Abstract
Background
Frequent premature ventricular contractions (PVC) have been associated with PVC-induced cardiomyopathy (CM) in some patients.
Objective
Understand the cardiac consequences of different PVC burden and minimum burden required to induce LV dysfunction.
Methods
RV apical PVCs at a coupling interval of 240ms were introduced at different PVC burden in 9 mongrel canines. A stepwise increase in PVC burden was implemented every 8 weeks from 0% (baseline), 7%, 14%, 25%, 33% to 50% using our premature pacing algorithm. Echocardiogram and 24-hr Holter were obtained at 4- and 8-week period at each PVC burden with a single blinded reader assessing all echocardiographic parameters including speckle tracking imaging (GE EchoPAC). CM was defined as LVEF < 50% or a decrease >10% points. IL-6 and pro-BNP levels were obtained at the end of each PVC burden.
Results
LVEF±SD (mean heart rate ± SD) for 0%, 7%, 14%, 33%, and 50% at 8 weeks for each PVC burden were 57±2.9% (85±13bpm); 54.4±3% (81±10bpm); 53.3±5% (77±12bpm); 51.1±4.2% (79±14bpm); 47.7±3.8% (80±14bpm); 44.7±1.9% (157±43bpm). PVC-induced CM was present in 11.1%, 44.4%, and 100% of animals with 25%, 33% and 50% PVC burden, respectively. E/A ratio and radial strain decreased while LA size increased beyond 33% PVC burden. No changes in pro-BNP and IL-6 levels were noted at any PVC burden.
Conclusion
LV systolic function (LVEF, and radial strain) declined linearly as PVC burden increased. PVC-induced CM developed in some canines with 25% and 33% PVC burden, but developed in all animals with 50% PVC burden.
Keywords: Premature ventricular contractions, LV dysfunction, cardiomyopathy, PVC-induced Cardiomyopathy
Introduction
Frequent premature ventricular contractions (PVCs) have been associated with an increased risk of sudden cardiac death (SCD) and have been identified as a reversible cause of non-ischemic cardiomyopathy (CM), referred to as a PVC-induced CM1-5. Although, radiofrequency ablation and antiarrhythmic drugs are accepted strategies to reverse LV dysfunction due to PVCs1, 3-7, the minimum burden, origin (LV, RV, outflow, endocardial, epicardial) and coupling interval of PVCs required to impair LV function are unknown8. The cardiac consequences of different PVC burdens and the minimum burden required to induce LV dysfunction or PVC-induced CM are important but challenging questions to answer because of significant PVC variability in the clinical setting9.
Using our unique premature pacing algorithm2, we sought to understand the progression of echocardiographic changes associated with incremental PVC burden (7%, 14%, 25%, 33% and 50% PVC burden) and determine the minimum PVC burden required to induce LV systolic dysfunction in our canine model.
Methods
A left thoracotomy was performed in 9 canines to implant an RV apical epicardial pacing lead and modified experimental device (St. Jude Medical, Inc., Sylamar, CA) with our premature pacing algorithm2. All animals participated in a baseline 4 to 6-week observation period (without PVCs, disabled premature pacing algorithm) during which they had a baseline echocardiogram at the beginning and end of this period. In addition, 24-hour Holter, pro-BNP and IL-6 serum levels were obtained at the end of baseline period. After this baseline period, all 9 animals were followed by five 8-week periods in which the PVC burden was increased in a stepwise fashion, from 7%, 14%, 25%, 33% and 50%, without interruption of PVCs between different burdens (Supplemental Figure 1). All PVCs originated from the RV apex with a coupling interval of 240ms, regardless of burden.
Holter monitors
A 24-hr Holter (GE SEER Light) was obtained within the 8-week period of each PVC burden to assess average heart rate, PVC burden and PVC count using MARS GE software (General Electric, Fairfield, CT, USA).
Echocardiographic evaluation
Echocardiograms (GE Vivid 7) were repeated at 4 and 8 weeks after initiation of each PVC increment. PVC burden protocol was concluded after completion of all 5 different PVC burdens (46 weeks total). To assess the chronic effects of frequent PVCs, the echocardiogram was performed at least 10 minutes after disabling the pacing algorithm (PVCs absent). PVC-induced CM was defined as a LVEF < 50% or LVEF drop >10% points.
Echocardiographic images were obtained (5MHz probe GE Vivid-7, Vingmed General Electric, Fairfield, CT, USA) following the American Society of Echocardiography guidelines10. LV function was assessed by LVEF (Simpson's formula), fractional shortening (FS), LV endsystolic and diastolic dimensions (LVESD, LVEDD), LV thickness, left atrial (LA) size, mitral valve (MV) function, and LV compliance (E/A ratio)10. Abnormal LV compliance (diastolic dysfunction) was defined as E/A ratio < 111. Speckle-tracking analysis was performed offline with an EchoPAC workstation (General Electric, USA). A short-axis (mid LV at level of papillary muscles) echocardiographic view was used to obtain radial and circumferential strain. Finally, LV dyssynchrony was assessed by the dispersion of QRS-to-peak strain (ms) between 6 different LV segments (earliest – last QRS-to-peak strain). All echocardiographic analysis was performed by a single reader blinded to the different PVC burdens.
Pro-Brain natriuretic peptide (BNP) and Interleukin-6 (IL-6) levels
Blood samples were obtained at baseline and at the end of each 8-week period for each incremental step of PVC burden without interruption of PVCs (premature pacing algorithm remained active). Blood tubes were spun to obtain serum and plasma, immediately stored at −73°C until the sample was analyzed. Pro-BNP and IL-6 levels were measured using canine-specific enzyme-linked immunosorbent assays (ELISA) (MyBioSource, Inc.). Samples were analyzed in at least triplicate (n=3-6) in a 96 well plate format and absorbance data collected via plate reader (Tecan).
All procedures were approved by the McGuire Institutional Animal Care and Use Committee (IACUC) in accordance with USDA Animal Welfare Act Regulations and Standards.
Statistical analysis
All data is reported as the mean + SD. The actual percentage of PVCs was calculated using a repeated measures logistic regression model. This method controls for any intra-individual variability found in the results. The estimated proportion of PVCs and associated 95% confidence intervals (CIs) were calculated for each PVC burden level. The mean number of PVCs per day and heart rate was measured with a repeated measures ANOVA; associated 95% CIs were also calculated.
The change in LVEF between different PVC burdens was compared using repeated measures ANOVA. This model included a fixed effect for time, which had a unique PVC burden for each time point as well as a random effect to account for relationship within each animal. Separate repeated measure ANOVA models were fit for each of the outcomes using the baseline and 8-week observation for each PVC burden level (Table 1). Using these models, each PVC burden level (7%, 14%, 25%, 33%, 50%) was compared to baseline (0%) at the Bonferroni-corrected Type-I error rate of 0.01 (0.05/5). No formal analysis was made for the degree of mitral regurgitation (MR) due to numerical convergence issues; summaries of the different degrees of MR for each PVC burden level were presented instead. Statistical analysis was performed using SAS/STAT® Software (SAS Institute, Inc. Cary, NC).
Table 1.
Holter data at each predicted PVC burden.
| Anticipated PVC burden | ||||||
|---|---|---|---|---|---|---|
| Holter Dataa | 0% | 7% | 14% | 25% | 33% | 50% |
| Actual PVC Burden (%) | 0.018 (0.016, 0.021) | 7.8 (7.5, 8.1) | 14.9 (14.5, 15.4) | 25.2 (24.5,25.9) | 32.8 (32.0, 33.7) | 49.5 (28.6, 50.5) |
| #PVC / day | 22 (0, 64) | 9,000 (7K, 11K) | 17,000 (14K, 19K) | 33.000 (30K, 36K) | 45,000 (42K, 48K) | 76,000 (71K, 82K) |
| Heart Rate (bpm) | 85 (71, 99) | 81 (67, 95) | 77 (62, 91) | 79 (65, 93) | 82 (67, 96) | 157 (143, 171) |
Estimated percentages (Actual PVC Burden) and means (Number of PVCs per day and heart rate) over the predicted PVC burden levels. #PVC/day = Number of PVCs per day.
K Estimates are given in the thousands (×1000).
Results
24-hour Holter
PVC burden and count, and mean heart rate (HR) are summarized in Table 1. Representative ECGs of different PVC burdens in a single animal are shown in Supplemental Figure 2. The actual PVC burden was similar to the programmed or desired PVC burden. The HR appeared to be fairly consistent across the different PVC burden, except for the 50% PVC burden, where the HR increased dramatically.
Echocardiogram
PVC-induced CM (drop on LVEF > 10% points or LVEF < 50%) was absent in all animals after 8-week exposure of 7% and 14% PVC burden. PVC-induced CM was present in 1/9 (11.1%), 4/9 (44%), and 9/9 (100%) of animals with 25%, 33% and 50% PVC burden, respectively. For the same PVC burden, severity of PVC-induced CM did not change significantly between 4 and 8 weeks.
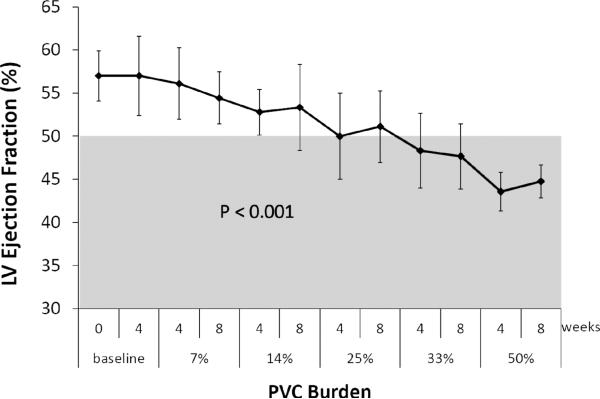
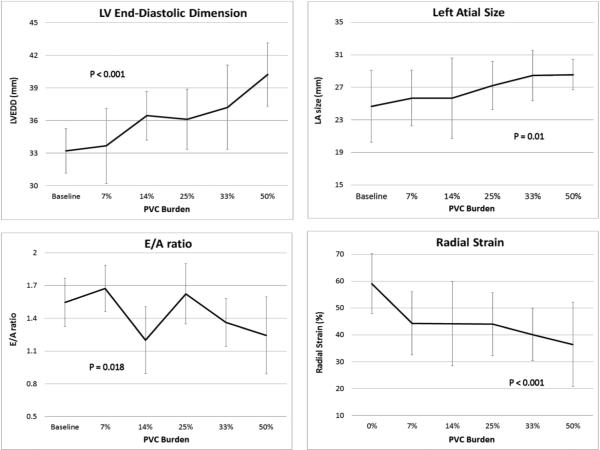
The mean 8-week echocardiographic parameters are displayed in Table 2. The change in LVEF (P<0.001), LVEDD (P<0.001), E/A ratio (P=0.018), LA size (P=0.011), radial and circumferential strain (P<0.001 and P=0.025, respectively) demonstrated significant differences between different PVC burden levels. No differences were observed between the 4- and 8-week observation points for any of the echocardiographic parameters (P>0.05, Supplemental Table 1). As the predicted PVC burden increased, changes in the LVEF, LVEDD, E/A ratio, LA size and radial strain were observed (Figure 1 and 2). Compared to baseline, significant differences in the LVEF and LVEDD were observed starting at 14% PVC and continued throughout subsequent PVC burden until 50%. A similar pattern was observed for E/A ratio, LA size, and radial stain, but the significant differences began at 33% PVC burden. There was no significant difference in LV circumferential strain until PVC burden >33%. No statistical differences in LV hypertrophy (posterior and septal wall thickness) and LV dyssynchrony (QRS-to-peak radial strain) were observed between different PVC burdens.
Table 2.
Echocardiographic parameters (mean ± SD) after 8 weeks for each PVC burden (4-week parameters can be seen in Supplemental Table 1).
| Baseline | 7% | 14% | 25% | 33% | 50% | P Value† | |
|---|---|---|---|---|---|---|---|
| LVEF (%) | 57 ± 2.9 | 54.4 ± 3.0‡ | 53.3 ± 5.0‡ | 51.1 ± 4.2‡ | 47.7 ± 3.8‡ | 44.8 ± 1.9‡ | <0.001 |
| FS (%) | 33.1 ± 4.5 | 30.0 ± 4.0 | 30.9 ± 4.1 | 29.0 ± 4.8‡ | 25.7 ± 4.2‡ | 24.3 ± 3.0‡ | <0.001 |
| LVEDD (mm) | 32.7 ± 2.6 | 33.7 ± 3.5‡ | 36.4 ± 2.2‡ | 36.1 ± 2.8‡ | 37.2 ± 3.9‡ | 40.2 ± 2.9‡ | <0.001 |
| LA Size (mm) | 24.6 ± 3.0 | 25.7 ± 3.4 | 25.7 ± 4.9 | 27.2 ± 2.9 | 28.4 ± 3.1‡ | 28.6 ± 1.9‡ | 0.011 |
| PW (mm) | 9.1 ± 1.1 | 9.8 ± 1.3 | 9.8 ± 1.1 | 9.2 ± 1.0 | 9.1 ± 1.2 | 9.3 ± 1.3 | NS |
| SW (mm) | 10.4 ± 1.3 | 10.3 ± 0.9 | 10.0 ± 1.1 | 9.7 ± 0.7 | 9.9 ± 1.1 | 9.3 ± 0.7 | NS |
| E/A ratio | 1.7 ± 0.3 | 1.7 ± 0.2 | 1.2 ± 0.3 | 1.6 ± 0.3 | 1.4 ± 0.2‡ | 1.2 ± 0.4‡ | 0.018 |
| MR grade | 0 – trace | 0 – trace | 0 – trace | Trace | Trace - 1+ | Trace - 1+ | - |
| Radial strain | 59 ± 11.2 | 44.3 ± 11.8‡ | 44.1 ± 15.6‡ | 44 ± 11.7‡ | 40.1 ± 9.7‡ | 36.4 ± 15.7‡ | <0.001 |
| Circumf. Strain | −18.1 ± 9 | −16.9 ± 4.7 | −18.4 ± 5.7 | −15.6 ± 7.3 | −16.2 ± 5.3 | −13.8 ± 6.7‡ | 0.025 |
| QRS-to-peak strain | 32.0 ± 21.5 | 39.1 ± 34.7 | 47.8 ± 34.3 | 46.2 ± 28.1 | 69.0 ± 47.3 | 66.2 ± 41.6 | NS |
P value, repeated measures one-way ANOVA;
P-values correspond to a test that at least one of the means differs from another.
P<0.01 when compared to baseline (0%).
LVEDD, LV end-diastolic dimension; PW, posterior wall thickness; SW, septal wall thickness; MR, mitral regurgitation (grade 0 – 3+); Circumf, circumferential.
Figure 1.
Progression of LV ejection fraction after 4 and 8 weeks of a progressive incremental PVC burden starting from 0% (baseline) to 7, 14, 24, 33 and 50%. P value, repeated measures one-way ANOVA.
Figure 2.
Estimated means of LVEDD, LA size, E/A ratio, and strain that showed a significant change between PVC burden levels (0%, 7%, 14%, 25%, 33% and 50%). P value, repeated measures one-way ANOVA. Details are given in Table 2.
Even though no statistical test was performed assessing the relationship between PVC burden and MR severity, a clear relationship is apparent. At baseline, a third (N=3, 33%) of the animals had trace MR, with the remainder being rated ‘None’ (N=6, 67%). After exposure to a PVC burden of 25%, all animals (N=9, 100%) had trace MR. At 50% PVC burden, four of the animals (N=4, 43%) had 1+ MR with the remainder (N=5, 57%) having trace MR, demonstrating a clear increase in MR (Table 2).
Biomarkers
Serum IL-6 levels did not change significantly between 0, 7, 14, 25, 33 and 50% PVC burden (22.6 ± 8 , 23.8 ± 11, 24.0 ± 9, 21.4 ± 11, 22.7 ± 7 and 21.0 ± 8 pg/mL, respectively), whereas pro-BNP levels remained below clinically significant levels without a clear correlation with PVC burden (87.4 ± 68, 33.4 ± 29, 33.6 ± 31, 60.4 ± 49, 93.4 ± 100.1 and 35.9 ± 27 pg/mL at 0, 7, 14, 25, 33 and 50% PVC, respectively).
Discussion
This is the first animal study to assess the cardiac consequences of different PVC burdens (from 7 to 50%) of chronic (>2 months) RV apical PVCs at a fixed level of prematurity (240ms coupling interval) in otherwise structurally normal canine hearts. We demonstrated that: 1) LV function declines linearly as PVC burden increases (Figure 1) ; 2) a minimum and a mean PVC burden of 25% and 33% is required to induce CM (defined as LVEF < 50% or LVEF drop >10% points) as this occurred in 1 out of 9 animals and 4 out of 9 animals, respectively, compared with all animals with 50% PVC burden; 3) statistical reduction in LVEF and increase in LVEDD were noted with as little as 14% PVC burden despite a preserved LV systolic function (LVEF >50%, Figure 1 and 2); 4) LV systolic function (assessed by radial strain) decreases with as little as 7% PVC burden even with a preserved LV ejection fraction, 5) LA size increases while E/A ratio decreases with PVC burden greater than 33% (Table 2).
Significant limitations exist to identify a mean or minimal PVC burden in clinical studies, due to large variability of PVC origin and coupling interval between patients. A small retrospective clinical study7 suggested that a mean PVC burden of 24% (assessed by 24-hour Holters) is required to develop PVC-induced CM (LVEF < 50%), while, almost no patients developed CM with a 10% or lower PVC burden. However, assessment of PVC burden based on a single 24-hour Holter monitor is an inaccurate measure of true long-term PVC burden because of a high variability of spontaneous PVC frequencies over extended periods of time9. The difference in the minimum and mean PVC burden required to induce CM between published retrospective clinical studies and our canine study could be explained by: 1) methodology (retrospective vs. prospective study), 2) difference in PVC location or coupling intervals, 3) underestimation of PVC burden by a single 24-hour Holter, and/or 4) inter-species variability in susceptibility to PVC-induced cardiomyopathy. Therefore, an animal model with a constant PVC burden is key to determine the relationship between PVC burden and development of PVC-induced CM.
Similar to clinical data1, 4, 6, 7, 12, some animals appear to be more susceptible to develop PVC-induced CM, as not all animals develop LV dysfunction even at a 25 and 33% PVC burden despite identical origin and coupling interval. This individual susceptibility to PVC exposure suggests the presence of a genotype or molecular phenotype that predisposes to the development of this CM. This molecular phenotype could be associated with differences in junctophylin-2 (scaffolding protein known to regulate the interaction between the Ryanodine receptor and L-type calcium channel) and L-type Calcium channel found to be altered in PVC-induced CM13.
Our study revealed that LV systolic function deteriorates as the PVC burden increases. A clinical study by Wijnmaalen et. al.14 showed that subtle LV systolic dysfunction associated with frequent PVCs can be identified if assessed by speckle-tracking imaging even when LV ejection fraction is considered preserved (LVEF > 50%). They supported this finding by showing that radial, circumferential and longitudinal strain normalized after elimination of chronic PVCs. This data is consistent with our animal study, where all animals had an early decrease in radial strain prior to the development of PVC-induced CM (Table 2 and Figure 2, Supplemental Figures 3-8). Thus, our study supports that radial strain imaging can be used to detect a “pre-clinical” stage of PVC-induced CM or predict the development of PVC-induced CM when LVEF is above 50%. Moreover, assessment of LV mechanics using speckle-tracking imaging (dispersion of QRS-to peak radial strain on 6 different LV segments) showed a trend towards increased LV dyssynchrony as PVC burden is increased (Table 2).
To our knowledge, only one small clinical study suggests improvement in LA and LV diastolic dysfunction after radiofrequency ablation of PVCs15. Our experimental study suggests that mild LA enlargement and LV diastolic dysfunction (changes in E/A ratio) could be associated with states of high PVC burden (> 33%, Figure 2). In contrast, mitral regurgitation has been previously reported in patients with PVC-induced CM4, 8. Future clinical and animal studies are required to better understand the effects of PVCs on diastolic function and LA dimensions. For now, we can only speculate that LA dilatation is unlikely related to the subtle changes in MR alone, but rather the combination of MR, AV dissociation and diastolic dysfunction.
Surprisingly, pro-BNP levels did not increase as the PVC burden increased and cardiomyopathy developed. However, blood samples were only obtained while PVCs were present (premature pacing algorithm enabled). We speculate that post-extrasystolic potentiation during PVCs maintain a stable hemodynamic state that prevents BNP elevation as demonstrated in prior canine's studies of post-extrasystolic potentiation where paired pacing (analogous to ventricular bigeminy) did not compromise cardiac output16-18. This was also clinically apparent since these animals did not appear to develop clinical signs of heart failure. The absence of IL-6 changes confirms that PVC-induced CM is not mediated by an inflammatory response as first reported in histopathological analysis2.
Mechanism of PVC-induced Cardiomyopathy
Our study provides some insight into the mechanism of PVC-induced CM, since 44% of the animals developed CM (LVEF <50%) when exposed to 33% PVC burden despite a mean heart rate of 82 bpm (Table 1). Furthermore, a gradual and linear decline in LVEF and radial strain at PVC burden from 7 to 33% PVC burden suggests that tachycardia plays little or no role in the development of PVC-induced CM.
The reason for the significant increase in HR between 33 and 50% PVC burden remains elusive. We can only speculate that this is not only due to the increase in PVC burden but also changes in autonomic tone due to a chronic and cumulative exposure to frequent PVCs. Even though we cannot rule out tachycardia as a contributing mechanism at 50% PVC burden in this series of animals (mean heart rate 157 ± 43 bpm, we believe this is unlikely since: 1) 4 out of the 9 animals had a heart rate between 103 – 126 bpm when exposed to 50% PVC burden yet they all developed CM (mean LVEF of 45%), 2) canine models of tachy-induced cardiomyopathy have been described with HR > 180 bpm19, 20, and 3) our original manuscript where our animals were exposed to only 3-month PVC (bigeminal pattern) with a mean heart rate of 130 ± 13 bpm developed LV dysfunction of a similar magnitude.
Besides PVC burden, small retrospective clinical studies highlighted other PVC features that may potentially contribute to the development of cardiomyopathy. In some studies, QRS duration and epicardial origin may be correlated with the development of PVC-induced CM7, 21, 22, while in others, the impact of PVC origin and coupling interval (prematurity) remains poorly understood12, 23-25. The discrepancy may be related to limited sampling duration for PVCs which fails to capture true PVC burden and/or location. Future prospective clinical studies and animal models are needed to clarify the contribution of these PVC features to the development of PVC-induced CM.
Limitations
Due to the incremental PVC burden protocol, we cannot exclude the possibility that the development of PVC-induced CM was related to the cumulative effect of PVCs frequency. However, the severity of PVC-induced CM at a 50% PVC burden (after gradual stepwise increase in PVC burden) was no different from our original published model with a 3-month single burden PVC exposure. The latter also demonstrated LV dysfunction of a similar magnitude. This suggests that there was little or no cumulative effect of PVCs. The strength of this protocol is that each animal served as its own control to assess the effects of different PVC burden on LV function and development of PVC-induced CM.
Exposure to each PVC burden was for a duration of 8 weeks. Based on our initial report2, the effect of chronic exposure to PVCs in canines appears to plateau at 8 weeks. Thus, we postulate an insignificant or no further deterioration of LV function occurs beyond 8 weeks. In contrast to clinical data suggesting the need of prolonged PVC exposure to induce CM26, our PVC canine model develops CM with a shorter but consistent (uninterrupted) 8-week PVC burden. We speculate that longer periods of PVC exposure are required to induce CM in humans due to variability in PVC burden9, 27.
Ventricular ectopy was limited only to the RV apex and may not apply to PVCs of other origins, such as LV and RVOT. Yet, our findings are relevant since one of the largest case series (40+ patients) of PVC-induced CM reported similar number of cases between different PVC origins24, as well as unifocal or multifocal PVCs. Similarly, another study reported no difference in the hazard ratio for the development of PVCs between LV, RVOT and non-RVOT PVCs, while 70% of PVC-induced CM was associated with non-RVOT PVCs7.
Pro-BNP levels were obtained during active ventricular ectopy, in contrast to echocardiographic images which were obtained 5-to-10 minutes after premature pacing algorithm was disabled. Thus, it is possible that post-extrasystolic potentiation maintained sufficient hemodynamic stability to prevent significant release or change in BNP levels.
This study was performed only in structurally normal hearts. The minimum PVC burden required to deteriorate LV systolic function in subjects with preexisting structural heart disease remains unclear.
All animals were between 1-2 years old. Thus, it is unclear if the same PVC burden at older ages would have a different impact on the development of PVC-induced cardiomyopathy.
Conclusions
LV function declined linearly as PVC burden increased. PVC-induced CM (LVEF < 50% or LVEF drop >10% points) was present in a few canines with 25% and 33% PVC burden without a difference in mean heart rate, while PVC-induced CM was present in all animals with 50% PVC burden. However, subtle LV systolic dysfunction can be demonstrated by a decrease in LV ejection fraction and radial strain strain even at PVC burdens below 25%. Our study supports that speckle-tracking imaging can be used to assess early stages of PVC-induced CM or predict the development of PVC-induced CM when LVEF is above 50%. Moreover, a decrease in E/A ratio suggests that LV diastolic dysfunction also develops as PVC burden increases.
Supplementary Material
Clinical Perspectives.
This study determined for the first time, the cardiac consequences of different PVC burdens (from 7 to 50%) in otherwise structurally normal canine hearts. We demonstrated that LV systolic function declined linearly as PVC burden increased. The minimum and mean PVC burden required to induced cardiomyopathy (LVEF < 50% or LVEF drop >10% points) was 25% and 33%, respectively, while all animals developed a cardiomyopathy (CM) when exposed to 50% burden. Additionally, changes in LV radial by speckle tracking echocardiography were detectable with as little as 7% PVC burden and prior to the development of PVC-induced CM. Thus, LV strain may represent a new method of detecting pre-clinical stages of PVC-induced CM, allowing us to identify patients with frequent PVCs and preserved LVEF at imminent risk of developing a CM. Finally, mild LA enlargement and LV diastolic dysfunction (changes in E/A ratio) may be present in high PVC burden states (>33%, trigeminy) suggesting that LV diastolic dysfunction could contribute to heart failure in patients with frequent PVCs.
While, future randomized clinical studies are needed to compare outcomes between different treatment strategies in PVC-induced cardiomyopathy, these studies should include assessments of LV diastolic dysfunction and LA size after PVC suppression. Moreover, additional studies are also needed in patients with frequent PVCs to validate the use of LV strain to identify subclinical or early stages of PVC-induced CM.
Acknowledgement
We wish to acknowledge Katrina Stumpf for her unconditional support to complete this study.
Funding
Project was funded primarily through a Scientist Development Grant from AHA (National Center Award # SDG9310032) to J.F. Huizar. Statistical assistance through a National Institute of Health grant (# UL1TR000058) to VCU Research Incubator. Additional research support was provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Biomedical Laboratory Research and Development through a Career Development Award grant 1IK2BX001561-01A2 to M.D. Shultz. The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government.
Conflict of Interest
Tan A – Research support from Boston Scientific Corp (BS). and Biotronik, Inc. (BTK); Hu Y – None; Potfay J – None; Kaszala K – Research support from Medtronic, Inc (MDT); Howren M – None; Sima A – None; Shultz M – None; Koneru JN – Honoraria from MDT, BTK, and Atricure; Ellenbogen KA – Research support from BS, Biosense Webster (BW), MDT, St. Jude Medical (SJM), NIH, Consultant for BS, SJM, Atricure, Medtronic, Honoraria from MDT, BS, BTK, BW and Atricure; Huizar JF – Research support from BS, BTK and SJM.
Abbreviations
- PVCs
Premature ventricular contractions
- SCD
Sudden cardiac death
- CM
Cardiomyopathy
- LVEF
LV ejection fraction
- FS
Fractional shortening
- LVESD
LV end-systolic dimension
- LVEDD
LV end-diastolic dimension
- LA
Left atria
- MV
Mitral valve
- MR
Mitral regurgitation
- PW
Posterior wall
- SW
Septal wall
- HR
Heart rate
- Bpm
beats per minute
- CIs
Confidence intervals
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bogun F, Crawford T, Reich S, Koelling TM, Armstrong W, Good E, Jongnarangsin K, Marine JE, Chugh A, Pelosi F, Oral H, Morady F. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: Comparison with a control group without intervention. Heart Rhythm. 2007;4:863–867. doi: 10.1016/j.hrthm.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Huizar JF, Kaszala K, Potfay J. Left ventricular systolic dysfunction induced by ventricular ectopy: A novel model for premature ventricular contraction-induced cardiomyopathy. Circ Arrhythm Electrophysiol. 2011;4:543–549. doi: 10.1161/CIRCEP.111.962381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taieb JM, Maury P, Shah D, Duparc A, Galinier M, Delay M, Morice R, Alfares A, Barnay C. Reversal of dilated cardiomyopathy by the elimination of frequent left or right premature ventricular contractions. J Interv Card Electrophysiol. 2007;20:9–13. doi: 10.1007/s10840-007-9157-2. [DOI] [PubMed] [Google Scholar]
- 4.Takemoto M, Yoshimura H, Ohba Y, Matsumoto Y, Yamamoto U, Mohri M, Yamamoto H, Origuchi H. Radiofrequency catheter ablation of premature ventricular complexes from right ventricular outflow tract improves left ventricular dilation and clinical status in patients without structural heart disease. J Am Coll Cardiol. 2005;45:1259–1265. doi: 10.1016/j.jacc.2004.12.073. [DOI] [PubMed] [Google Scholar]
- 5.Yarlagadda RK, Iwai S, Stein KM, Markowitz SM, Shah BK, Cheung JW, Tan V, Lerman BB, Mittal S. Reversal of cardiomyopathy in patients with repetitive monomorphic ventricular ectopy originating from the right ventricular outflow tract. Circulation. 2005;112:1092–1097. doi: 10.1161/CIRCULATIONAHA.105.546432. [DOI] [PubMed] [Google Scholar]
- 6.Sarrazin JF, Labounty T, Kuhne M. Impact of radiofrequency ablation of frequent post-infarction premature ventricular complexes on left ventricular ejection fraction. Heart Rhythm. 2009;6:1543–1549. doi: 10.1016/j.hrthm.2009.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baman TS, Lange DC, Ilg KJ. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm. 2010;7:865–869. doi: 10.1016/j.hrthm.2010.03.036. [DOI] [PubMed] [Google Scholar]
- 8.Lee GK, Klarich KW, Grogan M, Cha YM. Premature ventricular contraction-induced cardiomyopathy: A treatable condition. Circ Arrhythm Electrophysiol. 2012;5:229–236. doi: 10.1161/CIRCEP.111.963348. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt G, Ulm K, Barthel P, Goedel-Meinen L, Jahns G, Baedeker W. Spontaneous variability of simple and complex ventricular premature contractions during long time intervals in patients with severe organic heart disease. Circulation. 1988;78:296–301. doi: 10.1161/01.cir.78.2.296. [DOI] [PubMed] [Google Scholar]
- 10.Gottdiener JS, Bednarz J, Devereux R. American society of echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17:1086–1119. doi: 10.1016/j.echo.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Teshima K, Asano K, Sasaki Y, Kato Y, Kutara K, Edamura K, Hasegawa A, Tanaka S. Assessment of left ventricular function using pulsed tissue doppler imaging in healthy dogs and dogs with spontaneous mitral regurgitation. The Journal of veterinary medical science / the Japanese Society of Veterinary Science. 2005;67:1207–1215. doi: 10.1292/jvms.67.1207. [DOI] [PubMed] [Google Scholar]
- 12.Sun Y, Blom NA, Yu Y, Ma P, Wang Y, Han X, Swenne CA, van der Wall EE. The influence of premature ventricular contractions on left ventricular function in asymptomatic children without structural heart disease: An echocardiographic evaluation. Int J Cardiovasc Imaging. 2003;19:295–299. doi: 10.1023/a:1025418531853. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Eltit JM, Kaszala K, Tan A, Jiang M, Zhang M, Tseng GN, Huizar JF. Cellular mechanism of premature ventricular contraction-induced cardiomyopathy. Heart Rhythm. 2014 doi: 10.1016/j.hrthm.2014.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wijnmaalen AP, Delgado V, Schalij MJ, van Huls van Taxis CF, Holman ER, Bax JJ, Zeppenfeld K. Beneficial effects of catheter ablation on left ventricular and right ventricular function in patients with frequent premature ventricular contractions and preserved ejection fraction. Heart. 2010;96:1275–1280. doi: 10.1136/hrt.2009.188722. [DOI] [PubMed] [Google Scholar]
- 15.Akkaya M, Roukoz H, Adabag S, Benditt DG, Anand I, Li JM, Zakharova M, Tholakanahalli V. Improvement of left ventricular diastolic function and left atrial reverse remodeling after catheter ablation of premature ventricular complexes. J Interv Card Electrophysiol. 2013;38:179–185. doi: 10.1007/s10840-013-9836-0. [DOI] [PubMed] [Google Scholar]
- 16.Braunwald E, Ross J, Jr., Frommer PL, Williams JF, Jr., Sonnenblick EH, Gault JH. Clinical observations on paired electrical stimulation of the heart. Effects on ventricular performance and heart rate. Am J Med. 1964;37:700–711. doi: 10.1016/0002-9343(64)90019-1. [DOI] [PubMed] [Google Scholar]
- 17.Braunwald NS, Gay WA, Jr., Morrow AG, Braunwald E. Sustained, paired electrical stimuli: Slowing of the ventricular rate and augmentation of contractile force. Am J Cardiol. 1964;14:385–393. doi: 10.1016/0002-9149(64)90083-9. [DOI] [PubMed] [Google Scholar]
- 18.Cooper MW. Postextrasystolic potentiation. Do we really know what it means and how to use it? Circulation. 1993;88:2962–2971. doi: 10.1161/01.cir.88.6.2962. [DOI] [PubMed] [Google Scholar]
- 19.Shinbane JS, Wood MA, Jensen DN, Ellenbogen KA, Fitzpatrick AP, Scheinman MM. Tachycardia-induced cardiomyopathy: A review of animal models and clinical studies. J Am Coll Cardiol. 1997;29:709–715. doi: 10.1016/s0735-1097(96)00592-x. [DOI] [PubMed] [Google Scholar]
- 20.Spinale FG, Holzgrefe HH, Mukherjee R, Arthur SR, Child MJ, Powell JR, Koster WH. LV and myocyte structure and function after early recovery from tachycardia-induced cardiomyopathy. Am J Physiol. 1995;268:H836–847. doi: 10.1152/ajpheart.1995.268.2.H836. [DOI] [PubMed] [Google Scholar]
- 21.Carballeira Pol L, Deyell MW, Frankel DS, Benhayon D, Squara F, Chik W, Kohari M, Deo R, Marchlinski FE. Ventricular premature depolarization qrs duration as a new marker of risk for the development of ventricular premature depolarization-induced cardiomyopathy. Heart Rhythm. 2014;11:299–306. doi: 10.1016/j.hrthm.2013.10.055. [DOI] [PubMed] [Google Scholar]
- 22.Yokokawa M, Kim HM, Good E. Impact of QRS duration of frequent premature ventricular complexes on the development of cardiomyopathy. Heart Rhythm. 2012;9:1460–1464. doi: 10.1016/j.hrthm.2012.04.036. [DOI] [PubMed] [Google Scholar]
- 23.Del Carpio Munoz F, Syed FF, Noheria A, Cha YM, Friedman PA, Hammill SC, Munger TM, Venkatachalam KL, Shen WK, Packer DL, Asirvatham SJ. Characteristics of premature ventricular complexes as correlates of reduced left ventricular systolic function: Study of the burden, duration, coupling interval, morphology and site of origin of PVCs. J Cardiovasc Electrophysiol. 2011;22:791–798. doi: 10.1111/j.1540-8167.2011.02021.x. [DOI] [PubMed] [Google Scholar]
- 24.Olgun H, Yokokawa M, Baman T, Kim HM, Armstrong W, Good E, Chugh A, Pelosi F, Jr., Crawford T, Oral H, Morady F, Bogun F. The role of interpolation in pvc-induced cardiomyopathy. Heart Rhythm. 2011;8:1046–1049. doi: 10.1016/j.hrthm.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 25.Kawamura M, Badhwar N, Vedantham V, Tseng ZH, Lee BK, Lee RJ, Marcus GM, Olgin JE, Gerstenfeld EP, Scheinman MM. Coupling interval dispersion and body mass index are independent predictors of idiopathic premature ventricular complex-induced cardiomyopathy. J Cardiovasc Electrophysiol. 2014;25:756–762. doi: 10.1111/jce.12391. [DOI] [PubMed] [Google Scholar]
- 26.Yokokawa M, Kim HM, Good E, Chugh A, Pelosi F, Jr., Alguire C, Armstrong W, Crawford T, Jongnarangsin K, Oral H, Morady F, Bogun F. Relation of symptoms and symptom duration to premature ventricular complex-induced cardiomyopathy. Heart Rhythm. 2012;9:92–95. doi: 10.1016/j.hrthm.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 27.Duygu Bas H, Baser K, Hoyt J, Yokokawa M, LaBounty T, Morady F, Bogun F. Effect of circadian variability in frequency of premature ventricular complexes on left ventricular function. Heart Rhythm. 2015 doi: 10.1016/j.hrthm.2015.07.038. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.