Abstract
A platform system for shoulder arthroplasty can include a convertible modular humeral stem and/or a metal-backed glenoid component to facilitate straightforward conversion from either a hemiarthroplasty or anatomic total shoulder arthroplasty to a subsequent anatomic total shoulder arthroplasty, or more frequently, reverse total shoulder arthroplasty without any revision to the stem and/or glenoid baseplate. Recent studies have demonstrated a decreased rate of intraoperative humeral fracture, complications, and blood loss when a platform system is used and the humeral stem is not exchanged during revision arthroplasty. Future studies with larger patient cohorts are necessary to truly evaluate the potential value and limitations of this technology.
Keywords: Platform system, Total shoulder arthroplasty, Reverse total shoulder arthroplasty, Shoulder hemiarthroplasty, Revision shoulder arthroplasty
Introduction
The volume of shoulder arthroplasty procedures performed in the USA has increased substantially over the past decade, from 14,000 shoulder hemiarthroplasty (HA) and total shoulder arthroplasty (TSA) procedures performed in 2000 to over 46,000 performed in 2008, an increase of nearly 12 % per year [1]. If this trend continues, an estimated 100,000 shoulder arthroplasties will be performed annually this year [2]. While at least part of these increases are due to an aging population that desires to remain active, a large percentage of this increase is due to rising popularity of and expanding indications for reverse total shoulder arthroplasty (RTSA) [3•].
Accompanying this exponential increase in primary shoulder arthroplasty is an expected increase in the incidence of revision shoulder arthroplasty. The estimated rate of revision for failed shoulder arthroplasties has grown by 400 % over the last 20 years, making revisions account for up to 10 % of all shoulder arthroplasty [4–6]. Revision shoulder arthroplasty is most often indicated for multiple modes of failure, with glenoid component loosening being the most common. Revision arthroplasty can be significantly more challenging than the index procedure due to the frequent need for component removal, which can lead to bone loss [7].
Recently, due to success of reverse total shoulder arthroplasty for rotator cuff tear arthropathy, the indications have expanded to use of this procedure as a revision option or salvage for failed prior arthroplasty, including revision of failed shoulder hemiarthroplasty or failed anatomic shoulder arthroplasty [8, 9•]. Conversion of prior arthroplasty to a reverse shoulder arthroplasty can be technically demanding and fraught with complications. These challenges led to the recent introduction of a platform system for shoulder arthroplasty, which can include a convertible modular humeral stem and/or a metal-backed glenoid component to facilitate straightforward conversion from either a hemiarthroplasty or anatomic total shoulder arthroplasty (ATSA) to a RTSA without removal of the stem or glenoid baseplate [10•].
Uses and advantages of a platform system
A platform system for shoulder arthroplasty offers system flexibility and interchangeability for subsequent revision surgery. This would allow, in theory, for a less demanding and time-consuming revision surgery, and potentially reduce complications associated with the removal of glenoid or humeral components. A platform system consists of two potential modular components: a versatile humeral stem and a metal-backed glenoid component.
Humeral stem in a platform system for shoulder arthroplasty
Conversion of a traditional HA or ATSA to RTSA requires the removal and reimplantation of a humeral stem. As humeral stem loosening is exceedingly rare due to good integration with host bone, humeral shaft corticotomy is often required for stem removal, which is associated with a high rate of fracture [11, 12]. Additional fracture risk may rise from cerclage wire fixation which may be required to stabilize diaphyseal osteotomies or from diaphyseal perforation of the revision stem. One recent study noted a 21 % intraoperative humeral shaft or tuberosity fracture rate during stem removal during conversion to RTSA [13]. Other studies have noted humeral fracture rates of up to 25 % during stem removal at revision [10•, 12, 14, 15]. Additional risks of humeral stem removal include potential loss of humeral bone stock, nerve injury, periprosthetic fracture, and malunion or nonunion of a humeral osteotomy with later humeral component loosening [11, 14, 16, 17•].
The use of a platform system allows conversion of a hemiarthroplasty or ATSA to RTSA without removal of the humeral stem (Table 1). Compared to patients in whom stem removal is required, this virtually eliminates the risk of intraoperative humeral fracture. A recent study reported a 0 % rate of humeral tuberosity or shaft fractures in patients with platform humeral stems converted to RTSA [13]. A similar study of 26 patients with full modular stems likewise reported no intraoperative humeral complications [18].
Table 1.
Current commercially available platform systems in the USA
| Manufacturer/name | HA option? | ATSA option? | RTSA option? |
|---|---|---|---|
| Biomet Comprehensive | Yes | Yes | Yes |
| Depuy Global Unite | Yes | Yes | Yes |
| Exactech Equinoxe | Yes | Yes | Yes |
| Tornier Ascend Flex | Yes | Yes | Yes |
| Integra Titan | Yes | Yes | Yes |
| Smith & Nephew PROMOS | Yes | Yes | Yes |
| Lavender Medical UNIC | Yes | Yes | Yes |
HA hemiarthroplasty, ATSA anatomic total shoulder arthroplasty, RTSA reverse total shoulder arthroplasty
Metal-backed glenoid component in a platform system for shoulder arthroplasty
Glenoid component loosening is one of the most common complications in ATSA and represents 25 % of all complications related to TSA [19]. Often, glenoid component loosening is not isolated, but combined with a rotator cuff tear, glenohumeral instability or component malposition [20]. Glenoid revision is indicated for painful glenoid loosening or glenoid malposition or wear in instances where the rotator cuff remains competent. Often, as mentioned before, glenoid bone loss and rotator cuff deficiency, particularly the subscapularis, often necessitate conversion to a glenosphere for RTSA at the time of revision [10•]. A platform system utilizes a versatile metal-backed glenoid that allows simple exchange of the polyethylene component when revising ATSA, or conversion to a glenosphere when converting from ATSA to RTSA.
Metal-backed glenoids are not a new concept; they have been debated since Neer and colleagues published their results in the 1980s [21]. Numerous authors have published failures of metal-backed components. Taunton and co-authors reported on 83 ATSA with a metal-backed, bone-ingrowth glenoid component and found a 40 % rate of glenoid component loosening and 25 % rate of polyethylene wear with metal wear of the glenoid component [22]. Boileau, et al reported a 20 % loosening rate of metal-backed glenoid components compared to 0 % in all polyethylene glenoids in a prospective study of 40 patients undergoing ATSA [23]. Improvements in modern implant design may ameliorate these issues, as a recent study that included twelve primary platform ATSA with metal-backed glenoid components revised to RTSA did not report any metal-backed glenoid revisions [10•].
Clinical outcomes using platform systems
As platform systems are a relatively new advent in the evolution of shoulder arthroplasty design, only limited case series exist describing clinical outcomes utilizing such technology. Castagna, et al recently published a series of 26 patients who underwent conversion of a previous shoulder arthroplasty to an RTSA using a platform system [18]. The index operation in 18 of the patients was hemiarthroplasty for fracture; the remaining 8 patients had an ATSA for glenohumeral arthritis. The authors reported that the use of a fully modular system allowed avoidance of humeral stem removal in all patients, and the metal-back glenoid in revision of ATSA, resulting in a short operative time and few intraoperative complications (Fig. 1). At an average of 32 months follow-up, the average constant score improved from 25 points to 48 points, while the EuroQol Visual Analog Scale (EQ-VAS) improved from 40 preoperatively to 70 postoperatively. All patients improved in terms of range of motion and follow-up imaging obtained at final follow-up demonstrated good integration of the implants without any evidence of loosening [18].
Fig. 1.
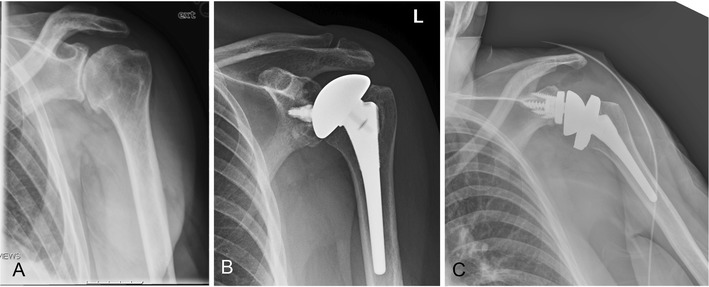
A 72-year-old female with left shoulder pain due to osteoarthritis (a) underwent anatomic total shoulder arthroplasty using a convertible humeral stem (b). She later fell and suffered a subscapularis rupture, which failed primary repair. She was later converted to an RTSA, maintaining her previous stem, with an excellent functional result (c)
A recent study published by Wieser, et al evaluated outcomes in 48 patients with hemiarthroplasties and eight patients with ATSA converted to RTSA with (n = 43) and without (n = 13) stem exchange to elucidate potential advantages of a platform system [17•]. The authors found significantly shorter surgical time and lower average blood loss in patients without stem exchange. Intraoperative complications were also significantly lower in patients without stem exchange (8 %) compared to patients with stem exchange (30 %). Clinical outcomes were assessed in patients who did not have intraoperative complications. Average Constant scores improved from 30 to 48 in the stem-retaining group, which was not significantly different from the stem-removal group (in patients without intraoperative complications), who had an improvement from 24 to 45 [17•]. Although these results are promising, several limitations of this study should be noted. The average time to revision of the index shoulder arthroplasty was only 38 months, which is quite short and raises the question of component malposition as an etiology for many of the revisions included in the study. Furthermore, the authors state that improper placement of the initial stem may preclude retention; this idea is supported by the fact that one third of the shoulders underwent removal of a modular stem, and those patients who underwent exchange of a modular stem often required subsequent surgery [17•].
Kany, et al recently reported their experience with a platform shoulder arthroplasty system in 29 patients, including five hemiarthroplasties, eight ATSA with cemented glenoid components and 16 ATSA with metal-backed glenoid components [10•]. Of these, three ATSA with cemented glenoids were converted to ATSA with metal-backed glenoids, and the remainder of the included arthroplasties was converted to RTSA. The authors found that the humeral stem could be maintained in 72 % of patients, with the remaining patients requiring stem change due to a high position that prevented reduction of the new RTSA. Corticotomy or humeral shaft windows were not required for stem removal. Only two metal-backed glenoid components required exchange during conversion from ATSA to RTSA, both due to loosening in the setting of Walch type B2 glenoid bone wear. Clinically, patients demonstrated significant improvement, from an average preoperative Constant score of 27 to 60, postoperatively. At a mean follow-up of 28 months, no radiological glenoid or stem loosening was noted [10•].
Limitations and complications associated with platform systems
While designed to reduce intraoperative complications such as blood loss, humeral fracture and glenoid bone loss due to the time and effort involved in component removal during revision shoulder arthroplasty, platform systems have associated limitations and complications that require mention. When choosing to maintain a convertible humeral prosthetic stem, the surgeon must accept the position of the stem, which is certainly a limitation if the position is suboptimal [9•]. Care must be taken at the index operation to utilize meticulous surgical technique to appropriately position the stem, not only to improve the longevity of the index implant, but to allow for revision without any need for stem removal. Based on existing studies, even when presumably good surgical technique is utilized, it is possible that removal of a convertible stem may be required at the time of revision to appropriately reduce the revision prosthesis and achieve adequate soft tissue tension in revision to RTSA. In addition to humeral length, excessive or abnormal humeral version may also require humeral component removal especially in revision to RTSA.
Limitations of a metal-backed glenoid component, as discussed previously, also exist. With improvements in design, wear characteristics have likely improved since the initial results published by Neer [21], although no clinical outcomes studies have confirmed this. For surgeons concerned with the implications of utilizing a metal-backed glenoid, systems exist in which only the humeral stem is convertible and a traditional glenoid component can be used.
Conclusions
Platform systems in shoulder arthroplasty offer significant versatility and numerous advantages, particularly in the revision setting, by decreasing the amount of surgical exposure needed during revision surgery, often eliminating the need for humeral osteotomy and thus reducing the incidence of intraoperative humeral fractures, decreasing surgical time, decreasing blood loss and decreasing overall complications during conversion from previous arthroplasty. Further studies with larger patient cohorts are necessary, however, as the existing literature is limited to small case series with heterogeneous populations.
Compliance with ethical standards
Conflict of interest
Brian C. Werner declares that he has no conflict of interest.
Joshua S. Dines reports grants and personal fees from Arthrex, personal fees from Conmed Linvatec, and personal fees from Ossur, outside the submitted work.
David M. Dines reports royalties received from Biomet Inc. and consulting fees from Tornier Inc.. In addition he is the developer of the Biomet Comprehensive Reverse Total Shoulder System.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Shoulder Arthroplasty
Contributor Information
Brian C. Werner, Phone: 212-606-1000, Email: wernerb@hss.edu
Joshua S. Dines, Email: dinesj@hss.edu
David M. Dines, Email: dinesd@hss.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93:2249–54. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 2.Trofa D, Rajaee SS, Smith EL. Nationwide trends in total shoulder arthroplasty and hemiarthroplasty for osteoarthritis. Am J Orthop (Belle Mead NJ) 2014;43:166–72. [PubMed] [Google Scholar]
- 3.•.Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elb Surg. 2015;24:91–7. doi: 10.1016/j.jse.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 4.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elb Surg. 2010;19:1115–20. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Hollatz MF, Stang A. Nationwide shoulder arthroplasty rates and revision burden in Germany: analysis of the national hospitalization data 2005 to 2006. J Shoulder Elb Surg. 2014;23:e267–74. doi: 10.1016/j.jse.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Matsen FA, 3rd, Li N, Gao H, Yuan S, Russ SM, Sampson PD. Factors affecting length of stay, readmission, and revision after shoulder arthroplasty: a population-based study. J Bone Joint Surg Am. 2015;97:1255–63. doi: 10.2106/JBJS.N.01107. [DOI] [PubMed] [Google Scholar]
- 7.Abboud JA, Anakwenze OA, Hsu JE. Soft-tissue management in revision total shoulder arthroplasty. J Am Acad Orthop Surg. 2013;21:23–31. doi: 10.5435/JAAOS-21-01-23. [DOI] [PubMed] [Google Scholar]
- 8.Austin L, Zmistowski B, Chang ES, Williams GR., Jr Is reverse shoulder arthroplasty a reasonable alternative for revision arthroplasty? Clin Orthop Relat Res. 2011;469:2531–7. doi: 10.1007/s11999-010-1685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.•.Chuinard C. CORR insights(R): conversion of stemmed hemi- or total to reverse total shoulder arthroplasty—advantages of a modular stem design. Clin Orthop Relat Res. 2015;473:661–2. doi: 10.1007/s11999-014-4043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.•.Kany J, Amouyel T, Flamand O, Katz D, Valenti P. A convertible shoulder system: is it useful in total shoulder arthroplasty revisions? Int Orthop. 2015;39:299–304. doi: 10.1007/s00264-014-2563-z. [DOI] [PubMed] [Google Scholar]
- 11.Gohlke F, Rolf O. Revision of failed fracture hemiarthroplasties to reverse total shoulder prosthesis through the transhumeral approach : method incorporating a pectoralis-major-pedicled bone window. Oper Orthop Traumatol. 2007;19:185–208. doi: 10.1007/s00064-007-1202-x. [DOI] [PubMed] [Google Scholar]
- 12.Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–85. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 13.Dilisio MF, Miller LR, Siegel EJ, Higgins LD. Conversion to reverse shoulder arthroplasty: humeral stem retention versus revision. Orthopedics. 2015;38:e773–9. doi: 10.3928/01477447-20150902-54. [DOI] [PubMed] [Google Scholar]
- 14.Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Shoulder Elb Surg. 2005;14:258–63. doi: 10.1016/j.jse.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Sahota S, Sperling JW, Cofield RH. Humeral windows and longitudinal splits for component removal in revision shoulder arthroplasty. J Shoulder Elb Surg. 2014;23:1485–91. doi: 10.1016/j.jse.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 16.Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure—midterm results. Int Orthop. 2011;35:53–60. doi: 10.1007/s00264-010-0990-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.•.Wieser K, Borbas P, Ek ET, Meyer DC, Gerber C. Conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res. 2015;473:651–60. doi: 10.1007/s11999-014-3985-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castagna A, Delcogliano M, de Caro F, et al. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37:1297–305. doi: 10.1007/s00264-013-1907-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elb Surg. 1997;6:495–505. doi: 10.1016/S1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 20.Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elb Surg. 2006;15:19–22. doi: 10.1016/j.jse.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Neer CS, 2nd, Morrison DS. Glenoid bone-grafting in total shoulder arthroplasty. J Bone Joint Surg Am. 1988;70:1154–62. [PubMed] [Google Scholar]
- 22.Taunton MJ, McIntosh AL, Sperling JW, Cofield RH. Total shoulder arthroplasty with a metal-backed, bone-ingrowth glenoid component. medium to long-term results. J Bone Joint Surg Am. 2008;90:2180–8. doi: 10.2106/JBJS.G.00966. [DOI] [PubMed] [Google Scholar]
- 23.Boileau P, Avidor C, Krishnan SG, Walch G, Kempf JF, Mole D. Cemented polyethylene versus uncemented metal-backed glenoid components in total shoulder arthroplasty: a prospective, double-blind, randomized study. J Shoulder Elb Surg. 2002;11:351–9. doi: 10.1067/mse.2002.125807. [DOI] [PubMed] [Google Scholar]


