Abstract
Background
Our objective was to characterize national trends in inflammatory bowel disease (IBD)-related hospitalizations for children. We hypothesized that over time, improvements in care would be associated with a decrease in hospitalization rates, similar to what has been observed in Canadian children with IBD.
Methods
Retrospective, serial, cross-sectional analysis of annual, nationally representative samples of children with IBD.
Results
Overall, discharges for all children irrespective of diagnosis decreased from 1988 to 2011 (P for trend <0.001). In contrast, discharges for children with IBD rose over the same time period from 6.1 (95% confidence interval [CI], 4.0–8.2) to 8.2 (95% CI, 5.5–10.9) per 100,000 individuals per year (P for trend <0.001). More of this rise occurred in hospitalizations that did not have IBD-related endoscopy or surgery performed (P for trend <0.001). Although mean length of stay decreased over the study period (P for trend <0.001), total hospital days increased over the latter half of the study with a significant increase over the entire study period (P for trend <0.001).
Conclusions
Contrary to clinically informed hypotheses, nationally representative rates of hospitalization for pediatric patients with IBD have increased since the mid-1990s. This directly contrasts with stable rates over the preceding years. Most of the expansion in hospital care seems to be related to hospitalizations that do not include procedures. Several lines of future research may greatly facilitate a better understanding of the epidemiologic, therapeutic, and health care resource issues at play.
Keywords: national trends, Crohn’s disease, ulcerative colitis, nationwide inpatient sample, variance-weighted regression
Management of pediatric inflammatory bowel disease (IBD) has changed markedly over the last 2 decades. Anti-tumor necrosis factor-a (anti-TNFa) therapies such as infliximab and adalimumab supplement immunomodulators and other therapies in the clinician’s armamentarium.[1] Surgical techniques and management for IBD have also evolved over the same time period.[2–7]
The impact of these shifts in clinical management of IBD on hospital care for these conditions has not been well characterized. Hospital care, as an indicator of morbidity, unmet care needs, and poorly controlled IBD, is a key measure of the impact of clinical advances. In Canada, rates of hospitalization and intra-abdominal surgery among universally insured patients with IBD declined among children during the years 1994 to 2007, concomitant with the increasing use of immunomodulators.[8] Limited evidence suggests that hospitalizations are also decreasing in subsets of adults with IBD in specific regions in the United States.9 However, trends for children over the past 2 decades in the United States remain largely unknown.
The central aim of this study was to characterize trends in hospital care for pediatric patients with IBD. We hypothesized that the United States would experience a decrease in hospitalization rates, similar to what has been observed in Canadian children with IBD.[8] By including all-payer data in the United States and by examining patient hospitalizations across 2 decades, we aimed to provide a comprehensive picture of changing hospitalization rates in the United States over time.
MATERIALS AND METHODS
Data Source
Children with IBD were identified from annual cross-sectional analyses of discharges using the Healthcare Cost and Utilization Project’s (HCUP) Nationwide Inpatient Sample (NIS), compiled by the Agency for Healthcare Research and Quality (AHRQ). Based on the sampling methodology and statistical weighting variables, discharge data were obtained that are generalizable to the U.S. population.[10] We used the NIS rather than the Kids’ Inpatient Database, also compiled by AHRQ, because we wanted to begin our study period before the advent of anti-TNFa therapies and analyze year-over-year trends, whereas the Kids’ Inpatient Database is only released every 3 years, and its data were not available until 1997. Year-over-year patterns of hospitalization for children and adults have been published based on the NIS.[11–13] Trends of all hospitalized children in the NIS were obtained from HCUPnet, an online, easy-to-use gateway into HCUP data.[14]
Our analysis included deidentified national data and was therefore considered exempt from our institutional review board. We used the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) checklist in reporting this study.[15]
Study Population and Definitions of Variables
Using the NIS, discharges for patients aged 1 to 17 years old with IBD were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes of 555.x (Crohn’s disease) and 556.x (ulcerative colitis). The combination of diagnosis codes used in defining the sample has been described previously and includes a primary diagnosis code of 555.x or 556.x and coding for an IBD-related complication.[16–18] We excluded discharges that did not include the 555.x and 556.x codes for IBD, discharges with codes of other forms of colitis (eosinophilic, allergic, microscopic, and ischemic), and discharges with codes for irritable bowel syndrome. Ages were combined to protect privacy, per AHRQ requirements when reporting small numbers.[19] Additionally, we created variables to capture IBD-related procedures, using endoscopic and surgical procedure codes used previously (see Table, Supplemental Digital Content 1, http://links.lww.com/IBD/A609).[20]
Nationally representative estimates of encounter-level information were obtained using statistical weights provided by AHRQ.[21] Hospital discharges were census adjusted for each respective calendar year[22] and reported as the number of discharges per 100,000 individuals per year. Trend corrections, available from HCUP, were applied to the analyses over the study period.[10]
We next obtained summary statistics for lengths of stay. As a secondary marker of hospitalization burden, we calculated total hospital days, determined by multiplying the annual mean length of stay by the census-adjusted discharge rate. We included an analysis of short stays, defined as 0 or 1 day duration, to indirectly address the possibility that hospitalizations for same-day infusions or procedures substantially contribute to the overall trend of hospitalizations. We also investigated the possibility that the recent rise in Clostridium difficile infections could be contributing to increases in hospitalization.[23–27]
Statistical Analysis
All analyses were conducted using Stata version 12.0 (StataCorp, College Station, TX). Appropriate survey estimation commands were used in Stata to account for the stratified sampling technique of the NIS. Trends across time were analyzed using the weighted estimates and the corresponding SEs. The P for trend test was conducted using variance-weighted leastsquares regression, an approach demonstrated previously.[28–30] Trends were analyzed over the entire study period (1988–2011) as yearly point estimates with 95% confidence intervals (CIs). We performed segmented regression where trends were discordant from the beginning to the end of the study period. Analyses were repeated with the second model using weighted negative binomial regression to account for count data and to ensure stable results.
RESULTS
Study Population
We identified a total of 24,816 unweighted discharges for children aged 1 to 17 years old with IBD from 1988 to 2011. A very small proportion of discharges contained codes for both Crohn’s disease and ulcerative colitis (1.1%; 95% CI, 1.0–1.1). There were missing data for less than 1% of discharges for gender and no missing data for age, length of stay, disease type, or procedures. Characteristics of the study sample are presented in Table 1. All analyses below were repeated with the second model using weighted negative binomial regression to account for count data and to ensure stable results (see Table, Supplemental Digital Content 2, http://links.lww.com/IBD/A610).
TABLE 1.
Characteristics of the Study Sample
| Characteristic |
Unweighted Discharges N ¼ 24,816 |
Weighted Discharges N ¼ 127,653 (95% CI) |
Weighted Percentage (95% CI) |
|---|---|---|---|
| Gender | |||
| Female | 12,145 | 62,098 (54,871–69,325) | 48.8a (47.9–49.8) |
| Age, yr | |||
| 1–9 | 3008 | 15,646 (13,285–18,007) | 12.3 (11.6–13.0) |
| 10–17 | 21,808 | 112,007 (99,300–124,713) | 87.7 (87.0–88.4) |
| Disease type | |||
| Crohn’s disease | 15,299 | 78,794 (69,318–88,271) | 61.7 (60.6–62.8) |
| Ulcerative colitis | 9237 | 47,466 (41,917–53,016) | 37.2 (36.1–38.3) |
| Bothb | 280 | 1392 (1155–1629) | 1.1 (1.0–1.2) |
| Discharges | |||
| With IBD procedures | 12,447 | 64,053 (56,428–71,678) | 50.2 (48.9–51.4) |
| Without IBD procedures | 12,369 | 63,600 (55,992–71,207) | 49.8 (48.6–51.1) |
Weighted percentage for gender is discrepant due to missing data (108 of 24,816 missing).
Approximately, 1% of discharges contained codes for both Crohn’s disease and ulcerative colitis.
Overall Trends and IBD-specific Trends in Hospital Care
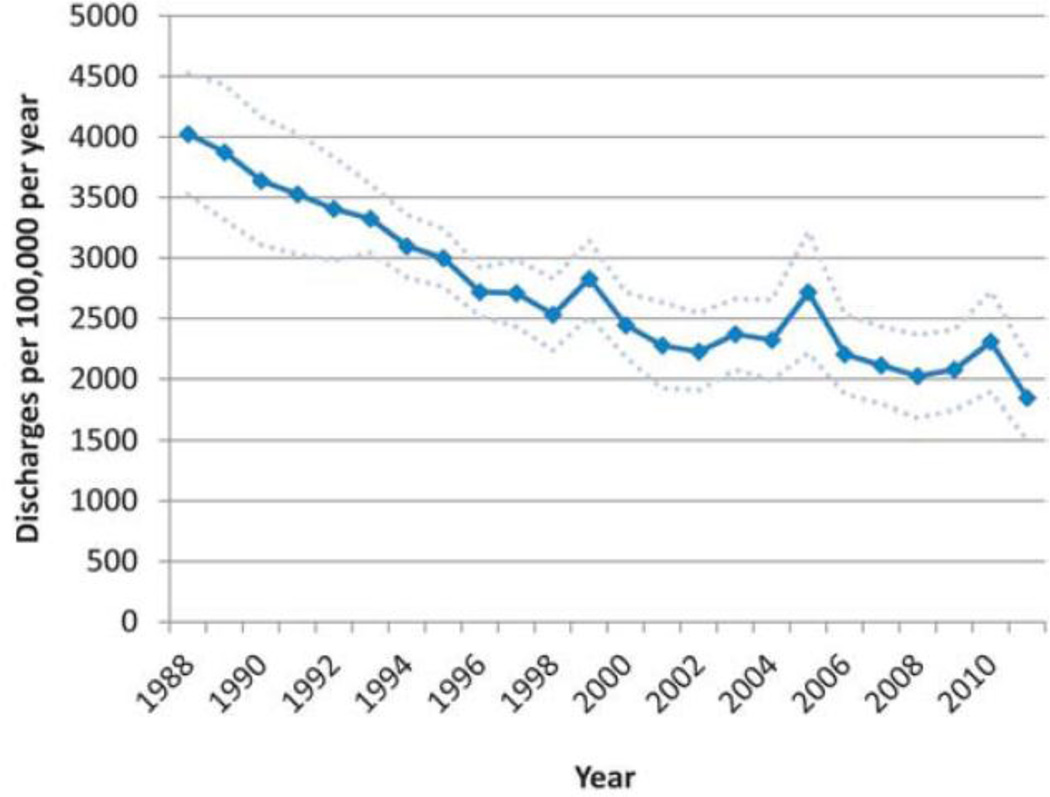
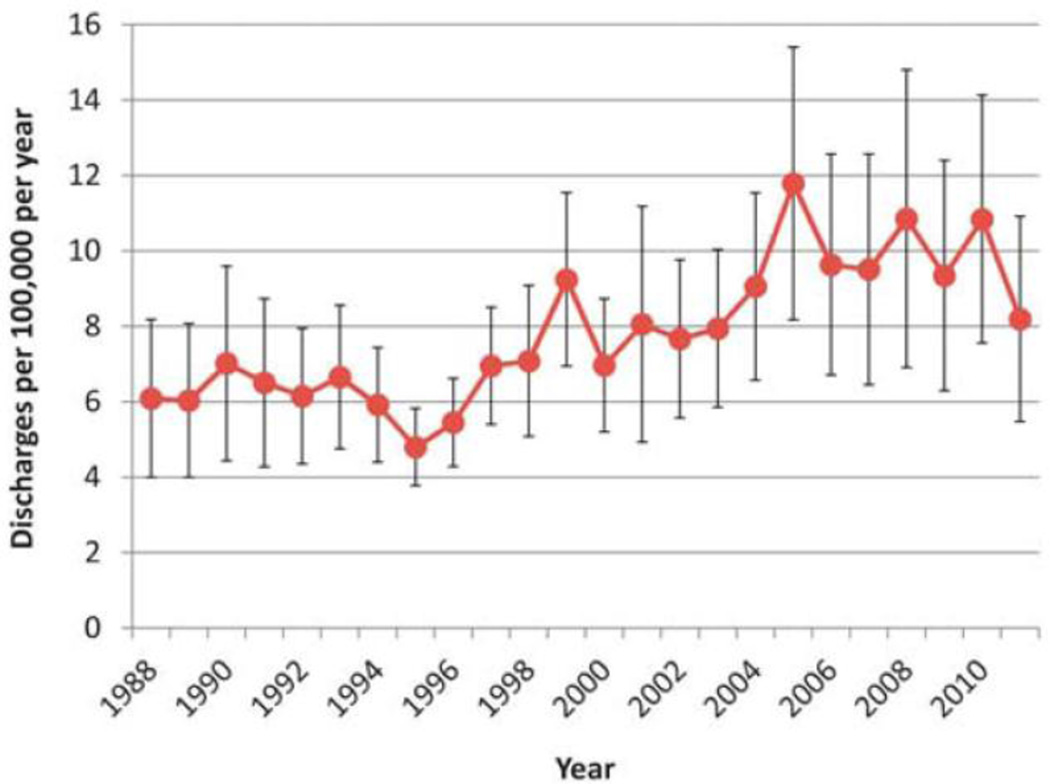
Overall, discharges for all children aged 1 to 17 years old in the United States, irrespective of diagnosis, decreased from 4026 (95% CI, 3525–4528) per 100,000 individuals per year in 1988 to 1846 (95% CI, 1504–2187) per 100,000 individuals per year in 2011 (P for trend <0.001; Fig. 1). In contrast, discharges for children aged 1 to 17 years old with IBD in the United States rose over the same time period from 6.1 (95% CI, 4.0–8.2) per 100,000 individuals per year in 1988 to 8.2 (95% CI, 5.5–10.9) per 100,000 individuals per year in 2011 (P for trend <0.001; Fig. 2). The increase in discharge frequency occurred chiefly in the later years, beginning in the mid-1990s. Discharges excluding short stays (≤1 d) did not change the significance in overall trend in rates and did not represent a majority of the increase seen over the latter part of the study period (see Fig., Supplemental Digital Content 3, http://links.lww.com/IBD/A611). IBD discharges for which infections with C. difficile were coded, accounted for a small proportion (2.1%; 95% CI, 1.8–2.4) of total IBD discharges from 1994 to 2011. We are unable to report annual estimates, as earlier years contained insufficient numbers to report and maintain confidentiality.
FIGURE 1. Total hospitalizations with any diagnosis, 1 to 17 years old.
Overall, discharges decreased from 1988 to 2011 (P for trend <0.001). Each upper and lower bound traces (dotted lines) represent 2 SEs from the mean, as 95% CIs were not available from HCUPnet.
FIGURE 2. IBD hospitalizations, 1 to 17 years old.
In contrast to the overall trend, discharges for children with IBD increased from 6.1 (95% CI, 4.0–8.2) per 100,000 per year in 1988 to 8.2 (95% CI, 5.5–10.9) per 100,000 per year in 2011 (P for trend <0.001).
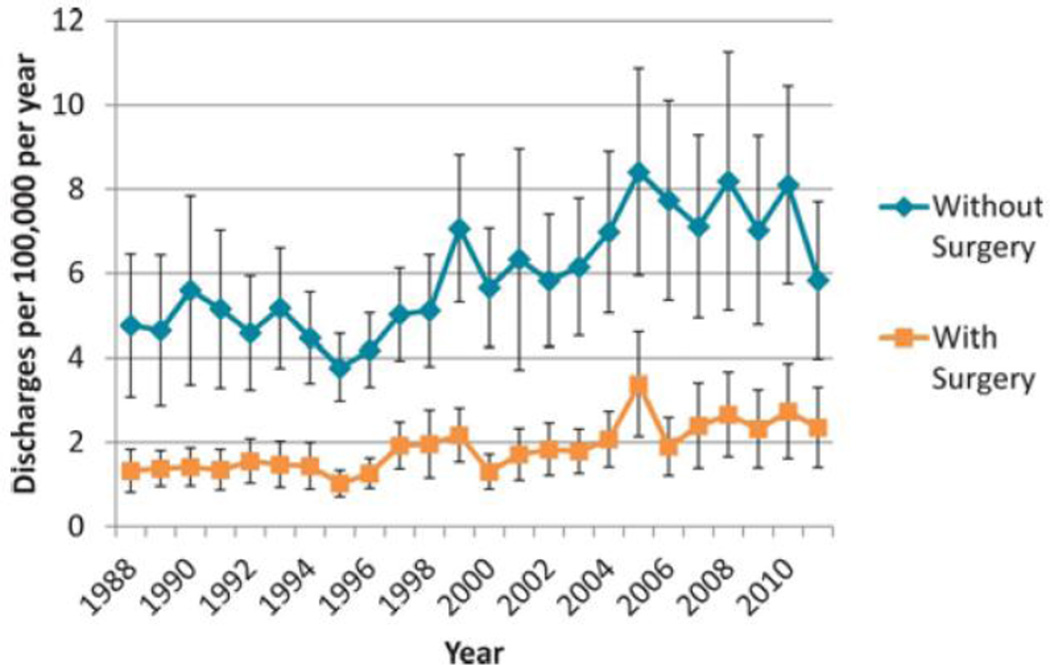
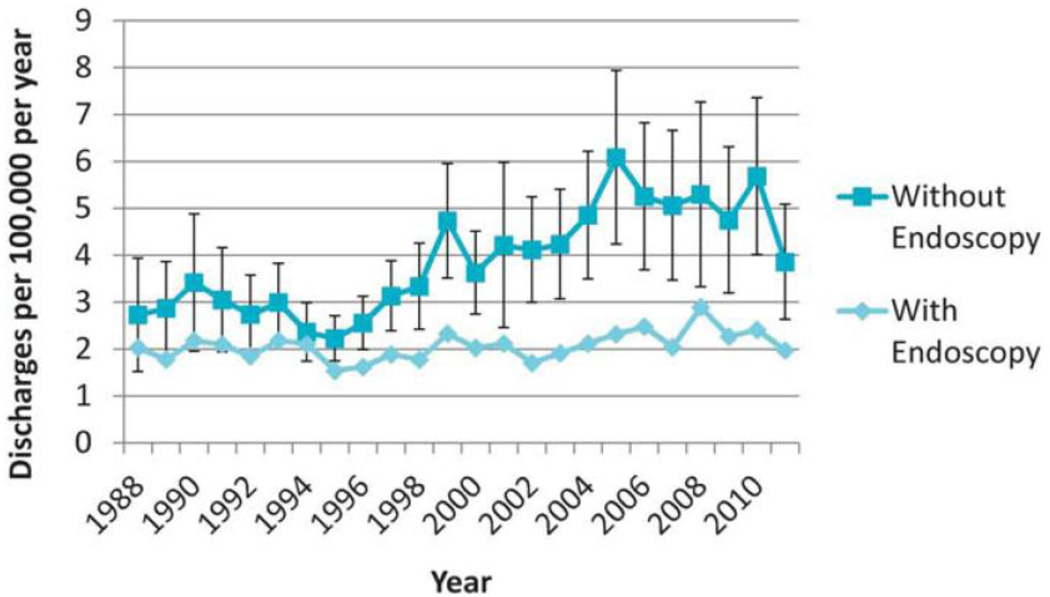
Trends in Hospitalizations With and Without Surgery
Both hospitalizations with and without surgeries significantly increased over the study period (Ps for trend <0.001; Fig. 3), but the rate in rise is more evident in those hospitalizations without surgery. Hospitalizations without surgeries were further analyzed (Fig. 4). Of hospitalizations without surgeries, those without endoscopy rose significantly (P for trend <0.001), whereas the trend in hospitalizations with endoscopy did not significantly change over the study period (P for trend = 0.078).
FIGURE 3. Hospitalizations with and without surgeries.
Both hospitalizations with and without surgeries significantly increased over the study period (Ps for trend <0.001), but the rate in rise is more evident in those hospitalizations without surgery.
FIGURE 4. Hospitalizations without surgeries, by endoscopy.
Among hospitalizations without surgeries, those without endoscopy rose significantly (P for trend <0.001), whereas those with endoscopy did not significantly change over the study period (P for trend = 0.078).
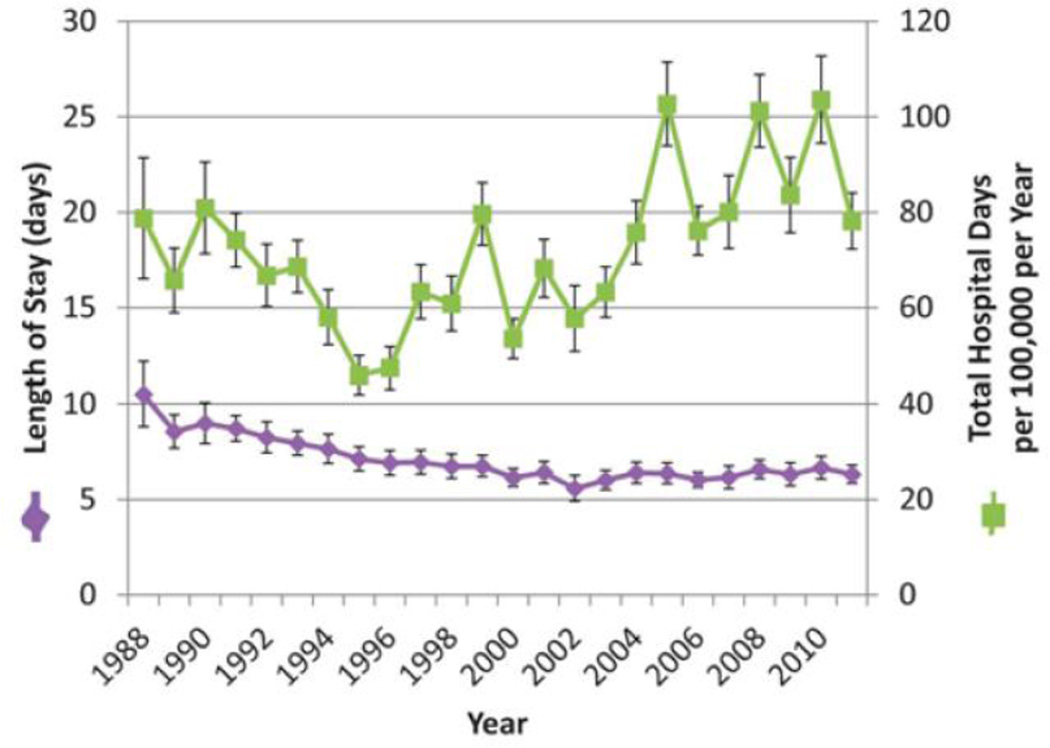
Trends in Length of Stay and Total Hospital Days
Mean lengths of stay for IBD-related hospital care decreased over the study period from 10.5 (95% CI, 8.8–12.2) to 6.3 days (95% CI, 5.8–6.8; P for trend <0.001; Fig. 5). IBD-related total hospital days were 79 (95% CI, 66–91) per 100,000 individuals per year in 1988. Total hospital days decreased to 46 (42–50) per 100,000 individuals per year in 1995 (P for trend <0.001; 1988–1995) before increasing through the end of the study period to 78 (95% CI, 72–84; P for trend <0.001; 1996–2011). Of note, the overall trend in hospital days rose significantly from 1988 to 2011 (P for trend <0.001).
FIGURE 5. Hospital length of stay and total hospital days.
Mean lengths of stay for IBD-related hospital care decreased over the study period from 10.5 (95% CI, 8.8–12.2) to 6.3 days (95% CI, 5.8–6.8; P for trend <0.001). IBD-related total hospital days were 79 (95% CI, 66–91) per 100,000 individuals per year in 1988. Total hospital days decreased to 46 (42–50) per 100,000 per year in 1995 (P for trend <0.001, 1988–1995), before increasing through the end of the study period to 78 (95% CI, 72–84; P for trend <0.001, 1996–2011). Of note, the overall trend in hospital days rose significantly from 1988 to 2011 (P for trend <0.001).
DISCUSSION
In this assessment of nearly a quarter century of hospital discharges for children with IBD in the United States, we have identified an increasing rate of hospitalizations. This rise is consistent with other recent analyses of IBD trends in children,[18,31] although these studies are over a much shorter time period and report only interrupted time trends. In contrast with our findings of increasing rates of hospitalization in IBD, other analyses of HCUP data have shown stable or decreasing rates of other chronic diseases in childhood.[32–34] This seems to suggest that IBD is different from other chronic diseases in its need for inpatient resources.
It is noteworthy that the greatest increase in hospitalizations without procedures coincides with the increase in total hospitalizations after the mid-1990s. The reasons for the rise in nonprocedural hospitalization rates over the past decade among children are unclear and merit further examination. Explanations and future areas of research for our findings may include a possible shifting epidemiology of disease, evolving clinical management, and disparities in healthcare resource utilization.
Epidemiology of IBD Informed by Hospitalization Patterns
Overall disease incidence and prevalence patterns for children with IBD at the national level are not well established. A recent systematic review of international trends including 32 countries identified an overall increase in incidence in both Crohn’s disease and ulcerative colitis from the 1960s to early 2000s.[35] The 2 U.S. studies addressing temporal trends included in this review were limited to 2 different time periods and geographic regions. They also identified contradictory results: a 118% increase in incidence in a single institution in Texas[36] and an 11% decrease in a statewide population study in Minnesota.[37] A national study of U.S. private payer data found a less than 10% increase in prevalence from 2004 to 2009.[38] Taken together, these studies illustrate the limited data available to inform current understanding of changes in disease prevalence. In other locales where long-term data are available, a gradual increase in incidence is seen.[35] In the context of our study, it seems unlikely that a change in disease epidemiology alone is responsible for the abrupt increase. Additionally, as our data include hospitalizations only (not outpatient visits), our estimates likely under-represent national prevalence. Further work, including direct measurement of disease incidence and prevalence in the United States, is needed to help address this question.
Evolving Therapies for IBD
Substantial changes in IBD therapy have occurred during our study period, notably the introduction of anti-TNFa therapies in 1998.[39] Although the Food and Drug Administration did not approve infliximab for use in pediatric Crohn’s disease until 2006,[40] it may have been used off-label, similar to many other medications in pediatrics.[41–45] Additionally, thiopurine medications, such as azathioprine and 6-mercaptopurine, have been used to treat Crohn’s disease since the early 1960s, but were not widely used until more recently in the 1990s, before the introduction of anti-TNFa therapies.[1,46,47] The extent to which anti-TNFa therapies or thiopurines have gained favor in practice at the national level for children is unknown. This remains a ripe area for future investigation.
It is noteworthy that anti-TNFa therapies were approved for use immediately before the rise in IBD-related discharges for children seen in our study. This temporal association is intriguing, though of unclear significance. The association may be explained by medical causes (e.g., infections or other complications of therapy) or system-based changes (e.g., limited outpatient infusion sources). The proportionally small numbers of short-stay hospitalizations throughout the study period and during the last decade of study suggest that same-day infusions are not driving the overall increase in hospitalizations. Further investigation is warranted to clarify what relationship, if any, exists between anti-TNFa therapies and trends in hospital care for children.
Changes in surgical technique may also have affected discharge rates during the study period. For multistage surgeries involving bowel resection, temporary diverting ostomy, and subsequent anastomosis, there has been a shift in practice pattern from a 1 or 2 surgery sequence to the current predominant practice pattern involving 2 or 3 surgeries.[5,48] If all other factors remained constant, we would expect to see an increase in the per capita rate of discharges where an IBD-related surgery was performed. Although our data support the finding of increasing surgical hospitalizations, these hospitalizations do not seem to be the driving force in the rise of all IBD hospitalizations. It was beyond the scope of this study to investigate the nuances of surgical procedure patterns and coding, which also remains an important focus of future work.
Infections with C. difficile did not appear to represent a major driver of increasing hospitalizations in this study. Investigation into other infections that complicate care for IBD may shed additional light onto how comorbid conditions and immunosuppressant therapies affect IBD hospitalizations.
Health Care Resource Utilization for IBD
Length of stay for hospital discharges with IBD decreased throughout our study. This trend generally mirrors those found in other studies during the same time period,[33,49] suggesting that decreases in length of stay are not an IBD-specific trend. Moreover, because of the increase in frequency of discharges, the total number of patient days in the hospital is increasing over time at the national level. Of note, the nadir of total hospital days coincides with the time period of widespread managed care pressures on hospital resource utilization in the mid-1990s. This highlights not only the need for understanding the rise in discharges for IBD but also in understanding indications for hospital admission. For example, premature discharge may result in readmissions and potentially increase the number of discharges and overall total hospital days. This phenomenon, which cannot be discerned with deidentified data in this study, would be important to assess with longitudinal patient-level data like those used in the recent study from Ontario.[8]
Variation in outpatient management may also lead to increased use of the hospital in diagnosis and management of patients with IBD. Changes in outpatient management could potentially be related to temporal shifts in the workforce (e.g., nurse practitioner versus physician, adult versus pediatric, generalist versus subspecialist, medical versus surgical) or utilization of these clinicians within new or changing systems that could potentially lead to disparate rates of hospital utilization. In the setting of scarce provider resources, various hybrid models of care could enable adequate coverage, by extending subspecialists’ expertise in initial evaluations and cooperative management with hospitalists[50] and primary care physicians,[51] or through telemedicine.[52–56] A natural experiment of these strategies could also inform our understanding of hospital utilization.
Limitations
This study has several important limitations common to studies using hospital administrative data. First, the NIS contains encounter-level data. As such, we are unable to assess for hospital readmissions or make patient-level associations across discharges. Second, we were reliant on the coding process, which may have underestimated or overestimated discharges with IBD. We are not aware of coding changes related to IBD that would have led to case identification at higher rates later in the study period. If the increase seen were due to temporal coding changes, we would expect an initial change with return to a steady discharge rate, which was not seen. Third, risk stratification for disease severity and comorbidities would enable investigators to put trends of discharges and lengths of stay into perspective. Although administrative data risk scores to stratify severity of some IBD hospitalizations are available,[20,57,58] they have not been validated for study in pediatric patients. Fourth, medication data were not available for examination, which precludes direct assessment of whether treatment with anti-TNFa therapies was associated with patterns of hospital care for IBD; we instead report temporal associations.
CONCLUSIONS
Contrary to clinically informed hypotheses, nationally representative rates of hospitalization for children with IBD have increased since the mid-1990s. This directly contrasts with stable rates over the preceding years. Moreover, most of the growth in the frequency of hospital care seems to be related to hospitalizations that do not include surgical or endoscopic procedures. Several lines of future research may greatly facilitate a better understanding of the epidemiologic, therapeutic, and health care resource issues at play.
Supplementary Material
REFERENCES
- 1.Markowitz J, Grancher K, Kohn N, et al. Immunomodulatory therapy for pediatric inflammatory bowel disease: changing patterns of use, 1990–2000. Am J Gastroenterol. 2002;97:928–932. doi: 10.1111/j.1572-0241.2002.05611.x. [DOI] [PubMed] [Google Scholar]
- 2.Hwang JM, Varma MG. Surgery for inflammatory bowel disease. World J Gastroenterol. 2008;14:2678–2690. doi: 10.3748/wjg.14.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nandivada P, Poylin V, Nagle D. Advances in the surgical management of inflammatory bowel disease. Curr Opin Gastroenterol. 2012;28:47–51. doi: 10.1097/MOG.0b013e32834d8fcb. [DOI] [PubMed] [Google Scholar]
- 4.Fichera A, Michelassi F. Surgical treatment of Crohn’s disease. J Gastrointest Surg. 2007;11:791–803. doi: 10.1007/s11605-006-0068-9. [DOI] [PubMed] [Google Scholar]
- 5.Gardiner KR, Dasari BVM. Operative management of small bowel Crohn’s disease. Surg Clin North Am. 2007;87:587–610. doi: 10.1016/j.suc.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Leonor R, Jacobson K, Pinsk V, et al. Surgical intervention in children with Crohn’s disease. Int J Colorectal Dis. 2007;22:1037–1041. doi: 10.1007/s00384-007-0281-3. [DOI] [PubMed] [Google Scholar]
- 7.Umanskiy K, Fichera A. Health related quality of life in inflammatory bowel disease: the impact of surgical therapy. World J Gastroenterol. 2010;16:5024–5034. doi: 10.3748/wjg.v16.i40.5024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benchimol EI, Guttmann A, To T, et al. Changes to surgical and hospitalization rates of pediatric inflammatory bowel disease in Ontario, Canada (1994–2007) Inflamm Bowel Dis. 2011;17:2153–2161. doi: 10.1002/ibd.21591. [DOI] [PubMed] [Google Scholar]
- 9.Herrinton LJ, Liu L, Fireman B, et al. Time trends in therapies and outcomes for adult inflammatory bowel disease, Northern California, 1998–2005. Gastroenterology. 2009;137:502–511. doi: 10.1053/j.gastro.2009.04.063. [DOI] [PubMed] [Google Scholar]
- 10.AHRQ. [Accessed January 19, 2013];Overview of the nationwide inpatient sample. Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 11.Davis MM, Patel MS, Gebremariam A. Decline in varicella-related hospitalizations and expenditures for children and adults after introduction of varicella vaccine in the United States. Pediatrics. 2004;114:786–792. doi: 10.1542/peds.2004-0012. [DOI] [PubMed] [Google Scholar]
- 12.Patel MS, Gebremariam A, Davis MM. Herpes zoster-related hospitalizations and expenditures before and after introduction of the varicella vaccine in the United States. Infect Control Hosp Epidemiol. 2008;29:1157–1163. doi: 10.1086/591975. [DOI] [PubMed] [Google Scholar]
- 13.Zickafoose JS, Benneyworth BD, Riebschleger MP, et al. Hospitalizations for intussusception before and after the reintroduction of rotavirus vaccine in the United States. Arch Pediatr Adolesc Med. 2012;166:350–355. doi: 10.1001/archpediatrics.2011.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.AHRQ. [Accessed February 5, 2014];Welcome to HCUPnet. HCUPnet: a tool for identifying, tracking, and analyzing national hospital statistics. Available at: http://hcupnet.ahrq.gov/
- 15.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:W163–W194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 16.Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol. 2008;103:2789–2798. doi: 10.1111/j.1572-0241.2008.02054.x. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen GC, Bayless TM, Powe NR, et al. Race and health insurance are predictors of hospitalized Crohn’s disease patients undergoing bowel resection. Inflamm Bowel Dis. 2007;13:1408–1416. doi: 10.1002/ibd.20200. [DOI] [PubMed] [Google Scholar]
- 18.Pant C, Anderson MP, Deshpande A, et al. Trends in hospitalizations of children with inflammatory bowel disease within the United States from 2000 to 2009. J Investig Med. 2013;61:1036–1038. doi: 10.2310/JIM.0b013e31829a4e25. [DOI] [PubMed] [Google Scholar]
- 19.AHRQ. [Accessed January 19, 2013];Requirements for publishing with HCUP data. Available at: http://www.hcup-us.ahrq.gov/db/publishing.jsp.
- 20.Ananthakrishnan AN, McGinley EL, Binion DG, et al. A novel risk score to stratify severity of Crohn’s disease hospitalizations. Am J Gastroenterol. 2010;105:1799–1807. doi: 10.1038/ajg.2010.105. [DOI] [PubMed] [Google Scholar]
- 21.AHRQ. [Accessed March 11, 2014];HCUP on-line tutorial series. Available at: http://www.hcup-us.ahrq.gov/tech_assist/tutorials.jsp.
- 22.US Census Bureau DID. [Accessed January 7, 2013];Population estimates. Available at: http://www.census.gov/popest/data/intercensal/national/nat2010.html.
- 23.Navaneethan U, Venkatesh PG, Shen B. Clostridium difficile infection and inflammatory bowel disease: understanding the evolving relationship. World J Gastroenterol. 2010;16:4892–4904. doi: 10.3748/wjg.v16.i39.4892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ananthakrishnan AN, McGinley EL, Saeian K, et al. Temporal trends in disease outcomes related to Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:976–983. doi: 10.1002/ibd.21457. [DOI] [PubMed] [Google Scholar]
- 25.Ananthakrishnan AN. Clostridium difficile infection: epidemiology, risk factors and management. Nat Rev Gastroenterol Hepatol. 2011;8:17–26. doi: 10.1038/nrgastro.2010.190. [DOI] [PubMed] [Google Scholar]
- 26.Dumyati G, Stevens V, Hannett GE, et al. Community-associated Clostridium difficile infections, Monroe County, New York, USA. Emerging Infect Dis. 2012;18:392–400. doi: 10.3201/eid1803.102023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khanna S, Pardi DS, Aronson SL, et al. The epidemiology of community acquired Clostridium difficile infection: a population-based study. Am J Gastroenterol. 2012;107:89–95. doi: 10.1038/ajg.2011.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patrick SW, Schumacher RE, Benneyworth BD, et al. Neonatal abstinence syndrome and associated health care expenditures United States, 2000–2009. JAMA. 2012;307:1934–1940. doi: 10.1001/jama.2012.3951. [DOI] [PubMed] [Google Scholar]
- 29.Benneyworth BD, Gebremariam A, Clark SJ, et al. Inpatient health care utilization for children dependent on long-term mechanical ventilation. Pediatrics. 2011;127:e1533–e1541. doi: 10.1542/peds.2010-2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weisberg S. Applied linear regression. In: Balding DJ, Cressie NAC, Fisher NI, editors. Wiley Series in Probability and Statistics. 3rd. Hoboken, NJ: Wiley-Interscience; 2005. [Google Scholar]
- 31.Debruyn JCC, Soon IS, Hubbard J, et al. Nationwide temporal trends in incidence of hospitalization and surgical intestinal resection in pediatric inflammatory bowel diseases in the United States from 1997 to 2009. Inflamm Bowel Dis. 2013;19:2423–2432. doi: 10.1097/MIB.0b013e3182a56148. [DOI] [PubMed] [Google Scholar]
- 32.Hasegawa K, Tsugawa Y, Brown DFM, et al. Childhood asthma hospitalizations in the United States, 2000–2009. J Pediatr. 2013;163:1127.e3–1133.e3. doi: 10.1016/j.jpeds.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raphael JL, Mueller BU, Kowalkowski MA, et al. Shorter hospitalization trends among children with sickle cell disease. [Accessed March 13, 2013];Pediatr Blood Cancer. 2012 doi: 10.1002/pbc.24065. Available at: http://onlinelibrary.wiley.com/doi/10.1002/pbc.24065/full. [DOI] [PubMed] [Google Scholar]
- 34.Wei CC, Wang W, Smoyer WE, et al. Trends in pediatric primary membranoproliferative glomerulonephritis costs and complications. Pediatr Nephrol. 2012;27:2243–2250. doi: 10.1007/s00467-012-2249-y. [DOI] [PubMed] [Google Scholar]
- 35.Benchimol EI, Fortinsky KJ, Gozdyra P, et al. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2011;17:423–439. doi: 10.1002/ibd.21349. [DOI] [PubMed] [Google Scholar]
- 36.Malaty HM, Fan X, Opekun AR, et al. Rising incidence of inflammatory bowel disease among children: a 12-year study. J Pediatr Gastroenterol Nutr. 2010;50:27–31. doi: 10.1097/MPG.0b013e3181b99baa. [DOI] [PubMed] [Google Scholar]
- 37.Loftus CG, Loftus EV, Harmsen WS, et al. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940–2000. Inflamm Bowel Dis. 2007;13:254–261. doi: 10.1002/ibd.20029. [DOI] [PubMed] [Google Scholar]
- 38.Kappelman MD, Moore KR, Allen JK, et al. Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Dig Dis Sci. 2012;58:519–525. doi: 10.1007/s10620-012-2371-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.FDA. [Accessed June 4, 2013];Infliximab product approval information: licensing action. Available at: http://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/ApprovalApplications/TherapeuticBiologicApplications/ucm093327.htm.
- 40.FDA. [Accessed June 4, 2013];FDA approves remicade for children with Crohn’s disease. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2006/ucm108656.htm.
- 41.Shah SS, Hall M, Goodman DM, et al. Off-label drug use in hospitalized children. Arch Pediatr Adolesc Med. 2007;161:282–290. doi: 10.1001/archpedi.161.3.282. [DOI] [PubMed] [Google Scholar]
- 42.Yoon EY, Dombkowski KJ, Rocchini A, et al. Off-label utilization of antihypertensive medications in children. Ambul Pediatr. 2007;7:299–303. doi: 10.1016/j.ambp.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Conroy S, Choonara I, Impicciatore P, et al. Survey of unlicensed and off label drug use in paediatric wards in European countries. European network for drug investigation in children. BMJ. 2000;320:79–82. doi: 10.1136/bmj.320.7227.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Turner S, Longworth A, Nunn AJ, et al. Unlicensed and off label drug use in paediatric wards: prospective study. BMJ. 1998;316:343–345. doi: 10.1136/bmj.316.7128.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pandolfini C, Impicciatore P, Provasi D, et al. Off-label use of drugs in Italy: a prospective, observational and multicentre study. Acta Paediatr. 2002;91:339–347. doi: 10.1080/08035250252834030. [DOI] [PubMed] [Google Scholar]
- 46.Ramadas AV, Gunesh S, Thomas GAO, et al. Natural history of Crohn’s disease in a population-based cohort from Cardiff (1986–2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–1206. doi: 10.1136/gut.2009.202101. [DOI] [PubMed] [Google Scholar]
- 47.Park SH, Yang SK, Park SK, et al. Long-term prognosis of Crohn’s disease and its temporal change between 1981 and 2012: a hospital based cohort study from Korea. Inflamm Bowel Dis. 2014;20:488–494. doi: 10.1097/01.MIB.0000441203.56196.46. [DOI] [PubMed] [Google Scholar]
- 48.Malafosse M. Crohn’s disease: current surgical treatment (article in French) Bull Acad Natl Med. 2007;191:1143–1156. discussion 1157–1158. [PubMed] [Google Scholar]
- 49.Pati S, Lorch SA, Lee GE, et al. Health insurance and length of stay for children hospitalized with community-acquired pneumonia. J Hosp Med. 2012;7:304–310. doi: 10.1002/jhm.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bekmezian A, Chung PJ, Yazdani S. Staff-only pediatric hospitalist care of patients with medically complex subspecialty conditions in a major teaching hospital. Arch Pediatr Adolesc Med. 2008;162:975–980. doi: 10.1001/archpedi.162.10.975. [DOI] [PubMed] [Google Scholar]
- 51.Di Guglielmo MD, Plesnick J, Greenspan JS, et al. A new model to decrease time-to-appointment wait for gastroenterology evaluation. Pediatrics. 2013;131:e1632–e1638. doi: 10.1542/peds.2012-2372. [DOI] [PubMed] [Google Scholar]
- 52.Marcin JP, Ellis J, Mawis R, et al. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113:1–6. doi: 10.1542/peds.113.1.1. [DOI] [PubMed] [Google Scholar]
- 53.Mattioli L, Goertz K, Ardinger R, et al. Pediatric cardiology: auscultation from 280 miles away. Kans Med. 1992;93:326, 347–350. [PubMed] [Google Scholar]
- 54.Mulgrew KW, Shaikh U, Nettiksimmons J. Comparison of parent satisfaction with care for childhood obesity delivered face-to-face and by telemedicine. Telemed J E Health. 2011;17:383–387. doi: 10.1089/tmj.2010.0153. [DOI] [PubMed] [Google Scholar]
- 55.Mahnke CB, Jordan CP, Bergvall E, et al. The pacific asynchronous teleHealth (PATH) system: review of 1,000 pediatric teleconsultations. Telemed J E Health. 2011;17:35–39. doi: 10.1089/tmj.2010.0089. [DOI] [PubMed] [Google Scholar]
- 56.Malone F, Callahan CW, Chan DS, et al. Caring for children with asthma through teleconsultation: “ECHO-Pac, the electronic children’s hospital of the pacific”. Telemed J E Health. 2004;10:138–146. doi: 10.1089/tmj.2004.10.138. [DOI] [PubMed] [Google Scholar]
- 57.Ananthakrishnan AN, McGinley EL, Binion DG, et al. Simple score to identify colectomy risk in ulcerative colitis hospitalizations. Inflamm Bowel Dis. 2010;16:1532–1540. doi: 10.1002/ibd.21225. [DOI] [PubMed] [Google Scholar]
- 58.Kaplan GG. Editorial: administrative database studies in IBD: a cautionary tale. Am J Gastroenterol. 2010;105:1808–1810. doi: 10.1038/ajg.2010.232. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.