Abstract
Changing demographics mean that many patients with soft tissue rheumatism, osteoarthritis, inflammatory arthritis, large joint prostheses, and age-related co-morbidities are seeking to work beyond the traditional retirement age. In this chapter we review the evidence on musculoskeletal health and work at older ages. We conclude that musculoskeletal problems are common in older workers and have a substantial impact on their work capacity. Factors that influence their job retention are described, together with approaches that may extend working life. Many gaps in evidence were found, notably on the health risks and benefits of continued work in affected patients and on which interventions work best. The roles of physicians and managers are also considered.
Keywords: older worker, musculoskeletal disorder, job loss, sickness absence
Introduction
In Europe, the proportion of people aged >65 years is expected by 2050 to represent 30% of the population; worldwide, the support ratio (of adults of working age to those aged >65 and <15) is projected to be only one-third of that in 1950 [1]. Therefore, in most countries, an economic imperative exists to encourage people to remain in productive work to older ages. Governments have responded by developing policies to encourage labour force participation in later life by, for example, delaying the age at which people can draw state pension benefits, abolishing the ‘default’ retirement age, and legislating against workplace age and disability discrimination.
The delayed availability of pension benefits as well as improved population health has led to many older individuals recognising the financial need and opportunity to remain in the workforce longer. A steady rise in those working beyond traditional retirement age has been observed [2, 3].
This changing age profile in employment brings with it potential pros and cons. It is feasible that work at older ages can benefit health [4]; on the other hand, it may be challenging for those with serious health limitations. In this chapter we consider the relation between work and health at older ages, focussing particularly on musculoskeletal health, and a number of associated questions:
How feasible is work, for those with chronic musculoskeletal disorders (MSDs)?
Is work beneficial for people with chronic MSDs?
How limited in employment are affected patients? How often does poor musculoskeletal health prevent their working?
What interventions can increase work productivity in people with chronic MSDs?
What are the predictors of work disability due to MSDs?
Where affected individuals wish to work for longer, or feel they need to, what can be done to support them?
What role can health care professionals and managers play in extending gainful employment?
We first review the pattern of musculoskeletal complaints in later middle age; then consider what is known about their impact on employment; finally we review potential interventions, including what clinicians can do to support older workers with MSDs. Gaps in research are highlighted.
To inform the review, searches were performed in Medline and Google Scholar, as well as a hand search of recent volumes of two journals of occupational medicine and three journals of rheumatology (details available on request).
The relation of musculoskeletal symptoms and pathology to age
Regional pain
Musculoskeletal symptoms are common in older middle life. In a survey of adults aged ≥50 years from North Staffordshire [5], back pain in the previous four weeks affected about 1 in 3 people aged 50-59 years. Similar proportions reported knee or shoulder pain, while a fifth to a quarter reported pains in the hip, neck, distal upper limbs or feet. Almost two-thirds of those affected experienced moderate to extreme interference with their work and household duties.
Age is a major risk factor for prevalent regional pain. Thus, in a random sample of the Dutch population [6], pain affecting the elbow, hip, or foot, was about 1.5 times more common in people aged 45-64 years than in those aged 25-44; in the Quebec Health Survey [7], odds of upper extremity pain causing frequent disturbance in work activity were raised by 1.7-3.4-fold in those aged ≥50 vs. 18-24 years; in a survey of over 4,000 adults from 16 British general practices [8], pain lasting for ≥3 months and ‘highly disabling or severely limiting’ affected 10% of 55-64 year-old but was rare in young adults; and in a sample drawn from 40 British general practices, sciatica was 5-8 times more common in people age 55-65 than in those aged 16-24 [9].
For uncomplicated LBP the trend with age is somewhat flatter and less consistent. Many studies have found a moderate age-related rise, peaking and flattening off in the second half of working life; but some have found little relation. In a review of 22 such investigations [10], <50% had reported a positive association. However, even in LBP, there is a general if moderate tendency for disabling effects to become commoner at older ages. In the CUPID study [11], comprising >12,000 workers across 47 occupational groups from 18 countries, disabling LBP was 55% more prevalent at 50-59 than at 20-29 years; and in a British population survey [12], the 12-month prevalence of troublesome LBP was roughly doubled in a similar age comparison.
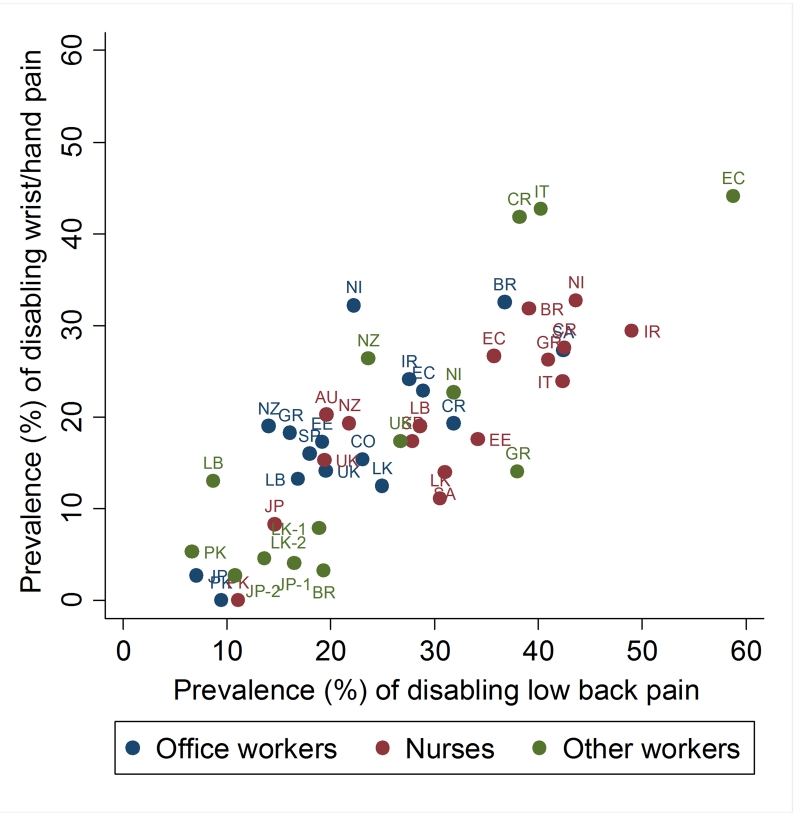
The prevalence of disabling pain varies markedly by country and setting, even among workers doing jobs with similar physical exposures. Figure 1 illustrates the variation, for example, in 1-month prevalence of disabling LBP and wrist/hand pain among 40-59 year-olds from the occupations and countries of the CUPID study [11]. Such variation indicates that report of disability depends importantly on factors other than the work environment (see also Chapter 3).
Figure 1. The one-month prevalence of disabling low back and wrist/hand pain by occupational group and country in workers aged 40-59 years from the CUPD study (adapted from ref 11).
Brazil = BR, Ecuador = EC, Colombia = CO, Costa Rica = CR, Nicaragua = NI, United Kingdom = UK, Spain = SP, Italy = IT, Greece = GR, Estonia = EE, Lebanon = LB, Iran = IR, Pakistan = PK, Sri Lanka = LK, Japan = JP, South Africa = SA, Australia = AU, New Zealand = NZ
Women are more likely than men to report pain which they attribute to work, for reasons that have been much debated [13]. The impact of this on work capacity may be growing, since more women work nowadays and most of this growth has been seen in women >50 years of age.
Osteoarthritis
Symptomatic knee osteoarthritis (OA) affects ~2.5-7% of adults aged 45-59 years and ~7-15% of 60-69 year-olds worldwide [14]. In the UK, the prevalence of knee pain in the over-40s is ~20-28% [15], and half of cases have radiographic OA. Cartilage injury, a strong risk factor for knee OA, is fairly common at a population level [16], while asymptomatic defects in knee cartilage are highly prevalent in middle age [17].
In a probability sample of the US population, radiographic hip OA was confirmed in 2% of adults aged 55-59, 2.7% of those aged 60-64, and 3.4% of those aged 65-69 [18]. Doctor-diagnosed OA was ~20 times higher in 55-64 year-olds than in those aged 25-34 [19].
Large joint OA is a major cause of disability, a growing proportion of which is borne by people who regard themselves still of working age. Thus, during 2010-2011, 92,000 primary knee joint replacements and 5,800 revisions were performed in England and Wales (up over four years by 41% and 77%): one-third of replacements occurred in patients aged <65 years [20]; in Finland, 45% of implants are received by patients <65 years [21]; and in Denmark, 51% of hip replacements in 2010 took place before age 70 [22].
Rheumatoid arthritis
Rheumatoid arthritis (RA) is far less common than OA, but its prevalence rises steeply with age. In HANES-I, doctor-diagnosed disease was 11 times higher in 55-64 year-olds than in 25-34 year-olds [19], while the incidence in the British Norfolk Arthritis Register was six times higher in this age group than in 15-24 year-olds [23]).
Ankylosing spondylitis
Ankylosing spondylitis (AS) is usually thought of as a young person’s disease, but diagnosis is often delayed and symptoms tend to persist into later life. Thus, with suboptimal disease control, vocational handicap becomes commoner with age.
Osteoporosis
This disease has rarely been studied in the occupational setting, in token of which our search for this review found no relevant hits on risks of osteoporotic fracture in older workers from manual occupations. Nonetheless, the overall 10-year risk of fracture from age 50 is in the order of 7-10%, reflecting the growing propensity to low trauma osteoporotic fractures at older ages [24].
The impact of musculoskeletal disorders on work participation at older ages
In this review, health-related ‘work participation’ encompasses various employment-related outcomes, ranging from usual paid work at one extreme to health-related job loss at the other. This last event may take the form of early retirement on health grounds or, in some countries, entitlement to a state-funded disability pension; in-between the extremes, patients may remain at work with amended or restricted duties, or diminished productivity (sometimes called ‘presenteeism’); or they may be employed but on sick leave; or they may have lost a job and be unemployed but not yet retired.
Rates of these outcomes fluctuate considerably by time and place. Thus, during 1971-2005, rates of new disability pensioning for MSDs increased >12-fold in similarly-aged Swedish women [25]. Across 10 European countries a large variation exists in the proportion of 50-64 year-olds in paid employment [26]; among those with self-perceived poor health, odds of health-related retirement were elevated everywhere, but by >4-fold in Sweden and Denmark and far less in France and the Netherlands. In the National Health Service, rates of ill-health retirement have varied >10-fold between employing organisations [27].
Non-medical factors contribute to this variation. Local employment conditions, rules of entitlement and support systems, individuals’ behaviour and preferences all play a role. Thus, higher rates of disability pensioning exist among women living alone, or socially isolated, or with limited savings [25]; ill-health retirement rates peak at times that coincide with enhanced pension entitlements [27,28].
Consistently across a large literature, however, age and musculoskeletal health are significant determinants.
As might be expected, long-term work disability strongly relates to age. Thus, for example, all-cause incidence of work disability in Norway rose 4.6-fold over follow-up in those aged 60-62 versus 20-22 years at baseline [29]; in a Danish national registry, risk of transition from work to disability pension was 2.5 times higher at 50-59 than at 20-29 [30]; and in a Dutch cohort, disability pensioning after a decade was ~8-fold higher in 55-64 year-olds than in those initially aged 18-34 [31].
Soft tissue rheumatism and osteoarthritis
Musculoskeletal complaints commonly underlie reduced work participation. In one systematic review [32], 25 studies were found on MSDs and disability pensioning, encompassing 58,000 workers. The pooled relative risk (RR) for disability pensioning was elevated 2.23-fold in those with MSDs. Among included studies, risks of pensioning were more than doubled in nursing aids with inflammatory disease or frequent LBP [33], increased 2-3-fold in Danish municipal workers affected by MSDs of hips and knees [34], and ~3 times more likely in Finnish civil servants [35] relative to other workers. When 24,000 twins from Finland were followed over three decades, disability pensioning due to any MSD occurred in 7.6% of the sample, a third of this ascribed to OA [36]. In Greek nurses, absenteeism attributed to knee pain was ~12 times commoner after ≥45 than at ≤30 years [37].
Associations with job loss appear to be general to impaired musculoskeletal health, rather than specific to anatomical site or pathology. Thus, disability pensioning has been linked with pain in the low-back, hips and knees, as described above [33, 34], but also after other patterns of regional pain and with arthritis. In 3,318 Danish employees followed over two years, long-term sick leave, disability retirement, and early retirement pensioning were related to neck or shoulder pain at baseline (RRs ~1.6-1.9) [38]; in the Kuopio Ischemic Heart Disease Risk Factor Study, odds of disability retirement were increased for those at baseline with a back problem, OA, RA, or a history of serious previous injury [39] (Table 1). In the British NorStOP study, 25% of employed patients consulting a family doctor with OA had left the workplace six years later [40]; in the five European countries National Health and Wellness Survey, among a sample of mainly middle-aged interviewees, OA was frequently linked with unemployment, absenteeism and presenteeism [41]; while in the Australian ‘45 and Up’ study, treatment for OA in the previous month carried a two-fold higher risk of ill-health retirement [42].
Table 1. Age-adjusted associations of prevalent disease with incidence of disability retirement in the Kuopio Ischemic Heart Disease Risk Factor Study (adapted from Krause et al [39]).
| Variable | Odds Ratio | 95% CI |
|---|---|---|
| Serious injury in the past | 2.73 | 1.45-5.15 |
| Osteoarthritis | 2.19 | 1.24-3.86 |
| Rheumatoid arthritis | 1.51 | 0.56-4.03 |
| Back problems | 1.60 | 0.97-2.67 |
Associations have also been found with a physician’s diagnosis of MSD [43] and with frequently taken analgesia. Thus, in the Finnish twins study, those taking analgesic drugs on >10 days/year were twice as like to receive a MSD-ascribed disability pension during the subsequent three decades [36].
Sick leave is a strong predictor of future disability pensioning. In a French cohort of 20,434 utility workers, sick leave of >7 days for a MSD in 1990-2 carried a >3-4.6-fold higher risk of disability pensioning over a 13-year follow-up [44]; in a population sample of 176,600 Swedes, those with sick leave of >7 days for a MSD in 1985 were 5.7 times more likely than those without to take a MSD-related disability pension in 1991-6 [45].
Whilst the association between musculoskeletal ill-health and job loss is rather non-specific, more severe or extensive symptoms appear consistently to carry a higher risk of poor employment outcome. For example, in a Norwegian study, the odds of disability pensioning over 14 years rose monotonically with number of painful anatomical sites in the year before baseline, being ~4-fold higher in those with 9 or 10 painful sites [46]; in another population survey from Norway, long-term disability was 3.5 times more likely in those with generalised pain in the week before baseline than in those with localised LBP [47]; and among Finnish workers attending occupational health services with upper limb pain, >50% reported reduced productivity at work [48], the main risk factors among older employees being high pain intensity and pain-related sleep disturbance (OR 6.0 in the top tertile), rather than diagnosis.
Inflammatory arthritis
In general, RA is a more disabling condition than OA or soft tissue rheumatism, and has a more profound impact on employment. Disability begins early, rises linearly with time and, within 10 years of disease onset, >50% of patients fail to maintain a full-time job [14]. In a large cohort with RA, only 10% remained in employment 30 years after disease onset [49]. Job retention rates were lower in occupations with high physical demands than when work was flexible and self-paced. Similarly, when economically active patients with RA from the Norfolk Arthritis Register were followed for ~8.6 years, one-third had stopped work for health reasons at a rate 32 times greater than a matched control group [50].
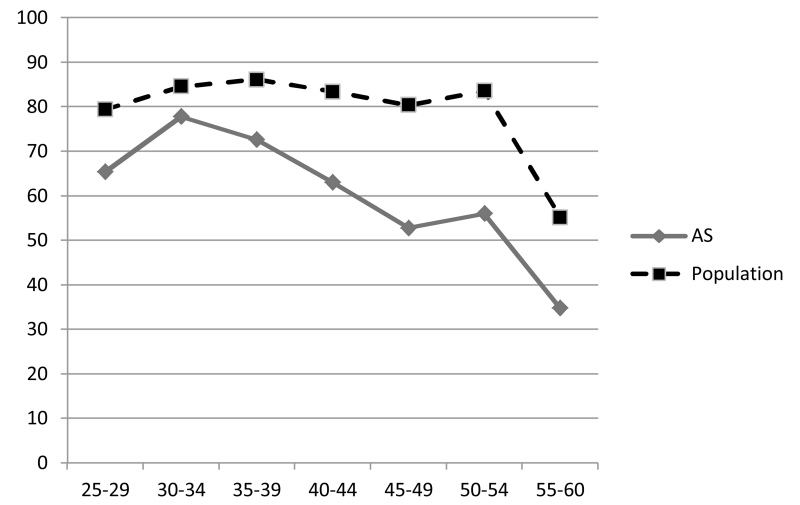
In outpatients with AS, psoriatic arthropathy, and SLE, enrolled into a national German database, those aged 50-70 years had disability pension rates of 28%, 32% and 61% respectively, versus 37% for patients with RA [51]. The costs ascribed by the human capital approach to lost work productivity were estimated at 82%, 87% and 145% of those for similarly aged outpatients with RA. Although comparison between diseases of differing age at onset is not straight-forward, these findings suggest that inflammatory arthropathies of various kinds can have a substantial career-limiting impact on patients’ ability to work. Further evidence on this comes from Dutch employment data on patients with AS (Figure 2) [52]. Among those initially in work, the age- sex-adjusted withdrawal rate over follow-up was three times that in the general population, notably in men with a manual job (elevated 5.2-fold), although still doubled in white-collar occupations [53].
Figure 2. Proportion (%) of men in the Dutch population in full-time employment, by age and health status: men with ankylosing spondylitis vs. all men (adapted from Boonen et al [53]).
Comorbidities
Workers with MSDs may cope less well if they have concurrent medical problems which otherwise might be compatible with working. In evidence of this, one report found that among patients with arthritis, those who were also clinically depressed were significantly more likely to become work-disabled [54]. Treatment of depression in people with OA lessens their pain intensity and the interference with daily activities of their arthritis [55], and so perhaps benefits their work participation.
The modifying effect of work activity
Manual employment is clearly associated with risk of disability pension from a MSD. Thus, among 3,674 people in the nationally representative Health Survey 2000 in Finland, disability retirement attributed to MSDs was ~3-6 times higher in manual as compared with non-manual occupations [56]. Adjustment for physical working conditions attenuated the socioeconomic gradient by almost two-thirds, indicating that these drive much of the relationship.
The authors further explored social differences using longitudinal data on a 10% sample of the Finnish workforce, followed during 1997-2010. Among 55-64 year-olds, disability retirement rates for back disorders were elevated 4.4-6.5-fold in manual vs. upper class non-manual workers, 5.0-6.6-fold for arthrosis, and 4.8-6.7-fold for all MSDs combined. MSDs accounted for 54-76% of the excess in disability retirement by work status [57].
Other studies have reached similar conclusions. In one investigation of socioeconomic inequalities in middle-aged men from Malmo, incidence of disability pensioning from MSDs was 3.5-fold higher in blue-collar than in ‘higher level’ white-collar workers [58]. In a study of 16,000 Finnish twins, work mainly involving lifting and carrying, or described as physically heavy, doubled the long-term risk of a MSD-related disability pension [59]; in the Kuopio Ischemic Heart Disease Risk Factor Study, odds of disability retirement were elevated by a high level of back, neck, or overall musculoskeletal strain in employment at baseline, and with very heavy or repetitive work, and work involving a lot of crouching or postural discomfort (Table 2) [39]; MSD-related disability pensioning was ~3-4 times commoner where work involved frequent lifting, regular loading of muscles, working in an uncomfortable position, or a heavy physical workload.
Table 2. Associations of physical working conditions with incidence of disability retirement in men from the Kuopio Ischemic Heart Disease Risk Factor Study (adapted from Krause et al [39]).
| Variable | Odds Ratio | 95% CI |
|---|---|---|
| Physical Work | ||
| Light | 1.00 | - |
| Moderately active | 2.14 | 1.09-4.20 |
| Heavy or very heavy | 3.27 | 1.61-6.63 |
| Work in uncomfortable position | ||
| Very little | 1.00 | - |
| Some | 2.12 | 1.03-4.34 |
| Much | 2.64 | 1.38-5.06 |
| Crouching | ||
| None | 1.00 | - |
| Some | 1.78 | 0.94-3.34 |
| Much | 2.45 | 1.08-5.52 |
| Musculoskeletal strain index | ||
| First quartile | 1.00 | - |
| Second quartile | 1.81 | 0.77-4.27 |
| Third quartile | 2.00 | 0.83-4.82 |
| Fourth quartile | 2.96 | 1.29-6.78 |
| Repetitive strain Index | ||
| First tertile | 1.00 | - |
| Second tertile | 1.43 | 0.71-2.87 |
| Third tertile | 2.08 | 1.17-3.70 |
| Back strain | ||
| Little | 1.00 | - |
| Moderate | 1.53 | 0.66-3.53 |
| Much | 2.49 | 1.22-5.07 |
| Neck strain | ||
| Little | 1.00 | - |
| Moderate | 1.08 | 0.47-2.48 |
| Much | 1.86 | 0.95-3.62 |
Risk estimates (which are not mutually adjusted) were adjusted for age in four bands
Long-term studies in blue-collar industries have characterised the scale of the problem. For example, Jarvholm et al [60] studied disability pension rates among ~325,000 Swedish construction workers followed for 28 years. One in 5 of the workforce received a disability pension (Table 3). Rock workers fared worse, with rates ~4-times greater than non-manual employees and twice that of electricians. Other occupations at high risk of pensioning included concrete workers, insulators, brick layers, roofers, painters and floor layers. It was estimated that blue-collar workers lost 2.25 years of working life on average; ~70-80% of the loss was in workers aged ≥50 at pensioning 45-60% of all disability pensions at this age were MSD-related.
Table 3. Relative risks of disability pension before age 65 in the construction industry (adapted from Järvholm et al [60]).
| Occupation | RR | 95% CI | DP (%) |
|---|---|---|---|
| Rock workers | 2.16 | 1.96-2.39 | 37.4 |
| Concrete workers | 1.94 | 1.81-2.09 | 29.8 |
| Insulators | 1.90 | 1.69-2.14 | 21.2 |
| Roofers | 1.88 | 1.62-2.17 | 24.1 |
| Painters | 1.88 | 1.75-2.03 | 20.1 |
| Brick-layers | 1.77 | 1.63-1.93 | 25.3 |
| Earth-moving workers | 1.75 | 1.61-1.90 | 24.5 |
| Crane operators | 1.71 | 1.55-1.88 | 33.6 |
| Floor-layers | 1.71 | 1.55-1.89 | 18.9 |
| Woodworkers | 1.53 | 1.43-1.63 | 17.6 |
| Sheet-metal workers | 1.50 | 1.38-1.64 | 15.6 |
| Plumbers and pipe fitters | 1.41 | 1.30-1.52 | 19.7 |
| Electricians | 1.00 | - | 10.2 |
| Foremen | 0.65 | 0.60-0.70 | 12.7 |
| Salaried employees | 0.54 | 0.48-0.59 | 10.8 |
| All occupations | (18.5) |
% DP – Proportion receiving a disability pension between 1980-2008
Is work at older ages good for musculoskeletal health?
Work at older ages may carry physical benefits, such as maintained muscle strength and mobility; and psychological benefits, such as sustained motivation and sense of purpose, social engagement and mental activity [4]. On the other hand, older workers may struggle with the demands of work [4], while planned normal retirement can carry benefits of its own [61, 62]. A trade-off exists therefore between opposing influences on health. Where does the balance lie?
An influential best evidence synthesis [63] for the British Department for Work and Pensions has concluded that work is ‘generally good’ for health. Using a ‘review of reviews’ methodology, the authors interrogated >10 electronic databases and search engines, abstracting materials from many peer-reviewed and grey literature reports. Findings leant heavily on ‘well referenced and structured’ narrative reviews in lieu of the few available systematic reviews and meta-analyses; quality criteria were loosely specified and findings were assessed qualitatively and were not combined to compute meta-estimates of effect.
Much of the evidence came from studies of workers with common musculoskeletal complaints. As such, its conclusion might appear to be at odds with the evidence presented above on MSDs as a cause of early retirement. However, the evidence base was considerably slimmer at older ages (eight narrative reviews, one research summary, one official inquiry on health inequalities, and 13 original studies), and none of it had musculoskeletal health as an exposure or outcome of interest. More generally, it was concluded that older workers vary in their work capability, that they do not necessarily take more sick leave than younger workers, and that early retirement can have positive or negative effects on health depending on context; however, no evidence was adduced regarding patients with large joint disease, or inflammatory arthropathy, or in those whose jobs were physically demanding.
It should be stressed that, while MSDs are consistent risk factors for impaired work participation, most affected individuals can and still do work successfully. A review of patients with OA, although finding “a mild negative effect” on work participation, concluded that “many patients …managed to stay in work despite limitations” [64]; among 8,781 51-61 year-olds from the US Health and Retirement Survey, 63% reported ≥1 musculoskeletal conditions: most were still at work, 1 in 7 of whom (a national estimate of 1.32 million citizens) worked despite a disability [65].
However, participation in work may not mean that work is ‘good’ for those with MSDs. One reason to draw a more guarded conclusion is that many occupational activities are recognised to cause development and progression of musculoskeletal disease – e.g. frequent kneeling, squatting, climbing, and heavy lifting probably play a role in OA knee [66]; occupational kneeling and squatting carry a higher risk of meniscal injury [16]; heavy lifting is a risk factor for hip OA (see Chapter 8); and lifting and frequent bending or twisting have consistently been associated with LBP [10]. A further concern for patients who receive a large joint arthroplasty and remain in physically demanding occupations is that joint loading could contribute to a greater risk of joint failure, through wear and tear and aseptic loosening. A third consideration is that physical work may be more painful to perform and may aggravate affected workers’ symptoms.
Evidence of harm (or benefit) in these circumstances is wanting. Thus, a systematic review [67] found plentiful data on return-to-work times following knee surgery, but almost nothing on how the nature of work affects long-term clinical outcomes such as knee pain, quality of life, knee function, and need for joint revision. Instead, a few reports described the general advice that surgeons offer patients: most recommended avoiding intense or high-impact activities post-surgery. In one small case series a greater risk of polyethylene failure was reported in individuals who were more active, based on their occupation or retirement status [68], but in another small study of knee revisions, no relation was found to physical activity at work and leisure following surgery [69]. The optimum long-term advice for patients with knee surgery wishing to resume their previous work is therefore moot. The knowledge gap is timely to fill, given the growing number of patients with large joint replacements who are still working, or seeking work.
More generally, further research is needed on the health risks and benefits of continued employment in older patients with MSDs and their determinants, to ensure personal advice is evidence-based and that measures to support and protect them are optimised.
Promoting work participation in older people with musculoskeletal disorders
In reporting higher rates of work disability and job loss in manual workers with MSDs, some authors have called for improved working conditions, to combat socioeconomic differentials [56]. Others have exhorted doctors to increase their efforts to treat or prevent underlying health problems [70]. Such calls assume a predominantly biomedical relationship between working with a MSD and employment: physical stressors aggravate or cause injured and diseased tissues, which in turn render work uncomfortable and ultimately untenable. However, much evidence indicates that non-medical factors matter greatly too.
Reference has been made to large variations in rates of MSD-attributed disability, sickness absence and ill-health retirement that are not simply explained by work demands [11, 26, 27,71]; also, to associations with non-biomedical risk factors [25, 27,28] and substantial variations over time [25]. It follows that ergonomic improvements and better medical care, although relevant, are elements of a bigger picture. It may even be that leaving work is the best outcome for a particular patient. Below we consider the current evidence on interventions to improve work participation.
Soft tissue rheumatism
Interventions to reduce sickness absence and job loss from musculoskeletal causes can take many forms, and may be directed at the individual, or at their workplace and employer, their access to services, or at the medical teams sharing their care.
In 2012, one of us undertook a systematic review of interventions to improve work participation in those with MSDs [67]. No trial was specific to older workers. In all, 42 studies were identified, including 34 randomised controlled trials (RCTs), embracing, for example, exercise therapy, work hardening, physical therapy, psychological therapy, behavioural therapy, improved education, rehearsal of work techniques, use of lumbar supports, ‘participatory’ ergonomics (to control workplace risks and adapt the physical environment), lighter duties, reduced hours, training of managers and doctors, extra support services and case managers. Studies were typically small and of limited quality. No intervention was clearly superior to alternatives. Most interventions appeared beneficial although effect sizes were generally small, and there was evidence of publication bias, suggesting that benefits may have been over-stated. The cost-effectiveness of interventions was not established.
If this appraisal of the evidence appears disheartening, it may be added that the trials mostly involved patients with soft tissue rheumatism, perhaps at the milder end of the disease spectrum. Sickness absence in these circumstances may be socially and behaviourally patterned – it has been shown, for example, that rates of MSD-related sickness absence vary ~ 30-fold internationally between workers doing essentially the same jobs [71] (see also Chapter 3). Also, since this review, an approach based on risk stratification (targeting interventions at those who may most benefit) has shown some promise [72].
A few observational studies also suggest that health-related job loss is not inevitable, even in industries with high demands. In a cohort of roofers aged 40-59 years, ~8% of those with musculoskeletal problems left work on health grounds over the following year [73]. However, individuals fell into three camps: men who had requested and received a job accommodation (e.g. altered work schedule, modified job tasks, lighter duties, changed equipment), men who had asked for an accommodation but had not received it, and a group who neither requested nor received it. In comparison with this last group, the odds of health-related job loss in men from the first were reduced 76%, but in those who asked and went without, they were raised >2-fold.
In a survey of Danish employees [38], firms with flexible employment practices had only half the two-year incidence of work disability from MSDs relative to traditionally organised firms.
In the Health and Retirement Survey [74], <20% of adults aged 51-61 years who reported working with a musculoskeletal disability had received an accommodation at work (e.g. someone to help them out, reduced working hours, rest periods, an altered job, special equipment). Over the following two years, 25% of this group discontinued work. Rates of job loss, were lower, however, only in individuals fortunate enough to enjoy the help of colleagues.
These data suggest that employers may be able to increase work retention in older people with MSDs if more adaptive and flexible work patterns can be offered.
Osteoarthritis
The review by Palmer et al [67] found no trials on interventions to promote work participation in patients with OA, while another review [75], on vocational rehabilitation and chronic arthritis, found the evidence to be “scanty”. However, a cross-sectional study from Johnston County [76] reported that symptomatic knee OA was significantly less common in workplaces with supportive employment policies (those allowing job switching and paid sick leave or disability benefits). This apparent benefit could arise from selection out of work of affected cases, so longitudinal research is needed to clarify interpretation.
A second study [77] found a high rate of unemployment in patients awaiting joint replacement, arthroscopy or hip resurfacing: 30% of those in work when symptoms began had quit their job because of their joint problem. Almost three-quarters had not been offered modifications to help them cope at work. Non-sedentary employment carried a greater risk of health-related job loss than work mainly involving sitting (Hazard ratio (HR) 2.7). In addition, health-related job loss was greater in those employed by a ‘micro’-firm (<10 employees, HR 1.9), presumably reflecting the limited flexibility of small employers to accommodate work sharing and alternative duties. However, the study highlights measures that in some circumstances may be job protective.
Inflammatory arthritis
A question of particular interest to physicians is whether better control of symptoms improves work participation. Intuitively, this should follow, but little has been published for example on drug treatments for OA or soft tissue rheumatism and work participation. By contrast, there is interest in, and a growing evidence base on the impact on work of disease-modifying and biologic drug treatments for inflammatory arthritis and spondylopathies.
This question is considered fully in Chapters 11 and 12. Suffice it to say that for AS, a systematic review by van der Burg et al [78] drew guardedly positive conclusions: evidence was found that biologic therapy reduced absenteeism, presenteeism, and to a lesser extent job loss, but studies were small and with methodological limitations. For RA, a second review drew similar conclusions [79]. Employment status improved in four of 13 studies, absence from work in all 10 studies, and presenteeism in seven of nine studies assessing these outcomes. A decline has been charted in RA-related work disability in Finland over the time since methotrexate and disease-modifying anti-rheumatic drugs have been widely prescribed [80]. These observations suggest that work outcomes in RA and AS may benefit from better disease control. Therefore clinicians can play a role, at least in some circumstances, in improving the work prospects of their patients.
Summary and pointers for practice.
MSDs are very common; their prevalence generally rises in older people
At older ages they have a considerable impact on patients’ employment prospects
Factors that influence job retention at this stage include the type of MSD, its severity and treatment, the presence of comorbid illness, people’s attitudes to work and retirement, and the work environment’s demands
Interventions to optimise symptom control and provide a more flexible adaptive work environment can substantially improve older people’s prospects of working
On present evidence, far more needs to done in these areas if patients are to realise this possibility
Gaps in research.
The health risks and benefits of work at older ages require further elaboration, especially in workers with major joint disease
Interventions to extend working life are under-developed and under-tested. Because the population is ageing and patients are likely to work for longer, this gap in knowledge is urgent to fill, in relation to MSDs and many other chronic diseases of ageing
Acknowledgments
Funding
This work has been undertaken under the auspices of the Arthritis UK MRC Centre for Musculoskeletal Health & Work. KTP also wishes to acknowledge core funding support from the Medical Research Council.
Footnotes
Conflict of interest
None.
Contributor Information
Professor Keith Palmer, Medical Research Council Lifecourse Epidemiology Unit, University of Southampton, Southampton General Hospital, Southampton SO16 6YD, UK; ARUK-MRC Centre for Musculoskeletal Health and Work, Tel: (023) 80777624, Fax no: (023) 80704021, ktp@mrc.soton.ac.uk.
Dr Nicola Goodson, Department of Musculoskeletal Biology 1, Institute of Aging and Chronic Diseases, University of Liverpool, University Hospital Aintree, Liverpool L9 7AL; ARUK-MRC Centre for Musculoskeletal Health and Work, Tel: (0151 529 5889), Fax no (0151) 5295888, ngoodson@liverpool.ac.uk.
References
- 1.World Health Organisation. Department of Economic and Social Affairs World Population Ageing: 1950-2050. http://www.un.org/esa/population/publications/worldageing19502050/
- 2.Office for National Statistics [accessed 234/01/15];Pension Trends. Chapter 4: The Labour Market and Retirement, 2013 Edition. http://www.ons.gov.uk/ons/dcp171766_297899.pdf.
- 3.The Times [accessed 23/01/15];Number of over-65s in work tops 1m for first time. 2013 Jun 12th; http://www.thetimes.co.uk/tto/business/economics/article3789087.ece.
- 4.Wegman DH. Older workers. Occupational Medicine: State of the Art Reviews. 1999;14:537–57. 102:79-88. [PubMed] [Google Scholar]
- 5.Thomas E, Peat G, Harris L, et al. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110:361–8. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Picavet HSJ, Schouten JSAG. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC3-study. Pain. 2003;102:167–78. doi: 10.1016/s0304-3959(02)00372-x. [DOI] [PubMed] [Google Scholar]
- 7.Leroux I, Dionne CE, Bourbonnais R, et al. Prevalence of musculoskeletal pain and associated factors in the Quebec working population. Int Arch Occup Environ Health. 2005;78:379–86. doi: 10.1007/s00420-004-0578-2. [DOI] [PubMed] [Google Scholar]
- 8.Parsons S, Breen A, Foster NE, et al. Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Fam Pract. 2007;24:308–16. doi: 10.1093/fampra/cmm027. [DOI] [PubMed] [Google Scholar]
- 9.Palmer KT, Griffin MJ, Syddall HE, et al. The relative importance of whole-body vibration and occupational lifting as risk factors for low-back pain. Occup Environ Med. 2003;60:715–21. doi: 10.1136/oem.60.10.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burdorf A, Sorock G. Positive and negative evidence of risk factors for back disorders. Scand J Work Environ Health. 1997;23:243–56. doi: 10.5271/sjweh.217. [DOI] [PubMed] [Google Scholar]
- 11.Coggon D, Ntani G, Palmer KT, et al. the CUPID Collaboration Disabling musculoskeletal pain in working populations: Is it the job, the person, or the culture? Pain. 2013;154:856–63. doi: 10.1016/j.pain.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walsh K, Cruddas M, Coggon D. Low back pain in eight areas of Britain. J Epidemiol & Comm Health. 1992;46:227–30. doi: 10.1136/jech.46.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heilskov-Hansen T. Physical work exposure and sex differences in work-related musculoskeletal disorders. Faculty of Health and Medical Sciences, University of Copenhagen; 2014. PhD thesis. [Google Scholar]
- 14.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bulletin of the World Health Organisation. 2003;81:646–56. [PMC free article] [PubMed] [Google Scholar]
- 15.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker P, Reading I, Cooper C, et al. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60:794–7. doi: 10.1136/oem.60.10.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cicuttini F, Ding C, Wluka A, et al. Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults. A prospective study. Arth Rheum. 2005;52:2033–9. doi: 10.1002/art.21148. [DOI] [PubMed] [Google Scholar]
- 18.Tepper S, Hochberg MC. Factors associated with hip osteoarthritis: Data from the first National Health and Nutrition Examination Survey (NHANES-1) Am J Epidemiol. 1993;137:1081–8. doi: 10.1093/oxfordjournals.aje.a116611. [DOI] [PubMed] [Google Scholar]
- 19.Cuningham LS, Kelsey JL. Epidemiology of musculoskeletal impairments and associated disability. Am J Public Health. 1984;74:574–9. doi: 10.2105/ajph.74.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Joint Registry for England and Wales 8th Annual Report. 2011 http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/NJR%208th%20Annual%20Report%202011.pdf.
- 21.Paavolainen P, Hamalainen M, Mustonen H, et al. Registration of arthroplasties in Finland. A nationwide prospective project. Acta Orthop Scand Suppl. 1991;241:27–30. doi: 10.3109/17453679109155101. [DOI] [PubMed] [Google Scholar]
- 22.Overgaard S. Dansk Hoftealloplastik Register. Årsrapport 2011 [Danish Hip Arthroplasty Register. Annual report 2011] Dansk Hoftealloplastik Register [Danish Hip Arthroplasty Register]; Odense: [PubMed] [Google Scholar]
- 23.Symmons DPM, Barrett EM, Bankhead CR, et al. The incidence of rheumatoid arthritis in the United Kingdom: results from the Norfolk Arthritis Register. B J Rheumatol. 1994;33:735–739. doi: 10.1093/rheumatology/33.8.735. [DOI] [PubMed] [Google Scholar]
- 24.van Staa TP, Dennison EM, Leufkens HG, et al. Epidemiology of fractures in England and Wales. Bone. 2001;29:517–22. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]
- 25.Gustafsson K, Aronsson G, Marklund S, et al. Social integration, socioeconomic conditions and type of ill health preceding disability pension in young women: a Swedish population-based study. Int J Behav Med. 2014;21:77–87. doi: 10.1007/s12529-012-9287-5. [DOI] [PubMed] [Google Scholar]
- 26.Alavinia SM, Burdorf A. Unemployment and retirement and ill-health: a cross-sectional analysis across European countries. Int Arch Occup & Environ Health. 2008;82:39–45. doi: 10.1007/s00420-008-0304-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poole CJ. Retirement on grounds of ill health: cross sectional survey in six organisations in United Kingdom. BMJ. 1997;314:929–32. doi: 10.1136/bmj.314.7085.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gleeson D, Gallagher J. Ill health retirement among healthcare workers in the Southern Health Board of the Republic of Ireland. Occup Med. 2005;55:364–8. doi: 10.1093/occmed/kqi098. [DOI] [PubMed] [Google Scholar]
- 29.Eriksen W, Natvig B, Bruusgaard D. Sleep problems: a predictor of long-term work disability? A four-year prospective study. Scand J Public Health. 2001;29:23–31. [PubMed] [Google Scholar]
- 30.Pedersen J, Bjorner JB, Burr H, et al. Transitions between sickness absence, work, unemployment, and disability in Denmark 2004-2008. Scand J Work Environ Health. 2012;38:516–26. doi: 10.5271/sjweh.3293. [DOI] [PubMed] [Google Scholar]
- 31.Schuring M, Robroek SJW, Otten FWJ, et al. The effect of ill health and socioeconomic status on labor force exit and re-employment: a prospective study with ten years follow-up in the Netherlands. Scand J Work Environ Health. 2013;39:134–43. doi: 10.5271/sjweh.3321. [DOI] [PubMed] [Google Scholar]
- 32.Van Rijn RM, Robroek SJW, Brouwer S, et al. Influence of poor health on exit from paid employment: a systematic review. Occup Environ Med. 2014;71:295–301. doi: 10.1136/oemed-2013-101591. [DOI] [PubMed] [Google Scholar]
- 33.Jensen LD, Ryom PK, Christensen MV, et al. Differences in risk factors for voluntary early retirement and disability pension: a 15-year follow-up in a cohort of nurses’ aides. BMJ Open. 2012;2:e000991. doi: 10.1136/bmjopen-2012-000991. doi:10.11.36/bmjopen-2012-000991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lund T, Iversen L, Poulsen KB. Work environment factors, health, lifestyle and marital status as predictors of job change and early retirement in physically heavy occupations. Am J Ind Med. 2001;40:161–9. doi: 10.1002/ajim.1084. [DOI] [PubMed] [Google Scholar]
- 35.Kuoppala J, Lamminpää A, Väänänen-Tomppo I, et al. Employee well-being and sick leave, occupational accident, and disability pension. JOEM. 2011;53:633–40. doi: 10.1097/JOM.0b013e31821aa48c. [DOI] [PubMed] [Google Scholar]
- 36.Ropponen A, Narusyte J, Alexanderson K, et al. Stability and change in health behaviours as predictors for disability pension: a prospective cohort study of Swedish twins. BMC Public Health. 2011;11:678–88. doi: 10.1186/1471-2458-11-678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alexopoulos EC, Tanagra D, Detorakis I, et al. Knee and low back complaints in professional hospital nurses: Occurrence, chronicity, care seeking and absenteeism. Work. 2011;38:329–35. doi: 10.3233/WOR-2011-1136. [DOI] [PubMed] [Google Scholar]
- 38.Lund T, Csonka A. Risk factors in health, work environment, smoking status, and organizational context for work disability. Am J Ind Med. 2003;44:492–501. doi: 10.1002/ajim.10298. [DOI] [PubMed] [Google Scholar]
- 39.Krause N, Lynch J, Kaplan GA, et al. Predictors of disability retirement. Scand J Work Environ Health. 1997;23:403–13. doi: 10.5271/sjweh.262. [DOI] [PubMed] [Google Scholar]
- 40.Wilkie R, Pransky G. Improving work participation for adults with musculoskeletal conditions. Best Practice & Research in Clinical Rheumatology. 2012;26:733–42. doi: 10.1016/j.berh.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 41.Kingsbury SR, Gross HJ, Isherwood G, et al. Osteoarthritis in Europe: impact on health status, work productivity and use of pharmacotherapies in five European countries. Rheumatol. 2014;53:937–47. doi: 10.1093/rheumatology/ket463. [DOI] [PubMed] [Google Scholar]
- 42.Pit SW, Shrestha R, Schofield D, et al. Partial and complete retirement due to ill-health among mature age Australians. Public Health. 2013;127:561–71. doi: 10.1016/j.puhe.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 43.Laine S, Gimeno D, Virtanen M, et al. Job strain as a predictor of disability pension: the Finnish Public Sector Study. J Epidemiol Community Health. 2009;63:24–30. doi: 10.1136/jech.2007.071407. [DOI] [PubMed] [Google Scholar]
- 44.Alexanderson K, Kivimäki M, Ferrie JE, et al. Diagnosis-specific leave as a long-term predictor of disability pension: a 13-year follow-up of the GAZEL cohort study. J Epidemiol Community Health. 2012;66:155–9. doi: 10.1136/jech.2010.126789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kivimäki M, Ferrie JE, Hagberg J, et al. Diagnosis-specific sick leave as a risk marker for disability pension in a Swedish population. J Epidemiol Community Health. 2007;61:915–20. doi: 10.1136/jech.2006.055426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kamaleri Y, Natvig B, Ihlebaek CM, et al. Does the number of musculoskeletal pain sites predict work disability? Eur J Pain. 2009;13:426–30. doi: 10.1016/j.ejpain.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 47.Natvig B, Eriksen W, Bruusgaard D. Low back pain as a predictor of long-term work disability. Scand J Public Health. 2002;30:288–92. doi: 10.1080/14034940210133951. [DOI] [PubMed] [Google Scholar]
- 48.Detaille SI, Heerkens YF, Engels JA, et al. Common prognostic factors of work disability among employees with a chronic somatic disease: a systematic review of cohort studies. Scand J Work Environ Health. 2009;35:261–81. doi: 10.5271/sjweh.1337. [DOI] [PubMed] [Google Scholar]
- 49.Yelin E, Henke C, Epstein W. The work dynamics of the person with rheumatoid arthritis. Arth Rheum. 1987;30:507–512. doi: 10.1002/art.1780300504. [DOI] [PubMed] [Google Scholar]
- 50.Barrett EM, Scott DGI, Wiles NJ, et al. The impact of rheumatoid arthritis on employment status in the early years of disease: a UK community-based study. Rheumatol. 2000;39:1403–9. doi: 10.1093/rheumatology/39.12.1403. [DOI] [PubMed] [Google Scholar]
- 51.Huscher D, Merkesdal S, Thiele K, et al. for the German Collaborative Arthritis Centres Cost of illness in rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and systemic lupus erythematosus in Germany. Ann Rheum Dis. 2006;65:1175–83. doi: 10.1136/ard.2005.046367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boonen A, Chorus A, Miedema H, et al. Employment, work disability, and work days lost in patients with ankylosing spondylitis: a cross sectional study of Dutch patients. Ann Rheum Dis. 2001;60:353–8. doi: 10.1136/ard.60.4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boonen A, Chorus A, Landewe R, et al. Manual jobs increase the risk of patients with ankylosing spondylitis withdrawing from the labour force, also when adjusted for job related withdrawal in the general population. Ann Rheum Dis. 2002;61:658. doi: 10.1136/ard.61.7.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li X, Gignac MAM, Anis AH. Workplace, psychosocial factors, and depressive symptoms among working people with arthritis: a longitudinal study. J Rheumatol. 2006;33:1849–55. [PubMed] [Google Scholar]
- 55.Lin EHB, Katon W, Von Kroff M, et al. for the IMPACT investigators Effect of improving depression care on pain and functional outcomes among older adults with arthritis a randomized controlled trial. JAMA. 2003;290:2428–9. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- 56.Polvinen A, Gould R, Lahelma E, et al. Socioeconomic differences in disability retirement in Finland: the contribution of ill-health, health behaviours and working conditions. Scand J Public Health. 2013;41:470–8. doi: 10.1177/1403494813482400. [DOI] [PubMed] [Google Scholar]
- 57.Polvinen A, Laaksonen M, Gould R, et al. The contribution of major diagnostic causes to socioeconomic differences in disability retirement. Scand J Work Environ Health. 2014;40:353–60. doi: 10.5271/sjweh.3411. [DOI] [PubMed] [Google Scholar]
- 58.Månsson N-O, Råstam L, Eriksson K-F, et al. Socioeconomic inequalities and disability pension in middle-aged men. Int J Epidemiol. 1998;37:1019–25. doi: 10.1093/ije/27.6.1019. [DOI] [PubMed] [Google Scholar]
- 59.Kärkkäinen S, Pitkäniemi J, Silventoinen K, et al. Physical workload and risk of early retirement: prospective population-based study among middle-aged men. J Occup Environ Med. 2002;44:930–9. doi: 10.1097/00043764-200210000-00012. [DOI] [PubMed] [Google Scholar]
- 60.Järvholm B, Stattin M, Robroek SJW, et al. Heavy work and disability pension – a long term follow-up of Swedish construction workers. Scand J Work Environ Health. 2014;40:335–42. doi: 10.5271/sjweh.3413. [DOI] [PubMed] [Google Scholar]
- 61.Midanik LT, Soghikian K, Ransom LJ, et al. The effect of retirement on mental health and health behaviors: The Kaiser Permanente retirement study. Journal of Gerontology: Social Sciences. 1995;50:S59–S61. doi: 10.1093/geronb/50b.1.s59. [DOI] [PubMed] [Google Scholar]
- 62.Salokangas RK, Joukamaa M. Physical and mental health changes in retirement age. Psychotherapy Pschosom. 1991;55:100–7. doi: 10.1159/000288415. [DOI] [PubMed] [Google Scholar]
- 63.Waddell G, Burton AK. Is work good for your health and well-being? The Stationery Office; London: 2006. ISBN 0 11 7036943. [Google Scholar]
- 64.Bieleman HJ, Bierma-Zeinstra SMA, Oosterveld FGJ, et al. The effect of osteoarthritis of the hip or knee on work participation. J Rheumatol. 2011;38:1835–43. doi: 10.3899/jrheum.101210. [DOI] [PubMed] [Google Scholar]
- 65.Yelin EH. Musculoskeletal conditions and employment. Arthr Rheum. 1995;8:311–317. doi: 10.1002/art.1790080417. [DOI] [PubMed] [Google Scholar]
- 66.Palmer KT. Occupational activities and osteoarthritis of the knee. Brit Med Bulletin. 2012;102:147–70. doi: 10.1093/bmb/lds012. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Palmer KT, Harris EC, Linaker C, et al. Effectiveness of community- and workplace-based interventions to manage musculoskeletal-related sickness absence and job loss – a systematic review. Rheumatol. 2012;51:230–242. doi: 10.1093/rheumatology/ker086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Heck DA, Clingman JK, Kettlekamp DG. Gross polyethylene failure in total knee arthroplasty. Orthopedics. 1992;15:23–8. doi: 10.3928/0147-7447-19920101-07. [DOI] [PubMed] [Google Scholar]
- 69.Jones DL, Cauley JA, Kriska AM, et al. Physical activity and risk of revision total knee arthroplasty in individuals with knee osteoarthritis: A matched case-control study. Rheumatol. 2004;31:1384–90. [PubMed] [Google Scholar]
- 70.Pit SW, Shrestha R, Schofield D, et al. Health problems and retirement due to ill-health among Australian retirees aged 45-64 years. Health Policy. 2010;94:175–81. doi: 10.1016/j.healthpol.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 71.Coggon D, Ntani G, Vargas-Prada S, other members of the CUPID Collaboration International variation in musculoskeletal sickness absence: Findings from the CUPID study. Occup Environ Med. 2013;70:575–84. doi: 10.1136/oemed-2012-101316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Foster NE, Mullis R, Hill JC, et al. on behalf of the Team IBS Effect of stratified care for low back pain in family practice (IMPaCT Back): a prospective population-based sequential comparison. Ann Fam Med. 2014;12:102–111. doi: 10.1370/afm.1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Welch L, Haile E, Boden LI, et al. Musculoskeletal disorders among construction roofers – physical function and disability. Scand J Work Environ Health. 2009;35:56–63. doi: 10.5271/sjweh.1302. [DOI] [PubMed] [Google Scholar]
- 74.Yelin E, Sonneborn D, Trupin L. The prevalence and impact of accommodations of the employment of persons 51-61 years of age with musculoskeletal conditions. Arthritis Care Res. 2000;13:168–76. doi: 10.1002/1529-0131(200006)13:3<168::aid-anr6>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 75.Vlieland TP, de Buck PD, van den Hout WB. Vocational rehabilitation programs for individuals with chronic arthritis. Current Opinion in Rheumatology. 2009;21:183–8. doi: 10.1097/BOR.0b013e328324e6eb. [DOI] [PubMed] [Google Scholar]
- 76.Chen J-C, Linnan L, Callahan LF, et al. Workplace policies and prevalence of knee osteoarthritis: the Johnston county osteoarthritis project. Occup Environ Med. 2007;64:798–805. doi: 10.1136/oem.2006.030148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Palmer KT, Milne P, Poole J, et al. Employment characteristics and job loss in patients awaiting surgery on the hip or knee. Occup Environ Med. 2005;62:54–57. doi: 10.1136/oem.2004.014977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Van der Burg LR, Ter Wee MM, Boonen A. Effect of biological therapy on work participation in patients with ankylosing spondylitis: a systematic review. Ann Rheum Dis. 2012;71:1924–33. doi: 10.1136/annrheumdis-2012-201914. [DOI] [PubMed] [Google Scholar]
- 79.Ter Wee MM, Lems WF, Usan H, et al. The effect of biological agents on work participation in rheumatoid arthritis patients: a systematic review. Ann Rheum Dis. 2012;71:161–71. doi: 10.1136/ard.2011.154583. [DOI] [PubMed] [Google Scholar]
- 80.Rantalaiho VM, Kautiainen H, Jarvenpaa S, et al. Decline in work disability caused by early rheumatoid arthritis: results from a nationwide Finnish register, 2000-8. Ann Rheum Dis. 2013;72:672–7. doi: 10.1136/annrheumdis-2011-200701. [DOI] [PubMed] [Google Scholar]