Abstract
Background:
Case-oriented small group discussions (COSGDs) can help students to correlate and integrate the basic science of dental materials into clinical application. We used COSGDs along with didactic lectures in dental material curriculum and hypothesized that case-oriented group discussions would be more effective than traditional lecture alone in terms of performance of students, student perception on the above two teaching methodologies and the feasibility in classes of 2010, 2011 and 2012.
Methods:
A total of 170 students were taught using both COSGD and didactic lecture in a randomized controlled crossover trial design. Their performance was assessed through multiple-choice questions (MCQs) as part of the formative assessment, and their perception was assessed through Likert scale questionnaire.
Results:
The mean difference in the scores between case-oriented group discussions with lecture and didactic lecture showed significant difference only in few topics. Around 94–96% of students perceived COSGD with didactic lecture help them understand theory better; 76–92% of students feel more comfortable asking questions in a group discussion; 89–98% of students feel such discussions motivate them and 91–100% of students agree that discussions make the subject interesting in the respective years of 2010, 2011 and 2012.
Conclusion:
Effectiveness of COSGD in terms of scores through MCQs is comparable to traditional lecture. However, most of the students perceive COSGD help them understand the theory better; co-relate clinically; more motivating and interesting than a traditional lecture. Feasibility in institution needs more time and resources to conduct COSGD within the dental material curriculum.
Key Words: Case-based learning, dental education, dental materials, preclinical training, problem-solving, small group discussions
INTRODUCTION
The Institute of Medicine report in 1995 stressed the need for change in dental education with better application of basic science to clinical problems and experimentation with different models of education, practice and performance assessment.[1] Rajiv Gandhi University of Health Sciences curriculum in the State of Karnataka, India for undergraduate dental students, advocates the use of learner-oriented methods such as problem-solving abilities and self-directed learning. Conventional curriculum prescribes dental materials in the 1st year undergraduate syllabus. The didactic lecture format is the predominant mode of teaching method, which is more teacher than student-centered.
Passive nature of didactic lectures leads to low receptivity from the audience and can be ineffective in retaining what is learnt and in problem-solving. With students having no clinical exposure in their initial year of dental training and the prescribed textbooks of dental materials focusing solely on material aspect, interpreting dental materials (that requires analytical skill) becomes difficult. It is left to the ability of the student to mentally visualize the clinical situation, which makes the subject rather unappealing. Informal feedback from senior students and exam result analysis of the previous classes showed more disinterest and failures in dental materials. Traditional lectures with limitations of time cannot explain all relevant clinical scenarios. Cuseo listed out few deleterious outcomes of large size lecture such as faculty overdependence on lecture, reduced student interaction; less achievement of Blooms taxonomy level of learning objectives and lower depth of student thinking especially on 1st year students.[2]
The promising trend globally is to have a problem-based integrated student centered learning with active participation and self-directed learning[3] that can facilitate analytical, problem-solving skills and team work with group discussions. Dental curricula have to shift their focus on core competencies with patient-centered education.[4]
Case-based learning (CBL) is based on the principle of using a case or a problem or an inquiry to stimulate, support knowledge, skills and attitude that requires a degree of prior knowledge from students to help in clinical case solving. Cases place situations in a realistic setting and can aid the students in applying the basic information. CBL also promotes team based approach, motivation, scientific inquiry and integration of knowledge and practice.[5] Du et al. concluded that -CBL was found to be more effective than lecture based education for 4th year dental students in oral leukoplakia in the School of Stomatology at Wuhan University and suggested that CBL be added in future oral medicine curriculum for dental students.[6] Tao et al. in the Department of Dentistry, Shangai Jiao Tong University applied CBL with randomization in two groups in the clinical practice and found the favorable response of students towards CBL than traditional methods.[7] Ghosh had implemented case-oriented problem-solving tutorials with didactic lectures in physiology to improve understanding and motivation among students.[3] A survey among dental graduates by Keeve et al. showed CBL curriculum had a positive effect on core competencies of students.[4]
Clinical application of dental materials contributes majorly to a student's or a dentist's clinical competence. Case-oriented small group discussions (COSGDs) may provide an excellent platform for student-centered learning with the integration of basic science and clinical application. The Department of Prosthodontics at M S Ramaiah Dental College introduced some basic topics in dental materials to 1st year dental students using didactic lectures complemented with clinical case problems. We hypothesized that that COSGD with the didactic lecture was better than lecture alone on the understanding of dental materials with the null hypothesis that there would be no difference between them.
The aims and objectives of the study were to evaluate:
Effectiveness of COSGD with didactic lecture over didactic lecture alone on understanding of some topics of dental materials
Students’ perception toward COSGD over traditional lecture
Feasibility of introducing student-centered learning in the institution.
METHODS
Study population and setting
A total of 170 students between the age range of 18–22 years in the first semester of dental undergraduate course in the consecutive class of 2010, 2011 and 2012 were taught five topics in dental materials in the Department of Prosthodontics. The female: male ratio in all classes were 3:1. Each class was divided into two batches, A and B with equal aptitude and assimilation, based on their test scores after a didactic lecture on an introductory topic. A stratified random sampling was done to ensure that each of the batches A and B had equal representation based on the scores of the test with the mean scores of both batches being the same.
Study design
A randomised controlled cross over trial was planned as shown in Figure 1. The interventions of didactic lecture and COSGD were done to assess their effect on the study subjects. All three classes of 2010, 2011 and 2012 were taught the same five topics. The assigned lectures were conducted based on university guidelines. The lecture classes were held once a week. The lesson plan for the lectures remained the same for both batches A and B. Since the topics were new to all students, a 40 min didactic lecture was conducted for both the batches separately. The COSGD group had an additional 20 min of case-based discussion.
Figure 1.
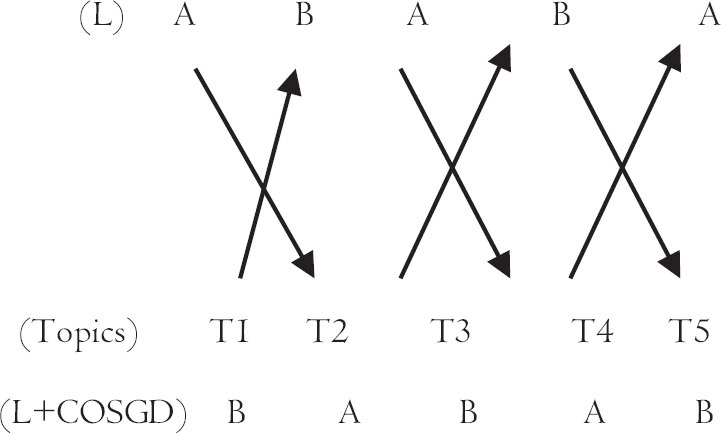
Flowchart shows the scheme of crossover study design for lecture with group discussion (L+COSGD) & lecture (L) for the batches A & B
The methodology used in this study is a slight modification of the CBL process. Here, a clinical problem is formulated by the facilitator with specific learning outcomes which is given to the students to later solve with group discussions and brainstorming with prior knowledge and present the solutions to the rest of the groups as shown in Annexure 1. Areas for improvement are identified with the help of the facilitator. Integration into practice can be assessed once the students enter the clinical years in future.
After the lecture was taken, the COSGD batch of 25–30 students, were divided into five groups, each of 5–6 students. All the students in the COSGD group were given worksheets with five clinical case problems. Each of the problem was assigned to each of these groups. The students of each group were instructed to discuss the respective problem assigned to them as well as briefly discuss the rest of the clinical problems, come out with solutions and present them within the group. The students were encouraged to discuss the problems and clarified any differing views with their peers. The teacher was only a facilitator to assist the group in structuring their thoughts, apply their reasoning ability and identify solutions.
The cross over after each topic allowed each of the batches to be part of the lecture and COSGD format to rule out any bias. Separate teachers were assigned for each topic to rule out bias in teaching styles and were trained to conduct small group discussions. The study design was approved by the Ethical Committee (Institutional Review Board). Informed consent was obtained from the students to take part in the study prior to the commencement of the study.
Student evaluation
Students were evaluated 2–3 days after the lecture or lecture + COSGD through an objective assessment in the form of single best answer multiple-choice questions (MCQs) (type A of Hubbard and Clemans). The MCQ was designed with greater emphasis on clinical application (70%) and less on recall (30%). They were structured according to the learning objectives of the respective topic. A total of 15 assessments were carried out for three consecutive years.
Student perception
The second objective of this study was to evaluate the student's perception of the new teaching methodology. It is important to get prompt feedback from the students before attempting to change the T-L method. The students were given a 10 statement 5 point Likert scale questionnaire to evaluate their perception on the two teaching methodologies. The first five of the statements were worded favorably towards COSGD and the last five were favorable towards didactic lecture format. This was to make the students respond to the statements after some thought rather than agree or disagree automatically.[5] The validity of the questionnaire was tested through a pilot study and discussion with subject experts.
Statistical analysis
The data were analyzed using SPSS software (version 10.S). The number and percentage were presented for categorical data, mean and standard deviation for continuous data in tables. Frequency distribution of the students was used to assess the student perception. To test for the difference in mean score between lecture and group discussion considering years, a multilevel analysis was attempted. Two-way ANOVA was performed for comparing class wise (2010, 2011 and 2012) mean scores by levels of teaching methods (two groups) simultaneously. P < 0.05 was considered as statistically significant. The student's scores of COSGD and lecture were analyzed using descriptive statistics. Two-way ANOVA was performed for comparing class wise (2010, 2011 and 2012) mean scores by levels of teaching methods (two groups) simultaneously.
RESULTS
Student evaluation
Table 1 shows mean scores (with standard deviations) of the students in each of the topics in the corresponding class of 2010, 2011 and 2012. A significant difference was found among the classes (2010, 2011 and 2012) for all the topics except for the topic four. There was a significant difference between two methods of teaching on topic two (P = 0.03) and on topic three (P = 0.044). The rest of the topics showed no significant difference between two methods of teaching.
Table 1.
Mean scores of students with case oriented small group discussion and lecture in the class of 2010, 2011 and 2012

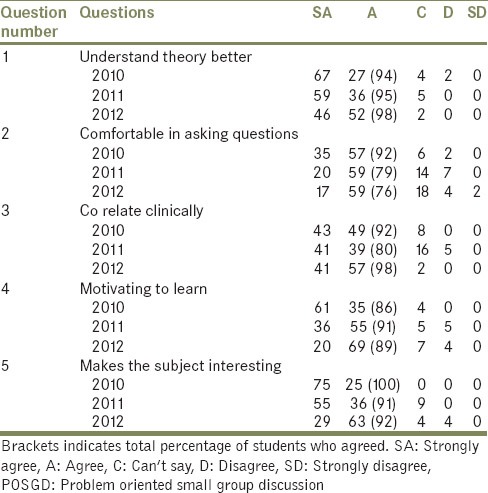
Student perception
Table 2 shows most students in classes 2010, 2011 and 2012 strongly felt group discussions help them understand the subject better than lecture class [Table 2, Q1 and Q6]. They are more comfortable in asking questions in a small group discussion set up than in a traditional lecture class [Table 2, Q2 and Q7]. Students also strongly felt that they are able to relate the theory into clinical application better with a small group discussion [Table 2, Q3 and Q8]. Group discussions also motivated them to learn [Table 2 Q4 and Q9] and made the subject more interesting [Table 2 Q5 and Q10]. Class 2010 felt more comfortable in asking questions, discussions made the subject interesting and helped in clinical correlation than the class of 2011 and 2012. Class 2012 understood the theory better with discussions than 2010 and 2011. Class 2011 were more motivated to learn than 2010 and 2012.
Table 2.
Percentages of student response for POSGD with lecture in the class of 2009, 2010 and 2011
DISCUSSION
Student evaluation
The evaluation of COSGD scores with didactic lectures scores showed significant difference only in two topics of the 15 topics covered for the classes 2010, 2011 and 2012. The reason could be that these two topics were taught hands on in the practical curriculum. Manipulating gypsum products and heat cure resin are practical exercises followed in the curriculum that students have to perform and could be the reason that the students scored better in the above respective topics. This provides a cue that the practical application of theory in curriculum complemented with case-based problem-solving group discussions may help in better understanding of the subject. A significant difference in scores between all the classes for all topics [Table 1] could be attributed to the differences in the aptitude of the students. Class 2010 and 2011 in all the topics scored better compared to 2012. CBL with student centered education in oral medicine curriculum complemented in better understanding of the subject.[5]
Student perception
Differences were also noted with respect to perception towards COSGD amongst the classes 2010, 2011 and 2012. Class 2010 felt more favorable toward CBL than class 2011 and 2012. This may indicate that student perception toward teaching methodology may be directly related to scoring in formative assessments, which could be explored in future. Effect of gender on performance was not evaluated as the majority of the students were females in all classes.
In contrast to the performance on MCQ, majority of students perceived COSGD better for learning than didactic lecture. Group discussion creates an active learning environment which can allow greater understanding of the problem from a conceptual point. The dynamics of discussion itself may encourage learning through peers and the discussions create an environment in which students may not dread asking a “foolish” question.[7]
Zhang et al. at used CBL in selected stomatological courses and found a good student response and high acceptance at the Shangai Jiao Tong University.[8] Online case based discussions in periodontology for clinical undergraduate students received appreciation from students in the Faculty of Medicine at Ghent University though no significant differences were found in the test scores.[9] McKenzie found CBL positively affected students’ knowledge, attitude and skills at the University of Alabama.[10] Kumar and Gadbury-Amyot continue to implement case-based and team-based learning in oral medicine and radiology at the Department of Oral Pathology at the University of Missouri based on positive student feedback.[11]
Over 76% of students feel more comfortable asking questions in a group discussion than in a didactic lecture because group discussion can act as a nonthreatening platform to clarify their doubts. Group discussions can be used to formally integrate previous knowledge through active integrating discussion.[12] Jones et al. assessed small team active learning in an integrated pharmacokinetics course series and found the course had a positive impact on student's ability to apply concepts to case-based scenarios, but little ability to critically evaluate new material.[13] Katsuragi added problem learning tutorials to a traditional lecture-based curriculum in a dental school and found students were comfortable in the discussions.[14]
Over 79% of the students feel group discussions help them co-relate the topic better clinically for a patient than a lecture class, supporting the encoding specificity of the learning theory. Knowledge being a combination of information and application requires encoding of the said information with the applied activity at the time of learning for successful retrieval. A similarity between the learned and applied situation enhances the performance of the individual.[15] Small group discussions allow integration of information from different sources, fusing broader concepts to specific cases.[16]
One of the principles of learning includes “meaning orientation” in which knowledge and skills are learned with understanding, as compared to “rote learning,” which is associated with only superficial understanding. COSGD allows students to correlate theory with application, thereby triggering intrinsic motivation.
A large majority of the students feel group discussions motivate them to learn more, vindicating student-centered learning over tutor centered learning. Intrinsic motivation arises from the expectation of the long term utility of a learning task. As dentistry is an applied science, the learning experience with learning objectives must have a direct relevance to the care of humans in health and disease. Steinert assessed student perception through focus group discussions on small group teaching in a medical school and found that students emphasized more group atmosphere, facilitation skills and on clinical relevance of problem cases, critical thinking skills and integration of basic and clinical sciences.[17] CBL was an effective tool that led to significant improvement of self-reported student satisfaction, motivation and engagement in traditional pharmacology course.[18]
A vast majority of students feel such discussions make the subject more interesting. Active participation, meaningful learning and problem-based group discussions are itself the highest level of learning. Information is better understood, processed and retrieved if learners have the opportunity to elaborate on that information. The elaboration may be in the form of discussion. Botelho and O’Donnell found problem orientated small group discussion in fixed prosthodontic simulation laboratory course provides beneficial peer to peer interaction which is known to facilitate learning. Small group discussion with problem orientation can stimulate deep learning, thereby enhancing the learning experience and help the student correlate prior knowledge acquired through the didactic lecture into actual application.[15] This methodology may help students who have a poor factual recollection.[19]
Small group discussions with the active problem-solving abilities have been experimented with the problem-based learning (PBL) around the world. Rich et al. found a significant difference in performance of students on mock patients in -PBL than traditional educational methodology in preclinical and clinical periodontics and the students rated the PBL model favorably.[20] Ghosh concluded that it was possible to have a PBL module in the form of case-oriented problem-solving tutorials coexistent with the traditional didactic lecture module in the 1st year of medical education under a conventional curriculum.[3] The feedback gains insight into the student learning preferences with respect to COSGD. It is also encouraging toward introducing more student-centered learning methods.
The limitation of the study was that more number of topics could have been covered using the COSGD method. Formative assessments after a gap of 4–6 months could have assessed the long-term retention of information. Comparing summative assessments with traditional methods can also provide substantiate evidence for recommending COSGDs in the curriculum. We also recommend inclusion of clinical postings for 1st year dental curriculum for clinical exposure. Feasibility of introducing COSGD in institutions provides a great advantage for both the teachers and the students in integrating knowledge and practice. The positive student response could influence the inclusion of COSGD in the Rajiv Gandhi University curriculum in all the disciplines of dentistry.
CONCLUSION
Case-oriented small group discussions with lectures are comparable to traditional lectures in terms of student scoring in formative assessments. However, the students showed a positive response toward COSGDs. As a teaching methodology in dental materials, case-oriented discussions can add to the effectiveness of a lecture. Small group discussions can enhance the clinical application of basic science knowledge. Students feel more comfortable in clarifying doubts and raising questions thereby motivating the student for effective learning experience.
ACKNOWLEDGMENTS
Dr. Medha Joshi Head of Quality Assurance Cell for her valuable guidance in drafting this article, Mr. Jagannath for help in statistical analysis and Dr. Kotamballi N. Chidambaramurthy, Head, Complementary and Alternative Medicine, M S Ramaiah Medical College for his valuable suggestions.
Annexure 1
Sample problem for the students:
A clinician while manipulating dental stone that was stored in the laboratory found that setting time of the stone was retarded. What could be the reason? How can it be avoided?
Teacher's guidelines for the problem:
Establish learning objectives from the problem given to each group
Problem is analyzed by the group
Group discussion on possible solutions
Identify solutions and clarify with facilitator if required
Group shares the results
Group discusses with the rest of the batch in the time allotted
Assessment of students.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Callis AN, Mccann AL, Schneiderman ED, Babler WJ, Lacy ES, Hale DS. Application of basic science to clinical problems: Traditional vs. Hybrid problem-based learning. J Dent Educ. 2010;74:1113–24. [PubMed] [Google Scholar]
- 2.Cuseo J. The empirical case against large class size: adverse effects on the teaching, learning and retention of first-year students. The Journal of Faculty Development. 2007;21:5–21. [Google Scholar]
- 3.Ghosh S. Combination of didactic lectures and case-oriented problem-solving tutorials toward better learning: Perceptions of students from a conventional medical curriculum. Adv Physiol Educ. 2007;31:193–7. doi: 10.1152/advan.00040.2006. [DOI] [PubMed] [Google Scholar]
- 4.Keeve PL, Gerhards U, Arnold W, Zimmer S, Zollner A. Job requirements compared to dental school education: Impact of a case-based learning curriculum. Gesellschaftfür Med Ausbild. 2012;29 doi: 10.3205/zma000824. Doc54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams B. Case based learning – A review of the literature: Is there scope for this educational paradigm in prehospital education? Emerg Med J. 2005;22:577–81. doi: 10.1136/emj.2004.022707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du GF, Li CZ, Shang SH, Xu XY, Chen HZ, Zhou G. Practising case-based learning in oral medicine for dental students in China. Eur J Dent Educ. 2013;17:225–8. doi: 10.1111/eje.12042. [DOI] [PubMed] [Google Scholar]
- 7.Tao L, Tang Y, Zhu MY, Zhu YQ. Application of case-based learning in clinical practice of dental students. Shanghai Kou Qiang Yi Xue. 2011;20:209–12. [PubMed] [Google Scholar]
- 8.Zhang SY, Zheng JW, Yang C, Zhang ZY, Shen GF, Zhang JZ, et al. Case-based learning in clinical courses in a Chinese college of stomatology. J Dent Educ. 2012;76:1389–92. [PubMed] [Google Scholar]
- 9.Koole S, De Wever B, Aper L, Vervaeke S, Derese A, De Bruyn H. Using online periodontal case-based discussions to synchronize theoretical and clinical undergraduate dental education. Eur J Dent Educ. 2012;16:52–8. doi: 10.1111/j.1600-0579.2011.00719.x. [DOI] [PubMed] [Google Scholar]
- 10.McKenzie CT. Dental student perceptions of case-based educational effectiveness. J Dent Educ. 2013;77:688–94. [PubMed] [Google Scholar]
- 11.Kumar V, Gadbury-Amyot CC. A case-based and team-based learning model in oral and maxillofacial radiology. J Dent Educ. 2012;76:330–7. [PubMed] [Google Scholar]
- 12.Gelula MH. Clinical discussion sessions and small groups. Surg Neurol. 1997;47:399–402. doi: 10.1016/s0090-3019(96)00342-4. [DOI] [PubMed] [Google Scholar]
- 13.Jones CE, Dyar SC, McKeever AL. Small-team active learning in an integrated pharmacokinetics course series. Am J Pharm Educ. 2012;76:153. doi: 10.5688/ajpe768153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katsuragi H. Adding problem-based learning tutorials to a traditional lecture-based curriculum: A pilot study in a dental school. Odontology. 2005;93:80–5. doi: 10.1007/s10266-005-0054-9. [DOI] [PubMed] [Google Scholar]
- 15.Botelho MG, O’Donnell D. Assessment of the use of problem-orientated, small-group discussion for learning of a fixed prosthodontic, simulation laboratory course. Br Dent J. 2001;191:630–6. doi: 10.1038/sj.bdj.4801253. [DOI] [PubMed] [Google Scholar]
- 16.Patel VL, Arocha JF, Branch T, Karlin DR. Relationship between small group problem-solving activity and lectures in health science curricula. J Dent Educ. 2004;68:1058–80. [PubMed] [Google Scholar]
- 17.Steinert Y. Student perceptions of effective small group teaching. Med Educ. 2004;38:286–93. doi: 10.1046/j.1365-2923.2004.01772.x. [DOI] [PubMed] [Google Scholar]
- 18.Tayem YI. The impact of small group case-based learning on traditional pharmacology teaching. Sultan Qaboos Univ Med J. 2013;13:115–20. doi: 10.12816/0003204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das N, Sinha S. Problem-oriented small-group discussion in the teaching of biochemistry laboratory practicals. Biochem Educ. 2000;28:154–55. [PubMed] [Google Scholar]
- 20.Rich SK, Keim RG, Shuler CF. Problem-based learning versus a traditional educational methodology: A comparison of preclinical and clinical periodontics performance. J Dent Educ. 2005;69:649–62. [PubMed] [Google Scholar]


