Abstract
Objectives
To determine if street triage is effective at reducing the total number of people with mental health needs detained under section 136, and is associated with cost savings compared to usual police response.
Design
Routine data from a 6-month period in the year before and after the implementation of a street triage scheme were used to explore detentions under section 136, and to populate a decision analytic model to explore the impact of street triage on the cost to the NHS and the criminal justice sector of supporting people with a mental health need.
Setting
A predefined area of Sussex, South East England, UK.
Participants
All people who were detained under section 136 within the predefined area or had contact with the street triage team.
Interventions
The street triage model used here was based on a psychiatric nurse attending incidents with a police constable.
Primary and secondary outcome measures
The primary outcome was change in the total number of detentions under section 136 between the before and after periods assessed. Secondary analysis focused on whether the additional costs of street triage were offset by cost savings as a result of changes in detentions under section 136.
Results
Detentions under section 136 in the street triage period were significantly lower than in the usual response period (118 vs 194 incidents, respectively; χ2 (1df) 18.542, p<0.001). Total NHS and criminal justice costs were estimated to be £1043 in the street triage period compared to £1077 in the usual response period.
Conclusions
Investment in street triage was offset by savings as a result of reduced detentions under section 136, particularly detentions in custody. Data available did not include assessment of patient outcomes, so a full economic evaluation was not possible.
Keywords: MENTAL HEALTH, HEALTH ECONOMICS, HEALTH SERVICES ADMINISTRATION & MANAGEMENT
Strengths and limitations of this study.
This is the first study of street triage in the UK, and so provides the first indication of potential impact of a national roll-out of such a programme.
This is a pragmatic evaluation which makes use of routinely collected data.
The study design is limited by the lack of patient outcome data necessary to carry out a full economic evaluation, so the cost-effectiveness of street triage is still unknown.
The economic model relies on a number of assumptions, although these were selected to be conservative in order to avoid overestimating the expected benefits of street triage.
Introduction
The importance of investment in the interface between mental health services and the criminal justice system (CJS) has been highlighted,1 with research identifying substantial gaps between the two sectors for individuals with enduring moderate to severe mental health needs,2–4 and policy documents calling for better working between police and the National Health Service (NHS).2 3 A recent government press release5 described the new concept of street triage, where mental health nurses accompany police officers to incidents where there is an indication that someone is in need of mental healthcare. The aim is to provide support, assessment, care and treatment as quickly as possible. Initial reports suggest that street triage can help keep people out of custodial settings on section 136 of the Mental Health Act 1983 (removal of an apparently mentally disordered person from a public place to a place of safety), thus reducing demands on police time and resources.5 Further, economic modelling suggests that the implementation of street triage would have minimal effects on individual-level average costs.6 However, no evaluation of street triage services has been undertaken, so the effectiveness and cost-effectiveness of the service is unknown. This study used routinely available data to determine if street triage could reduce the total number of people with mental health needs detained under section 136, and if it is associated with cost savings compared to usual police response.
Methods
Setting
The evaluation uses data from Sussex Partnership NHS Trust, one site chosen to pilot street triage in the UK. Street triage was implemented in Eastbourne, a defined catchment area within Sussex.
Design
Routine data from a 6-month period in the year before and after the implementation of a street triage scheme were used to explore detentions under section 136, and to populate a decision analytic model. Street triage started in October 2013. Allowing for a 6-month ‘settling-in period’, data from 1 April to 30 September 2014 (the ‘after’ or ‘street triage’ arm) was compared with data from 1 April to 30 September 2013 before street triage was established (the ‘before’ or ‘usual response’ arm).
Data
Data were provided by the Sussex Partnership NHS Foundation Trust on the number of people within the street triage catchment area being brought to custody or to an NHS place of safety under section 136 in the two 6-month periods of interest.
Data were also available on the street triage team response to mental health-related incidents, such as referral to other services, for the last 4 months of the 6-month ‘after’ period. In analysis, these data were extrapolated to cover the full 6-month period, taking the mean number of responses per month and multiplying by six.
To test whether differences in detentions under section 136 before and after street triage were due to the implementation of street triage or were a result of other unrecorded factors in the area, we also examined detentions under section 136 in the rest of Sussex over the same two periods. Eastbourne is a somewhat deprived (although not the most deprived) area in Sussex, has a similar population size to the other local authority districts in Sussex, and is mostly urban like most of the other districts.
Sample
The sample consisted of all people thought to have mental health needs who came to the attention of the police and were subject to, or potentially could have been subject to, detention under section 136 of the Mental Health Act over the two time periods, in the street triage catchment area and Sussex as a whole.
Interventions
Various models of street triage exist. The model of street triage implemented in Sussex contains the following key elements:
The street triage team consists of one dedicated police constable and one psychiatric nurse;
The team physically attends the scene of incidents reported, unless they are already attending another incident, in which case telephone support is provided;
Call handlers filter calls to Sussex Police and allocate incidents to the street triage team if there is an indication that the incident requires support for mental health needs or crises;
The street triage team are not the initial response to emergency or life-threatening events;
Street triage respond in an unmarked police car, but the officer wears standard police uniform and the nurse wears a lanyard and an arm band with ‘nurse’ printed on it;
Street triage is available during hours of peak need, including Wednesday to Friday 16.30 to 00.00, and 09.00 to 00.00 on Saturday and Sunday, thus, there are periods when street triage is unavailable.
Usual response to mental health incidents, prior to implementation of street triage and during periods when street triage is unavailable, consists of police attendance at all incidents. Police officers then make a decision on whether to detain the individual under section 136 and take them to a place of safety, or to take no further action.
Economic evaluation
Resources and unit costs
The economic analysis took an NHS and criminal justice sector perspective, including police and street triage response to an incident, and the immediate actions taken (referral to services, detention under section 136 and taken to custody or hospital), therefore, a 1-day time horizon was adopted. Unit costs applied to resource use data, and the source of the unit costs are detailed in online supplementary appendix 1. All costs are nationally applicable and reported in pounds sterling for the 2013–2014 financial year. Discounting was not applied as each period of the study was <1 year.
Street triage was costed using a top-down (or macro) costing approach, which involves taking the total cost of a service and dividing this by the total number of service contacts. A microcosting approach, involving a bottom-up calculation of the cost of each service contact for each individual is known to underestimate the total cost of a service, due to the difficulty of allocating all relevant indirect resources (those not directly associated with an individual service user, such as training, supervision, managerial and administrative overheads, etc) on an individual basis, and so the macrocosting approach was considered to be a more conservative estimate. Macrocosting involved calculation of the cost of one police officer and one mental health nurse to provide street triage for 52.5 hours/week, over the 26-week period of the study. Unit costs, detailed in online supplementary appendix 1, were based on relevant salary scales and included employer on-costs (national insurance and superannuation) and overheads (administration, management, facilities etc). This total cost was then divided by the total number of contacts street triage made over the entire 26-week period.
By contrast, the cost of police attendance at incidents was calculated using a microcosting approach (applying a cost per minute to the number of minutes per contact) because there is no discrete budget for police attendance at incidents involving people who may have mental health needs to allocate across the total number of incidents.
Not all data necessary to fully cost street triage and police attendance prior to street triage were available from the Sussex data set. Where necessary, data were taken from existing literature, or appropriate assumptions made, which are outlined in table 1. In particular, data on police attendance at incidents which did not result in the application of section 136 were not available for the ‘before’ period or for the times in the ‘after’ period when street triage was unavailable. Since data on street triage attendance that did not result in section 136 is available, this means we are not comparing like with like between the two periods. The following assumptions were made to fill these gaps:
In the ‘after’ period, street triage is available for approximately 30% of the week. However, the hours of availability were determined on the basis of peak need, and the clinical team advised that approximately 65% of all incidents happened during these peak hours, allowing the number of incidents occurring during the hours in which street triage was not available to be estimated;
In the ‘before’ period, we assumed that the total number of incidents attended, whether involving section 136 or not, was equal to the total number of incidents in the ‘after’ period, calculated as described above, allowing the number of incidents in which the police attended but did not detain the person to be estimated.
Table 1.
Sources of resource use data and assumptions made
| Resource components | Data source | Assumption if data unavailable |
|---|---|---|
| Before street triage implemented | ||
| Number of incidents attended by police ending in section 136 | Sussex data set | |
| Number of incidents attended by police ending in no further action | Assumption | Total number of incidents attended (calculated as described in text above) minus number of incidents attended ending in detention |
| Referral to other services for those people brought to custody | Clinical team advice | 1 GP contact (referred to GP as a minimum, so this is a conservative assumption) |
| After street triage implemented | ||
| Number of incidents attended by street triage team ending in section 136 detention | Sussex data set | |
| Number of incidents attended by street triage team ending in referral to alternative service | Sussex data set | |
| Number of incidents attended by street triage team ending in no further action | Sussex data set | |
| Number of incidents attended by police when street triage unavailable ending in section 136 detention | Sussex data set | |
| Number of incidents attended by police when street triage unavailable ending in no further action | Assumption | Calculated as described in text above |
| Duration of police attendance prior to street triage team arriving | Sussex data set | |
| Referral to other services by street triage team (GP, A&E, mental health team, other) | Sussex data set | |
| Number of contacts with service referred to (GP, A&E, mental health team, other) | Clinical team advice | 1 contact |
| Before and after street triage implemented | ||
| Length of stay in hospital | Clinical team advice | 1 day |
| Length of stay in custody | Heslin et al6 | 12 hours |
| Mental Health Act assessment (mandatory if brought to custody) | Heslin et al6 | 3 hours for two section 12 doctors plus an Approved Mental Health Professional |
| Duration of incidents attended by police ending in section 136 (for microcosting purposes) | Heslin et al6 | 511 min |
| Duration of incidents attended by police ending in no further action (for microcosting purposes) | Heslin et al6 | 276 min |
GP, general practitioner.
Data analysis
Method of economic evaluation
We conducted a cost-offset analysis, which assesses whether the cost of providing a new service, in this case street triage, is offset by the savings as a result of the implementation of the service. A full economic evaluation was not feasible due to the lack of data on the health and quality-of-life effects of police or street triage attendance on the individuals involved.
Sussex data
All data were analysed using STATA V.11.(StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP, 2009) For each arm, the total number and percentage were calculated for: incidents where a person is brought to any place of safety; incidents where a person is brought to an NHS-designated place of safety; incidents where a person is brought to a custody suite as a place of safety; and alternative responses of the street triage team (eg, referral to alternative services). The χ2 analyses were used to test for differences between arms.
Differences in the use of section 136 between the two arms were tested using the number of sections as a proportion of the relevant population. For Eastbourne, the area in which street triage was implemented, the denominator was 99 412, and for the rest of the County of Sussex, the denominator was 688 654 (total population 778 066 minus 99 412, based on 2011 census data).7
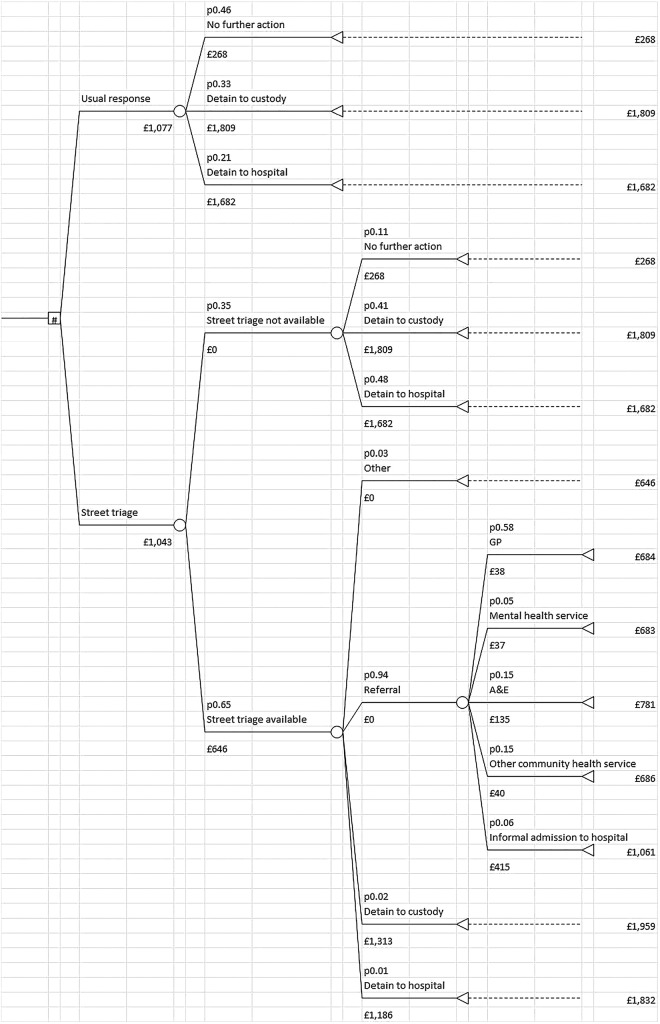
Decision model
A decision model was developed to compare the cost implications of providing street triage with the usual response. The decision model was populated with the Sussex data described above, information from previous research,6 and discussion with clinicians involved in providing street triage services. The model, presented in figure 1, contains the pathway through services in the usual response arm and the pathway through services in the presence of a street triage model, that includes one pathway for the times when street triage is available and a second for when street triage is unavailable.
Figure 1.
Decision analytic model of the cost of street triage compared to usual response.
Sensitivity analyses
A number of sensitivity analyses were undertaken to test the robustness of the model to the assumptions made and the generalisability of the model results:
The cost of a Mental Health Act assessment was assumed to involve 3 hours of two doctors and an Approved Mental Health Professional. Based on advice from the clinical team, this was varied to two doctors for 1 hour each and an Approved Mental Health Professional for 8 hours.
Length of stay in custody was assumed to be 12 hours, and was informed by published evidence.6 This was increased to 15 hours, following advice from the clinical team.
The time police spend at an incident ending in detention or in no further action when street triage was not available was informed by published evidence.6 Both values were reduced by 50% and increased by 150% in sensitivity analysis.
The clinical team advised that approximately 65% of all incidents happened during the periods in which street triage was available, allowing the number of incidents occurring during the hours in which street triage was not available to be estimated. The percentage was varied between 55% and 67% in sensitivity analysis.
Results
Changes in section 136 detentions
In the street triage period, there were 118 section 136 detentions, compared to 194 in the usual response period. This is a statistically significant difference of 39% in section 136 use (χ2 (1df) 18.542, p<0.001). Detentions in custody were significantly lower in the street triage period compared to the usual response period (56 vs 119 cases; χ2 22.700, p<0.001). The number of detentions in hospital was also lower in the street triage period, but not significantly so (62 vs 75; χ2 1.234, p>0.05).
In the rest of Sussex, the total number of section 136 applications increased by 10% (from 559 in the ‘before’ period to 614 in the ‘after’ period), although this increase was not statistically significant (χ2 2.581, p>0.05). The number of people being detained in custody increased by 6% (from 341 to 363; χ2 0.688, p>0.05), and the number detained in hospital increased by 15% (from 218 to 251; χ2 2.323, p>0.05).
The nature of the current evaluation means it is not possible to control for various factors which may be influencing the results, such as geographical boundaries. It is therefore possible that reductions seen in the street triage arm, and increases seen in the rest of Sussex, were a result of an increase in incidents in the street triage catchment area being picked up by police in the surrounding geographical areas. Because of the distances between catchment areas, this was thought to be unlikely. However, even assuming that 50% of the increase in the rest of the county were incidents in the street triage catchment, there is still a significantly lower number of detentions under section 136 in the street triage arm than the usual response arm (χ2 6.7881, p=0.009).
Street triage response to incidents
Data on actions taken by the street triage team in response to mental health-related incidents were available for a 4-month period during the study period (June–September 2014; breakdown available in online supplementary appendix 2). In almost 90% of incidents, the street triage team referred individuals to alternative services, primarily to a general practitioner (GP) (55%), accident and emergency (14%) or other community services (14%). Nine individuals were admitted to hospital on an informal basis (6%).
Only four individuals were subject to a section 136 detention by the street triage team, three taken to custody (2%) and one to hospital (<1%). Extrapolating this to the full 6-month period suggests that the street triage team were responsible for approximately 5% of the total detentions under section 136 in the ‘after’ period (6 of 118), with the remainder occurring when the street triage team was not available.
No data on actions taken was available for the period before street triage was introduced, so comparisons cannot be made. However, the clinical team advised that the Approved Mental Health Professional who sees people in custody always refers individuals to their GP as a minimum and sometimes refers to community mental health or drug and alcohol services.
Economic analysis
Resource use data included in the model
Table 2 summarises the resource elements per incident for inclusion in the economic model, including number of detentions, attendances and referrals to other services, for the ‘before’ and ‘after’ periods. The ‘after’ period includes resource elements when street triage was available and when it was unavailable. Data on referrals and calculation of total attendances used information available only in the last 4 months of the ‘after’ period, so where necessary, the results reported in table 2 have been adjusted to cover the full 6-month period.
Table 2.
Resource use elements
| Resource components | ‘Before’ | ‘After’ |
|
|---|---|---|---|
| Street triage | Police | ||
| Number | Number | Number | |
| Detentions | |||
| Total section 136—custody | 119 | 5* | 51† |
| Total section 136—hospital | 75 | 2* | 60† |
| Attendances | |||
| Total attendances | 358‡ | 233* | 125‡ |
| Referrals | |||
| Referrals to GP | 119¶ | 126* | 51¶ |
| Referrals to mental health service | 0 | 12* | 0 |
| Referrals to A&E | 0 | 36* | 0 |
| Referrals to other community service | 0 | 30* | 0 |
| Informal hospital admission | 0 | 14* | 0 |
| Other not associated with a referral cost | 0 | 9*§ | 0 |
*As data for 2 months of street triage was missing, data have been extrapolated to cover the full 6-month period (average number per month multiplied by six).
†Total detentions minus detentions implemented by street triage.
‡Calculated based on assumed probabilities described in table 3.
¶Based on expert advice that all people detained in custody are subsequently referred to the GP.
§Includes unknown, no further action, follow-up with family, arrest/breach of the peace.
GP, general practitioner.
Model probabilities
Probabilities entered into the model, including the source of these probabilities, are detailed in table 3. A number of assumptions were made where data were unavailable, and these are also outlined in the table.
Table 3.
Probabilities entered into the decision analytic model
| Event point | Probabilities | Source |
|---|---|---|
| Usual response (‘before’ arm) | ||
| Section 136 detention in custody | 0.33 | Data and assumption 1 |
| Section 136 detention in hospital | 0.21 | Data and assumption 1 |
| No further action | 0.46 | Assumption 1 |
| Street triage (‘after’ arm) | ||
| Proportion of time street triage available | 0.65 | Assumption 2 |
| Proportion of time street triage unavailable | 0.35 | Assumption 2 |
| Response when street triage available | ||
| Referral | 0.94 | Data |
| Section 136 detention in custody | 0.02 | Data |
| Section 136 detention in hospital | 0.01 | Data |
| No further action* | 0.03 | Data |
| Services street triage refer to:† | ||
| GP | 0.58 | Data |
| Mental health service | 0.05 | Data |
| A&E | 0.15 | Data |
| Other community service | 0.15 | Data |
| Informal referral to hospital | 0.06 | Data |
| Response during periods when street triage not available | ||
| Section 136 detention in custody | 0.41 | Data and assumption 1 |
| Section 136 detention in hospital | 0.48 | Data and assumption 1 |
| No further action | 0.11 | Assumption 3 |
| ||
Some sets of probabilities do not add up to 1 due to rounding.
*Includes follow-up with family.
†Excludes unknown and arrest.
GP, general practitioner.
Cost of street triage
The street triage team consisted of one police constable and one nurse providing the service for 52.5 h each week. Given the 26-week duration of the evaluation, the total cost of street triage was estimated to be £148 785 over the study period (£586+£518×52.5 h×26 weeks). The street triage team attended a total of 233 incidents over the ‘after’ period of the study, giving an estimated unit cost of £639 per incident attended.
Costs included in the model
All costs included in the model are listed in table 4, including the method of calculation and source of data. All costs are rounded to the nearest whole number.
Table 4.
Costs entered into the decision analytic model
| Resource component | Total cost, £ | Resource detail |
|---|---|---|
| Usual response (‘before’) and police response when street triage not available (‘after’) | ||
| Section 136 detention in custody | 1809 | £0.976×511 min6 (cost of officer attendance) plus £426×12 h6 (cost of time in custody) plus £7718 (cost of mental health act assessment) plus £388 (cost of referral to the GP) |
| Section 136 detention in hospital | 1682 | £0.976×511 min6 (cost of officer attendance) plus £4158 (cost of inpatient bed day) plus £7718 (cost of mental health act assessment) |
| No further action | 268 | £0.976×276 min6 (cost of officer attendance) |
| Street triage (‘after’) | ||
| Street triage per attendance, including police attendance while waiting for street triage team | 646 | £639 plus £0.976×8 min (cost of police officer first attendance) |
| Section 136 detention in custody | 1313 | £426×12 h6 (cost of time in custody) plus £7718 (cost of mental health act assessment) plus £388 (cost of referral to the GP) |
| Section 136 detention in hospital | 1186 | £4158 (cost of inpatient bed day) plus £7718 (cost of mental health act assessment) |
| Referral to GP | 38 | £388 (cost of one GP appointment) |
| Referral to mental health service | 37 | £378 (cost of one appointment with community mental health team) |
| Referral to A&E | 135 | £13512 (cost of one A&E attendance) |
| Referral to other community health service | 40 | £408 (cost of one social worker appointment) |
| Informal admission to hospital | 415 | £4158 (cost of one inpatient bed day) |
GP, general practitioner.
Figure 1 presents the decision analytic model complete with costs and probabilities. The figure shows that the average cost per person entering the usual response arm of the model is £1077. This compares with £1043 for the street triage arm, a difference of £34 less per person entering the model in the street triage arm. If we assume the same number of people enter each arm of the model over a 6-month period (n=358 based on assumptions described in table 2), this represents a cost saving of £12 172 in the street triage arm over the 6-month study period.
The results were also broken down into cost by payer. From a CJS perspective, the average cost per person entering the usual response arm of the model is £559. This compares with £470 for the street triage arm, a difference of £89 less per person entering the model in the street triage arm. If we assume the same number of people enter each arm of the model over a 6-month period (n=358 based on assumptions described in table 2), this represents a cost saving of £31 862 to criminal justice in the street triage arm over a 6-month period.
From an NHS perspective, the average cost per person entering the usual response arm of the model is £517. This compares with £574 for the street triage arm, a difference of £57 more per person entering the model in the street triage arm. If we assume the same number of people enter each arm of the model over a 6-month period (n=358 based on assumptions described in table 2), this represents an additional cost of £20 406 to the NHS in the street triage arm over a 6-month period.
Sensitivity analyses
The results of the sensitivity analyses, outlined above, are detailed in online supplementary appendix 3 and show that the estimated cost savings in favour of street triage in the main analysis (−£34) are sensitive to the assumptions made, with results ranging from −£116 in favour of street triage to +£48 in favour of usual response.
Varying the time taken by each professional involved in carrying out a mental health act assessment, as per advice from the clinic team, reduced the total cost per incident for both groups, but resulted in no cost difference between the groups (£991 street triage vs £991 usual response).
Adjusting the average duration of a custody stay from 12 to 15 h again on the advice of the clinical team, increased cost savings in favour of street triage to –£55 (£1063 street triage vs £1118 usual response). Similarly, increasing the time police are assumed to spend in attendance at incidents which resulted in detentions under section 136 or in no further action, increased cost savings in favour of street triage (to −£91 and −£89, respectively) compared to the main analysis. However, the opposite was seen when police time at incidents was reduced (cost difference +£25 and +£23, respectively).
Results were similar when the proportion of cases being seen by street triage was varied from 65% to 67%, with cost savings of −£36 in favour of street triage, and to 55%, generating cost savings of −£29 in favour of street triage.
Discussion
This study found that the number of detentions under section 136, and the number of detentions in custody were significantly reduced in the street triage (‘after’) period compared to the usual response (‘before’) period. Differences in detentions in the ‘before’ and ‘after’ periods are unlikely to be explained by unobserved factors or changes in the geographical area, given that the results for the rest of the county suggest detentions over time have, in fact, increased.
Of particular note is the finding that only 6% (7/118) of cases detained under section 136 in the street triage period took place at a time when street triage was available, with the majority of cases being detained by police officers out of street triage hours. Interestingly, the proportion of sections to no further actions went up when street triage was not available. Although we have no data on why this is, we hypothesise the following reasons: (1) as police get accustomed to relying on street triage and on the decision-making of mental health professionals, it is possible that during times when the service is not operational, without the support of the street triage team, police become more risk averse in making the decision to detain or not when they come into contact with individuals who they perceive are in need of care and control; (2) as street triage was implemented during evenings and weekends, it is possible that many of these contacts were alcohol related and required no further action. By contrast, during weekdays (when street triage was not available), less contacts may be related to alcohol use and, thus, be ‘real’ mental health crises that require the police to use sections.
The study also found that the additional investment in the street triage team (£148 784 over 6 months) was offset by savings resulting from reduced detentions, with the main analysis suggesting that street triage may be a cost-saving option. Although this result was sensitive to variation in the model assumptions, cost differences did not differ greatly between the two groups in any of the analyses, giving some confidence in the conclusion that the cost of the street triage team is entirely or largely offset.
Street triage is designed to refer people to the most appropriate service while avoiding detaining people, and one potential knock-on effect of referring people to appropriate services, is to reduce the likelihood of mental health crisis, and thus, subsequent presentations to police or mental health crisis services. The savings generated by the street triage team are, therefore, likely to be greater than the estimates presented here. In addition, improved access to appropriate services, combined with reductions in detentions under section 136, would be expected to have positive impacts on the mental health and quality of life of people who come to the attention of the police. Although the current study was not able to evaluate the impact of street triage on health outcomes, compared to usual response, the cost savings outlined combined with potential improvements in the health status of the individuals involved, suggests that street triage could potentially be a more cost-effective intervention than usual response, although there is no evidence to support this from this study, and further research to explore this is needed.
This study was limited in a number of important ways. First, as this was a pragmatic evaluation, relying on retrospective data rather than an experimental study, such as a randomised controlled trial, it is not possible to fully attribute the reduction in detentions to the street triage team, as other unobserved factors may be influencing the outcomes. However, street triage does not easily lend itself to study under randomised controlled conditions, and the results of the wider geographical area provide some support for the value of the results reported. Furthermore, to the best of our knowledge, no other major area-level changes occurred over the period of the study, in either the local police service or local mental health services. We therefore conclude that observed changes are likely to be due to the implementation of street triage. Further, retrospective routine data is susceptible to reporting errors and missing data which is something that could not be controlled for or examined in these analyses.
Second, the lack of data on outcomes for people who have contact with the police and the street triage service is an important omission. A qualitative study is currently being conducted on the experiences of people who come into contact with the police in the context of a mental health crisis, both in relation to street triage services and usual police response, but these data are not yet available, and are not easily amenable to economic evaluation. Future evaluations should consider the collection of data on mental health and quality-of-life outcomes, including preference-based measures capable of generating quality-adjusted life years (QALYs),9 such as the EQ-5D (EuroQol 5 dimensions).10 QALYs are preferred by the National Institute of Health and Care Excellence for the development of guidelines,11 and would enable full assessment of the cost-effectiveness and cost utility of street triage.
Third, a number of assumptions were required due to the lack of certain pieces of information. This is especially problematic around the assumption that the same number of cases would have entered the model in the street triage and usual response arm. As aforementioned, it is likely that an effect of referring people on to other services, rather than detaining them, is that they would be getting more appropriate care faster. Therefore, it is possible that there would be a reduction in the number of people entering the model over time in the street triage arm. However, this needs to be balanced against the possibility of an increase of referrals to street triage over time as the service becomes better known. We have been unable to account for this in the decision model as we had no appropriate sources of information on what the impact on recontact might be. However, where possible, we have varied other assumptions, according to expert opinion from the clinical team, in order to explore the impact of the assumptions included in the analysis. This also relates to the limitation of a lack of data on the number/proportion of incidents under police response that do not result in a detention under section 136. This could drastically influence the results of the cost analyses, and further research on this is essential in order to inform future economic analyses. Finally, we have not been able to include information on people who were moved from one place of safety to another. However, these are likely to have been minimal.
Acknowledgments
The authors would like to thank key members of the Sussex Partnership NHS Foundation Trust, and the Sussex Police, who spent much time providing and aiding interpretation of data: Christina Henman, Sarah Gates, Diane Roskilly and Marian Trendall.
Footnotes
Twitter: Follow Sarah Byford at @sarahbyford1
Contributors: MH was responsible for the design, analysis and interpretation of the study, drafted the initial manuscript and approved the final manuscript. LC, MP and VB were involved in design and interpretation of the study, revised the manuscript and approved the final manuscript. SB was senior researcher involved in design and interpretation of the study, revised the manuscript and approved the final manuscript.
Funding: This work was supported by East Sussex Joint Commissioning Unit.
Competing interests: None declared.
Disclaimer: Lynne Callaghan was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South West Peninsula. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Royal College of Psychiatrists. Mental health and the economic downturn: National priorities and NHS solutions. London: Royal College of Psychiatrists, 2009. [Google Scholar]
- 2.Adebowale V. Independent Commission on Mental Health and Policing Report London: Independent Commission on Mental Health and Policing, 2013. [Google Scholar]
- 3.Bradley K. The Bradley Report: Lord Bradley's Review of People with Mental Health Problems or Learning Disabilities in the Criminal Justice System London: Department of Health, 2009. [Google Scholar]
- 4.Rutherford M. Blurring the Boundaries: the convergence of mental and criminal justice policy: legislation systems and practice. London: Sainsbury Centre for Mental Health, 2010. [Google Scholar]
- 5.Department of Health. Extending the street triage scheme: new patrols with nurses and the police. 2013. [13/09/2013]. https://www.gov.uk/government/news/extending-the-street-triage-scheme-new-patrolswith-nurses-and-the-police [Google Scholar]
- 6.Heslin M, Callaghan L, Barrett B et al. . Costs of the police service and mental health care pathways experienced by individuals with enduring mental health needs. Br J Psychiatry In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Office of National Statistics. Neighbourhood statistics: Population Density 2013. http://neighbourhood.statistics.gov.uk/dissemination/viewFullDataset.do?instanceSelection=033488&productId=2491&$ph=60_61_62&datasetInstanceId=33488&startColumn=1&numberOfColumns=8&containerAreaId=6275000 (accessed 12 Feb 2015).
- 8.Curtis L. Unit Costs of Health and Social Care 2014. Personal Social Services Research Unit: University of Kent, 2014. [Google Scholar]
- 9.Malek M.2001. Implementing QALYs. http://www.medicine.ox.ac.uk/bandolier/painres/download/whatis/ImplementQALYs.pdf.
- 10.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 1990;16: 199–208. doi:10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 11.National Institute of Health and Care Excellence. The guidelines manual 2012. https://www.nice.org.uk/article/pmg6/chapter/7-assessing-cost-effectiveness
- 12.Department of Health. NHS reference costs 2013/14. https://www.gov.uk/government/publications/nhs-reference-costs-2013-to-2014 (accessed 11 Feb 2015).