Abstract
Objective
We identify drinking styles that place teens at greatest risk of later alcohol use disorders (AUD).
Design
Population-based cohort study.
Setting
Victoria, Australia.
Participants
A representative sample of 1943 adolescents living in Victoria in 1992.
Outcome measures
Teen drinking was assessed at 6 monthly intervals (5 waves) between mean ages 14.9 and 17.4 years and summarised across waves as none, one, or two or more waves of: (1) frequent drinking (3+ days in the past week), (2) loss of control over drinking (difficulty stopping, amnesia), (3) binge drinking (5+ standard drinks in a day) and (4) heavy binge drinking (20+ and 11+ standard drinks in a day for males and females, respectively). Young Adult Alcohol Use Disorder (AUD) was assessed at 3 yearly intervals (3 waves) across the 20s (mean ages 20.7 through 29.1 years).
Results
We show that patterns of teen drinking characterised by loss of control increase risk for AUD across young adulthood: loss of control over drinking (one wave OR 1.4, 95% CI 1.1 to 1.8; two or more waves OR 1.9, CI 1.4 to 2.7); binge drinking (one wave OR 1.7, CI 1.3 to 2.3; two or more waves OR 2.0, CI 1.5 to 2.6), and heavy binge drinking (one wave OR 2.0, CI 1.4 to 2.8; two or more waves OR 2.3, CI 1.6 to 3.4). This is not so for frequent drinking, which was unrelated to later AUD. Although drinking was more common in males, there was no evidence of sex differences in risk relationships.
Conclusions
Our results extend previous work by showing that patterns of drinking that represent loss of control over alcohol consumption (however expressed) are important targets for intervention. In addition to current policies that may reduce overall consumption, emphasising prevention of more extreme teenage bouts of alcohol consumption appears warranted.
Keywords: young adulthood, adolescence, drinking, binge drinking, alcohol use disorder
Strengths and limitations of this study.
The Victorian Adolescent Health Cohort Study is a 20-year Australian longitudinal study of adolescent development.
The study has maintained a high retention.
It provides unique prospective data on a broad range of adolescent health risk behaviours.
It has followed participants into adulthood, including detailed assessment of alcohol and drug use.
Non-response is often associated with more extreme behaviours, such as alcohol and drug use, and can introduce bias in estimates of association. We correct for this by imputing missing data using the methods of multiple imputation.
The 1-week reference period for reporting alcohol use will not necessarily capture the full extent of drinking in this age group. This means that estimates provided are likely to be conservative in some cases.
Analyses are based on self-report; however, there is reasonable evidence to show that self-reports are reliable and valid when made in a confidential setting. Participants were assured of confidentiality without consequence for disclosure.
Alcohol dependence and abuse continue to be major contributors to the total burden of disease, with consequences extending beyond health to social and economic outcomes.1–3 Alcohol use commonly begins in adolescence with drinkers being at higher risk of later alcohol use disorders (AUDs) than their non-drinking adolescent peers.4 Recent decades have seen the rise of adolescent drinking in many countries, with secular trends towards earlier ages of alcohol initiation.4 5 This has focused interest in public health and clinical interventions in adolescents as a means of reducing risk of AUDs.
There is now considerable evidence showing continuity of teen drinking into young adulthood and later adult life, including progression to alcohol dependence in adulthood.6 However, most research has focused on a particular drinking style (eg, binge drinking), which precludes comparison of the diversity of ways in which young people use alcohol.7–12 AUDs have likewise been measured infrequently and prior to peak age of onset in the mid-20s,7 8 which raises questions about whether AUD in this period has been well enough characterised. Greater clarity around which patterns of teen alcohol use are most prognostic of later AUD diagnoses has considerable potential to enhance targeting of preventive intervention; however, cohort studies that cross the transition from adolescence to young adulthood remain scant.
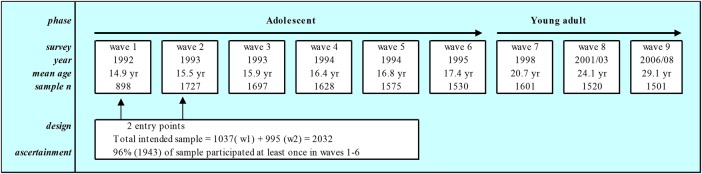
One study with rich developmental data on alcohol use in a cohort of around 2000 young Australians followed across 9 waves from adolescence to young adulthood is the Victorian Adolescent Health Cohort Study (VAHCS). Detailed assessments of alcohol use were taken at 6 monthly intervals across the teens (6 waves) and at 3 yearly intervals across the 20s (3 waves). Adolescent data provide a unique opportunity to define a range of common teen drinking styles (eg, frequent drinking, binge drinking, heavy binge drinking and loss of control over drinking). Clinical assessments of AUD in young adulthood provide an opportunity to examine risk relationships before, during and after their peak age of onset across the 20s.
Findings already published from VAHCS have identified frequent teen drinking and antisocial behaviour as key predictors of AUDs at 21 years of age.10 In this study, we extend our investigations to include other teen drinking styles, and across three young adult waves covering the 20s. Specifically, we examined the extent to which four common teen drinking styles—frequent drinking, binge drinking, heavy binge drinking and loss of control over drinking—predict AUD diagnoses in young adulthood; and whether risks differ by gender and age of AUD diagnosis in young adulthood.
Methods
Sample recruitment and procedure
Data were drawn from a nine wave population-based longitudinal study of 2032 adolescents followed from puberty to adulthood (VAHCS). Data collection protocols were approved by the Human Research Ethics Committee of the Royal Children's Hospital. The VAHCS sample was selected with a two-stage cluster sampling procedure. At the first stage, 44 Government, independent and Catholic schools were chosen to represent each school stratum in the state of Victoria. At the second stage, a single intact year 9 class (aged 14–15 years) was randomly selected from each school to constitute the wave 1 sample (n=1037). School retention rates to year 9 in 1992 were 98%, ensuring a close-to-representative sampling frame. Six months later, when the study population moved into year 10 (aged 15–16 years), a second intact class from each participating school was selected at random, giving a total intended sample of 2032 (wave 2).
Participants were then interviewed at 6-month intervals during their teenage years (waves 3–6), and were followed up at three time points in young adulthood: age 20.7 (wave 7), 24.1 (wave 8) and 29.1 years (wave 9) (see figure 1). From a total sample of 2032 students, 1943 (95.6%) participated at least once during the first six (adolescent) waves; of these, 1760 (53% female) participated in at least one adult wave. By the end of wave 9, 15 participants were known to have died, 108 were lost to follow-up and 319 refused participation. In this paper, we have only used adolescent data from waves 2 to 6, as by design around half of the adolescents did not participate in wave 1.
Figure 1.
Sampling and ascertainment in the Victorian Adolescent Health Cohort (est 1992).
Measures
Adult AUD (waves 7, 8 and 9)
AUDs were defined by meeting criteria for alcohol abuse or dependence.13–15 This was based on a comprehensive review showing that (1) the two criterion sets do not differ in prevalence, severity or age of onset and (2) the 11 AUD criteria can be best modelled as a single dimension rather than as two dimensions.16 Abuse and dependence were classified using the Composite International Diagnostic Interview (CIDI).17 The CIDI is a structured diagnostic interview designed for use by non-clinical professionals, based on Diagnostic and Statistical Manual of Mental Disorders (DSM) IV (1994) criteria. The CIDI is the most widely used interview in large epidemiological studies and CIDI assessments have been shown to have adequate inter-rate reliability and test–retest reliability.18 19 The CIDI was only administered to participants who reported consuming more than 11 standard drinks in the past 12 months.
Alcohol abuse was defined by meeting at least one of the following criteria: recurrent alcohol use resulting in failure to fulfil major obligations at work, school or home; recurrent alcohol use in situations where it is physically hazardous; recurrent alcohol-related legal problems; and continued use despite persistent or recurrent social or interpersonal problems caused or worsened by the effects of alcohol. Alcohol dependence was defined by meeting at least three of the following criteria: tolerance as indicated by a need to increase amounts of alcohol in order to become intoxicated; withdrawal as indicated by physiological withdrawal symptoms; use of more alcohol or for a longer time than originally intended; a persistent desire or unsuccessful effort to cut down or control use; a great deal of time obtaining alcohol, using alcohol, or recovering from its effects; the reduction or dismissal of important social, occupational or recreational activities due to alcohol use; and continued use despite knowledge of having persistent or recurrent physical or psychological problems that are likely to have been caused or worsened by alcohol.
Teenage drinking patterns (waves 2–6)
At each wave, participants who reported drinking alcohol in the previous week were asked to fill in a diary that recorded all types of alcohol (eg, beer, cider, spirits, mixed drinks, wine, etc), brand names and amounts (eg, glass, can, etc) consumed on each day/occasion in the 7 days prior to the survey. The responses enabled calculations of the number of standard drink units (10 g alcohol) of alcohol consumed each day.
Four patterns of adolescent drinking were defined:
Frequent drinking was defined at each wave as drinking on 3 or more days during the recorded diary week. Persistence of frequent drinking across adolescent waves was classified as none, one wave, or two or more waves.
Loss of control over drinking was defined by two separate items asking respondents whether they had ever (1) found themselves unable to stop drinking; (2) consumed so much alcohol that they could not remember what had happened the night before. Response categories were no–never, yes–once and yes–more than once. At each wave, adolescents were considered to have trouble controlling their alcohol intake if they reported either behaviour more than once, or both behaviours at least once. Across adolescent waves, we identified those who reported these difficulties at no waves, at one wave and at two or more waves.
Binge drinking was defined as having consumed five or more standard drinks on at least 1 day during the recorded diary week. Drinking was defined as having had less than five standard drinks on any 1 day. We identified the maximum level of drinking during adolescence and classified the persistence of that drinking behaviour into five categories: none (no drinking in adolescence); drinking less than five standard drinks at one wave (reference category); drinking less than five standard drinks at two or more waves; drinking more than five standard drinks at one wave and at two or more waves.
Heavy binge drinking was defined as having consumed >20 standard drinks for males and >11 standard drinks for females on at least 1 day over the diary week.20 Drinking was classified as male and females drinking alcohol below these gender-defined levels on any day in the diary week. After identifying the maximum level of drinking in adolescence, we created five categories of drinking behaviour: none (no drinking in adolescence); drinking at one wave (reference category) and at two or more waves; heavy binge drinking at one wave and at two or more waves.
For measures of binge and heavy binge drinking, the reference group was defined by one wave of drinking below the number of units used to classify binge drinking, as non-drinking is not a normative behaviour for Australian adolescents.
Potential confounding factors
The unique contribution of teen drinking to later AUDs, over and above other psychosocial determinants, has not been clearly established.7 Individual level factors such as teen mental disorders, personality traits (such as antisocial behaviour) and other substance use may play a significant role. Likewise, social factors including parental substance use, as well as the larger socioeconomic context of the adolescent, may raise risk for AUDs in young adulthood. Potential confounding factors selected for this analysis are listed below.
Adolescent antisocial behaviour
Antisocial behaviour was assessed at each wave using 10 items from the Self-Report Early Delinquency Scale.21 Items included property damage (vandalism, car damage, making graffiti), interpersonal conflict (fighting, carrying weapons, running away from home, expulsion from school) and theft (stealing property from parents or others, stealing cars). Questions concerning alcohol or other substance use were not included. Participants were asked if they had engaged in any of these behaviours: never, once or more than once in the past 6 months. Antisocial behaviour at each wave was defined as engaging in two or more antisocial behaviours at least once or one antisocial behaviour more than once. Adolescent antisocial behaviours were then defined on three levels: no antisocial behaviour; antisocial behaviour at one wave; and antisocial behaviour on two or more waves.
Adolescent depressive symptoms
At each adolescent wave, symptoms of depression and anxiety were assessed using the computerised Clinical Interview Schedule-Revised (CIS-R).22 The CIS-R is a structured questionnaire employing ICD-10 criteria,23 designed for assessing symptoms of depression and anxiety in non-clinical populations. This scale generates scores (0–4) on 14 subscales of common psychiatric symptoms associated with depression and anxiety. Total scores were dichotomised at a threshold (score ≥12) to identify symptoms of depression/anxiety where clinical intervention would be appropriate.24 25 During adolescence, we identified those with none, one, and two or more waves of depressive symptoms.
Adolescent tobacco use
At each wave, cigarette smoking was assessed with a self-report diary over the previous 7 days and daily smokers were identified as those smoking 6 or 7 days in the previous week. Adolescents who reported smoking daily at any one wave were classified as daily smokers during adolescence.
Adolescent cannabis use
At each wave, participants reported their cannabis use during the past 6 months. Individuals reporting weekly or daily cannabis use were classified as weekly+ cannabis users. During adolescence, we identified those with none, one, and two or more waves of weekly+ cannabis use.
Adolescent parental background factors
Parental divorce or separation in adolescence (by wave 6) was identified either prospectively or retrospectively if the adolescent was absent at wave 6. Highest level of parental education in adolescence: secondary school not completed; secondary school completed or vocational qualification; university degree. Participants were asked whether their parents drank on: none, most days or every day. They were also asked whether their parents smoked cigarettes: never, occasionally, most days or every day. Variables derived for parental alcohol and tobacco use identified whether either parent drank alcohol or smoked most days or every day during their own adolescence.
Auxiliary variables
A selection of variables was included in the imputation model (see Data analysis section) as auxiliary variables, as these were thought to be related to the missingness of the data. From the adolescent waves we included age at wave 2. From the adult waves, we included frequency of drinking, level of drinking, smoking status and cannabis use, and for wave 7 only we included CIS-R. These adult variables had the same definition as the adolescent variables.
Data analysis
We estimated the prevalence of each type of adolescent drinking behaviour, adolescent and parental background factors, and adult AUDs at each wave by sex. We also estimated the prevalence of adult AUDs at each wave stratified by sex and level of adolescent drinking. Logistic generalised estimating equations (GEEs) were used to investigate the associations between the adolescent drinking variables and the repeated binary measures of AUDs in adulthood. The effect of each adolescent drinking measure was estimated in a separate model. We first estimated the effects of adolescent drinking measure after adjusting for wave and gender. We then further adjusted for all potential confounding factors. All interactions between adolescent drinking behaviour, wave and gender were entered into the model and tested for significance. There was no evidence of interactions between any of these variables and they were not retained in the final models. All effects were tested for statistical significance using the Wald test.
Missing data were assumed to be missing at random and handled using multiple imputation.26 We imputed 20 complete data sets separately for males and females, under a multivariate normal model, incorporating all the analysis and auxiliary variables. Wave 1 was omitted, as it contained observations from only 46% of the cohort. Wave 1 responses were used to fill in wave 2 data for 57 participants who were seen only at wave 1, as the same measures had been collected at the earlier wave. Waves 2–9 were imputed for all participants (N=1943) who completed the survey at least once in adolescence (waves 2–6). The imputation model contained 42 key variables used in the analysis and 14 auxiliary variables. Of 56 variables included in the imputation model, 16% of the variables had <10% missing values, 48% had ≥10% to <20% missing and 36% had ≥20% to <30% missing. A maximum level of drinking variable (coded 0/1/2/3) was created at each wave, with four levels: no drinking, no binge drinking, binge drinking and heavy binge drinking. These variables were log transformed before imputation. After imputation, transformed variables were converted back to their original scale and all were categorised for analysis, with adaptive rounding used for binary measures.27 Fifteen deceased participants were excluded from the imputed data sets. Frequencies and ORs were obtained by averaging results across the imputed data sets; inferences under multiple imputation were made using Rubin's rules.26 Monte Carlo error estimates were obtained for all estimates presented and confirmed that 20 imputed data sets were sufficient. All data analysis was undertaken using Stata (StatCorp. Stata (release 13 2013). College Station, Texas: Stata Corporation; 2013).
Results
The majority of adolescents were not drinking on 3 or more days a week in adolescence; 90% of females and 78% of males (table 1). Around 1 in 10 adolescents reported loss of control over drinking at two or more waves. Only 32% of males and 41% of females reported no alcohol use in adolescence. Around twice as many males (28%) reported binge drinking at two or more waves compared to females (14%). Rates of heavy binge drinking at one wave were similar for males and females, around 1 in 10. Eight per cent of males and 5% of females reported heavy binge drinking persistently in adolescence. The adolescent and parental background factors were similar for males and females, with the exception of antisocial behaviour: which had higher rates for males; and depressive symptoms: which had higher rates for females. Higher rates of AUDs (DSM-IV dependence or abuse) were seen for males than for females.
Table 1.
Summary of adolescent drinking behaviours and background factors, and young adult alcohol use disorders, by gender
| Measure | Male (n=931) |
Female (n=997) |
||||
|---|---|---|---|---|---|---|
| n | Per cent | (95% CI) | n | Per cent | (95% CI) | |
| Adolescent drinking patterns | ||||||
| Frequent drinking | ||||||
| None | 729 | 78 | (75 to 81) | 897 | 90 | (88 to 92) |
| 1 wave | 140 | 15 | (12 to 18) | 69 | 7 | (5 to 9) |
| 2+ waves | 62 | 7 | (5 to 8) | 31 | 3 | (2 to 4) |
| Loss of control over drinking | ||||||
| None | 704 | 76 | (73 to 79) | 787 | 79 | (76 to 82) |
| 1 wave | 135 | 15 | (12 to 17) | 122 | 12 | (10 to 14) |
| 2+ waves | 92 | 10 | (8 to 12) | 89 | 9 | (7 to 11) |
| Binge drinking | ||||||
| None | 299 | 32 | (29 to 35) | 409 | 41 | (38 to 44) |
| 1 wave drinking | 112 | 12 | (10 to 15) | 166 | 17 | (14 to 19) |
| 2+ waves drinking | 82 | 9 | (7 to 11) | 109 | 11 | (9 to 13) |
| 1 wave binge drinking | 172 | 19 | (16 to 21) | 176 | 18 | (15 to 20) |
| 2+ waves binge drinking | 265 | 28 | (25 to 32) | 137 | 14 | (11 to 16) |
| Heavy binge drinking | ||||||
| None | 299 | 32 | (29 to 35) | 409 | 41 | (38 to 44) |
| 1 wave drinking | 164 | 18 | (15 to 20) | 203 | 20 | (18 to 23) |
| 2+ waves drinking | 280 | 30 | (27 to 33) | 229 | 23 | (20 to 26) |
| 1 wave heavy binge drinking | 111 | 12 | (10 to 14) | 107 | 11 | (9 to 13) |
| 2+ waves heavy binge drinking | 76 | 8 | (6 to 10) | 48 | 5 | (3 to 6) |
| Adolescent background factors | ||||||
| Daily smoking | 236 | 25 | (22 to 28) | 255 | 26 | (23 to 28) |
| Weekly+ cannabis use | ||||||
| None | 756 | 81 | (78 to 84) | 901 | 90 | (88 to 92) |
| 1 wave | 82 | 9 | (6 to 11) | 36 | 4 | (2 to 5) |
| 2+ waves | 93 | 10 | (8 to 12) | 60 | 6 | (5 to 8) |
| Depressive symptoms | ||||||
| None | 661 | 71 | (68 to 74) | 450 | 45 | (42 to 48) |
| 1 wave | 133 | 14 | (12 to 17) | 176 | 18 | (15 to 20) |
| 2+ waves | 138 | 15 | (12 to 17) | 371 | 37 | (34 to 40) |
| Antisocial behaviour | ||||||
| None | 364 | 39 | (36 to 43) | 626 | 63 | (60 to 66) |
| 1 wave | 192 | 21 | (17 to 24) | 151 | 15 | (13 to 18) |
| 2+ waves | 375 | 40 | (37 to 44) | 219 | 22 | (19 to 25) |
| Parental background factors | ||||||
| Daily drinking | 287 | 31 | (28 to 34) | 322 | 32 | (29 to 35) |
| Daily smoking | 361 | 39 | (35 to 42) | 395 | 40 | (37 to 43) |
| Divorce/separation | 214 | 23 | (20 to 26) | 221 | 22 | (20 to 25) |
| Highest level of education | ||||||
| High school not completed | 268 | 29 | (26 to 32) | 375 | 38 | (34 to 41) |
| High school completed | 342 | 37 | (33 to 40) | 326 | 33 | (30 to 36) |
| University degree | 321 | 34 | (31 to 38) | 297 | 30 | (27 to 33) |
| Young adult alcohol use disorder | ||||||
| Wave 7 (mean age 20.7 years) | 216 | 23 | (20 to 26) | 133 | 13 | (11 to 16) |
| Wave 8 (mean age 24.1 years) | 258 | 28 | (25 to 31) | 125 | 13 | (10 to 15) |
| Wave 9 (mean age 29.1 years) | 180 | 19 | (16 to 22) | 82 | 8 | (6 to 10) |
Table 2 estimates the frequency of young adult AUDs stratified by adolescent drinking behaviour, gender and wave. For males, highest rates of AUDs were seen at waves 7 and 8 in those reporting more than one wave of frequent drinking, binge drinking, heavy binge drinking and loss of control over drinking. For females, highest rates of AUDs were seen at wave 7 for those reporting more than one wave of frequent drinking and loss of control over drinking.
Table 2.
Summary of adolescent drinking behaviours by young adult alcohol use disorders, gender and wave
| Adolescent measure | Young adult alcohol use disorder |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Males |
Total | Females |
|||||||||||
| Wave 7 |
Wave 8 |
Wave 9 |
Wave 7 |
Wave 8 |
Wave 9 |
|||||||||
| Per cent | (95% CI) | Per cent | (95% CI) | Per cent | (95% CI) | Per cent | (95% CI) | Per cent | (95% CI) | Per cent | (95% CI) | |||
| Adolescent drinking patterns | ||||||||||||||
| Frequent drinking | ||||||||||||||
| None | 729 | 20 | (16 to 23) | 24 | (21 to 27) | 19 | (16 to 22) | 897 | 12 | (10 to 14) | 12 | (10 to 14) | 7 | (6 to 9) |
| 1 wave | 140 | 33 | (24 to 42) | 38 | (29 to 47) | 20 | (12 to 28) | 69 | 19 | (8 to 30) | 21 | (10 to 32) | 12 | (2 to 22) |
| 2+ waves | 62 | 45 | (31 to 59) | 47 | (33 to 61) | 20 | (7 to 33) | 31 | 44 | (25 to 63) | 15 | (1 to 29) | 23 | (6 to 40) |
| Loss of control over drinking | ||||||||||||||
| None | 704 | 19 | (16 to 23) | 23 | (20 to 26) | 16 | (13 to 19) | 787 | 11 | (9 to 13) | 11 | (8 to 13) | 6 | (4 to 8) |
| 1 wave | 135 | 29 | (19 to 39) | 38 | (28 to 47) | 27 | (18 to 37) | 122 | 16 | (8 to 23) | 16 | (9 to 24) | 13 | (6 to 20) |
| 2+ waves | 92 | 44 | (32 to 57) | 48 | (36 to 60) | 35 | (22 to 47) | 89 | 30 | (20 to 41) | 24 | (13 to 35) | 20 | (10 to 29) |
| Binge drinking | ||||||||||||||
| None | 299 | 13 | (9 to 18) | 15 | (11 to 20) | 16 | (11 to 20) | 409 | 6 | (4 to 8) | 9 | (6 to 12) | 6 | (3 to 8) |
| 1 wave drinking | 112 | 18 | (9 to 27) | 23 | (14 to 32) | 15 | (7 to 23) | 166 | 12 | (7 to 18) | 12 | (6 to 18) | 8 | (3 to 13) |
| 2+ waves drinking | 82 | 17 | (6 to 28) | 27 | (16 to 39) | 14 | (5 to 23) | 109 | 22 | (13 to 31) | 16 | (8 to 23) | 8 | (2 to 14) |
| 1 wave binge drinking | 172 | 23 | (16 to 31) | 29 | (21 to 36) | 22 | (15 to 30) | 176 | 19 | (12 to 26) | 17 | (11 to 24) | 12 | (7 to 18) |
| 2+ waves binge drinking | 265 | 39 | (32 to 45) | 43 | (36 to 50) | 25 | (18 to 32) | 137 | 23 | (15 to 31) | 15 | (8 to 22) | 11 | (5 to 17) |
| Heavy binge drinking | ||||||||||||||
| None | 299 | 13 | (9 to 18) | 15 | (11 to 20) | 16 | (11 to 20) | 409 | 6 | (4 to 8) | 9 | (6 to 12) | 6 | (3 to 8) |
| 1 wave drinking | 164 | 17 | (10 to 25) | 23 | (15 to 30) | 16 | (9 to 22) | 203 | 13 | (8 to 18) | 13 | (7 to 18) | 8 | (3 to 13) |
| 2+ waves drinking | 280 | 24 | (18 to 30) | 31 | (25 to 37) | 20 | (15 to 26) | 229 | 24 | (18 to 30) | 17 | (12 to 22) | 9 | (5 to 13) |
| 1 wave binge drinking | 111 | 39 | (28 to 50) | 42 | (30 to 54) | 25 | (14 to 35) | 107 | 16 | (8 to 25) | 18 | (9 to 26) | 13 | (6 to 20) |
| 2+ waves binge drinking | 76 | 50 | (37 to 63) | 53 | (41 to 66) | 30 | (18 to 43) | 48 | 23 | (11 to 36) | 10 | (0 to 20) | 18 | (6 to 30) |
Table 3 presents estimates of association between young adult AUD and adolescent measures of frequent drinking and loss of control over drinking. After adjustment for sex, wave and adolescent and parental background factors, there is no statistical evidence of an association between frequent drinking and AUDs. After adjustment, those who reported loss of control over drinking at one wave (OR 1.4, 95% CI 1.1 to 1.8) and two or more waves (OR 1.9, 95% CI 1.4 to 2.7) had increased odds of AUD compared to those who did not report loss of control over drinking at any wave.
Table 3.
Predictors of young adult alcohol use disorder: adolescent frequency of drinking and loss of control over drinking
| Measures | Unadjusted model |
Adjusted model* |
||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | p Value | OR | (95% CI) | p Value | |
| Frequent drinking in adolescence | ||||||
| Drinking pattern | <0.001† | 0.13† | ||||
| None | 1 | 1 | ||||
| 1 wave | 1.7 | (1.3 to 2.2) | 1.2 | (0.89 to 1.6) | ||
| 2+ waves | 2.6 | (1.8 to 3.6) | 1.4 | (0.98 to 2.0) | ||
| Wave | <0.001† | <0.001† | ||||
| Wave 7 (mean age 20.7 years) | 1 | 1 | ||||
| Wave 8 (mean age 24.1 years) | 1.1 | (0.96 to 1.3) | 1.1 | (0.96 to 1.3) | ||
| Wave 9 (mean age 29.1 years) | 0.70 | (0.57 to 0.85) | 0.69 | (0.56 to 0.85) | ||
| Gender | ||||||
| Female | 1 | 1 | ||||
| Male | 2.2 | (1.8 to 2.6) | <0.001 | 2.2 | (1.8 to 2.6) | <0.001 |
| Loss of control over drinking in adolescence | ||||||
| Drinking pattern | <0.001† | <0.001† | ||||
| None | 1 | 1 | ||||
| 1 wave | 1.8 | (1.4 to 2.4) | 1.4 | (1.1 to 1.8) | ||
| 2+ waves | 3.1 | (2.4 to 4.2) | 1.9 | (1.4 to 2.7) | ||
| Wave | <0.001† | <0.001† | ||||
| Wave 7 (mean age 20.7 years) | 1 | 1 | ||||
| Wave 8 (mean age 24.1 years) | 1.1 | (0.96 to 1.3) | 1.1 | (0.96 to 1.3) | ||
| Wave 9 (mean age 29.1 years) | 0.70 | (0.57 to 0.85) | 0.69 | (0.56 to 0.85) | ||
| Gender | ||||||
| Female | 1 | 1 | ||||
| Male | 2.4 | (2.0 to 2.8) | <0.001 | 2.2 | (1.8 to 2.7) | <0.001 |
*Adjusted for adolescent daily smoking, weekly+ cannabis use, depressive symptoms and antisocial behaviour, and parental daily drinking, daily smoking, divorce/separation and level of education.
†p Value from joint test of significance.
Table 4 presents estimates of association between young adult AUDs and adolescent binge drinking and heavy binge drinking. After adjustment, there was an increase in the odds of AUD in those reporting drinking below binge levels on two or more occasions (OR 1.5, 95% CI 1.1 to 2.1), binge drinking on one occasion (OR 1.7, 95% CI 1.3 to 2.3) and binge drinking on two or more occasions (OR 2.0, 95% CI 1.5 to 2.6) compared to those who reported drinking below binge levels at only one wave. Similar associations were observed between heavy binge drinking and AUD after adjustment.
Table 4.
Predictors of young adult alcohol use disorder: adolescent binge and heavy binge drinking
| Measure | Unadjusted model |
Adjusted model* |
||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | p Value | OR | (95% CI) | p Value | |
| Binge drinking in adolescence | ||||||
| Drinking pattern | <0.001† | <0.001† | ||||
| None | 1.5 | (1.0 to 2.1) | 1.3 | (0.93 to 1.9) | ||
| 1 wave drinking | 1 | 1 | ||||
| 2+ waves drinking | 1.8 | (1.3 to 2.6) | 1.5 | (1.1 to 2.1) | ||
| 1 wave binge drinking | 2.2 | (1.6 to 3.0) | 1.7 | (1.3 to 2.3) | ||
| 2+ waves binge drinking | 3.2 | (2.5 to 4.0) | 2.0 | (1.5 to 2.6) | ||
| Wave | <0.001† | <0.001† | ||||
| Wave 7 (mean age 20.7 years) | 1 | 1 | ||||
| Wave 8 (mean age 24.1 years) | 1.1 | (0.96 to 1.3) | 1.1 | (0.96 to 1.3) | ||
| Wave 9 (mean age 29.1 years) | 0.70 | (0.57 to 0.85) | 0.69 | (0.56 to 0.85) | ||
| Gender | ||||||
| Female | 1 | 1 | ||||
| Male | 2.1 | (1.7 to 2.5) | <0.001 | 2.1 | (1.7 to 2.6) | <0.001 |
| Heavy binge drinking in adolescence | ||||||
| Drinking pattern | <0.001† | <0.001† | ||||
| None | 1.5 | (1.1 to 2.0) | 1.3 | (0.96 to 1.8) | ||
| 1 wave drinking | 1 | 1 | ||||
| 2+ waves drinking | 2.2 | (1.7 to 2.8) | 1.7 | (1.3 to 2.2) | ||
| 1 wave binge drinking | 2.9 | (2.1 to 4.0) | 2.0 | (1.4 to 2.8) | ||
| 2+ waves binge drinking | 4.1 | (2.9 to 5.8) | 2.3 | (1.6 to 3.4) | ||
| Wave | <0.001† | <0.001† | ||||
| Wave 7 (mean age 20.7 years) | 1 | 1 | ||||
| Wave 8 (mean age 24.1 years) | 1.1 | (0.96 to 1.3) | 1.1 | (0.96 to 1.3) | ||
| Wave 9 (mean age 29.1 years) | 0.69 | (0.57 to 0.85) | 0.69 | (0.56 to 0.85) | ||
| Gender | ||||||
| Female | 1 | 1 | ||||
| Male | 2.2 | (1.8 to 2.6) | <0.001 | 2.2 | (1.8 to 2.7) | <0.001 |
*Adjusted for adolescent daily smoking, weekly+ cannabis use, depressive symptoms and antisocial behaviour, and parental daily drinking, daily smoking, divorce/separation and level of education.
†p Value from joint test of significance.
Discussion
AUDs increased across early adulthood (21–24 years) before declining in the late 20s (29 years), with cases consistently higher in males than in females. Episodes of loss of control over drinking, binge drinking and heavy binge drinking in teenage females and males were common (21% and 25%, 32% and 47%, 16% and 20%, for females and males, respectively) and associated with significant risk for AUDs well into young adulthood. While we found that the risk of AUD in young adulthood was higher for males than for females, we found no statistical evidence that the associations between teenage drinking behaviour and AUD differed for males and females.
There are a number of explanations for our findings, not all of which imply causal relationships. For example, loss of control while drinking in adolescence (as defined in this analysis) may simply be preclinical features of later dependence that aggregate across the adolescent period into a diagnostic syndrome in young adulthood. In this way, binge drinking may not be causal but simply a characteristic of the early course of AUDs, with continuities in peer and/or family binge drinking culture playing an important role in maintaining teen drinking patterns into young adulthood. Broader social drivers that determine alcohol availability and acceptability of alcohol use may likewise drive continuity in drinking behaviours.5 28
It is, however, also possible that early loss of control over drinking does have fundamental consequences. Imaging studies have now catalogued a broad range of neurodevelopmental effects of alcohol intake during the teenage years.29 Recent studies have shown that acute episodes of alcohol intake during adolescence is linked with alcohol-related neurotoxicity in cortical brain regions relevant to frontoparietotemporal networks.30 Long-term effects consistent with these findings are also being reported. For example, recent results from a 37-year follow-up of young men (mean age 18 years) conscripted to the Swedish military in 1969 show substantial elevations in risk of pre-senile dementia in those reporting earlier alcohol intoxication.
Furthermore, repeated high-dose alcohol exposures followed by abstinence can kindle (or sensitise) receptors in the central nervous system—γ-aminobutyric acid (GABAA) and N-methyl-d-aspartate (NMDA)—that control excitability, neural plasticity and memory.31 The consequences of kindling, particularly in adolescence, may be more intense withdrawal symptoms that perpetuate alcohol use potentially leading to more complex and severe alcohol use problems. Of particular concern, our results show that loss of control drinking in a single session in adolescence may induce other effects.
A significant strength of this study is the high frequency of observations during the adolescent and young adult period. In a repeated measures design with this frequency of observations, bias due to recall errors or motivational revision of past behaviour is minimised. Such gains in accuracy substantially enhance study precision in characterising progression of alcohol use over time, particularly in those with early onset of alcohol use.32 High retention rates within the VAHCS sample also minimise differential attrition in those involved in risky behaviours.33 However, self-report measures may have led to possible under-reporting of some behaviours,34 leading to conservative estimates of risk. To minimise this possibility, participants were assured of confidentiality without consequence for disclosure. Furthermore, the 1-week reference period for reporting alcohol use will not necessarily capture the full extent of drinking in this age group. This means that estimates provided are likely to be conservative in some cases. Finally, non-response is often associated with more extreme behaviours, such as alcohol and drug use, and can introduce bias in estimates of association. In this paper, we correct for this by imputing missing data, using methods of multiple imputation.
Findings from this study suggest that teens who report loss of control and binge drinking behaviours are at higher risk of developing serious alcohol problems in adulthood than those who do not binge drink. Effective intervention in adolescence should be targeted at multiple levels. The public health response should be on prevention or delay of the onset of drinking. There is also an important need to create a different culture around alcohol use that addresses high rates of binge drinking behaviour. The importance of the drinking culture has long been recognised, particularly in young people.35 New approaches that use social marketing strategies to reframe the youth drinking culture are showing promise and gaining greater prominence in the prevention arena;36 however, not all strategies deliver equally37 and there is more work to be done refining these approaches. Beyond universal approaches, there will continue to be a small group of teens who progress to very high-risk alcohol use behaviour defined by loss of control drinking (including the need for hospitalisation). For this high-risk group, clinical interventions may be necessary.38 Further research on drivers of the epidemiological associations we report, and their neurobiological and health consequences, is needed to more greatly enhance targeting of high-risk groups of young people and to ensure the most effective alignment of prevention activities and resources.
Acknowledgments
The authors thank the VAHCS participants for their involvement. The study has been funded by grants from the National Health and Medical Research Council of Australia (NHMRC), the Australian Research Council (ARC), the Australian Rotary Health Research Fund, the Victorian Health Promotion Foundation and the Victoria Government Infrastructure Support Fund.
Footnotes
Contributors: CAO, HR and GCP led the conceptualisation and writing of the manuscript. HR completed the data analysis. JS, PKS, YB and CH were involved in critical revision of the manuscript. All the authors approved the final version of the manuscript.
Funding: The project has been funded for consecutive waves of data collection through the National Health and Medical Research Council (NHMRC) of Australia. Preparation of this paper was supported by The Financial Markets for Children Foundation. CAO is funded by an Australian Research Council (ARC) Principal Research Fellowship (DP130101459). GCP is funded by a NHMRC Senior Principal Research Fellowship.
Competing interests: None declared.
Ethics approval: The Royal Children's Hospital Human Research Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Begg S, Vos T, Barker B et al. Burden of disease and injury in Australia, 2003. Australian Institute of Health and Welfare AIHW, 2007. [Google Scholar]
- 2.Rehm J, Mathers C, Popova S et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009;373:2223–33. 10.1016/S0140-6736(09)60746-7 [DOI] [PubMed] [Google Scholar]
- 3.Teesson M, Hall W, Slade T et al. Prevalence and correlates of DSM-IV alcohol abuse and dependence in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Addiction 2010;105:2085–94. 10.1111/j.1360-0443.2010.03096.x [DOI] [PubMed] [Google Scholar]
- 4.Degenhardt L, O'Loughlin C, Swift W et al. The persistence of adolescent binge drinking into adulthood: findings from a 15-year prospective cohort study. BMJ Open 2013;3:e003015 10.1136/bmjopen-2013-003015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organisation. Global status report: alcohol and young people. World Health Organisation, 2001. [Google Scholar]
- 6.McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: a systematic review of cohort studies. PLoS Med 2011;8:e1000413 10.1371/journal.pmed.1000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Englund MM, Egeland B, Oliva EM et al. Childhood and adolescent predictors of heavy drinking and alcohol use disorders in early adulthood: a longitudinal developmental analysis. Addiction 2008;103(Suppl 1):23–35. 10.1111/j.1360-0443.2008.02174.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Merline A, Jager J, Schulenberg JE. Adolescent risk factors for adult alcohol use and abuse: stability and change of predictive value across early and middle adulthood. Addiction 2008;103(Suppl 1):84–99. 10.1111/j.1360-0443.2008.02178.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oesterle S, Hill KG, Hawkins JD et al. Positive functioning and alcohol-use disorders from adolescence to young adulthood. J Stud Alcohol Drugs 2008;69:100–11. 10.15288/jsad.2008.69.100 [DOI] [PubMed] [Google Scholar]
- 10.Bonomo YA, Bowes G, Coffey C et al. Teenage drinking and the onset of alcohol dependence: a cohort study over seven years. Addiction 2004;99:1520–8. 10.1111/j.1360-0443.2004.00846.x [DOI] [PubMed] [Google Scholar]
- 11.Wells JE, Horwood LJ, Fergusson DM. Drinking patterns in mid-adolescence and psychosocial outcomes in late adolescence and early adulthood. Addiction 2004;99:1529–41. 10.1111/j.1360-0443.2004.00918.x [DOI] [PubMed] [Google Scholar]
- 12.D'Amico EJ, Ellickson PL, Collins RL et al. Processes linking adolescent problems to substance-use problems in late young adulthood. J Stud Alcohol Drugs 2005;66:766–75. 10.15288/jsa.2005.66.766 [DOI] [PubMed] [Google Scholar]
- 13.Kahler CW, Strong DR. A Rasch model analysis of DSM-IV alcohol abuse and dependence items in The National Epidemiological Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res 2006;30:1165–75. 10.1111/j.1530-0277.2006.00140.x [DOI] [PubMed] [Google Scholar]
- 14.Kahler CW, Strong DR, Read JP et al. Mapping the continuum of alcohol problems in college students: a Rasch model analysis. Psychol Addict Behav 2004;18:322–33. 10.1037/0893-164X.18.4.322 [DOI] [PubMed] [Google Scholar]
- 15.Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from The National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med 2006;36:931–41. 10.1017/S003329170600746X [DOI] [PubMed] [Google Scholar]
- 16.Martin CS, Chung T, Langenbucher JW. How should we revise diagnostic criteria for substance use disorders in the DSM-V? J Abnorm Psychol 2008;117:561 10.1037/0021-843X.117.3.561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Composite International Diagnostic Interview (CIDI): interviewer's manual. World Health Organization, 1993. [Google Scholar]
- 18.Andrews G, Peters L. The psychometric properties of the composite international diagnostic interview. Soc Psychiatry Psychiatr Epidemiol 1998;33:80–8. 10.1007/s001270050026 [DOI] [PubMed] [Google Scholar]
- 19.Wittchen HU, Robins LN, Cottler LB et al. Cross-cultural feasibility, reliability and sources of variance of the Composite International Diagnostic Interview (CIDI). The Multicentre WHO/ADAMHA Field Trials. Br J Psychiatry 1991;159:645–53, 658 10.1192/bjp.159.5.645 [DOI] [PubMed] [Google Scholar]
- 20.Livingston M, Laslett AM, Dietze P. Individual and community correlates of young people's high-risk drinking in Victoria, Australia. Drug Alcohol Depend 2008;98:241–8. 10.1016/j.drugalcdep.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 21.Moffitt TE, Silva PA. Self-reported delinquency: results from an instrument for New Zealand. Aust N Z J Criminol 1988; 21:13 10.1177/000486588802100405 [DOI] [Google Scholar]
- 22.Lewis G, Pelosi AJ, Glover E et al. The development of a computerized assessment for minor psychiatric disorder. Psychol Med 1988;18:737–45. 10.1017/S0033291700008448 [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization, 1993. [Google Scholar]
- 24.Harrington R, Fudge H, Rutter M et al. Adult outcomes of childhood and adolescent depression: II. Links with antisocial disorders. J Am Acad Child Adolesc Psychiatry 1991;30:434–9. 10.1097/00004583-199105000-00013 [DOI] [PubMed] [Google Scholar]
- 25.Lewis G, Pelosi AJ, Araya R et al. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med 1992;22:465–86. 10.1017/S0033291700030415 [DOI] [PubMed] [Google Scholar]
- 26.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons, 2004. [Google Scholar]
- 27.Bernaards CA, Belin TR, Schafer JL. Robustness of a multivariate normal approximation for imputation of incomplete binary data. Stat Med 2007;26:1368–82. 10.1002/sim.2619 [DOI] [PubMed] [Google Scholar]
- 28.Patton GC, Coffey C, Cappa C et al. Health of the world's adolescents: a synthesis of internally comparable data. Lancet 2012;379:1665–75. 10.1016/S0140-6736(12)60203-7 [DOI] [PubMed] [Google Scholar]
- 29.Welch KA, Carson A, Lawrie SM. Brain structure in adolescents and young adults with alcohol problems: systematic review of imaging studies. Alcohol Alcohol 2013;48:433–44. [DOI] [PubMed] [Google Scholar]
- 30.Jacobus J, Thayer RE, Trim RS et al. White matter integrity, substance use, and risk taking in adolescence. Psychol Addict Behav 2013;27:431–42. 10.1037/a0028235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Becker H. Kindling in alcohol withdrawal. Alcohol Health Res World 1998;22:25–33. [PMC free article] [PubMed] [Google Scholar]
- 32.Parra GR, O'Neill SE, Sher KJ. Reliability of self-reported age of substance involvement onset. Psychol Addict Behav 2003;17:211–18. 10.1037/0893-164X.17.3.211 [DOI] [PubMed] [Google Scholar]
- 33.Thygesen LC, Johansen C, Keiding N et al. Effects of sample attrition in a longitudinal study of the association between alcohol intake and all-cause mortality. Addiction 2008;103:1149–59. 10.1111/j.1360-0443.2008.02241.x [DOI] [PubMed] [Google Scholar]
- 34.Boden JM, Fergusson DM, Horwood LJ. Illicit drug use and dependence in a New Zealand birth cohort. Aust N Z J Psychiatry 2006;40:156–63. 10.1111/j.1440-1614.2006.01763.x [DOI] [PubMed] [Google Scholar]
- 35.Pederson W. Drinking games adolescents play. Br J Addict 1990;85:1483–90. 10.1111/j.1360-0443.1990.tb01632.x [DOI] [PubMed] [Google Scholar]
- 36.Mattern JL, Neighbors C. Social norms campaigns: examining the relationship between changes in perceived norms and changes in drinking levels. J Stud Alcohol Drugs 2004;65:489–93. 10.15288/jsa.2004.65.489 [DOI] [PubMed] [Google Scholar]
- 37.Wechsler H, Nelson TF, Lee JE et al. Perception and reality: a national evaluation of social norms marketing interventions to reduce college students’ heavy alcohol use. J Stud Alcohol Drugs 2003;64:484–94. 10.15288/jsa.2003.64.484 [DOI] [PubMed] [Google Scholar]
- 38.Conrod PJ, Castellanos-Ryan N, Mackie C. Long-term effects of a personality-targeted intervention to reduce alcohol use in adolescents. J Consult Clin Psychol 2011;79:296–306. 10.1037/a0022997 [DOI] [PubMed] [Google Scholar]