Abstract
Objective
This randomized controlled trial examined the effectiveness of a nurse assisted online cognitive-behavioral self-management intervention for war-related posttraumatic stress disorder (PTSD), compared to optimized usual primary care PTSD Treatment (OUC) to reduce PTSD symptoms.
Method
Participants were 80 veterans of recent military conflicts with PTSD as assessed by the PTSD Checklist (PCL) seeking primary care treatment at one of three Veterans Affairs (VA) and four Army clinics. DESTRESS-PC consisted of logins to a secure website three times per week for 6 weeks with monitoring by a study nurse. All participants received nurse care management in the form of phone check-ins every two weeks and feedback to their primary care providers. Blinded raters assessed outcomes 6, 12, and 18 weeks post-randomization.
Results
DESTRESS-PC was associated with a significantly greater decrease in PTSD symptoms compared to OUC (F(3, 186)=3.72, p=.012). The effect was largest at the 12-week assessment (ΔPCL=12.6±16.6 versus 5.7±12.5, p<0.05) with the treatment effect disappearing by the 18-week follow-up. Notably, there was a dose effect; number of logins correlated significantly with PTSD outcomes, with more logins associated with greater PTSD symptom improvement. None of the secondary outcomes (depression, anxiety, somatic symptoms, and functional status) showed statistically significant improvement; however, the treatment effect on depression approached significance (F(3, 186)=2.17, p=.093).
Conclusions
DESTRESS-PC shows promise as a means of delivering effective, early PTSD treatment in primary care. Larger trials are needed.
Keywords: Posttraumatic Stress Disorder, Depression, Military mental health, Primary care Telehealth
1. Introduction
Posttraumatic stress disorder is known to be a prevalent and disabling disorder; yet, treatment is often delayed or doesn’t happen at all [1–3]. Recent studies in the US military have estimated PTSD prevalence in up to 17% after deployment and 9% in military primary care settings. A minority of those who are symptomatic receive any formal mental health treatment in the months following their return from the war zone. Hoge and colleagues [4] examined recently returned Iraq and Afghanistan War veterans with PTSD, generalized anxiety disorder, or major depression, and found that 81% acknowledged having a problem while only 41% reported interest in receiving help. Only 30% and 14% reported professional help or mental health specialist care in the past year, respectively [4]. PTSD after deployment is particularly debilitating: it is associated with a 13.7–17.3% rate of early attrition in OIF/OEF veterans [5]. Moreover, service members and veterans with PTSD exhibit high rates of co-morbid mental health disorders [6].
Although evidence-based PTSD interventions such as cognitive-behavioral therapy (CBT) and selective serotonin reuptake inhibitors are available, many with PTSD are reluctant to access services provided in specialty mental health care settings. Indeed, the median number of years to first treatment is 12 years in the general population [3]. Further, in the military, service members with clinically significant symptoms point to the stigma associated with mental illness, lack of confidence in mental health treatment and mental health professionals, and fear of embarrassment or being viewed as weak as reasons for not seeking care [4,7]. Given these barriers to care for PTSD, there is a pressing need for a widely available, efficacious, non-stigmatizing intervention for those who might otherwise refuse or delay treatment.
Primary care is a logical setting to target early PTSD intervention efforts because: (1) it facilitates the early identification of patients who need treatment; (2) most mental health services are delivered from primary care [8], so primary care offers wider access, and therefore broader population coverage, than treatment offered exclusively in specialty care populations; and (3) mental health care delivered in a primary care context may constitute a more acceptable treatment setting, particularly in the military and VA where stigma is great.
Research demonstrates that nearly 50% of those with PTSD in the general US population indicate a preference for self-management [9]. In a study of self-managed treatment for depression, Selmi and colleagues suggest that patients suffering from mental health disorders may find self-managed treatment appealing because of ease of use and disengagement from specialty care [10].
The Internet has been shown to be an effective modality for the delivery of high-fidelity self-care – for depression, PTSD, and alcohol abuse [11–16]. Likewise, it allows patients to take a more direct role in the delivery of their healthcare [17]. In previous work we conducted a randomized controlled trial of an Internet-based self-management CBT treatment for military personnel with PTSD related to the 9–11 Pentagon attack and the subsequent Iraq and Afghanistan conflicts [12]. The intervention led to a 43% reduction in PTSD symptoms and performed significantly better than a comparison treatment consisting of supportive counseling in reducing PTSD symptoms [12]. Here we describe a follow-on study of a modified version of our earlier Internet-based PTSD self-management intervention used this time in DoD and VA primary care clinics.
We hypothesized that a nurse-assisted, online self-management CBT intervention for PTSD in primary care primary care patients would be more effective than an optimized version of usual PTSD care alone (optimized usual care, OUC) for reduction of PTSD symptoms.
2. Material and methods
The design was a two parallel arm randomized controlled trial comparing DESTRESS-PC (Delivery of Self Training and Education for Stressful Situations-Primary Care version) to OUC in primary care. We selected a two parallel arm randomized effectiveness trial design using broad inclusion criteria, because randomization maximizes the validity of study findings and broad inclusion criteria enhance the generalizability of study findings. The DESTRESS-PC intervention was delivered over 6 weeks via 18 logins (three per week) to a secure server and a registered nurse (RN, DESTRESS Nurse) assigned to each recruitment site provided participant ad hoc assistance was provided by a registered nurse (RN, DESTRESS Nurse) assigned to each recruitment site. The nurse introduced participants to the Web-based DESTRESS-PC interface, responded to their questions, reengaged them by phone or other means if two or more consecutive logons were missed, kept primary care providers apprised of patients’ status, and provided weekly updates to a research team mental health specialist. Participants were assessed at baseline and at 6, 12 and 18 weeks post-randomization for PTSD as well as depression, anxiety, somatic symptoms, and functional status.
Participants were 80 recently deployed military service members and veterans referred by their primary care providers after screening positive for PTSD. Study candidates completed a screening battery, and after a complete description of the study, their written informed consent was obtained prior to enrollment in the study. To meet inclusion criteria, candidates had had to be war veterans seeking care at a participating VA or DoD primary care clinic, report war-related trauma during deployment (to include military sexual trauma), screen positive on a 4-item PTSD screener [18], and meet criteria for PTSD on the Clinician-Administered PTSD Scale (CAPS) using the 1–2 scoring rule [19]. Individuals were excluded for: (1) active engagement in trauma-focused mental health treatment in the previous 2 months; (2) recent history of failed specialty mental health treatment for PTSD or an associated condition; (3) acute psychosis, psychotic episode, or psychotic disorder diagnosed within the past 2 years; (4) active substance dependence in the past year; (5) active suicidal or homicidal ideation within the past 2 months; (6) currently taking antipsychotic or mood-stabilizing medication; (7) unstable administration schedule or dosing of any antidepressant, anxiolytic, or sedative-hypnotic during the last month; or (8) acute or unstable physical illness.
2.1. Randomization
Randomization was performed centrally from Walter Reed’s Deployment Health Clinical Center with subsequent notification of the site investigator and the site’s DESTRESS Nurse. Stratification of randomization by healthcare site and gender was done to facilitate exploratory analyses on trial outcomes [20]; and employed a random permuted blocking scheme (1:1 allocation ratio with variable block size of four to six) [21] was employed. We blinded the outcome raters in this trial; however, the nature of the intervention precluded blinding of providers and participants. Participants were randomized to DESTRESS-PC plus OUC or OUC alone.
2.2. DESTRESS-PC intervention
The DESTRESS-PC intervention utilizes uses a variant of CBT-based and stress inoculation training approaches in a nurse-guided online patient self-management paradigm. As an empirically validated treatment for PTSD [22], CBT is a logical treatment approach to incorporate into a self-management model, particularly because it easily translates into this method of treatment delivery. A non-trauma focused CBT approach was selected to avoid questions about the safety of “hot affect” techniques such as exposure therapy delivered online.
Participants assigned to the DESTRESS-PC arm were asked to log on the secure Web site three times each week for 6 weeks and complete various homework activities. By logging on to the website, participants were able to access educational information about PTSD, stress, and trauma, as well as common comorbid problems and symptoms they might experience post-trauma (e.g., depression, survivor guilt). As their logins progressed, they were provided with information on strategies to manage anger and to promote better sleep hygiene, as well as in-depth information on how to perform and practice two easy stress management strategies: deep, slow diaphragmatic breathing and simple progressive muscle relaxation. In addition, participants learned cognitive reframing techniques, such as how to challenge unhelpful thought patterns and alter self-talk to manage demanding situations effectively. Patients were also asked to generate a hierarchy of difficult and avoided situations that triggered deployment memories or were generally stressful.
At each login, participants were asked to make ratings of their PTSD symptoms and a global rating of their level of depression. Each login consisted of a new set of educational materials followed by a homework assignment to practice new techniques and skills learned. Broken up into five units, these assignments promoted stress-reduction skills, self-monitoring, application of stress management techniques to each stress hierarchy item, processing and coping with a particularly salient or intense traumatic memory as well as very significant current day stressors, and relapse prevention. Participants were required to complete each homework to continue subsequent content. Each login was intended to take 15–30 minutes and homework assignments another half-hour. Participants were encouraged to contact the DESTRESS Nurse for assistance if needed. Likewise, the DESTRESS Nurses were able to access a private portion of the DESTRESS-PC Web site where they could monitor compliance and symptom levels.
All participants were given up to 8 weeks to complete the treatment program and were subsequently denied access to the DESTRESS website. In very rare cases, participants were allowed 10 weeks to complete the program if the DESTRESS Nurse felt that there were sufficient extenuating circumstances preventing the participant from completing the program in the designated timeframe. Participants who took more than 8 weeks to complete the program had their follow-up assessments delayed accordingly and were yoked to a matched participant from the OUC group who had their assessments similarly delayed.
2.3. Optimized usual PTSD care (OUC)
Optimized usual PTSD care (OUC) consisted of usual primary care PTSD treatment augmented with low intensity care management, feedback to the primary care provider, and training of the clinic providers in management of PTSD. It was designed to approximate the level of PTSD care normally provided in primary care while incorporating the nonspecific treatment elements of the DESTRESS intervention.
Participants received three 15 minute telephone check-ins with the DESTRESS Nurse, to allow the nurse to monitor their progress, answer questions, and assess them for risk at weeks two, four, and six, ad hoc access by e-mail or phone for questions, and in-person consultation in the event of urgent needs or matters impacting participant safety. The DESTRESS Nurse reported relevant symptom information to the participant’s primary care provider at baseline and throughout the study. Additionally, clinic providers (physicians, mid-level providers, nurses) received pre-study didactic training regarding management of and clinical tools for PTSD and associated conditions (e.g., suicidal and violent ideation and related risk).
2.4. Primary outcome
The PTSD Checklist, Civilian Version [23] was used as the primary outcome measure to assess PTSD symptom severity at baseline and at the 6-, 12- and 18-week follow-ups. It is a 17-item measure that assesses the symptoms of PTSD in the DSM-IV and yields a total score ranging from 17 to 85. The civilian version was used because it measures PTSD symptoms from any cause. This is important because preexisting PTSD may be exacerbated by “war-related trauma”.
2.5. Secondary outcomes
The Patient Health Questionnaire (PHQ) was used to assess depression, anxiety, and somatic symptom severity at baseline and the three follow-ups. The PHQ is a brief self-report assessment of common mental disorders developed specifically for primary care. The PHQ allows brief provisional primary care diagnoses of several disorders including major depression, panic disorder, other anxiety disorders, and multisomatoform disorder.
Symptoms of major depression were assessed using the 8-item PHQ depression scale (PHQ-8). The PHQ-8 is the same as the PHQ-9, but does not have a suicidal ideation question. The PHQ-9 has been evaluated as a diagnostic screen for a depressive disorder and as a measure of depression severity [24].
Somatic symptoms were measured with the widely used and validated 15 item Patient Health Questionnaire (PHQ-15) [25] A score ≥ 15 indicates high somatic symptom severity based on data from primary care settings [25].
PHQ anxiety sections include panic and generalized anxiety symptoms. Data support their applicability, validity, and reliability in general medical and psychosomatic patient populations [26,27]. Similar to the PHQ scales for depression and somatic symptoms, the anxiety scales correspond well to symptom-based diagnostic criteria in DSM-IV.
The Medical Outcomes Study Short Form-36 (SF-36) [28] was used at baseline and the three follow-ups to evaluate the physical (PCS) and mental (MCS) component summary measures of health functioning. The SF-36 is a widely used measure of health related quality of life with established reliability and validity [28].
2.6. Analysis plan
To account for the dependence of observations produced by repeated measurements of participants over time, we used the PROC MIXED procedure (mixed-model regression) with the REPEATED statement in SAS. Because the PROC MIXED procedure uses all of the available data and restricted maximum likelihood to estimate the unknown variance-covariance parameters, it ensures a robust handling of missing follow-up data [29]. We examined the effects of time, treatment group, and the treatment group by time interaction on the primary outcome (PCL scores) for the entire sample and for the two types of recruitment sites (VA, DoD) separately. For the secondary outcomes, we examined the effects of the same three predictors for the entire sample only. We controlled for recruitment site and gender in the analyses because randomization was stratified on these factors.
2.7. Sample size calculation
Based on the results of our pilot study [12], we calculated an expected effective size of .60. Thus, we needed about 45 participants per study arm to achieve 80% power at α=.05. Factoring in the 30% attrition rate, we sought to randomize a total of 128 participants.
3. Results
3.1. Sample characteristics
Fig. 1 summarizes participant recruitment, eligibility, enrollment, randomization, dropouts, and follow-up. Of the 252 participants who were screened for the trial, 119 were ineligible, 40 were excluded, and 13 dropped out prior to randomization. The remaining 80 participants were randomly assigned to the two study arms, 43 DESTRESS-PC and 37 to OUC. Sixty-six participants completed the study through the (final) 18-week follow-up. There was no association between treatment condition and the percentage of participants that were lost to follow-up, χ2(1)=.76, p=.384. Those who completed the follow-up did not differ from those lost to follow-up with regard to baseline characteristics. On the SF-36, completers reported significantly better mental health than those lost to follow-up, t(78)=2.74, p=.008.
Fig. 1.
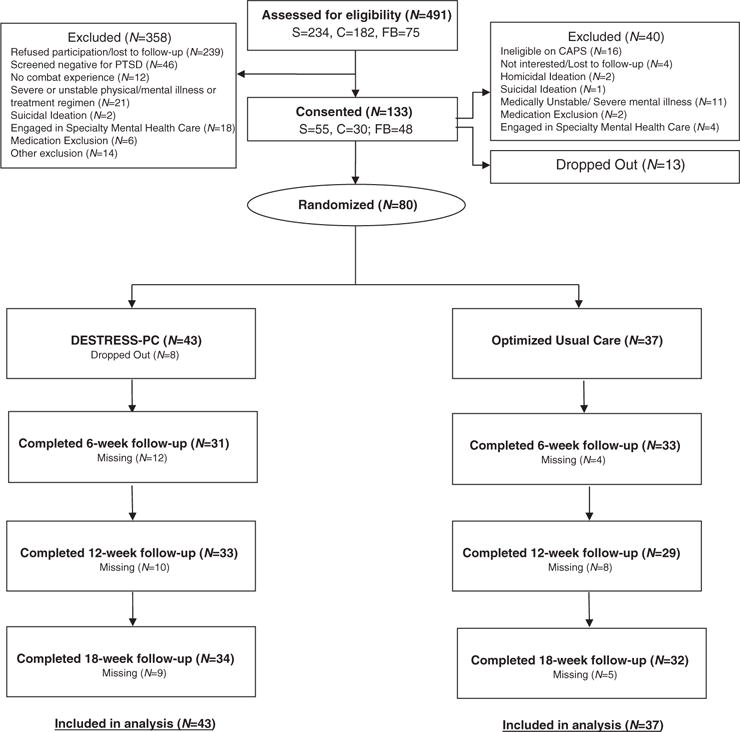
CONSORT diagram showing participant flow through screening, enrollment, randomization, treatment, and follow-up. S=Savannah VA; C=Charleston VA; FB=Fort Bragg.
There were no statistically significant differences between the individuals assigned to DESTRESS-PC (n=43) and those assigned to Optimized Usual Care (n=37) in terms of baseline demographic characteristics or pre-treatment symptomatology, suggesting random allocation achieved baseline comparability across the two study arms (Table 1).
Table 1.
Baseline characteristics
| Variable | OUC (n=37)
|
DPC (n=43)
|
||
|---|---|---|---|---|
| n/M | %/SD | n/M | %/SD | |
| Demographics characteristics | ||||
| Age | 36.7 | 9.75 | 36.2 | 7.75 |
| Male | 31 | 83.8% | 34 | 79.1% |
| Married | 25 | 67.6% | 26 | 60.5% |
| Some College | 22 | 59.5% | 27 | 62.8% |
| White, Not Hispanic | 21 | 56.8% | 23 | 53.5% |
| Army | 34 | 91.9% | 37 | 86.0% |
| Active Duty | 21 | 56.8% | 27 | 64.3% |
| Enlisted | 35 | 94.6% | 39 | 92.9% |
| Symptom Levels | ||||
| PCL | 55.16 | 10.89 | 58.56 | 10.01 |
| PHQ9 | 11.86 | 4.54 | 13.84 | 5.41 |
| PHQ15 | 12.43 | 4.91 | 12.44 | 5.16 |
| Physical functioning | 68.78 | 22.96 | 68.37 | 24.80 |
| Mental functioning | 47.64 | 25.66 | 39.83 | 29.66 |
Note. OUC=Optimized Usual Care. No between-group differences reach statistical significance when p<.10.
3.2. Intent to treat analysis
3.2.1. Primary outcome – PTSD checklist (PCL)
Table 2 provides the adjusted means (controlling for recruitment site) for the total PCL scores across the four time points. The DESTRESS-PC group improved at a faster rate than the OUC group and showed larger treatment gains (treatment by time interaction, F(3, 186)=3.72, p=.012; main effects for time, F(3, 186)=17.21, p<.001, and recruitment site, F(1, 77)=8.32, p=.005), with the largest treatment effect seen at 12 weeks, t(186)=2.44, p=.016 and diminishing by the 18-week follow-up (see Fig. 2). Six-week effect size was 0.23 (small), 12-week effect size was 0.47 (medium), and 18-week effect size was 0.08.
Table 2.
Means and standard deviations for treatment outcome measures
| Assessment | Optimized Usual Care
|
Treatment
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Min | Max | Mean | S.D. | N | Min | Max | Mean | S.D. | |
| PCL | ||||||||||
| Baseline | 33 | 31 | 78 | 54.48 | 11.23 | 40 | 25 | 78 | 58.00 | 9.95 |
| 6-week | 29 | 23 | 71 | 48.52 | 13.97 | 29 | 20 | 114 | 50.72 | 18.76 |
| 12-week | 25 | 17 | 72 | 47.36 | 17.45 | 30 | 19 | 83 | 43.80 | 18.33 |
| 18-week | 27 | 17 | 68 | 42.74 | 14.42 | 31 | 18 | 77 | 44.58 | 16.43 |
| PHQ-8 | ||||||||||
| Baseline | 33 | 4 | 22 | 11.67 | 4.65 | 40 | 3 | 22 | 13.53 | 5.43 |
| 6-week | 29 | 2 | 21 | 10.24 | 5.12 | 29 | 2 | 22 | 11.00 | 6.65 |
| 12-week | 25 | 0 | 22 | 10.40 | 6.77 | 30 | 0 | 23 | 9.66 | 7.04 |
| 18-week | 25 | 0 | 21 | 8.96 | 5.62 | 30 | 0 | 21 | 10.23 | 7.01 |
| PHQ-15 | ||||||||||
| Baseline | 33 | 5 | 27 | 13.31 | 5.04 | 40 | 2 | 27 | 13.25 | 5.64 |
| 6-week | 29 | 2 | 23 | 11.86 | 5.18 | 29 | 1 | 23 | 11.90 | 5.63 |
| 12-week | 25 | 1 | 27 | 12.16 | 6.80 | 30 | 1 | 25 | 11.37 | 6.70 |
| 18-week | 25 | 0 | 23 | 10.79 | 6.48 | 30 | 1 | 25 | 11.38 | 6.16 |
Fig. 2.

PCL PTSD symptoms (treatment × time interaction).
3.2.2. Secondary outcomes
For the PHQ-8, there was a main effect for time, F(3, 186)=10.34, p<.001, and a trend towards a treatment by time interaction, F(3, 186)=2.17, p=.093. None of the interaction terms for the other three secondary outcomes (i.e., PHQ-15, SF-36 MCS, SF-36 PCS) were significant.
3.2.3. Treatment adherence
Of the 43 participants who were randomized to the DESTRESS-PC arm, 28 (65%) completed at least 6 logins, 18 (42%) completed at least 12 logins, and 15 (35%) completed all 18 logins. The correlation between the number of logins completed and the decrease in PCL scores was r=.36, p=.041 at the 12-week assessment and r=.34, p=.052 at the 18-week assessment (see Table 3). There was some suggestion that adherence may have been differentially related to PCL scores for DoD versus VA sites (VA sites, r=.47, p=.026 and r=.48, p=.023; DoD sites, r=.16, p=.632 and r=−.05, p=.883). However, the study was not powered to detect a difference and the interaction was not statistically significant. There was no difference between the number of sessions completed for the participants from the VA versus DoD (10.6±7.6 vs 8.5±6.2; t(41)=.93, p=.36).
Table 3.
Average change in PCL symptoms by total logins completed
| Logins completed | n | Mean change (SD)
|
||
|---|---|---|---|---|
| 6-week assessment | 12-week assessment | 18-week assessment | ||
| 0 to 6 | 9 | 3.00 (11.31) | 3.78 (10.56) | 4.33 (10.01) |
| 7 to 12 | 7 | 3.33 (9.350) | 10.00 (19.91) | 6.86 (10.57) |
| 13 to 18 | 18 | 11.06 (11.04) | 18.41 (16.33) | 16.78 (16.56) |
| F (p) | 2.05 (0.147) | 2.63 (0.088) | 2.82 (0.075) | |
4. Discussion
Though the overall study benefits of online self-management of primary care patients with PTSD were measurable and statistically significant. are modest and transient, there are reasons for guarded optimism. Though benefits were modest and decreased soon after discontinuation of online self-management, there are reasons for pursuing further related work.
First, the goal of using a nurse assisted web-based approach to self-management was to broaden the availability of effective treatment options for patients reluctant to otherwise engage in PTSD treatment. One recent study found that the median time to first treatment of PTSD was 12 years [3], and the need to extend the reach of appropriate psychological treatments is great. From a public health perspective, approaches with a relatively small but positive effect may represent an important therapeutic advance if these approaches can help to extend population treatment reach [30]. Many if not most in various populations and communities use primary care services several times each year. Ways of efficiently allowing patients to sample a generally effective method of treatment on their own terms may even be a stepping stone for higher intensity forms of evidence-based PTSD psychotherapy.
Second, the fact that adherence to online self-management was significantly associated with PTSD symptom improvement, and future studies might test whether suggest that ‘booster sessions’ or other strategies to extend or improve adherence online self-management may offer can yield more robust improvements over time. Offering nurses extra training in patient engagement strategies such as motivational interviewing may improve uptake and adherence. Furthermore, the intervention tested was text intensive, and future studies should assess adherence as a function of differing delivery formats, including use of animation and video vignettes.
One rationale for studying a primary care-based self-management approach is the potential to intervene earlier in a greater proportion with untreated symptoms. Median time to first PTSD treatment is an estimated 12 years [3], and the need to extend the reach of effective treatment is great. From a public health perspective, a small individual benefit may represent an important population advance if treatment reach is extended [30]. This trial did not evaluate treatment reach, but it is worth noting that of the 491 primary care patients approached for study participation, 239 (49%) refused participation. Refusal reasons are not known, but high rates suggest online self-management is less than widely attractive. This is consistent with previous literature showing that web-based treatments are often effective, but few patients choose it and lack of adherence is common [31].Unfortunately, however, the literature on Web-based treatment for various mental disorders has thus far suggested that it is often effective, but surely less than a panacea. Disappointingly few patients actually choose to use it when given the option, and lack of adherence among those who initiate it is common [31]. Offering skilled primary care nurses training experiences in patient engagement strategies such as motivational interviewing may be one way of improving uptake and adherence.
Third, DESTRESS-PC could be blended more integrally with medication treatment, with primary care providers monitoring and prescribing appropriate medications and trained nurses monitoring DESTRESS-PC psychological treatment. A similar blended approach could also be fruitful for those living in rural and remote areas or for whom in-person visits to specialty care are a hardship. DESTRESS-PC could be interspersed with less frequent in-person visits to reinforce the development of coping and self-management repertoires.
There are caveats to our study that should be considered when interpreting the study findings. Most importantly, the sample size was small, and participation refusal rate was high, factors which that may reduce the external validity and generalizability of the study findings. Another consequence of the small sample size was our a lack of power to detect differences in participation, adherence, and effect between VA and DoD active duty service participants. We found trends to suggest that VA veterans adhered and responded better to nurse assisted online self-management intervention than did active duty DoD beneficiaries, but perhaps due to sample size these differences did not reach statistical significance, perhaps due to the small size of our sample. Lastly, the study design (an effectiveness design employing a usual care treatment comparison) made no effort to control for nonspecific effects such as contact time. Hence, the study is unsuitable for assessing the effectiveness of particular DESTRESS-PC treatment components.
The intervention we tested was text intensive, and future studies should emphasize the difference in treatment adherence with differing delivery formats such as the use of animation and video vignettes. As previously noted, training nurses in engagement techniques may enhance patient initiation, adherence, persistence, and therapeutic outcomes.
4.1. Conclusions
We have found that primary care patients with military related PTSD randomly assigned to 8 weeks of nurse- assisted online CBT self-management experienced significantly greater mean improvement in PTSD symptoms than did those patients who were assigned to optimized usual PTSD care alone. Improvement in the online self-management group was greatest at the 12-week follow-up, but decreased after discontinuation of online treatment, showing no with essentially no remaining benefit at 18-week follow-up. Additional research to increase adherence may improve outcomes.
In summary, this study shows that DESTRESS-PC may be a promising intervention and provide another option for primary care patients with PTSD. Additional research to improve adherence may improve outcomes.
Acknowledgments
Special thanks to our DESTRESS Nurses, Karen May, RN, MSN, PMHNP-BC, Christi Oates, RN, BSN, and Cheri Portee, RN, BSN, for their extensive effort in support of this project.
References
- 1.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):603–13. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 4.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 5.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–32. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 6.Kozaric-Kovacic D, Borovecki A. Prevalence of psychotic comorbidity in combat-related post-traumatic stress disorder. Mil Med. 2005;170(3):223–6. doi: 10.7205/milmed.170.3.223. [DOI] [PubMed] [Google Scholar]
- 7.Hoge CW, Toboni HE, Messer SC, Bell N, Amoroso P, Orman DT. The occupational burden of mental disorders in the U.S. military: psychiatric hospitalizations, involuntary separations, and disability. Am J Psychiatry. 2005;162(3):585–91. doi: 10.1176/appi.ajp.162.3.585. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–23. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(Suppl. 5):4–12. [discussion 3–4] [PubMed] [Google Scholar]
- 10.Selmi PM, Klein MH, Greist JH, Sorrell SP, Erdman HP. Computer-administered cognitive-behavioral therapy for depression. Am J Psychiatry. 1990;147(1):51–6. doi: 10.1176/ajp.147.1.51. [DOI] [PubMed] [Google Scholar]
- 11.Wagner B, Schulz W, Knaevelsrud C. Efficacy of an internet-based intervention for posttraumatic stress disorder in Iraq: a pilot study. Psychiatry Res. 2012;195:85–8. doi: 10.1016/j.psychres.2011.07.026. [DOI] [PubMed] [Google Scholar]
- 12.Litz B, Engel C, Bryant R, Papa A. A randomized, controlled proof-of-concept trial of an internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Am J Psychiatry. 2007;164(11):1676–83. doi: 10.1176/appi.ajp.2007.06122057. [DOI] [PubMed] [Google Scholar]
- 13.Lange A, Rietdijk D, Hudcovicova M, van de Ven JP, Schrieken B, Emmelkamp PM. Interapy: a controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. J Consult Clin Psychol. 2003;71(5):901–9. doi: 10.1037/0022-006X.71.5.901. [DOI] [PubMed] [Google Scholar]
- 14.Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. J Med Internet Res. 2002;4(1):e3. doi: 10.2196/jmir.4.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glueckauf RL, Pickett TC, Ketterson TU, Loomis JS, Rozensky RH. Preparation for the delivery of telehealth services: a self-study framework for expansion of practice. Prof Psychol Res Pr. 2003;34(2):159–63. [Google Scholar]
- 16.Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, et al. Impact of a patient-centered, computer-based health information/support system. Am J Prev Med. 1999;16(1):1–9. doi: 10.1016/s0749-3797(98)00108-1. [DOI] [PubMed] [Google Scholar]
- 17.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 18.Prins A, Ouimette P, Kimmerling R, Camerond RP, Hugelshofer DS, Shaw-Hegwer J, et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Prim Care Psychiatry. 2004;9(1):9–14. [Google Scholar]
- 19.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD Scale. J Trauma Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 20.Kernan WN, Viscoli CM, Makuch RW, Brass LM, Horwitz RI. Stratified randomization for clinical trials. J Clin Epidemiol. 1999;52(1):19–26. doi: 10.1016/s0895-4356(98)00138-3. [DOI] [PubMed] [Google Scholar]
- 21.Schulz KF, Grimes DA. Generation of allocation sequences in randomised trials: chance, not choice. Lancet. 2002;359(9305):515–9. doi: 10.1016/S0140-6736(02)07683-3. [DOI] [PubMed] [Google Scholar]
- 22.Cahill SP, Rothbaum B, Resick PA, Follette VM. Cognitive-behavioral therapy for adults. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. 2nd. New York (NY): Guilford Publications; 2009. pp. 139–222. [Google Scholar]
- 23.Weathers FW, Litz BT, Herman JA, Huska JA, Keane TM. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Proceedings of the Annual Convention of the International Society for Traumatic Stress Studies; 1993; San Antonio, TX. [Google Scholar]
- 24.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(1):509–21. [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 27.Lowe B, Grafe K, Zipfel S, Spitzer RL, Herrmann-Lingen C, Witte S, et al. Detecting panic disorder in medical and psychosomatic outpatients: comparative validation of the Hospital Anxiety and Depression Scale, the Patient Health Questionnaire, a screening question, and physicians’ diagnosis. J Psychosom Res. 2003;55(6):515–9. doi: 10.1016/s0022-3999(03)00072-2. [DOI] [PubMed] [Google Scholar]
- 28.Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: a user’s manual. Boston (MA): Health Measurement Lab; 1994. [Google Scholar]
- 29.Littell R, Woodward SH, Young HE, Sheikh JI. SAS system for mixed models. Cary (NC): SAS Institute Inc; 1996. [Google Scholar]
- 30.Koepsell TD, Zatzick DF, Rivara FP. Estimating the population impact of preventive interventions from randomized trials. Am J Prev Med. 2011;40(2):191–8. doi: 10.1016/j.amepre.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boasso A, Kadesch H, Litz BT. Internet-based interventions for PTSD. In: Friedman M, editor. Handbook of PTSD: Science and practice. 2nd. New York (NY): Guilford Press; 2014. pp. 557–70. [Google Scholar]


