Choledochal cysts are cystic dilatation of the biliary tree which may involve the extrahepatic or the intrahepatic biliary radicals or both, most commonly involving the main portion of the common bile duct. Although congenital these may be diagnosed at any age, though in more than 60 % diagnosis is made before the age of 10 years [1]. These range in incidence from 1 in 1000 in Asian population (most of the cases are seen in Japan) to less than 1 in 100,000 in Western countries, and there is also an unexplained female:male preponderance, commonly reported as 4:1 or 3:1 [1]. We report an extremely rare case of combined dilatation of both the cystic duct as well as the common bile duct (CBD) in a 14-year-old boy who presented with mild epigastric discomfort. Cystic dilatation of the cystic duct is very rare and not well recognized. Awareness of this type of malformation as a distinct entity of choledochal cyst would help in correct preoperative diagnosis and subsequent management.
A 14-year-old male patient was brought by his parents with complaints of mild pain in the epigastrium since the last 3 days. The patient was well built with no signs of malnutrition and had normal vitals. There was past history of similar episodes of mild pain which occurred once in every 3–4 months since the last 3 years. No history of fever or jaundice was present. On abdominal examination, there was no swelling, tenderness, guarding or rigidity. His blood tests including liver function tests and tumour markers were within normal limits.
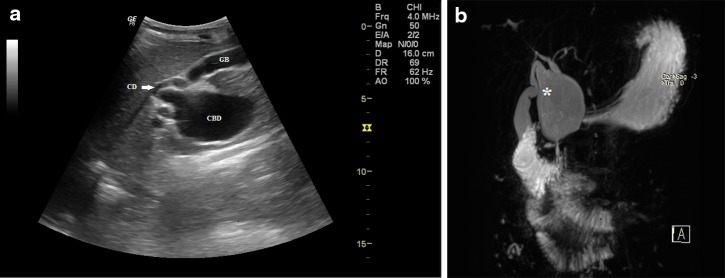
Ultrasound of the abdomen revealed cystic dilatation of the common bile duct along with dilatation of the adjacent portion of the cystic duct (Fig. 1a, ESM 1). On colour Doppler flow imaging no flow was seen (ESM 2). No intraluminal echogenic content was seen in the biliary system. Intrahepatic biliary radicals were normal. Gall bladder was distended and was normal in wall thickness. No peri-cholecystic fluid was seen. Pancreatic duct was not dilated and pancreas was normal. Rest of the abdominal organs were normal. Based on the sonographic appearance, an impression of type VI choledochal cyst (cystic duct dilatation) along with cystic dilatation of CBD (type I cyst) was made. These findings were confirmed on MRCP which was done to better define the anatomy and to search for any other pathology. It revealed a dilatation of about 7 cm in length and 4 cm in transverse diameter involving both the CBD and proximal cystic duct; both the ducts were joined by a wide communication (Fig. 1b). Further, it was seen on MRCP (clip 1) that the distal most part of CBD (1.4 cm) was of normal calibre, measuring 4 mm and was opening normally into the second part of duodenum. The pancreatic duct measured 1.5 mm and was normal.
Fig. 1.
Combined dilatation of both the cystic duct as well as the common bile duct in a 14-year-old boy who presented with mild epigastric discomfort. a Abdominal ultrasound image showing a cystic lesion involving the common bile duct (CBD) and the adjacent portion of the cystic duct (CD), GB (gall bladder); b thick-slab coronal oblique MR cholangiopancreatography image showing fusiform dilatation of the CBD involving the cystic duct via a wide communication (asterisk)
Considering the inherent risk of malignancy, surgical removal of the cyst was suggested. However, in the absence of any significant symptoms, the parents of the boy refused any surgical intervention. He was discharged with the advice of close follow-up.
Alonso-Lej et al. proposed the first classification system for choledochal cysts in 1959 [2], describing three types of biliary duct dilation. Todani and colleagues in 1977 [3] expanded this classification to include intrahepatic duct cysts as well as multiple cysts; this modified classification is presently the most accepted one. Cystic dilatation of the cystic duct is very rare; however, it was not included in the Todani classification. Serradel et al. [4] described a case of isolated dilatation of the cystic duct as ‘‘type VI choledochal cyst’’, an addition to the Todani classification. Combined dilatation of the cystic duct and the common bile duct (as seen in our case) is extremely rare and though documented in few case reports, it has not yet been included in the (Todani) classification of choledochal cysts. Yoon in 2011 [5] described the imaging features of choledochal cysts with involvement of the cystic duct in three cases; in one of the case only cystic duct was dilated and in other two both the cystic and common bile ducts were involved, and proposed that these variant anomalies be included in the classification of choledochal cysts.
We propose that type VI cysts should be further divided into two types: type VIA involving isolated dilatation of the cystic duct (type VI as proposed by Serradel et al.) and type VIB involving combined dilatation of cystic duct as well as the CBD (similar to the present case). Awareness of this type of malformation as a distinct entity of choledochal cyst would help in correct preoperative diagnosis and subsequent management.
Electronic supplementary material
Supplementary material 1: Fig. 1c. Combined dilatation of both the cystic duct as well as the CBD in a 14-year-old boy who presented with mild epigastric discomfort. Cystic lesion involving the CBD and the adjacent portion of the cystic duct (JPEG 96 kb)
Supplementary material 2: Fig. 1d. Combined dilatation of both the cystic duct as well as the CBD in a 14-year-old boy who presented with mild epigastric discomfort. No flow was seen on CDFI in the lesion (JPEG 114 kb)
Supplementary material 3: Clip 1: Thick-slab coronal MR cholangiopancreatography video showing fusiform dilatation of the CBD involving the cystic duct via a wide communication. (WMV 223 kb) (WMV 223 kb)
Compliance with ethical standards
Conflict of interest
None.
Informed consent
Informed consent was taken from father of the patient (as he was minor) for publication of this report.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). No animals were used during the study.
References
- 1.Bhavsar SM, Vora BH, Girivappa HV. Choledochal cysts: a review of literature. Saudi J Gastroenterol. 2012;18:230–236. doi: 10.4103/1319-3767.98425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alonso-Lej F, Rever WB, Pessango DJ. Congenital choledochal cyst, with a report of two, and an analysis of 94 cases. Int Abstr Surg. 1959;108:1–10. [PubMed] [Google Scholar]
- 3.Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: classification, operative procedures, and review thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–269. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 4.Serena Serradel AF, Santamaria Linares E, et al. Cystic dilatation of the cystic duct: a new type of biliary cyst. Surgery. 1991;109:320–322. [PubMed] [Google Scholar]
- 5.Yoon JH. Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three cases. Br J Radiol. 2011;84:e18–e22. doi: 10.1259/bjr/77844300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1: Fig. 1c. Combined dilatation of both the cystic duct as well as the CBD in a 14-year-old boy who presented with mild epigastric discomfort. Cystic lesion involving the CBD and the adjacent portion of the cystic duct (JPEG 96 kb)
Supplementary material 2: Fig. 1d. Combined dilatation of both the cystic duct as well as the CBD in a 14-year-old boy who presented with mild epigastric discomfort. No flow was seen on CDFI in the lesion (JPEG 114 kb)
Supplementary material 3: Clip 1: Thick-slab coronal MR cholangiopancreatography video showing fusiform dilatation of the CBD involving the cystic duct via a wide communication. (WMV 223 kb) (WMV 223 kb)