Abstract
Splenosis is defined as the acquired heterotopic autotransplantation of splenic tissue in other sites of the body after splenic rupture, usually due to either traumatic or iatrogenic causes. It is often found incidentally and is usually asymptomatic. These implants are not limited to the left upper quadrant of the abdomen, however, and splenosis in other locations can mimic various pathologic entities. There are several reports on abdominal splenosis, but intrathoracic and subcutaneous splenosis are rare. We report two cases of intrathoracic and subcutaneous splenosis that were diagnosed using spleen scintigraphy, avoiding the need for an invasive procedure.
Keywords: Spleen, Intrathoracic splenosis, Subcutaneous splenosis, Spleen scintigraphy
Introduction
Splenosis involves the ectopic autotransplantation of splenic tissue after trauma or iatrogenic event [1]. The splenic implants derive their blood supply from surrounding tissue and develop into mature splenic tissue [2]. Splenosis is usually asymptomatic and needs no further treatment. While it commonly occurs in the abdomen, it can occur anywhere in the body. The imaging finding of splenosis can mimic malignancy and other metastatic lesions [3].
In this paper, we present two rare cases of intrathoracic and subcutaneous splenosis diagnosed using technetium-99m (99mTc-)-labeled denatured red blood cell (RBC) imaging. Along with an atypical location of the lesions and a history of splenectomy, denatured RBC scans can confirm a diagnosis of splenosis. Patients can thus avoid unnecessary invasive diagnostic procedures or surgery.
Case Reports
Patient 1
A 35-year-old man presented to the neurology department of our hospital, complaining of headache, fever and a chilly sensation for 7 days. The patient’s vital signs were stable (temperature, 39 °C; pulse rate, 92 beats/min; systolic blood pressure, 126 mmHg; diastolic blood pressure, 70 mmHg). Laboratory study revealed an elevated white blood cell count (15,070/μl; normal range 4000–10,800/μl). Other serum laboratory test results were within normal limits (hemoglobin 16 g/dl, normal range 13.0–18.0 g/dl; platelet count 315,000/μl, normal range 130,000– 400,000 /μl). No other abnormal findings were noted on physical examination. The patient had a history of splenectomy and chest tube insertion after a traffic accident 10 years earlier. After 2 days, he complained of aggravated febrile sensation, myalgia, and chilly sensation, with yellow-colored sputum.
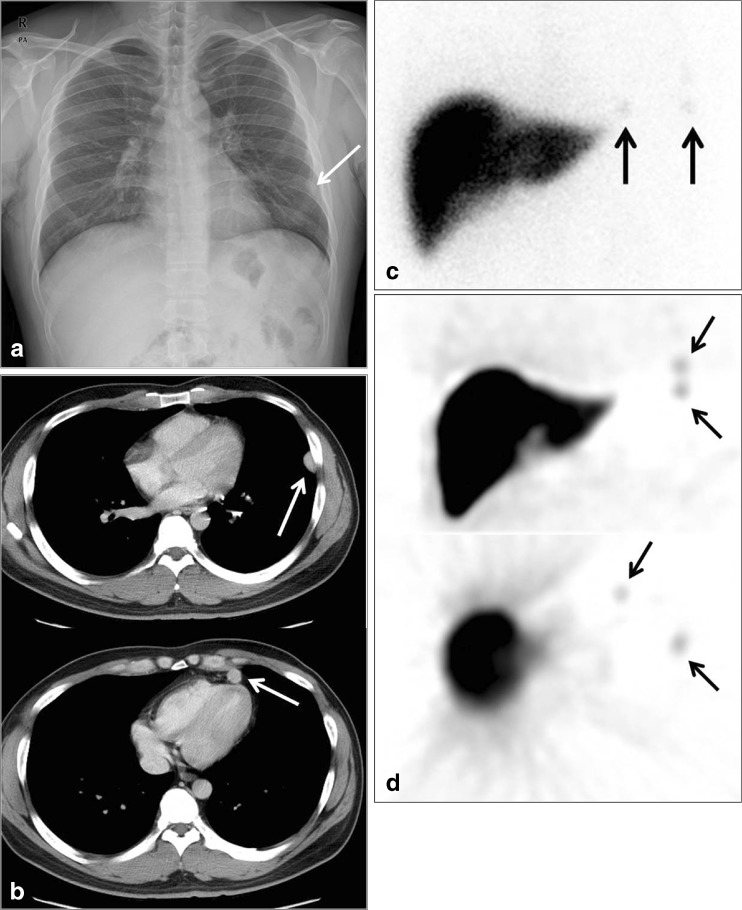
A chest x-ray image showed multiple pulmonary nodules in the left lower lobe and left chest wall (1.5 cm; Fig. 1a), and contrast-enhanced chest computed tomography (CT) was performed for further evaluation of the nodules. Chest CT revealed multiple well-defined and enhanced nodular lesions of varying size (0.3 cm–2 cm) in the left pleura, extrapleural space, left diaphragm, and anterior mediastinum (Fig. 1b).
Fig. 1.
Intrathoracic splenosis in a 35-year-old man. a Posteroanterior (PA) chest x-ray image shows 1.5-cm nodular opacities in the left lower lobe (LLL) (arrow). b Chest CT axial image shows well-enhanced nodules in the pleura and anterior mediastinum. There is no delineation of normal spleen in the splenic fossa (not shown). c Planar image of 99mTc-labeled denatured RBC scintigraphy. Two foci of uptake are found in the left lower chest area (arrow). d Coronal and axial single-photon emission computed tomography (SPECT) images of spleen scintigraphy. Multifocal increased uptake is observed in the mediastinum and pleura (arrow). LLL left lower lobe
To rule out the possibility of intrathoracic splenosis, a 99mTc-labeled denatured RBC scan was performed. On scan images, multiple foci of radiotracer uptake were observed (Fig. 1c, d), and this finding was interpreted as intrathoracic splenosis. The patient was subsequently diagnosed with intrathoracic splenosis and bronchitis, and was treated with oral non-steroidal anti-inflammatory drugs to relieve symptoms. There was no change in thoracic splenosis on 3-month follow-up CT.
Patient 2
A 39-year-old woman presented with stomach cancer diagnosed at a local clinic. The patient had a history of spine surgery 30 years earlier and splenectomy 20 years earlier due to trauma. No abnormal finding was noted on physical examination at the time of the visit to our medical center. The patient’s vital signs were stable (temperature, 36.8 °C; pulse rate, 72 beats/min; systolic blood pressure, 100 mmHg; diastolic blood pressure, 60 mmHg). Laboratory studies revealed a slightly elevated white blood cell count (10,376/μl; normal range 4000–10,800/μl) and slightly decreased serum hemoglobin level (11.5 g/dl; normal range 13.0–18.0 g/dl). Platelet (251,000/μl; normal range, 130,000–400,000/μl) and hematocrit (46.1 %; normal range, 38.0–52.0 %) levels were within normal limits. Gastric endoscopic biopsy was performed for histopathological diagnosis. The results of biopsy revealed a poorly differentiated adenocarcinoma located on the anterior wall of the gastric antrum.
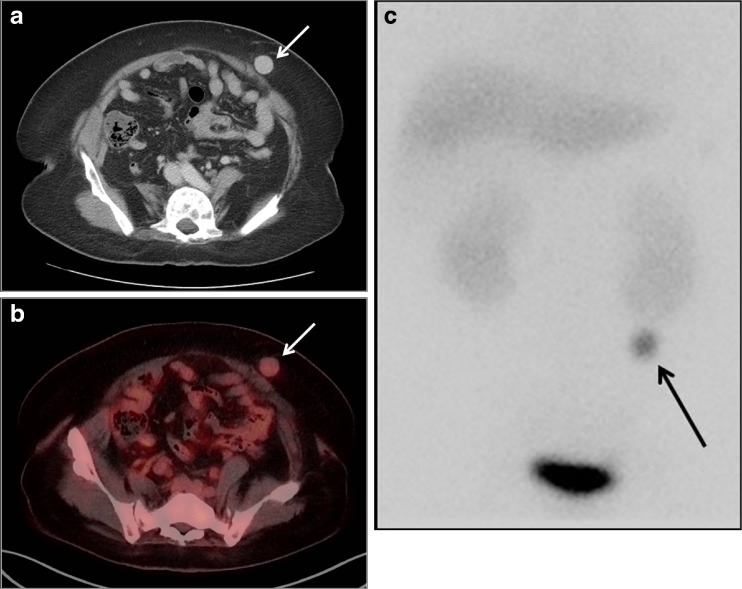
For preoperative assessment, contrast-enhanced abdominal CT was performed. On abdominal CT images, a 2.2-cm well-defined and enhanced solitary nodule located in the subcutaneous layer of the left lower quadrant of the abdominal wall was noted (Fig. 2a). In addition, the spleen was not observed in the splenic recess. To assess the possibility of a metastatic abdominal wall lesion, F-18-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT was performed. On FDG PET/CT images, a well-defined subcutaneous nodule with mildly increased FDG uptake (maximum standardized uptake value of 1.8) was shown (Fig. 2b).
Fig. 2.
Subcutaneous splenosis in a 39-year-old woman. a Contrast-enhanced abdominal CT image shows a 2.2-cm well-defined enhanced nodule in the subcutaneous fat layer of the left lower quadrant of the abdominal wall (arrow). b FDG PET/CT finding. Mildly increased FDG uptake is observed in the lesion noted on the abdominal CT images (arrow). c Planar image of 99mTc-labeled denatured RBC scintigraphy. Focal areas of increased uptake are observed in the left lower quadrant of the abdomen (arrow)
Because of low FDG uptake on FDG PET/CT, the possibility of splenosis was considered, and a 99mTc-labeled denatured RBC spleen scan was performed. On spleen scan images, increased radiotracer uptake was observed in the left lower abdominal wall (Fig. 2c), and the subcutaneous nodule was therefore diagnosed as splenosis. Total gastrectomy and Roux-en-Y esophagojejunostomy was performed for the treatment of gastric cancer. The patient's condition remained stable at follow-up for more than 1 year. There was no change in subcutaneous splenosis on 10-month follow-up CT.
Discussion
Ectopic splenic tissue usually presents as accessory spleen or splenosis [1]. Accessory spleen is congenital, and has normal splenic tissue, with blood supply from the splenic artery [2]. Splenosis is an acquired benign disease, defined as autotransplantation of ectopic splenic tissue in other anatomic areas of the body after trauma or iatrogenic spleen injury [3]. It occurs in up to 65 % of cases of splenic rupture, with an average period of 18.8 years to presentation, although the incidence of splenosis in the general population is unclear [4, 5]. Splenosis is incidentally diagnosed during abdominal surgery or autopsy, and is generally asymptomatic [1]. The mechanism of splenosis involves the implantation of spleen fragments into sites other than the spleen bed, with the blood supply derived from surrounding tissue, and the formation of small splenic nodules with functional activity similar to that of the mature spleen [6]. In addition, the splenetic tissue can maintain normal immunological function [6]. The differential diagnosis of splenosis versus other pathologic conditions by ultrasonography, CT, and magnetic resonance imaging (MRI) is very difficult, because splenosis has no typical radiologic findings [3]. It is a benign condition that is often misdiagnosed as a malignant or metastatic lesion [1–3].
Abdominal splenosis is the most common form of the condition, while intrathoracic splenosis is less common [4]. One study found that abdominal or pelvic splenosis and intrathoracic splenosis occurred in 65 % and 18 % of patients, respectively, who had suffered splenic or diaphragmatic injury [7]. To the best of our knowledge, fewer than 20 cases of subcutaneous splenosis have been reported in the literature, including our case [8]. Intrathoracic splenosis occurs after thoracoabdominal trauma involving injury to the diaphragm and spleen [3, 7]. Splenic tissue is mainly found as pleural-based nodules in the left hemithorax [7]. It has been reported to be manifested as multiple lesions in 75 % of cases, with attenuation of lesions similar to that of normal splenic tissue [4]. The implanted splenic tissue should be differentiated from other pathologic conditions including primary tumor, metastasis, and infection [3]. Subcutaneous splenosis is rare, and the majority of cases occur after abdominal surgery or gunshot wound [3, 4]. It may be confused with tumors located in the subcutaneous layer, such as lymphoma, cutaneous lymphoid hyperplasia, and Kaposi sarcoma, or subcutaneous vascular malformation [3].
It is generally accepted that asymptomatic splenic implants should not be removed, as splenic tissue may be immunologically functional [1]. Several studies have demonstrated that preoperative diagnosis of splenosis should be obtained through the use of 99mTc-labeled denatured RBC spleen imaging rather than biopsy or invasive surgery [9, 10]. This scanning technique has shown the greatest sensitivity and specificity for the confirmation of splenic tissue [7]. 99mTc-labeled denatured RBCs are sequestered by ectopic splenic tissue, and radioactivity in splenic tissue can be detected using nuclear imaging [7, 9]. Importantly, denatured RBC spleen imaging has shown high sensitivity for the detection of very small or multiple foci of ectopic splenic tissue that are not detected by CT or MRI [2]. Intrathoracic and subcutaneous splenosis are relatively rare [7–10]. This report presents cases of incidentally found mass lesions located in the thorax and subcutaneous layer in patients with a history of splenectomy. Appropriate 99mTc-labeled denatured RBC spleen scanning was performed, and the diagnosis of splenosis was confirmed. The use of this imaging technology allows patients to avoid unnecessary invasive and surgical procedures. In patients with an atypically located mass who have a history of splenectomy or spleen injury, the clinician should strongly consider the possibility of splenosis and should perform a denatured RBC spleen scan.
In conclusion, with the use of T99mTc-labeled denatured RBC spleen imaging, a diagnosis of intrathoracic and subcutaneous splenosis, which is a rare form of splenosis, can be obtained without the need for invasive procedures. The Tc-99 m-labeled denatured RBC scan is therefore the non-invasive diagnostic modality of choice for the evaluation of splenosis.
Acknowledgements
This work was supported in part by the Soonchunhyang University Research Fund.
The manuscript has not been published previously and is not under consideration for publication elsewhere. All co-authors listed on the title page have approved the manuscript.
Conflict of interest
Ji Min Kim, Sang Mi Lee, Jiyoun Choi, Jiwon Lyu, and Moon Soo Lee declare that they have no conflict of interest.
Ethical Statement
This study was approved by an institutional review board of the Soonchunhyang University Cheonan Hospital, and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The institutional review board of our university waived the need to obtain informed consent.
References
- 1.Ha MK, Kwon OJ, Lee KS, Hwang YY, Hong EK. Splenosis with cyclic abdominal pain misdiagnosed as ovarian dermoid cyst. J Korea Surg Soc. 2002;62:450–2. [Google Scholar]
- 2.Akay S, Ilica AT, Battal B, Karaman B, Guvenc I. Pararectal mass: an atypical location of splenosis. J Clin Ultrasound. 2012;40:443–7. doi: 10.1002/jcu.20843. [DOI] [PubMed] [Google Scholar]
- 3.Lake ST, Johnson PT, Kawamoto S, Hruban RH, Fishman EK. CT of Splenosis: patterns and pitfalls. AJR Am J Reontrgenol. 2012;199:W686–93. doi: 10.2214/AJR.11.7896. [DOI] [PubMed] [Google Scholar]
- 4.Javadrashid R, Paak N, Salehi A. Combined subcutaneous, intrathoracic and abdominal splenosis. Arch Iran Med. 2010;13:436–9. [PubMed] [Google Scholar]
- 5.Sorensen SF, Mortensen FV, Hellberg Y, Ladekarla M. Diffuse abdominal splenosis mimicking peritoneal metastases in a 35-year-old man with a resectable carcinoma of the ampulla of Vater. Case Rep Oncol. 2013;6:467–71. doi: 10.1159/000355233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rickert CH, Maasjosthusmann U, Probst-Cousin S, August C, Gullotta F. A unique case of cerebral spleen. Am J Surg Pathol. 1998;22:894–6. doi: 10.1097/00000478-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Yammine JN, Yatim A, Barbari A. Radionuclide imaging in thoracic splenosis and a review of the literature. Clin Nucl Med. 2003;28:121–3. doi: 10.1097/01.RLU.0000048681.29894.BA. [DOI] [PubMed] [Google Scholar]
- 8.Papakonstaninou E, Kalles V, Papapanagiotou I, Piperos T, Karakaxas D. Subcutaneous splenosis of the abdominal wall: report of a case and review of the literature. Case Rep Surg. 2013;2013:454321. doi: 10.1155/2013/454321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malik UF, Martin MR, Patel R, Mahmoud A. Parenchymal thoracic splenosis: history and nuclear imaging without invasive procedures may provide diagnosis. J Clin Med Res. 2010;2:180–4. doi: 10.4021/jocmr401w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crivellaro C, Cabrini G, Gay E, Sara R, Rossetti C. Intrathoracic splenosis : evaluation by Tc-99m–labelled heat-denatured erythrocyte SPECT/CT. Eur J Nucl Med Mol Imaging. 2011;38:412. doi: 10.1007/s00259-010-1656-1. [DOI] [PubMed] [Google Scholar]