Abstract
The purpose of this study was to determine the predictors of stereoacuity outcome in visually mature subjects with exotropia following surgical correction. Visually mature subjects who were surgically aligned and had been tested for stereoacuity in the postoperative period were studied retrospectively. Subjects were grouped with respect to their responses to Titmus or TNO stereotests. Characteristics such as amblyopia, anisometropia, and characteristics of the exodeviation such as time of onset, duration, intermittency, presence of an A or V pattern, distance-near disparity, coexisting vertical deviation, and inferior oblique overaction, were compared between the groups. One hundred and four visually mature subjects with exotropia met the inclusion criteria. Stereoacuity was achieved in 77% of the study group and only 9% of these could achieve fine stereoacuity. Negative stereoacuity was more frequently associated with larger deviation angles, higher anisometropia, inferior oblique overaction, pattern strabismus, coexisting vertical strabismus, and distance-near disparity, but not at a statistically significant level. The optimal cutoff for strabismus duration was 20 years for a positive stereoacuity outcome. Any-level visual acuity difference was found to decrease the chance for positive stereoacuity significantly. The odds ratios for the stereoacuity positivity were 4.05 for strabismus duration <20 years, 7.9 for strabismus onset >1 year of age, 3.79 for weaker eye visual acuity >20/25 and 9.85 for intermittency of strabismus. Intermittence of exotropia was the strongest predictor for positive stereoacuity. Exotropia onset after 1 year of age, absence of any-level visual acuity difference, and strabismus duration <20 years were the other predictors with decreasing power.
Introduction
Exodeviations may be progressive in nature. Although uncommon, an exophoria (X) may deteriorate to an intermittent exotropia (X(T)) and may eventually become a constant exotropia (XT).1, 2 Studies have shown that there is an ongoing deterioration of stereoacuity during progressive nature of exodeviation from exophoria (X) to constant exotropia (XT).3, 4, 5, 6 Subjects with X(T) usually demonstrate fine near stereoacuity until late in the course of the condition. Although well aligned, those with a constant exotropia usually have poor stereoacuity postoperatively.5, 6, 7 Stereoacuity thresholds for adults with strabismus have been studied before, but there are few studies that study stereoacuity and exotropia.8, 9, 10, 11, 12, 13 O'Neal et al14 studied 20 X(T) adult subjects and stereoacuity improved at near in 75% and at distance in 45% of the subjects following surgical realignment. Peters and Archer15 reported the presence of measurable stereoacuity ranging 40–200 arcsec postoperatively in four of eight longstanding XT subjects, but they did not identify the factors that might affect stereoacuity outcome.
The goal of this study is to determine if predictors of postoperative stereoacuity outcome can be identified in surgically corrected, visually mature and exotropic subjects.
Materials and methods
This is a retrospective cross-sectional study. We reviewed the clinical records of 211 patients who underwent strabismus surgery for exotropia between January 2006 and September 2013. All data collection was approved by our Institutional Review Board.
Inclusion criteria were having no other eye comorbidity except amblyopia of vision >20/63, being at or >12 years of age at the time of strabismus surgery, having satisfactory motor alignment (<10 prism dioptres (pd) horizontal and <4 pd vertical), and having stereoacuity test results in the postoperative period. Sensory, paralytic, consecutive and congenital exodeviations were excluded.
Visual acuity values were converted to Log MAR units for the analyses. The best-corrected visual acuity values of the amblyopic eyes were taken for the analyses if there was amblyopia.
Stereoacuity was tested with Titmus (Stereo Optical Co, Chicago, IL, USA) or TNO stereotests (15th edition, Lameris Ootech BV). TNO stereogram results were preferably used for analysis when available. Stereopsis was considered ‘fine' if the stereoacuity threshold was 60 arcsec or better, ‘moderate' if it was 80 to 480 arcsec and ‘gross' if it was worse than 480 arcsec. Patients who could not pass the Titmus Random dot Stereo Butterfly test or TNO screening plates (I–III) were graded as stereoacuity negative. Only the near stereoacuity thresholds were evaluated since we did not have the ability to evaluate distance stereoacuity.
Stereoacuity thresholds were recorded both pre- and postoperatively in subjects with X(T) who had sufficient control of strabismus at near. Surgical correction was decided if the exotropia control scores were four (exotropia >50% of the exam before dissociation) or five (constant exotropia) for either distance or near according to Mohney and Holmes' X(T) control scale.16
Anisometropia was not treated as a categorical variable: instead, any level of interocular refractive difference, measured as a spherical equivalent, was included in anisometropia analyses.
Strabismus onset time was recorded for each patient using data in their files. Some patients had professional diagnosis just after the complaints started, whereas in others strabismus onset was determined based on the histories given by the patients or parents and confirmed with inspection of old photographs. The duration from the onset to the last surgery was calculated as strabismus duration and recorded for each patient.
Stereoacuity positive and negative groups were compared with respect to age and sex distribution, strabismus onset (before or after 1 year of age), intermittency and duration, visual acuity of the weaker eye, anisometropia, presence of motility imbalances complicating strabismus, such as inferior oblique overaction, A of V pattern, distance–near disparity, and accompanying vertical strabismus.
Statistical analyses
Either independent samples T-test or Mann Whitney U-test was used to compare the continuous variables of the stereoacuity positive and negative groups after testing equality of variances of the groups with Levene's test. Categorical variables of the groups were compared using either Pearson chi-square test or Fisher Exact test. Variables that had significant effect on the outcome were further analysed. Optimal cutoff values of the continuous variables (strabismus duration and weaker eye visual acuity) were determined using receiver operating characteristics (ROC) curve analysis. The binary logistic regression (method=enter) model was used to predict the odds of postoperative positive stereoacuity response based on the values of the independent variables (predictors: strabismus duration, strabismus onset, weaker eye visual acuity, and intermittency of strabismus). The odds were defined as the probability of a positive stereoacuity response divided by the probability of a negative stereoacuity response.
Results
A total of 104 patients, who were 12–73 years of age, met the inclusion criteria. Fifty-nine of them were female and 45 of them were male. Patient characteristics are given in Table 1. Seventy-nine of the patients had constant exotropia and 25 had intermittent exotropia just before the surgery. Some constant-exotropia patients gave the history of decompensation from intermittent to constant deviation, but not all of them were inquired with this respect. The mean number of surgical procedures per patient was 1.25 for the study group to reach the defined motor success criteria. Surgical corrections consisted of bilateral lateral rectus recessions or combined lateral rectus recession combined with a medial rectus resection. Twenty-five patients (24%) had a second procedure to correct residual deviations and one (0.96%) required second surgery to correct a consecutive esotropia. All subjects with pattern strabismus underwent surgery to collapse the pattern. Twenty-three (22%) exotropic patients had a vertical deviation component arising from asymmetrical IOOA or other vertical muscle imbalance. The surgical plan involved operating on the vertical component of the deviation in 14 subjects (13%) who had 8 pd or more vertical deviation or inferior oblique overaction.
Table 1. Analysis of patient characteristics and stereoacuity.
| Patient characteristics |
Stereoacuity |
P-value | |
|---|---|---|---|
| Absent (N=24) | Present (N=80) | ||
| Sex | |||
| Female | 15 (62.5%) | 44 (55%) | 0.640 |
| Male | 9 (37.5%) | 36 (45%) | |
| Age (years)a | 30.88±10.81 | 27.75±15.17 | 0.350 |
| Strabismus duration (years)b | 24.5±19.5 | 16±16 | 0.005 |
| Deviation angle (prism dioptres)b | 48±20 | 40±26 | 0.089 |
| Anisometropia (dioptres)b | 0.375±0.75 | 0.25±0.875 | 0.593 |
| Visual acuity of the weaker eye (log MAR)b | 0.1±0.4 | 0.0±0 | 0.007 |
| Diplopia | 3 (12.5%) | 12 (15%) | 1 |
| Inferior oblique overaction | 8 (33.3%) | 15 (18.8%) | 0.162 |
| Pattern strabismus | 8 (33.3%) | 17 (21.3%) | 0.277 |
| Coexisting vertical component | 7 (29.2%) | 16 (20%) | 0.402 |
| Distance–near disparity | 8 (33.3%) | 23 (28.8%) | 0.800 |
| Intermittent deviation | 1 (4%) | 24 (30%) | 0.009 |
| Onset of strabismus (<1year of age) | 9 (37.5%) | 6 (7.5%) | 0.001 |
Pearson χ2-test and Fisher Exact test (Monte Carlo), independent T-test and Mann Whitney U-test (Monte Carlo). Bold indicates significant P-values.
Mean±SD.
Median±interquartile range.
Different levels of stereoacuity thresholds were detected in 80 patients (77%) postoperatively; 7 had fine (60 arcsec or better), 32 had moderate (80–480 arcsec), and 41 had gross stereoacuity thresholds. Preoperative stereoacuity thresholds were measured in 24 of the 25 intermittent exotropias; 3 had fine, 13 had moderate, and 8 had gross stereoacuity thresholds. In the postoperative period, nine patients improved to a better category, 13 stayed at the same category and 2 deteriorated to a lower category. Consecutive small-angle esotropia caused the deteriorations. None of the seven subjects with fine stereoacuity threshold in the postoperative period had amblyopia, anisometropia, inferior oblique overaction, alphabetic pattern, and coexisting vertical deviation, but three of them did have a distance–near disparity.
There was a trend towards having larger angle of deviation, higher anisometropia, inferior oblique overaction, A or V patterns, accompanying vertical deviation, and distance–near disparity in the stereoacuity negative group, but not at a statistically significant level. The stereoacuity negative group was also found significantly more often associated with early onset (P=0.001) and a longer duration of strabismus (P=0.005). In addition, the mean visual acuity of the weaker eye was significantly lower in the stereoacuity absent group (P=0.007). Statistical analyses of the group characteristics are given in Table 1.
The stereoacuity positive group was found significantly associated with intermittency of exotropia (P=0.009). The optimal cutoff point of the strabismus duration for a positive stereoacuity outcome was found to be 20 years using ROC curve analysis. The predictive value of ‘strabismus duration of <20 years' for a positive stereoacuity outcome was found significant (sensitivity=57.5%, specificity=75%, AUC=0.689, P=0.005). The optimal cut-off point of visual acuity in the weaker eye for a positive stereoacuity outcome was determined as 0.1 log MAR unit (20/25) in ROC curve analysis. The predictive value of the weaker eye visual acuity better than 0.1 log MAR unit or absence of any-level visual acuity difference for a positive stereoacuity outcome was significant (sensitivity=76.3%, specificity=54.2%, AUC=0.647, P=0.030). Logistic regression analysis showed that odds ratios for a positive stereoacuity response were 4.05 for strabismus duration <20 years (P=0.007); 7.9 for strabismus onset over 1 year of age (P=0.001); 3.79 for weaker eye visual acuity better than 0.1 log MAR unit (P=0.006); and 9.85 for the for the intermittency of strabismus (P=0.029; Table 2).
Table 2. Logistic regression analysis of patient factors for stereoacuity.
| Variables | P-value | OR |
95% CI |
|
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Strabismus duration (<20 years) | 0.007 | 4.059 | 1.457 | 11.310 |
| Strabismus onset (<1 year of age) | 0.001 | 7.929 | 2.435 | 25.813 |
| Visual Acuity better than (0.1 log MAR) | 0.006 | 3.794 | 1.462 | 9.849 |
| Intermittent deviation | 0.029 | 9.857 | 1.258 | 77.218 |
Abbreviations: CI, confidence interval; OR, odds ratio. Logistic regression (method=enter).
Discussion
Exotropia is a common condition and there is often a long period before a visually mature patient will seek treatment. During the discussion regarding treatment, it would be desirable to be able to discuss chances for a functional result as well as correct the exotropia. Information on the sensory outcome exists for visually immature children, but factors influencing the chance of obtaining stereoacuity in visually mature individuals are unknown. We would like to know what the predictors of a positive stereoacuity response after exotropia surgery in visually mature subjects. In this study, we have tried to define predictors and their power to predict stereoacuity outcome in visually mature subjects are. We will discuss each parameter studied.
Intermittent vs constant forms of exodeviation
Wu et al5 compared sensory results of X(T) and XT groups with or without a previous history of intermittency: 74% of the X(T) group achieved fine stereoacuity, but no XT subject was able to achieve this level. Gross stereoacuity achievement rates were 100%, 79% and 33% in X(T), XT with and without a history of intermittency groups, respectively. They concluded that their XT patients may have missed the best time for treatment. In the study of Abroms et al,6 postoperative fine stereoacuity rates were 93% in X(T) and 29% in XT. These studies were performed in a predominantly paediatric age population. We studied on an older, visually mature population with a longer duration of their exodeviation compared with those studies. In our study on visually mature subjects, the postoperative stereoacuity positivity rates were lower. We found that intermittence of exotropia was the strongest predictor of positive stereoacuity. Odds ratio of intermittence for the positive stereoacuity was 9.85. Stereoacuity was positive in 96% of the X(T) subjects but only 17% achieved fine stereoacuity, and these rates decreased to 71% and 5% for XT cases, respectively.
Age of onset of the exodeviation
One of the most important factors determining the prognosis for stereoacuity outcome in strabismus is the age of onset of strabismus. Fawcett et al17 studied the critical period for acquiring stereopsis in a group of strabismic children. They found that the critical period begins soon after birth, peaks sharply at 3.5 months but shows continued chance for development to at least 4.6 years. Birch and Salomoa18 observed a rapid period of stereopsis maturation until 18 months of age in normal healthy infants. The onset of exotropia can occur early in life and in some cases the strabismic period can intersect the critical period for stereopsis development and maturation. Patients having strabismus onset during this period will be expected to have a worse stereoacuity outcome. Choi and Kim19 studied stereopsis results in a group of exotropic children with an onset before 12 months. Only X(T) subjects (25%) could achieve fine stereopsis in their group. There were 15 subjects with a history of strabismus onset before 12 months in our group, and 40% of them recovered some stereoacuity, but only one, who was still in the intermittent phase during surgery, achieved fine stereoacuity. We evaluated ‘exotropia onset after one year of age' in the logistic regression model. It was a significant predictor for postoperative positive stereoacuity and its odds ratio was 7.9 (P=0.001).
Duration of the exodeviation
Stereoacuity outcome after surgical realignment was found significantly associated with the duration of constant strabismus in visually immature subjects.6, 11 Abroms et al6 studied 76 subjects with acquired XT or X(T) and found that subjects had a significantly greater chance of having postoperative fine stereoacuity if they were surgically aligned within 5 years from the onset of the strabismus. Is there a critical duration of misalignment in visually mature subjects beyond which recovery of stereoacuity is not possible despite successful surgical alignment? Previously, Lal and Holmes9 reported that misalignment for up to 4 years did not preclude the development of postoperative stereoacuity in adult acquired strabismic patients. In the study of Fawcett et al,11 patients with 12 months or less of constant eye misalignment achieved significantly better random dot stereoacuity than subjects with a longer period of eye misalignment. Our study group had a wide range of the duration of the exotropia (ranging from 6 months to 57 years) and the mean duration of the exodeviation for the whole group was relatively long (19±13 years). This gave us an opportunity to evaluate strabismus duration in ROC curve analysis and to see if there was a discrimination threshold for stereoacuity outcome. Twenty years of strabismus duration was defined as the optimal cutoff point over which stereoacuity positivity significantly decreased (P=0.007). The positive predictivity of strabismus duration <20 years for stereoacuity was found to be 88.5% and the odds ratio was found to be 4. We could not make a similar analysis of strabismus duration for the achievement of fine stereopsis, as there were only seven patients who achieved this. The longest duration of exotropia that permitted fine stereoacuity was 45 and 12.5 years for the X(T) and XT groups, respectively. On the basis of these findings, we can say that though strabismus duration has a degrading effect on stereoacuity, there can be exceptional cases.
Exodeviation plus characteristics (inferior oblique overaction, A and V patterns, coexisting vertical deviation, or distance–near incomitance)
Subjects with longer strabismic periods usually have additional features complicating their strabismus, such as inferior oblique overaction and A or V patterns that produce vertical incomitance.20 The effects of these features on stereoacuity outcome have not been studied in visually mature subjects with exotropia. In this study distance–near incomitance was equally distributed in both stereoacuity negative and positive groups, but inferior oblique overaction, A or V patterns, and coexisting vertical deviations were more frequent in the stereoacuity negative group. There was a lower prevalence of these features in the stereoacuity positive group, but it did not reach a statistically significant level. Nevertheless, none of the subjects having these features could achieve fine stereoacuity. Subjects having these features have a decreased opportunity to achieve optimal motor alignment compared with uncomplicated exodeviations. In the previous studies, Leske and Holmes21 defined maximum angle of horizontal deviation consistent with true stereopsis as 4 pd. Similarly, Fawcet et al11 reported poor stereoacuity outcome in cases with postsurgical residual angle of 5 pd or more. We did not measure very small latent deviations and microstrabismic cases regularly unless they had diplopia in the postoperative period, but residual deviations might have been responsible for some of negative or low stereoacuity responses in this study. We think that complicated exotropias have less precise motor alignment and consequently decreased opportunity to achieve fine stereoacuity thresholds.
Amblyopias
Stereoacuity and visual acuity are known to affect each other; however, stereopsis is a function not always linearly correlated with visual acuity.22 It has been shown that reduction of visual acuity with a neutral density filter over one eye did not raise stereoscopic threshold even if the acuity was decreased to a level of 20/63.23 For this reason, we excluded subjects who had amblyopic eye acuity <20/63 level. Nevertheless, the stereoacuity negative group was found significantly more frequently associated with mild to moderate amblyopia. We looked for optimal threshold level of weaker eye visual acuity below which stereoacuity positivity decreased significantly using ROC curve analysis and found 20/25 level. This finding meant to us that any-level visual acuity difference degraded stereoacuity and the odds ratios of equal vision in both eyes for a positive stereoacuity response was 3.79 (P=0.006). Wallace et al24 studied stereopsis in anisometropic children and found that among subjects whose amblyopic eye acuity outcome was within one line of the fellow-eye visual acuity, stereoacuity was worse than that of children with normal vision of the same age. These data also support our findings.
Limitations of the study
Limitations of our study arise from the retrospective nature of the study. We did not strictly measure all micro deviations and latent deviations in orthotropic patients in the postoperative period. We therefore could not discriminate how the residual deviation angles within our success criteria affect stereoacuity recovery in our study group. Another limitation was accuracy of the histories taken from patients or relatives related to the onset of their strabismus. It was not possible, in all patients, to confirm the onset of the exotropia with photographs or with a confirmed professional diagnosis. We have relied on only the histories given by the parents in few cases, but as far as we have observed parents are not wrong in exodeviation diagnosis most of the time although they can misdiagnose esodeviations frequently in the childhood period. Evaluation of stereoacuities using the Titmus stereotest can be considered another limitation since this test possesses some monocular clues.25 To prevent false positivity of stereoacuity, we routinely ask our patients whether they could see in depth or not during the testing procedure.
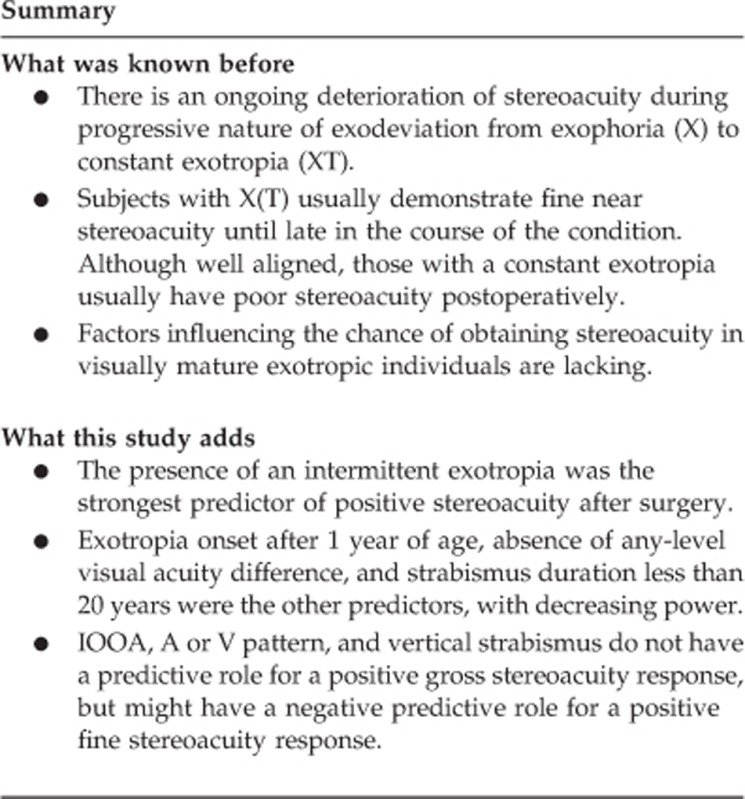
Conclusions
The presence of an intermittent exotropia was the strongest predictor of positive stereoacuity after surgery. Exotropia onset after 1 year of age, absence of any-level visual acuity difference and strabismus duration <20 years were the other predictors, with decreasing power. Other strabismus characteristics such as IOOA, A or V pattern, and vertical strabismus do not have a predictive role for a positive gross stereoacuity response, but might have a negative predictive role for a positive fine stereoacuity response. Further studies on larger series of patients are needed to better identify the role of strabismus characteristics on fine stereoacuity outcome.
Acknowledgments
We would like to thank our mentor Albert W Biglan for his invaluable contributions throughout this research. This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
The authors declare no conflict of interest.
References
- 1Jampolsky A, Scott A. Ocular deviations. Int Ophthal Clin 1964; 4: 567–579. [Google Scholar]
- 2Von Noorden GK, Campos EC. Exodeviations Lampert R, Cox K Binocular Vision and Ocular Motility. Mosby: St. Louis, 2002; 356–372. [Google Scholar]
- 3Hatt SR, Haggerty H, Buck D, Adams W, Strong NP, Clarke MP. Distance stereoacuity in intermittent exotropia. Br J Ophthalmol 2007; 91: 219–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4Yıldırım C, Mutlu FM, Chen Y, Altınsoy HI. Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol 1999; 128: 222–230. [DOI] [PubMed] [Google Scholar]
- 5Wu H, Sun J, Xia X, Xu L, Xu X. Binocular status after surgery for constant and intermittent exotropia. Am J Ophthalmol 2006; 142(5): 822–826. [DOI] [PubMed] [Google Scholar]
- 6Abroms AD, Mohney BG, Rush DP, Parks M, Tong PY. Timely surgery in intermittent and constant exotropia for superior sensory outcome. Am J Ophthalmol 2001; 131: 111–116. [DOI] [PubMed] [Google Scholar]
- 7Stathacopoulos RA, Rosenbaum AL, Zanoni D, Stager DR, McCall LC, Ziffer AJ et al. Distance stereoacuity: assessing control in intermittent exotropia. Ophthalmology 1993; 100: 495–500. [DOI] [PubMed] [Google Scholar]
- 8Tarannum F, Abadan KA, Saba S, Mohammad A. Gains beyond cosmesis: recovery of fusion and stereopsis in adults with longstanding strabismus following successful surgical realignment. Indian J Ophthalmol 2009; 57: 141–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9Lal G, Holmes JM. Postoperative stereoacuity following realignment for chronic acquired strabismus in adults. J AAPOS 2002; 6: 233–237. [DOI] [PubMed] [Google Scholar]
- 10Fawcett SL, Felius J, Stager DR. Predictive factors underlying the restoration of macular binocular vision in adults with acquired strabismus. J AAPOS 2004; 8: 439–444. [DOI] [PubMed] [Google Scholar]
- 11Fawcett SL, Stager DR Sr, Felius J. Factors influencing stereoacuity outcomes in adults with acquired strabismus. Am J Ophthalmol 2004; 138: 931–935. [DOI] [PubMed] [Google Scholar]
- 12Mets MB, Beauchamp C, Haldi BA. Binocularity following surgical correction of strabismus in adults. Trans Am Ophthalmol Soc 2003; 101: 201–208. [PMC free article] [PubMed] [Google Scholar]
- 13Currie ZI, Shipman T, Burke JP. Surgical correction of large-angle exotropia in adults. Eye 2003; 17: 334–339. [DOI] [PubMed] [Google Scholar]
- 14O.Neal TD, Rosenbaum AL, Stathacopoulos RA. Distance improvement in intermittent exotropic patients following strabismus surgery. J Pediatr Ophthalmol Strabismus 1995; 32: 353–357. [DOI] [PubMed] [Google Scholar]
- 15Peters ER, Archer SM. Long-standing, large–angle exotropia in adults. Am Orthopt J 2007; 57: 104–106. [DOI] [PubMed] [Google Scholar]
- 16Mohney BG, Holmes JM. An office- based scale for assessing control in intermittent exotropia. Strabismus 2006; 14: 147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17Fawcett SL, Wang Y, Birch EE. The critical period for susceptibility of human stereopsis. Invest Ophthalmol Vis Sci 2005; 46: 521–525. [DOI] [PubMed] [Google Scholar]
- 18Birch EE, Salomao S. Infant random dot stereoacuity cards. J Pediatr Ophthalmol Strabismus 1998; 35: 86–90. [DOI] [PubMed] [Google Scholar]
- 19Choi YM, Kim SH. Comparison of clinical features between two different types of exotropia before 12 months of age based on stereopsis outcome. Ophthalmology 2013; 120: 3–7. [DOI] [PubMed] [Google Scholar]
- 20Wilson ME, Parks MM. Primary inferior oblique overaction in congenital esotropia, accommodative esotropia, and intermittent exotropia. Ophthalmology 1989; 96: 950–957. [DOI] [PubMed] [Google Scholar]
- 21Leske DA, Holmes JM. Maximum angle of horizontal strabismus consistent with true stereopsis. J AAPOS 2004; 8: 28–34. [DOI] [PubMed] [Google Scholar]
- 22Odell NV, Hatt SR, Leske DA, Adams WE, Holmes JM. The effect of induced monocular blur on measures of stereoacuity. J AAPOS 2009; 13: 136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23Von Noorden GK, Campos EC. Binocular vision and space perception Lampert R, Cox K Binocular Vision and Ocular Motility. 6th ed. Mosby: St Louis, 2002, pp 7–35. [Google Scholar]
- 24Wallace DK, Lazar EL, Melie M, Birch EE, Holmes JM, Hopkins KB et alon behalf of the Pediatric Eye Disease Investigator Group. Stereoacuity in children with anisometropic amblyopia. J AAPOS 2011; 15: 455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25Morrison D, McSwain W, Donahue S. Comparison of sensory outcomes in patients with monofixation versus bifoveal fusion after surgery for intermittent exotropia. J AAPOS 2010; 14: 47–51. [DOI] [PubMed] [Google Scholar]


