2013.
- 287.Malik M., Camm J.A. Heart Rate Variability. Armonk, NY: Futura Publishing; 1995. [Google Scholar]
- 288.Miwa K. Cardiac dysfunction and orthostatic intolerance in patients with myalgic encephalomyelitis and a small left ventricle. Heart Vessels. 2014 doi: 10.1007/s00380-014-0510-y. [DOI] [PubMed] [Google Scholar]
- 289.Mainardi L.T., Bianchi A.M., Baselli G., Cerutti S. Pole-tracking algorithms for the extraction of time-variant heart rate variability spectral parameters. IEEE Trans. Biomed. Eng. 1995;42(3):250–259. doi: 10.1109/10.364511. [DOI] [PubMed] [Google Scholar]
- 290.Cordero D.L., Sisto S.A., Tapp W.N., LaManca J.J., Pareja J.G., Natelson B.H. Decreased vagal power during treadmill walking in patients with chronic fatigue syndrome. Clin. Auton. Res. 1996;6(6):329–333. doi: 10.1007/BF02556303. [DOI] [PubMed] [Google Scholar]
- 291.Jackson M.L., Bruck D. Sleep abnormalities in chronic fatigue syndrome/myalgic encephalomyelitis: a review. J. Clin. Sleep Med. 2012;8(6):719–728. doi: 10.5664/jcsm.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Ohashi K., Yamamoto Y., Natelson B.H. Activity rhythm degrades after strenuous exercise in chronic fatigue syndrome. Physiol. Behav. 2002;77(1):39–44. doi: 10.1016/S0031-9384(02)00808-9. [DOI] [PubMed] [Google Scholar]
- 293.VanElzakker M.B. Chronic fatigue syndrome from vagus nerve infection: a psychoneuroimmunological hypothesis. Med. Hypotheses. 2013;81(3):414–423. doi: 10.1016/j.mehy.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 294.Hollingsworth K.G., Hodgson T., Macgowan G.A., Blamire A.M., Newton J.L. Impaired cardiac function in chronic fatigue syndrome measured using magnetic resonance cardiac tagging. 2012. [DOI] [PMC free article] [PubMed]
- 295.Beaumont A., Burton A.R., Lemon J., Bennett B.K., Lloyd A., Vollmer-Conna U. Reduced cardiac vagal modulation impacts on cognitive performance in chronic fatigue syndrome. 2012. [DOI] [PMC free article] [PubMed]
- 296.Boneva R.S., Decker M.J., Maloney E.M., Lin J.M., Jones J.F., Helgason H.G., Heim C.M., Rye D.B., Reeves W.C. Higher heart rate and reduced heart rate variability persist during sleep in chronic fatigue syndrome: A population-based study. 2007. [DOI] [PubMed]
- 297.Frith J., Zalewski P., Klawe J.J., Pairman J., Bitner A., Tafil-Klawe M., Newton J.L. Impaired blood pressure variability in chronic fatigue syndrome--a potential biomarker. QJM. 2012;105(9):831–838. doi: 10.1093/qjmed/hcs085. [DOI] [PubMed] [Google Scholar]
- 298.Ocon A.J., Messer Z.R., Medow M.S., Stewart J.M. Increasing orthostatic stress impairs neurocognitive functioning in chronic fatigue syndrome with postural tachycardia syndrome. Clin. Sci. 2012;122(5):227–238. doi: 10.1042/CS20110241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Ravindran M., Adewuyi O., Zheng Y., Rayhan R.U., Le U., Timbol C., Merck S., Esteitie R., Read C., Cooney M., Baraniuk J. Dyspnea in Chronic Fatigue Syndrome (CFS): comparison of two prospective cross-sectional studies. Glob. J. Health Sci. 2013;5(2):94–110. doi: 10.5539/gjhs.v5n2p94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Ganong W.F. Appleton & Lange: Stamford. CT: Rev. Med. Physiol; 1997. [Google Scholar]
- 301.Bonow R.O., Mann D.L., Zipes D.P., Libby P., Braunwald E. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia, PA: Elsevier Saunders; 2012. [Google Scholar]
- 302.Li H., Yu X., Liles C., Khan M., Vanderlinde-Wood M., Galloway A., Zillner C., Benbrook A., Reim S., Collier D., Hill M.A., Raj S.R., Okamoto L.E., Cunningham M.W., Aston C.E., Kem D.C. Autoimmune basis for postural tachycardia syndrome. 2014. [DOI] [PMC free article] [PubMed]
- 303.Choy A.M., Lang C.C., Roden D.M., Robertson D., Wood A.J., Robertson R.M., Biaggioni I. Abnormalities of the QT interval in primary disorders of autonomic failure. Am. Heart J. 1998;136(4 Pt 1):664–671. doi: 10.1016/S0002-8703(98)70014-6. [DOI] [PubMed] [Google Scholar]
- 304.Scott A., Norton M., Mabillard H., Newton J.L. Shortened QTc interval in Chronic Fatigue Syndrome. IAMEME Bulletin. 2012;19(3/4):202–211. [Google Scholar]
- 305.Lewis I., Pairman J., Spickett G., Newton J.L. Clinical characteristics of a novel subgroup of chronic fatigue syndrome patients with postural orthostatic tachycardia syndrome. J. Intern. Med. 2013;273(5):501–510. doi: 10.1111/joim.12022. [DOI] [PubMed] [Google Scholar]
- 306.Badham S.P., Hutchinson C.V. Characterising eye movement dysfunction in myalgic encephalomyelitis/chronic fatigue syndrome. Graefes Arch. Clin. Exp. Ophthalmol. 2013;251(12):2769–2776. doi: 10.1007/s00417-013-2431-3. [DOI] [PubMed] [Google Scholar]
- 307.Hutchinson C.V., Maltby J., Badham S.P., Jason L.A. Vision-related symptoms as a clinical feature of chronic fatigue syndrome/myalgic encephalomyelitis? Evidence from the DePaul Symptom Questionnaire. Br. J. Ophthalmol. 2014;98(1):144–145. doi: 10.1136/bjophthalmol-2013-304439. [DOI] [PubMed] [Google Scholar]
- 308.Newton J.L., Okonkwo O., Sutcliffe K., Seth A., Shin J., Jones D.E. Symptoms of autonomic dysfunction in chronic fatigue syndrome. 2007. [DOI] [PubMed]
- 309.Jason L.A., Unger E.R., Dimitrakoff J.D., Fagin A.P., Houghton M., Cook D.B., Marshall G.D., Jr, Klimas N., Snell C. Minimum data elements for research reports on CFS. 2012. [DOI] [PMC free article] [PubMed]
- 310.Crofford L.J., Young E.A., Engleberg N.C., Korszun A., Brucksch C.B., McClure L.A., Brown M.B., Demitrack M.A. Basal circadian and pulsatile ACTH and cortisol secretion in patients with fibromyalgia and/or chronic fatigue syndrome. Brain Behav. Immun. 2004;18(4):314–325. doi: 10.1016/j.bbi.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 311.Demitrack M.A., Crofford L.J. Evidence for and pathophysiologic implications of hypothalamic-pituitary-adrenal axis dysregulation in fibromyalgia and chronic fatigue syndrome. 1998. [DOI] [PubMed]
- 312.Jerjes W.K., Cleare A.J., Wessely S., Wood P.J., Taylor N.F. Diurnal patterns of salivary cortisol and cortisone output in chronic fatigue syndrome. J. Affect. Disord. 2005;87(2-3):299–304. doi: 10.1016/j.jad.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 313.Nijhof S.L., Rutten J.M., Uiterwaal C.S., Bleijenberg G., Kimpen J.L., Putte E.M. The role of hypocortisolism in chronic fatigue syndrome. Psychoneuroendocrinology. 2014;42:199–206. doi: 10.1016/j.psyneuen.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 314.Poteliakhoff A. Adrenocortical activity and some clinical findings in acute and chronic fatigue. J. Psychosom. Res. 1981;25(2):91–95. doi: 10.1016/0022-3999(81)90095-7. [DOI] [PubMed] [Google Scholar]
- 315.Roberts A.D., Wessely S., Chalder T., Papadopoulos A., Cleare A.J. Salivary cortisol response to awakening in chronic fatigue syndrome. Br. J. Psychiatry. 2004;184:136–141. doi: 10.1192/bjp.184.2.136. [DOI] [PubMed] [Google Scholar]
- 316.Torres-Harding S., Sorenson M., Jason L., Maher K., Fletcher M.A., Reynolds N., Brown M. The associations between basal salivary cortisol and illness symptomatology in chronic fatigue syndrome. J. Appl. Biobehav. Res. 2008;13:157–180. doi: 10.1111/j.1751-9861.2008.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Powell D.J., Liossi C., Moss-Morris R., Schlotz W. Unstimulated cortisol secretory activity in everyday life and its relationship with fatigue and chronic fatigue syndrome: a systematic review and subset meta-analysis. Psychoneuroendocrinology. 2013;38(11):2405–2422. doi: 10.1016/j.psyneuen.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 318.Sorrells S.F., Caso J.R., Munhoz C.D., Hu C.K., Tran K.V., Miguel Z.D., Chien B.Y., Sapolsky R.M. Glucocorticoid signaling in myeloid cells worsens acute CNS injury and inflammation. J. Neurosci. 2013;33(18):7877–7889. doi: 10.1523/JNEUROSCI.4705-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Woon F.L., Dunn C.B., Hopkins R.O. Predicting cognitive sequelae in survivors of critical illness with cognitive screening tests. Am. J. Respir. Crit. Care Med. 2012;186(4):333–340. doi: 10.1164/rccm.201112-2261OC. [DOI] [PubMed] [Google Scholar]
- 320.Hopkins R.O., Suchyta M.R., Farrer T.J., Needham D. Improving post-intensive care unit neuropsychiatric outcomes: Understanding cognitive effects of physical activity. Am. J. Respir. Crit. Care Med. 2012;186(12):1220–1228. doi: 10.1164/rccm.201206-1022CP. [DOI] [PubMed] [Google Scholar]
- 321.Pandharipande P.P., Girard T.D., Ely E.W. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 2014;370(2):185–186. doi: 10.1097/sa.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 322.Pandharipande P.P., Girard T.D., Jackson J.C., Morandi A., Thompson J.L., Pun B.T., Brummel N.E., Hughes C.G., Vasilevskis E.E., Shintani A.K., Moons K.G., Geevarghese S.K., Canonico A., Hopkins R.O., Bernard G.R., Dittus R.S., Ely E.W., BRAIN-ICU Study Investigators Long-term cognitive impairment after critical illness. N. Engl. J. Med. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Dinkel K., MacPherson A., Sapolsky R.M. Novel glucocorticoid effects on acute inflammation in the CNS. 2003. [DOI] [PubMed]
- 324.Padgett D.A., Glaser R. How stress influences the immune response. Trends Immunol. 2003;24(8):444–448. doi: 10.1016/S1471-4906(03)00173-X. [DOI] [PubMed] [Google Scholar]
- 325.Goosens K.A., Sapolsky R.M. Stress and Glucocorticoid Contributions to Normal and Pathological Aging. Boca Raton, FL: Taylor & Francis Group, LLC; 2007. [PubMed] [Google Scholar]
- 326.Baram T.Z., Hatalski C.G. Neuropeptide-mediated excitability: A key triggering mechanism for seizure generation in the developing brain. 1998. [DOI] [PMC free article] [PubMed]
- 327.Cleare A.J., Bearn J., Allain T., McGregor A., Wessely S., Murray R.M., O'Keane V. Contrasting neuroendocrine responses in depression and chronic fatigue syndrome. 1995. [DOI] [PubMed]
- 328.Rohleder N., Schommer N.C., Hellhammer D.H., Engel R., Kirschbaum C. Sex differences in glucocorticoid sensitivity of proinflammatory cytokine production after psychosocial stress. Psychosom. Med. 2001;63(6):966–972. doi: 10.1097/00006842-200111000-00016. [DOI] [PubMed] [Google Scholar]
- 329.Smith A.K., White P.D., Aslakson E., Vollmer-Conna U., Rajeevan M.S. Polymorphisms in genes regulating the HPA axis associated with empirically delineated classes of unexplained chronic fatigue. Pharmacogenomics. 2006;7(3):387–394. doi: 10.2217/14622416.7.3.387. [DOI] [PubMed] [Google Scholar]
- 330.Kavelaars A., Kuis W., Knook L., Sinnema G., Heijnen C.J. Disturbed neuroendocrine-immune interactions in chronic fatigue syndrome. J. Clin. Endocrinol. Metab. 2000;85(2):692–696. doi: 10.1210/jc.85.2.692. [DOI] [PubMed] [Google Scholar]
- 331.Jason L., Porter N., Shelleby E., Till L., Bell D.S., Lap C.W., Rowe K., Meirleir K.D. Examining criteria to diagnose ME/CFS in pediatric samples. J. Behav. Health Med. 2010;3(3):186–195. doi: 10.1037/h0100551. [DOI] [Google Scholar]
- 332.Meyer J.D., L.A.; Shukla S.K., Clevidence D., Yale S., Stegner A. Cook D. Post-exertion malaise in chronic fatigue syndrome: Symptoms and gene expression. Fatigue: Biomed. Health Behav; 2013. [Google Scholar]
- 333.Yuan Z., R. Z.N., Zhang X., Seto E. Histone Deacetylase Activity Assay. In: Chellappan S., editor. Chromatin Protocols. New York: Springer; 2009. [DOI] [Google Scholar]
- 334.Arnold M.C., Papanicolaou D.A., O’Grady J.A., Lotsikas A., Dale J.K., Straus S.E., Grafman J. Using an interleukin-6 challenge to evaluate neuropsychological performance in chronic fatigue syndrome. Psychol. Med. 2002;32(6):1075–1089. doi: 10.1017/S0033291702006086. [DOI] [PubMed] [Google Scholar]
- 335.Pall M.L. Nitric oxide synthase partial uncoupling as a key switching mechanism for the NO/ONOO- cycle. Med. Hypotheses. 2007;69(4):821–825. doi: 10.1016/j.mehy.2007.01.070. [DOI] [PubMed] [Google Scholar]
- 336.Peckerman A., LaManca J.J., Dahl K.A., Chemitiganti R., Qureishi B., Natelson B.H. Abnormal impedance cardiography predicts symptom severity in chronic fatigue syndrome. Am. J. Med. Sci. 2003;326(2):55–60. doi: 10.1097/00000441-200308000-00001. [DOI] [PubMed] [Google Scholar]
- 337.Cho H.J., Skowera A., Cleare A., Wessely S. Chronic fatigue syndrome: an update focusing on phenomenology and pathophysiology. Curr. Opin. Psychiatry. 2006;19(1):67–73. doi: 10.1097/01.yco.0000194370.40062.b0. [DOI] [PubMed] [Google Scholar]
- 338.Bakheit A.M., Behan P.O., Dinan T.G., Gray C.E., O’Keane V. Possible upregulation of hypothalamic 5-hydroxytryptamine receptors in patients with postviral fatigue syndrome. BMJ. 1992;304(6833):1010–1012. doi: 10.1136/bmj.304.6833.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Spath M., Welzel D., Farber L. Treatment of chronic fatigue syndrome with 5-HT3 receptor antagonists--preliminary results. . Scand. J. Rheumatol. . 2000;113:72–77. doi: 10.1080/030097400446698. [DOI] [PubMed] [Google Scholar]
- 340.Vassallo C.M., Feldman E., Peto T., Castell L., Sharpley A.L., Cowen P.J. Decreased tryptophan availability but normal post-synaptic 5-HT2c receptor sensitivity in chronic fatigue syndrome. Psychol. Med. 2001;31(4):585–591. doi: 10.1017/S0033291701003580. [DOI] [PubMed] [Google Scholar]
- 341.Badawy A.A., Morgan C.J., Llewelyn M.B., Albuquerque S.R., Farmer A. Heterogeneity of serum tryptophan concentration and availability to the brain in patients with the chronic fatigue syndrome. J. Psychopharmacol. (Oxford) 2005;19(4):385–391. doi: 10.1177/0269881105053293. [DOI] [PubMed] [Google Scholar]
- 342.Glass J.M., Lyden A.K., Petzke F., Stein P., Whalen G., Ambrose K., Chrousos G., Clauw D.J. The effect of brief exercise cessation on pain, fatigue, and mood symptom development in healthy, fit individuals. J. Psychosom. Res. 2004;57(4):391–398. doi: 10.1016/S0022-3999(04)00080-7. [DOI] [PubMed] [Google Scholar]
- 343.Baraniuk J.N., Zheng Y. Relationships among rhinitis, fibromyalgia, and chronic fatigue. Allergy Asthma Proc. 2010;31(3):169–178. doi: 10.2500/aap.2010.31.3311. [DOI] [PubMed] [Google Scholar]
- 344.Jason L.A., So S., Brown A., Sunnquist M., Evans M. Testretest reliability of the DePaul Symptom Questionnaire. Fatigue Biomed. Health Behav. 2015;3(1):16–32. doi: 10.1080/21641846.2014.978110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Meeus M., Nijs J., Meirleir K.D. Chronic musculoskeletal pain in patients with the chronic fatigue syndrome: A systematic review. 2007. [DOI] [PubMed]
- 346.van Wilgen C.P., Keizer D. The sensitization model to explain how chronic pain exists without tissue damage. Pain Manag. Nurs. 2012;13(1):60–65. doi: 10.1016/j.pmn.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 347.Mendell L.M., Wall P.D. Responses of single dorsal cord cells to peripheral cutaneous unmyelinated fibres. Nature. 1965;206:97–99. doi: 10.1038/206097a0. [DOI] [PubMed] [Google Scholar]
- 348.Martinez-Lavin M., Solano C. Dorsal root ganglia, sodium channels, and fibromyalgia sympathetic pain. Med. Hypotheses. 2009;72(1):64–66. doi: 10.1016/j.mehy.2008.07.055. [DOI] [PubMed] [Google Scholar]
- 349.McEwen B.S., Kalia M. The role of corticosteroids and stress in chronic pain conditions. Metabolism. 2010;59(Suppl. 1):S9–S15. doi: 10.1016/j.metabol.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 350.Vargas-Alarcon G., Alvarez-Leon E., Fragoso J.M., Vargas A., Martinez A., Vallejo M., Martinez-Lavin M. A SCN9A gene-encoded dorsal root ganglia sodium channel polymorphism associated with severe fibromyalgia. BMC Musculoskelet. Disord. 2012;13:23. doi: 10.1186/1471-2474-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Bennett G.J. Update on the neurophysiology of pain transmission and modulation: focus on the NMDA-receptor. J. Pain Symptom Manage. 2000;19(1) Suppl.:S2–S6. doi: 10.1016/S0885-3924(99)00120-7. [DOI] [PubMed] [Google Scholar]
- 352.Luo Z.D., Cizkova D. The role of nitric oxide in nociception. Curr. Rev. Pain. 2000;4(6):459–466. doi: 10.1007/s11916-000-0070-y. [DOI] [PubMed] [Google Scholar]
- 353.Johnson C. 2014. Fibromyalgia: A brain disorder? [Google Scholar]
- 354.Melzack R. The McGill Pain Questionnaire: Major properties and scoring methods. Pain . 1975;1:277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 355.Niblett S.H., King K.E., Dunstan R.H., Clifton-Bligh P., Hoskin L.A., Roberts T.K., Fulcher G.R., McGregor N.R., Dunsmore J.C., Butt H.L., Klineberg I., Rothkirch T.B. Hematologic and urinary excretion anomalies in patients with chronic fatigue syndrome. Exp. Biol. Med. (Maywood) 2007;232(8):1041–1049. doi: 10.3181/0702-RM-44. [DOI] [PubMed] [Google Scholar]
- 356.Booth N.E., Myhill S., McLaren-Howard J. Mitochondrial dysfunction and the pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Int. J. Clin. Exp. Med. 2012;5(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 357.Ciregia F., Giusti L., Da Valle Y., Donadio E., Consensi A., Giacomelli C., Sernissi F., Scarpellini P., Maggi F., Lucacchini A., Bazzichi L. A multidisciplinary approach to study a couple of monozygotic twins discordant for the chronic fatigue syndrome: a focus on potential salivary biomarkers. J. Transl. Med. 2013;11:243. doi: 10.1186/1479-5876-11-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Keller D.M. Many Fibromyalgia patients have small-fiber polyneuropahty. [Online] 2012. http://www.medscape.com/ viewarticle/772864?src=smo_neuro [Accessed on: 10/28/2012]. 2012.
- 359.Oaklander A.L., Herzog Z.D., Downs H.M., Klein M.M. Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Pain. 2013;154(11):2310–2316. doi: 10.1016/j.pain.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Serra J., Collado A., Solà R., Antonelli F., Torres X., Salgueiro M., Quiles C., Bostock H. Hyperexcitable C nociceptors in fibromyalgia. Ann. Neurol. 2014;75(2):196–208. doi: 10.1002/ana.24065. [DOI] [PubMed] [Google Scholar]
- 361.Üçeyler N., Zeller D., Kahn A.K., Kewenig S., Kittel-Schneider S., Schmid A., Casanova-Molla J., Reiners K., Sommer C. Small fibre pathology in patients with fibromyalgia syndrome. Brain. 2013;136(Pt 6):1857–1867. doi: 10.1093/brain/awt053. [DOI] [PubMed] [Google Scholar]
- 362.Chalaye P., Lafrenaye S., Goffaux P., Marchand S. The role of cardiovascular activity in fibromyalgia and conditioned pain modulation. 2014. [DOI] [PubMed]
- 363.Napadow V., Kim J., Clauw D.J., Harris R.E. Decreased intrinsic brain connectivity is associated with reduced clinical pain in fibromyalgia. Arthritis Rheum. 2012;64(7):2398–2403. doi: 10.1002/art.34412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Pujol J., Macià D., Garcia-Fontanals A., Blanco-Hinojo L., López-Solà M., Garcia-Blanco S., Poca-Dias V., Harrison B.J., Contreras-Rodríguez O., Monfort J., Garcia-Fructuoso F., Deus J. The contribution of sensory system functional connectivity reduction to clinical pain in fibromyalgia. Pain. 2014;155(8):1492–1503. doi: 10.1016/j.pain.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 365.Hargrove J.B., Bennett R.M., Simons D.G., Smith S.J., Nagpal S., Deering D.E. Quantitative electroencephalographic abnormalities in fibromyalgia patients. Clin. EEG Neurosci. 2010;41(3):132–139. doi: 10.1177/155005941004100305. [DOI] [PubMed] [Google Scholar]
- 366.Fuster J.M. The Prefrontal Cortex. Elsevier; 2009. [DOI] [Google Scholar]
- 367.Rohani R., Piryaei A., Jahanshahi A., Sadeghi Y., Mirnajafi-Zadeh J. Effect of low-frequency stimulation on kindling induced changes in rat dentate gyrus: an ultrastructural study. Acta Neurol. Belg. 2014;114(1):47–53. doi: 10.1007/s13760-013-0243-1. [DOI] [PubMed] [Google Scholar]
- 368.Tupal S., Faingold C.L. The amygdala to periaqueductal gray pathway: plastic changes induced by audiogenic kindling and reversal by gabapentin. Brain Res. 2012;1475:71–79. doi: 10.1016/j.brainres.2012.07.044. [DOI] [PubMed] [Google Scholar]
- 369.Tomoda A., Mizuno K., Murayama N., Joudoi T., Igasaki T., Miyazaki M., Miike T. Event-related potentials in Japanese childhood chronic fatigue syndrome. J. Pediatr. Neurol. 2007;5:199–208. [Google Scholar]
- 370.Johnston S., Brenu E.W., Staines D.R., Marshall-Gradisnik S. The adoption of chronic fatigue syndrome/myalgic encephalomyelitis case definitions to assess prevalence: A systematic review. . Ann. Epidemiol. . 2013;23(6):371–376. doi: 10.1016/j.annepidem.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 371.Fischer D.B., William A.H., Strauss A.C., Unger E.R., Jason L., Marshall G.D., Jr, Dimitrakoff J.D. Chronic Fatigue Syndrome: The Current Status and Future Potentials of Emerging Biomarkers. Fatigue. 2014;2(2):93–109. doi: 10.1080/21641846.2014.906066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Johnston S., Brenu E.W., Staines D., Marshall-Gradisnik S. The prevalence of chronic fatigue syndrome/ myalgic encephalomyelitis: a meta-analysis. Clin. Epidemiol. 2013;5:105–110. doi: 10.2147/CLEP.S39876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Holmes G.P., Kaplan J.E., Gantz N.M., Komaroff A.L., Schonberger L.B., Straus S.E., Jones J.F., Dubois R.E., Cunningham-Rundles C., Pahwa S., et al. Chronic fatigue syndrome: a working case definition. Ann. Intern. Med. 1988;108(3):387–389. doi: 10.7326/0003-4819-108-3-387. [DOI] [PubMed] [Google Scholar]
- 374.Ali I., O’Brien P., Kumar G., Zheng T., Jones N.C., Pinault D., French C., Morris M.J., Salzberg M.R., O’Brien T.J. Enduring Effects of Early Life Stress on Firing Patterns of Hippocampal and Thalamocortical Neurons in Rats: Implications for Limbic Epilepsy. PLoS One. 2013;8(6):e66962. doi: 10.1371/journal.pone.0066962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Xue T., Yuan K., Zhao L., Yu D., Zhao L., Dong T., Cheng P., von Deneen K.M., Qin W., Tian J. Intrinsic brain network abnormalities in migraines without aura revealed in resting-state fMRI. PLoS One. 2012;7(12):e52927. doi: 10.1371/journal.pone.0052927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Xu Z., Wang Y., Jin M., Yue J., Xu C., Ying X., Wu D., Zhang S., Chen Z. Polarity-dependent effect of low-frequency stimulation on amygdaloid kindling in rats. Brain Stimulat. 2013;6(2):190–197. doi: 10.1016/j.brs.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 377.Smith M.A., Weiss S.R., Abedin T., Kim H., Post R.M., Gold P.W. Effects of amygdala kindling and electroconvulsive seizures on the expression of corticotropin-releasing hormone in the rat brain. Mol. Cell. Neurosci. 1991;2(2):103–116. doi: 10.1016/1044-7431(91)90002-6. [DOI] [PubMed] [Google Scholar]
- 378.Botterill J.J., Fournier N.M., Guskjolen A.J., Lussier A.L., Marks W.N., Kalynchuk L.E. Amygdala kindling disrupts trace and delay fear conditioning with parallel changes in Fos protein expression throughout the limbic brain. Neuroscience. 2014;265:158–171. doi: 10.1016/j.neuroscience.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 379.Beheshti Nasr S.M., Moghimi A., Mohammad-Zadeh M., Shamsizadeh A., Noorbakhsh S.M. The effect of minocycline on seizures induced by amygdala kindling in rats. Seizure. 2013;22(8):670–674. doi: 10.1016/j.seizure.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 380.Ninomiya S., Esumi S., Ohta K., Fukuda T., Ito T., Imayoshi I., Kageyama R., Ikeda T., Itohara S., Tamamaki N. Amygdala kindling induces nestin expression in the leptomeninges of the neocortex. Neurosci. Res. 2013;75(2):121–129. doi: 10.1016/j.neures.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 381.Chiang S., Haneef Z. Graph theory findings in the pathophysiology of temporal lobe epilepsy. Clin. Neurophysiol. 2014;125(7):1295–1305. doi: 10.1016/j.clinph.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Lee S.S., Murata R., Matsuura S. Developmental study of hippocampal kindling. Epilepsia. 1989;30(3):266–270. doi: 10.1111/j.1528-1157.1989.tb05297.x. [DOI] [PubMed] [Google Scholar]
- 383.Rosenkranz J.A., Venheim E.R., Padival M. Chronic stress causes amygdala hyperexcitability in rodents. 2010. [DOI] [PMC free article] [PubMed]
- 384.Arnsten A.F. Stress signalling pathways that impair prefrontal cortex structure and function. Nat. Rev. Neurosci. 2009;10(6):410–422. doi: 10.1038/nrn2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Sapolsky R.M. Stress hormones: good and bad. Neurobiol. Dis. 2000;7(5):540–542. doi: 10.1006/nbdi.2000.0350. [DOI] [PubMed] [Google Scholar]
- 386.Sapolsky R.M. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch. Gen. Psychiatry. 2000;57(10):925–935. doi: 10.1001/archpsyc.57.10.925. [DOI] [PubMed] [Google Scholar]
- 387.LeDoux J. The emotional brain: The mysterious underpinnings of emotional life. New York: Simon & Schuster; 1998. [Google Scholar]
- 388.Gupta A. Unconscious amygdalar fear conditioning in a subset of chronic fatigue syndrome patients. Med. Hypotheses. 2002;59(6):727–735. doi: 10.1016/S0306-9877(02)00321-3. [DOI] [PubMed] [Google Scholar]
- 389.Sulheim D., Fagermoen E., Winger A., Andersen A.M., Godang K., Müller F., Rowe P.C., Saul J.P., Skovlund E., Øie M.G., Wyller V.B. Disease mechanisms and clonidine treatment in adolescent chronic fatigue syndrome: a combined cross-sectional and randomized clinical trial. JAMA Pediatr. 2014;168(4):351–360. doi: 10.1001/jamapediatrics.2013.4647. [DOI] [PubMed] [Google Scholar]
- 390.Walsh K.B., Teijaro J.R., Zuniga E.I., Welch M.J., Fremgen D.M., Blackburn S.D., von Tiehl K.F., Wherry E.J., Flavell R.A., Oldstone M.B. Toll-like receptor 7 is required for effective adaptive immune responses that prevent persistent virus infection. Cell Host Microbe. 2012;11(6):643–653. doi: 10.1016/j.chom.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Hooper P.L., Hightower L.E., Hooper P.L. Loss of stress response as a consequence of viral infection: implications for disease and therapy. Cell Stress Chaperones. 2012;17(6):647–655. doi: 10.1007/s12192-012-0352-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Agliari E., Barra A., Vidal K.G., Guerra F. Can persistent Epstein-Barr virus infection induce chronic fatigue syndrome as a Pavlov reflex of the immune response? J. Biol. Dyn. 2012;6(2):740–762. doi: 10.1080/17513758.2012.704083. [DOI] [PubMed] [Google Scholar]
- 393.Bachstetter A.D., Norris C.M., Sompol P., Wilcock D.M., Goulding D., Neltner J.H., St Clair D., Watterson D.M., Van Eldik L.J. Early stage drug treatment that normalizes proinflammatory cytokine production attenuates synaptic dysfunction in a mouse model that exhibits age-dependent progression of Alzheimer’s disease-related pathology. J. Neurosci. 2012;32(30):10201–10210. doi: 10.1523/JNEUROSCI.1496-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Rajeevan M.D., Dimulescu I., Murray U., Falkenberg V. R., Unger E.A. Pathway-focused genetic evaluation of immune and inflammation related genes with chronic fatigue syndrome. 2015. [DOI] [PubMed]
- 395.Jason L.A., Sunnquist M., Kot B., Brown A. Unintended consequences of not specifying exclusionary illnesses for Systemic Exertion Intolerance Disease. Diagnostics. 2015;5:272–286. doi: 10.3390/diagnostics5020272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Jason L.A., Sunnquist M., Brown A., Newton J.L., Strand E.B., Vernon S.D. Chronic fatigue syndrome versus Systemic Exertion Intolerance Disease. Fatigue: Biomed. Health Behav; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]


