Abstract
Objectives
We sought to characterize the number and types of care transitions in the last 6 months of life made by patients who used hospice and examined factors associated with having multiple transitions in care.
Design, Setting, and Participants
We performed a retrospective cohort study of fee-for-service Medicare beneficiaries, aged 66 years or older who died between July 1, 2011 and December 31, 2011, and were enrolled in hospice at some time during the last 6 months of life. We used hierarchical generalized linear modeling to identify patient, hospice, and regional factors associated with transitions. We also described the sequence of transitions across healthcare settings.
Measures
Healthcare transitions after hospice enrollment included from/to hospital, skilled nursing facility, home health agency program, hospice, or home without receiving any service above.
Results
Among 311,090 hospice decedents, 31,675 (10.2%) had at least one transition after hospice enrollment and this varied substantially across the United States. A total of 6.6% of all decedents had more than one transition in care after hospice enrollment, with a range from 2–19 transitions. Among hospice users with transitions, 53.4% were admitted to hospitals, 17.7% were admitted to skilled nursing facilities, 9.6% used home health agencies, and 25.8% had transitions to home without receiving services we examined. In adjusted analyses, decedents who were younger, nonwhite, enrolled in a for-profit or small hospice program, or had less access to hospital-based palliative care had significantly higher odds of having at least one transition.
Conclusion
A notable proportion of hospice users experience at least one transition in care in the last 6 months of life, suggesting further research on their impact on patients and families is warranted.
Keywords: Hospice, transitions in care, end-of-life care
INTRODUCTION
Previous research has highlighted that care at the end of life can be fragmented, with poor coordination and communication among health care providers.1,2 The Institute of Medicine report Dying in America has raised the concern that people nearing the end of life often experience multiple transitions, which could create burdens for patients and families.3 While hospice use has been embraced as an indicator of quality of end-of-life care,4–6 hospice enrollees may have transitions in care across healthcare settings. Furthermore, hospice disenrollment occurs and has been shown to be associated with substantially increased hospital utilization and costs.7–9 Such transitions in care can cause substantial anxiety for patients and their family members:10,11 they are especially vulnerable to chaotic transitions and poor patient outcomes because of unfamiliar settings and providers, and lack of adequate communication regarding goals of care.12–14
Despite important concerns about fragmentation in care at the end of life, little is known about the number and types of transitions experienced by hospice users prior to death. A small number of studies have examined this issue.7,15–18 One study found that 6% of patients with lung or colorectal cancer were admitted to the hospital at least once after hospice enrollment.15 Two studies reported hospitalization and hospice disenrollment among Medicare hospice users with cancer7 or heart failure.17 A recent study analyzed Medicare, Medicaid and Minimum Data Set data from a single safety net health care system and found that 9.9% of 3,771 hospice patients had hospitalization during or after hospice ended.16 These studies were limited to specific populations or settings, as well as focused on transitions from hospice to hospital. Only one study reported hospitalization and skilled nursing facility (SNF) admission within 30 days after live discharge from hospice.18 These studies have not identified the number or type of transitions across settings, nor the factors that are associated with transitions in care at the end of life.
Accordingly, we sought to describe the frequency and types of transitions during the last 6 months of life for decedents who enrolled with hospice. To accomplish this aim, we analyzed Medicare claims data for all fee-for-service Medicare decedents who used hospice in the last 6 months of life and died in 2011, and used multivariable analyses to identify patient, hospice, and regional factors associated with increased likelihood of transitions. Findings from this research can be useful for understanding patterns of and risk factors for increased fragmentation in care at the end of life.
METHODS
Overview
We included all possible transitions across healthcare settings because little is known about transition in care after hospice enrollment. Current recommendations encouraged transition to hospice and palliative programs, yet hospice is not the end of care trajectory. Understanding the current patterns of transitions after hospice can identify the areas where improvement of hospice programs would further comfort beneficiaries and their family. Given that hospitalization incurs substantial costs and hospitalization from hospice directly indicated a larger failure of the healthcare system, we also examined the associations between patient/market factors and transitions from hospice to hospital.
Study design and sample
We conducted a retrospective analysis of all fee-for-service Medicare beneficiaries older than 66 years who died between July 1, 2011, and December 31, 2011. We limited our sample to Medicare Parts A and B beneficiaries who had enrolled in the Medicare hospice benefit at some time during their last 6 months prior to death. The study was reviewed by the institutional review board of Yale University and was exempt from full review.
Measurement
Outcomes
Our primary outcome was a binary variable indicating patients who had at least one transition in care after initial enrollment with hospice. All inquiries of transition started after the decedent’s earliest hospice claim in the 6 months prior to death. We focused on transitions across healthcare settings, including transferring from/to hospital, skilled nursing facility (SNF), home health agency (HHA) program, hospice, or “home” without receiving services from the four healthcare settings above. The category home is arbitrary, meaning that patients 1) were discharged from hospital or SNF, or were disenrolled from HHA or hospice (regardless of inpatient hospice or home hospice) and 2) did not receive care from any of above. Of note, “home” entails the patients disenrolled from hospice. We measured these transitions because they would most likely involve changes in the patient’s care team, leading to concerns regarding fragmented care. We did not include transitions between inpatient hospice and home hospice because this type of transition would likely be managed by a single hospice provider and involve continuity in the care team. We calculated the total number of transitions each beneficiary experienced, and identified the health care settings of the first and second transitions. For transfers to/from the hospital setting, we also assessed the occurrence of emergency department (ED) visits, intensive care unit (ICU) admissions, and in-hospital death.
Covariates
Following the Andersen behavioral model,19 we conceptualized the factors that might be associated with transitions in care into predisposing (such as age, education, and race), need (such as clinical conditions and comorbidities) and enabling (such as income and market factors) variables. Predisposing factors included patient age (categorized as 66–69 years, 70–74 years, 75–79 years, 80–84 years, and ≥85 years), race/ethnicity (non-Hispanic white, black, Hispanic, and other), gender and census based estimates of percentage of adults with high school education or less at the zip code level.
Need factors included primary diagnosis based on the International Classification of Diseases, Ninth Revision (ICD-9) codes and categorized as follows: neoplasms; mental disorders; diseases of the nervous system and sense organs; diseases of the circulatory system; diseases of the respiratory system; symptoms, signs, and ill-defined conditions; and other. We also ascertained chronic conditions using data from the Master Beneficiary Summary File including heart disease (acute myocardial infarction, heart failure, and ischemic heart disease), Alzheimer’s disease or dementia, kidney disease, diabetes, chronic obstructive pulmonary disease or asthma, depression, stroke, and cancer (breast, colorectal, prostate, lung, and endometrial). We then categorized decedents based on their count of comorbid conditions. Using revenue center code values of 0655 and 0656, we determined whether beneficiaries had used hospice Inpatient Respite Care or General Inpatient Care before the date of the first healthcare transition or the date of death if they did not have transition.20 We also adjusted for time from hospice enrollment to death (a continuous variable from 0 day to 179 days).
We identified enabling factors including income and market factors using the county of residence and the hospital referral region (HRR) for each beneficiary. We used data pertaining to the county in which the patient resided using the Area Resource File, which included metropolitan residence status, median county-level income, the percentage of individuals in health maintenance organizations (HMOs) in the county, and the number of physicians, hospital beds, skilled nursing facility beds, hospices, and home health agencies per 1,000 people aged 65 and older in the county. Also, we used HRRs to approximate markets. Prior literature generally used counties or HRRs to define hospice market,21,22 but results are often insensitive to the choices between HRRs and counties.23 Another reason we used HHRs was the concern about small sample size at the county level. We employed the Herfindahl–Hirschman Index24 as the HRR-level measure of hospice facility market competition (<0.15, 0.15–0.25, and ≥0.25, indicating competitive, moderately concentrated, and highly concentrated market, respectively). We included the characteristics of hospice agency where the decedent first used hospice based on the Provider of Services file, including ownership (for-profit and nonprofit), duration of hospice operation (years; <10, 10–18, 18–23, and >=24), size (measured as the number of individuals cared for during the study period by the hospice categorized at the quartiles of the distribution), and inpatient service provision status (none, provided by staff, under contract arrangement, and both). We included each hospice’s accreditation, including none, The Joint Commission’s Home Care Accreditation Program, Community Health Accreditation Program, and Accreditation Commission for Health Care. We also included factors about whether hospice was regulated by Certificate of Need (CON)25 and the percentage of hospitals reporting palliative care services (categorized as ≤20%, 21–40%, 41–60%, 61–80%, and ≥80%),26 both were state-level characteristics reported in 2011.
Statistical Analysis
We used standard descriptive statistics to describe the patient sample and prevalence of transitions by type of transition overall and for each state. We described the trajectories of transitions – the proportions of hospice users in terms of the first transition healthcare setting among those with at least one transition, and the second transition healthcare setting according to the first healthcare setting.
Using 4-level hierarchical generalized linear models (HGLMs), we identified patient-, hospice-, HRR-, and state-level factors that were significantly associated with having a transition. To reduce variability caused by low hospice volumes, we excluded from the HGLM analysis hospices that had less than fifteen decedents during the study period. We used the variance inflation factors of independent variables using multivariate linear regression models to assess potential multicollinearity within the model. We assessed the variation at the hospice, HRR and state levels using the covariance estimate at each level, derived from the random effect of HGLMs. We also employed the same model to identify factors that were associated with hospitalization from hospice directly. All statistical analyses were completed using SAS, version 9.3 (SAS Institute, Cary, NC), and a two-tailed p<.05 was used to define statistical significance.
RESULTS
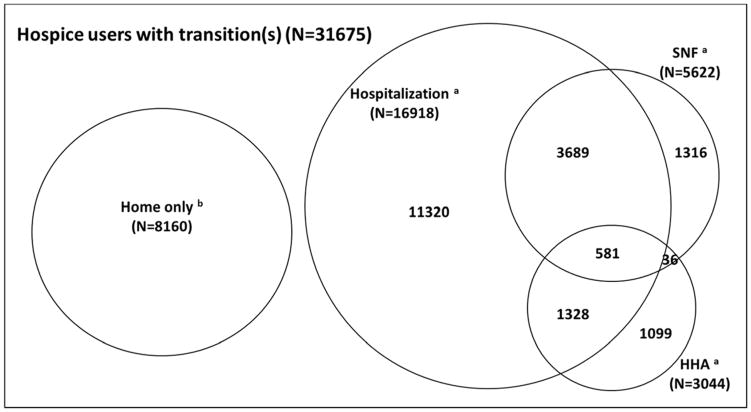
The full study sample consisted of 311,090 decedents who used hospice during the last 6 months of life. A total of 10.2% (N=31,675) of them had at least one healthcare transition after hospice enrollment (mean = 2.3; median = 2; SD =1.7). A total of 6.6% of all decedents had more than one transition in care after hospice enrollment, with a range from 2–19 transitions. The most common type of transition was to the hospital: 53.4% of decedents who had healthcare transitions were admitted to a hospital, although many other types of transitions also occurred (Figure 1). A total of 16,918 decedents had at least one hospitalization after hospice enrollment (mean = 1.32; SD =0.73), with a range from 1–9 hospitalizations. Characteristics of hospice users who had and did not have at least one transition were summarized in Table 1. Compared with those who did not have transitions, hospice users who had transitions were more likely to be younger or non-white, have comorbidities, or receive inpatient hospice care (all P-values <.001).
Figure 1.
Utilization Patterns among 31,675 Hospice Users (10% of All Hospice Users) with at Least One Healthcare Transition
The transitions shown are the numbers of decedents who had been transitioned to these healthcare settings.
a: Can have transitions to home or hospice re-enrollment
b: Can have hospice re-enrollment, but did not have transitions to hospital, SNF, or HHA
SNF: Skilled nursing facility; HHA: Home health agency
Table 1.
Patient Characteristics According to Healthcare Transition Status among Hospice Users
| Sample characteristics | Having transitions after hospice enrollment | Not having transitions after hospice enrollment | p-value |
|---|---|---|---|
|
| |||
| Sample size | 31,675 (10.2%) | 279,415 (89.2%) | |
|
Predisposing Factors
| |||
| Age | <.001 | ||
| 66–69 | 2,428 (7.7%) | 18,825 (6.7%) | |
| 70–75 | 3,396 (10.7%) | 28,787 (10.3%) | |
| 75–79 | 4,500 (14.2%) | 38,282 (13.7%) | |
| 80–84 | 6,187 (19.5%) | 54,275 (19.4%) | |
| 85+ | 15,164 (47.9%) | 139,246 (49.8%) | |
| Sex | <.001 | ||
| Male | 13,521 (42.7%) | 116,106 (41.6%) | |
| Female | 18,154 (57.3%) | 163,309 (58.4%) | |
| Race | <.001 | ||
| White | 26,297 (83.0%) | 246,995 (88.4%) | |
| Black | 3,360 (10.6%) | 17,842 (6.4%) | |
| Hispanic | 1,344 (4.2%) | 9,541 (3.4%) | |
| Other | 674 (2.1%) | 5,037 (1.8%) | |
| Education (>=high school; missing no=175) | <.001 | ||
| < 60% | 48 (0.2%) | 262 (0.1%) | |
| 60 – 70 | 688 (2.2%) | 4,291 (1.5%) | |
| 70 – 80 | 5,486 (17.3%) | 40,010 (14.3%) | |
| 80 – 90 | 19,625 (62.0%) | 174,770 (62.6%) | |
| ≥ 90 | 5,804 (18.3%) | 59,931 (21.5%) | |
|
| |||
|
Need Factors
| |||
| Numbers of Comorbidity | <.001 | ||
| 0–2 | 3,192 (10.1%) | 35,875 (12.8%) | |
| 3 | 4,017 (12.7%) | 41,286 (14.8%) | |
| 4 | 5,869 (18.5%) | 55,532 (19.9%) | |
| 5 | 6,719 (21.2%) | 58,140 (20.8%) | |
| 6 | 5,953 (18.8%) | 46,865 (16.8%) | |
| 7–8 | 5,925 (18.7%) | 41,717 (14.9%) | |
| Primary diagnosis for hospice enrollment | <.001 | ||
| Neoplasms | 9,535 (30.1%) | 88,125 (31.5%) | |
| Mental disorders | 3,173 (10.0%) | 27,910 (10.0%) | |
| Diseases of the nervous system | 2,534 (8.0%) | 21,548 (7.7%) | |
| Diseases of the circulatory system | 6,009 (19.0%) | 50,950 (18.2%) | |
| Diseases of the respiratory system | 3,031 (9.6%) | 23,768 (8.5%) | |
| Symptoms, signs, and ill-defined conditions | 6,055 (19.1%) | 49,024 (17.6%) | |
| Other | 1,338 (4.2%) | 18,090 (6.5%) | |
| Receiving respite or general inpatient hospice care | <.001 | ||
| No | 16,169 (68.8%) | 204,257 (71.0%) | |
| Yes | 7,346 (31.2%) | 83,318 (29.0%) | |
|
| |||
|
Enabling Factors
| |||
| Median household income (missing no=175) | <.001 | ||
| < $33,000 | 478 (1.5%) | 2,242 (0.8%) | |
| $33,000 – $39,999 | 7,128 (22.5%) | 52,040 (18.6%) | |
| $40,000 – $49,999 | 12,065 (38.1%) | 106,660 (38.2%) | |
| $50,000 – $62,999 | 7,956 (25.1%) | 77,420 (27.7%) | |
| ≥ $63,000 | 4,024 (12.7%) | 40,902 (14.7%) | |
| Metropolitan statistical area | <.001 | ||
| No | 2,992 (9.4%) | 22,907 (8.2%) | |
| Micropolitan | 4,328 (13.7%) | 35,755 (12.8%) | |
| Metropolitan | 24,331 (76.9%) | 220,602 (79.0%) | |
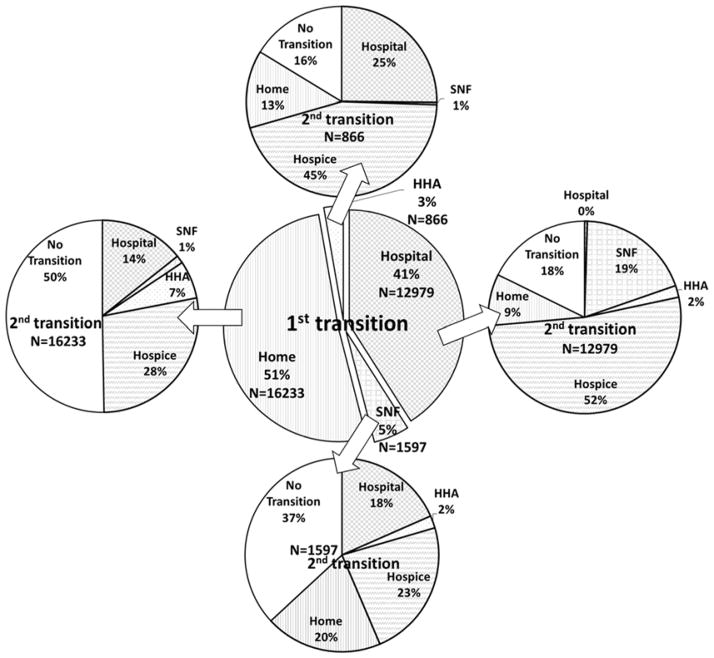
We characterized the first and second transitions after hospice enrollment (Figure 2). For the first transition, 41% were transitioned from hospice to hospital, 5% to SNF, 3% to HHA, and 51% were disenrolled from hospice and received no services from the healthcare settings we examined. The second transition depended on the location of the first transition. For example, if the first transition was from hospice to hospital, the second transition was as follows: 52% transitioned from hospital to hospice, 19% to SNF, 2% to HHA, 9% to home, and 18% of them died in hospital (i.e., no transition).
Figure 2.
The First and Second Healthcare Transitions among 31,675 Hospice Users Who Had at Least One Transition
SNF: Skilled nursing facility; HHA: Home health agency; “No Transition” means that patients died within the first transition healthcare setting; “Home” means that patients did not receive any service from hospital, SNF, HHA, or hospice
The proportion of decedents who experienced at least one transition after hospice enrollment varied substantially across states (Table 2). The mean proportion of hospice users in a state who had at least one healthcare transition was 10.3% and ranged from 6.9% in Idaho to 20.6% in Florida. The proportion who had a transition to hospital ranged from 1.6% in North Dakota to 13.4% in Mississippi; the proportion who had a transition to SNF ranging from 0.3% in Hawaii to 4.1% in Alabama; and the proportion who had a transition to HHA ranged from 0.1% in South Dakota to 2.1% in Alabama. The proportion who had a transition to home without receiving any services we examined ranged from 4.6% in South Dakota to 11.6% in Florida. For hospice enrollees, Alabama is the state with the highest proportions of ED visits and ICU admission, and District of Columbia with the highest proportion of in-hospital death.
Table 2.
Variations of Healthcare Transition and Utilization of Hospital-Based Services after Hospice Enrollment across States
| Measures | Mean | Std Dev | Minimum | Maximum |
|---|---|---|---|---|
| Healthcare transition | ||||
| Healthcare transitions after hospice enrollment (%) a | 10.3 | 2.9 | 6.9 | 20.6 |
| Hospitalization after hospice enrollment (%) | 5.2 | 2.6 | 1.6 | 13.4 |
| Skilled nursing facility admission after hospice enrollment (%) | 1.7 | 0.7 | 0.3 | 4.1 |
| Home health agency service utilization after hospice enrollment (%) | 0.9 | 0.5 | 0 | 2.1 |
| Transitions to home (%) | 6.5 | 1.4 | 4.6 | 11.6 |
| Utilization of hospital-based services | ||||
| Emergency department visit after hospice enrollment (%) | 4.3 | 2.4 | 1.1 | 11.3 |
| Intensive care unit admission after hospice enrollment (%) | 1.8 | 1.2 | 0 | 4.8 |
| In-hospital death after hospice enrollment (%) | 1.9 | 1.1 | 0.5 | 5.5 |
The unit of analysis is state (each value represented the mean of state means). Healthcare transition refers to any transition from/to hospital, skilled nursing facility, home health agency program, hospice, or home (meaning no services from hospital, skilled nursing facility, home health agency program, or hospice).
Decedents may have more than one transitions
In the multivariable analyses, we found younger adults, male, non-white, and those with more comorbidities were more likely to have healthcare transitions after hospice enrollment, compared with older adults, female, white, and those with fewer comorbidities (Table 3). Compared with hospice users who had cancer as their primary diagnosis for hospice enrollment, hospice users whose primary diagnosis were mental disorders, diseases of the nervous system or symptoms, signs, and ill-defined conditions were less likely to have transitions. Decedents who used hospice inpatient care were more likely to have healthcare transitions, compared with those who did not use hospice inpatient care. Geographic factors, such as income and metropolitan residence, were not significantly associated with healthcare transitions. Decedents who were enrolled in a nonprofit hospice, a larger hospice, or a hospice in business for a longer period of time were less likely to have healthcare transitions.
Table 3.
Adjusted Odds Ratios and 95% CIs of at Least One Healthcare Transition or Hospitalization after Hospice Enrollment a
| Transition in care OR (95% CI) |
Hospitalizationb OR (95% CI) |
|
|---|---|---|
|
Predisposing Factors
| ||
| Age | ||
| 66–69 | 1.38 (1.31, 1.46) | 1.5 (1.39, 1.62) |
| 70–74 | 1.22 (1.17, 1.28) | 1.39 (1.31, 1.49) |
| 75–79 | 1.17 (1.12, 1.21) | 1.33 (1.25, 1.4) |
| 80–84 | 1.11 (1.07, 1.15) | 1.22 (1.16, 1.28) |
| 85+ | reference | reference |
| Sex | ||
| Male | 1.19 (1.16, 1.22) | 1.1 (1.06, 1.14) |
| Female | reference | reference |
| Race | ||
| White | reference | reference |
| Black | 1.59 (1.52, 1.67) | 1.93 (1.82, 2.05) |
| Hispanic | 1.31 (1.22, 1.4) | 1.36 (1.23, 1.51) |
| Other | 1.37 (1.25, 1.51) | 1.38 (1.21, 1.58) |
| Percent ≤ HS education of zip code | ||
| Less than 60% | 1.04 (0.7, 1.55) | 1.79 (1.11, 2.9) |
| 60 to <70% | 1.11 (0.98, 1.26) | 1.29 (1.08, 1.54) |
| 70 to <80 % | 1.08 (1, 1.16) | 1.17 (1.05, 1.31) |
| 80 to <90% | 1.06 (1, 1.11) | 1.11 (1.02, 1.2) |
| 90% or more | reference | reference |
|
| ||
|
Need Factors
| ||
| Numbers of Comorbidity | ||
| 0–2 | reference | reference |
| 3 | 1.01 (0.95, 1.06) | 1.12 (1.03, 1.22) |
| 4 | 1.02 (0.97, 1.07) | 1.23 (1.13, 1.33) |
| 5 | 1.06 (1.01, 1.12) | 1.34 (1.24, 1.45) |
| 6 | 1.1 (1.04, 1.15) | 1.47 (1.35, 1.59) |
| 7–8 | 1.14 (1.08, 1.20) | 1.61 (1.48, 1.74) |
| Primary diagnosis for hospice enrollment | ||
| Neoplasms | reference | reference |
| Mental disorders | 0.78 (0.74, 0.82) | 0.66 (0.61, 0.71) |
| Diseases of the nervous system and sense organs | 0.73 (0.69, 0.77) | 0.65 (0.6, 0.7) |
| Diseases of the circulatory system | 1.01 (0.97, 1.05) | 1.03 (0.97, 1.09) |
| Diseases of the respiratory system | 1 (0.95, 1.05) | 1.16 (1.09, 1.24) |
| Symptoms, signs, and ill-defined conditions | 0.93 (0.9, 0.97) | 0.82 (0.78, 0.87) |
| Other | 0.87 (0.82, 0.93) | 0.63 (0.57, 0.7) |
| Receiving hospice inpatient services | ||
| No | 0.68 (0.66, 0.7) | 0.57 (0.54, 0.59) |
| Yes | reference | reference |
| Days of hospice enrollment (continuous variable) | 1.01 (1.01, 1.01) | 1.01 (1.01, 1.01) |
|
| ||
|
Enabling Factors
| ||
| Median income of county | ||
| Less than $33,000 | 1.12 (0.95, 1.33) | 1.79 (1.11, 2.9) |
| $33,000–40,000 | 1.04 (0.96, 1.13) | 1.29 (1.08, 1.54) |
| $40,000–50,000 | 0.99 (0.93, 1.06) | 1.17 (1.05, 1.31) |
| $50,000–63,000 | 1.01 (0.95, 1.07) | 1.11 (1.02, 1.2) |
| $63,000 or more | reference | reference |
| Hospice ownership | ||
| Nonprofit | 0.93 (0.89, 0.97) | 0.74 (0.69, 0.8) |
| For-profit | reference | reference |
| Year of hospice operation | ||
| ≥24 | 0.95 (0.89, 1.02) | 0.8 (0.73, 0.88) |
| 19–24 | 0.91 (0.86, 0.97) | 0.78 (0.71, 0.85) |
| 10–19 | 0.93 (0.88, 0.97) | 0.86 (0.8, 0.92) |
| <10 | reference | reference |
| Number of hospice admission during study period | ||
| ≥1,247 | 0.76 (0.71, 0.81) | 0.85 (0.76, 0.94) |
| 545–1247 | 0.78 (0.73, 0.82) | 0.77 (0.71, 0.84) |
| 241–545 | 0.8 (0.77, 0.84) | 0.81 (0.76, 0.87) |
| <241 | reference | reference |
| County-level HMO penetration rate (quartile) | ||
| ≥31.14% | 0.97 (0.91, 1.03) | 0.94 (0.86, 1.04) |
| 19.47–31.14% | 0.92 (0.87, 0.98) | 0.87 (0.8, 0.94) |
| 11.75–19.47% | 0.97 (0.92, 1.01) | 0.95 (0.89, 1.02) |
| <11.75% | reference | reference |
| County-level Hospice number per-1,000-people-65-and-older | ||
| ≥0.126 | 0.96 (0.92, 1.01) | 0.9 (0.84, 0.97) |
| 0.063–0.126 | 0.89 (0.85, 0.94) | 0.84 (0.78, 0.91) |
| 0.020–0.063 | 0.95 (0.9, 1.01) | 0.91 (0.84, 0.99) |
| <0.020 | reference | reference |
| State certificate of need health laws | ||
| No | 0.83 (0.76, 0.9) | 0.72 (0.61, 0.86) |
| Yes | reference | reference |
| State access to palliative care in hospitals | ||
| ≥81% | 0.84 (0.68, 1.05) | 0.59 (0.39, 0.91) |
| 61–80% | 0.91 (0.74, 1.11) | 0.79 (0.53, 1.17) |
| 41–60% | 0.9 (0.73, 1.1) | 0.8 (0.53, 1.2) |
| 21–40% | 1.08 (0.86, 1.36) | 1.11 (0.7, 1.77) |
| ≤20% | reference | reference |
|
| ||
|
Covariance Parameter Estimates in the 4-Level HGLM
| ||
| Hospice | 0.1256 | 0.2338 |
| Hospital referral region | 0.0146 | 0.0282 |
| State | 0.0055 | 0.0436 |
OR: Odds ratio; CI: Confidence interval; HGLM: Hierarchical generalized linear model
adjusting for predisposing, need and enabling factors, clustered by hospice, hospital referral region, and state
hospitalization directly from hospice
Several market factors were associated with the likelihood of experiencing at least one transition in care in the multivariable analysis. Decedents in areas that were in the second quartile in terms of HMO penetration rate and number of hospices per 1,000 people aged 65 and older were less likely to have healthcare transitions, compared with the corresponding lowest quartile areas. The absence of CON regulations was associated with decreased odds of healthcare transitions. Hospice market concentration, county-level physician number, or county-level hospital bed number was not associated with the likelihood of transition. Based on the covariance parameter estimates in the 4-level HGLM, the variation was much larger at the hospice level, compared with HRR and state levels. Additionally, our analyses showed that the predisposing, need, and enabling factors generally had similar impact on at least one transition and hospitalization from hospice, with differences in terms of magnitude (Table 3).
DISCUSSION
We found approximately 10% of the hospice users nationally had at least one transition after their hospice enrollment, although in some states, the proportion with at least one transition exceeded 20%. Such transitions may place patients at risk for discontinuity of care and medical errors and cause increased stress for caregivers.27–30 As Medicare reimburses for hospice inpatient care to support patients with complicated needs,31,32 it is surprising that so many patients have a transition in care. Furthermore, the provider- and state-level variation in the proportion of hospice users who have transitions in care suggests that transitions may be influenced by provider and market factors and not solely by patient and family preferences. This is the first study of which we know to document using contemporary data the national patterns of healthcare transitions among hospice enrollees.
Our study advances current knowledge about healthcare transitions and care trajectories at the end of life. While a number of studies pertaining to older adults have examined healthcare transitions from home and nursing homes to hospital and then to hospice care, a small number of studies investigated transitions after hospice enrollment, and most of these studies have been limited to specific populations, settings, or transitions.7,9,15–18 Using national data, Aldridge et al. reported that approximately 11% of Medicare decedents disenrolled from hospice before death in 2010, but the authors did not examine transitions in care to other providers.9 Teno et al. described transitions after hospice disenrollment;18 however, transitions in care before disenrollment may be overlooked. For example, beneficiaries could have transitions such as hospitalization without hospice disenrollment.
Our study adds to the extant literature by understanding transition trajectories after hospice enrollment, national variation of the transitions, and factors associated with transitions. We found that some hospice beneficiaries might have numerous transitions across different healthcare settings and more than 50% of beneficiaries who had at least one transition have been admitted to hospital. These transitions are not only expensive, but may not lead to better patient care or quality of life. Many of these transitions may be avoidable through advance care planning, appropriate provider-to-provider communication, and proper hospice inpatient care.3,33,34 Efforts to reduce post-hospice transitions could result in substantial cost saving and improve quality of end-of-life care.
Similar to other studies examining hospice disenrollment, several predisposing factors were associated with transitions.15,17,30 We found that patients who were non-white were more likely to have healthcare transitions. Plausible explanations include cultural and religious tradition about death, mistrust about the hospice program, and lack of knowledge about hospice care.15,17,35 Patients with more comorbidities were more likely to have transitions, reflecting that these patients and their family members had an increased need for additional care. In addition to patient characteristics, several hospice characteristics are associated with the likelihood of transitions: Patients were less likely to have transitions if they were enrolled in hospice program which was non-profit, had been in business longer, and had a larger patient base, consistent with the findings in prior studies examining hospice disenrollment.18,36 We were surprised that states which do not have CON laws were associated with a decreased likelihood of transitions, compared with states with CON laws. This finding appears inconsistent with the expectation, according to the public interest theory, that government policies enhance efficiency and equity.37 However, CON laws could be a marker of access to hospice, which may be associated with hospice behavior. For example, Carlson et al. have shown that states without a CON policy were independently associated with greater geographic access to hospice.38 Additionally, states which have higher access to palliative care in hospitals tended to be less likely to have transitions, compared with states with lower access to palliative care, indicating that hospital-based palliative care teams may influence care transitions to and from hospitals for hospice enrollees. Efforts to increase access to palliative care in hospitals may decrease transitions.
Our study also expands previous work by finding that substantial variation was observed at the hospice level, rather than at the HRR or state level, indicating that provider behavior may be a key determinant of transitions in care. Given the adverse consequences resulting from transitions, there has been national attention to care transitions in the United States.3 Our findings suggest that healthcare transitions after hospice enrollment might be used as a quality indicator for hospice care. Indeed, the Centers for Medicare and Medicaid Services (CMS) created the Hospice Quality Reporting Program to provide consumer and provider hospice quality, mandated by the Affordable Care Act of 2010.39 Transitions in care defined in this study are based on the administrative data and could quickly and efficiently provide a performance measure and support quality improvement efforts.
Although we employed the CMS definition of transitions in care,40 we recognize that not all post-hospice enrollment transitions are the same. We cannot ascertain from our data what the cause of the transition was; however, some transitions may be more likely to reflect family and patient preferences whereas other transitions may be more indicative of fragmented care. For instance, hospitalization from hospice directly could indicate a larger failure (since hospice was supposed to minimize hospitalizations) whereas hospitalization from home after being discharged from hospice was more likely to reflect family and patient preferences. Therefore, our analyses have specifically examined transitions from hospice to hospital, in addition to any transitions in care. The results were qualitatively similar (see Table 3). Nevertheless, future research identifying and examining care transitions which deviate from patient preferences is needed.
Our study has several limitations. As a cross-sectional study, we are unable to make causal inferences, although the descriptive findings are novel. In addition, although transitions in care may be disruptive to patients and their families, we lacked information about patient and family preferences and hence cannot assess the full impact of such transitions. However, prior literature has shown that patient preferences explain little of regional variation in end-of-life healthcare utilization.41,42 Also, we had data only on decedents and hence we could not analyze the trajectories of patients who were enrolled in hospice but did not die during the study period, which could be a topic for future research. Last, we determined transition in care using the admission and discharge dates of the Medicare claims. When there was continuity of care within a certain clinical setting, we did not consider it as transition in care, even if a beneficiary received care from two different providers within that setting. Thus, the average numbers of transitions would be underestimated.
The Medicare hospice benefit policy at the time of this research was that hospice enrollees were required to forgo curative care for their primary condition. The CMS is launching a pilot program43 in which Medicare beneficiaries who enroll in hospice can continue to receive both curative and palliative treatments at the same time, which may result in increased transitions in care. Nonetheless, we found that approximately 10% of hospice users have transitions in care after hospice enrollment. More than 6% had more than one transitions, which may be disruptive to end-of-life care. We also found substantial geographical variation in the proportion of hospice users that have transition in care, suggesting the fragmentation in end-of-life care vary across the United States. Future studies that examine the impact of such transitions in care at the end of life on costs and the experience of patients and their families are warranted.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by grant 1R01CA116398-01A2 from the National Cancer Institute (Drs. Aldridge and Bradley); the John D. Thompson Foundation (Dr. Bradley); and grant 1R01NR013499-01A1 from the National Institute of Nursing Research (Dr. Aldridge).
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Financial Disclosures: Dr. Gross receives support from Medtronic, Inc., Johnson & Johnson, Inc., and 21st Century Oncology. These sources of support were not used for any portion of the current manuscript. None of the other coauthors have conflicts to report.
Author Contributions: Dr. Wang had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Wang, Aldridge, Gross, Canavan, Cherlin, Bradley.
Acquisition of data: Bradley.
Analysis and interpretation of data: Wang, Aldridge, Gross, Canavan, Cherlin, Hürzeler, Bradley.
Drafting of the manuscript: Wang, Aldridge, Gross, Bradley.
Critical revision of the manuscript for important intellectual content: Wang, Aldridge, Gross, Canavan, Cherlin, Hürzeler, Bradley.
Statistical analysis: Wang.
Obtained funding: Aldridge, Bradley.
Administrative, technical, and material support: Canavan, Cherlin, Hürzeler.
Study supervision: Wang, Aldridge, Gross, Bradley.
References
- 1.NIH State-of-the-Science Conference Statement on improving end-of-life care. NIH Consens State Sci Statements. 2004;21:1–26. [PubMed] [Google Scholar]
- 2.Gerardi D. Team Disputes at End-of-Life: Toward an Ethic of Collaboration. Perm J. 2006;10:43–44. doi: 10.7812/tpp/06-030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Dying in America. [Accessed March 20, 2015];Improving Quality and Honoring Individual Preferences Near the End of Life. 2014 doi: 10.7205/MILMED-D-15-00005. Available at http://www.nap.edu/openbook.php?record_id=18748. [DOI] [PubMed]
- 4.Earle CC, Park ER, Lai B, et al. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003;21:1133–1138. doi: 10.1200/JCO.2003.03.059. [DOI] [PubMed] [Google Scholar]
- 5.Grunfeld E, Urquhart R, Mykhalovskiy E, et al. Toward population-based indicators of quality end-of-life care: Testing stakeholder agreement. Cancer. 2008;112:2301–2308. doi: 10.1002/cncr.23428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NQF endorses cancer measures [news release] Washington, DC: National Quality Forum; Aug 10, 2012. [Accessed September 15, 2014]. (online). Available at http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_Cancer_Measures.aspx. [Google Scholar]
- 7.Carlson MD, Herrin J, Du Q, et al. Impact of hospice disenrollment on health care use and Medicare expenditures for patients with cancer. J Clin Oncol. 2010;28:4371–4375. doi: 10.1200/JCO.2009.26.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aldridge MD, Schlesinger M, Barry CL, et al. National hospice survey results: For-profit status, community engagement, and service. JAMA Intern Med. 2014;174:500–506. doi: 10.1001/jamainternmed.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aldridge MD, Canavan M, Cherlin E, et al. Has Hospice Use Changed? 2000–2010 Utilization Patterns. Med Care. 2015;53:95–101. doi: 10.1097/MLR.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tai E, Buchanan N, Townsend J, et al. Health status of adolescent and young adult cancer survivors. Cancer. 2012;118:4884–4891. doi: 10.1002/cncr.27445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rickerson E, Harrold J, Kapo J, et al. Timing of hospice referral and families’ perceptions of services: Are earlier hospice referrals better? J Am Geriatr Soc. 2005;53:819–823. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 12.Davis MM, Devoe M, Kansagara D, et al. “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27:1649–1656. doi: 10.1007/s11606-012-2169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meier DE, Beresford L. Palliative care’s challenge: Facilitating transitions of care. J Palliat Med. 2008;11:416–421. doi: 10.1089/jpm.2008.9956. [DOI] [PubMed] [Google Scholar]
- 14.Hauser JM. Lost in transition: The ethics of the palliative care handoff. J Pain Symptom Manage. 2009;37:930–933. doi: 10.1016/j.jpainsymman.2009.02.231. [DOI] [PubMed] [Google Scholar]
- 15.Cintron A, Hamel MB, Davis RB, et al. Hospitalization of hospice patients with cancer. J Palliat Med. 2003;6:757–768. doi: 10.1089/109662103322515266. [DOI] [PubMed] [Google Scholar]
- 16.Unroe KT, Sachs GA, Dennis ME, et al. Hospice use among nursing home and non-nursing home patients. J Gen Intern Med. 2015;30:193–198. doi: 10.1007/s11606-014-3080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Unroe KT, Greiner MA, Johnson KS, et al. Racial differences in hospice use and patterns of care after enrollment in hospice among Medicare beneficiaries with heart failure. Am Heart J. 2012;163:987–993 e3. doi: 10.1016/j.ahj.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Teno JM, Plotzke M, Gozalo P, et al. A national study of live discharges from hospice. J Palliat Med. 2014;17:1121–1127. doi: 10.1089/jpm.2013.0595. [DOI] [PubMed] [Google Scholar]
- 19.Phillips KA, Morrison KR, Andersen R, et al. Understanding the context of healthcare utilization: Assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–596. [PMC free article] [PubMed] [Google Scholar]
- 20.Hospice Medicare Billing Codes Sheet. CGS Administrators; [Assessed January 1, 2015]. (online) Available at http://www.cgsmedicare.com/hhh/education/materials/pdf/hospice_medicare_billing_codes_sheet.pdf. [Google Scholar]
- 21.Iwashyna TJ, Chang VW, Zhang JX, et al. The lack of effect of market structure on hospice use. Health Serv Res. 2002;37:1531–1551. doi: 10.1111/1475-6773.10562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wennberg JE, Copper MM, editors. The Dartmouth Atlas of Health Care. Chicago: American Hospital Publishing; 1998. [PubMed] [Google Scholar]
- 23.McLaughlin CG, Normolle DP, Wolfe RA, et al. Small-area variation in hospital discharge rates. Do socioeconomic variables matter? Med Care. 1989;27:507–521. doi: 10.1097/00005650-198905000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Zwanziger J, Melnick GA, Mann JM. Measures of hospital market structure: A review of the alternatives and a proposed approach. Socioecon Plann Sci. 1990;24:81–95. doi: 10.1016/0038-0121(90)90014-x. [DOI] [PubMed] [Google Scholar]
- 25.National Conference of State Legislatures. [Accessed September 26, 2014];Certificate of need: state health laws and programs (online) Available at http://www.ncsl.org/research/health/con-certificate-of-need-state-laws.aspx.
- 26.Center to Advance Palliative Care. [Accessed September 23, 2014];A state-by-state report card on access to palliative care in our nation’s hospitals. (online). Available at http://www.capc.org/reportcard/findings.
- 27.Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 28.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boockvar K, Fishman E, Kyriacou CK, et al. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med. 2004;164:545–550. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- 30.Gozalo P, Teno JM, Mitchell SL, et al. End-of-life transitions among nursing home residents with cognitive issues. N Engl J Med. 2011;365:1212–1221. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Hospice and Palliative Care Organization. [Assessed February 16, 2015];Managing hospice respite care. (online). Available at http://www.nhpco.org/sites/default/files/public/regulatory/Respite_Tip_sheet.pdf.
- 32.National Hospice and Palliative Care Organization. [Assessed February 16, 2015];Managing general inpatient care for symptom management. (online) Available at http://www.nhpco.org/sites/default/files/public/regulatory/GIP_Tip_GIP_Sheet.pdf.
- 33.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: A systematic review. Palliat Med. 2014;28:1000–1025. doi: 10.1177/0269216314526272. [DOI] [PubMed] [Google Scholar]
- 34.Evans WG, Cutson TM, Steinhauser KE, et al. Is there no place like home? Caregivers recall reasons for and experience upon transfer from home hospice to inpatient facilities. J Palliat Med. 2006;9:100–110. doi: 10.1089/jpm.2006.9.100. [DOI] [PubMed] [Google Scholar]
- 35.Givens JL, Tjia J, Zhou C, et al. Racial and ethnic differences in hospice use among patients with heart failure. Arch Intern Med. 2010;170:427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carlson MD, Herrin J, Du Q, et al. Hospice characteristics and the disenrollment of patients with cancer. Health Serv Res. 2009;44:2004–2021. doi: 10.1111/j.1475-6773.2009.01002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santerre RE, Neun SP. Health Economics: Theory, Insights and Industry Studies. 4th. 2007. [Google Scholar]
- 38.Carlson MD, Bradley EH, Du Q, et al. Geographic access to hospice in the United States. J Palliat Med. 2010;13:1331–138. doi: 10.1089/jpm.2010.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Medicare and Medicaid Services. [Assessed February 17, 2015];Hospice Quality Reporting. (online). Available at http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Hospice-Quality-Reporting/index.html.
- 40.Centers for Medicare and Medicaid Services. [Accessed July 5, 2015];Transition of Care Summary. Available at http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/8_Transition_of_Care_Summary.pdf.
- 41.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences? A Study of the US Medicare Population. Med Care. 2007;45:386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teno JM, Mitchell SL, Kuo SK, et al. Decision-making and outcomes of feeding tube insertion: A five-state study. J Am Geriatr Soc. 2011;59:881–886. doi: 10.1111/j.1532-5415.2011.03385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Armour S. Wall Street Journal (Online) New York, N.Y: Jul 20, 2015. [Accessed July 21, 2015]. Medicare Expanding Access to Hospice Care. Available at http://www.wsj.com/articles/medicare-expanding-access-to-hospice-care-1437404431. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.