Abstract
Ultrasound-guided renal access for percutaneous nephrolithotomy (PCNL) is a safe, effective, and low-cost procedure commonly performed worldwide, but a technique underutilized by urologists in the United States. The purpose of this article is to familiarize the practicing urologist with methods for ultrasound guidance for percutaneous renal access. We discuss two alternative techniques for gaining renal access for PCNL under ultrasound guidance. We also describe a novel technique of using the puncture needle to reposition residual stone fragments to avoid additional tract dilation. With appropriate training, ultrasound-guided renal access for PCNL can lead to reduced radiation exposure, accurate renal access, and excellent stone-free success rates and clinical outcomes.
Introduction
Ultrasound-guided caliceal puncture in percutaneous nephrolithotomy (PCNL) is a radiation-free and low-cost technique associated with high success rates among trained urologists.1–5 In the United States, however, the majority of urologists utilize fluoroscopy to obtain renal tract access.6 Advantages of ultrasound guidance over fluoroscopy include reduction of radiation exposure and financial cost, real-time imaging of the collecting system and renal parenchyma, detection of radiolucent stones, improved visualization of adjacent viscera, clearer delineation of the anterior and posterior calices, and the potential to avoid vascular injury with Doppler flow imaging.7 This technique is often the preferred method for percutaneous nephrostomy tube placement among interventional radiologists and has been safely applied in pregnant and pediatric patients for whom radiation exposure is a significant concern.1
While ultrasound-guided PCNL has been described in Asia and Europe, utilization in the United States has been limited. We present two approaches—transverse and longitudinal—for ultrasound-guided needle access into the collecting system for PCNL. We also present the novel use of ultrasound-guided needle puncture to reposition residual stone fragments into areas accessible through the initial renal access tract, sparing the patient from additional tract dilation and increasing procedural stone clearance rates through a single tract. With appropriate training and experience, urologists in a diversity of practice settings in the United States can implement these techniques.
Technique
Setup and ultrasound imaging
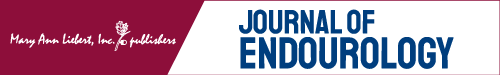
1. Before the procedure, collect preoperative urine for culture and sensitivities. Prior stone culture results may be helpful, if available, in the case of recurrent stone formers. Computed tomography imaging is often used to delineate renal and perirenal anatomy, as well as stone characteristics (Fig. 1). Administer preoperative antibiotics according to the institutional antibiotic guidelines.
2. Determine the method of anesthesia based on patient comorbidities. We find that general anesthesia with endotracheal intubation reduces movement and maximizes accuracy for instrument placement.
3. Position the patient in the supine or lithotomy position to facilitate placement of an externalized ureteral stent. This can be used intraoperatively for retrograde saline injection if caliceal dilation is needed.
4. After intubation, reposition the patient into the prone position.
-
5. Use a curved array ultrasound transducer in the 3.5 MHz range to visualize the renal parenchyma, collecting system, stones, and surrounding organs. As a general guideline, the depth of the ultrasound should be set to the 8–12 cm range. Selection of the actual depth should depend on maximizing the size of the kidney on the imaging screen. Gain should be set to the midrange so as to increase the contrast of the stone and needle against the collecting system and renal parenchyma to clearly visualize these points of interest. Areas of hyperechoic signal accompanied with postacoustic shadowing localize renal stones.
a. Doppler flow can facilitate visualization of vascular structures both within and surrounding the kidney.8 If the calices are difficult to visualize, gentle, active, or passive retrograde injection of saline through the externalized ureteral catheter can be done. While diuretic administration has been shown to transiently dilate the calices and improve access,1 we do not routinely administer diuretics for these cases.
6. Using ultrasonography, determine the target calix. The posterior calix is chosen in most instances, except when the stone is present in the otherwise inaccessible anterior calix.
FIG. 1.
Computed tomography (CT) scan demonstrating a large left kidney staghorn calculus.
Ultrasound-guided puncture in the longitudinal or transverse imaging planes (Step 7 or 8)
-
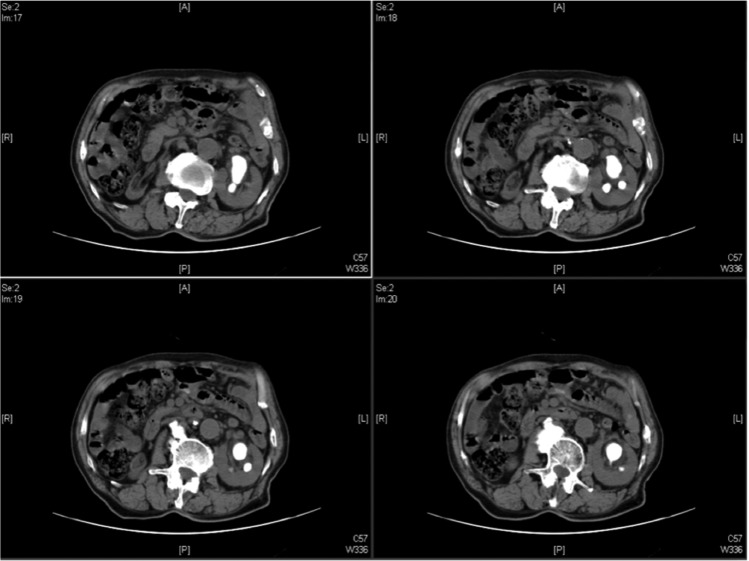
7. Longitudinal needle insertion (Fig. 2)
a. Using an 18- to 24-gauge needle with an echogenic tip, puncture the skin either in front of or behind the probe such that it travels parallel to the long axis of the probe (Fig. 2A).
b. Keeping the entire needle fully visualized from skin to kidney (Fig. 2F, white arrow), direct the tip of the needle into the end of the chosen calix (Fig. 2B, yellow dots; Fig. 2C). Close coordination between the hand holding the ultrasound probe (to maintain good visualization of the caliceal target) and the hand holding the needle (to bring the needle into the imaging plane) is required Fig. 2D,E. Ultrasonographic imaging can be used to avoid puncturing the surrounding viscera, such as the colon, spleen, and liver. Doppler signal can be used to identify blood vessels to avoid them within the kidney as well.
c. Avoid skin entry with the needle at too oblique an angle, which can make subsequent dilation and access more challenging. This is particularly relevant in lower pole access, in which oblique needle insertion from the caudal position behind the probe can result in the nephroscope abutting the patient's iliac crest (Fig. 2D).
-
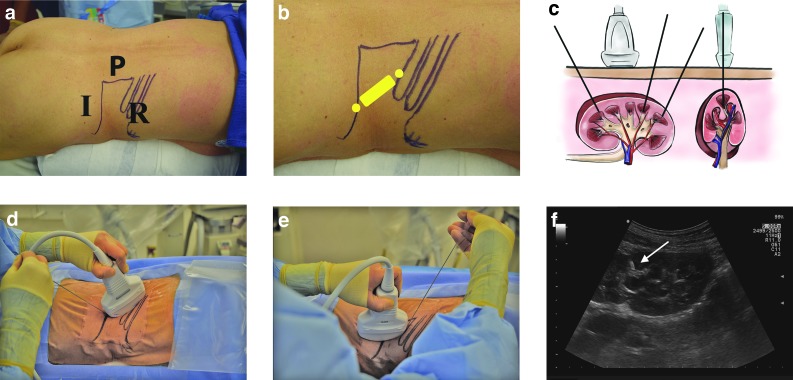
8. Transverse needle insertion (Fig. 3)
a. Using the access needle, puncture the skin orthogonal to the long axis of the probe (Fig. 3B).
b. Continuously sweep the probe back and forth to visualize the needle path and guide the needle tip to the target calix (Fig. 3C). Similar to the longitudinal needle insertion technique, ultrasonographic imaging can be used to avoid puncturing the surrounding viscera and blood vessels.
c. Avoid the surrounding viscera, such as the colon, spleen, and liver. Doppler signal can be used.
d. The needle can be inserted into the skin at any distance from the side of the ultrasound probe (Fig. 3C,D), allowing a greater range in the angle of entry and avoiding rib shadowing.
FIG. 2.
The longitudinal approach to renal access. (a) Anatomical landmarks used for percutaneous nephrolithotomy in the prone position. (P marks the paraspinous muscle, I the iliac crest, and R the 12th rib). (b) Image demonstrates a common placement for the ultrasound probe (yellow rectangle) oriented along the longitudinal axis of the kidney. In this illustration, the probe is placed below the 12th rib and must be tilted cephalad to image the kidney. In some cases, placing the probe above the 12th rib or higher may be necessary to achieve appropriate renal access. Two potential sites of needle entrance are marked with the yellow dots. (c) Schematic drawing of the coronal and axial views of the needle approach with the ultrasound probe positioned along the longitudinal axis of the kidney. A needle (represented by the black lines) can be inserted into a posterior calix of choice with the path of insertion in full view of the imaging plane. (d) Intraoperative image of a needle puncture through the lower pole. The nondominant hand holds the ultrasound probe, while the dominant hand holds the needle. (e) Intraoperative image of a needle puncture through the upper pole. (f) Ultrasonographic image of the kidney along its longitudinal axis demonstrating that the needle (white arrow) can be imaged along its entire insertion path as it enters the renal calix.
FIG. 3.
The transverse approach to renal access. (a) Anatomical landmarks are again presented for percutaneous nephrolithotomy in the prone position (P marks the paraspinous muscle, I the iliac crest, and R the 12th rib). (b) Image demonstrates how the ultrasound probe (yellow rectangular) is oriented along the transverse axis of the kidney for the transverse needle insertion technique. Two potential points of entry for the needle are marked by yellow dots. The location of the probe along the kidney axis and of the needle insertion relative to the probe head can change depending on the desired calix of entry and the patient's anatomy. (c) Schematic drawing of the coronal and axial views of the needle approach with the ultrasound probe positioned along the transverse axis of the kidney. A needle (represented by the black lines) can be inserted into a posterior calix of choice while ultrasound imaging shows the needle in cross section as a single echogenic point. (d) Intraoperative photographs demonstrate typical hand positions for the transverse needle insertion technique. The nondominant hand holds the ultrasound probe, while the dominant hand holds the needle. The needle can enter the patient's body from any distance to the head of the probe. In this picture, the needle is advanced from the back of the probe. (e) Intraoperative image of a transverse needle puncture where the needle is inserted from in front of the probe. The choice of insertion site depends on the desired angle of entry into the kidney calix of choice. (f) Ultrasonographic image of the kidney along its transverse axis demonstrates how the needle tip (white arrow) is imaged as it enters the renal calix. The probe is swept back and forth to keep the needle tip in view as it is inserted into the kidney.
Tract dilation
9. Tract dilation can be performed under ultrasonographic or fluoroscopic guidance, depending on the surgeon's comfort level with each imaging modality.
10. Once caliceal entry with the access needle is confirmed, remove the needle stylet and advance a guidewire into the collecting system through the needle and create a 1-cm skin incision surrounding the wire. We routinely use a J-tipped coaxial guidewire for maintenance of access and for dilation, although selection of the wire type will vary depending on the surgeon's preference.
11. Dilate the tract with a 10F fascial dilator, followed by a safety wire introducer. Through the safety wire introducer, insert a second coaxial guidewire into the collecting system and remove the introducer. Secure the safety wire to the drapes. Use either a serial dilator system or a balloon dilator for further fascial dilation, and position the access sheath for entry into the collecting system over the guidewire.
12. An offset rigid nephroscope and lithotripter device can be used for stone fragmentation and removal.
13. After stone removal, a nephrostomy tube and/or ureteral stent can be placed for renal drainage as clinically indicated.
Ultrasound-guided needle repositioning of residual stone
1. Intraoperative imaging may reveal the residual stone in an inaccessible location from the initial access tract, often due to the sharp angle of the infundibulum used for access relative to the residual stone location.
2. Under ultrasound guidance, insert a 24-gauge percutaneous renal access needle into the calix containing the residual stone.
3. Use the needle tip to dislodge the stone from the lower calix and push it into the renal pelvis, where it can be accessed, fragmented, and removed through the original access tract (Supplementary Video S1; Supplementary Data are available online at www.liebertpub.com/end).
Equipment
1. Ultrasound with transducer in the 3.5 MHz range
2. Eighteen- to 24-gauge needle with an echogenic tip
3. J-tipped coaxial guidewires
4. Fascial dilators
5. Safety wire introducer
6. Access tract serial or balloon dilator set with sheath
7. C-arm with omnipaque if needed for tract dilation
8. Rigid nephroscope and lithotripter device for lithotripsy
9. Nephrostomy tube or stent as clinically indicated
Role in Urologic Practice
Indications and contraindications for ultrasound-guided renal access are similar to fluoroscopic renal access. Ultrasound-guided renal access can be used for a range of stone configurations, including single pelvic or caliceal stones, renal units containing multiple stones, or staghorn calculi. Ultrasound guidance is preferred in special populations such as children and pregnant women to minimize radiation exposure. While the presence of hydronephrosis may facilitate ultrasonographic renal imaging, it is not required for efficient needle puncture.
Difficulty with needle visualization by ultrasound carries a risk of inaccurate needle placement and perforation of the surrounding viscera and vasculature. Published literature shows that the most common complications of ultrasound-guided PCNL by urologists are urinary-tract infection (1.1%), hemorrhage (1.9%), sepsis (0.76%), inferior vena cava injury (0.15%), gallbladder injury (0.15%), and death (0.3%).8 Major complications occurred in 3.3% of patients and minor complications in 5%.8 Multiple studies have demonstrated no difference in hospital stay, stone-free rates, or postoperative complication rates between patients who undergo ultrasound- versus fluoroscopy-guided renal tract access for PCNL.4,9 One case-matched study comparing outcomes of ultrasound- and fluoroscopy-guided PCNL in 5806 patients found that postoperative hemorrhage and blood transfusion rates were significantly higher in the fluoroscopy group (11.1% vs 3.8%, p = 0.001), although they noted the use of larger access sheaths in the fluoroscopy group (22.6F vs 29.5F, p < −0.001) and longer hospital stays in the ultrasound group (5.3 vs 3.5 days, p < 0.001).10
Utilizing ultrasound to achieve percutaneous renal access for PCNL has been established as safe and effective, with excellent clinical outcomes. Used in combination, ultrasound and fluoroscopy during PCNL can achieve comparable clinical outcomes and stone-free rates relative to fluoroscopy alone.11,12 A randomized prospective trial comparing outcomes of ultrasound-guided PCNL access to traditional fluoroscopic access in 224 patients demonstrated increased accuracy of puncture, fewer number of puncture attempts, shorter operative time, and reduced radiation exposure time, with similar rates of procedural success and length of hospital stay for the ultrasound group.7 In another study, urology residents undergoing PCNL training were able to achieve decreased radiation exposure time and higher accuracy of puncture for pure ultrasound-guided PCNL, although 6 of 32 patients required fluoroscopic adjustment.12 In a single-center study of 700 patients who underwent complete ultrasound-guided PCNL in China, 92.6% of patients with a single calculus and 82.9% of patients with staghorn or multiple stones were rendered stone free.13 In comparison, fluoroscopy-guided PCNL resulted in a 98.5% clearance rate for a solitary stone and 71% for complex staghorn stones in another study.14
In this study, we describe two methods for ultrasound-guided renal access during PCNL, which can be implemented in most operating rooms in the United States. While a learning curve exists to master these techniques, their adoption may lead to reduced radiation exposure for patients, urologists, and ancillary health providers when performing PCNL. Using an access needle to reposition residual stone(s) into an accessible calix is a novel application of ultrasound during PCNL. This technique presumes that the stone being repositioned is small enough to pass through the infundibulum to an accessible area of the kidney, such as the renal pelvis. Flexible nephroscopy and laser lithotripsy through the initial tract remain our first-line approach to reaching residual stone fragments. However, needle repositioning may be helpful when the angle of the calix harboring the residual stone is too sharp from the access tract of entry for a flexible nephroscope to navigate. However, there are potential risks to applying this technique. New needle punctures carry a small risk of infection, bleeding, and tissue injury and should only be attempted in cases where a stone is amenable to safe displacement. However, a primary advantage of this technique is that it may help the surgeon avoid the morbidity associated with dilation of multiple renal access tracts.11,15,16 Ultrasound-guided stone repositioning may be a pragmatic and safe strategy for patients undergoing PCNL and merits future study.
There are advantages and disadvantages to both the transverse and longitudinal approaches for ultrasound-guided percutaneous renal access. With the longitudinal needle technique, the trajectory of the needle can be fully visualized. However, the needle must be perfectly aligned with the plane of ultrasound imaging. This can be challenging particularly when the skin-to-stone distance is long. Failure to image the needle tip can result in inadvertent injury to the surrounding structures. In the longitudinal approach, the needle sometimes enters the skin at an oblique angle, which may make subsequent tract dilation and lithotripsy more challenging. In the transverse approach, the needle can enter the skin at a greater range of distances from the probe head and angles to the skin. Thus, rib shadowing is more easily avoided. However, then the needle is never fully visualized and the operator must adjust the imaging plane constantly to coordinate with needle advancement. These advantages and disadvantages should dictate the use of each technique specific for the patient's body habitus, renal anatomy, and stone location.
The importance of reducing radiation exposure should not be underestimated, both for the physician as well as the patient. Over the course of their careers, urologists may be exposed to radiation on a regular and cumulative basis,17,18 and patients with recurrent stones may be subjected to repeated radiation exposure during evaluation and subsequent procedures.19–21 This is particularly relevant in younger patients as radiation exposure is correlated with increased risk for malignancy over time.22 Replacing fluoroscopy with ultrasound for renal access, as well as for stone repositioning, may mitigate these healthcare risks.
Supplementary Material
Abbreviation Used
- PCNL
percutaneous nephrolithotomy
Acknowledgments
The authors thank Catherine Tsai for providing the medical illustrations used in Figures 2 and 3. Funding source: K12-DK-07-006: Multidisciplinary K12 Urologic Research Career Development Program (TC).
Author Disclosure Statement
The authors declare no conflicts of interest.
References
- 1.Lojanapiwat B. The ideal puncture approach for PCNL: Fluoroscopy, ultrasound or endoscopy? Indian J Urol 2013;29:208–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basiri A, Ziaee AM, Kianian HR, Mehrabi S, Karami H, Moghaddam SMH. Ultrasonographic versus fluoroscopic access for percutaneous nephrolithotomy: A randomized clinical trial. J Endourol 2008;22:281–284 [DOI] [PubMed] [Google Scholar]
- 3.Chi Q, Wang Y, Lu J, Wang X, Hao Y, Lu Z, et al. . Ultrasonography combined with fluoroscopy for percutaneous nephrolithotomy: An analysis based on seven years single center experiences. Urol J 2014;11:1216–1221 [PubMed] [Google Scholar]
- 4.Karami H, Rezaei A, Mohammadhosseini M, Javanmard B, Mazloomfard M, Lotfi B. Ultrasonography-guided percutaneous nephrolithotomy in the flank position versus fluoroscopy-guided percutaneous nephrolithotomy in the prone position: A comparative study. J Endourol 2010;24:1357–1361 [DOI] [PubMed] [Google Scholar]
- 5.Karami H, Arbab AHMM, Rezaei A, Mohammadhoseini M, Rezaei I. Percutaneous nephrolithotomy with ultrasonography-guided renal access in the lateral decubitus flank position. J Endourol 2009;23:33–36 [DOI] [PubMed] [Google Scholar]
- 6.Miller NL, Matlaga BR, Lingeman JE. Techniques for fluoroscopic percutaneous renal access. J Urol 2007;178:15–23 [DOI] [PubMed] [Google Scholar]
- 7.Agarwal M, Agrawal MS, Jaiswal A, Kumar D, Yadav H, Lavania P. Safety and efficacy of ultrasonography as an adjunct to fluoroscopy for renal access in percutaneous nephrolithotomy (PCNL). BJU Int 2011;108:1346–1349 [DOI] [PubMed] [Google Scholar]
- 8.Fulgham PF, Gilbert BR. Practical Urological Ultrasound. New York: Springer, 2013, pp. 47–70. [Google Scholar]
- 9.Zhou X, Gao X, Wen J, Xiao C. Clinical value of minimally invasive percutaneous nephrolithotomy in the supine position under the guidance of real-time ultrasound: Report of 92 cases. Urol Res 2008;36:111–114 [DOI] [PubMed] [Google Scholar]
- 10.Andonian S, Scoffone CM, Louie MK, Gross AJ, Grabe M, Daels FP, et al. . Does imaging modality used for percutaneous renal access make a difference? A matched case analysis. J Endourol 2013;27:24–28 [DOI] [PubMed] [Google Scholar]
- 11.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol 2007;51:899–906 [DOI] [PubMed] [Google Scholar]
- 12.Jagtap J, Mishra S, Bhattu A, Ganpule A, Sabnis R, Desai MR. Which is the preferred modality of renal access for a trainee urologist: Ultrasonography or fluoroscopy? Results of a prospective randomized trial. J Endourol 2014;28:1464–1469 [DOI] [PubMed] [Google Scholar]
- 13.Yan S, Xiang F, Yongsheng S. Percutaneous nephrolithotomy guided solely by ultrasonography: A 5-year study of >700 cases. BJU Int 2013;112:965–971 [DOI] [PubMed] [Google Scholar]
- 14.Chibber P. Percutaneous nephrolithotomy for large and staghorn calculi. J Endourol 1993;7:293–295 [DOI] [PubMed] [Google Scholar]
- 15.Ganpule AP, Desai M. Management of the staghorn calculus: Multiple-tract versus single-tract percutaneous nephrolithotomy. Curr Opin Urol 2008;18:220–223 [DOI] [PubMed] [Google Scholar]
- 16.Muslumanoglu AY, Tefekli A, Karadag MA, Tok A, Sari E, Berberoglu Y. Impact of percutaneous access point number and location on complication and success rates in percutaneous nephrolithotomy. Urol Int 2006;77:340–346 [DOI] [PubMed] [Google Scholar]
- 17.Bush W, Brannen G, Gibbons R, Correa R, Jr., Elder J. Radiation exposure to patient and urologist during percutaneous nephrostolithotomy. J Urol 1984;132:1148–1152 [DOI] [PubMed] [Google Scholar]
- 18.Hellawell GO, Mutch SJ, Thevendran G, Wells E, Morgan RJ. Radiation exposure and the urologist: What are the risks? J Urol 2005;174:948–952 [DOI] [PubMed] [Google Scholar]
- 19.Ferrandino MN, Bagrodia A, Pierre SA, Scales CD, Jr., Rampersaud E, Pearle MS, et al. . Radiation exposure in the acute and short-term management of urolithiasis at 2 academic centers. J Urol 2009;181:668–673 [DOI] [PubMed] [Google Scholar]
- 20.Fahmy NM, Elkoushy MA, Andonian S. Effective radiation exposure in evaluation and follow-up of patients with urolithiasis. Urology 2012;79:43–47 [DOI] [PubMed] [Google Scholar]
- 21.Jellison FC, Smith JC, Heldt JP, Spengler NM, Nicolay LI, Ruckle HC, et al. . Effect of low dose radiation computerized tomography protocols on distal ureteral calculus detection. J Urol 2009;182:2762–2767 [DOI] [PubMed] [Google Scholar]
- 22.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. National Research Council of the National Academies. The National Academies Press. Washington, DC, 2006. http://www.nap.edu/read/11340/chapter/1#iii [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.