Abstract
The control of noncommunicable diseases (NCDs) was addressed by the declaration of the 66th UN General Assembly followed by the World Health Organisation’s NCD 2020 Action Plan. There is a clear need to better apply evidence in public health settings to tackle both behaviour-related factors and the underlying social and economic conditions. This article describes concepts of evidence based public health and outlines a set of actions that are essential for a successful global NCD prevention. The authors describe the importance of knowledge translation with the goal of increasing the effectiveness of public health services, replying on both quantitative and qualitative evidence. In particular, the role of capacity building is highlighted because it is fundamental to progress in controlling NCDs. Important challenges for capacity building include the need to bridge diverse disciplines, build the evidence base across countries, and the lack of formal training in public health sciences. As brief case examples, several successful capacity building efforts are highlighted to address challenges and further evidence-based decision making. The need for a more comprehensive public health approach, addressing social, environmental and cultural conditions, has led to a whole-of government and whole-of society strategies that are now on the agenda due to efforts such as the WHO's NCD 2020 Action Plan and the Health 2020 European Policy Framework. These efforts need research to generate evidence in new areas (e.g., equity, sustainability), training to build public health capacity, and a continuous process of improvement and knowledge generation and translation.
Keywords: capacity building, evidence-based public health, knowledge translation, NCD 2020 Action Plan, NCD prevention, training
Introduction
The epidemiologic evidence accumulated over past few decades shows that noncommunicable diseases (NCDs) are the leading causes of morbidity and mortality globally.1 These NCDs (e.g., heart disease, cancer, stroke, diabetes), no longer diseases of affluence, affect all countries across all income groups with almost 80% of NCDs occurring in low-and middle-income countries.2 Globally, the leading risk factors for NCD are high blood pressure (12.8% of all deaths globally), tobacco use (8.7%), high blood glucose (5.8%), physical inactivity (5.5%), obesity (4.8%), high cholesterol (4.5%), and alcohol use (3.8%).1 Underlying these behaviour-related factors are the social and economic environments (poverty, social displacement, inequality).3, 4 The global burden of NCDs constitutes a major public health challenge that may undermine social and economic development in any country.
The prominence of NCD control is illustrated by the declaration of the high-level meeting of the 66th UN General Assembly calling upon the international community and each Member State to intensify their efforts in the prevention and control of NCDs.5 As a follow-up and to operationalize this document, the World Health Assembly 66 in May 2013 approved global actions - including a comprehensive global monitoring - framework (the WHO global action plan for the prevention and control of NCDs 2013–2020).6 Within this framework, the recommended NCD interventions and use of 25 indicators at the country level requires considerable efforts in strengthening public health capacities at national and international levels. Evidence, in the form of quantitative and qualitative data, forms the basis by which public health officials will accomplish the NCD goals laid out in these international plans.
In a study of 27 organisations from 16 European countries, the majority of respondents (52%) reported that evidence-based methods are currently poorly integrated into public health.7 Putting this evidence to use in public health settings requires sufficient capacity (capacity is the availability of resources, structures and adequately trained workforce to deliver the “preventive dose“ of an NCD intervention and is comprised of resources (manpower, funds and other), skills, and structures.8, 9) building.10
There are several important challenges in workforce capacity building. First, the call for new approaches in public health such as “health in all policies”11 highlights the need for diverse disciplines to accomplish global public health objectives.12, 13 Some of the most important innovations are likely to occur outside of the health sector (e.g., urban planning, economics, agriculture, communication). Second, the evidence base for public health varies considerably across countries,7, 14 which hampers efforts in regions where the evidence for effective interventions is sparse. And third, it is likely that fewer than half of the individuals in the public health workforce have had any formal training in a public health discipline such as epidemiology or health education.15 An even smaller percentage of these professionals have formal graduate training from a school of public health or other public health programme. For example, it is noted that 15 years following the break-up of the Soviet Union, there is still very limited capacity to implement effective health programmes and policies in the eastern European region.16 A solution to this problem is wider dissemination of effective training programmes to increase knowledge and skills of public health practitioners
In this article, we describe the concepts of evidence-based public health (EBPH), the importance of capacity building, approaches for capacity building, and future direction to affect global efforts to control NCDs.
Defining Evidence-Based Public Health
EBPH involves several key concepts:17
Making decisions based on the best available scientific and/or rigorous programme evaluation evidence;
Applying programme planning and quality improvement frameworks;
Engaging the community and stakeholders in assessment and decision making;
Adapting and implementing evidence-based interventions for specific populations or settings; and
Conducting sound evaluation.
By using an evidence-based approach, activities in public health practice are explicitly linked with the underlying scientific evidence that demonstrates the causes of NCDs, epidemiologic patterns in NCDs and NCD risk factors, intervention effectiveness, and external validity.
When applying the principles of EBPH in a global context for NCD prevention and control, it is important to first understand the context for intervention and then to identify key processes in the translation of EBPH from one population or geographic setting to another. Context refers to the often-difficult-to-measure characteristics of the agency, community, sociocultural, and political/economic surroundings in which an NCD intervention is to be implemented or evaluated.17, 18 These contextual variables may be important moderators of an intervention effect, yet too often they are ignored or not reported.19 Contextual factors may have an effect on external validity (i.e., the degree to which findings from a study or set of studies can be generalizable to and relevant for populations, settings, time periods other than those in which the original studies were conducted).20
Knowledge Translation and Capacity Building to Address NCDs
To address a number of the issues in EBPH, the concept of knowledge translation is central. Knowledge translation is the term to denote “a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically sound application of knowledge.”21 Its purpose is improving population health, providing more effective health services and products, and strengthening the health care system. Knowledge translation for NCD control occurs within a complex social system of interactions between researchers and knowledge users.
When furthering knowledge translation for NCD prevention and control, seven important questions come to mind:
What is the size of the public health problem?
What is causing the public health problem?
Are there effective interventions for addressing the problem?
How do we best evaluate ongoing NCD interventions?
What information about the country-specific context of a particular intervention is helpful in deciding its potential use?
What data are needed to decide if the intervention could be translated to a different setting or population?
Is there political will to implement an effective intervention?
Questions 1–4 tend to be addressed via scientific studies and quantitative data. The latter questions (nos. 5–7) tend to rely more on the art of public health, qualitative data, and professional judgment. A large-scale strategic plan, such as the NCD 2013–2020 Plan can serve as a catalyst for addressing many of these questions. There are important considerations, both at the macro- and micro-levels.
At the macro-level, NCD control requires a multi-sector, comprehensive approach—in particular stronger leadership is needed from policy makers, public health professionals, and advocates.22 Policy measures are sometimes (falsely) portrayed as a choice between responsibility of individuals versus restriction of freedom.23 There is a need for strong leadership and new policies, practices, and participation beyond the confines of traditional public health agencies and services.23 Often this macro view is grounded in the societal view of the role of government and the shared governance arrangement between citizens and policy bodies. For example, the social insurance systems of Germany and Austria have been evolving constantly since the 1880s when the Bismarck model of Social Health Insurance was established.24 These are systems based on solidarity and population-wide coverage of health care and a remarkable pluralism of actors and organisational structures. There is ongoing discussion regarding how shared governance could generate a “global response” to chronic disease and what the part of established national governance structures can be.25
At a more micro-level, better information is needed on how an effective NCD intervention can be transferred from one population or setting to another. Several authors have described the factors influencing intervention translation.14, 26–28 Based on a review of 43 articles examining intervention translation, Cambon and colleagues identified five domains (Table 1).26 These domains mainly relate to the external validity of an NCD intervention,29 which too often is missing from the literature and must be developed from reading the gray literature or interviewing intervention developers.
Table 1.
Factors related to the translation of interventions
| Domain | Examples |
|---|---|
| Underlying health problem |
|
| Population (target of the intervention) |
|
| Implementation |
|
| Professionals |
|
| Environment |
|
The role of capacity building
An adequate national capacity is needed to develop national policy frameworks, with the goal of implementing and evaluating community-based initiatives and programmes for the prevention of NCD through approaches that are based on best available evidence. The important role of capacity building (e.g., move training toward prevention, increase the skills of professionals) has been noted as a “grand challenge” for NCD control.30
One of the priority goals of capacity development is to ensure that sufficient education is provided to public health professionals to enable them to implement evidence-based strategies for NCD prevention. This can be achieved by: 1) supporting undergraduate programmes and courses in public health that are based on the integrated approach; and 2) supporting continuing education and postgraduate education in public health that are based on the integrated approach.
During last 25 years, the CINDI (Countrywide Integrated Noncommunicable Diseases Intervention) programme as a regional network for NCD prevention in the European Region of WHO played an important role in enhancing evidence-based public health training including exchange and dissemination of experience and best practice.9, 31, 32 CINDI’s regional approach has lead to a number of country-specific trainings in evidence-based public health.
A number of international capacity building activities were organized by WHO and CINDI.33 These included the preparation and dissemination of guidelines (e.g. guidelines for GPs on prevention in primary care, the CINDI dietary guide), teaching projects (e.g. the Pharmacy-based hypertension project) summer schools and workshops (e.g. summer schools on nutrition organized in Lithuania and Poland), collaboration on capacity building among several countries (e.g. a summer school on capacity building for six CINDI programme participating countries of central and eastern Europe hosted by CINDI- Canada in Halifax), educational site visits (e.g. a training week on preventive practice in CINDI-Austria for general practitioners from CINDI-Russia) long-term bilateral collaboration (e.g. between the North Karelia team and the Russian Karelia team on establishing a community-based integrated NCD prevention programme in the Russian Federation). In addition, the CINDI network has developed two types of annual structured training courses, described below.
From 1997–2007, an annual training seminar was offered to health professionals interested in the planning, implementation and evaluation of programmes for health promotion and noncommunicable disease prevention. The CINDI Winter School “New Public Health: Theory and Practice” - was coordinated by the WHO Regional Office for Europe and hosted by the National Public Health Institute of Finland in Helsinki. International faculty members were well recognised experts in public health. The week-long course included lectures, group discussions and individual consultations. The participants were encouraged to present their own programmes during the group discussions. It was aimed at presenting the background, principles, practical implementation, evaluation, results and experiences of the implementation of the integrated approach to NCD prevention. Pertinent theories, international frameworks, state-of-art in practice, as well as examples from a number of CINDI programmes were presented and discussed. The training course also supported the implementation of the EU TACIS projects of health promotion in Russia and the Republic of Moldova.
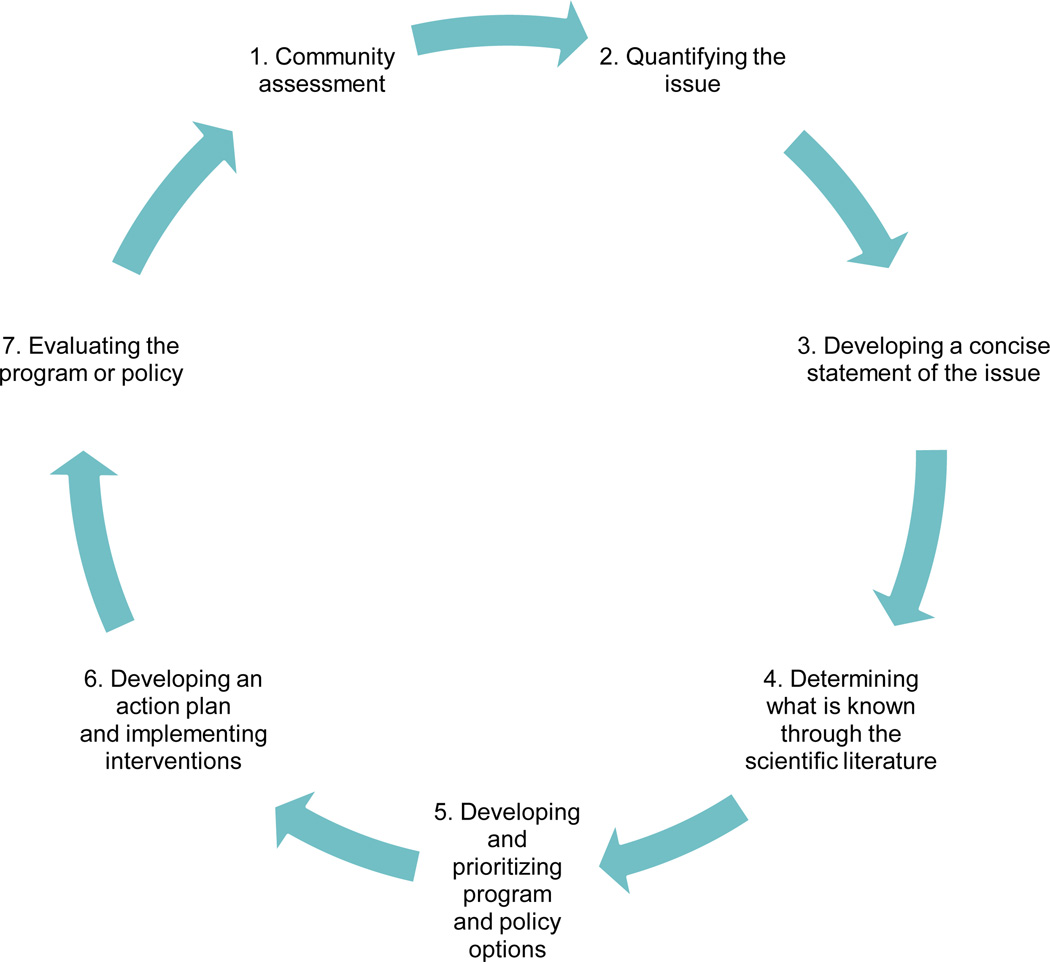
Since 2002, a training course entitled: “Evidence-based Public Health: A Course in Chronic Disease Prevention” – has been organised annually. This was the first European-American collaborative training effort on EBPH capacity building. It has been organised by the WHO Regional Office for Europe in collaboration with the Centers for Disease Control and Prevention and Control, the Prevention Research Center in St. Louis, CINDI-Austria, CINDI-Canada, CINDI-Finland, CINDI-Lithuania, and CINDI-Slovenia. The training seminar has been hosted by CINDI-Austria. The course is organised around a set of core domains (Figure 1) and detailed core competencies are described elsewhere.17, 34 The course has featured a train-the-trainer approach that helps create training programmes when participants return to their home countries. Theoretical knowledge was balanced with presentations on practical aspects of the implementation of evidence-based integrated intervention at local and national levels. Evaluations of this course have shown its beneficial impact in building skills and knowledge in evidence-based decision making.35, 36
Figure 1.
Training approach for evidence-based public health
In addition, numerous new professional contacts among the participants have been established as a result of the EBPH course. The course gave a fresh impetus and motivation to the further development of established programmes and was a powerful marketing tool of the usefulness of the integrated approach towards NCD prevention and control. This international training had numerous follow-ups and spin-offs. These include:
Opportunities for fellowships for the participants of the course to engage in graduate education in the United States;
The development of national/regional training materials and courses for capacity building in evidence-based NCD prevention (e.g., in Bulgaria, Lithuania, the Russian Federation, Georgia);
Dissemination of capacity building approaches at national and international meetings;
National/regional workshops or other training forms (e.g. Bulgaria, the Russian Federation); and
Stimulation of national NCD policy development (e.g., Lithuania, Bulgaria, Portugal).
Summary and Future Challenges
Noncommunicable diseases are not just one of the world’s most pressing health concerns but also a significant development challenge and a human rights issue. They have been recognized as such at the highest global political levels and are already reflected in various intergovernmental processes related to the post-2015 development agenda.37 They impede social and economic development and are driven by underlying social, economic, political, environmental and cultural factors, broadly known as “social determinants.”38 Noncommunicable diseases are an enormous and growing strain on health systems worldwide and also are the source of social and economic costs at national and household levels. Inequities are also apparent within countries, where NCD outcomes and risk factors are patterned along various socio-economic gradients or geographic areas.
Responding to NCDs is not simply a matter of changing individual behaviours in isolation; broader changes in social, economic, environmental and cultural contexts are also needed.4 Leadership and action from the health sector is the anchor for NCD responses. Significant, actions from other sectors and stakeholders is crucial, especially to address social determinants. Multisectoral action that tackle the underlying, overlapping and interacting social determinants of NCDs as a cornerstone of NCD responses has been endorsed at the highest political levels, such as in the 2011 “UN Political Declaration on Non-communicable Diseases.”5
WHO’s “Global Action Plan for the Prevention and Control of NCDs 2013–2020”6 and the Health 2020 European Policy framework39 already point the way forward for whole-of-government and whole-of-society responses. In this regard, we will need to draw increasingly on other disciplines to study effective governance structures for multisectoral coordination and participation, transparency and accountability mechanisms, human-rights-based approaches to NCDs, municipal and decentralized responses, and the role of the law. Practice-based evidence or case examples of action outside the health sector could also help in developing a practical framework for multisectoral action.40
NCD prevention will continue to challenge the field of EBPH. Limited frameworks and limited consensus on best practices, lack of data, and lack of appropriate methods are major barriers to greater integration of evidence-based methodologies into practice. To address these barriers, it will be important to develop innovations in methods to evaluate and monitor comprehensive interventions. Examples of the types of innovations required may include identifying new measures of health and well-being, equity and sustainability; implementing new systems for more timely and consistent data measures that are easily accessible; developing analytic procedures for mixed methods research designs that enable us to understand how temporal shifts in context influence the outcomes of NCD interventions; and applying integrative theories that describe how the scale-up of interventions takes hold both vertically, through levels of the system, and horizontally across sectors.41–44 These innovations will also need to be incorporated into knowledge generation, synthesis, and integration initiatives.45, 46
It has been noted that ”evidence without capacity is an empty shell” (Mohan Singh).47 In this regard, various forms and types of workforce training should be available at local, national and international levels. Future work will require expanding and improving the access of training initiatives such as the course on evidenced-based public health as well as building research capacity to guide evidence-based action on the social determinants of NCDs. Accessibility of training and multidisciplinary workforce development to meet the needs of the practitioners may require examining virtual and digital approaches. For example, social media opens the way for broader networks which can bring together transnational communities of interest.48 It also provides the opportunity of shortening dissemination chains by linking policy development on public health issues directly with large numbers of community based organisations, interest groups, and practitioners.
In addition to traditional approaches to capacity building through training initiatives, knowledge generation and translation activities require partnerships underpinned by effective exchanges between researchers and users to appropriately integrate the latest and most relevant research in decision-making.49 The Evidence Informed Policy and Practice in Europe project is an example that involves more than 40 partners from across Europe and internationally in order to increase all types of evidence use across all education sectors by developing capacity among researchers, policy makers and practitioners and strengthening connections between them. There are similar examples in other regions such as the WHO initiative in knowledge translation, the Evidence Policy Network which promotes a network of partnerships at all levels among health system policy makers and other stakeholders to improve health outcomes through context specific research evidence. Such expanding networks create new opportunities for synergies and collaborative learning from existing experiences and best practices to advance the field of evidence-based public health.
Acknowledgments
This study was made possible by the contributions of Evidence-Based Public Health course faculty members, including Drs. Elizabeth Baker, Carol Brownson, Claudia Campbell, Wayne Giles, Kathleen Gillespie, Erkki Vartiainen, and Jozica Maucek Zakotnic. We are also grateful to Ellen Jones, Chuck Gollmar, and John Robitscher of the National Association of Chronic Disease Directors.
Sources of Funding:
The Evidence-Based Public Health training programme was supported in part by: the National Association of Chronic Disease Directors contract number 482012; Cooperative Agreement Number U48/DP001903 from the Centers for Disease Control and Prevention, Prevention Research Centers Program.
Footnotes
Diclaimer: We warrant that the article is the Authors' original work. We warrant that the article has not received prior publication and is not under consideration for publication elsewhere.
Conflicts of Interests Declaration:
This statement is to certify that all Authors have seen and approved the manuscript being submitted, there is no conflict of interests.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. [Accessed July 4, 2012]; http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf.
- 2.World Health Organization. Geneva: WHO; 2011. Noncommunicable diseases country profiles. [Google Scholar]
- 3.World Health Organization. Geneva: WHO; 2011. Global status report on noncommunicable diseases 2010. Description of the global burden, their risk factors and determinants. [Google Scholar]
- 4.Cohen BE, Schultz A, McGibbon E, et al. A Conceptual Framework of Organizational Capacity for Public Health Equity Action (OC-PHEA) Can J Public Health. 2013 May-Jun;104(3):e262–e266. doi: 10.17269/cjph.104.3735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Nations. United Nations General Assembly resolution 66/2. [Accessed September 19, 2011]; http://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/66/2. [Google Scholar]
- 6.WHO. Geneva: WHO; 2013. [27 May 2013]. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. In: Follow-up to the Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. Sixty-Sixth World Health Assembly. [Google Scholar]
- 7.Latham J, Murajda L, Forland F, Jansen A. Capacities, practices and perceptions of evidence-based public health in Europe. Euro Surveill. 2013;18(10) doi: 10.2807/ese.18.10.20421-en. [DOI] [PubMed] [Google Scholar]
- 8.Marketing the heart health vision: delivering the “preventive dose”. Ottawa, Canada: Health Canada; 2000. WHO Collaborating Centre for Policy Development in the Prevention of Noncommunicable Disease. [Google Scholar]
- 9.World Health Organization Regional Office for Europe. Report on the 23rd Annual Meeting of Countrywide Integrated Noncommunicable Diseases Intervention (CINDI) Programme Directors. Paper presented at: CINDI Meeting; October 16–17, 2006; Banff, Canada. 2009. [Google Scholar]
- 10.Koplan JP, Puska P, Jousilahti P, Cahill K, Huttunen J. Improving the world's health through national public health institutes. Bull World Health Organ. 2005 Feb;83(2):154–157. [PMC free article] [PubMed] [Google Scholar]
- 11.Puska P, Stahl T. Health in all policies-the Finnish initiative: background, principles, and current issues. Annu Rev Public Health. 2010;31:315–328. 313. doi: 10.1146/annurev.publhealth.012809.103658. following 328. [DOI] [PubMed] [Google Scholar]
- 12.Beaglehole R, Dal Poz MR. Public health workforce: challenges and policy issues. Hum Resour Health. 2003 Jul 17;1(1):4. doi: 10.1186/1478-4491-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Institute of Medicine. The Future of the Public's Health in the 21st Century. Washington, DC: National Academies Press; 2003. [Google Scholar]
- 14.Cuijpers P, de Graaf I, Bohlmeijer E. Adapting and disseminating effective public health interventions in another country: towards a systematic approach. Eur J Public Health. 2005 Apr;15(2):166–169. doi: 10.1093/eurpub/cki124. [DOI] [PubMed] [Google Scholar]
- 15.Turnock BJ. Public Health: What it is and How it Works. Fourth. Sudbury, MA: Jones and Bartlett Publishers; 2009. [Google Scholar]
- 16.McKee M. The need for development assistance for health in the eastern European Region. Bull World Health Organ. 2005 Dec;83(12):883. [PMC free article] [PubMed] [Google Scholar]
- 17.Brownson RC, Baker EA, Leet TL, Gillespie KN, True WR. Evidence-Based Public Health. 2nd. New York: Oxford University Press; 2011. [Google Scholar]
- 18.Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health. 2002 Feb;56(2):119–127. doi: 10.1136/jech.56.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glasgow RE, Chambers D. Developing robust, sustainable, implementation systems using rigorous, rapid and relevant science. Clin Transl Sci. 2012 Feb;5(1):48–55. doi: 10.1111/j.1752-8062.2011.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green LW, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory, and knowledge dissemination, utilization, and integration in public health. Annu Rev Public Health. 2009 Jan 15; doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- 21.Canadian Institutes of Health Research. More About Knowledge Translation at CIHR. [Accessed June 16, 2013]; http://www.cihr-irsc.gc.ca/e/39033.html. [Google Scholar]
- 22.Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. Jama. 2004 Jun 2;291(21):2616–2622. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 23.Chokshi DA, Stine NW. Reconsidering the politics of public health. JAMA. 2013 Sep 11;310(10):1025–1026. doi: 10.1001/jama.2013.110872. [DOI] [PubMed] [Google Scholar]
- 24.Lameire N, Joffe P, Wiedemann M. Healthcare systems--an international review: an overview. Nephrol Dial Transplant. 1999;14(Suppl 6):3–9. doi: 10.1093/ndt/14.suppl_6.3. [DOI] [PubMed] [Google Scholar]
- 25.Magnusson RS. Global health governance and the challenge of chronic, non-communicable disease. J Law Med Ethics. 2010 Fall;38(3):490–507. doi: 10.1111/j.1748-720X.2010.00508.x. [DOI] [PubMed] [Google Scholar]
- 26.Cambon L, Minary L, Ridde V, Alla F. Transferability of interventions in health education: a review. BMC Public Health. 2012;12:497. doi: 10.1186/1471-2458-12-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cambon L, Minary L, Ridde V, Alla F. A tool to analyze the transferability of health promotion interventions. BMC Public Health. 2013 Dec 16;13(1):1184. doi: 10.1186/1471-2458-13-1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang S, Moss JR, Hiller JE. Applicability and transferability of interventions in evidence-based public health. Health Promot Int. 2006 Mar;21(1):76–83. doi: 10.1093/heapro/dai025. [DOI] [PubMed] [Google Scholar]
- 29.Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research: issues in external validation and translation methodology. Eval Health Prof. 2006 Mar;29(1):126–153. doi: 10.1177/0163278705284445. [DOI] [PubMed] [Google Scholar]
- 30.Daar AS, Singer PA, Persad DL, et al. Grand challenges in chronic non-communicable diseases. Nature. 2007 Nov 22;450(7169):494–496. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 31.WHO Regional Office for Europe. Copenhagen: WHO Europe; 2004. Policy Development and Implementation Processes in the CINDI and CARMEN Noncommunicable Disease Intervention Programmes. A Comparative Study. [Google Scholar]
- 32.WHO Regional Office for Europe. Copenhagen: WHO Europe; 2004. A strategy to prevent chronic disease in Europe. A focus on public health action. The CINDI vision. [Google Scholar]
- 33.WHO Regional Office for Europe. Copenhagen: WHO Europe; 2011. Strengthening of public health capacity and services for Europe: a framework for action. EUR/RC 61/10. [Google Scholar]
- 34.Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: A fundamental concept for public health practice. Annu Rev Public Health. 2009 Apr 21;30:175–201. doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- 35.Brownson RC, Diem G, Grabauskas V, et al. Training practitioners in evidence-based chronic disease prevention for global health. Promot Educ. 2007;14(3):159–163. [PubMed] [Google Scholar]
- 36.Gibbert WS, Keating SM, Jacobs JA, et al. Training the Workforce in Evidence-Based Public Health: An Evaluation of Impact Among US and International Practitioners. Prev Chronic Dis. 2013;10:E148. doi: 10.5888/pcd10.130120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.WHO. Geneva: WHO; 2013. May, The Millennium Development Goals and Tobacco Control: An Opportunity for Global Partnership. 2004. [Google Scholar]
- 38.WHO. Geneva: WHO; 2008. Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. [DOI] [PubMed] [Google Scholar]
- 39.WHO Regional Office for Europe. Copenhagen: WHO Europe; 2012. Health 2020: The European policy for health and wellbeing. [Google Scholar]
- 40.Barr V, Pedersen S, Pennock M, Rootman I. Ottawa, Ontario: Public Health Agency of Canada and World Health Organization; 2008. Health equity through intersectoral action: An analysis of 18 country case studies. [Google Scholar]
- 41.Best A, Moor G, Holmes B, et al. Health promotion dissemination and systems thinking: towards an integrative model. Am J Health Behav. 2003 Nov-Dec;27(Suppl 3):S206–S216. doi: 10.5993/ajhb.27.1.s3.4. [DOI] [PubMed] [Google Scholar]
- 42.Best A, Riley B, Norman C. Evidence Informed Public Health Policy and Practice through a Complex Lens: A Rapid Review. Ottawa, ON: Public Health Agency of Canada; 2007. [Google Scholar]
- 43.Hanson K, Ranson K, Oliveira-Cruz V, Mills A. Expanding access to priority health interventions: a framework for understanding the constraints to scaling-up. Journal of International Development. 2003;15:1–14. [Google Scholar]
- 44.Merzel C, D'Afflitti J. Reconsidering community-based health promotion: promise, performance, and potential. Am J Public Health. 2003 Apr;93(4):557–574. doi: 10.2105/ajph.93.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review--a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005 Jul;10(Suppl 1):21–34. doi: 10.1258/1355819054308530. [DOI] [PubMed] [Google Scholar]
- 46.Petticrew M, Tugwell P, Welch V, et al. Better evidence about wicked issues in tackling health inequities. J Public Health (Oxf) 2009 Sep;31(3):453–456. doi: 10.1093/pubmed/fdp076. [DOI] [PubMed] [Google Scholar]
- 47.Saan H. The road to evidence: the European path. Promot Educ. 2005;(Suppl 1):6–7. 41–42, 51–42. doi: 10.1177/10253823050120010102x. passim. [DOI] [PubMed] [Google Scholar]
- 48.Hamm MP, Chisholm A, Shulhan J, et al. Social media use by health care professionals and trainees: a scoping review. Acad Med. 2013 Sep;88(9):1376–1383. doi: 10.1097/ACM.0b013e31829eb91c. [DOI] [PubMed] [Google Scholar]
- 49.Bowen S, Zwi AB. Pathways to "evidence-informed" policy and practice: a framework for action. PLoS Med. 2005 Jul;2(7):e166. doi: 10.1371/journal.pmed.0020166. [DOI] [PMC free article] [PubMed] [Google Scholar]