Abstract
The Parinaud oculoglandular syndrome is a rare eye disease caused by different etiologic agents, including bacteria, viruses and fungi. It is characterized by a granulomatous conjunctivitis, accompanied by adjacent preauricular lymphadenopathy and can bring consequences if not treated promptly. We present a case of Parinaud oculoglandular syndrome caused by Sporothrix schenckii from the sporotrichosis epidemic in its zoonotic form occurring in Rio de Janeiro, Brazil.
Keywords: Syndrome, Eye, Fungi, Sporothrix schenckii, Sporotrichosis, Epidemic, Zoonotic
Introduction
Parinaud oculoglandular syndrome is a rare eye disease caused by different etiologic agents, including bacteria, viruses and fungi. It is characterized by a granulomatous conjunctivitis, accompanied by adjacent preauricular lymphadenopathy which is almost always caused by local trauma and can bring consequences if not treated promptly. We present a case caused by the dimorphic fungus Sporothrix schenckii from the sporotrichosis epidemic occurred in Rio de Janeiro, Brazil.
Case report
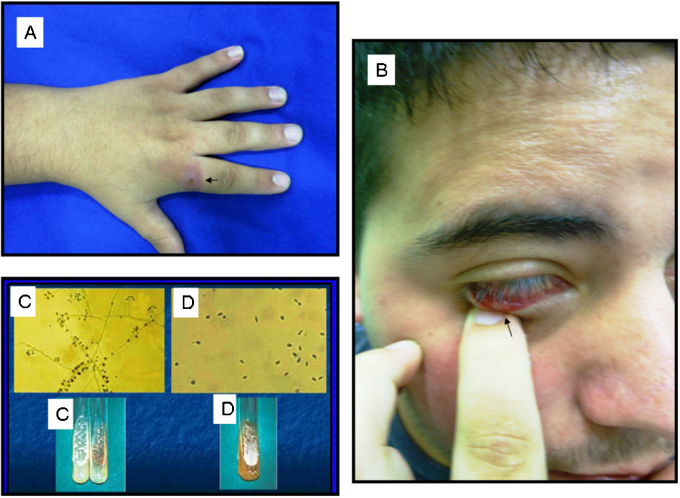
Male, 21 years-old, single, student, resident in Seropedica city/Rio de Janeiro state/Brazil. Refers to appearance of a finger injury two months after a sick cat scratch with subsequent involvement of the eye. The clinical examination presents erythematous crusted lesion of 0.3 cm in size, located on the index finger (Fig. 1A) and in the right eye was observed a small rounded painful lesion with sessile base and soft consistency, located in the lower tarsal conjunctiva (Fig. 1B) and preauricular lymphadenopathy. A fungal culture was realized with isolation of the fungus S. schenckii (Fig. 1C and D). Itraconazole 100 mg day was administered and the patient is in regular monitoring in Dermatology and Ophthalmology Departments.
Fig. 1.
(A) Erythematous crusted lesion on the index finger. (B) Small rounded lesion in the lower tarsal conjunctiva. (C) Sporothrix schenckii: this fungus is dimorphic with a mycelial phase (25 °C). (D) Sporothrix schenckii: this fungus is dimorphic with a yeast phase (37 °C).
Discussion
Parinaud's oculoglandular syndrome is a curious medical condition and it has been associated with several different infectious diseases, especially to cat scratch disease (Bartonella henselae), but sometimes it has been reported in granulomatous chronic infectious like tuberculosis, atypical mycobacteria and syphilis [1] and even some viruses (herpes simplex virus) [2]. Fungal infections also have been associated to this syndrome especially sporotrichosis (S. schenckii) [3], blastomycosis (Blastomyces dermatitidis) [4] and coccidioidomycosis (Coccidioides immitis) [5]. Sporotrichosis is a subacute or chronic mycosis that affect all ages, currently distributed throughout the world, especially in tropical and subtropical zone [6]. Infection almost always occurs by traumatic inoculation of soil, plants and organic matter contaminated with fungus [6] and may be localized in the conjunctiva as a primary infection or may be secondary involving of the eyelid and face [7]. Numerous soft, yellow, granulomatous nodules, which may ulcerate, develop in the palpebral or bulbar conjunctiva of the involved eye [7]. The preauricular and submandibular lymph nodes are grossly enlarged and may suppurate [7]. There is no evidence how the infectious agent has been disseminated throughout the Rio de Janeiro municipality and its outskirts, but it is beyond reasonable doubt that the close interaction with cats represents a key form of transmission of the fungus [8], [9], [10]. Felines have very close contact with contaminated soil and organic matter and constitute a reservoir of this agent [11]. The gold standard for sporotrichosis diagnosis is culture [6] and drug of choice to treat these patients has been oral itraconazole [6]. Ophthalmologists and dermatologists must be aware of its occurrence especially in endemic regions in order to avoid diagnostic pitfalls.
Authors’ contributions
Cassio Porto Ferreira and JoséAugusto da Costa Nery: clinical care and paper preparation. Ana Cristina Oliveira de Almeida: laboratorydiagnosis, paper preparation and English review. Luiz Cláudio Ferreira: technical support. Suzana Corte-Real and Fátima Conceição-Silva: laboratory diagnosis and paper preparation.
Conflict of interest statement
None.
Role of funding source
None.
Ethical approval
The authors declare that a written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. Ethics committee approval: CEP 14/2001 Instituto Oswaldo Cruz–CPqHEC/FIOCRUZ.
Acknowledgement
The authors thank Dr Euzenir Nunes Sarno, PhD, for the support and valuable tips.
References
- 1.Huang M.C., Dreyer E. Parinaud's oculoglandular conjunctivitis and cat-scratch disease. Int Ophthalmol Clin. 1996;36(3):29–36. doi: 10.1097/00004397-199603630-00005. [DOI] [PubMed] [Google Scholar]
- 2.Caputo G.M., Byck H. Concomitant oculoglandular and ulceroglandular fever due to herpes simplex type I. Am J Med. 1992;93:577–580. doi: 10.1016/0002-9343(92)90588-3. [DOI] [PubMed] [Google Scholar]
- 3.Ribeiro A.S.A., Bisol T., Menezes M.S. Síndrome oculoglandular de Parinaud causada por esporotricose. Rev Bras Oftalmol. 2010;69(5):317–322. [Google Scholar]
- 4.Bartley G.B. Blastomycosis of the eyelid. Ophthalmology. 1995;102:2020–2023. doi: 10.1016/s0161-6420(95)30760-9. [DOI] [PubMed] [Google Scholar]
- 5.Wood T.R. Ocular coccidioidomycosis. Report of a case presenting as Parinaud's oculoglandular syndrome. Am J Ophthalmol. 1967;64(3):587–590. [PubMed] [Google Scholar]
- 6.Lopes-Bezerra L.M., Schubach A.O., Costa R.O. Sporothrix schenckii and sporotrichosis. An Acad Bras Cienc. 2006;78:293–308. doi: 10.1590/s0001-37652006000200009. [DOI] [PubMed] [Google Scholar]
- 7.Hampton D.E., Adesina A., Chodosh J. Conjunctival sporotrichosis in the absence of antecedent trauma. Cornea. 2002;21:831–833. doi: 10.1097/00003226-200211000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Schubach A.O., Barros M.B.L., Wanke B. Epidemic sporotrichosis. Curr Opin Infect Dis. 2008;21:129–133. doi: 10.1097/QCO.0b013e3282f44c52. [DOI] [PubMed] [Google Scholar]
- 9.Schubach A.O., Schubach T.M., Barros M.B. Epidemic cat-transmitted sporotrichosis. N Engl J Med. 2005;353(11):1185–1186. doi: 10.1056/NEJMc051680. [DOI] [PubMed] [Google Scholar]
- 10.Ferreira C.P., do Valle A.C.F., Freitas D.F.S., Reis R., Galhardo M.C.G. Pregnancy during a sporotrichosis epidemic in Rio de Janeiro, Brazil. Int J Gynaecol Obstet. 2012;117:294–295. doi: 10.1016/j.ijgo.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Dustan R.W., Reiman K.A., Langhan R.F. Feline sporothricosis. J Am Vet Med Assoc. 1986;189:880–883. [PubMed] [Google Scholar]