Abstract
Findings regarding the protective effect of social role functioning on suicide ideation in individuals with schizophrenia have been mixed. One reason for such inconsistencies in the literature may be that individuals with prominent negative symptoms of schizophrenia may not experience a desire for social closeness, and therefore social role functioning may not influence suicide risk in these individuals. The aim of this study was to examine the moderating effects of self-reported desire for social closeness and interviewer-rated negative symptoms on the relationship between social role functioning and suicide ideation. Our sample consisted of 162 individuals who had been diagnosed with schizophrenia-spectrum disorders; all participants completed self-report questionnaires and clinician-administered interviews, and moderation hypotheses were tested with a non-parametric procedure. The results indicated that motivation and pleasure-related negative symptoms moderated the relationship between social role functioning and suicide ideation; self-reported desire for social closeness and negative symptoms related to expression did not have such a moderating effect. Specifically, better social role functioning was associated with less suicide ideation only in those individuals who had low motivation and pleasure-related negative symptoms; no significant relationship was observed between social role functioning and suicide ideation among those with elevated motivation and pleasure-related negative symptoms. These findings suggest that assessing for negative symptoms and social role functioning may inform suicide risk assessments in individuals with schizophrenia, and improving social role functioning may reduce suicide ideation among those with few motivation and pleasure-related negative symptoms.
Keywords: Social anhedonia, Social closeness, Belonging, Moderation, Protective factors
1. Introduction
Suicide is a significant public health problem and ranks as the 10th leading cause of death in the United States, with a rate of approximately 13 deaths per 100,000 people (Centers for Disease Control and Prevention, 2015). Among individuals with schizophrenia, risk for death by suicide is substantially higher than the general population (Hawton et al., 2005); research suggests that individuals with schizophrenia are at nearly 13 times higher risk for suicide than individuals without schizophrenia (Bushe et al., 2010), suggesting that it is critical to characterize risk factors for suicide among individuals with schizophrenia. One important and common risk factor for death by suicide among individuals with schizophrenia is suicide ideation (Hor and Taylor, 2010; Kasckow et al., 2010; Montross et al., 2005). Because of its proximal nature as a risk factor for death by suicide, suicide ideation is often used as an outcome in studies of suicide risk among individuals with schizophrenia (e.g., Kasckow et al., 2014; Yan et al., 2013).
Therefore, it is essential to identify variables that are associated with suicide ideation, as such variables can possibly be targeted to reduce suicide risk. One set of variables that has been linked to suicide risk in individuals with schizophrenia, as well as other populations, can be characterized as social functioning (e.g., poor or unstable social support, social isolation, and withdrawal from others; Balhara and Verma, 2012; Caldwell and Gottesman, 1992; Heila et al., 1999; Koeda et al., 2012; Lyu and Zhang, 2014; Saarinen et al., 1999). The assumption in studies of social functioning and suicide risk appears to be that individuals desire social support, and when this desire is not met, suicide ideation may be elevated. The interpersonal theory of suicide (Joiner, 2005) indicates that a sense of thwarted belongingness (i.e., lack of reciprocal caring relationships and belonging with valued others) is a proximal risk factor for suicide. Variables such as social isolation and size of social network are indicators of thwarted belongingness, which leads to suicide ideation (Joiner, 2005; Van Orden et al., 2010).
Individuals with prominent negative symptoms of schizophrenia may not experience this desire for social belonging and closeness (Kring et al., 2013). Social anhedonia is a core negative symptom of schizophrenia (Blanchard et al., 2011; Horan et al., 2006) that it is consistently elevated in clinical samples (Blanchard et al., 1998) and is stable across time and psychiatric symptom status (Blanchard et al., 2001). Importantly, Kring et al. (2013) found that individuals with experiential deficits in motivation and pleasure were less likely to endorse a desire for close relationships and social engagement. Moreover, multiple studies have identified a positive correlation between negative symptoms (assessed broadly through the negative symptoms subscale of the Positive and Negative Syndrome Scale [Kay et al., 1986]) and suicide ideation (Tarrier et al., 2004; Umut et al., 2013; Yan et al., 2013). Though there have been mixed findings regarding the role of negative symptoms and risk for suicide attempts or death by suicide (e.g., Luckhoff et al., 2014; McGirr et al., 2006; Umut et al., 2013; Yan et al., 2013), the extant literature consistently provides evidence that negative symptoms may be an important consideration in risk for suicide ideation among individuals with schizophrenia.
As noted above, many studies have found relationships between social functioning and suicide risk in schizophrenia (e.g., Koeda et al., 2012; Lyu and Zhang, 2014). However, negative symptoms and related lack of desire for social closeness may provide an explanation for other studies that have not identified relationships between suicide risk and indicators of social support (e.g., positive evaluations of social role functioning, social support, recent loss; Gooding et al., 2013; Heila et al., 1999; Lopez-Morinigo et al., 2014; Yan et al., 2013). It could be that individual differences in negative symptoms and the desire for social affiliation explain prior inconsistent findings regarding social functioning and suicide ideation among individuals with schizophrenia. Individuals with schizophrenia who do not desire social closeness or who have elevated negative symptoms may not experience social support as a protective factor against suicide ideation. However, those with schizophrenia who desire social closeness or have few negative symptoms may find social support to be protective against suicide ideation, similar to individuals without schizophrenia. These interactions have not yet been investigated. Additionally, it is unclear whether self-reported desire for social closeness or interviewer-rated negative symptoms more globally may be more important in these interactions.
As is evident from the literature, social support and functioning can be defined in numerous ways. Of particular relevance to individuals with schizophrenia, social role functioning can be used to capture various aspects of social support, including frequency of interactions, size of network, and closeness of relationships (Goodman et al., 1993). Consequently, we hypothesized that self-reported desire for social closeness and interviewer-rated negative symptoms would each moderate the relationship between social role functioning and suicide ideation in a sample of adults with schizophrenia. We expected that clinician-rated negative symptoms would show a stronger effect, as negative symptoms may affect social functioning more globally and would be less reliant on participant insight. Additionally, we anticipated that this interaction would indicate that those who valued social closeness or had few negative symptoms and had good social role functioning would endorse the lowest levels of suicide ideation; however, we anticipated that social role functioning would not significantly influence suicide ideation among those who did not value social closeness or had elevated negative symptoms.
2. Methods
2.1 Participants
We utilized data from 162 participants diagnosed with schizophrenia or schizoaffective disorder (based on the Structured Clinical Interview for DSM-IV; First et al., 2001) collected as part of a larger study validating a new instrument for the assessment of negative symptoms (Kring et al., 2013); a complete description of the methods has been reported elsewhere (Kring et al., 2013; Reddy et al., 2014). The sample was 57.4% male, with a mean age of 46.84 (SD = 9.48, Range = 23-65). Participants were primarily Black/African-American (50.3%) or White/Caucasian (40.3%), and not married (73.5%). Most participants were not employed (76.4%), and about one-third of the sample resided in supervised living situations (19.2%) or transient/short-term housing (14.9%).
2.2 Measures
The 24-item expanded version of the Brief Psychiatric Rating Scale (BPRS; Overall and Gorham, 1962; Ventura et al., 1993) was used to measure clinical symptomatology. Items were rated by interviewers on a 7-point scale, ranging from “not reported” to “very severe,” based on symptom frequency and severity during the past week. For the current study, the BPRS suicidality item was used to assess suicide ideation. This item is rated based on the frequency and severity of reported thoughts of death or suicide, as well as suicidal intent and plans. Additionally, depression items, anxiety items, and the positive symptoms subscale (Kopelowicz et al., 2008) were used as covariates.
Social role functioning was assessed with the Role Functioning Scale (RFS; Goodman et al., 1993), a four-item clinical interview that has been found to provide reliable and valid assessments of patient role functioning (e.g., Edmondson et al., 2012; Yamada et al., 2010). In the present analysis, we summed items assessing functioning in family relationships and functioning in friendships as our measure of social role functioning.
The Social Closeness Scale from the Multidimensional Personality Questionnaire (MPQ-SC; Tellegen and Waller, 2008) is a true-false self-report trait questionnaire used to measure desire for social affiliation. The 22-item MPQ-SC reflects the following characteristics: sociable, values close relationships, warm/affectionate, and welcomes support. The MPQ-SC has been shown to have high internal consistency (i.e., alphas above .80) and good convergent validity (Aday and Cornelius, 2006; Llerena et al., 2013).
The Clinical Assessment Interview for Negative Symptoms (CAINS; Kring et al., 2013) is a widely-used interview that was employed to assess negative symptoms in two domains: (1) expression and (2) motivation and pleasure (MAP). CAINS items are rated on a scale of 0 to 4 by an interviewer, and higher scores reflect greater impairment related to each negative symptom. The MAP subscale consisted of nine items (e.g., assessing expected and past-week pleasure derived from various activities, family relationships), whereas the expression subscale consisted of four items (e.g., assessing facial expression as well as speech characteristics). Cronbach’s alpha suggests strong internal consistency reliability, and correlations with related measures suggest good convergent and divergent validity (Kring et al., 2013).
2.3 Procedures
Participants were recruited from community mental health centers at four geographically diverse sites (see Kring et al., 2013 for a complete description). All participants provided informed consent and then completed self-report measures, clinical rating scales, and functional outcome assessments. Procedures were identical at all sites and were approved by each site’s institutional review board.
2.4 Data Analysis
Moderation was assessed with a nonparametric procedure using the PROCESS macro (Hayes, 2013) for SPSS (IBM Corporation, 2014), with the predictor and moderators centered prior to analyses. In the first analysis, social role functioning was entered as the predictor variable, suicide ideation was entered as the outcome variable, and desire for social closeness was entered as the moderator. In the second and third analyses, the predictor and outcome variables remained the same, and each negative symptom subscale score was entered as the moderator. Additionally, in all three analyses, depressive symptoms, anxiety symptoms, and positive symptoms of schizophrenia were entered as covariates, as each of these variables is a risk factor for suicide and was significantly correlated with suicide ideation (see Table 1). Parameters were set at 95% percentile-based confidence intervals (CIs). If the CI for the interaction term does not include zero, significant moderation is present.
Table 1.
Descriptive statistics and correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | --- | ||||||||
| 2. Depression | −.058 | --- | |||||||
| 3. Anxiety | −.058 | .420*** | --- | ||||||
| 4. Positive symptoms |
.063 | .265** | .290*** | --- | |||||
| 5. Social closeness |
.125 | −.045 | −.114 | −.124 | --- | ||||
| 6. Negative symptoms- MAP |
.065 | .173* | .037 | .304*** | −.263** | --- | |||
| 7. Negative symptoms- Express |
−.060 | .085 | .002 | .134 | −.113 | .249** | --- | ||
| 8. Social role functioning |
−.212** | −.039 | −.009 | −.272** | .154 | −.558*** | −.227** | --- | |
| 9. Suicide ideation |
−.019 | .300*** | .332*** | .256** | .002 | .004 | −.002 | − .089 |
--- |
|
| |||||||||
| Mean | 46.84 | 1.96 | 2.57 | 1.97 | 9.28 | 13.85 | 4.91 | 9.57 | 1.19 |
| SD | 9.48 | 1.26 | 1.39 | 0.81 | 2.80 | 6.40 | 3.63 | 2.97 | 0.50 |
Note: p < .05;
p < .01;
p < .001.
Depression measured by the Brief Psychiatric Rating Scale item 3; Anxiety measured by the Brief Psychiatric Rating Scale item 2; Positive symptoms measured by the Brief Psychiatric Rating Scale-Positive Symptoms subscale; Social closeness measured by the Multidimensional Personality Questionnaire-Social Closeness subscale; Negative symptoms-MAP measured by the Clinical Assessment Interview for Negative Symptoms-Motivation and Pleasure subscale; Negative symptoms-Express measured by the Clinical Assessment Interview for Negative Symptoms-Expression subscale; Social role functioning measured by the Role Functioning Scale sum of items 3 and 4; Suicide ideation measured by the Brief Psychiatric Rating Scale item 4. Social closeness, Negative symptoms, and Social role functioning correlations and descriptive statistics presented prior to centering for analyses.
3. Results
Descriptive statistics and bivariate zero-order correlations are presented in Table 1. Of note, the scores for the suicide ideation item ranged from not present (1) to moderate (4); no participants scored in the moderately severe (5), severe (6), or extremely severe (7) range. The average score was 1.19 (SD = 0.50), suggesting that the mean level of suicide ideation was low, but there was a range of severity present.
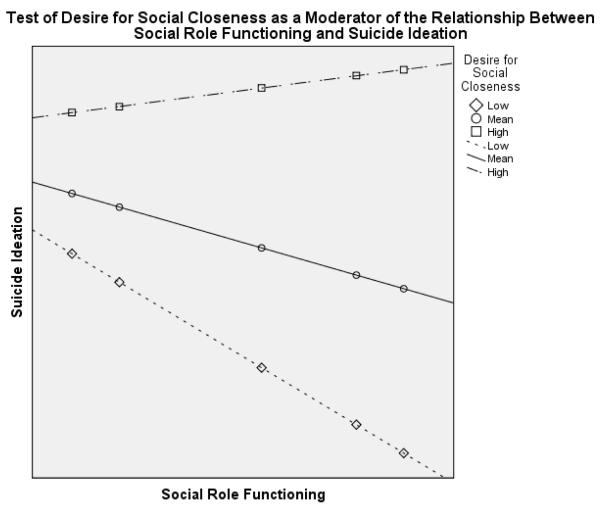
Results of the nonparametric procedure indicated that our hypotheses were partially supported. The model that tested self-reported desire for social closeness as a moderator was significant, R2 = .15, F(6, 144) = 4.35, p = .001. However, desire for social closeness did not moderate the relationship between social role functioning and suicide ideation in our sample (see Table 2); the interaction did not significantly add to the variance explained by the model, ΔR2 = .00, F(1, 144) = 0.04, p = .843 (see Figure 1 for plot of the interaction).
Table 2.
Nonparametric model results predicting suicide ideation
| Analysis | Predictor | Regression coefficient |
Standard error |
t | p | Lower limit of 95% CI |
Upper limit of 95% CI |
|---|---|---|---|---|---|---|---|
| 1 (MPQ-SC) | Constant | .758 | .097 | 7.796 | .000 | .566 | .950 |
| Depression | .052 | .032 | 1.646 | .102 | −.011 | .115 | |
| Anxiety | .075 | .028 | 2.712 | .008 | .020 | .129 | |
| Positive symptoms | .056 | .045 | 1.253 | .212 | −.033 | .145 | |
| Role functioning | −.002 | .011 | −.169 | .866 | −.024 | .020 | |
| Social closeness | .006 | .012 | .503 | .616 | −.017 | .029 | |
| Interaction | .001 | .004 | .199 | .843 | −.007 | .008 | |
| 2 (CAINS- MAP) |
Constant | .646 | .106 | 6.087 | .000 | .436 | .855 |
| Depression | .075 | .035 | 2.168 | .032 | .007 | .143 | |
| Anxiety | .070 | .030 | 2.342 | .021 | .011 | .129 | |
| Positive symptoms | .131 | .048 | 2.726 | .007 | .036 | .226 | |
| Role functioning | −.015 | .014 | −1.045 | .298 | −.042 | .013 | |
| Negative symptoms- MAP |
−.008 | .007 | −1.143 | .255 | −.021 | .006 | |
| Interaction | .004 | .002 | 2.417 | .017 | .001 | .007 | |
| 2 (CAINS- Express) |
Constant | .648 | .098 | 6.627 | .000 | .455 | .842 |
| Depression | .078 | .033 | 2.340 | .021 | .012 | .143 | |
| Anxiety | .068 | .028 | 2.421 | .017 | .012 | .123 | |
| Positive symptoms | .105 | .044 | 2.395 | .018 | .018 | .191 | |
| Role functioning | .001 | .012 | .070 | .945 | −.023 | .024 | |
| Negative symptoms- Express |
.001 | .010 | .063 | .950 | −.018 | .019 | |
| Interaction | −.001 | .003 | −.400 | .690 | −.007 | .005 |
Note: CI: Confidence interval. MPQ-SC: Multidimensional Personality Questionnaire-Social Closeness subscale. CAINS-MAP: Clinical Assessment Interview for Negative Symptoms-Motivation and Pleasure subscale. CAINS-Express: Clinical Assessment Interview for Negative Symptoms-Expression subscale. Suicide ideation measured by the Brief Psychiatric Rating Scale item 4; Depression measured by the Brief Psychiatric Rating Scale item 3; Anxiety measured by the Brief Psychiatric Rating Scale item 2; Positive symptoms measured by the Brief Psychiatric Rating Scale positive symptoms subscale; Role functioning measured by the Role Functioning Scale sum of items 3 and 4; Social closeness measured by the Multidimensional Personality Questionnaire-Social Closeness subscale; Negative symptoms-MAP measured by the Clinical Assessment Interview for Negative Symptoms-Motivation and Pleasure subscale; Negative symptoms-Express measured by the Clinical Assessment Interview for Negative Symptoms-Expression subscale. Interaction term is the multiplied effects of role functioning and social closeness (Analysis 1), motivation and pleasure-related negative symptoms (Analysis 2), or expression-related negative symptoms (Analysis 3).
Figure 1.
Effects of role functioning on suicide ideation plotted by low, average, and high desire for social closeness.
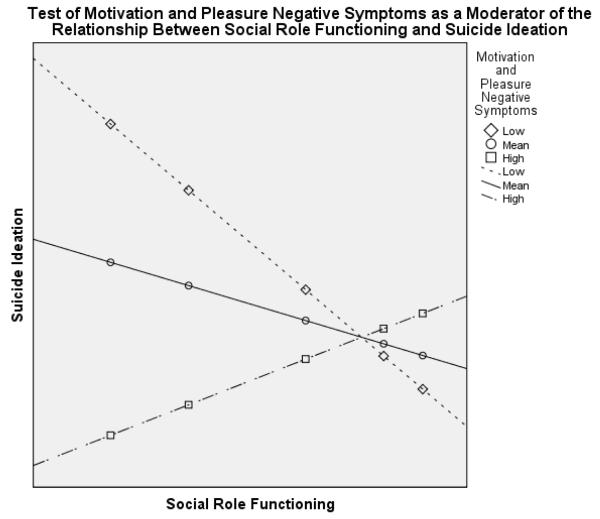
The model that tested motivation and pleasure-related negative symptoms as a moderator was also significant, R2 = .26, F(6, 130) = 7.77, p < .001. The interaction term added significantly to the predictive power of the model, ΔR2 = .03, F(1, 130) = 5.84, p = .017 (see Figure 2 for plot of the interaction), indicating that motivation and pleasure-related negative symptoms moderated the relationship between social role functioning and suicide ideation (see Table 2). The Johnson-Neyman technique indicated that the moderator was significant at CAINS-MAP scores below −5.22 (23.36% of all scores were below this cutoff, equivalent to 8.63 in non-centered scores), but not above this score (76.64% of scores), suggesting that social role functioning had a significant effect on suicide ideation when motivation and pleasure-related negative symptoms were low.
Figure 2.
Effects of role functioning on suicide ideation plotted by low, average, and high motivation and pleasure negative symptoms.
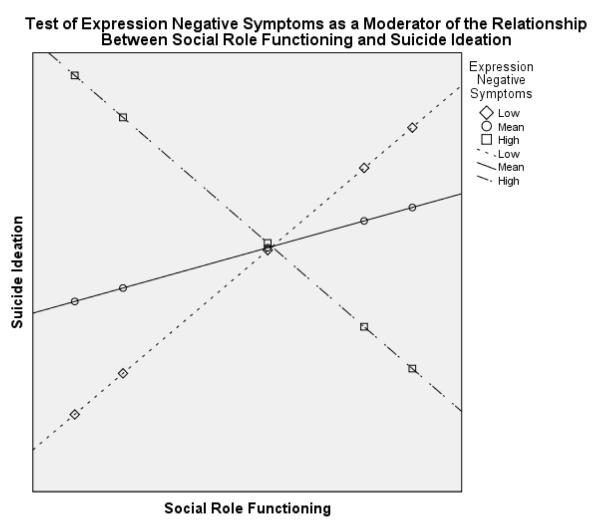
Finally, the model that tested expression-related negative symptoms as a moderator was significant, R2 = .21, F(6, 147) = 6.39, p < .001, though expression-related negative symptoms were not a significant moderator in this model (see Table 2), as the interaction term was not significant, ΔR2 = .00, F(1, 147) = 0.16, p = .690 (see Figure 3 for plot of the interaction).1
Figure 3.
Effects of role functioning on suicide ideation plotted by low, average, and high expression negative symptoms.
4. Discussion
The aim of this study was to identify whether self-reported desire for social closeness and interviewer-rated negative symptoms would influence the protective effect of social role functioning on suicide ideation in individuals with schizophrenia. The results of the current study suggest that better social role functioning was associated with less suicide ideation only in those individuals who had low motivation and pleasure-related negative symptoms. These findings were limited to motivation and pleasure-related negative symptoms, as the interaction of self-reported desire for social closeness and social role functioning was not significantly related to suicide ideation, nor was the interaction of expression-related negative symptoms and social role functioning. This is partially consistent with our original hypotheses, and lends credence to the rationale that insight into symptoms may influence self-ratings. This finding also suggests that broader negative symptoms, particularly those related to motivation and pleasure, may be important to consider in suicide risk, as opposed to self-reports of desire for social closeness or negative symptoms related to emotional expression.
This study adds context to prior reviews that have identified relationships between social support or isolation and risk for suicide among individuals with schizophrenia (e.g., Balhara and Verma, 2012; Caldwell and Gottesman, 1992). Unlike in previous studies (e.g., Tarrier et al., 2004; Umut et al., 2013; Yan et al., 2013), we did not find a significant relationship between negative symptoms and suicide ideation; however, we identified a significant interaction. Therefore, our findings fill a gap in the existing literature related to the interactive effects of negative symptoms, which may influence social functioning (e.g., Kring et al., 2013), and social role functioning in relation to suicide risk. This interaction may explain the inconsistent findings regarding whether social support and social role functioning act as protective factors against suicide in individuals with schizophrenia (e.g., Heila et al., 1999; Lopez-Morinigo et al., 2014; Yan et al., 2013).
This study also indicates that Joiner’s (2005) interpersonal theory of suicide may provide an explanation of suicide risk among individuals with few negative symptoms of schizophrenia, but may not be the most appropriate model from which to conceptualize suicide risk in those with prominent negative symptoms. Negative symptoms may affect the desire for social belonging and motivation to seek belonging (e.g., Kring et al., 2013). Therefore, individuals with prominent negative symptoms may not experience a thwarted need for belonging and, as such, may not be at elevated risk for suicide due to thwarted belongingness. Instead, suicide risk among individuals with elevated negative symptoms (e.g., Umut et al., 2013; Yan et al., 2013) may be due to other causes, such as demoralization (Drake et al., 1985).
These results suggest promising clinical interventions to potentially reduce suicide risk among individuals with schizophrenia. Of particular importance may be enhancing social functioning among individuals with few motivation and pleasure-related negative symptoms to reduce suicide ideation, and therefore risk for death by suicide. Clinicians may develop a collaborative clinical focus on increasing frequency of social contact, reducing withdrawal from others, improving reciprocity in social relationships, making contributions to others, and reducing dependency or destructive behaviors in relationships. Social skills training, an evidence-based group intervention, may be particularly beneficial in increasing social functioning among individuals with schizophrenia (Bellack, Mueser, Gingerich, & Agresta, 2004). Additionally, the results of this study also indicate that assessing for social functioning, as well as negative symptoms, may be beneficial when assessing suicide risk in individuals with schizophrenia.
This study had several limitations. The sample was relatively small and was recruited as part of a larger study focused on negative symptoms, which may have introduced bias. However, the sample was recruited from four sites across the country and the gender distribution was relatively equal, which increases the likelihood of generalizability. Yet, our sample was predominantly single (never married) and White or Black, which may limit generalizability to individuals who are married or identify as other races. The stabilized outpatient sample may also limit generalizability to more symptomatic individuals. Additionally, as is common in studies that utilize self-report measures, we cannot rule out the possibility of social desirability bias in responding. Also, while we controlled for many risk factors for suicide, there may be other psychiatric symptoms or areas of functioning that influence suicide ideation but were outside the scope of this study. The one-item measure of suicide ideation may also limit reliability, and average scores on this item were relatively low. Finally, because this study was cross-sectional, causal assumptions cannot be made. Future research may address some of these limitations by utilizing longitudinal data collection, recruiting a larger or acutely high-risk sample, or using multimethod multitrait data collection to assess a range of variables in multiple ways to reduce the likelihood of bias.
In conclusion, these findings indicate that individuals with few negative symptoms appear to benefit from social interactions, as those with better social role functioning had lower suicide ideation than those with poorer role functioning. This suggests that clinical interventions should focus on improving social functioning to potentially reduce suicide risk in individuals with few negative symptoms of schizophrenia.
Acknowledgements
None.
Funding body agreements and policies
This work was supported by NIH grant (1R01MH082839) to Dr. Blanchard. Writing of this manuscript was supported by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs (Dr. Jahn and Dr. Park’s time). The funding sources had no role in study design or in the collection, analysis and interpretation of data, or in the writing of this report.
Footnotes
Because of established gender differences in suicide, negative symptoms, and social support, we ran all analyses separately in men and women. The interactions for the MPQ-SC and CAINS-Expression analyses remained non-significant for both genders. The interaction for the CAINS-MAP analysis became non-significant for both men and women, possibly due to low power.
Conflict of Interest
Dr. Raquel E. Gur participated in an advisory board for Otsuka unrelated to the study. Dr. Jack J. Blanchard has received honoraria and travel support from F. Hoffman-La Roche and Genentech for consulting. All other authors declare that they have no conflicts of interest.
Contributors
Danielle R. Jahn formulated hypotheses, analyzed data, and wrote portions of the manuscript. Melanie E. Bennett and Stephanie G. Park wrote portions of the manuscript, consulted on writing, provided input on hypotheses and analyses, conferred on interpretation of results, and reviewed the manuscript. Raquel E. Gur, William P. Horan, Ann M. Kring, and Jack J. Blanchard designed and ran the larger study from which this data was drawn, provided input on hypotheses and analyses, and reviewed the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aday LA, Cornelius LJ. Designing and Conducting Health Surveys: A Comprehensive Guide. third ed Jossey-Bass; San Francisco: 2006. [Google Scholar]
- Balhara YPS, Verma R. Schizophrenia and suicide. East Asian Arch. Psychiatry. 2012;22(3):126–133. [PubMed] [Google Scholar]
- Bellack AS, Mueser KT, Gingerich S, Agresta J. Social skills training for schizophrenia: a step-by-step guide. second ed Guilford; New York: 2004. [Google Scholar]
- Blanchard JJ, Collins LM, Aghevli M, Leung WW, Cohen AS. Social anhedonia and schizotypy in a community sample: the Maryland Longitudinal Study of Schizotypy. Schizophr. Bull. 2011;37(3):587–602. doi: 10.1093/schbul/sbp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard JJ, Horan WP, Brown SA. Diagnostic differences in social anhedonia: a longitudinal study of schizophrenia and major depressive disorder. J. Abnorm. Psychol. 2001;110(3):363–371. doi: 10.1037//0021-843x.110.3.363. [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Mueser KT, Bellack AS. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr. Bull. 1998;24(3):413–424. doi: 10.1093/oxfordjournals.schbul.a033336. [DOI] [PubMed] [Google Scholar]
- Bushe CJ, Taylor M, Haukka J. Mortality in schizophrenia: a measurable clinical endpoint. J. Psychopharmacol. 2010;24(11,S4):17–25. doi: 10.1177/1359786810382468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell CB, Gottesman II. Schizophrenia—a high-risk factor for suicide: clues to risk reduction. Suicide Life-Threat. Behav. 1992;22(4):479–493. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [Retrieved February 23, 2015];Injury prevention & control: data & statistics (WISQARS) Fatal Injury Reports. from http://www.cdc.gov/injury/wisqars/fatal_injury_reports.html.
- Drake R, Whitaker A, Gates C, Cotton P. Suicide among schizophrenics: a review. Compr. Psychiatry. 1985;26(1):90–100. doi: 10.1016/0010-440x(85)90053-7. [DOI] [PubMed] [Google Scholar]
- Edmondson M, Pahwa R, Lee KK, Hoe M, Brekke JS. A dual change model of life satisfaction and functioning for individuals with schizophrenia. Schizophr. Res. 2012;139(1-3):110–115. doi: 10.1016/j.schres.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Edition (SCID-I/P) Biometrics Research, New York State Psychiatric Institute; New York: 2001. [Google Scholar]
- Gooding PA, Sheehy K, Tarrier N. Perceived stops to suicidal thoughts, plans, and actions in persons experiencing psychosis. Crisis. 2013;34(4):273–281. doi: 10.1027/0227-5910/a000194. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Sewell DR, Cooley EL, Leavitt N. Assessing levels of adaptive functioning: the Role Functioning Scale. Community Ment. Health J. 1993;29(2):119–131. doi: 10.1007/BF00756338. [DOI] [PubMed] [Google Scholar]
- Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br. J. Psychiatry. 2005;187(1):9–20. doi: 10.1192/bjp.187.1.9. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; New York: 2013. [Google Scholar]
- Heila H, Keikkinen ME, Isometsa ET, Henriksson MM, Marttunen MJ, Lonnqvist JK. Life events and completed suicide in schizophrenia: a comparison of suicide victims with and without schizophrenia. Schizophr. Bull. 1999;25(3):519–531. doi: 10.1093/oxfordjournals.schbul.a033398. [DOI] [PubMed] [Google Scholar]
- Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J. Psychopharmacol. 2010;24(11,S4):81–90. doi: 10.1177/1359786810385490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan WP, Kring AM, Blanchard JJ. Anhedonia in schizophrenia: a review of assessment strategies. Schizophr. Bull. 2006;32(2):259–273. doi: 10.1093/schbul/sbj009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corporation . IBM SPSS Statistics for Windows. version 22.0 IBM Corporation; Armonk, NY: 2014. [Google Scholar]
- Joiner T. Why People Die by Suicide. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Kasckow J, Golshan S, Zisook S. Does age moderate the relationship between depressive symptoms and suicidal ideation in middle-aged and older patients with schizophrenia and subthreshold depression? Am. J. Geriatr. Psychiatry. 2014;22(5):437–441. doi: 10.1016/j.jagp.2013.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasckow J, Liu N, Haas GL, Phillips MR. Case-control study of the relationship of depressive symptoms to suicide in a community-based sample of individuals with schizophrenia in China. Schizophr. Res. 2010;122(1-3):226–231. doi: 10.1016/j.schres.2010.02.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr. Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Koeda A, Otsuka K, Nakamura H, Yambe T, Fukumoto K, Onuma Y, Saga Y, Yoshioka Y, Mita T, Mizugai A, Sakai A, Endo S. Characteristics of suicide attempts in patients diagnosed with schizophrenia in comparison with depression: a study of emergency room visit cases in Japan. Schizophr. Res. 2012;142(1-3):31–39. doi: 10.1016/j.schres.2012.08.029. [DOI] [PubMed] [Google Scholar]
- Kopelowicz A, Ventura J, Liberman RP, Mintz J. Consistency of Brief Psychiatric Rating Scale factor structure across a broad spectrum of schizophrenia patients. Psychopathol. 2008;41(2):77–84. doi: 10.1159/000111551. [DOI] [PubMed] [Google Scholar]
- Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am. J. Psychiatry. 2013;170(2):165–172. doi: 10.1176/appi.ajp.2012.12010109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llerena K, Park SG, McCarthy JM, Couture SM, Bennett ME, Blanchard JJ. The Motivation and Pleasure Scale-Self Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr. Psychiatry. 2013;54(5):568–574. doi: 10.1016/j.comppsych.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Morinigo J-D, Fernandes A, Chang C-K, Hayes R, Broadbent M, Stewart R, David A, Dutta R. Suicide completion in secondary mental healthcare: a comparison study between schizophrenia spectrum disorders and all other diagnoses. BMC Psychiatry. 2014;14(213):1–10. doi: 10.1186/s12888-014-0213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luckhoff M, Koen L, Jordaan E, Neihaus D. Attempted suicide in a Xhosa schizophrenia and schizoaffective disorder population. Suicide Life-Threat. Behav. 2014;44(2):167–174. doi: 10.1111/sltb.12066. [DOI] [PubMed] [Google Scholar]
- Lyu J, Zhang J. Characteristics of schizophrenia suicides compared with suicides by other diagnosed psychiatric disorders and those without a psychiatric disorder. Schizophr. Res. 2014;155(1-3):59–65. doi: 10.1016/j.schres.2014.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montross LP, Zisook S, Kasckow J. Suicide among patients with schizophrenia: a consideration of risk and protective factors. Ann. Clin. Psychiatry. 2005;17(3):173–182. doi: 10.1080/10401230591002156. [DOI] [PubMed] [Google Scholar]
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol. Rep. 1962;10(3):799–812. [Google Scholar]
- Reddy LF, Green MF, Rizzo S, Sugar CA, Blanchard JJ, Gur RE, Kring AM, Horan WP. Behavioral approach and avoidance in schizophrenia: an evaluation of motivational profiles. Schizophr. Res. 2014;159(1):164–170. doi: 10.1016/j.schres.2014.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarinen PI, Lehtonen J, Lonnqvist J. Suicide risk in schizophrenia: an analysis of 17 consecutive suicides. Schizophr. Bull. 1999;25(3):533–542. doi: 10.1093/oxfordjournals.schbul.a033399. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Barrowclough C, Andrews B, Gregg L. Risk of non-fatal suicide ideation and behaviour in recent onset schizophrenia: the influence of clinical, social, self-esteem and demographic factors. Soc. Psychiatry Psychiatr. Epidemiol. 2004;39(11):927–937. doi: 10.1007/s00127-004-0828-3. [DOI] [PubMed] [Google Scholar]
- Tellegen A, Waller NG. Exploring personality through test construction: Development of the Multidimensional Personality Questionnaire. In: Boyle GJ, Matthews J, Saklofske DH, editors. Handbook of Personality Theory and Testing: Vol. II. Personality Measurement and Assessment. Sage; Thousand Oaks, CA: 2008. pp. 261–292. [Google Scholar]
- Umut G, Altun ZO, Danismant BS, Kucukparlak I, Karamustafalioglu N, Ilnes MC. The correlation of suicide attempt and suicidal ideation with insight, depression and severity of illness in schizophrenic patients. Dusunen Adam. 2013;26(4):341–350. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr. The interpersonal theory of suicide. Psychol. Rev. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green MF, Shaner A. Brief Psychiatric Rating Scale (BPRS) expanded version: Scales, anchor points and administration manual. Int. J. Methods Psychiatr. Res. 1993;3(App. 1):227–243. [Google Scholar]
- Yamada A-M, Lee KK, Dinh TQ, Barrio C, Brekke JS. Intrinsic motivation as a mediator of relationships between symptoms and functioning among individuals with schizophrenia spectrum disorders in a diverse urban community. J. Nerv. Ment. Dis. 2010;198(1):28–34. doi: 10.1097/NMD.0b013e3181c8aa71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan F, Xiang Y-T, Hou Y-Z, Ungvari GS, Dixon LB, Chan SSM, Lee EHM, Li W-Y, Li W-X, Zhu Y-L, Chiu HFK. Suicide attempt and suicidal ideation and their associations with demographic and clinical correlates and quality of life in Chinese schizophrenic patients. Soc. Psychiatry Psychiatr. Epidemiol. 2013;48(3):447–454. doi: 10.1007/s00127-012-0555-0. [DOI] [PubMed] [Google Scholar]