Abstract
Modular hip replacement components offer numerous advantages, and the modular femoral component has become standard for contemporary total hip implants. Recent reports of mechanically assisted crevice corrosion (MACC) at the head-neck junction, and associated adverse local tissue reactions (ALTRs), have renewed concerns for complications attributed to modularity. This manuscript describes the diagnosis, prognosis, and treatment options for MACC and highlights how appropriate pre-revision evaluation and planning, in conjunction with meticulous surgical technique, should be followed to avoid complications and achieve optimal surgical outcomes. Future directions for research include biomechanical, clinical, and retrieval studies.
Keywords: Total hip arthroplasty, Revision total hip arthroplasty, Trunnion, Mechanically assisted crevice corrosion (MACC), Modular taper corrosion, Adverse local tissue reaction (ALTR)
Introduction
Adverse local tissue reaction (ALTR) associated with mechanically assisted crevice corrosion (MACC) is the biological reaction to corrosion and debris products from a junction of an implant where at least one of the two members is fabricated from metal alloy [1,2]. Jacobs and colleagues have noted that, to date, this phenomenon has been only described for cobalt-chromium (CoCr) alloys [3]. MACC may occur at any such junction, but this manuscript will focus on the head-neck junction of femoral hip replacement implants. MACC, the concept of a combination of fretting and crevice corrosion causing breakdown at the femoral head-neck taper in modular implants, was first reported in 1981 [4] and appears to be increasing in prevalence [2,5•]. The process may occur in metal-on-polyethylene (MoP), metal-on-metal (MoM), and metal-on-ceramic (MoC) articulations.
Diagnosis
Our current definition of MACC agrees with that recently reported by the Rush University group [6•]. They found that patients who present with new onset of postoperative pain, in whom the implants are well fixed and infection has been ruled out, should be evaluated with serum cobalt (Co) and chromium (Cr) levels. In the reported population, patients initially presented with new pain at a mean of 4.3 years (range, 0.4–25.1 years) after their index surgery [6•]. Because a prior study from their institution that followed serum Co and Cr levels over time in successful hip replacements showed no patient had a serum Co greater than 1 part per billion (ppb) [7•], they suggest that 1 ppb is the minimum Co requirement for the diagnosis of MACC in patients with MoP total hip arthroplasty (THA). We have also found that intra-articular (IA) serum levels of Co and Cr, although not mandatory, can be helpful in confirming MACC [8]. This is particularly helpful in patients with inconclusive symptoms, bilateral THA, or transient pain. We have found that IA Co levels are elevated on average 137 times (range, 31–279 times) the serum levels. IA Cr levels average 320 times higher (range, 20–834 times).
The diagnosis of MACC in patients with MoM hips is more complex because of the ionic contribution of the surface wear (and therefore higher acceptable Co levels). A minimum Co requirement for the diagnosis of MACC in MoM hips is not known. A disproportionate elevation of Co over Cr appears to be a common finding in corrosion failure, presumably because of precipitation of chromium ortho-phosphate (CrPO4) as a corrosion product. The Co to Cr ratio may therefore be helpful, but is not pathognomonic of MACC. Although Plummer and colleagues found that the abnormal serum Co level was significantly elevated above the serum Cr level (by a mean 11 to 2 ppb ratio) in MACC [6•], less dramatic but asymmetrical ratios have been described with metal-on-metal total hip replacements [9], and this disproportionate ratio is not present in all MACC cases [10]. Further, Fehring and colleagues have found that the Co:Cr ratio is not a predictive biomarker for ALTR (they looked at metal-on-metal total hip replacement only) [9].
It is important to note that the new onset of pain, stiffness, or dysfunction after successful arthroplasty outcome is not MACC or ALTR in the majority of cases. The clinician should consider common intra- and extra-articular causes of postoperative pain as part of the work-up, including infection, loosening, stress reaction, tendonitis, bursitis, and referred pain [11–13]. In addition to careful comparison of serial orthogonal radiographs, erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP) should also be obtained. In MACC, radiographs may show osteolysis (60 % of patients (9/15) in one study [5•]), although it may be subtle (Fig. 1). Metal artifact reduction sequence (MARS) magnetic resonance imaging (MRI), obtained if there is suspicion of MACC-causing ALTR, may be read as normal in 31 % (4/13) of cases [5•]. Characteristics of MACC-associated ALTR on MRI have not been specifically described, but positive findings may include fluid collections, capsular thickening, synovitis, osteolysis, bone and muscle edema, tendon disruptions, and so called “pseudotumors” [15]. Of note, one study examining CoP hip replacements with MRI found 18 % had periprosthetic fluid collections, so fluid alone may not be a reliable sign of ALTR [16].
Fig. 1.
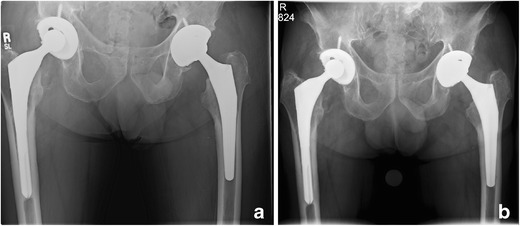
Anteroposterior (AP) pelvis radiograph showing bilateral total hip arthroplasties (THA) and immediate postoperative view of left THA (a), and 3-year follow-up of left THA, and 6-year postoperative view of right THA (b), with highly crosslinked polyethylene (HXLPE) liners and cobalt alloy femoral heads. There is no evidence of infection on work-up, but note progressive femoral osteolysis in zones 1 and 7 [14] of the left hip (right side of radiograph) consistent with mechanically assisted crevice corrosion (MACC)
Prognosis
The prognosis of MACC is currently not very well understood. Of particular concern is the fact that, unlike osteolysis from particulate debris, irreversible soft tissue damage to the supporting musculature and hip capsule may occur in the most serious cases. In our study of 15 patients [5•], the 3 patients with symptoms lasting the longest (average 38 months; range 34–43 months) had the most irreversible and destructive changes and required constrained reconstruction. The remaining 9 patients that had undergone surgery had symptoms on average 8.7 months (range, 3–24 months). In Plummer and colleagues’ study, 13 of 27 patients ultimately had need of a constrained acetabular liner, because of severe damage of the abductors [6•].
Many factors may affect the prognosis of patients with MACC, and these have yet to be elucidated. When followed over 10 years, serum metal ion levels vary in patients with well-functioning THAs, depending on the specific type of prosthesis used [7•]. However, the Co level remained less than 1 ppb in this cohort, and it is unclear if there is a gradual increase in corrosion products from all tapers or if some tapers have significant corrosion and others do not. Retrieval analysis seems to support the latter hypothesis [2,17]. MACC is both a chemical and mechanical process; patient and implant characteristics as well as biomechanical reconstruction parameters likely contribute to the ultimate degree of taper damage.
Currently, in patients with mild or transient symptoms and a normal MARS MRI, we consider following the patient with serial serum Co and Cr levels at 6-month intervals and MARS MRI at 6 months, 1 year, and yearly (until more is known about this process). If the patient is participating in high-impact activities, we recommend that they stop, in order to diminish peak forces transmitted to the prosthesis. Toxicology consultation may be indicated if the metal levels are greater than 10 ppb and systemic symptoms are present [18]. If a patient chooses to accept the risks of surgery, we will consider revision once MACC is confirmed by at least two elevated serum metal ion levels.
We are following a number of patients with bilateral THA and surgically treated MACC on only one side. The prognosis is unknown for the uninvolved hip, but we are currently recommending careful surveillance follow-up and would consider checking serum Co and Cr levels if otherwise unexplained symptoms occur.
Long-term prognosis after revision surgery for MACC is guarded, and ongoing research is needed. In our experience, the Co level falls more precipitously than the Cr level, after removal of the cobalt-chrome alloy femoral head and cleaning of the taper. The degree of soft tissue damage found at revision surgery is likely to positively correlate with the risk of hip instability, infection, and prosthesis loosening. It is unknown at this time if either the level or duration (or both) of intraarticular or serum ions, corrosion products, and/or fretting products correlates with the patient’s symptoms or tissue damage. There may be patient factors that attenuate or augment response [19].
Functional outcome and patient-reported outcome measures (PROMs) after revision for MACC have not yet been reported; in our experience, there is a range of outcomes. In a subset of patients treated for MACC with conversion to a ceramic head, serum Co and Cr levels decreased at a mean follow-up of 2.7 years and all Co levels were less than 1 ppb [6•]. For the cohort as a whole, at a mean follow-up of 25 months (range, 2–48 months), the average Harris hip score improved from a mean of 56.5 to a mean of 86.5 after surgery [6•].
Treatment options
Once the diagnosis has been made and the prognosis is reviewed with the patient, a shared decision-making discussion should be initiated. Revision surgery should be considered in patients with pain, stiffness, and dysfunction [5•,6•,13], as well as those that are less symptomatic with evidence of very high systemic ion levels [18], progressive bone loss, or evidence of soft tissue pathology in the affected hip on MARS MRI.
If the surgeon opts to treat the patient non-operatively, careful ongoing clinical assessments to rule out Trendelenburg limp, new abductor weakness, or soft tissue swelling/vascular obstruction are imperative. Based on the incomplete current understanding of this malady, interval 6-month clinical exams seem be a practical approach. Laboratory testing at 6–12-month intervals (serum Co and Cr) and MARS MRI examinations yearly are a conservative but appropriate approach, knowing that irreversible soft tissue damage can occur [5•]. This recommendation may be changed as more information about the natural history of MACC becomes available.
If surgery is pursued, it is essential to rule out concomitant periprosthetic joint infection (PJI), loosening, and other causes of pain. These diagnoses may occur in conjunction with MACC. Yi and co-authors have addressed the possibility that synovial tests might help diagnose infection in revision THA for corrosion [20]. In the subgroup of patients in their study with non-MoM bearings (n = 30) with corrosion, the data for diagnostic performance was no different than the larger group of 150 samples. The authors concluded that PJI is extremely difficult to diagnose when it occurs with MACC, and the synovial fluid white blood count (WBC) can frequently be falsely positive. A manual count of the cells is necessary in cases of corrosion because metal or amorphous material, fragmented cells, or clots make the sample inaccurate in one third of cases. When a manual count is performed, synovial fluid WBC count and differential were helpful in diagnosing PJI: the optimal cutoffs found were 4350 WBC/μL and 85 % PMN, respectively.
The surgeon must next be prepared for instability from soft tissue loss and necrosis. Either larger revision ceramic heads or constrained components [21] should be available at the time of revision; of note, use of a titanium revision sleeve and a ceramic head with constrained liners may not be Food and Drug Administration (FDA) approved. “Off-label” usage should be discussed with the patient pre-operatively and makes sense in our practice based on previous successful reports in the literature [6•] as well as our own experience [5•].
The primary goal of revision surgery is to remove the generator of the Co and Cr ions. Secondary goals include repair of soft tissues and restoration of hip stability. Again, as we do not thoroughly understand the major mechanical contributing factors to MACC, removal of the offending implant makes practical sense. Based on the RUSH University experience with successful revision of constructs that include well-fixed cobalt alloy stem stems by changing only the femoral head [6•], it seems that in MoP constructs with MACC that the head may be the primary source of ion fretting and corrosion products. Therefore, we recommend at a minimum revising to a BIOLOX revision femoral head, with a titanium sleeve (CeramTec GmbH, Plochingen, Germany), or an OXINIUM oxidized zirconium (Smith and Nephew, Memphis, Tennessee, USA) that is compatible with the taper of the femoral component being revised.
The taper must first be cleaned (we use a surgical sponge and saline at first and a more abrasive surface, such as a clean disposable scratch pad (Bovie Medical Corp., Clearwater, Florida, USA), if necessary) and then examined. If there is destructive corrosion that compromises the mechanical integrity of the stem [2,22], even a well-fixed femoral component should be replaced using contemporary revision techniques. Examples of tapers that cannot safely accept the revision sleeve include a slanted stem taper, a stem taper with broad truncation, and a crushed stem taper [22].
Other options, when a revision ceramic head is not available through the manufacturer for a given taper, include use of a custom titanium sleeve [10] (Fig. 2) or BioBall universal modular neck adapter (Merete Medical Inc., Berlin, Germany).
Fig. 2.
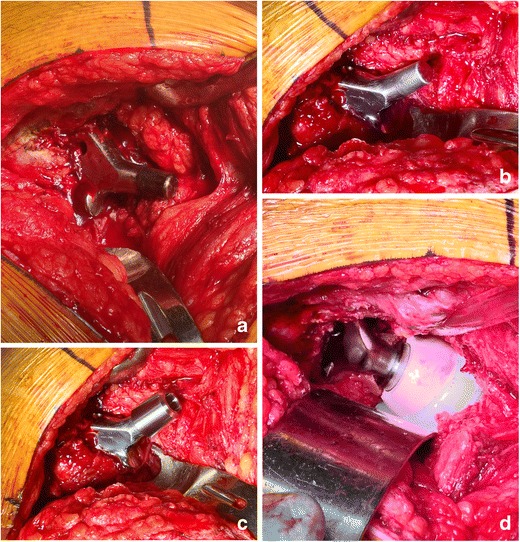
Intra-operative photographs of a THA revision for MACC demonstrating a black corrosion on non-contemporary trunnion, b cleaned trunnion, c custom titanium sleeve to allow use of ceramic femoral head, and d reduced THA with new HXLPE liner and ceramic revision femoral head
The acetabular side of the hip construct should also be addressed in cases of MACC, in our opinion. A modular liner exchange should be considered, where appropriate. In MoP constructs, third body corrosion and fretting products have likely damaged the polyethylene and may even be embedded. Metal-on-metal (MoM) constructs are more complicated. For modular acetabular components that are well positioned, we recommend removing the cobalt alloy liner, cleaning the taper surface, and revising to a highly cross-linked polyethylene (HXLPE) liner if the locking mechanism is intact. If the metal liner cannot be removed, we recommend explantation of the entire component and revision to a titanium or tantalum shell with a ceramic or HXLPE liner. If a monolithic cobalt alloy acetabulum is well fixed and in satisfactory position, the surgeon may consider converting the femoral side to a modular, dual-mobility-style femoral component. What that allows is a less destructive acetabular revision and conversion of the femur to a ceramic head in conjunction with a HXLPE head. Although the cobalt alloy monolithic shell is left in the patient, there are no surfaces subject to significant friction or corrosion. This may also be an “off-label” usage.
Care should be paid to restore soft issues that are available, and we have reattached indurated and friable abductors with suture anchors. Hip abductor bracing should be considered in the postoperative period if needed to maximize stability during healing. We currently remove devitalized tissue that is expendable, wash with antibiotic irrigation, and continue antibiotics for 24 h. We have reported a deep surgical infection rate of 1/12 [5•] and Plummer and colleagues reported 1/27 [6•] for a total of 2/39 (5.1 %), which is a higher infection rate than one would expect for revision hip surgery in general. This likely relates to the toxic effect of the ions and metallic debris as well as the associated devitalized tissue [23].
Complications and long-term issues
Serum metal ions are not always dramatically elevated in MACC, particularly in MoP cases. If systemic illness does occur, prognosis is best addressed by toxicologists [18].
More commonly, local tissue toxicity is more relevant, and we have demonstrated consistently toxic levels Co and Cr in IA aspirations of patients with MACC [8]. Susceptibility to periprosthetic infection, tissue necrosis, joint fluid cell death, aseptic lymphocyte-dominated vasculitis-associated lesions (ALVALs) and elevations in peripheral white blood cells, ESR, and CRP have all been described [5•,6•]. We have also seen two cases of late loosening of the acetabular component, which we think are related to progressive bone death and a type of “biological momentum” of necrosis, even after the cobalt generator (i.e., the cobalt alloy femoral head) has been removed.
The most prevalent short-term issues associated with MACC in the limited reports to date include hip instability and gait abnormality associated with periarticular tissue necrosis. This is a very serious problem because this appears to be a permanent ramification of MACC.
Revision to a ceramic femoral head does potentially carry the risk of ceramic fracture. Fracture debris can be very challenging to remove and make revision surgery fraught with complexity [24,25]. BIOLOX delta femoral heads, a so-called “fourth-generation ceramic,” has a very low fracture rate [26], and revision head fracture has not been reported, to our knowledge.
Careful patient follow-up of revision surgeries is indicated until longer term studies are available. Co and Cr ion levels almost always decrease over time after revision, although Cr levels seem to diminish less rapidly. We have seen a variation in clinical results after revision, somewhat depending on the degree of soft tissue loss and damage at the time of revision. We have also witnessed cases of late prosthesis loosening that we think may be related to biological progression of necrosis, even after revision to a non-cobalt head.
Prevention
Until MACC is understood more completely, the clinician should, in our opinion, take steps aimed at minimizing the possibility of ALTR after THA. Elimination of cobalt-alloy femoral heads seems prudent. Use of third-generation ceramics such as BIOLOX delta (CeramTec GmbH, Plochingen, Germany) or OXINIUM oxidized zirconium (Smith and Nephew, Memphis, Tennessee, USA) for primary and revision THA surgery makes sense. In revision surgery, use of a titanium ceramic sleeve with a ceramic femoral head is recommended to avoid ceramic fracture due to stress risers generated in the previously used trunnion.
In some studies, high construct offset, patient BMI, longer implant necks, and larger femoral heads have been associated with MACC [27]. If metal heads are employed, a clean, dry taper, optimum impaction technique, and minimum appropriate head size and construct offset may be important.
Surgeons should follow all arthroplasty patients with routine surveillance visits and consider checking laboratory values of Co and Cr if the patient presents with unexplained pain when loosening and infection are ruled out. We currently do not screen all patients for MACC but have a high level of suspicion if symptoms are present.
Future directions
MACC is incompletely understood, and future research should focus on biomechanical, clinical, and retrieval studies that elucidate its cause and treatment. Clinical studies outlining diagnosis, prognosis, and management will complement those that look at causative factors leading to failure due to corrosion at the head/neck taper. In vitro biomechanical studies of taper adhesion and fretting corrosion, possibly using wear simulation machines, may also be helpful. Finally, retrieval analysis of both corroded and functioning tapers may elucidate the mechanism of this problem.
Conclusions
Modular hip replacement components offer numerous advantages and are likely not going to be replaced by monolithic stems. MACC at the head-neck junction is now recognized as causing ALTR at a higher prevalence than when modularity was first introduced. This manuscript describes the current knowledge about diagnosis, prognosis, and treatment options for MACC and highlights how appropriate pre-revision evaluation and planning, in conjunction with meticulous surgical technique, should be followed to avoid complications and achieve optimal outcomes in its treatment.
Compliance with ethical standards
Conflict of interest
Brigham McKenney declares that he has no conflict of interest.
Brian J. McGrory has served as a consultant to Smith and Nephew, Inc., and as editor-in-chief of Arthroplasty Today.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Hip: Metal-on-Metal
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res. 1993;27(12):1533–1544. doi: 10.1002/jbm.820271210. [DOI] [PubMed] [Google Scholar]
- 2.Morlock MM. The taper disaster - how could it happen? Hip Int. 2015;25(4):339–346. doi: 10.5301/hipint.5000269. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs JJ, Cooper HJ, Urban RM, Wixson RL, Della Valle CJ. What we know about taper corrosion in total hip arthroplasty. J Arthroplasty. 2014;29:668–669. doi: 10.1016/j.arth.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 4.Lucas LC, Buchanan RA, Lemons JE. Investigations on the galvanic corrosion of multialloy total hip prostheses. J Biomed Mater Res. 1981;15(5):731–747. doi: 10.1002/jbm.820150509. [DOI] [PubMed] [Google Scholar]
- 5.•.McGrory BJ, MacKenzie J, Babikian G. A high prevalence of corrosion at the head-neck taper with contemporary Zimmer non-cemented hip components. J Arthroplasty. 2015;30(7):1265–1268. doi: 10.1016/j.arth.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 6.•.Plummer DR, Berger RA, Paprosky WG, Sporer SM, Jacobs JJ, Della Valle CJ. Diagnosis and management of adverse local tissue reactions secondary to corrosion at the head-neck junction in patients with metal on polyethylene bearings. J Arthroplasty. August 1 2015:. Follow-up manuscript to 2012 Journal of Bone and Joint Surgery study describing diagnosis and management of mechanically assisted crevice corrosion (MACC). The cohort has a majority of total hips of one vendor but describes the diagnosis in various designs and vendors. The authors show that in the short term a cobalt alloy stem that is well fixed may be left in place and revising the femoral head to a titanium sleeve and ceramic femoral head leads to a significant decrease in serum cobalt levels.
- 7.•.Levine BR, Hsu AR, Skipor AK, et al. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty. J Bone Joint Surg. 2013;95(6):512–518. doi: 10.2106/JBJS.L.00471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Payson AM, McGrory BJ, MacKenzie J. High intra-articular hip cobalt and chromium levels in mechanically assisted crevice corrosion. Paper presented at: Orthopaedic Research Society, 2016, 2015; Orlando, FL.
- 9.Fehring TK, Carter JL, Fehring KA, Odum SM, Griffin WL. Cobalt to chromium ratio is not a key marker for adverse local tissue reaction (ALTR) in metal-on-metal hips. J Arthroplasty. 2015;30(9 Suppl):107–109. doi: 10.1016/j.arth.2015.02.049. [DOI] [PubMed] [Google Scholar]
- 10.Leibiger T, McGrory BJ. Custom titanium sleeve for surgical treatment of mechanically assisted crevice corrosion in the well-fixed, non-contemporary stem in total hip arthroplasty. Arthroplasty Today. 2015;1(4):107–110. doi: 10.1016/j.artd.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lanting BA, MacDonald SJ. The painful total hip replacement. Diagnosis and deliverance. Bone Joint J. 2013;95-B(Supple A):70–73. doi: 10.1302/0301-620X.95B11.32948. [DOI] [PubMed] [Google Scholar]
- 12.Nam D, Nunley RM, Sauber TJ, Johnson SR, Brooks PJ, Barrack RL. Incidence and location of pain in young, active patients following hip arthroplasty. J Arthroplasty. 2015;30:1971–1975. doi: 10.1016/j.arth.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 13.Whitehouse MR, Endo M, Zachara S, et al. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J. 2015;97-B(8):1024–1030. doi: 10.1302/0301-620X.97B8.34682. [DOI] [PubMed] [Google Scholar]
- 14.Gruen T, McNeice G, Amstutz HC. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 15.Sana M, Morozov P, McGrory BJ, Farraher SJ, Abrahams TG. MRI findings of adverse local tissue reaction due to mechanically assisted crevice corrosion in total hip replacement, 2016.
- 16.Bisseling P, de Wit BW, Hol AM, van Gorp MJ, van Kampen A, van Susante JL. Similar incidence of periprosthetic fluid collections after ceramic-on-polyethylene total hip arthroplasties and metal-on-metal resurfacing arthroplasties: results of a screening metal artifact reduction sequence-MRI study. Bone Joint J. 2015;97-B(9):1175–1182. doi: 10.1302/0301-620X.97B9.35247. [DOI] [PubMed] [Google Scholar]
- 17.Collier JP, Surprenant VA, Jensen RE, Mayor MB. Corrosion at the interface of cobalt-alloy heads on titanium-alloy stems. Clin Orthop Rel Res. 1991;271:305–312. [PubMed] [Google Scholar]
- 18.Tower S. Arthroprosthetic cobaltism: identification of the at-risk patient. Alaska Med. 2010;52:28–32. [PubMed] [Google Scholar]
- 19.Pacheco KA. Allergy to surgical implants. J Allergy Clin Immunol Pract. 2015;3(5):683–695. doi: 10.1016/j.jaip.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Yi PH, Cross MB, Moric M, et al. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res. 2015;473(2):498–505. doi: 10.1007/s11999-014-3902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Velott T, McGrory BJ, Rana A. A second generation constrained acetabular component for treatment of complex hip replacement instability. Curr Orthop Pract. 2015;26(2):136–141. doi: 10.1097/BCO.0000000000000201. [DOI] [Google Scholar]
- 22.Zimmer I. Zimmer option technique; www.productcompatibility.zimmer.com.
- 23.Prieto HA, Berbari EF, Sierra RJ. Acute delayed infection: increased risk in failed metal on metal total hip arthroplasty. J Arthroplasty. 2014;29(9):1808–1812. doi: 10.1016/j.arth.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 24.Allain J, Roudot-Thoraval F, Delecrin J, Anract P, Migaud H, Goutallier D. Revision total hip arthroplasty performed after fracture of a ceramic femoral head. A multicenter survivorship study. J Bone Joint Surg. 2003;85-A(5):825–830. doi: 10.2106/00004623-200305000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Tai SMM, Parker L, de Roeck NJ, Skinner JA. Case report: recurrent catastrophic ceramic femoral head failure in total hip arthroplasty. Case Rep Orthop. 2014;2014:1–4. doi: 10.1155/2014/837954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Massin P, Lopes R, Masson B, Mainard D, Society TFHaK Does Biolox Delta ceramic reduce the rate of component fractures in total hip replacement. Orthop Tramatol: Surg Res. 2014;100(6):S317–321. doi: 10.1016/j.otsr.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 27.Hussenbocus S, Kosuge D, Solomon LB, Howie DW, Oskouei RH. Head-neck taper corrosion in hip arthroplasty. Biomed Research International. 2015;2015. [DOI] [PMC free article] [PubMed]


