Abstract
Objective:
To define medical student goals in the neurology clerkship and explore the association between goal setting and student performance, clerkship satisfaction, self-directed learning (SDL), and interest in neurology.
Methods:
A 4-year prospective study of consecutive second- to fourth-year medical students rotating through a required 4-week neurology clerkship was conducted. A goal-generating cohort (first 2 years) was enrolled to describe the breadth of student-derived goals. A goal-evaluating cohort (second 2 years) was used to evaluate the frequency of goal achievement and assess associations with performance (e.g., National Board of Medical Examiners [NBME], examination), satisfaction, and SDL behaviors (both based on 5-point Likert scale).
Results:
Of 440 evaluable students, 201 were goal-generating and 239 goal-evaluating. The top 3 goals were (1) improvement in neurologic examination, (2) understanding neurologic disease, and (3) deriving a differential diagnosis. More than 90% (n = 216/239) of students reported achieving goals. Achievers reported significantly higher clerkship satisfaction (4.2 ± 0.8 vs 2.8 ± 1.0, p < 0.0001), greater interest in neurology (71% vs 35%, p = 0.001), and higher observed tendency toward SDL (4.5 ± 0.5 vs 4.1 ± 0.8, p < 0.0001). After adjusting for age and training, NBME scores were 1.7 points higher in achievers (95% confidence interval 0.1–3.2, p = 0.04).
Conclusion:
Students consistently generated similar goals for a required neurology clerkship. Goal achievers had better adjusted standardized test scores, higher satisfaction, and greater tendency toward SDL. This student-generated, goal-setting program may be particularly appealing to clinicians, educators, and researchers seeking resource-lean mechanisms to improve student experience and performance in the clinical clerkships.
Goal setting is an essential component of medical practice. Physicians and patients routinely set treatment goals, therapists and physiatrists begin rehabilitation with shared team goal setting, health care teams work to establish goals of care, and numerous practitioners use goal setting to change social and behavioral habits to improve health. Goal setting is also an important component of medical education. Goal-setting theory has influenced student, teacher, and curricular design for more than 4 decades.1 The importance of goal setting is not new to education. Learning objectives in the clerkships have long represented instructor-generated expectations and provide the basis for assessment.2,3 Student-derived goals also provide a crucial method for self-reflection, motivation, and verbalization of student expectations.4
Numerous studies have evaluated the effects of goal setting on nonmedical learners,4,5 first-year and senior medical students, and residents.6–11 Two studies evaluating goal setting in senior medical students demonstrated the importance of more specific as opposed to general goals.12,13 In medical residents, factors associated with goal attainment have included an individualized learning plan,7 resident reflection,10 coaching,9 and types of goals set.14 Despite this existing literature, few studies have focused specifically on goal setting in the clinical clerkship or in neurology. The neurology clerkship is a critical time in medical training when students experience the breadth of neurologic practice, learn to apply skills in neurologic examination, garner interest in the field, and develop lifelong learning practices. Thus, the neurology clerkship represents a critical time in medical training for blending both student-generated goals with faculty-directed expectations to ensure both competence and personalization of instruction in neurology.
To further define self-reported medical student goals in the neurology clerkship and to explore the association between goal setting and student performance, clerkship satisfaction, self-directed learning (SDL), and interest in neurology, we designed a prospective cohort study of medical student goal setting and achieving in the neurology core clerkship (NCC) at a single institution.
METHODS
All consecutive second- to fourth-year medical students rotating through the compulsory 4-week NCC from August 2010 to August 2014 were eligible for inclusion and considered evaluable if they completed initial clerkship goal setting. The primary study objectives were (1) to describe the breadth of student-derived goals for the neurology clerkship, (2) to describe the frequency of goal attainment in goal-setting students, and (3) to explore whether goal attaining is associated with higher performance, greater satisfaction, more SDL behaviors, and greater interest in neurology. To evaluate these objectives, 2 cohorts were enrolled: a goal-generating cohort and a goal-evaluating cohort.
Standard protocol approvals, registrations, and patient consents.
Institutional review board approval was sought, and this study was determined to be exempt.
Goal-generating cohort.
Students rotating through the NCC from August 2010 to August 2012 were enrolled in the goal-generating cohort and data were gathered to determine a consensus list of all student-derived goals for the NCC. Students were required to complete a baseline survey at the time of clerkship entry asking them to self-generate a list of top 3 goals for the 4-week clerkship. Responses were collected by rotation group. Goals representing similar themes were grouped and categorized according to the common topic. Goals were then ranked according to the frequency of student report. At the completion of this cohort, the 10 most frequently reported goals by proportion of the entire cohort were grouped and used for the goal-evaluating cohort.
Goal-evaluating cohort.
Students rotating through the NCC from August 2012 to August 2014 were enrolled in the goal-evaluating cohort and data on student-specific goal setting and goal achieving were gathered. Students were also required to complete a baseline survey at the time of clerkship entry. Students were asked to provide (1) demographic data on age, sex, year of training, and prior advanced degree (e.g., master's degree, doctorate degree, or other), and (2) to select 3 goals from the list of top 10 goals derived from their peers in the preceding goal-generating cohort. An option to list “other goals” was also provided but students were limited to only 3 total goals. To measure goal attainment, at clerkship completion, all students were required to complete an end-of-clerkship evaluation requiring them to rate the degree to which they agreed that they had achieved their goals (5-point Likert scale from 1 = strongly disagree to 5 = strongly agree). To assess the association between goal achieving and performance, scores on the National Board of Medical Examiners (NBME) neurology shelf examination (a nationally recognized standardized assessment of clinical knowledge) were collected. To assess the association between goal achieving and student satisfaction, students were asked to rate the following: (1) overall educational value of the clerkship (5-point Likert scale, 1 = poor to 5 = excellent), (2) interest in neurology as a potential future specialty at clerkship entry (5-point Likert scale, 1 = very unlikely to 5 = very likely), and (3) interest in neurology as a potential future specialty at clerkship end. To explore the association between personal goal achieving, student skills, and SDL behaviors, students were required to select 3 faculty or resident clinical evaluators with whom they interacted during the 4-week required clerkship. Faculty and residents were provided instructions on evaluation standards to ensure greater consistency in assessment. Evaluations included 9 questions rating students on clinical knowledge and skills including the following: basic science knowledge, clinical knowledge, data gathering, physical examination skills, patient presentation skills, problem solving, clinical judgment, future housestaff potential, and tendency to conduct SDL (5-point Likert scale from 1 = strongly disagree to 5 = strongly agree).
Statistical analysis.
Statistical analysis was performed using Stata/IC version 13.1 (2014; StataCorp, College Station, TX). For the goal-generating cohort, descriptive statistics were performed to determine the proportion of students in each rotation group, year, and in the entire cohort that reported each self-generated goal. For the goal-evaluating cohort, descriptive statistics for goals set were calculated similarly to the goal-generating cohort. Once enrolled, no students dropped out. Analysis of variance was used to compare goal reporting over each of the 4 years of study. To determine goal attainment, students rating their degree of having achieved goals as “agree” or “strongly agree” were designated as goal achievers and those rating “strongly disagree,” “disagree,” or “neutral” were designated as nonachievers. Unpaired Student t tests were used to compare continuous variables between achievers and nonachievers, and Fisher exact tests and analysis of variance were used for categorical variables. When missing, variables were excluded from analysis; goal achievement was available for all. Given the exploratory nature of this analysis, minimal educationally significant differences were not defined and results should be considered descriptive. Simple linear regression was used to determine variables that were significantly associated with differences in NBME shelf examination performance (p < 0.10). These variables were then included in the multiple linear regression model to assess the adjusted association between achieving goals (by 5-point Likert scale) and shelf score.
RESULTS
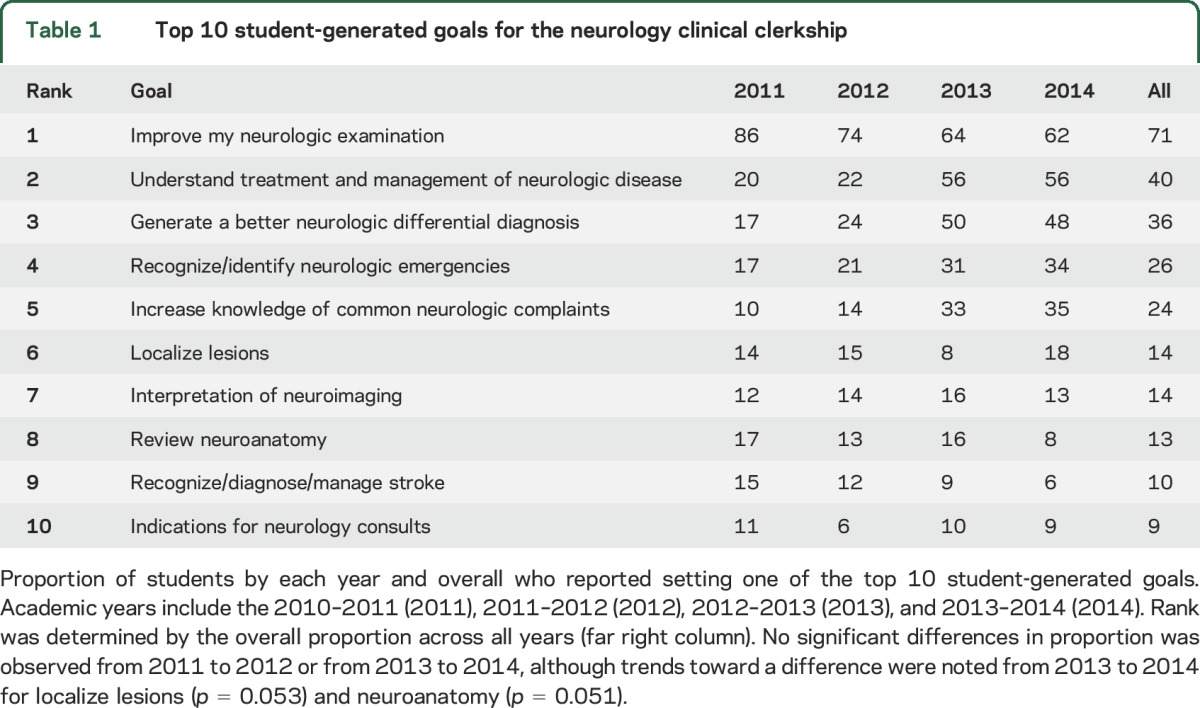
A total of 440 evaluable students were enrolled over the 4 years (11 students did not set initial clerkship goals and were not considered evaluable): 201 in the goal-generating cohort and 239 in the goal-evaluating cohort. The 3 most commonly reported goals included improvement in the neurologic examination, understanding of the management of neurologic disease, and generation of a neurologic differential diagnosis (table 1). The breadth of goals reported in the goal-generating cohort was large and ranged from specific goals such as “learn how to handle stroke” and “migraine treatment and prognosis” to more general goals such as “practice oral presentation skills” and “understand duties of a neurologist” (table e-1 on the Neurology® Web site at Neurology.org). Despite this range, the scope of commonly reported goals remained highly consistent over time with the same top 3 goals being listed in each of the 4 years of study.
Table 1.
Top 10 student-generated goals for the neurology clinical clerkship
Of the 239 students enrolled in the goal-evaluating cohort, 90.4% (n = 216) agreed or strongly agreed that they achieved their 3 goals during the clerkship (e.g., goal achievers) while 9.6% (n = 23) disagreed or reported neutral rating (e.g., nonachievers). Age, year of training, sex, and proportion with an advanced degree were not statistically different between achievers and nonachievers (table 2). Student satisfaction with the educational value of the clerkship was significantly higher in achievers than in nonachievers (table 2, mean rating 4.2 ± 0.8 vs 2.8 ± 1.0, p < 0.0001). While self-report of interest in neurology at clerkship entry was low and not different between the groups (mean rating 2.5 ± 0.9 vs 2.2 ± 1.1, p = 0.17), interest in neurology at clerkship end was significantly higher in achievers (3.5 ± 1.1) compared to nonachievers (2.3 ± 1.3, p < 0.0001), and the proportion who reported an improvement in their interest in neurology (any higher rating at clerkship end) was also higher in the achievers (71% vs 35%, p = 0.001). Interest in neurology at clerkship end strongly correlated with overall educational value of the clerkship (r = 0.6238, p < 0.0001).
Table 2.
Comparison of student characteristics, performance, and satisfaction between goal achievers and nonachievers
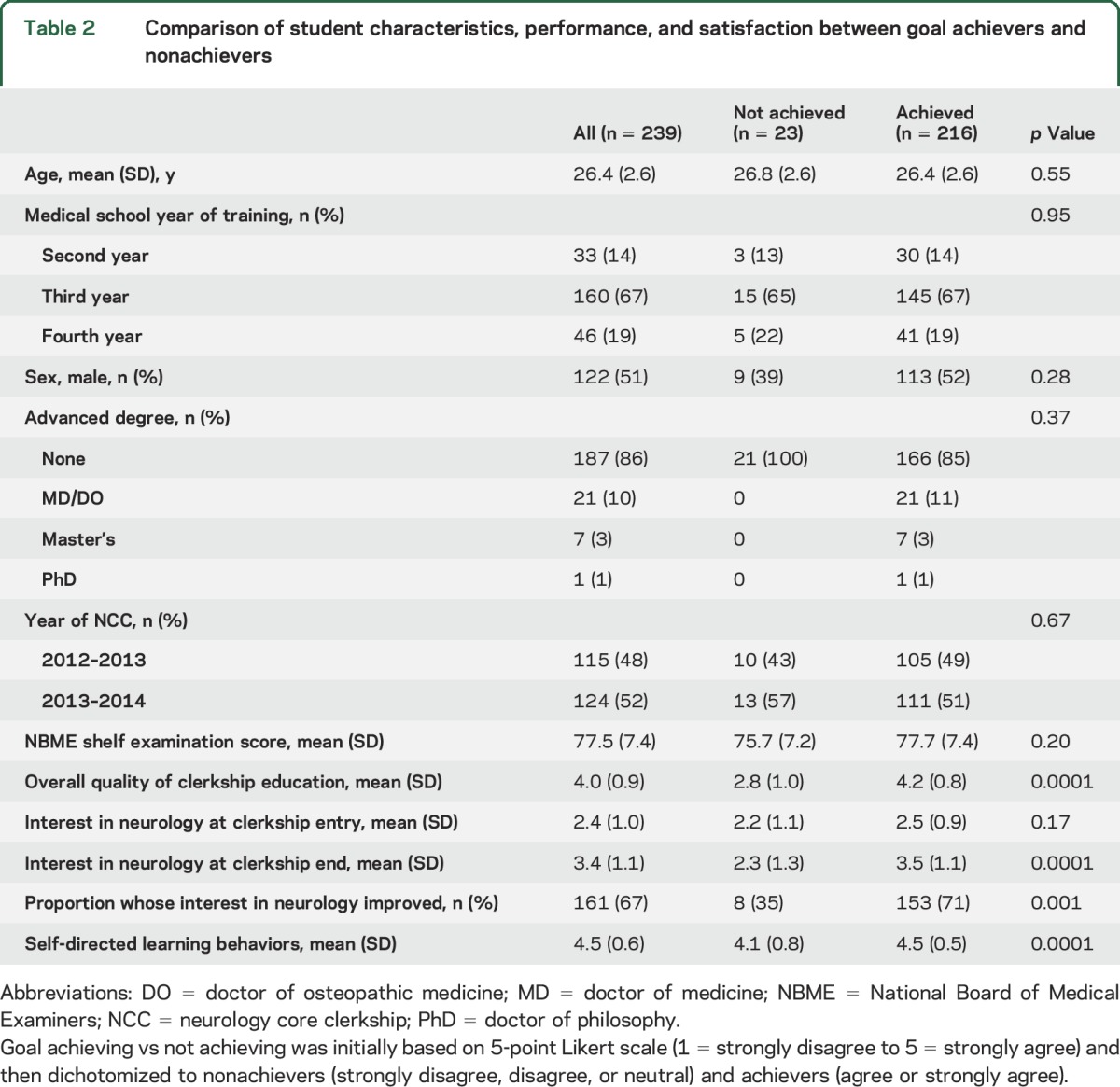
Resident and faculty rating of students' tendency toward SDL was statistically higher in goal achievers (4.5 ± 0.5) compared to nonachievers (4.1 ± 0.8, p < 0.0001, table 2) despite the fact that the evaluators (e.g., resident and faculty) and those being evaluated (e.g., students) were not aware of the other's rating. Faculty and resident evaluation of basic and clinical knowledge, data gathering, examination skills, problem solving, clinical judgment, and future housestaff potential were high and not significantly different between achievers and nonachievers (table e-2A). There was a trend toward higher physical examination skills in the goal achievers (4.2 ± 0.6 vs 3.9 ± 0.6, p = 0.058) but no significant differences in the mean clinical evaluation rating of specific skills between those who did and did not set a goal encompassing that skill. For example, students who set the goal of improving physical examination skills did not have higher clinical evaluation scores for physical examination skills (table e-2B).
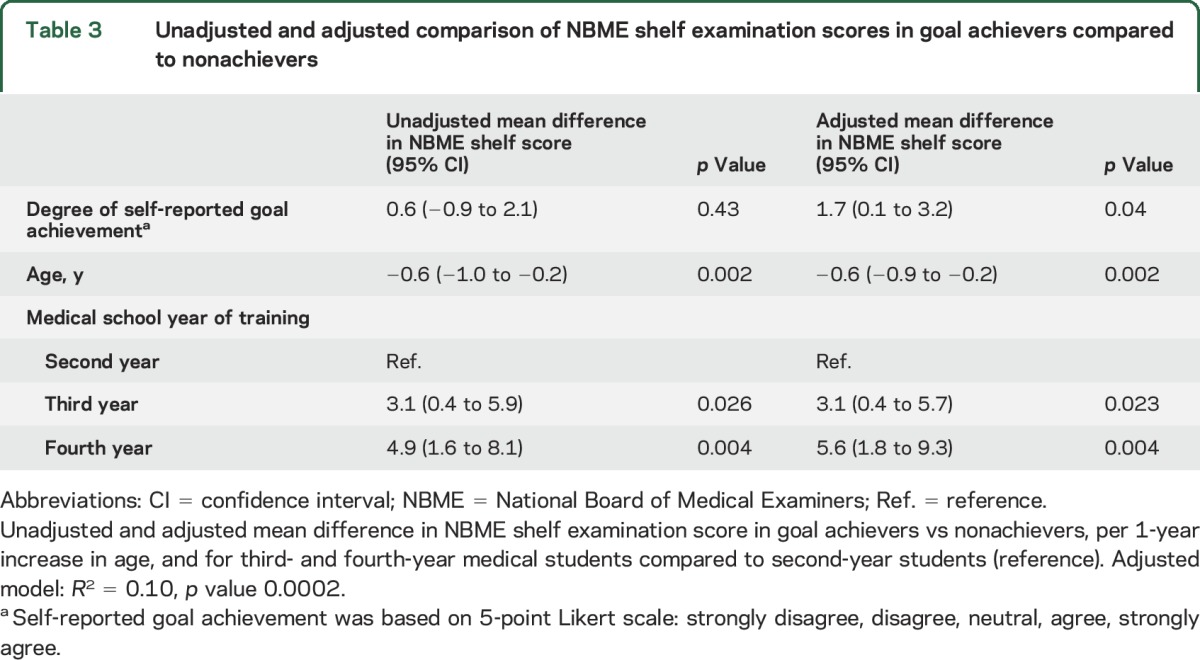
There was no significant difference in mean NBME shelf examination scores between goal achievers (mean 77.7, 95% confidence interval [CI] 76.8–78.7) and nonachievers (75.7, 72.6–78.6, p = 0.20). Results of the unadjusted linear regression of NBME shelf examination score revealed that younger age and higher level of medical school training were significantly associated with higher shelf scores (table 3). Self-reported goal achievement was not associated with higher NBME shelf examination scores (β = −0.6, 95% CI −0.9 to 2.1, p = 0.43). Rotation sequence (i.e., number of prior clerkships) and sex, which have been associated with differences in standardized examination scores previously, were also not significantly associated with differences in examination scores in this study (rotation number: β = −0.13, 95% CI −0.46 to 0.20, p = 0.43; male sex: β = −0.20, 95% CI −2.1 to 1.7, p = 0.84). After adjusting for age and level of training (established factors shown to be associated with standardized testing performance),15–19 higher self-reported goal achievement was significantly associated with a 1.7-point-higher mean NBME shelf examination score (β = −1.7, 95% CI 0.1–3.2, p = 0.04).
Table 3.
Unadjusted and adjusted comparison of NBME shelf examination scores in goal achievers compared to nonachievers
DISCUSSION
In this study, we comprehensively define the 10 most common student-generated goals for the neurology clerkship derived from more than 400 medical students rotating through this mandatory clinical experience at a single institution. The scope, nature, and relative frequencies of these goals remained highly consistent over the 4 years of study with the same top 3 goals represented in each year (i.e., improvement in the neurologic examination, understanding of the treatment and management of neurologic disease, and generation of a neurologic differential diagnosis). More than 90% of students reported achieving their goals during the 4-week rotation. Students who did not report attaining their goals at clerkship end had poorer satisfaction with the clerkship, less interest in neurology as a future career, and fewer observed SDL behaviors. NBME shelf examination scores were not associated with self-reported goal achievement in our unadjusted model. After adjusting for 2 factors that have been consistently associated with standardized testing performance in multiple studies,15–19 significantly higher examination scores were found in those reporting greater goal attainment.
According to the goal-setting theory by Locke and Latham,20 establishing specific high-level goals leads to more internal motivation, greater personal investment, improved satisfaction, and a higher level of performance. In short, goal setting actively engages students in the responsibility for their own learning. According to Locke and Latham,20 the association between higher performance and goal setting involves 4 underlying principles or mechanisms: (1) that greater effort is required to achieve higher goals, which improves studying, learning, and thereby performance; (2) that specific goals direct attention toward task-relevant activity limiting irrelevant energy expenditure and improving task success; (3) that goals motivate one to maximize existing abilities and capitalize on personal skills; and (4) that goals also provide an impetus to seek out new knowledge and apply it in a task-relevant manner. Of note, goal setting alone may be insufficient, and studies suggest that committing to achieving one's goals is necessary to improve performance.21 Goal attainment requires students to construct a plan and take an active role in their educational path as opposed to assuming static absorption and memorization of instructor-derived facts.
In medicine, where the logarithmic expansion of knowledge requires ongoing self-assessment and awareness of potential gaps in knowledge and core competencies, lifelong learning and the ability to develop and set high-level goals to close these gaps are crucial. Lifelong learning is a fundamental aspect of being a medical professional. Studies evaluating skills required for optimal lifelong learning emphasize the concept of the “self-regulated learner,” one who has the ability to proactively monitor learning needs, set appropriate academic goals, and strive for successful achievement.22 According to this theory, learners with greater capacity to set, monitor, and assess academic goals are more likely to be self-regulated. In the current study, students with a greater observed tendency to self-direct their learning were also more likely to report goal achievement and perform at a higher level. Those observed to be less self-directed were also less likely to report achieving goals and showed lower performance. While a standardized measure of SDL was not used and a causal link cannot be drawn from the data presented here, differences in the ability to self-direct one's learning may be an important component of goal setting and achieving. Future studies will further define the degree to which differences in SDL, student learning styles, study strategies, motivation to learn, and personality traits influence attainment of goals and performance.
The association between greater satisfaction with the neurology clerkship and greater interest in neurology at clerkship end are important findings of this study. Even though most US medical schools now require neurology as a core clerkship, this trend has only been a recent one and the average length of neurology clerkships (2–4 weeks) remains significantly shorter than most other core clerkships (typically 6–8 weeks), leaving less time for educational and clinical exposure. In contrast to other core clerkships (e.g., internal medicine, surgery, pediatrics), only a small proportion of medical students rotating through our clerkship decide to pursue neurology as a primary residency. Thus, in comparison to a core clerkship that serves as the touchstone for a student's future specialty, a neurology clerkship may encounter a learner who understandably feels less invested with the clinical experience. The strong correlation between the overall rating of the education value of the clerkship and the interest in neurology at clerkship end suggests that such exposure may be important for garnering enthusiasm for evaluating patients with neurologic disease, which is pervasive in our rapidly expanding aging population. While these data cannot assess causality or exclude that differences in student barometers of self-rating may have driven some of this result (i.e., greater tendency toward high self-assessment rating in all domains for the goal achievers compared to nonachievers), we must note that interest in neurology was not different between goal achievers and nonachievers at baseline. Of note, considerable literature has questioned whether students can reliably self-assess their performance, and recent studies have highlighted self-monitoring (i.e., continuous monitoring of performance during active learning) as a more reliable measure than self-assessment (i.e., summative self-reflection at activity completion).23,24 Nevertheless, studies also show that despite these concerns regarding self-assessment, student perceptions and opinions critically influence generation of learning goals.25
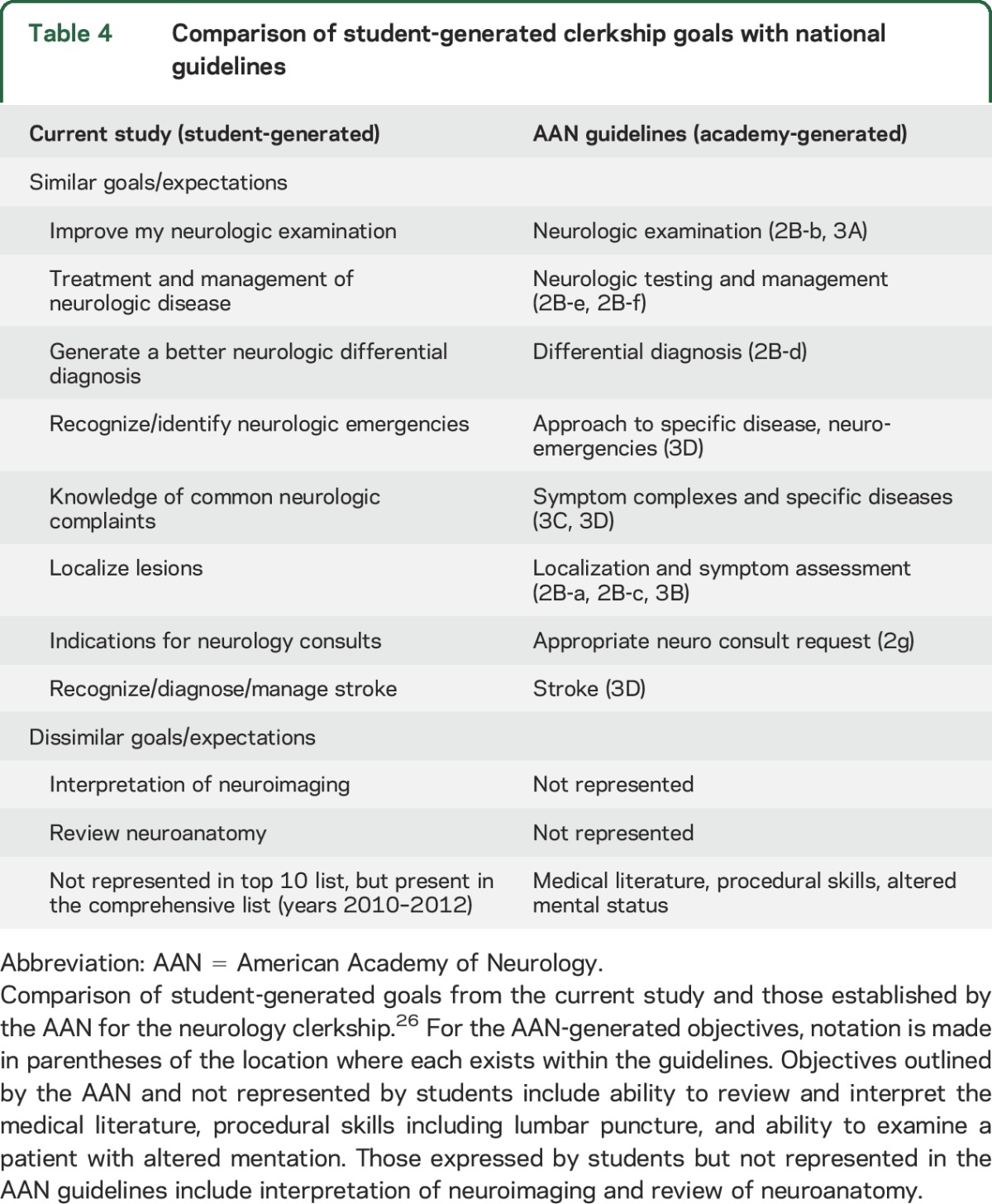
Of note, the self-generated goals reported by students in this study are strikingly similar to national guidelines established for the neurology clerkship (table 4).26 Of the primary objectives and key content outlined by the American Academy of Neurology Consortium of Neurology Clerkship Directors, 8 critical content areas overlapped between students and clerkship directors, while only a limited few did not. Developing skills for approaching medical literature, lumbar puncture skills, and the examination of patients with altered mental status were not represented in the top 10 student goals but were included in national guidelines. Interpretation of neuroimaging and review of neuroanatomy were strongly important to students but not as highly represented in the national guideline. Other than these few discrepancies, the majority of core objectives for the clerkship (e.g., neurologic examination, management of neurologic disease, localization, differential diagnosis, and common neurologic complaints) were similarly emphasized by both groups. While specific to the neurology clerkship at our institution, this finding if reproduced in other areas would suggest that substantial overlap exists between student goals and clinical educator objectives. Given that most clerkships have standard opportunities at clerkship entry (i.e., orientation) and clerkship end (i.e., end of clerkship examination) to engage students in goal setting and monitoring, this approach was easily integrated into our clerkship without additional resource requirements. Prior studies have strongly supported the importance of ongoing monitoring of goals over time, which can present challenges to feasibility and resource allocation. However, engaging residents and faculty with whom these students rotate in probing student goals has proven feasible in other arenas.4 Given the importance of internal motivation, self-generated goals may offer a resource-lean method for leveraging student drive while maintaining integrity of educational objectives for learning.
Table 4.
Comparison of student-generated clerkship goals with national guidelines
Goal-setting programs that complement existing curricula may prove particularly attractive to clinical educators. Given the growing demands on faculty time, gradual reduction in institutional resource capacity, growing medical school costs, and reduction in budgets for medical education, a teaching strategy that enhances the student experience and requires very little demand on already limited resources is appealing. In this study, while goal achievers were more likely to report greater clerkship satisfaction, more interest in neurology, and have higher observed SDL behaviors, this did not necessarily translate into greater knowledge as assessed by unadjusted NBME shelf examination scores. In our clerkship, the NBME shelf examination comprises 25% of the clerkship grade and substantial educational consequences exist for students who fail repeatedly. This substantial intrinsic source of motivation may confound the ability to statistically resolve educationally meaningful performance outcomes. After adjusting for factors known to be associated with standardized testing performance, goal achieving was significantly associated with higher performance. These data underscore the complexity of standardized knowledge examinations, the inherent motivation to perform highly on “high stakes” examinations, and the importance of a strong curricular environment (i.e., lectures, clinical rotations, etc.). While resource-lean goal setting and monitoring alone may not be sufficient to improve knowledge acquisition, these data support this activity as one component of an optimal clerkship experience. Further studies to identify, predict, and potentially mentor students who demonstrate systematic failures to set and achieve goals across clerkships are still needed.
This study does have limitations. These data were generated from a single clerkship at a single institution. Broader generalization requires further study. Goal achievement in this study was determined by student self-report. Prior studies have suggested that in certain domains, student self-report may lack reliability.27,28 We are not aware of data informing the accuracy of medical student assessment of goal achievement. Future study would include additional external measures of attaining goals including competence in goal-relevant tasks or achievement of goal-related milestones. This study was not designed to determine the effects of serial goal setting or to refine students' goal-setting abilities. While these are important aspects of goal-setting abilities in medical education, the data presented in this study do not inform these areas of goal setting.
CONCLUSION
We describe a highly consistent top 10 list of student-generated goals for a required neurology clerkship at a single institution and demonstrate significantly higher adjusted NBME shelf examination scores, clerkship satisfaction, and observed SDL behaviors in students who reported achieving their goals. This program provided students with an active role in their education while maintaining the academic integrity of institutional and national guidelines for the clerkship. Given the lack of substantial cost, time, and resources required to conduct such a program, this strategy may be particularly appealing to medical educators and education researchers seeking resource-lean mechanisms to improve student experience and performance in the clinical clerkships.
Supplementary Material
GLOSSARY
- CI
confidence interval
- NBME
National Board of Medical Examiners
- NCC
neurology core clerkship
- SDL
self-directed learning
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Dr. Strowd participated in the study design, analysis and interpretation of data, the drafting, revising, and final approval of this manuscript. Dr. Salas participated in the study concept and design, analysis and interpretation of data, the drafting, revising, and final approval of this manuscript. Ms. Cruz participated in the acquisition of data, revising and final approval of this manuscript. Dr. Gamaldo participated in the study concept and design, analysis and interpretation of data, the drafting, revising, and final approval of this manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
R. Strowd has received grant funding from the American Academy of Neurology to support fellowship training and a project unrelated to the current study. Dr. Strowd serves as associated deputy editor for the Resident & Fellow Section of Neurology. R. Salas has entered into an agreement with UpToDate, Inc., to author articles and receive payment and/or royalties for said articles. T. Cruz reports no disclosures relevant to the manuscript. C. Gamaldo has entered into an agreement with UpToDate, Inc., to author articles and receive payment and/or royalties for said articles. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: a 35-year odyssey. Am Psychol 2002;57:705–717. [DOI] [PubMed] [Google Scholar]
- 2.Burke MJ, Brodkey AC. Trends in undergraduate medical education: clinical clerkship learning objectives. Acad Psychiatry 2006;30:158–165. [DOI] [PubMed] [Google Scholar]
- 3.Pangaro L, Bachicha J, Brodkey A, et al. Expectations of and for clerkship directors: a collaborative statement from the Alliance for Clinical Education. Teach Learn Med 2003;15:217–222. [DOI] [PubMed] [Google Scholar]
- 4.Morisano D, Hirsh JB, Peterson JB, Pihl RO, Shore BM. Setting, elaborating, and reflecting on personal goals improves academic performance. J Appl Psychol 2010;95:255–264. [DOI] [PubMed] [Google Scholar]
- 5.Emmons RA, Diener E. A goal-affect analysis of everyday situational choices. J Res Pers 1986;20:309–326. [Google Scholar]
- 6.Caverzagie KJ, Shea JA, Kogan JR. Resident identification of learning objectives after performing self-assessment based upon the ACGME core competencies. J Gen Intern Med 2008;23:1024–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li ST, Tancredi DJ, Co JP, West DC. Factors associated with successful self-directed learning using individualized learning plans during pediatric residency. Acad Pediatr 2010;10:124–130. [DOI] [PubMed] [Google Scholar]
- 8.Lockspeiser TM, Schmitter PA, Lane JL, Hanson JL, Rosenberg AA, Park YS. Assessing residents' written learning goals and goal writing skill. Acad Med 2013;88:1558–1563. [DOI] [PubMed] [Google Scholar]
- 9.George P, Reis S, Dobson M, Nothnagle M. Using a learning coach to develop family medicine residents' goal-setting and reflection skills. J Grad Med Educ 2013;5:289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toy EC, Harms KP, Morris RK, Simmons JR, Kaplan AL, Ownby AR. The effect of monthly resident reflection on achieving rotation goals. Teach Learn Med 2009;21:15–19. [DOI] [PubMed] [Google Scholar]
- 11.Hanley K, Zabar S, Charap J, et al. Self-assessment and goal-setting is associated with an improvement in interviewing skills. Med Educ Online 2014;19:24407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang A, Chou CL, Teherani A, Hauer KE. Clinical skills-related learning goals of senior medical students after performance feedback. Med Educ 2011;45:878–885. [DOI] [PubMed] [Google Scholar]
- 13.Stallworth LE, Palladino C, Leggio LE, Hudson VL, Elam RE, Richardson DS. Senior student goal setting during subinternship: a mixed-methods study. Teach Learn Med 2014;26:225–229. [DOI] [PubMed] [Google Scholar]
- 14.Li S, Paterniti D, Tancredi D, Co J, West D. Is residents' progress on individualized learning plans related to the type of learning goal set? Acad Med 2011;86:1293–1299. [DOI] [PubMed] [Google Scholar]
- 15.Ouyang W, Cuddy MM, Swanson DB. US medical student performance on the NBME subject examination in internal medicine: do clerkship sequence and clerkship length matter? J Gen Intern Med 2015;30:1307–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mercer A, Crotty B, Alldridge L, Le L, Vele V. GAMSAT: A 10-year retrospective overview, with detailed analysis of candidates' performance in 2014. BMC Med Educ 2015;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andriole DA, Jeffe DB. A national cohort study of U.S. Medical school students who initially failed step 1 of the United States medical licensing examination. Acad Med 2012;87:529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kleshinski J, Khuder SA, Shapiro JI, Gold JP. Impact of preadmission variables on USMLE step 1 and step 2 performance. Adv Heal Sci Educ 2009;14:69–78. [DOI] [PubMed] [Google Scholar]
- 19.Ogunyemi D, Taylor-Harris DS. Factors that correlate with the U.S. Medical Licensure Examination step-2 scores in a diverse medical student population. J Natl Med Assoc 2005;97:1258–1262. [PMC free article] [PubMed] [Google Scholar]
- 20.Locke EA, Latham GP. New directions in goal-setting theory. Curr Dir Psychol Sci 2006;15:265–268. [Google Scholar]
- 21.Akama K. Relations among self-efficacy, goal setting, and metacognitive experiences in problem-solving. Pschological Rep 2006;98:895–907. [DOI] [PubMed] [Google Scholar]
- 22.Burman NJ, Boscardin CK, Van Schaik SM. Career-long learning: relationship between cognitive and metacognitive skills. Med Teach 2014;36:715–723. [DOI] [PubMed] [Google Scholar]
- 23.McConnell MM, Regehr G, Wood TJ, Eva KW. Self-monitoring and its relationship to medical knowledge. Adv Heal Sci Educ 2012;17:311–323. [DOI] [PubMed] [Google Scholar]
- 24.Eva KW, Regehr G. Exploring the divergence between self-assessment and self-monitoring. Adv Heal Sci Educ 2011;16:311–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eva KW, Munoz J, Hanson MD, Walsh A, Wakefield J. Which factors, personal or external, most influence students' generation of learning goals? Acad Med 2010;85(10 suppl):S102–S105. [DOI] [PubMed] [Google Scholar]
- 26.Gelb DJ, Gunderson CH, Henry KA, Kirshner HS, Józefowicz RF. The neurology clerkship core curriculum. Neurology 2002;58:849–852. [DOI] [PubMed] [Google Scholar]
- 27.Lai NM, Teng CL. Self-perceived competence correlates poorly with objectively measured competence in evidence based medicine among medical students. BMC Med Educ 2011;11:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Woolliscroft JO, TenHaken J, Smith J, Calhoun JG. Medical students' clinical self-assessments: comparisons with external measures of performance and the students' self-assessments of overall performance and effort. Acad Med 1993;68:285–294. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


