Abstract
Objectives
To explore relations between loneliness and self-rated health among diversely-aged African American adults.
Methods
Associations between loneliness and self-rated health were investigated using covariate-adjusted linear regression models. Perceived social support was examined as a moderator. The potential indirect effects of stress and/or depressive symptoms were examined using nonparametric bootstrapping procedures.
Results
Greater loneliness was associated with poorer self-rated health (p = 0.008), and social support did not moderate. Stress and depressive symptoms yielded significant indirect effects in single and multiple mediator models (p values ≤ .05).
Conclusions
Loneliness may contribute to poorer health among African Americans. Results suggest that greater stress and depressive symptoms might underlie these associations, but longitudinal studies are needed to assess causal relations.
Keywords: loneliness, self-rated health, depression, stress
Loneliness is characterized as a distressing feeling that is attributable to a disconnection between one’s desired versus one’s actual social relationships.1 Loneliness appears to be highly prevalent; for example, as many as 20% to 39% of older adults report feelings of loneliness at any given time.2,3 These numbers are concerning given that loneliness has been associated with a host of undesirable physical and psychological health consequences. For example, loneliness has been associated with a reduction in physical activity,4 increased systolic blood pressure,5 daytime dysfunction and impaired sleep,6 anxiety,7 and depressive symptoms.8–10 Loneliness is associated with undesirable social factors as well, including poor communication decoding within interpersonal interactions.11 Furthermore, a negative relationship between loneliness and self-rated health has been frequently reported within the literature.12–14
Self-rated health is obtained by asking individuals to assess their own health status or to compare their health with their same aged peers.15 Although subjective in nature, self-rated health is of interest because it is one of the most frequently employed health indicators in empirical studies and is considered one of the best indictors of mortality.16 Although the physical and psychological health consequences of loneliness on self-rated health are understood, most studies in this area were conducted among aging and majority White samples, which limits the generalizability of these findings to other populations. Therefore, additional research on the associations of loneliness and self-rated health among diversely aged and racial/ethnic minority groups is recommended.
African Americans are important to study when assessing the impact of loneliness on self-rated health, given the numerous health disparities experienced by this ethnic group. For example, African Americans have the earliest onset of hypertension and develop high blood pressure at a higher rate than other ethnic groups.17 African American women have higher breast cancer mortality rates than women of all other ethnic groups; for example, they are 40% more likely to die of breast cancer than White women.18 Similarly, African American men have higher incidence and mortality rates for several cancers as compared with Whites and Hispanics (eg, lung and prostate cancer).19–21 These health disparities are also reflected in self-rated health, with African Americans over the age of 50 rating themselves as having poorer health on average than their White counterparts.22 Studies have indicated that a variety of characteristics, such as depressive symptoms, smoking, and less education, were associated with poorer self-rated health23 and self-rated health trajectories24 among African Americans. However, to our knowledge, no previous studies have examined the association of loneliness and self-rated health among African Americans of any age group. Such an area may be fruitful to explore, given the links between loneliness and poorer self-rated health among aging adults and majority White samples.12–14 Moreover, a better understanding of the various determinants of poorer self-rated health endorsed by African Americans might be helpful for targeting or adapting interventions to reduce disparities in health.
Many African American families benefit from a unique social structure. For example, as a result of cultural, social and economic factors, African Americans have commonly relied on extended family and informal networks as a source of support.25 Previous studies have found that the level of perceived social support experienced by African Americans has been associated with a variety of physical and psychological health outcomes. For example, greater social support has been linked with greater subjective life expectancy.26 Moreover, social support played a moderating role in the relations between optimism and psychosocial functioning in one study,27 and discrimination and distress in another.28 The positive effects of social support on various health outcomes may reflect that social support facilitates engagement in health promoting behaviors such as exercise, eating right, and not smoking; as well as greater adherence to medical regimens.29,30 However, the extent to which perceived social support might buffer an association between loneliness and self-rated health among African Americans is not known. Loneliness has been linked with minimal availability of social support in general,31 but perceived social support may still vary substantially among those experiencing loneliness.32
Conceptual models, such as the one proposed by Cacioppo and colleagues, outline the psychological and social consequences of loneliness and the negative impact it ultimately has on health.8,33 Consistent with this conceptual model, several studies support associations between loneliness and anxiety,7 loneliness and stress,34,35 and loneliness and depression.36,37 Likewise, there has been significant support for the role of anxiety/stress and depression on negative health outcomes38,39 and poorer self-rated health23,39–41 in the literature. However, to our knowledge, no previous studies have examined whether perceived stress and depressive symptoms account for the associations of loneliness and self-rated health. A better understanding of this association might be particularly important when studying African Americans, given their exposure to various social stressors (eg, discrimination and oppression) that have been found to negatively impact mental and physical health.42,43 For example, it is possible that African Americans who experience loneliness may be at a greater risk of psychological distress and negative health outcomes due to the psychologically taxing processes associated with both loneliness and other social stressors.
The current study examined associations between loneliness and self-rated health among a large sample of African American adults and investigated whether these associations were moderated by perceived social support. Based on the literature, we hypothesized that greater loneliness would be associated with poorer self-rated health, even after controlling for the influence of sociodemographics and depressive symptoms. We also hypothesized that social support would moderate these associations, such that the expected inverse relation between loneliness and self-rated health would be attenuated among those reporting greater social support. A secondary aim of this study was to assess if the expected association between loneliness and self-rated health was mediated by elevated stress and/or depressive symptoms. We hypothesized that higher levels of stress and depression would help to explain the relationship between loneliness and self-rated health.
METHODS
Participants and Procedures
Data were from the second year of a longitudinal cohort study focused on African American health. Data from this wave were analyzed because it represented the first year that loneliness was assessed. Participants represented a convenience sample originally recruited into the cohort study from a large Methodist mega-church in Houston, Texas. Recruitment strategies included printed and televised media within the church and in-person solicitation during church services and at a church health fair. Recruitment took place in the fall of 2008. Individuals were eligible to participate if they were ≥18 years old, residents of the Houston area, had a functional telephone number, and attended church.
Following enrollment, participants (N = 1501) completed the first wave of data collection. Approximately one year later, they were contacted via e-mail, phone, and/or mail to participate in the second wave. In total, 1375 participants (91.6% of the original sample) participated in the second wave. As with the first wave, surveys were completed in person at the church. Participants viewed questionnaire items on a computer screen and entered responses into the computer using the keyboard, and they were compensated with a $30 gift card following survey completion. Only participants with complete data on the measures described below (N = 1343, 89.5% of the original sample) were included in the current study. Data for the second wave were collected between January and August 2010.
Measures
Sociodemographics
Sociodemographics included age, sex, partner status (married/living with partner or single/widowed/divorced), total annual household income (<$40,000, $40,000–79,999, or ≥$80,000), educational level (<Bachelor’s degree, Bachelor’s degree, or ≥Master’s degree), and employment status (employed or unemployed).
Loneliness
Loneliness was assessed using a 3-item scale that asks respondents to indicate how often they “feel that [they] lack companionship,” “feel left out,” and “feel isolated from others.”44 Response categories were 1=hardly ever, 2=some of the time, and 3=often. Total scores could range from 3 to 9, with higher scores indicative of greater perceived loneliness. Cronbach's alpha for the 3-Item Loneliness Scale in this sample was 0.80.
Social support
Social support was measured using the Interpersonal Support Evaluation List (ISEL).45 The ISEL is a 12-item measure of functional social support that assesses the perceived availability of appraisal, tangible, and belonging types of support. Appraisal support items assess the availability of someone to talk with about problems and include: “I feel that there is no one I can share my most private worries and fears with.” Belonging support items assess the availability of people with whom one can do activities and include: “I don't often get invited to do things with others.” Tangible support items assess instrumental aid and include: “If I were sick, I could easily find someone to help me with my daily chores” (reverse scored). Response options for each item were as follows: 1=definitely true, 2=probably true, 3=probably false, and 4=definitely false. Total scores could range from 12 to 48, with higher scores indicative of greater social support. Cronbach's alpha for the ISEL-12 in this sample was 0.84.
Perceived stress
The Perceived Stress Scale-4 (PSS-4) was used to assess perceived stress.46 The PSS-4 is a 4-item self-report scale that was designed to assess the degree to which respondents find their lives to be stressful. The PSS-4 asks respondents to indicate how often they experienced certain situations, such as “In the last month, how often have you felt that you were unable to control the important things in your life?” and “In the last month, how often have you felt that things were going your way?” (reverse scored). Response categories were: 0=never, 1=almost never, 2=sometimes, 3=fairly often, and 4=very often. Responses were summed with a potential range of 0 to 16, where higher scores are indicative of greater perceived stress. Cronbach's alpha for the PSS-4 in this sample was 0.73.
Depressive symptoms
The Center for Epidemiological Studies Depression 10-item scale (CESD-10) was used to assess depressive symptoms.47,48 The CESD was developed to measure depressive symptoms in community non-clinical populations, and assesses the degree of depressive symptoms experienced over the past week. It includes items such as “I was bothered by things that usually don’t bother me,” and “I felt hopeful about the future” (reverse scored). Response categories were: 0=rarely or none of the time (< 1 day), 1=some or a little of the time (1–2 days), 2=occasionally or a moderate amount of time (3–4 days), and 3=all the time (5–7 days). Responses were summed with a potential range of 0 to 30, where higher scores are indicative of more depressive symptoms. Cronbach's alpha for the CESD-10 in this sample was 0.54.
Self-rated health
Self-rated health was assessed with a single item asking participants to rate their health in general, with 5 response options: 1= poor, 2=fair, 3=good, 4=very good, and 5=excellent. Research suggests this item is a reasonable substitute for multi-item measures and has good psychometric utility for the assessment of general health.15,49–54
Data Analysis
Preliminary analyses assessed participant characteristics using frequencies and descriptive statistics. A preliminary linear regression analysis was conducted to explore the relations between each sociodemographic variable and loneliness while controlling for the other sociodemographic variables.
Three linear regression models were conducted to assess the association between loneliness and self-rated health. The first model was adjusted for the covariates of age, sex, partner status, income, education, and employment status, and the second model was additionally adjusted for depressive symptoms. A final model added an interaction term along with the main effects of social support and all covariates to examine whether the association between loneliness and self-rated health was moderated by perceived social support.
Finally, the indirect effects of loneliness on self-rated health through stress and depressive symptoms were assessed using 2 single mediation models for stress and depressive symptoms, respectively, and a multiple mediator analysis that included both stress and depressive symptoms in the same model. Indirect effects were tested using a non-parametric, bias-corrected bootstrapping procedure.55 The bootstrapping procedure generated an empirical approximation of the sampling distribution of the product of the estimated coefficients in the indirect paths using 5000 resamples from the data set. Indirect effect models were adjusted for sociodemographics, including age, sex, partner status, income, education, and employment status.
All analyses were performed using Statistical Analysis Software version 9.3 (SAS Institute, Cary, NC). The statistical significance level was set at p ≤ .05.
RESULTS
Preliminary Analyses
Participants were 46.5 (±12.7 years) years old on average and were predominately women (76.3%). The age distribution of the sample was as follows: 18–25 (6.6%), 26–35 (13.4%), 36–45 (23.6%), 46–55 (32.1%), 56–66 (19.8%), and 67–87 (4.5%). Three quarters of participants were employed, 51.1% reported at least a Bachelor’s Degree, and 37.7% reported an annual household income of at least $80,000. Participant characteristics are displayed in Table 1. In this sample, 7.4% reported excellent health, 33.6% reported very good health, 44.5% reported good health, 13.0% reported fair health, and 1.5% reported poor health.
Table 1.
Participant Characteristics
| Participant Characteristics | Total Sample | |
|---|---|---|
| N = 1343 | ||
| Mean (Std) | N [%] | |
| Age | 46.5 (12.7) | - |
| Sex | ||
| Female | - | 1025 [76.3] |
| Male | - | 318 [23.7] |
| Education | ||
| < Bachelor’s Degree | - | 656 [48.8] |
| Bachelor’s Degree | - | 406 [30.2] |
| ≥ Master’s Degree | - | 281 [20.9] |
| Income | ||
| < $40,000 | - | 344 [25.6] |
| $40,000–79,999 | - | 493 [36.7] |
| ≥ $80,000 | - | 506 [37.7] |
| Partner status | ||
| Married/Living with partner | - | 606 [45.1] |
| Single/Widowed/Divorced | - | 737 [54.9] |
| Employment status | ||
| Employed | - | 1008 [75.1] |
| Unemployed | - | 335 [24.9] |
| Self-rated Health | 3.3 (8.6) | - |
| Loneliness | 4.5 (1.6) | - |
| Stress | 4.6 (3.0) | - |
| Depressive Symptoms | 9.2 (3.6) | - |
| Social Support | 38.9 (4.7) | |
Note.
Std = standard deviation. Loneliness = The 3-Item Loneliness Scale; Stress = Perceived Stress Scale; Depressive Symptoms = Center for Epidemiological Studies Depression 10-item scale; Social Support = The Interpersonal Support Evaluation List 12-item scale.
Results of a preliminary analysis assessing differences in loneliness as a function of sociodemographic variables are shown in Table 2. Controlling for the other sociodemographic variables, results indicated that women reported significantly greater loneliness than men (means = 4.6 versus 4.1), those without partners reported significantly greater loneliness than those who had partners (means = 4.9 versus 4.0), and those with annual incomes less than $40,000 a year reported significantly greater loneliness than those with annual incomes of $80,000 or more (means = 4.9 versus 4.2).
Table 2.
Adjusted Relations of Sociodemographics and Loneliness
| Unstandardized Coefficients |
||||
|---|---|---|---|---|
| Variables | β | Std. Error | t | p |
| Age | −.00 | .00 | −.09 | .93 |
| Sex | ||||
| Female | .23 | .10 | 2.27 | .02 |
| Male (REF) | ||||
| Education | ||||
| < Bachelor’s Degree (REF) | ||||
| Bachelor’s Degree | −.08 | .10 | −.76 | .44 |
| ≥ Master’s Degree | −.08 | .12 | −.66 | .51 |
| Income | ||||
| < $40,000 (REF) | ||||
| $40,000–79,999 | −.22 | .12 | −1.90 | .06 |
| ≥$80,000 | −.36 | .13 | −2.76 | <.01 |
| Partner status | ||||
| Married/Living with partner | −.77 | .10 | −8.06 | <.001 |
| Single/Widowed/Divorced (REF) | ||||
| Employment status | ||||
| Employed | .14 | .10 | 1.33 | .18 |
| Unemployed (REF) | ||||
Note.
Results represent relations between each sociodemographic variable and loneliness controlling for the other sociodemographic variables, as assessed using multiple linear regression. Loneliness = The 3-Item Loneliness Scale
Main Analyses
Results indicated that greater loneliness was associated with poorer self-rated health in analyses adjusted for sociodemographics (p < .0001). See Table 3. Further adjusting this model for depressive symptoms did change the pattern of results (β=−.043, SE=.016, t = −2.67, p = .008). Social support was not a significant moderator of the association between loneliness and self-rated health (p = .818).
Table 3.
Adjusted Relations of Loneliness and Self-rated Health
| Variables | β | Std. Error | t | p |
|---|---|---|---|---|
| Loneliness | −.098 | .01 | −6.79 | <.0001 |
| Age | −.003 | .00 | −1.79 | .07 |
| Sex | ||||
| Female | −.090 | .05 | −1.65 | .10 |
| Male (REF) | ||||
| Education | ||||
| < Bachelor’s Degree (REF) | ||||
| Bachelor’s Degree | .115 | .05 | 2.12 | .03 |
| ≥ Master’s Degree | .214 | .06 | 3.45 | <.01 |
| Income | ||||
| < $40,000 (REF) | ||||
| $40,000–79,999 | .048 | .06 | 0.77 | .44 |
| ≥$80,000 | .153 | .07 | 2.23 | .03 |
| Partner status | ||||
| Married/Living with partner | −.103 | .05 | −2.00 | .05 |
| Single/Widowed/Divorced (REF) | ||||
| Employment status | ||||
| Employed | .153 | .06 | 2.77 | .01 |
| Unemployed (REF) |
Note.
Results represent those from a linear regression examining relations of loneliness and self-rated health in covariate adjusted analysis. Loneliness = The 3-Item Loneliness Scale
Indirect Effect Analyses
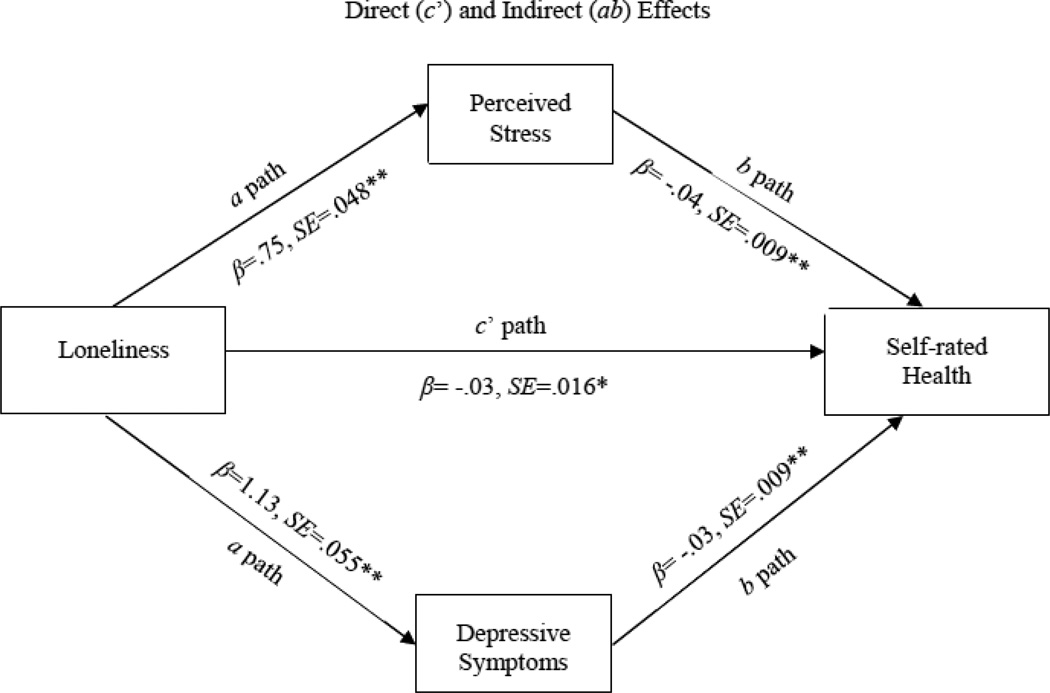
In single mediator models, stress and depressive symptoms each yielded significant indirect effects in the association between loneliness and self-rated health (p values ≤ .05; see Table 4). Greater loneliness was associated with greater perceived stress (β=.747, SE=.515, t = 15.63, p < .0001) and more severe depressive symptoms (β=1.034, SE=.055, t = 18.87, p < .0001), and greater stress and more severe depressive symptoms were each associated with poorer self-rated health (stress: β=−.063, SE=.008, t =−7.80, p < .0001; depressive symptoms: β= −.054, SE=.007, t = −7.60, p < .0001). Additionally controlling for depressive symptoms in the indirect effect model for stress yielded similar results (β= −.010, SE=.003, CIs.95 = −.0180, −.0049).
Table 4.
Indirect Effects of Loneliness on Self-rated Health through Stress and Depressive Symptoms
| Estimate of indirect effect | BCa 95% CI | |||
| Proposed Mediator | Effect Estimate | SE | Lower | Upper |
| Stress | −.047 | .007 | −.063 | −.034 |
| Depressive Symptoms | −.056 | .008 | −.073 | −.040 |
| Estimate of indirect effect | BCa 95% CI | |||
| Proposed Mediators | Effect Estimate | SE | Lower | Upper |
| Stress | −.031 | .008 | −.047 | −.017 |
| Depressive Symptoms | −.035 | .009 | −.053 | −.018 |
| Combined | −.066 | .009 | −.084 | −.049 |
Note.
Effect Estimate = The mean of the indirect effect estimates calculated across 5000 bootstrap samples. SE = The standard deviation of the 5000 bootstrap estimates of the indirect effect. BCa 95% CI= Bias corrected and accelerated 95% confidence interval. Loneliness = The 3-Item Loneliness Scale; Stress = Perceived Stress Scale; Depressive Symptoms = Center for Epidemiological Studies Depression 10-item scale.
Although stress and depressive symptoms are conceptually distinct, they were significantly correlated (r = .66, p < .01). A multiple mediator analysis was conducted to take into account any shared variance. Results indicated that stress and depressive symptoms were independently as well as jointly significant mediators of the total effect (p values ≤ .05; see Table 4 and Figure 1). Again, greater loneliness was associated with greater stress and more severe depressive symptoms, and greater stress and more severe depressive symptoms were associated with poorer self-rated health.
Figure 1.
Hypothesized Conceptual Model of the Direct (c’ path) and Indirect Effect (ab paths) of Loneliness on Self-rated Health through Proposed Mediators
**p ≤ .0001, *p < .05
Note.
Mediational results presented in Figure 1 represent those from the multiple mediator analysis.
DISCUSSION
To our knowledge, this study was the first to investigate the association between loneliness and self-rated health among a large and diversely aged African American sample. As hypothesized, loneliness was negatively associated with self-rated health over and above the influence of several sociodemographic variables. Moreover, the association between loneliness and self-rated health remained significant after depressive symptoms were taken into account. This finding provides further support for the negative association between loneliness and self-rated health and extends those relations to a diversely aged, predominately female sample of African American mega-church attendees.
Although religiosity has been linked to less loneliness in previous research among the elderly, the current study suggests that mega-church attendees are not immune from experiencing loneliness, and that loneliness may be implicated in African Americans’ poorer self-rated health.56 Therefore, it may be helpful to provide and integrate interventions to address loneliness within the church setting to help attenuate the potential effects of loneliness on health. Previous research suggests that interventions to address loneliness might include improving social skills, developing strategies to enhance social support, and increasing opportunities for social interaction.7,11 These issues seem potentially addressable within a church setting through support groups, Bible study, and other ministry efforts. Openly discussing the subject of loneliness within these platforms may lessen any stigmatizing feelings associated with experiencing loneliness. In addition, previous studies suggest that loneliness interventions might also entail the correction of maladaptive thinking (eg, negative attributions) via a more formalized intervention, such as cognitive-behavioral therapy.57 This type of intervention may be especially relevant for persons who have co-morbid depressive symptomology. This may be accomplished via referral to community mental health professionals; however, since church members often seek out the leaders of their church for both spiritual and personal problems,58 equipping the clergy with the appropriate skills to create and implement tailored mental health-behavior interventions (eg, cognitive restructuring exercises) might also be useful. Because some African Americans may consider loneliness and affective symptomatology to be the result of a loss of faith,59 clergy have an important role to play in de-stigmatizing loneliness and helping parishioners overcome various barriers to seeking help.
Interestingly, perceived social support was not supported as a moderator of the relationship between loneliness and self-rated health. This finding is contrary to results from previous studies in the area.60–62 However, it may be that the relationship between loneliness and social support is more dependent on the perceived quality of social support rather than its presence.63 Therefore, it may be that satisfaction with social support (not assessed in this study) may matter more in the association between loneliness and self-reported health than the mere availability of social support. This may be especially true among African Americans, who tend to benefit from a large and extended familial social structure,25 making the availability of social support less of a concern than might be the case with Whites. In addition, a previous study found that men and women have differences in the relational provisions that were linked with loneliness. For example, whereas men may feel lonely if they perceive a deficit in the social integration offered by relationships, women feel lonely if they feel that their relationships lack attachment.31 Therefore, men and women may perceive social support differently and may need varying relationship qualities to feel supported. These suppositions may provide direction for future research.
The current study also provides support for the potential role of stress and depressive symptoms in the association between loneliness and self-rated health. This finding suggests that interventions to reduce stress and depressive symptoms may be a helpful approach for reducing the potential effects of loneliness on self-rated health. This may be accomplished via formal referrals to community treatment professionals, and facilitated by the sponsorship of workshops and presentations in the church setting focused on psychoeducational information about mental health problems, its health-related sequelae, and empirically-based treatment options. Because mental health treatment may be more stigmatizing among African Americans compared to Whites,64 discussing psychological distress and associated treatment options within the church setting may feel less threatening than when introduced in other settings (eg, the physician’s office). However, these suggestions are speculative and require additional research. Future research should also investigate the role of stress and depressive symptoms in the association between loneliness and self-rated health using longitudinal designs (eg, cross-lagged panel designs, 2-dimensional modeling) to capture temporal processes and causal relations.
Limitations of the current study include the cross-sectional design, which precludes causal assumptions. Additionally, while this study extends the literature through the use of a large and diversely aged African American sample, the participants of the study were all attendees of a large Methodist church. Since this sample represents a subset of the larger African American population, results may not generalize to the larger African American population, as there may be substantive differences among African Americans who attend church, those who do not attend church and those who ascribe to varying faiths and denominations. Another limitation of the study is the low internal consistency produced by the depressive symptoms measure (CESD-10). While previous studies have used the CESD with an African American population and produced a more acceptable Cronbach’s alpha,65,66 clinical research has found that African Americans may exhibit atypical depressive symptomology,67 which may have influenced our results. In addition, this study’s use of the 10-item version of the CESD as opposed to the 20-item scale may have led to the less than desirable reliability. Regardless, the validity of these results should be considered in light of the reliability weaknesses of the CESD in this sample. However, given the dearth of research assessing relations between loneliness, depression, and self-rated health among African Americans, these results may at least provide direction for future work. Moreover, future research can expand upon the information obtained from this study by including a more diverse sample in future studies. While African Americans are a specific minority group, they are not representative of every minority group; therefore, more studies using other populations would lend additional support for the association between loneliness and self-rated health. Despite the fact that this sample identified as being primarily healthy, an association was still found between loneliness and self-rated health. While this provides stronger support for the connection between the 2 variables, an association between loneliness and health among African American groups and other ethnic minorities who are less healthy should be explored. In addition, future studies might compare relations between racial/ethnic groups, incorporate qualitative research to better understand how individuals experience loneliness and evaluate their health status, and use longitudinal designs to further extend the literature in this area. Finally, the current study investigated only 2 potential mediators of the relation between loneliness and self-rated health, and the variance accounted for by these psychosocial factors is likely to be low, as is commonly the case in behavioral research. Future work should strive to develop and evaluate more comprehensive conceptual frameworks to explain the noted associations.
In summary, the current study may be the first to examine the relationship between loneliness and self-rated health, as well as explore the moderating effect of social support and the indirect effects of stress and depressive symptoms, among a sample of African American church attendees. Results support a link between greater loneliness and poorer self-rated health that may be attributable, at least in part, to stress and depressive symptoms. This study extends the existing literature and suggests directions for future intervention research. However, additional studies are needed in order to add greater depth to our understanding of the association between loneliness and self-rated health, potentially by examining more comprehensive conceptual models and using longitudinal data.
Acknowledgments
Data collection and management were supported by funding from the University Cancer Foundation; the Duncan Family Institute through the Center for Community-Engaged Translational Research; the Ms. Regina J. Rogers Gift: Health Disparities Research Program; the Cullen Trust for Health Care Endowed Chair Funds for Health Disparities Research; the Morgan Foundation Funds for Health Disparities Research and Educational Programs; and the National Cancer Institute at the National Institutes of Health through The University of Texas MD Anderson's Cancer Center Support Grant (CA016672). Manuscript authorship and publication were supported by institutional funds from The University of Texas MD Anderson Cancer Center and the University of Houston. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the project supporters.
We would like to acknowledge the research staff at The University of Texas MD Anderson Cancer Center who assisted with implementation of the original project. We are also appreciative of the Patient-Reported Outcomes, Survey, and Population Research Shared Resource at The University of Texas MD Anderson Cancer Center, which was responsible for scoring the survey measures used in this research. Finally, we especially want to thank the church leadership and participants, whose efforts made this study possible.
Footnotes
Human Subjects Statement
All procedures were approved by the University of Texas MD Anderson Institutional Review Board. Informed consent was obtained from participants prior to data collection.
This work was largely completed while the first author was a Graduate Trainee in the Department of Health Disparities Research at The University of Texas MD Anderson Cancer Center, Houston, TX.
Conflict of Interest Statement
The authors have no competing interests pertaining to this research.
Contributor Information
Felicia D. Fisher, Department of Educational Psychology, College of Education, University of Houston, Houston, TX.
Lorraine R. Reitzel, Department of Educational Psychology, College of Education, University of Houston, Houston, TX.
Nga Nguyen, Department of Biostatistics, The University of Texas MD Anderson Cancer Center, Houston, TX.
Elaine J. Savoy, Department of Clinical Psychology, University of Houston, Houston, TX.
Pragati S. Advani, Department of Health Promotion and Behavioral Sciences, The University of Texas School of Public Health.
Adolfo G. Cuevas, Department of Psychology, Portland State University, Portland, OR.
Jennifer I. Vidrine, Department of Health Disparities Research, The University of Texas MD Anderson Cancer Center, Houston, TX.
David W. Wetter, Department of Health Disparities Research, The University of Texas MD Anderson Cancer Center, Houston, TX.
Lorna H. McNeill, Department of Health Disparities Research, The University of Texas MD Anderson Cancer Center, Houston, TX.
References
- 1.Pinquart M, Sörensen S. Risk factors for loneliness in adulthood and old age-a meta-analysis. In: Shohov SP, editor. Advances in Psychology Research. Hauppauge: Nova Science Publishers; 2003. pp. 111–143. [Google Scholar]
- 2.Theeke LA. Predictors of loneliness in U.S. adults over age sixty-five. Arch Psychiat Nurs. 2009;23(5):387–396. doi: 10.1016/j.apnu.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Savikko N, Routasalo P, Tilvis RS, et al. Predictors and subjective causes of loneliness in an aged population. Arch Gerontol Geriat. 2005;41(3):223–233. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol. 2009;28(3):354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawkley LC, Preacher KJ, Cacioppo JT. Loneliness impairs daytime functioning but not sleep duration. Health Psychol. 2010;29(2):124–129. doi: 10.1037/a0018646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Segrin C, Kinney T. Social skills deficits among the socially anxious: rejection from others and loneliness. Motiv Emot. 1995;19(1):1–24. [Google Scholar]
- 8.Cacioppo JT, Hawkley LC, Ernst JM, et al. Loneliness within a nomological net: an evolutionary perspective. J Res Pers. 2006;40(6):1054–1085. [Google Scholar]
- 9.Nolen-Hoeksema S, Ahrens C. Age differences and similarities in the correlates of depressive symptoms. Psychol Aging. 2002;17(1):116–124. doi: 10.1037//0882-7974.17.1.116. [DOI] [PubMed] [Google Scholar]
- 10.Chou KL, Chi I. Childlessness and psychological well-being in Chinese older adults. Int J Geriatr Psych. 2004;19(5):449–457. doi: 10.1002/gps.1111. [DOI] [PubMed] [Google Scholar]
- 11.Edwards R, Bello R, Brandau-Brown F, Hollems D. The effects of loneliness and verbal aggressiveness on message interpretation. South J Comm. 2001;66(2):139–150. [Google Scholar]
- 12.Pedersen PV, Grønbæk M, Curtis T. Associations between deprived life circumstances, wellbeing and self-rated health in a socially marginalized population. Eur J Public Health. 2012;22(5):647–652. doi: 10.1093/eurpub/ckr128. [DOI] [PubMed] [Google Scholar]
- 13.Nummela O, Seppanen M, Uutela A. The effect of loneliness and change in loneliness on self-rated health (SRH): a longitudinal study among aging people. Arch Gerontol Geriat. 2011;53(2):163–167. doi: 10.1016/j.archger.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 14.Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Budrys G. Unequal Health: How Inequality Contributes to Health or Illness. Lanham: Rowman & Littlefield; 2010. [Google Scholar]
- 17.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics-2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Breast cancer disparities (on-line) [Accessed August 8, 2013]; Available at: http://www.cdc.gov/features/vitalsigns/breastcancer/
- 19.Nelson CJ, Balk EM, Roth AJ. Distress, anxiety, depression, and emotional well-being in African-American men with prostate cancer. Psycho-oncol. 2010;19(10):1052–1060. doi: 10.1002/pon.1659. [DOI] [PubMed] [Google Scholar]
- 20.Haiman CA, Stram DO, Wilkens LR, et al. Ethnic and racial differences in the smoking-related risk of lung cancer. New Engl J Med. 2006;354(4):333–342. doi: 10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. United States cancer statistics (on-line) [Accessed August 12, 2013]; Available at: http://apps.nccd.cdc.gov/uscs/
- 22.Liang J, Quinones AR, Bennett JM, et al. Evolving self-rated health in middle and old age: how does it differ across black, hispanic, and white Americans? J Aging Health. 2010;22(1):3–26. doi: 10.1177/0898264309348877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuevas AG, Reitzel LR, Cao Y, et al. Mediators of discrimination and self-rated health among African Americans. Am J Health Behav. 2013;37(6):745–754. doi: 10.5993/AJHB.37.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayyagari P, Ullrich F, Malmstrom TK, et al. Self-rated health trajectories in the African American health cohort. PloS one. 2012;7(12):e53278. doi: 10.1371/journal.pone.0053278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Billingsley A. Climbing Jacob's Ladder: The Enduring Legacies of African-American Families. New York: Simon and Schuster; 1994. [Google Scholar]
- 26.Irby-Shasanmi A. Predictors of subjective life expectancy among African Americans. Res Aging. 2013;35(3):322–347. [Google Scholar]
- 27.Shelby RA, Crespin TR, Wells-Di Gregorio SM, et al. Optimism, social support, and adjustment in African American women with breast cancer. J Behav Med. 2008;31(5):433–444. doi: 10.1007/s10865-008-9167-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ajrouch KJ, Reisine S, Lim S, et al. Perceived everyday discrimination and psychological distress: does social support matter? Ethn Health. 2010;15(4):417–434. doi: 10.1080/13557858.2010.484050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Albrecht TL, Goldsmith DJ, Thompson T. Social support, social networks, and health. In: Thompson T, Miller K, Dorsey A, Parrott R, editors. Handbook of Health Communication. Hillsdale: Lawrence J. Erlbaum Associates; 2003. pp. 263–284. [Google Scholar]
- 30.Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 31.Bell RA, Gonzalez MC. Loneliness, negative life events, and the provisions of social relationships. Communication Quarterly. 1988;36(1):1–15. [Google Scholar]
- 32.Segrin C, Domschke T. Social support, loneliness, recuperative processes, and their direct and indirect effects on health. Health Commun. 2011;26(3):221–232. doi: 10.1080/10410236.2010.546771. [DOI] [PubMed] [Google Scholar]
- 33.Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aanes MM, Mittelmark MB, Hetland J. Interpersonal stress and poor health: the mediating role of loneliness. Eur Psychol. 2010;15(1):3. [Google Scholar]
- 35.Scott SB, Jackson BR, Bergeman CS. What contributes to perceived stress in later life? A recursive partitioning approach. Psychol Aging. 2011;26(4):830–843. doi: 10.1037/a0023180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jaremka LM, Fagundes CP, Glaser R, et al. Loneliness predicts pain, depression, and fatigue: understanding the role of immune dysregulation. Psychoneuroendocrino. 2013;38(8):1310–1317. doi: 10.1016/j.psyneuen.2012.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Izgar H. An investigation of depression and loneliness among school principals. Educ Sci Theor Pract. 2009;9(1):247–258. [Google Scholar]
- 38.Jaremka LM, Fagundes CP, Peng J, et al. Loneliness promotes inflammation during acute stress. Psychol Sci. 2013;24(7):1089–1097. doi: 10.1177/0956797612464059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Naicker K, Galambos NL, Zeng Y, et al. Social, demographic, and health outcomes in the 10 years following adolescent depression. J Adolesc Health. 2013;52(5):533–538. doi: 10.1016/j.jadohealth.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 40.Wiklund M, Malmgren-Olsson EB, Ohman A, et al. Subjective health complaints in older adolescents are related to perceived stress, anxiety and gender - a cross-sectional school study in northern Sweden. BMC Public Health. 2012;12:993. doi: 10.1186/1471-2458-12-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Theme Filha MM, Costa MA, Guilam MC. Occupational stress and self-rated health among nurses. Rev Lat-Am Enferm. 2013;21(2):475–483. doi: 10.1590/s0104-11692013000200002. [DOI] [PubMed] [Google Scholar]
- 42.Bureau of Justice Statistics. Criminal Victimization, 2008 (on-line) [Accessed August 8, 2013]; Available at: http://www.bjs.gov/index.cfm?ty=pbdetail&iid=1975.
- 43.Centers for Disease Control and Prevention. Age-sex-adjusted percentage of adults aged 18 and over who experienced serious psychological distress during the past 30 days, by race/ethnicity: United States, 2012 (on-line) [Accessed August 8, 2013]; Available at: http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201306_13.pdf.
- 44.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason I, Sarason BR, editors. Social Support: Theory, Research and Application. New York: Springer; 1985. pp. 73–94. [Google Scholar]
- 46.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 47.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1(3):385–401. [Google Scholar]
- 48.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (center for epidemiologic studies depression scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 49.DeSalvo KB, Fisher WP, Tran K, et al. Assessing measurement properties of two single-item general health measures. Qual Life Res. 2006;15(2):191–201. doi: 10.1007/s11136-005-0887-2. [DOI] [PubMed] [Google Scholar]
- 50.McHorney CA. Health status assessment methods for adults: past accomplishments and future challenges. Annu Rev Publ Health. 1999;20:309–335. doi: 10.1146/annurev.publhealth.20.1.309. [DOI] [PubMed] [Google Scholar]
- 51.Kempen GI. The MOS Short-Form General Health Survey: single item vs multiple measures of health-related quality of life: some nuances. Psychol Rep. 1992;70(2):608–610. doi: 10.2466/pr0.1992.70.2.608. [DOI] [PubMed] [Google Scholar]
- 52.Cunny KA, Perri M. Single-item vs multiple-item measures of health-related quality of life. Psychol Rep. 1991;69(1):127–130. doi: 10.2466/pr0.1991.69.1.127. [DOI] [PubMed] [Google Scholar]
- 53.Bierman AS, Bubolz TA, Fisher ES, Wasson JH. How well does a single question about health predict the financial health of medicare managed care plans? Eff Clin Pract. 1999;2(2):56–62. [PubMed] [Google Scholar]
- 54.Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol. 2009;170(3):343–351. doi: 10.1093/aje/kwp144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Beh Res Meth. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 56.Johnson DP, Mullins LC. Subjective and social dimensions of religiosity and loneliness among the well elderly. Rev Relig Res. 1989;31(1):3–15. [Google Scholar]
- 57.Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Social Psychol Rev. 2011;15(3):219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Taylor RJ, Ellison CG, Chatters LM, et al. Mental health services in faith communities: the role of clergy in black churches. Soc Work. 2000;45(1):73–87. doi: 10.1093/sw/45.1.73. [DOI] [PubMed] [Google Scholar]
- 59.Wittink MN, Jin Hui J, Lewis LM, Barg FK. Losing faith and using faith: older African Americans discuss spirituality, religious activities, and depression. J Gen Intern Med. 2009;24(3):402–407. doi: 10.1007/s11606-008-0897-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kool MB, Geenen R. Loneliness in patients with rheumatic diseases: the significance of invalidation and lack of social support. J Psychol. 2012;146(1–2):229–241. doi: 10.1080/00223980.2011.606434. [DOI] [PubMed] [Google Scholar]
- 61.Kalkan M, Epli-Koc H. Perceived social support from friends as determinant of loneliness in a sample of primary school. US-China Education Review. 2011;8(4):547–551. [Google Scholar]
- 62.Schnittger RI, Wherton J, Prendergast D, Lawlor BA. Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults. Aging Mental Health. 2012;16(3):335–346. doi: 10.1080/13607863.2011.629092. [DOI] [PubMed] [Google Scholar]
- 63.Segrin C, Passalacqua SA. Functions of loneliness, social support, health behaviors, and stress in association with poor health. Health Commun. 2010;25(4):312–322. doi: 10.1080/10410231003773334. [DOI] [PubMed] [Google Scholar]
- 64.Anglin DM, Link BG, Phelan JC. Racial differences in stigmatizing attitudes toward people with mental illness. Psychiat Serv. 2006;57(6):857–862. doi: 10.1176/ps.2006.57.6.857. [DOI] [PubMed] [Google Scholar]
- 65.Long Foley K, Reed PS, Mutran EJ, DeVellis RF. Measurement adequacy of the CES-D among a sample of older African-Americans. Psychiat Res. 2002;109(1):61–69. doi: 10.1016/s0165-1781(01)00360-2. [DOI] [PubMed] [Google Scholar]
- 66.Conerly RC, Baker F, Dye J, et al. Measuring depression in African American cancer survivors: The reliability and validity of the center for epidemiologic study-depression (CES-D) scale. J Health Psychol. 2002;7(1):107–114. doi: 10.1177/1359105302007001658. [DOI] [PubMed] [Google Scholar]
- 67.Wohi M, Lesser I, Smith M. Clinical presentations of depression in African American and white outpatients. Cult Divers Ment Health. 1997;3(4):279–284. doi: 10.1037/1099-9809.3.4.279. [DOI] [PubMed] [Google Scholar]